Abstract
Healthcare-associated infection is one of the most common and severe threats to patients’ health and remains a significant challenge for healthcare providers. Among healthcare-associated infections, urinary tract infection (UTI) is one of the most common infections. This study aimed to determine the global incidence of UTI among patients. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guideline was used to perform this systematic review and meta-analysis. The articles were searched from April 4 to August 5, 2022, from electronic databases (Scopus, PubMed, Web of Science, Google Scholar, DOAJ, and MedNar) using Boolean logic operators, MeSH terms, and keywords. The quality of the study was assessed using the JBI Critical Assessment tool. One thousand nine ninety three articles were retrieved from the electronic databases, of which 38 articles conducted on 981 221 patients were included in the current study. The study found the global pooled incidence of UTI accounted for 1.6%. Based on the subgroup analysis by survey period and WHO region, the highest incidence of UTI was reported in the African Region [3.6%] and among studies conducted between 1996 and 2001 [3.7%]. This study revealed the overall pooled incidence of UTI was 1.6%. The highest incidence of UTI (3.6%) was reported in the African region. This indicates that there is a need to implement safety measures.
Keywords: hospital acquired infection, nosocomial infection, urinary tract infection, healthcare associated infection, patient, patient safety, global
What do we already know about this topic?
• Urinary Tract Infection (UTI) is one of the most common infections in healthcare facilities.
• It remains a major cause of morbidity and mortality globally and is one of the most common infections in healthcare facilities.
• Until the current study was conducted, there was no study that provided a global and WHO’s region incidence of UTI.
How does your research contribute to the field?
• This study revealed that the overall pooled incidence of UTI was 1.6%.
• Based on the world health organizations’ region, UTI incidence estimates was high in African region [3.6%].
What are your research’s implications toward theory, practice, or policy?
• The finding of the current study can be used by national and international concerned agencies or organizations to take appropriate prevention measures and for planning and implementing effective UTI prevention and control programs, as well as other nosocomial infections which can contribute to better health service provision across the world.
Introduction
Healthcare-associated infections (HAI) pose one of the most severe threats to patients’ health and remain a major challenge for healthcare service providers globally.1,2 These infections are mainly caused by antimicrobial-resistant microorganisms. 3 HAI is the major cause of morbidity and mortality.4-6 which is associated with clinical, diagnostic, and therapeutic procedures.7,8
Despite the fact that there is no accurate data available, it is estimated that hundreds of millions of patients are affected by HAIs each year. Not only does this result in significant mortality, but it also results in service or financial losses for healthcare systems. Currently, there are no countries free from the HAI burden and antimicrobial resistance. 3
Furthermore, approximately 3 million healthcare professionals around the world are affected by HAI every year. 9 Among HAI, Urinary tract infection (UTI) is the most commonly encountered hospital-acquired infection and the major risk factor is urinary catheterization. 10 UTI is one of the most common bacterial infections and also it may be an emerging problem in patient in different parts of the world with high medical costs.11,12 Bacterial adherence to uroepithelial cells is essential for the initiation of infection in UTI. Pathogenic Escherichia coli is regarded as the main cause of nosocomial infections, including UTIs. 13 UTI account for more than 30% of HAIs reported by acute care hospitals. 14 UTI is considered the most common HAI, 15 accounting for up to 36% of all HAIs. 16
Similarly, among UTI, catheter-associated urinary tract infections (CA-UTIs) represent the majority of UTI accounting for up to 67% of UTIs in all hospital inpatients. 17 It is the most common nosocomial infection, accounting for up to 10% to 70% of all nosocomial infections.18,19 It is caused by instrumentation of the urinary tract with 80% traced to the use of indwelling urinary catheters. 20 CA-UTI is a serious health condition, which is associated with reduced quality of life, increased risk of hospitalization, and increased mortality. 21
Besides these problems, there is limited evidence regarding the global incidence of UTI. Some of the previous systematic reviews and meta-analysis conducted on lower urinary tract symptoms suggestive of benign prostatic hyperplasia, 22 factor associated with UTI,23,24 region specific, 25 and pathogenic and ward specific.26,27
Therefore, the aim of this systematic review and meta-analysis was to assess and estimate the regional and global incidence of UTI among patients. It can be used by both national and international concerned agencies or organizations to take appropriate prevention measures and for planning and implementing effective UTI prevention and control programs, which can contribute to better health service provision across the world.
Protocol
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guideline was used to perform this systematic review and meta-analysis. 28
Eligibility Criteria
Inclusion criteria
The studies that met the following inclusion criteria were included in the systematic review and meta-analysis:-
Study population: Patients admitted to the health facility were a study population.
Outcomes: The study reported a quantitative outcome (magnitude, frequency, rate, or incidence of urinary tract infection).
Language: Articles written in English.
Types of articles: Peer-reviewed full text, original, and published articles.
Publication year: Articles conducted anytime (not limited).
Study regions or countries: Not specified (not limited).
Exclusion criteria
The study did not report quantitative outcomes, case series, review articles, reports, conference abstracts, opinions, articles written in non-English, high risk of bias articles, and articles not available in full text were excluded from the current study.
Information Sources and Search Strategy
The articles were searched from SCOPUS, PubMed, Web of Science, Google Scholar, DOAJ, and MedNar, from April 4 to August 5, 2022. A combination of Boolean logic operators (AND, OR, and NOT), Medical Subject Headings (MeSH), and keywords (healthcare facility, nosocomial infection, urinary tract infection, patients, hospital acquired infection, healthcare associated infection) were used to retrieve the articles from the identified databases. The main keywords and index terms were checked across the included databases. Finally, references within eligible articles were further screened for additional articles.
The following search term was used in the initial searching of the articles from PubMed:- “incidence” [Mesh Terms] OR “incidence” [All Fields]) OR “Incidence” [Mesh Terms] OR “Incidence” [All Fields]) OR “Proportion” [Mesh Terms] OR “Proportion” [All Fields]) AND ((“Nosocomial” [Mesh Terms] OR “Nosocomial” [All Fields], OR “Hospital Acquired” [All Fields] OR “Hospital Acquired” [Mesh]) OR ((“Health Facility” [Mesh Terms] OR “Health Facility” [All Fields], OR “Healthcare Facility” [All Fields] OR “Healthcare Facility” [Mesh]) OR “ urinary tract infection” [All Fields] OR “Urinary tract Infection” AND ((“Infection” [Mesh Terms]] OR (“Disease” [All Fields] OR “Problems” [All Fields] OR “Hazards” [Mesh]) AND “Patient” [All Fields]) [Mesh]) OR “Patients” [All Fields]) OR “Service Users” [All Fields]) AND (“Developing Country” [Mesh Terms] OR “Developing Countries” [All Fields]) OR “Developed Countries” [Mesh Terms] OR (“Developed” [All Fields] AND “Countries” [All Fields]) OR “Developed Countries”[All Fields])).
Study Selection Process
The study selection process was performed using the PRISMA flow chart, indicating the number of articles included in the study and excluded from the study with the reasons of exclusion. Following the search for articles through the included electronic databases, duplicate articles were removed using the ENDNOTE software version X5 (Thomson Reuters, USA).
After duplicated articles were removed, the authors (DAM, AA, AA, AM, BM, and FA) independently screened the articles based on their titles and abstracts to determine their eligibility for the current study by applying the inclusion criteria. The authors (DAM, AA, AA, AM, BM, and FA) further evaluated the full texts of the relevant articles independently. Any disagreements made with respect to the inclusion of studies were resolved by consensus after discussion. Finally, studies that met the inclusion criteria were included in the current study.
Data Extraction Process
All authors (DAM, AA, AA, AM, BM, and FA) independently extracted the relevant data required for the current study from the included or eligible articles. To extract the data, a predetermined Microsoft Excel format consisting of study characteristics, including publication year, survey year or study period, country where the study was conducted, sample size, and primary outcomes, such as incidence of UTI among the patients. Any disagreement made regarding the data extraction was resolved through discussion.
Quality Assessment
The included articles were subjected to quality assessment by the authors (DAM, AA, AA, AM, BM, and FA) using Joanna Briggs Institute Critical Assessment Tools (JBI) for the incidence studies. 29 Then, they were evaluated by the authors (DAM, AA, AA, AM, BM, and FA) to confirm their relevance or eligibility to the current study.
The JBI critical appraisal tools have 9 evaluation criteria: (1) appropriate sampling frame; (2) proper sampling technique; (3) adequate sample size; (4) description of the study subject and setting description; (5) sufficient data analysis; (6) use of valid methods for the identified conditions; (7) valid measurement for all participants; (8) use of appropriate statistical analysis; and (9) adequate response rate. Then, each parameter was assigned a value 1 if “Yes” and 0 if “No.” Based on the total score, each article was graded as high quality (85% and above), moderate (60%-85% score), or low quality (60% score). Finally, the articles having a moderate and high quality were included in the study.
Disagreement was made between the authors, regarding the quality assessment was solved by discussion after repeating the same procedures.
Statistical Procedures and Data Analysis
A systematic review and meta-analysis were used to summarize data on UTI by pooling together the findings of studies reporting the incidence of UTI globally. The pooled incidence of UTI among patients was determined using Comprehensive Meta-Analysis version 3.0 statistical software. The pooled incidence of UTI among patients in the healthcare facility was visualized using a forest plot and a random-effects model.
The I-squared test (I2 statistics) was used to evaluate the heterogeneity between the included articles. The level of heterogeneity was then classified as no heterogeneity (0%), low (25%-50%), moderate (50%-75%), and high heterogeneity (>75%). 30 A random-effects model was used to analyze and report the data. Furthermore, subgroup analysis was conducted based on survey period, WHO region, and study areas/regions.
A sensitivity analysis was done to determine differences in pooled effects by dropping studies that were found to influence the summary estimates.
Results
Study Selection
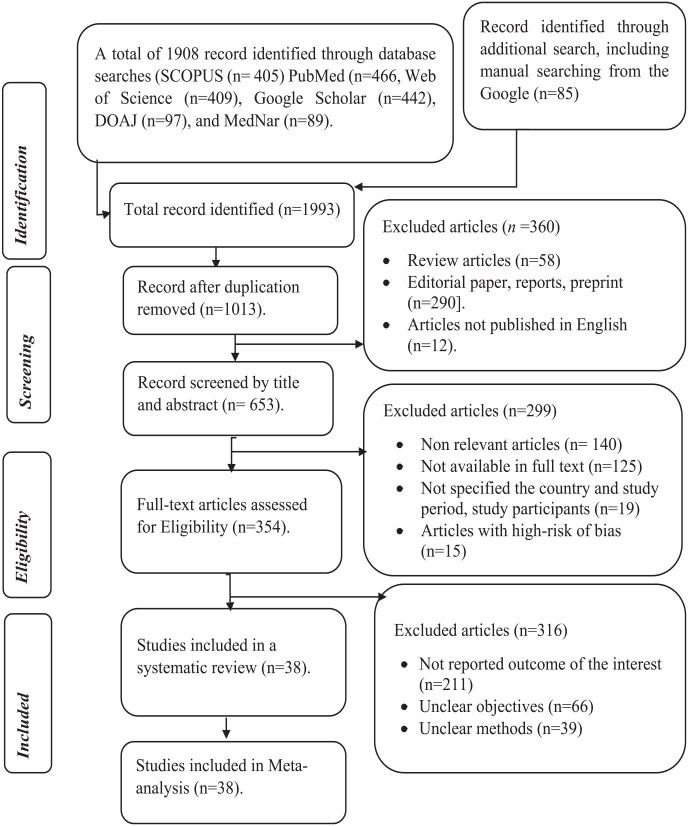
A total of 1993 articles were retrieved from the included electronic databases and manual searches from Google. Then, 980 duplicate articles were excluded. Out of 1013 articles, 360 were excluded after the evaluation was made based on titles and abstracts. Furthermore, 653 full-text studies were further assessed to determine their eligibility, of which 299 studies were excluded. Furthermore, 554 were evaluated based on the objective, methods, and outcome of interest by reading all contents of the articles. Finally, a total of 38 articles were included in the systematic review and meta-analysis (Figure 1).
Figure 1.
Study selection process of included articles for systematic review and meta-analysis, 2022.
Study Characteristics
This systematic review and meta-analysis included a total of 38 studies conducted on 981,221 patients (ranging from 105 31 to 633 990 32 study participants). Among the included studies, 7 were conducted in China,32-38 2 in each Switzerland,39,40 USA,41,42 Turkey,43,44 Iran,45,46 Italy,47,48 and Poland.49,50 However, one articles were selected from each Benin, 51 France, 52 Cuba, 53 Thailand, 54 Albania, 55 Malawi, 31 Saudi Arabia, 56 Ghana, 57 Argentina, 58 Ethiopia, 59 Tunisia, 60 Belgium, 61 Nepal, 62 Kuwait, 63 Germany, 64 Australia, 65 Herzegovina, 66 India, 67 Cameroon 68 (Table 1).
Table 1.
Overall Characteristics of the Articles Included in the Systematic Review and Meta-Analysis, 2022.
| Ref. | Author/s | Sample size (N) | Survey year | Publication year | Outcome (incidence of UTI) | Country | Risk of bias |
|---|---|---|---|---|---|---|---|
| Pittet et al 39 | Pittet et al | 1349 | 1996 | 1999 | 2.89 | Switzerland | Moderate |
| Ahoyo et al 51 | Ahoyo et al | 3130 | 2012 | 2014 | 11.1 | Benin | Moderate |
| Girard et al 52 | Girard et al | 286 | 2001 | 2006 | 7.69 | France | Moderate |
| Esen and Leblebicioglu 43 | Esen and Leblebicioglu | 236 | 2004 | 2001 | 15.68 | Turkey | Moderate |
| Izquierdo-Cubas et al 53 | Izquierdo-Cubas et al | 4240 | 2004 | 2008 | 0.5 | Cuba | Moderate |
| Danchaivijitr et al 54 | Danchaivijitr et al | 9865 | 2006 | 2007 | 1.6 | Thailand | Moderate |
| Faria et al 55 | Faria et al | 968 | 2003 | 2007 | 6.3 | Albania | Low |
| Nash et al 41 | Nash et al | 11 879 | 2006 | 2011 | 6.0 | USA | Low |
| Bunduki et al 31 | Bunduki et al | 105 | 2020 | 2021 | 3.81 | Malawi | Low |
| Huang et al 33 | Huang et al | 6717 | 2014-2018 | 2020 | 0.19 | China | Low |
| Balkhy et al 56 | Balkhy et al | 562 | 2003 | 2006 | 1.96 | Saudi Arabia | Low |
| Labi et al 57 | Labi et al | 2107 | 2016 | 2019 | 1.61 | Ghana | Low |
| Askarian et al 45 | Askarian et al | 3450 | 2008-2009 | 2012 | 1.4 | Iran | Low |
| Zotti et al 47 | Zotti et al | 9467 | 2000 | 2004 | 4.5 | Italy | Moderate |
| Gentili et al 48 | Gentili et al | 6263 | 2013-2018 | 2020 | 1.07 | Italy | Low |
| Durlach et al 58 | Durlach et al | 4249 | 2008 | 2012 | 3.1 | Argentina | Low |
| Mühlemann et al 40 | Miihlemann et al | 520 | 2000 | 2004 | 1.35 | Switzerland | Moderate |
| Lee et al 34 | Lee et al | 1021 | 2005 | 2006 | 0.8 | China | Low |
| Motbainor et al 59 | Motbainor et al | 238 | 2018 | 2020 | 2.1 | Ethiopia | Low |
| Strasheim et al 69 | Zhao et al | 134 637 | 2015-2017 | 2020 | 0.23 | China | Low |
| Kołpa et al 49 | Kołpa et al | 1849 | 2016-2017 | 2018 | 2.9 | Poland | Low |
| Ghali et al 60 | Ghali et al | 2729 | 2012-2020 | 2021 | 2.27 | Tunisia | Low |
| Vandael et al 61 | Vandael et al | 11 800 | 2017 | 2020 | 1.65 | Belgium | Low |
| Shrestha et al 62 | Shrestha et al | 300 | 2016 | 2020 | 16.0 | Nepal | Low |
| Alfouzan et al 63 | Alfouzan et al | 1408 | 2018-2019 | 2021 | 0.97 | Kuwait | Low |
| Magill et al 42 | Magill et al | 851 | 2009 | 2012 | 1.06 | USA | Moderate |
| Arefian et al 64 | Arefian et al | 62 154 | 2011-2014 | 2019 | 0.76 | Germany | Low |
| Russo et al 65 | Russo et al | 2767 | 2018 | 2019 | 2.4 | Australia | Low |
| Zhang et al 36 | Zhang et al | 4029 | 2012-2014 | 2016 | 0.52 | China | Low |
| Zhang et al 32 | Zhang et al | 633 990 | 2013-2017 | 2019 | 0.47 | China | Low |
| Isikgoz Tasbakan et al 44 | Tasbakan et al | 26 534 | 2011 | 2008-2013 | 1.82 | Turkey | Low |
| Custovic et al 66 | Custovic et al | 834 | 2010 | 2014 | 1.8 | Herzegovina | Moderate |
| Wang et al 37 | Wang et al | 1347 | 2013-2015 | 2019 | 2.0 | China | Low |
| Jiang et al 38 | Jiang et al | 13 695 | 2013-2019 | 2020 | 0.28 | China | Low |
| Heydarpour et al 46 | Heydarpou et al | 6000 | 2011-2014 | 2017 | 0.22 | Iran | Moderate |
| Sahu et al 67 | Sahu et al | 6864 | 2013-2014 | 2016 | 0.32 | India | Low |
| Nouetchognou et al 68 | Nouetchognou et al | 307 | 2013-2014 | 2016 | 3.91 | Cameroon | Low |
| Tomczyk-Warunek et al 50 | Tomczyk-Warunek et al | 2474 | 2018-2020 | 2021 | 1.25 | Poland | Low |
N = sample size; UTI = urinary tract infection; USA = United State of America.
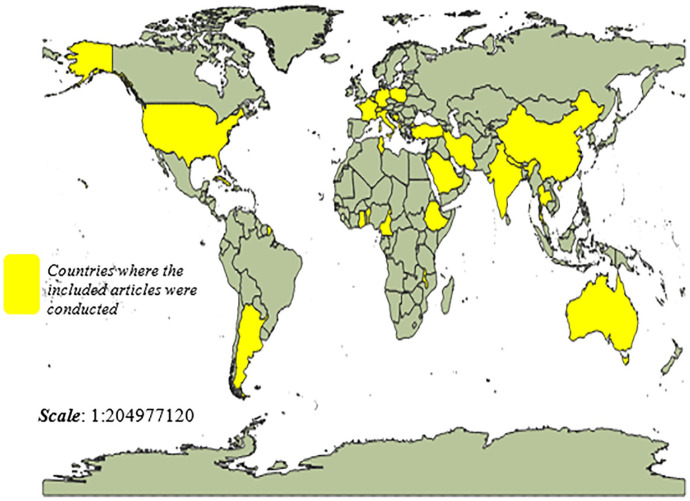
Based on the region, the majority of the studies were conducted in developing countries. In general, the included articles were conducted in 26 countries around the world. The yellow color on the map indicated the countries where the included articles were conducted (Figure 2).
Figure 2.
Countries of the world where the included articles were conducted.
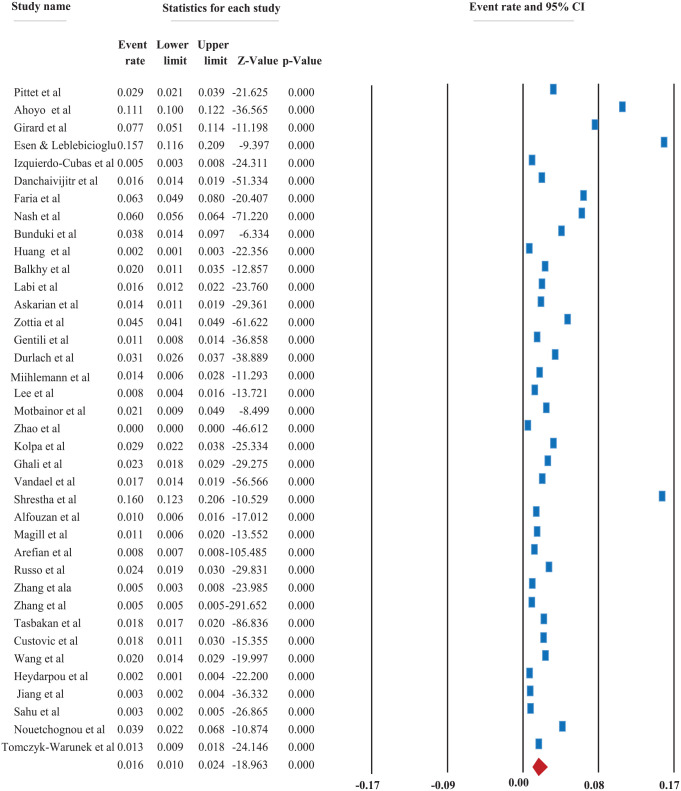
Incidence of Urinary Tract Infections
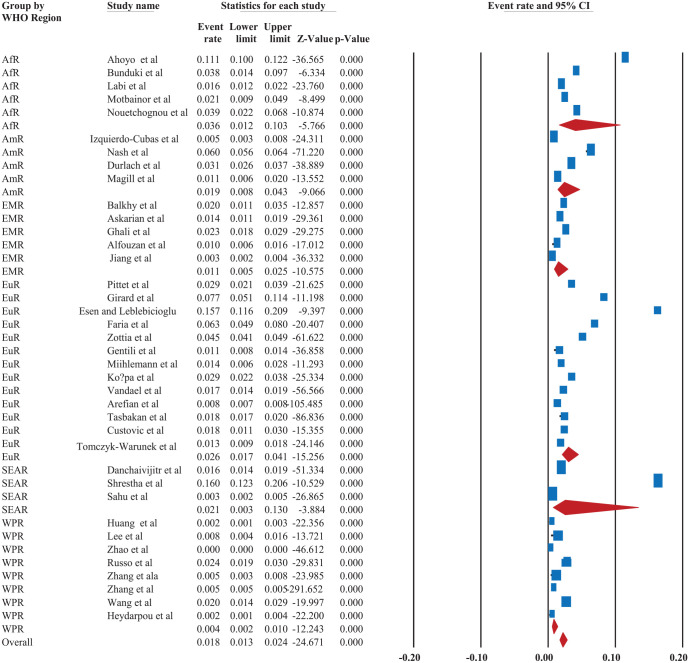
The worldwide incidence of UTI among patients was found to be 1.6% (95% CI: 1.0, 2.4) with a p-value of <.001; I2 = 79.02 (Figure 3).
Figure 3.
The forest plot shows an overall pooled incidence of urinary tract infections among patients, 2022.
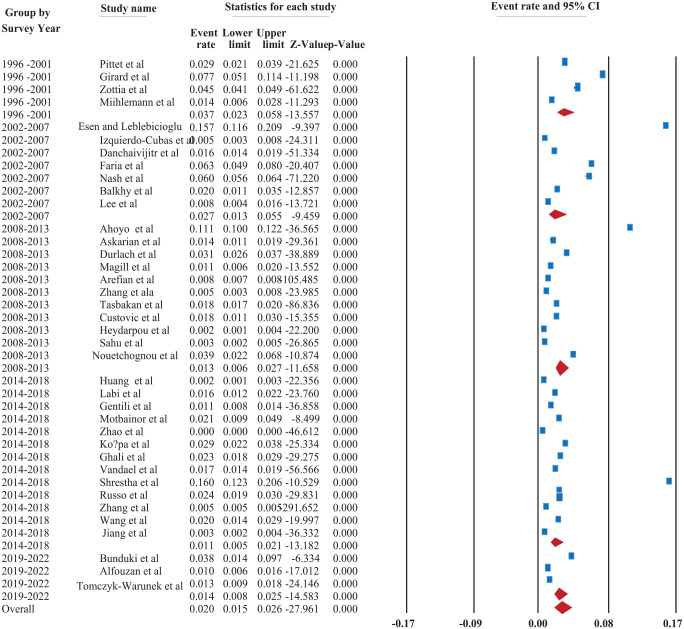
Based on subgroup analysis by survey year, studies conducted between 2014 and 218 had the lowest incidence of UTI among patients [1.1% (95% CI: 0.5, 2.1)], while studies conducted between 1996 and 2001 had the highest [3.7% (95% CI: 2.3, 5.8)]. The results of the current finding indicated that the incidence of UTI was declining from 3.7% (1996-2001) to 1.4% (2019-2022) (Figure 4).
Figure 4.
The forest plot shows the subgroup analysis of the pooled incidence of urinary tract infections among patients based on the survey period, 2022.
Based on the World Health Organization Region, the overall pooled incidence of UTI was 1.8% [95% CI: 1.3, 2.4] that was slightly lower than the pooled prevalence before subgroup analysis (1.6%).
The highest incidence of UTI was reported in the African Region, which accounted for 3.6% [95% CI: 1.2, 10.3], whereas the lowest incidence was reported in the Western Pacific Region, at 0.4% [95% CI: 0.2, 1.0] followed by Eastern Mediterranean Region and American region accounted for 1.1% [95% CI: 0.5, 2.5] and 1.9% [95% CI: 0.8, 4.3], respectively (Figure 5).
Figure 5.
The forest plot shows the subgroup analysis of the pooled incidence of urinary tract infections among patients based on World Health Organization’s Region of the world, 2022. ArR = African Region; AmR = American Region; EMR = Eastern Mediterranean Region; SEAR = South East Asian Region; WPR = Western Pacific Region; EuR = European Region.
Sensitivity Analysis Results
The sensitivity analysis was conducted by dropping the outcomes of samples expected to influence the pooled incidence of urinary tract infection. However, no substantial difference was observed in the incidence of urinary tract infection among patients (Table 2).
Table 2.
Sensitivity Analysis Based on Sample Size and Study Outcomes Expected to Effect the Pooled incidence of Urinary Tract Infection.
| Criteria | Pooled incidence | P-value |
|---|---|---|
| After dropping one lowest outcome | 1.8 (95% CI: 1.2, 2.7) | <.001 |
| After dropping one small sample size | 1.5 (95% CI: 1.0, 2.4) | <.001 |
| After dropping three largest outcomes | 1.3 (95% CI: 0.9, 1.9) | <.001 |
| After dropping two largest sample size | 1.7 (95% CI: 1.2, 2.4) | <.001 |
Discussion
Urinary tract infection were considered the most common healthcare-associated infection, 15 accounting for up to 36% of healthcare-associated infections. 16 Urinary tract infection is a serious health condition, which is associated with reduced quality of life, increased risk of hospitalization and increased mortality. 21 To determine the pooled incidence of urinary tract infection, the current study included 38 articles conducted on 981 221 patients (ranged from 105 31 to 633 990 32 study participants).
According to the current finding, the worldwide incidence of urinary tract infection among patients was found to be 1.6% (95% CI: 1.0, 2.4). The current study found a lower incidence of urinary tract infection compared to another study reporting a incidence rate of 9.33%. 24 The variation may be attributed to the scope of the study, the number of included articles, and study participants involved. Because, the latter study included 10 articles with a total of 8785 study participants with or without urinary tract infection.
Based on the subgroup analysis of the findings based on the survey period, the results of the current finding indicated that the incidence of urinary tract infection was declining from 3.7% (1996-2001) to 1.4% (2019-2022) (Figure 4).
After the findings were analyzed based on the survey year or period, the incidence of urinary tract infection was declined from 3.7% (1996-2001) to 1.1% (2014-2018). However, it was slightly increased from 1.1% (1996-2001) to 1.4% (2019-2022). The variation may be attributed to the number of studies included. Because, only 3 studies conducted from 2019 to 2022 in a few countries and met the eligible criteria were included in this study. Similarly, it may be related to the application of safety measures, including training and appropriate interventions or programs.
Furthermore, to compare the findings based on the World Health Organization regions’ of the world and determine the difference in outcomes, the highest incidence [3.6% (95% CI: 1.2, 10.3)] of urinary tract infection was reported in the African Region. This can be attributed to the fact that there is poor implementation of patient’s safety measures, including adequate interventions, training, precautions, or policy in developing countries, including African Regions. This indicates that the appropriate action should be taken by prioritizing the problems to improve the safety and service provision.
Furthermore, the study revealed that the lowest incidence of urinary tract infection was observed in Western Pacific Region accounted for 0.4%, followed by Eastern Mediterranean Region and American region accounted for 1.1% [95% CI: 0.5, 2.5] and 1.9% [95% CI: 0.8, 4.3]. The variation may be related to the variation in the scope of the studies, the infection reporting system, or surveillance system of the included countries as well as variations in the implementation of safety practices in the health facilities.
In general, the current study revealed that there is a variation incidence of urinary tract infection across the world, with the highest incidence reported in African regions. The finding indicates that there is a need to implement safety measures, particularly in low and middle-income countries such as the African Region, to maintain the health and safety of patients. Furthermore, strengthening the healthcare systems and of the countries in the World Health Organization’s African region is of paramount importance and can be achieved by educating and providing training to healthcare providers to enhance their skills. 70
Strength and Limitations
The current study employed multiple search strategies and standard tools for quality assessment and evaluation tools to reduce bias. This study included studies conducted at any time and all over the world. Furthermore, this study was conducted based on the PRISMA protocol.
However, there was an unequal distribution of the studies across the world as a result of limited articles. Furthermore, the incidence of urinary tract infection in many countries of the world were not included because of the lack of studies that met the eligibility criteria. The differences in the surveillance systems may lead to variation in incidence of UTI. As a result of variation in the unit of measurement employed, the authors could not able to determine the risk factors associated with the incidence of urinary tract infection. Furthermore, as a result of limited studies (systematic review and meta-analysis) conducted on the incidence of urinary tract infection, we can’t able to compare the current findings with other findings adequately.
Conclusions
This study revealed the overall pooled incidence of urinary tract infection was 1.6%. Urinary tract infection estimates varied among the WHO’s region of the world. However, the highest incidence was observed in African regions, which accounted for 3.7%. This indicates that there is a need to implement safety measures, including interventions for urinary tract infection to reduce the health affect posed by urinary tract infection and to improve patient safety.
Footnotes
Authors’ Contributions: DAM conceived the idea and had a major role in the review, extraction, and analysis of the data, writing, drafting, and editing of the manuscript. AA, AA, AM, BM, and FA have contributed to data extraction, analysis, and editing. Finally, the authors (DAM, AA, AA, AM, BM, and FA) read and approved the final version of the manuscript to be published and agreed on all aspects of this work.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval and Consent to Participate: Not applicable.
Consent for Publication: Not applicable.
Data Availability: Almost all data are included in this study. However, some data may be available from the corresponding authors on reasonable request.
ORCID iDs: Dechasa Adare Mengistu  https://orcid.org/0000-0002-0076-5586
https://orcid.org/0000-0002-0076-5586
Abdi Amin Abdukadir  https://orcid.org/0000-0002-0539-4059
https://orcid.org/0000-0002-0539-4059
References
- 1.World Health Organization (WHO). Report on the burden of endemic health care-associated infection worldwide. World Health Organization. 2011. Accessed February 30, 2021. http://apps.who.int/iris/bitstream/10665/80135/1/9789241501507_eng.pdf [Google Scholar]
- 2.Auta A, Adewuyi EO, Tor-Anyiin A, et al. Global prevalence of percutaneous injuries among healthcare workers: a systematic review and meta-analysis. Int J Epidemiol. 2018;47(6):1972-1980. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO). Global guidelines on the prevention of surgical site infection, 2016. Accessed November 26, 2021. https://apps.who.int/iris/bitstream/handle/10665/250680/9789241549882-eng.pdf?sequence=8 [PubMed]
- 4.World Health Organization. Prévention des infections nosocomiales: guide pratique. Organisation mondiale de la Santé. 2008. [Google Scholar]
- 5.Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM.CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16(3):128-140. [DOI] [PubMed] [Google Scholar]
- 6.Jarvis WR.Selected aspects of the socioeconomic impact of nosocomial infections: morbidity, mortality, cost, and prevention. Infect Control Hosp Epidemiol. 1996;17(8):552-557. [DOI] [PubMed] [Google Scholar]
- 7.Promotion OoDPaH. Why are healthcare-associated infections important? 2020. Accessed January 11, 2022. https://www.healthypeople.gov/2020/topics-objectives/topic/healthcareassociated-infections%0AGoal
- 8.Prevention CfDCa. Healthcare-Associated Infections (HAIs). 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/healthcare-associated-infections%0AGoal
- 9.World Health Organization ROfS-EAaR PO. Infection control practices. SEARO Regional Publication. 2004. [Google Scholar]
- 10.Trautner BW.Management of catheter-associated urinary tract infection. Curr Opin Infect Dis. 2010;23(1):76-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mohajeri P, Darfarin G, Farahani A.Genotyping of ESBL producing Uropathogenic Escherichia coli in west of Iran. Int J Microbiol. 2014;2014:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Melzer M, Petersen I.Mortality following bacteraemic infection caused by extended spectrum beta-lactamase (ESBL) producing E. coli compared to non-ESBL producing E. coli. Infect J. 2007;55(3):254-259. [DOI] [PubMed] [Google Scholar]
- 13.FarajzadehSheikh A, Veisi H, Shahin M, Getso M, Farahani A.Frequency of quinolone resistance genes among extended-spectrum β-lactamase (ESBL)-producing Escherichia coli strains isolated from urinary tract infections. Trop Med Health. 2019;47(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA.Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31(4):319-326. [DOI] [PubMed] [Google Scholar]
- 15.Meddings J, Rogers MAM, Krein SL, Fakih MG, Olmsted RN, Saint S.Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: an integrative review. BMJ Qual Saf. 2014;23(4):277-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allegranzi Nejad B, Castillejos G, Kilpatrick CK, Mathai E.Report on the burden of endemic health care-associated infection worldwide: A systematic review of the literature. World Health Organization. 2011. http://apps.who.int/iris/bitstream/10665/80135/1/9789241501507eng.pdf [Google Scholar]
- 17.Magill SS, Edwards JR, Bamberg W, et al. Multistate point-prevalence survey of health care–associated infections. New Engl J Med. 2014;370(13):1198-1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elvy J, Colville A.Catheter associated urinary tract infection: what is it, what causes it and how can we prevent it? J Infect Prev. 2009;10(2):36-41. [Google Scholar]
- 19.Waskiewicz A, Alexis O, Cross D.Supporting patients with long-term catheterisation to reduce risk of catheter-associated urinary tract infection. Br J Nurs. 2019;28(9):S4-S17. [DOI] [PubMed] [Google Scholar]
- 20.Kwak YG, Choi JY, Yoo H, et al. Korean nosocomial infections surveillance system, Intensive Care Unit Module Report: Summary of data from July 2013 through June 2014. Korean J Nosocomial Infect Control. 2015;20(2):49-60. [Google Scholar]
- 21.Temiz E, Piskin N, Aydemir H, et al. Factors associated with catheter-associated urinary tract infections and the effects of other concomitant nosocomial infections in intensive care units. Scand J Infect Dis. 2012;44(5):344-349. [DOI] [PubMed] [Google Scholar]
- 22.Lee SWH, Chan EMC, Lai YK. The global burden of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: a systematic review and meta-analysis. Sci Rep. 2017;7(1):1-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meddings J, Rogers M, Macy M, Saint S.Systematic review and meta-analysis: reminder systems to reduce catheter-associated urinary tract infections and urinary catheter use in hospitalized patients. Clin Infect Dis. 2010;51(5):550-560. [DOI] [PubMed] [Google Scholar]
- 24.Li F, Song M, Xu L, Deng B, Zhu S, Li X.Risk factors for catheter-associated urinary tract infection among hospitalized patients: a systematic review and meta-analysis of observational studies. J Adv Nurs. 2019;75(3):517-527. [DOI] [PubMed] [Google Scholar]
- 25.Ling ML, Apisarnthanarak A, Madriaga G.The burden of healthcare-associated infections in Southeast Asia: a systematic literature review and meta-analysis. Clin Infect Dis. 2015;60(11):1690-1699. [DOI] [PubMed] [Google Scholar]
- 26.Peng D, Li X, Liu P, et al. Epidemiology of pathogens and antimicrobial resistanceof catheter-associated urinary tract infections in intensivecare units: a systematic review and meta-analysis. Am J Infect Control. 2018;46(12):e81-e90. [DOI] [PubMed] [Google Scholar]
- 27.Bryce A, Hay AD, Lane IF, Thornton HV, Wootton M, Costelloe C.Global prevalence of antibiotic resistance in paediatric urinary tract infections caused by Escherichia coli and association with routine use of antibiotics in primary care: systematic review and meta-analysis. BMJ. 2016;i939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.JBI. The Joanna Briggs Institute. Critical appraisal tools for use in the JBI systematic reviews checklist for prevalence studies: The University of Adelaide. 2019. https://joannabriggs.org/sites/default/files/2019-05/JBI_Critical_AppraisalChecklist_for_Prevalence_Studies2017_0.pdf
- 30.Ades AE, Lu G, Higgins JPT. The interpretation of random-effects meta-analysis in decision models. Med Decis Making. 2005;25(6):646-654. [DOI] [PubMed] [Google Scholar]
- 31.Bunduki GK, Feasey N, Henrion MYR, Noah P, Musaya J.Healthcare-associated infections and antimicrobial use in surgical wards of a large urban central hospital in Blantyre, Malawi: a point prevalence survey. Infect Prev Pract. 2021;3(3):100163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang Y, Du M, Johnston JM, et al. Incidence of healthcare-associated infections in a tertiary hospital in Beijing, China: results from a real-time surveillance system. Antimicrob Resist Infect Control. 2019;8(1):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huang G, Huang Q, Zhang G, Jiang H, Lin Z.Point-prevalence surveys of hospital-acquired infections in a Chinese cancer hospital: from 2014 to 2018. J Infect Public Health. 2020;13(12):1981-1987. [DOI] [PubMed] [Google Scholar]
- 34.Lee MK, Chiu CS, Chow VC, Lam RK, Lai RW.Prevalence of hospital infection and antibiotic use at a university medical center in Hong Kong. J Hosp Infect. 2007;65(4):341-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhao X, Wang L, Wei N, et al. Epidemiological and clinical characteristics of healthcare-associated infection in elderly patients in a large Chinese tertiary hospital: a 3-year surveillance study. BMC Infect Dis. 2020;20(1):1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang Y, Zhang J, Wei D, Yang Z, Wang Y, Yao Z.Annual surveys for point-prevalence of healthcare-associated infection in a tertiary hospital in Beijing, China, 2012-2014. BMC Infect Dis. 2016;16(1):1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang L, Zhou KH, Chen W, Yu Y, Feng SF.Epidemiology and risk factors for nosocomial infection in the respiratory intensive care unit of a teaching hospital in China: a prospective surveillance during 2013 and 2015. BMC Infect Dis. 2019;19(1):145-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jiang AM, Liu N, Ali Said R, et al. Nosocomial infections ingastrointestinal cancer patients: bacterial profile, antibiotic resistance pattern, and prognostic factors. Cancer Manag Res. 2020;12(12):4969-4979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pittet D, Harbarth S, Ruef C, et al. Prevalence and risk factors for nosocomial infections in four university hospitals in Switzerland. Infect Control Hosp Epidemiol. 1999;20(1):37-42. [DOI] [PubMed] [Google Scholar]
- 40.Mühlemann K, Franzini C, Aebi C, et al. Prevalence of nosocomial infections in swiss children's hospitals. Infect Control Hosp Epidemiol. 2004;25(9):765-771. doi: 10.1086/502474 [DOI] [PubMed] [Google Scholar]
- 41.Nash MC, Strom JA, Pathak EB.Prevalence of major infections and adverse outcomes among hospitalized. ST-elevation myocardial infarction patients in Florida, 2006. BMC Cardiovasc Disord. 2011;11(1):69-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Magill SS, Hellinger W, Cohen J, et al. Prevalence of healthcare-associated infections in acute care hospitals in Jacksonville, florida. Infect Control Hosp Epidemiol. 2012;33(3):283-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Esen S, Leblebicioglu H; Study Group. Prevalence of nosocomial infections at intensive care units in Turkey: a multicentre 1-day point prevalence study. Scand J Infect Dis. 2004;36(2):144-148. [DOI] [PubMed] [Google Scholar]
- 44.Isikgoz Tasbakan M, Durusoy R, et al. Hospital-acquired urinary tract infection point prevalence in Turkey: differences in risk factors among patient groups. Ann Clin Microbiol Antimicrob. 2013;12(1):31-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Askarian M, Yadollahi M, Assadian O.Point prevalence and risk factors of hospital acquired infections in a cluster of university-affiliated hospitals in Shiraz, Iran. J Infect Public Health. 2012;5(2):169-176. [DOI] [PubMed] [Google Scholar]
- 46.Heydarpour F, Rahmani Y, Heydarpour B, Asadmobini A.Nosocomial infections and antibiotic resistance pattern in open-heart surgery patients at Imam Ali Hospital in Kermanshah, Iran. GMS Hyg Infect Control. 2017;12:Doc07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zotti CM, Messori Ioli G, Charrier L, et al. Hospital-acquired infections in Italy: a region wide prevalence study. J Hosp Infect. 2004;56(2):142-149. [DOI] [PubMed] [Google Scholar]
- 48.Gentili A, Di Pumpo M, La Milia DI, et al. A six-year point prevalence survey of healthcare-associated infections in an Italian teaching acute care hospital. Int J Environ Res Public Health. 2020;17(21):7724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kołpa M, Wałaszek M, Gniadek A, Wolak Z, Dobroś W.Incidence, microbiological profile and risk factors of healthcare-associated infections in intensive care units: a 10 year observation in a provincial hospital in southern Poland. Int J Environ Res Public Health. 2018;15(1):112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tomczyk-Warunek A, Blicharski T, Blicharski R, et al. Retrospective study of nosocomial infections in the orthopaedic and Rehabilitation Clinic of the Medical University of Lublin in the years 2018-2020. J Clin Med. 2021;10(14):3179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ahoyo TA, Bankolé HS, Adéoti FM, et al. Prevalence of nosocomial infections and anti-infective therapy in benin: results of the first nationwide survey in 2012. Antimicrob Resist Infect Control. 2014;3(1):17-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Girard R, Mazoyer MA, Plauchu MM, Rode G.High prevalence of nosocomial infections in rehabilitation units accounted for by urinary tract infections in patients with spinal cord injury. J Hosp Infect. 2006;62(4):473-479. [DOI] [PubMed] [Google Scholar]
- 53.Izquierdo-Cubas F, Zambrano A, Frómeta I, et al. National prevalence of nosocomial infections. cuba 2004. J Hosp Infect. 2008;68(3):234-240. [DOI] [PubMed] [Google Scholar]
- 54.Danchaivijitr S, Judaeng T, Sripalakij S, Naksawas K, Plipat T.Prevalence of nosocomial infection in Thailand 2006. J Med Assoc Thai. 2007;90(8):1524. [PubMed] [Google Scholar]
- 55.Faria S, Sodano L, Gjata A, et al. The first prevalence survey of nosocomial infections in the University Hospital Centre ‘Mother Teresa’ of Tirana, Albania. J Hosp Infect. 2007;65(3):244-250. [DOI] [PubMed] [Google Scholar]
- 56.Balkhy HH, Cunningham G, Chew FK, et al. Hospital- and community-acquired infections: a point prevalence and risk factors survey in a tertiary care center in Saudi Arabia. Int J Infect Dis. 2006;10(4):326-333. [DOI] [PubMed] [Google Scholar]
- 57.Labi AK, Obeng-Nkrumah N, Owusu E, et al. Multi-centre point-prevalence survey of hospital-acquired infections in Ghana. J Hosp Infect. 2019;101(1):60-68. [DOI] [PubMed] [Google Scholar]
- 58.Durlach R, McIlvenny G, Newcombe RG, et al. Prevalence survey of healthcare-associated infections in Argentina; comparison with England, Wales, Northern Ireland and South Africa. J Hosp Infect. 2012;80(3):217-223. [DOI] [PubMed] [Google Scholar]
- 59.Motbainor H, Bereded F, Mulu W.Multi-drug resistance of blood stream, urinary tract and surgical site nosocomial infections of Acinetobacter baumannii and Pseudomonas aeruginosa among patients hospitalized at felegehiwot referral hospital, Northwest Ethiopia: a cross-sectional study. BMC Infect Dis. 2020;20(1):92-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ghali H, Ben Cheikh A, Bhiri S, Khefacha S, Latiri HS, Ben Rejeb M.Trends of healthcare-associated infections in a Tuinisian University Hospital and impact of COVID-19 Pandemic. INQUIRY. 2021;58:00469580211067930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vandael E, Latour K, Goossens H, et al. Point prevalence survey of antimicrobial use and healthcare-associated infections in Belgian acute care hospitals: results of the Global-pps and ECDC-PPS 2017. Antimicrob Resist Infect Control. 2020;9(1):13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shrestha SK, Trotter A, Shrestha PK.Epidemiology and risk factors of healthcare-associated infections in critically ill patients in a Tertiary Care Teaching Hospital in Nepal: a prospective cohort study. Infect Dis Res Treat. 2022;15:11786337211071120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Alfouzan W, Dhar R, Abdo NM, Alali WQ, Rabaan AA.Epidemiology and microbiological profile of common healthcare associated infections among patients in the intensive care unit of a general hospital in Kuwait: a retrospective observational study. J Epidemiol Glob Health. 2021;11(3):302-309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Arefian H, Hagel S, Fischer D, et al. Estimating extra length of stay due to healthcare-associated infections before and after implementation of a hospital-wide infection control program. PLoS One. 2019;14(5):e0217159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Russo PL, Stewardson AJ, Cheng AC, Bucknall T, Mitchell BG.The prevalence of healthcare associated infections among adult inpatients at nineteen large Australian acute-care public hospitals: a point prevalence survey. Antimicrob Resist Infect Control. 2019;8(1):114-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Custovic A, Smajlovic J, Hadzic S, Ahmetagic S, Tihic N, Hadzagic H.Epidemiological surveillance of bacterial nosocomial infections in the surgical intensive care unit. Mater Sociomed. 2014;26(1):7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sahu M, Siddharth B, Choudhury A, et al. Incidence, microbiological profile of nosocomial infections, and their antibiotic resistance patterns in a high volume Cardiac Surgical Intensive Care Unit. Ann Card Anaesth. 2016;19(2):281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nouetchognou JS, Ateudjieu J, Jemea B, Mesumbe EN, Mbanya D.Surveillance of nosocomial infections in the Yaounde University Teaching Hospital, Cameroon. BMC Res Notes. 2016;9(1):505-508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Strasheim W, Kock MM, Ueckermann V, Hoosien E, Dreyer AW, Ehlers MM.Surveillance of catheter-related infections: the supplementary role of the microbiology laboratory. BMC Infect Dis. 2015;15(1):1-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Danwang C, Bigna JJ, Tochie JN, et al. Global incidence of surgical site infection after appendectomy: a systematic review and meta-analysis. BMJ Open. 2020;10(2):e034266. [DOI] [PMC free article] [PubMed] [Google Scholar]