ABSTRACT
Simulation has been shown to improve clinical learning outcomes, speed up the learning process and improve learner confidence, whilst initially taking pressure off busy clinical lists. The World Federation for Ultrasound in Medicine and Biology (WFUMB) state of the art paper on the use of simulators in ultrasound education introduces ultrasound simulation, its advantages and challenges. It describes different simulator types, including low and high-fidelity simulators, the requirements and technical aspects of simulators, followed by the clinical applications of ultrasound simulation. The paper discusses the role of ultrasound simulation in ultrasound clinical training, referencing established literature. Requirements for successful ultrasound simulation acceptance into educational structures are explored. Despite being in its infancy, ultrasound simulation already offers a wide range of training opportunities and likely holds the key to a broader point of care ultrasound education for medical students, practicing doctors, and other health care professionals. Despite the drawbacks of simulation, there are also many advantages, which are expanding rapidly as the technology evolves.
Keywords: Simulators, training, ultrasound
INTRODUCTION AND BACKGROUND
Unlike any other branch of medical imaging, there are unique challenges involved in learning how to safely use ultrasound equipment. Ultrasound practitioners must not only understand human anatomy, physiology, pathology, ultrasound image acquisition and “knobology” but also have the appropriate skills to perform the examination and the ability to integrate ultrasound findings into clinical decision-making. They must also possess the psychomotor skills for adequate hand-eye coordination to generate the ultrasound images.[1] After acquiring the essential anatomical, ultrasound physics and instrumentation knowledge, the traditional method for teaching ultrasound scanning and interpretation is hands-on training under the direct supervision and guidance of an instructor (tutor). While possible on a small scale, this method does not translate to an expanding workforce and mass training of new users simultaneously because many do not have access to qualified instructors.
This situation has been exacerbated by the expanding popularity of ultrasound as a result of technological developments and affordability, especially for point-of-care applications. Developments in hand held devices has seen ultrasound used by multiple clinical specialties throughout the world, not solely in medical imaging departments.
While lectures can be given to small or large groups of learners with little loss of impact other than lack of personal attention to questions, hands-on training is different. No effective multiplier for capable instructors exists, other than the use of less experienced instructors. The need for additional hands-on instructors existed even before the proliferation of point of care ultrasound (POCUS) but is now more pronounced than ever. This is further complicated by a need to scan a wide range of different pathologies in clinical training settings.
Whilst interpreting still images or cine clips of normal and abnormal findings is useful, actual scanning of different pathologies and body types in a clinical setting can be a challenge.
The severe acute respiratory syndrome coronavirus 2 pandemic has had a negative impact on ultrasound education and on medical education in general.[2,3] Coronavirus pandemic lockdowns and continued fear of corona virus disease 2019 (COVID-19) transmission have created many additional barriers to ultrasound education, most notably, preventing ultrasound learners from accessing clinical training sites for almost 2 years. The COVID-19 pandemic has also accelerated the need for training institutions to build in the flexibility to support remote instruction and ultrasound simulation.[4] Following other educational approaches such as teaching surgical procedures and advanced cardiac life support training for all staff in medical facilities, developers are now focused on creating physical models for ultrasound simulation.
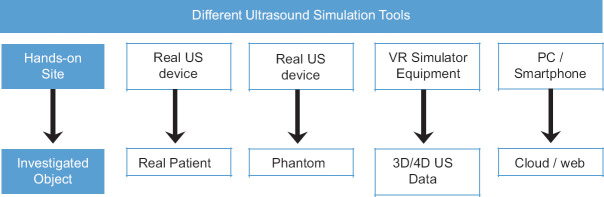
Simulation allows training in a safe environment without endangering actual patients or having to wait for a particular patient scenario to train on.[5,6] Physical simulators, or phantoms, were developed for both diagnostic and procedural practice, however they are limited in their educational value since most present normal anatomy or limited pathology. With the development of digital technologies, a new type of simulator has come into being: The digital or virtual simulator [Figure 1]. Each approach has advantages and disadvantages for leveraging available training data and various techniques.[7]
Figure 1.
General approach on ultrasound simulation tools. The distance to real world environment increases from left to right. Every simulation setting has its pros and cons and therefore different fields of application. US: Ultrasound; VR: Virtual reality; PC: Personal computer; 3D: 3-dimensional; 4D: 4-dimensional
Practical ultrasound training requires learning skill sets that apply to all clinical modalities, including the basic skills of how to adjust machine controls to optimize image quality and how to hold and manipulate the transducer.[8] The cognitive/psychomotor skills required to perform ultrasound are difficult to teach; rather they are developed by trial and error to effectively perform gross and fine motor skills, achieve self-efficacy and complete ultrasound examinations, thus making simulation the ideal learning tool.[8]
OVERVIEW OF SIMULATION TOOLS AND TECHNICAL ASPECTS
To achieve a systematic approach, it is crucial to understand the general differences of simulation-based settings [Figure 1]. Basically, there are two distinct simulation tools: Part-task trainers such as phantoms and animal models,[9] and full-task trainer such as virtual ultrasound simulators. A phantom is examined with an actual ultrasound device and probe. It can be self-made with, for example, foam, gelatin, or agar gel, or custom-made. Custom-madephantoms use similar acoustic velocity attributes as human tissue, such as silicone or might use animal parts such as porcine, chicken thighs or turkey breast.[10,11] The phantom replaces the body part e.g., abdomen, breast or fetus, with one specific pathology or training task. They can be referred to as low-fidelity simulators because of their static, nonchanging anatomy.[12] There are many different phantoms of single organs up to whole human bodies with several possible scanning areas. They are ideal for vascular simulation[13,14] or interventional training.[15]
A virtual ultrasound simulator is a stand-alone training system that does not use an actual ultrasound device. It uses mock probes or endoscopes and replaces the patient and the physical ultrasound image processing. In contrast to a physical phantom, the simulator can provide many different cases and is extendable by software updates. Some of the virtual ultrasound simulators even offer freehand puncture modules.
Pure web-or cloud-based simulators offer an alternative, less expensive simulation setting. They use a keyboard, mouse, or the smartphone touch display to navigate a virtual probe. Trainees can use them on their own personal computer (PC), tablet, or smartphone with or without Internet access.[16,17] Similar to playing computer games, there is a large difference when compared with real-time ultrasound scanning but these simulations enable the learner to improve their anatomical knowledge and hand-eye-coordination. Several online-interactive models or Applications (Apps) have been developed, but are often short-lived due to changing software-updates.
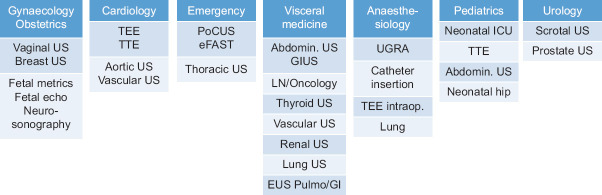
Virtual ultrasound simulators have an impressive diversity of technical components [Figure 2]. However, as there is no actual ultrasound system, it is not possible to compare different simulators by using technical parameters such as frequency, frame rate, or Doppler modes.
Figure 2.
Technical components of virtual ultrasound simulators - diversity of simulation settings. Components are assigned to four main groups (A-D) for better overview. See text for detailed explanations. 3D: 3-dimensional; US: Ultrasound; VR: Virtual reality; DOF: Degrees of freedom; PC: Personal computer
There are three different methods to simulate ultrasound images.[16]
Generative model-based simulation, or computer-generated virtual 3-dimensional (3D) artificial objects, are created by 3D artists with specialized software (e.g., blender). Via triangulation techniques, they firstly create surfaces of objects (data format.obj). Those interpretations lead to volumes (3D data). By modeling the anatomy, the desired organ is completely segmented into smaller and smaller volumes.[18,19] Finally, time series variations of these volumes result in animated 4-dimensional (4D) objects. These can be calculated by morphing flow techniques up to nearly endless resolution. This is especially suitable for small and uniformly moving organs such as the heart.[20] Regardless of the calculation effort, small gaps always remain in the end between distinct objects or organs. In this setting sometimes frames per second and spatial resolution may be stated as a result of very detailed animation. One drawback is that it is very difficult and time consuming to create different realistic pathologies. Further developments include the use of patient-specific pathological 3D-printed models for creating 3D/4D-objects or phantoms, particularly for cardiovascular and orthopedic diseases.[21,22]
Pseudo-ultrasound is generated by simulation from other imaging modalities such as computed tomography (CT) or magnetic resonance imaging (MRI). This so-called generative image-based simulation uses insonification, i.e., ultrasound wave propagation on 3D volumes from CT or MRI. These methods can more easily use real patient data with pathologies. Therefore, it is necessary to segment the CT and MRI images and assign them tissue properties.[23] Assumptions are made about ultrasound properties, such as reflection, transmission and attenuation, of the segmented structures based on the presumed relationship between CT Hounsfield units and ultrasound acoustic impedance.[16] There are no gaps between the organs, so that a continuum scan can be achieved. Depending on the simulation quality, it is possible to consider view-dependent artifacts. The genuine spatial resolution of CT and MRI limits the resolution of the simulated ultrasound images after transformation. Achieving the required level of detail can be challenging, particularly in abdominal ultrasound.
Real ultrasound 3D volumes from patients are used to simulate 2-dimensional (2D) ultrasound images. This so-called interpolation or interpolative simulation enables the highest realism. Complete original ultrasound data sets are acquired in the highest spatial resolution compared to CT/MRI, with different probe types and modes (B-mode, Doppler). View dependent effects such as artifacts or shadows cannot be simulated correctly, as they change with sonification angle. Therefore, the best images are simulated from a position similar to the original examination position (single volume). One solution is to record different viewpoints to gain several 3D volumes. Later it is possible to switch among them depending on the position of the probe (multiple volumes). Multiple volumes are ideal for complex pathologies, e.g., in abdominal ultrasound. Single volumes are useful for circumscribed clinical settings as vaginal ultrasound.[24] Volumes are often combined with feedback systems and input devices can track the learner’s activity.
Input devices describe the tracking of trainee’s activity. Tracking depends on the different hardware components used for example mock probes or endoscopes, mannequin models (not to be mixed up with the above-mentioned phantoms) or feedback systems. There are two common tracking methods: Electromagnetically and optical modes. Electromagnetic systems are the cheaper alternative, do not require free line of sight as optical systems do, and are mainly used for Apps, where the mock probe or endoscope has to be inserted into the patient/mannequin. They achieve poorer correlation to probe movements by the trainee (3–6 degrees of freedom [DOF]). In comparison optical tracking systems achieve higher volumes with 6-DOF probe tracking in the superior temporal and spatial resolution. They are more robust against interferences, especially when any nearby ferromagnetic material cannot be avoided (computer, metal, heating lights, etc.). Haptic feedback devices using pressure or vibration are a further alternative. Measurement of tool movements may lead to required corrections, triggering a feedback reaction via an induction motor. The tool has to be fixed for correct induction measurement (usually a joystick or mouse on a table). Therefore, these devices use only single volumes with <6-DOF and operate without a mannequin or phantom. This abstract setting can be a drawback but is suitable for simulation of interventional or invasive procedures (e.g., vaginal ultrasound). In contrast to all these settings, web-based systems do not operate in real time, with significantly <6-DOF stationary tools via graphic user interfaces (e.g., buttons and sliders).
The contents of the simulated database are of crucial importance when evaluating a simulator system. The database can be characterized according to the target group, e.g., the clinical specialty or different performance levels (students, sonographers, advanced users, etc.). A comparison of data quality is only possible within the same subgroup of simulation source (e.g., level of details in 3D simulation, quality of the original recording ultrasound device) [Figure 2]. Database quantity is especially important for different or rare pathologies, number of patients (with single or multiple pathologies) or several appointments of patients to evaluate disease progression. Finally, additional software can offer measurements, document individual learning progress or allow distinct training modules [Figure 2]. Some of the modern simulators combine virtual 3D animations with simulated ultrasound images, which to assist the trainee in visualizing the relationship between the probe position, the direction of the scan sector in the 3D organ’s anatomy, and the resulting 2D image.
Ultimately, the choice of simulation equipment should be aligned to the needs and demands of the users, the learning outcomes, clinical specialty and desired competency level, as well as operational considerations including financial capabilities.
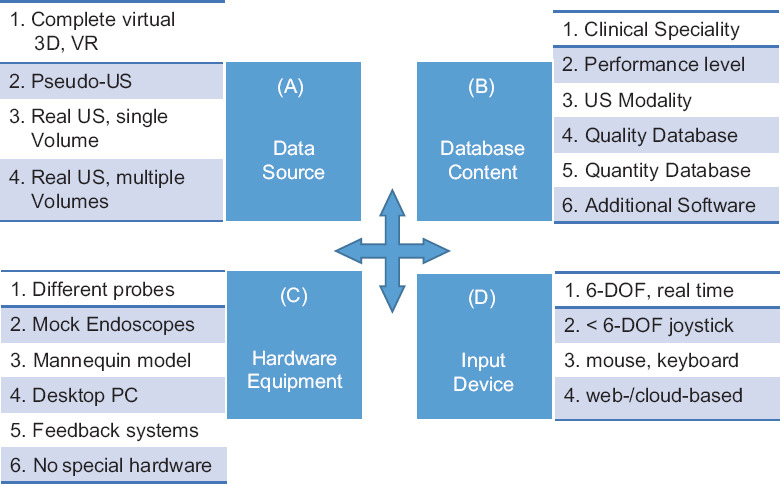
The application of simulators has been described in a wide range of clinical specialties [Figure 3]. Today, the main simulator companies on the market provide configurations to meet the different requirements of most clinical specialties, regardless of diagnostic or interventional techniques. In gynecology and obstetrics, simulation-assisted education has been used for over 20 years[25] and has led to improvements in patient-reported discomfort and perceived safety.[26]
Figure 3.
Clinical specialties. Clinical specialties with reported application fields – apart from radiology as the main interdisciplinary diagnostic and interventional specialty. US: Ultrasound; TTE: Transthoracic echocardiography; TEE: Transesophageal echocardiography; POCUS: Point of care US; eFAST: Extended focused assessment with sonography for trauma; GIUS: Gastrointestinal US; LN: Lymph nodes/neck; UGRA: US guided regional anesthesia; ICU: Intensive care unit; US: Ultrasound; GI: Gastrointestinal; Pulmo: Pulmonology
The standardized use of simulation has been encouraged in an American consensus report of a multi society task force including the American Institute of Ultrasound in Medicine.[27] It developed a consensus-based curriculum with competency assessment tools for obstetric and gynecologic ultrasound training. Furthermore, according to a recent French review, simulator-generated metrics helped to discriminate different ultrasound skills.[28] Performance scores can be obtained by using qualitative metrics, quantitative criteria and by assessing the quality of images.[28] British and Danish systematic reviews also found evidence of benefit from the use of simulation in obstetrics and gynecological ultrasound.[29,30] Nevertheless, there is relatively little data on how simulation-acquired skills correlate with clinical performance and if the skills are sustainable in the longer term.[29]
Cardiology is one of the most common clinical specialties for simulator-trained ultrasound. Simulators for echocardiography have been available for over three decades and highly sophisticated applications are now offered for both transesophageal and transthoracic echo and, since 2010, have contributed to approximately 50% of the simulation market [Figure 4]. Transesophageal simulators are the most expensive applications. A recent review focused on how to extrapolate the single simulation-acquired skills into a workflow of the whole examination procedure.[31] Simulation-based training of the peripheral vascular ultrasound is the other important cardiac subspecialty. Hereby, simulation of color flow Doppler images and Doppler spectral waveforms along with the corresponding B-mode images is especially challenging.[14,32] In the emergency department, several other applications emerged following the implementation of transesophageal simulators. Simulation as a training tool for POCUS has become an established part of the curriculum according to the American Academy of Emergency Physicians.[33,34] The importance of clinical lung ultrasound skills using simulation has been acknowledged for critical care setting.[10,35] Lung ultrasound simulation has been fundamental to clinical skills development at pace during the COVID-19 pandemic.[36,37,38] In Focused Assessment with Sonography for Trauma (FAST), standardization is important for all users, including prehospital use by paramedics.[39]
Figure 4.
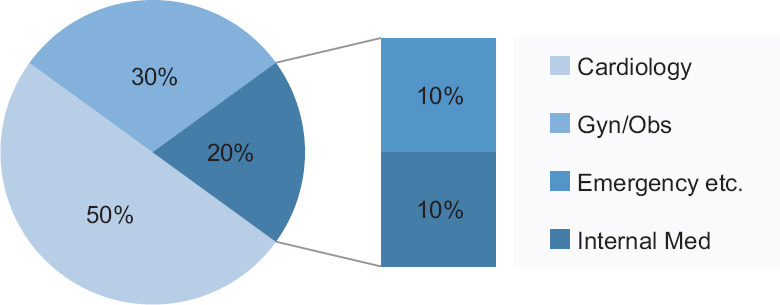
Ultrasound-simulator-market in healthcare – Distribution of clinical specialties. Estimation based on tenders since 2010, personal communication G. Jehle, Schallware. Gyn: Gynaecology; Obs: Obstetrics
Although a simulator-based approach would be the ideal solution to organize medical education in pediatrics without having to expose young and vulnerable patients to repetitive, nonexpert ultrasound examinations, so far relatively few systems include pediatric cases. Simulation-assisted training has become widely used in pediatric cardiology,[40] especially in the neonatal intensive care unit.[41] Focused neonatal cranial ultrasound training has been improved by simulation-based education according to a Canadian pediatric study.[42] Moreover, a simulation enhanced curriculum improved the POCUS competencies in umbilical catheter detection and interpretation.[43]
In anesthesia general catheter, management became a main application field for simulation-assisted education according to several international guidelines.[44] Simulation training resulted in increased use of ultrasound guidance for the insertion of central venous catheters.[45] Simulation-based examination could be successfully used for assessing the arterial catheter insertion performance[46] and improved the peripheral catheter insertion skills of nurses.[47] Simulation-assisted training using phantoms is established for ultrasound-guided regional anesthesia.[48,49,50] Online interactive simulation models have been used for teaching spinal sonoanatomy and training of lumbar puncture techniques.[17,51] Moreover, there has been a recent push to incorporate whole-body POCUS into anesthesiologists’ training and daily practice.[52]
Abdominal sonography is a challenging field for simulation due to the diversity of complex, closely related, and differently moving organs. Several studies investigated the feasibility of abdominal simulation[53,54] and demonstrated that simulator-assisted training improved ultrasound-scanning performance.[55] A Danish group developed a simulator-based test to discriminate performance levels[56] which made it possible to scale the teaching content according to different training levels and could so meet requirements from the beginner to the specialist.
Endosonography is an invasive procedure[57,58,59] and therefore particularly suitable for simulation-based education. Simulation-based training is helpful in the initial stages of learning where there is a steep learning curve, e.g., EUS-FNA/endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) in the gastrointestinal tract or for pulmonology.[20,60,61,62] According to an Indian review, skills acquired on a simulator could be transferred to real patients.[63] Urologic simulation-based education is taking an increasingly important role not only for surgical training but also for rectal sonography and ultrasound-guided prostate interventions.[64,65]
ULTRASOUND SIMULATION IN GENERAL SURGERY
Despite the widespread use of POCUS and recent adoption of ultrasound by numerous different subspecialties across the entire medical field,[66,67] no established and commonly agreed ultrasound curriculum is available in general surgery, but proposals have been put forward and regional experience has been published.[68,69,70] One ultrasound scenario, however, stands out as a generally accepted surgical task in most hospitals around the globe and that is the established use of FAST scanning in the trauma patient algorithm.[71] Interestingly, this application is also one of very few examples where simulation training with ultrasound has been reported to have a significant and positive impact on general surgery residents’ performance.[72] General surgery was among the first specialties to embrace simulation in the educational process and today is at the leading edge of this trend with extensive use of laparoscopic and recently robotic surgery simulation with the widespread use of Da Vinci systems worldwide.[73] Ultrasound scanners are now available as plug-in devices and picture-in-picture presentation for most laparoscopic equipment including robotic versions such as Da Vinci. Interestingly, one of the newest developments in general surgery utilizes a combination of real-time virtual ultrasound with 3D simulation and robotic surgery to obtain precise navigation of the surgical strategy in liver resection surgery.[74] With the general trend of ultrasound moving into clinical specialties, there can be little doubt that the near future will see the birth of an internationally accepted ultrasound curriculum for general surgery.
The challenge of implementing this into surgical resident programs at scale will require the development of a variety of ultrasound simulation-based education. This is obviously not an easy task and will require increased resources both staffing and financial. In order to avoid “reinventing the wheel” in this process, it is strongly recommended that the surgical educational environment join forces on a global scale and look to other specialties for lessons learned from their implementation of ultrasound and ultrasound simulation.
THE ROLE OF ULTRASOUND SIMULATION
With the availability of sophisticated ultrasound simulation equipment, it is even more important to define the role of ultrasound simulation. In one of the early meta-analyses, Stunt et al. reviewed 435 commercially available medical simulators that were marketed as methods for improving medical psychomotor skills training.[75] They found that only 6% of these simulators were accompanied by validation studies demonstrating an improvement in medical psychomotor skills following the use of the products. Fortunately, there has been a lot of progress since then, and therefore, it is important to discuss the future possible role of simulation in ultrasound using recent data.
A broader analysis of traditional barriers to ultrasound adoption and how simulation can overcome them is required. Despite the introduction of ultrasound into clinical medicine in 1942 by Dussik, adoption of POCUS was introduced by Gerhard Rettenmaier in clinical ultrasound,[76,77] but its widespread adoption was not immediate.[78] Recent improvements in performance, cost reduction, and miniaturization of ultrasound equipment have made ultrasound education and training the “last remaining hurdle” to widespread adoption of POCUS. Historical barriers to ultrasound training include the need for an ultrasound machine, a patient with a relevant pathologic condition, a qualified instructor, an opportunity and time to teach, and the ability to repeat this process until tasks are mastered [Table 1]. Each of these elements must be available for every ultrasound application a learner wishes to master. Recent studies conducted by Bahner et al. and Dinh et al. describe the common challenges in integrating ultrasound training into medical education.[8,79] Lack of funding, training resources, and space within existing curricula are cited as major obstacles. In addition, accessing patients specific pathologic conditions at time that correlates to didactic instruction can be challenging. Finally, the resources required to assess competency, track performance, provide feedback, and archive performance metrics are often underestimated by instructors [Table 1].
Table 1.
Barriers to ultrasound instruction and barriers to ultrasound curriculum integration
| Barriers to ultrasound instruction | Barriers to ultrasound curriculum integration |
|---|---|
| Ultrasound machine access | Lack of funding for machines and maintenance |
| Qualified instructors | Limited faculty time for instruction |
| Patients with pathology | Restricted clinical access to patients |
| Pediatric patients | Vulnerable and not accessible for nonexperts |
| Teaching moments | Crowded medical school curriculum |
| Refresher training opportunities | Lack of resources for assessment |
| Numbers of professionals needing to learn | Limited clinical placements |
| EUS | Invasive and potentially risky |
Traditional time-based progression apprenticeship models for ultrasound training face numerous challenges.[80,81,82,83] This “see one, do one, teach one” approach falls victim to the aforementioned barriers. Despite these challenges, some medical institutions have committed to comprehensive integration of ultrasound instruction across all years of medical school.[79,84,85,86,87,88,89] Many of these programs rely upon peer-to-peer ultrasound training paradigms. Time-based approaches to ultrasound education need to transition to strategies that are driven by performance outcomes. Recent advances in ultrasound simulation provide new education and training pathways.[4,90,91] They allow a reproducible, standardized and even trainer-independent assessment of the gained competency.[56] Moreover, ultrasound simulation technologies have been brought to the market that provide anytime-anywhere cloud-based didactic instruction with mobile optimization and refresher training.[4]
Driving forces for the introduction of simulation into ultrasound education include ease of repetition and opportunity for practice, exposure to wide variety of pathologies not easily obtained in short-term clinical training experiences and learning the basics on phantoms rather than in clinical setting which can reduce both patient and learner anxiety.
Ultrasound learners can now develop image acquisition, interpretation, and procedure skills through a variety of simulation technologies.[7,88,92,93,94,95,96,97,98,99,100,101,102,103,104] Additional ultrasound simulation applications have been developed to further assess how well learners can integrate ultrasound findings into clinical decision-making.[99,105]
Although scientific literature on ultrasound skill decay is limited, it suggests that competency in performing complex skills degrades over several months.[99] Cognitive aspects of complex skills appear to degrade first with notable degradation occurring approximately 3–6 months after training. Psychomotor elements persist longer but will eventually degrade as well, with notable decay occurring after 10–12 months.[106,107,108] Critically, among one of the first cognitive skills to show signs of degradation is the ability to prioritize and execute actions and responses in the appropriate order. Defining skill decay curves for different ultrasound applications is an important topic for future research and will inform the timing and frequency of refresher training using ultrasound simulators.[109]
ULTRASOUND SIMULATOR REQUIREMENTS AND DEMANDS
Ultrasound simulation systems should be judged based upon how well they address desired ultrasound-training objectives. This begins with achieving a consensus of what constitutes competency for a particular ultrasound application. Once the elements that lead to ultrasound competency for a particular application are identified, appropriate ultrasound simulation system requirements can be defined.
The objective structured assessment of ultrasound skills (OSAUS) criteria represent a consensus regarding the elements required to achieve ultrasound competency for specific ultrasound applications.[110] The OSAUS criteria were subsequently validated as a method to assess application-specific ultrasound competency.[110] Elements that contribute toward achieving ultrasound competency include understanding the indications for an ultrasound examination, anatomy skill, and applied knowledge of ultrasound equipment. Image optimization skills, the ability to independently perform a systematic ultrasound examination; interpret images and artifacts, document the examination, and apply the findings toward clinical decision-making are additional elements [Figure 5]. It is possible to practice these elements one by one or in combination mimicking normal clinical workflow. Different simulation equipment provides different solutions for these settings compared with [Figure 1].
Figure 5.
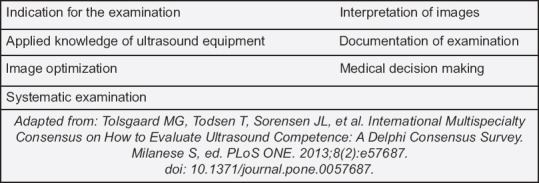
Elements of ultrasound competency
An alternative approach integrates ultrasound simulation into a broader ecosystem of ultrasound training applications designed to address all the elements required for ultrasound competency on an application-specific basis. This approach combines cloud-based didactic instruction, ultrasound image acquisition, interpretation, and procedure training using the PC-based performance tracking, and automated assessment powered by artificial intelligence (AI).[7,92,96,99,100,102,111,112]
The use of simulation for ultrasound training is not without pitfalls, as numerous factors influence whether an ultrasound simulation product is successfully adopted or not. The verisimilitude of any simulation experience is directly related to the product’s user interface and user experience. Recreating the “exact” experience of performing an ultrasound scan often requires the use of expensive technologies, which typically translate to higher ultrasound simulator costs. Research from flight and surgical simulators reveals that low-fidelity simulators often match, and sometimes outperform high-fidelity simulators, at much lower costs.[90,105,113,114,115] The degree of validation an ultrasound simulation application needs to demonstrate prior to attaining market acceptance will depend upon its intended training objective(s). Finally, the institutional commitment required to successfully integrate ultrasound simulation into existing curricula should not be overlooked. Successful adoption of ultrasound simulation will require ultrasound champions, integrating ultrasound simulation into lesson plans, incentivizing, and rewarding learner participation, and ensuring learners understand how to apply newly acquired ultrasound knowledge and skills toward clinical decision-making.
Successful performance of an ultrasound task is the best indicator of competency. However, when individuals fail to achieve success, an understanding of the specific elements that lead to failure will facilitate the provision of constructive feedback. The ability to provide feedback on weaknesses in declarative knowledge, procedural knowledge, or psychomotor skill is important for proper training. Selecting validated metrics that are predictive of competency is essential.[111] As such, a performance tracking and analytics feature coupled to the ultrasound simulation application is valuable. Declarative knowledge assessment involves assessing discrete knowledge parameters with reliable assessment questions. Procedural knowledge equates with the knowledge required to execute a task. It is assessed by having the subject progress through a series of steps to accomplish an assigned task. The degree of rigor and validation standards will depend on the procedure type and the nature of the assessment.
Advances in ultrasound simulation now allow for real-time automated performance assessment on a variety of ultrasound tasks. Advances powered by AI are automating and standardizing ultrasound competency assessment, which has previously relied upon subjective and/or checklist-driven assessments.[111,116,117,118] This creates a pathway for standardized assessment of large numbers of ultrasound learners.
SIMULATORS IN STUDENT AND TRAINEE ULTRASOUND EDUCATION
With the increasing use of simulation, there is the issue of effective training for those new to medical ultrasound imaging such as medical and sonography students as well as clinicians. The general consensus affirms that simulation has benefits for the initial skills development required by those learning diagnostic medical ultrasound.[119] Simulation training may not only involve dedicated simulator equipment using either mannequins or virtual reality, but also the use of simulated patients so that students can practice not only their scanning skills on a variety of body types but communication/interaction skills.[120,121,122] It has been shown that when teaching basic tasks, such as venous access or FAST scans, students that had access to simulation grasped the concepts faster and were more confident than those who only learnt at the bedside.[123,124] However, students learning FAST on live models were better able to acquire FAST windows in the clinical setting.[125,126,127,128]
In Australia, student sonographer’s curriculum includes 2200 clinical hours to learn to scan multiple body segments, including abdomen, pelvis, thyroid, breast, musculoskeletal, and the vascular anatomy. A review on the effectiveness of simulation for beginners in ultrasound training determined that when students moved from simulation to model patients, their level of competence did not reach a level that would allow them to scan patients unsupervised.[129] Through multiple studies comparing the outcomes of computer simulation versus live models, a common theme was that students still needed access to live models to hone their communication and scanning skills. This was particularly the situation with obstetric scanning, where simulators with static “fetus” do not reflect the clinical situation of mobile babies.
A disadvantage of simulation training is that it is highly resource intensive with high initial investment required. Furthermore, it can be difficult to train the students to perform documentation requirements. Introducing Dyad practice, which involves training students in pairs, increases the student to simulator ratio at the same time as providing peer support with learning.[130] Simulation may never fully replace learning in the clinical setting, but it is the first step in ensuring that new ultrasound students have the opportunity to practice skill in a safe learning space.
Future developments
As technology develops and simulation becomes more sophisticated, it is likely that further developments in ultrasound simulation will be realized. AI and deep learning, although in its infancy, is beginning to be integrated into ultrasound simulation in an attempt to provide realistic learning skills and experiences.[131] Tenewitz et al. reported the use of 3D printing to develop ultrasound phantoms for vascular access and biopsy[132] whilst other studies have been undertaken to determine the value of augmented reality in ultrasound education.[133,134] Nilsson et al., warn that careful evaluation of new technology is needed to determine cost-effectiveness as a learning resource.[135]
Financial support and sponsorship
Nil.
Conflicts of interest
Eric Savitsky serves as SonoSim CEO and has stock ownership. Meanwhile, Christoph F. Dietrich is a Co-Editor-in-Chief of the journal, and Adrian Saftoiu is an Associate Editor. This article was subject to the journal’s standard procedures, with peer review handled independently of the editors and their research groups.
REFERENCES
- 1.Nicholls D, Sweet L, Hyett J. Psychomotor skills in medical ultrasound imaging:An analysis of the core skill set. J Ultrasound Med. 2014;33:1349–52. doi: 10.7863/ultra.33.8.1349. [DOI] [PubMed] [Google Scholar]
- 2.Huang K, Zhao X, Chen X, et al. Analysis of digestive endoscopic results during COVID-19. J Transl Int Med. 2021;9:38–42. doi: 10.2478/jtim-2021-0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weissman S, Belyayeva A, Sharma S, et al. SARS-CoV-2 and acute diverticulitis:The expanding gastrointestinal manifestations of COVID-19 infection. J Transl Int Med. 2021;9:59–60. doi: 10.2478/jtim-2021-0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gottlieb M, Landry A, Egan DJ, et al. Rethinking residency conferences in the era of COVID-19. AEM Educ Train. 2020;4:313–7. doi: 10.1002/aet2.10449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nayahangan LJ, Dietrich CF, Nielsen MB. Simulation-based training in ultrasound –Where are we now? Ultraschall Med. 2021;42:240–4. doi: 10.1055/a-1352-5944. [DOI] [PubMed] [Google Scholar]
- 6.Nayahangan LJ, Albrecht-Beste E, Konge L, et al. Consensus on technical procedures in radiology to include in simulation-based training for residents:A European-wide needs assessment. Eur Radiol. 2021;31:171–80. doi: 10.1007/s00330-020-07077-0. [DOI] [PubMed] [Google Scholar]
- 7.Chung GK, Gyllenhammer RG, Baker EL, et al. Effects of simulation-based practice on focused assessment with sonography for trauma (FAST) window identification, acquisition, and diagnosis. Mil Med. 2013;178:87–97. doi: 10.7205/MILMED-D-13-00208. [DOI] [PubMed] [Google Scholar]
- 8.Bahner DP, Blickendorf JM, Bockbrader M, et al. Language of transducer manipulation:Codifying terms for effective teaching. J Ultrasound Med. 2016;35:183–8. doi: 10.7863/ultra.15.02036. [DOI] [PubMed] [Google Scholar]
- 9.Giovannini M. Learning in therapeutic EUS. Endosc Ultrasound. 2021;10:317–8. doi: 10.4103/EUS-D-21-00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pietersen PI, Madsen KR, Graumann O, et al. Lung ultrasound training:A systematic review of published literature in clinical lung ultrasound training. Crit Ultrasound J. 2018;10:23. doi: 10.1186/s13089-018-0103-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu Y, Glass NL, Glover CD, et al. Comparison of the development of performance skills in ultrasound-guided regional anesthesia simulations with different phantom models. Simul Healthc. 2013;8:368–75. doi: 10.1097/SIH.0b013e318299dae2. [DOI] [PubMed] [Google Scholar]
- 12.Lewiss RE, Hoffmann B, Beaulieu Y, et al. Point-of-care ultrasound education:The increasing role of simulation and multimedia resources. J Ultrasound Med. 2014;33:27–32. doi: 10.7863/ultra.33.1.27. [DOI] [PubMed] [Google Scholar]
- 13.Kamphuis ME, Greuter MJ, Slart RH, et al. Quantitative imaging:Systematic review of perfusion/flow phantoms. Eur Radiol Exp. 2020;4:15. doi: 10.1186/s41747-019-0133-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sheehan FH, Zierler RE. Simulation for competency assessment in vascular and cardiac ultrasound. Vasc Med. 2018;23:172–80. doi: 10.1177/1358863X17751656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim YH. Ultrasound phantoms to protect patients from novices. Korean J Pain. 2016;29:73–7. doi: 10.3344/kjp.2016.29.2.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blum T, Rieger A, Navab N, et al. A review of computer-based simulators for ultrasound training. Simul Healthc. 2013;8:98–108. doi: 10.1097/SIH.0b013e31827ac273. [DOI] [PubMed] [Google Scholar]
- 17.Ramlogan R, Niazi AU, Jin R, et al. A virtual reality simulation model of spinal ultrasound:Role in teaching spinal sonoanatomy. Reg Anesth Pain Med. 2017;42:217–22. doi: 10.1097/AAP.0000000000000537. [DOI] [PubMed] [Google Scholar]
- 18.Ripley B, Levin D, Kelil T, et al. 3D printing from MRI Data:Harnessing strengths and minimizing weaknesses. J Magn Reson Imaging. 2017;45:635–45. doi: 10.1002/jmri.25526. [DOI] [PubMed] [Google Scholar]
- 19.Rousian M, Koster MP, Mulders AG, et al. Virtual reality imaging techniques in the study of embryonic and early placental health. Placenta. 2018;64(Suppl 1):S29–35. doi: 10.1016/j.placenta.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 20.Naur TM, Nilsson PM, Pietersen PI, et al. Simulation-based training in flexible bronchoscopy and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA):A systematic review. Respiration. 2017;93:355–62. doi: 10.1159/000464331. [DOI] [PubMed] [Google Scholar]
- 21.Mooney JJ, Sarwani N, Coleman ML, et al. Evaluation of three-dimensional printed materials for simulation by computed tomography and ultrasound imaging. Simul Healthc. 2017;12:182–8. doi: 10.1097/SIH.0000000000000217. [DOI] [PubMed] [Google Scholar]
- 22.Sun Z. Clinical applications of patient-specific 3D printed models in cardiovascular disease:Current status and future directions. Biomolecules. 2020;10:1577. doi: 10.3390/biom10111577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu J, Kamath MV, Noseworthy MD, et al. Segmentation of images of abdominal organs. Crit Rev Biomed Eng. 2008;36:305–34. doi: 10.1615/critrevbiomedeng.v36.i5-6.10. [DOI] [PubMed] [Google Scholar]
- 24.Madsen ME, Konge L, Nørgaard LN, et al. Assessment of performance measures and learning curves for use of a virtual-reality ultrasound simulator in transvaginal ultrasound examination. Ultrasound Obstet Gynecol. 2014;44:693–9. doi: 10.1002/uog.13400. [DOI] [PubMed] [Google Scholar]
- 25.Acharya G, Morgan H, Henson G. Use of ultrasound to improve the safety of postgraduate training in obstetrics and gynaecology. Eur J Ultrasound. 2001;13:53–9. doi: 10.1016/s0929-8266(01)00114-8. [DOI] [PubMed] [Google Scholar]
- 26.Tolsgaard MG. Assessment and learning of ultrasound skills in Obstetrics &Gynecology. Dan Med J. 2018;65:B5445. [PubMed] [Google Scholar]
- 27.Abuhamad A, Minton KK, Benson CB, et al. Obstetric and gynecologic ultrasound curriculum and competency assessment in residency training programs:Consensus report. J Ultrasound Med. 2018;37:19–50. doi: 10.1002/jum.14519. [DOI] [PubMed] [Google Scholar]
- 28.Le Lous M, Klein M, Tesson C, et al. Metrics used to evaluate obstetric ultrasound skills on simulators:A systematic review. Eur J Obstet Gynecol Reprod Biol. 2021;258:16–22. doi: 10.1016/j.ejogrb.2020.12.034. [DOI] [PubMed] [Google Scholar]
- 29.Dromey BP, Peebles DM, Stoyanov DV. A systematic review and meta-analysis of the use of high-fidelity simulation in obstetric ultrasound. Simul Healthc. 2021;16:52–9. doi: 10.1097/SIH.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taksøe-Vester C, Dyre L, Schroll J, et al. Simulation-based ultrasound training in obstetrics and gynecology:A systematic review and meta-analysis. Ultraschall Med. 2021;42:e42–54. doi: 10.1055/a-1300-1680. [DOI] [PubMed] [Google Scholar]
- 31.Mahboobi S, Mahmood F, Bortman J, et al. Simulator-based training of workflow in echocardiography. J Cardiothorac Vasc Anesth. 2019;33:1533–9. doi: 10.1053/j.jvca.2018.09.020. [DOI] [PubMed] [Google Scholar]
- 32.Lee HS, Park P, Han S, et al. Effectiveness of flow volume measurement training using a custom-made Doppler flow simulator. Simul Healthc. 2021;16:73–7. doi: 10.1097/SIH.0000000000000469. [DOI] [PubMed] [Google Scholar]
- 33.Nti B, Pillarisetty LS. In:StatPearls. Treasure Island (FL): StatPearls Publishing Copyright ©2021, StatPearls Publishing LLC; 2021. Techniques and strategies in ultrasound simulation. [PubMed] [Google Scholar]
- 34.Dinh VA, Giri PC, Rathinavel I, et al. Impact of a 2-day critical care ultrasound course during fellowship training:A pilot study. Crit Care Res Pract. 2015;2015:675041. doi: 10.1155/2015/675041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu M, Wang T, Zhou Y, et al. Potential role of ACE2 in coronavirus disease 2019 (COVID-19) prevention and management. J Transl Int Med. 2020;8:9–19. doi: 10.2478/jtim-2020-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.POCUS Simulator Aids Training for COVID-19 Lung Ultrasound. 2020. [ [Last accessed on 2020 Jul]]. Available from: https://www.radmagazine.com/pocus-simulator-aids-training-for-covid-19-lung-ultrasound/
- 37.Wolstenhulme S, McLaughlan JR. Lung ultrasound education:Simulation and hands-on. Br J Radiol. 2021;94:20200755. doi: 10.1259/bjr.20200755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fang C, Jaworska J, Buda N, et al. Ultrasound of the chest and mediastinum in children, interventions and artefacts. WFUMB review paper (part 3) Med Ultrason. 2022;24:65–7. doi: 10.11152/mu-3323. [DOI] [PubMed] [Google Scholar]
- 39.McCallum J, Vu E, Sweet D, et al. Assessment of paramedic ultrasound curricula:A systematic review. Air Med J. 2015;34:360–8. doi: 10.1016/j.amj.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 40.Dayton JD, Groves AM, Glickstein JS, et al. Effectiveness of echocardiography simulation training for paediatric cardiology fellows in CHD. Cardiol Young. 2018;28:611–5. doi: 10.1017/S104795111700275X. [DOI] [PubMed] [Google Scholar]
- 41.Groves A. The future of cardiac ultrasound in the neonatal Intensive Care Unit. Clin Perinatol. 2020;47:499–513. doi: 10.1016/j.clp.2020.05.004. [DOI] [PubMed] [Google Scholar]
- 42.Mohammad K, Murthy P, Aguinaga F, et al. Simulation-based structured education supports focused neonatal cranial ultrasound training. J Ultrasound Med. 2020;39:1195–201. doi: 10.1002/jum.15207. [DOI] [PubMed] [Google Scholar]
- 43.Kochan MJ, Kim JS, Hoffman SB, et al. Point-of-care ultrasound to confirm umbilical line placement:Impact of a simulation enhanced curriculum on neonatal Intensive Care Unit provider competency. Simul Healthc. 2021;16:303–10. doi: 10.1097/SIH.0000000000000501. [DOI] [PubMed] [Google Scholar]
- 44.Frykholm P, Pikwer A, Hammarskjöld F, et al. Clinical guidelines on central venous catheterisation. Swedish Society of Anaesthesiology and Intensive Care Medicine. Acta Anaesthesiol Scand. 2014;58:508–24. doi: 10.1111/aas.12295. [DOI] [PubMed] [Google Scholar]
- 45.Day J, Winchester ZB, Cairns CA, et al. The impact of a comprehensive simulation-based training and certification program on resident central venous catheter complication rates. Simul Healthc. 2021;16:92–7. doi: 10.1097/SIH.0000000000000500. [DOI] [PubMed] [Google Scholar]
- 46.Golden A, Alaska Y, Levinson AT, et al. Simulation-based examination of arterial line insertion method reveals interdisciplinary practice differences. Simul Healthc. 2020;15:89–97. doi: 10.1097/SIH.0000000000000428. [DOI] [PubMed] [Google Scholar]
- 47.Amick AE, Feinsmith SE, Davis EM, et al. Simulation-based mastery learning improves ultrasound-guided peripheral intravenous catheter insertion skills of practicing nurses. Simul Healthc. 2022;17:7–14. doi: 10.1097/SIH.0000000000000545. [DOI] [PubMed] [Google Scholar]
- 48.Kim TE, Tsui BC. Simulation-based ultrasound-guided regional anesthesia curriculum for anesthesiology residents. Korean J Anesthesiol. 2019;72:13–23. doi: 10.4097/kja.d.18.00317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Udani AD, Harrison TK, Mariano ER, et al. Comparative-effectiveness of simulation-based deliberate practice versus self-guided practice on resident anesthesiologists'acquisition of ultrasound-guided regional anesthesia skills. Reg Anesth Pain Med. 2016;41:151–7. doi: 10.1097/AAP.0000000000000361. [DOI] [PubMed] [Google Scholar]
- 50.Chen XX, Trivedi V, AlSaflan AA, et al. Ultrasound-guided regional anesthesia simulation training:A systematic review. Reg Anesth Pain Med. 2017;42:741–50. doi: 10.1097/AAP.0000000000000639. [DOI] [PubMed] [Google Scholar]
- 51.Keri Z, Sydor D, Ungi T, et al. Computerized training system for ultrasound-guided lumbar puncture on abnormal spine models:A randomized controlled trial. Can J Anaesth. 2015;62:777–84. doi: 10.1007/s12630-015-0367-2. [DOI] [PubMed] [Google Scholar]
- 52.Li L, Yong RJ, Kaye AD, et al. Perioperative point of care ultrasound (POCUS) for anesthesiologists:An overview. Curr Pain Headache Rep. 2020;24:20. doi: 10.1007/s11916-020-0847-0. [DOI] [PubMed] [Google Scholar]
- 53.Terkamp C, Kirchner G, Wedemeyer J, et al. Simulation of abdomen sonography. Evaluation of a new ultrasound simulator. Ultraschall Med. 2003;24:239–4. doi: 10.1055/s-2003-41713. [DOI] [PubMed] [Google Scholar]
- 54.Østergaard ML, Ewertsen C, Konge L, et al. Simulation-based abdominal ultrasound training –A systematic review. Ultraschall Med. 2016;37:253–61. doi: 10.1055/s-0042-100452. [DOI] [PubMed] [Google Scholar]
- 55.Østergaard ML, Rue Nielsen K, Albrecht-Beste E, et al. Simulator training improves ultrasound scanning performance on patients:A randomized controlled trial. Eur Radiol. 2019;29:3210–8. doi: 10.1007/s00330-018-5923-z. [DOI] [PubMed] [Google Scholar]
- 56.Østergaard ML, Nielsen KR, Albrecht-Beste E, et al. Development of a reliable simulation-based test for diagnostic abdominal ultrasound with a pass/fail standard usable for mastery learning. Eur Radiol. 2018;28:51–7. doi: 10.1007/s00330-017-4913-x. [DOI] [PubMed] [Google Scholar]
- 57.Kovacevic B, Vilmann P. EUS tissue acquisition:From A to B. Endosc Ultrasound. 2020;9:225–31. doi: 10.4103/eus.eus_21_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khan Z, Hayat U, Moraveji S, et al. EUS-guided pancreatic ductal intervention:A comprehensive literature review. Endosc Ultrasound. 2021;10:98–102. doi: 10.4103/eus.eus_67_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Koo CS, Ho KY. The role of EUS-FNA in the evaluation of pancreatic cystic lesions. Endosc Ultrasound. 2020;9:71–5. doi: 10.4103/eus.eus_4_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Guo J, Sahai AV, Teoh A, et al. An international, multi-institution survey on performing EUS-FNA and fine needle biopsy. Endosc Ultrasound. 2020;9:319–28. doi: 10.4103/eus.eus_56_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Facciorusso A, Bajwa HS, Menon K, et al. Comparison between 22G aspiration and 22G biopsy needles for EUS-guided sampling of pancreatic lesions:A meta-analysis. Endosc Ultrasound. 2020;9:167–74. doi: 10.4103/eus.eus_4_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gabr MM, Frost T, Kudaravalli P, et al. Why is EUS-guided cyst-gastrostomy more common than cyst-duodenostomy:A disease state or endoscopist preference. Endosc Ultrasound. 2020;9:352–3. doi: 10.4103/eus.eus_39_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sehgal IS, Dhooria S, Aggarwal AN, et al. Training and proficiency in endobronchial ultrasound-guided transbronchial needle aspiration:A systematic review. Respirology. 2017;22:1547–57. doi: 10.1111/resp.13121. [DOI] [PubMed] [Google Scholar]
- 64.Rowley KJ, Liss MA. Systematic review of current ultrasound use in education and simulation in the field of urology. Curr Urol Rep. 2020;21:23. doi: 10.1007/s11934-020-00976-1. [DOI] [PubMed] [Google Scholar]
- 65.Fiard G, Descotes JL, Troccaz J. Simulation-based training in urology:A systematic literature review. Prog Urol. 2019;29:295–311. doi: 10.1016/j.purol.2019.03.003. [DOI] [PubMed] [Google Scholar]
- 66.Dietrich CF, Goudie A, Chiorean L, et al. Point of care ultrasound:A WFUMB position paper. Ultrasound Med Biol. 2017;43:49–58. doi: 10.1016/j.ultrasmedbio.2016.06.021. [DOI] [PubMed] [Google Scholar]
- 67.Beal EW, Sigmond BR, Sage-Silski L, et al. Point-of-care ultrasound in general surgery residency training:A proposal for milestones in graduate medical education ultrasound. J Ultrasound Med. 2017;36:2577–84. doi: 10.1002/jum.14298. [DOI] [PubMed] [Google Scholar]
- 68.Mollenkopf M, Tait N. Is it time to include point-of-care ultrasound in general surgery training?A review to stimulate discussion. ANZ J Surg. 2013;83:908–11. doi: 10.1111/ans.12363. [DOI] [PubMed] [Google Scholar]
- 69.Nassour I, Spalding MC, Hynan LS, et al. The surgeon-performed ultrasound:A curriculum to improve residents'basic ultrasound knowledge. J Surg Res. 2017;213:51–9. doi: 10.1016/j.jss.2017.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hosseini M, Bhatt A, Kowdley GC. Effectiveness of an early ultrasound training curriculum for general surgery residents. Am Surg. 2018;84:543–6. doi: 10.1177/000313481808400428. [DOI] [PubMed] [Google Scholar]
- 71.Osterwalder J, Mathis G, Hoffmann B. New perspectives for modern trauma management –Lessons learned from 25 years FAST and 15 years E-FAST. Ultraschall Med. 2019;40:560–83. doi: 10.1055/a-0924-5455. [DOI] [PubMed] [Google Scholar]
- 72.McLean D, Hewitson L, Atkinson P, et al. ULTRASIM:Ultrasound in trauma simulation. CJEM. 2019;21:125–8. doi: 10.1017/cem.2018.56. [DOI] [PubMed] [Google Scholar]
- 73.Chen R, Rodrigues Armijo P, Krause C, et al. A comprehensive review of robotic surgery curriculum and training for residents, fellows, and postgraduate surgical education. Surg Endosc. 2020;34:361–7. doi: 10.1007/s00464-019-06775-1. [DOI] [PubMed] [Google Scholar]
- 74.Lv A, Li Y, Qian HG, et al. Precise navigation of the surgical plane with intraoperative real-time virtual sonography and 3D simulation in liver resection. J Gastrointest Surg. 2018;22:1814–8. doi: 10.1007/s11605-018-3872-0. [DOI] [PubMed] [Google Scholar]
- 75.Stunt J, Wulms P, Kerkhoffs G, et al. How valid are commercially available medical simulators? Adv Med Educ Pract. 2014;5:385–95. doi: 10.2147/AMEP.S63435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dietrich CF, Bolondi L, Duck F, et al. History of Ultrasound in Medicine from its birth to date (2022), on occasion of the 50 Years Anniversary of EFSUMB. A publication of the European Federation of Societies for Ultrasound In Medicine and Biology (EFSUMB), designed to record the historical development of medical ultrasound. Med Ultrason. 2022 doi: 10.11152/mu-3757. doi: 10.11152/mu-3757. Epub ahead of print. PMID: 35574917. [DOI] [PubMed] [Google Scholar]
- 77.Jenssen C, Ewertsen C, Piscaglia F, et al. 50th years anniversary of EFSUMB:Initial roots, maturation, and new shoots. Ultraschall Med. 2022;43:227–31. doi: 10.1055/a-1790-0504. [DOI] [PubMed] [Google Scholar]
- 78.Shampo MA, Kyle RA. Karl Theodore Dussik-pioneer in ultrasound. Mayo Clin Proc. 1995;70:1136. doi: 10.4065/70.12.1136. [DOI] [PubMed] [Google Scholar]
- 79.Dinh VA, Fu JY, Lu S, et al. Integration of ultrasound in medical education at United States medical schools:A National Survey of Directors'Experiences. J Ultrasound Med. 2016;35:413–9. doi: 10.7863/ultra.15.05073. [DOI] [PubMed] [Google Scholar]
- 80.Vozenilek J, Huff JS, Reznek M, et al. See one, do one, teach one:Advanced technology in medical education. Acad Emerg Med. 2004;11:1149–54. doi: 10.1197/j.aem.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 81.Li S, Monachese M, Salim M, et al. Standard reporting elements for the performance of EUS:Recommendations from the FOCUS working group. Endosc Ultrasound. 2021;10:84–92. doi: 10.4103/EUS-D-20-00234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tyberg A, Mishra A, Cheung M, et al. Learning curve for EUS-guided biliary drainage:What have we learned? Endosc Ultrasound. 2020;9:392–6. doi: 10.4103/eus.eus_42_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Li J, Zhi X, Chen J, et al. Deep learning with convex probe endobronchial ultrasound multimodal imaging:A validated tool for automated intrathoracic lymph nodes diagnosis. Endosc Ultrasound. 2021;10:361–71. doi: 10.4103/EUS-D-20-00207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bahner DP, Adkins EJ, Hughes D, et al. Integrated medical school ultrasound:Development of an ultrasound vertical curriculum. Crit Ultrasound J. 2013;5:6. doi: 10.1186/2036-7902-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fox JC, Schlang JR, Maldonado G, et al. Proactive medicine:The “UCI 30,”an ultrasound-based clinical initiative from the University of California, Irvine. Acad Med. 2014;89:984–9. doi: 10.1097/ACM.0000000000000292. [DOI] [PubMed] [Google Scholar]
- 86.Nelson BP, Hojsak J, Dei Rossi E, et al. Seeing is believing:Evaluating a point-of-care ultrasound curriculum for 1st-year medical students. Teach Learn Med. 2017;29:85–92. doi: 10.1080/10401334.2016.1172012. [DOI] [PubMed] [Google Scholar]
- 87.Hoppmann RA, Rao VV, Poston MB, et al. An integrated ultrasound curriculum (iUSC) for medical students:4-year experience. Crit Ultrasound J. 2011;3:1–12. doi: 10.1007/s13089-011-0052-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Miller GT, Scerbo MW, Zybak S, et al. Learner improvement from a simulation-enhanced ultrasonography curriculum for first-year medical students. J Ultrasound Med. 2017;36:609–19. doi: 10.7863/ultra.15.12025. [DOI] [PubMed] [Google Scholar]
- 89.Wilson SP, Mefford JM, Lahham S, et al. Implementation of a 4-year point-of-care ultrasound curriculum in a Liaison Committee on Medical Education-Accredited US Medical School. J Ultrasound Med. 2017;36:321–5. doi: 10.7863/ultra.16.03068. [DOI] [PubMed] [Google Scholar]
- 90.Liteplo AS, Carmody K, Fields MJ, et al. SonoGames:Effect of an innovative competitive game on the education, perception, and use of point-of-care ultrasound. J Ultrasound Med. 2018;37:2491–6. doi: 10.1002/jum.14606. [DOI] [PubMed] [Google Scholar]
- 91.Tayal VS, Blaivas M, Foster T. Simulation medicine. In: Nelson BP, Katz D, editors. Ultrasound Program Management:A Comprehensive Resource for Administrating Point-of-Care, Emergency, and Clinical Ultrasound. Switzerland: Springer; 2018. pp. 127–44. [Google Scholar]
- 92.Azizi K, Ismail M, Aftab U, et al. Effectiveness of high-fidelity simulation in training emergency medicine physicians in point of care ultrasonography in Pakistan:A Quasi-Experimental Study. Cureus. 2020;12:e8659. doi: 10.7759/cureus.8659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Damp J, Anthony R, Davidson MA, et al. Effects of transesophageal echocardiography simulator training on learning and performance in cardiovascular medicine fellows. J Am Soc Echocardiogr. 2013;26:1450–6. doi: 10.1016/j.echo.2013.08.008. e2. [DOI] [PubMed] [Google Scholar]
- 94.Ferrero NA, Bortsov AV, Arora H, et al. Simulator training enhances resident performance in transesophageal echocardiography. Anesthesiology. 2014;120:149–59. doi: 10.1097/ALN.0000000000000063. [DOI] [PubMed] [Google Scholar]
- 95.Skinner AA, Freeman RV, Sheehan FH. Quantitative feedback facilitates acquisition of skills in focused cardiac ultrasound. Simul Healthc. 2016;11:134–8. doi: 10.1097/SIH.0000000000000132. [DOI] [PubMed] [Google Scholar]
- 96.Monti JD, Perreault MD. Impact of a 4-hour introductory eFAST training intervention among ultrasound-Naïve U. S. Military Medics. Mil Med. 2020;185:e601–8. doi: 10.1093/milmed/usaa014. [DOI] [PubMed] [Google Scholar]
- 97.Maw A, Jalali C, Jannat-Khah D, et al. Faculty development in point of care ultrasound for internists. Med Educ Online. 2016;21:33287. doi: 10.3402/meo.v21.33287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Rebel A, Hester DL, DiLorenzo A, et al. Beyond the “E”in OSCE. Anesth Analg. 2018;127:1092–6. doi: 10.1213/ANE.0000000000003317. [DOI] [PubMed] [Google Scholar]
- 99.Rowley KJ, Wheeler KM, Pruthi DK, et al. Development and implementation of competency-based assessment for urological ultrasound training using SonoSim:A preliminary evaluation. Indian J Urol. 2020;36:270–5. doi: 10.4103/iju.IJU_22_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Preven DW, Kachur EK, Kupfer RB, et al. Proceedings of The American Institute of Ultrasound in Medicine Annual Convention. New York: 2018. Can Ultrasound Naïve First-Year Medical Students Develop Hands-on Skills in Image Acquisition after Reviewing Online Ultrasound Modules? In: AIUM 2018. [Google Scholar]
- 101.Savitsky E, Iseli M, Savitsky E. In:Presentation at the 2015 CRESST Conference. Redondo Beach, CA: 2015. Creation of an Ontology for the assessement of Fundamentals of Medical Ultrasound. [Google Scholar]
- 102.Chung GK. National Center for Research on Evaluation, Standards, and Student Testing. The Effects of Practicing with a Virtual Ultrasound Trainer on FAST Window Identification, Acquisition, and Diagnosis. CRESST Report 787. 2011:99. [Google Scholar]
- 103.Iseli MR, Cai L. Creation of a Knowledge and Skills Ontology for Fundamentals of Ultrasonography (Final Deliverable, CRESST Pélagique Project Report: SBIR Phase II). Los Angeles: University of California, Los Angeles, National Center for Research on Evaluation, Standards, and Student Testing (CRESST) 2016 [Google Scholar]
- 104.Prat G, Charron C, Repesse X, et al. The use of computerized echocardiographic simulation improves the learning curve for transesophageal hemodynamic assessment in critically ill patients. Ann Intensive Care. 2016;6:27. doi: 10.1186/s13613-016-0132-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lewiss RE, Hayden GE, Murray A, et al. SonoGames:An innovative approach to emergency medicine resident ultrasound education. J Ultrasound Med. 2014;33:1843–9. doi: 10.7863/ultra.33.10.1843. [DOI] [PubMed] [Google Scholar]
- 106.Arthur W, Jr, Bennett W, Jr, Stanush PL, et al. Factors that influence skill decay and retention:A quantitative review and analysis. Hum Perform. 1998;11:57–101. [Google Scholar]
- 107.Driskell JE, Willis RP, Copper C. Effect of overlearning on retention. J Appl Psychol. 1992;77:615. [Google Scholar]
- 108.Arthur W, Day EA, Villado AJ, et al. Decay, transfer, and the reacquisition of a complex skill: An investigation of practice schedules, observational rehearsal, and individual differences. 2007. [[Last accessed on 2022 Dec 29]]. Available from: https://apps.dtic.mil/sti/pdfs/ADA482766.pdf .
- 109.Pusic MV, Kessler D, Szyld D, et al. Experience curves as an organizing framework for deliberate practice in emergency medicine learning. Acad Emerg Med. 2012;19:1476–80. doi: 10.1111/acem.12043. [DOI] [PubMed] [Google Scholar]
- 110.Todsen T, Tolsgaard MG, Olsen BH, et al. Reliable and valid assessment of point-of-care ultrasonography. Ann Surg. 2015;261:309–15. doi: 10.1097/SLA.0000000000000552. [DOI] [PubMed] [Google Scholar]
- 111.Iseli MR, Lee J, Schenke K. Simulation-Based Assessment of Ultrasound Proficiency (Final Deliverable, CRESST Pélagique Project Report:SBIR Phase III) Los Angeles: University of California, Los Angeles, National Center for Research on Evaluation, Standards, and Student Testing (CRESST); 2019. [Google Scholar]
- 112.Liu E, Bhutani MS, Sun S. Artificial intelligence:The new wave of innovation in EUS. Endosc Ultrasound. 2021;10:79–83. doi: 10.4103/EUS-D-21-00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hochmitz I, Yuviler-Gavish N. Physical fidelity versus cognitive fidelity training in procedural skills acquisition. Hum Factors. 2011;53:489–501. doi: 10.1177/0018720811412777. [DOI] [PubMed] [Google Scholar]
- 114.Lefor AK, Harada K, Kawahira H, et al. The effect of simulator fidelity on procedure skill training:A literature review. Int J Med Educ. 2020;11:97–106. doi: 10.5116/ijme.5ea6.ae73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Alessi SM. Fidelity in the design of instructional simulations. J Comput Based Instr. 1988;15:40–7. [Google Scholar]
- 116.Lenchus JD, Carvalho CM, Ferreri K, et al. Filling the void:Defining invasive bedside procedural competency for internal medicine residents. J Grad Med Educ. 2013;5:605–12. doi: 10.4300/JGME-D-13-00030.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Millington SJ, Wong RY, Kassen BO, et al. Improving internal medicine residents'performance, knowledge, and confidence in central venous catheterization using simulators. J Hosp Med. 2009;4:410–6. doi: 10.1002/jhm.570. [DOI] [PubMed] [Google Scholar]
- 118.Walzak A, Bacchus M, Schaefer JP, et al. Diagnosing technical competence in six bedside procedures:Comparing checklists and a global rating scale in the assessment of resident performance. Acad Med. 2015;90:1100–8. doi: 10.1097/ACM.0000000000000704. [DOI] [PubMed] [Google Scholar]
- 119.Sidhu HS, Olubaniyi BO, Bhatnagar G, et al. Role of simulation-based education in ultrasound practice training. J Ultrasound Med. 2012;31:785–91. doi: 10.7863/jum.2012.31.5.785. [DOI] [PubMed] [Google Scholar]
- 120.Blickendorf JM, Adkins EJ, Boulger C, et al. Trained simulated ultrasound patients:Medical students as models, learners, and teachers. J Ultrasound Med. 2014;33:35–8. doi: 10.7863/ultra.33.1.35. [DOI] [PubMed] [Google Scholar]
- 121.Reid-Searl K, Bowman A, McAllister M, et al. The masked educator-innovative simulation in an Australian undergraduate Medical Sonography and Medical Imaging program. J Med Radiat Sci. 2014;61:233–40. doi: 10.1002/jmrs.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Eroglu O, Coskun F. Medical students'knowledge of ultrasonography:Effects of a simulation-based ultrasound training program. Pan Afr Med J. 2018;30:122. doi: 10.11604/pamj.2018.30.122.14820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Turner EE, Fox JC, Rosen M, et al. Implementation and assessment of a curriculum for bedside ultrasound training. J Ultrasound Med. 2015;34:823–8. doi: 10.7863/ultra.34.5.823. [DOI] [PubMed] [Google Scholar]
- 124.McGraw R, Chaplin T, McKaigney C, et al. Development and evaluation of a simulation-based curriculum for ultrasound-guided central venous catheterization. CJEM. 2016;18:405–13. doi: 10.1017/cem.2016.329. [DOI] [PubMed] [Google Scholar]
- 125.Bentley S, Mudan G, Strother C, et al. Are live ultrasound models replaceable?Traditional versus simulated education module for FAST exam. West J Emerg Med. 2015;16:818–22. doi: 10.5811/westjem.2015.9.27276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Juo YY, Quach C, Hiatt J, et al. Comparative analysis of simulated versus live patient-based FAST (Focused Assessment With Sonography for Trauma) training. J Surg Educ. 2017;74:1012–8. doi: 10.1016/j.jsurg.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 127.Todsen T, Jensen ML, Tolsgaard MG, et al. Transfer from point-of-care Ultrasonography training to diagnostic performance on patients –A randomized controlled trial. Am J Surg. 2016;211:40–5. doi: 10.1016/j.amjsurg.2015.05.025. [DOI] [PubMed] [Google Scholar]
- 128.Okasha HH, El-Meligui A, Pawlak KM, et al. Practical approach to linear EUS examination of the mediastinum. Endosc Ultrasound. 2021;10:406–13. doi: 10.4103/EUS-D-21-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Bradley K, Quinton A, Aziz A. Determining if simulation is effective for training in ultrasound:A narrative review. Sonography. 2019;7:22–32. [Google Scholar]
- 130.Tolsgaard MG, Madsen ME, Ringsted C, et al. The effect of dyad versus individual simulation-based ultrasound training on skills transfer. Med Educ. 2015;49:286–95. doi: 10.1111/medu.12624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Peng B, Huang X, Wang S, et al. A real-time medical ultrasound simulator based on a generative adversarial network model. Proc Int Conf Image Proc. 2019;2019:4629–33. doi: 10.1109/icip.2019.8803570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Tenewitz C, Le RT, Hernandez M, et al. Systematic review of three-dimensional printing for simulation training of interventional radiology trainees. 3D Print Med. 2021;7:10. doi: 10.1186/s41205-021-00102-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Ebner F, De Gregorio A, Schochter F, et al. Effect of an augmented reality ultrasound trainer app on the motor skills needed for a kidney ultrasound:Prospective trial. JMIR Serious Games. 2019;7:e12713. doi: 10.2196/12713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Rosenfeldt Nielsen M, Kristensen EQ, Jensen RO, et al. Clinical ultrasound education for medical students:Virtual reality versus e-learning, a randomized controlled pilot trial. Ultrasound Q. 2021;37:292–6. doi: 10.1097/RUQ.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 135.Nilsson PM, Todsen T, Subhi Y, et al. Cost-effectiveness of mobile app-guided training in extended focused assessment with sonography for trauma (eFAST):A randomized trial. Ultraschall Med. 2017;38:642–7. doi: 10.1055/s-0043-119354. [DOI] [PubMed] [Google Scholar]