Abstract
Simple Summary
The discovery of antibiotics was a breakthrough in medicine. However, bacterial defense mechanisms driven by genetic variation resulted in resistance to these compounds relatively quickly. Moreover, new classes of antibiotics have not been developed for 30 years. Within the European Union, the EU Parliament and Council Regulation No. 2019/6, which concerns veterinary medicinal products, is currently in force. The current goal is to reduce the use of antibiotics and to stop the rise of drug resistance in bacteria because such antimicrobial resistant organisms can be transmitted to humans through the consumption of animal products or direct contact with animals (dogs, cats, etc.). For this reason, there is a growing interest in essential oils (EOs). As natural mixtures (usually of terpenes and their derivatives), they may consist of about 20–60 components with 1–3 dominant component(s). An important feature of EOs is their hydrophobicity, which allows them to react with lipids present in bacterial cell membranes and mitochondria, disrupting the functioning of cell structures and consequently making them more permeable to other components or antibiotics. In the present manuscript, the activity of two EOs (patchouli and tea tree) was assessed, and their interaction with gentamicin and enrofloxacin was studied.
Abstract
In this paper, we show the effect of some essential oils (EOs) on staphylococci, including multidrug-resistant strains isolated from pyoderma in dogs. A total of 13 Staphylococcus pseudintermedius and 8 Staphylococcus aureus strains were studied. To assess the sensitivity of each strain to the antimicrobial agents, two commercial EOs from patchouli (Pogostemon cablin; PcEO) and tea tree (Melaleuca alternifolia; MaEO) as well as two antibiotics (gentamicin and enrofloxacin) were used. The minimum inhibitory concentration (MIC) followed by checkerboards in the combination of EO-antibiotic were performed. Finally, fractional inhibitory concentrations were calculated to determine possible interactions between these antimicrobial agents. PcEO MIC ranged from 0.125 to 0.5 % v/v (1.2–4.8 mg/mL), whereas MaEO MIC was tenfold higher (0.625–5% v/v or 5.6–44.8 mg/mL). Gentamicin appeared to be highly prone to interacting with EOs. Dual synergy (38.1% of cases) and PcEO additive/MaEO synergism (53.4%) were predominantly observed. On the contrary, usually, no interactions between enrofloxacin and EOs were observed (57.1%). Both commercial EOs were characterized by natural composition without artificial adulteration. Patchouli and tea tree oils can be good alternatives for treating severe cases of pyoderma in dogs, especially when dealing with multidrug-resistant strains.
Keywords: essential oils, patchouli, tea tree, staphylococci, pyoderma, MIC, checkerboards
1. Introduction
Antibacterial therapies are mainly based on antibiotics. However, they are not always effective and can sometimes be invasive or cause side effects (hair or hearing loss, diarrhea, irritability, lack of appetite, etc.). Moreover, they increasingly encounter antibiotic resistance, which is a therapeutic and economic problem.
Purulent dermatitis (pyoderma) is the most common bacterial skin disease of dogs accompanying other dermatological problems, manifesting as a complication of the underlying disease, such as allergies (food allergy, atopic dermatitis, allergy to flea bites), internal diseases (hypothyroidism, adrenal hyperfunction), seborrhea and inflammation of the sebaceous glands, parasites (Demodex canis, scabies, etc.), hormonal fluctuations, anatomical predispositions (e.g., skin folds), or abnormal functioning of the immune system [1]. Puppies that have not yet developed a level of immunity and older dogs or steroid-treated individuals are the most vulnerable [2]. Pyoderma is much more common in dogs with short coats than in those with longer hairs, where the dense hair and undercoat provide a better barrier against bacterial penetration [3].
The symptoms that occur in pyoderma are varied and depend on the type of inflammation, the area of the skin and the intensity of the disease. The most common include erythema, blisters, itching, hair loss (alopecia), ulceration, coat and skin discoloration, scabs, pustules, and purulent lesions. It is also possible that skin lesions have an endocrine basis with other symptoms, such as lethargy, weight gain, or excessive thirst [4].
In the case of pyoderma in dogs, the most commonly isolated pathogen is a Gram-positive coccus classified as a Staphylococcus pseudintermedius. S. pseudintermedius is believed to colonize the skin and mucous membranes in small numbers in 80% of healthy dogs. Bacteria less commonly found in purulent lesions include other coagulase-positive staphylococci (S. aureus or S. schleiferi subsp. coagulans), Gram-negative bacilli—such as Pseudomonas aeruginosa, Proteus spp., and Escherichia coli—or yeast-like fungi (Malassezia sp., Candida sp.) [5]. These microorganisms are the natural commensal microflora of the skin in dogs; nevertheless, when they are abundant and the animal’s immune system declines, they can be the cause of skin lesions.
Antibiotics (and other antimicrobial agents not classified as antibiotics) used in the treatment of pyoderma in dogs should be characterized by a broad spectrum of action and high efficacy against the abovementioned microorganisms, i.e., mainly S. pseudintermedius. The drug must reach high concentrations in the skin and have as few side effects as possible. The most important attribute is strong bactericidal activity. Cephalosporins (e.g., first-generation cephalexin or third-generation cefovecin (Convenia)), fluoroquinolones (enrofloxacin, marbofloxacin, ciprofloxacin), aminoglycosides (amikacin, gentamicin), lincosamides (clindamycin), and amoxicillin/clavulanic acid are among the most commonly used antibiotics in the control of purulent dermatitis in dogs [6].
In recent years, there has been growing antibiotics resistance in staphylococci isolated from dogs. In addition to S. aureus (methicillin-resistant Staphylococcus aureus—MRSA), methicillin-resistant Staphylococcus pseudintermedius (MRSP) strains have appeared. This means resistance of these bacteria to antibiotics included in the β-lactam group. Additionally, these pathogens tend to be multidrug-resistant, which poses a problem in selecting the correct antibiotic during treatment [7]. They occur in the pharynx, nasal cavity, rectum, and periosteal area as asymptomatic carriage. Moreover, these bacteria are often isolated from dog bite wounds [8].
Because of this, there has been growing interest in essential oils (EOs) and their use in medicine, cosmetology, and the food industry. EOs are obtained from various plant materials (leaves, buds, fruits, flowers, herbs, branches, bark, wood, roots, and seeds) via steam distillation through their maceration with fats or pressing [9]. Essential oils are volatile, liquid, transparent or rarely colored, and soluble in fat and organic solvents. As natural mixtures of an extraordinarily complex nature, they can consist of up to 100–200 chemical compounds in a wide variety of concentrations: several are present in high concentrations (a total of 20–70%) compared to other components (trace amounts). The amount varies depending on the part and species of the plant. They are chemical derivatives of terpenes and terpenoids [10].
Despite a number of studies on the composition of individual oils, detailed knowledge of their mechanism of action is still limited. Of particular importance is determining the effects of EOs on various microorganisms, especially how they act in combination with other antimicrobial compounds [11].
Essential oils are believed to have important antiseptic, antibacterial, antiviral, antioxidant, antiparasitic, antifungal, and insecticidal activities [12]. An important characteristic of EOs is hydrophobicity, which allows them to dissociate from the lipids present in the bacterial cell membrane and mitochondria, making them more permeable by disrupting cell structures. This ultimately results in bacterial cell death due to the leakage of critical molecules and ions from the bacterial cell at a high rate [13]. EOs can thus serve as a powerful tool for inhibiting the growing phenomenon of bacterial resistance [14]. The overall concept of some antimicrobial synergy is based on the principle that combination of two or more antimicrobial agents may enhance efficacy, reduce/decrease toxicity or side effects of one of agent used, increase bioavailability, lower the dose of, e.g., antibiotics, and reduce the advance of antimicrobial resistance [15]. New and highly effective antimicrobial combinations of drugs that contain natural product(s) have recently become a research priority.
The aim of the study was to evaluate the antimicrobial activity of patchouli and tea tree essential oils applied alone and in combination with gentamicin and enrofloxacin as an alternative in the treatment of purulent skin inflammation in dogs against S. pseudintermedius and S. aureus, especially in regard to multidrug-resistant isolates.
2. Materials and Methods
2.1. Bacterial Strain Origin and Identification
All strains were isolated and collected in the veterinary laboratory (West Pomerania, Szczecin, Poland) during routine tests of swabs/skin scrapings from acute pyoderma cases in the years 2019–2021. Strains were then systematically banked (VIABANK™, MWE Medical Wire, Corsham, UK) in order to produce autovaccines and kept in a frozen state (≤−30 °C) until research (no animals were directly involved in this experiment). A total of 12 S. pseudintermedius and 7 S. aureus strains were archived. Additionally, an S. aureus reference strain (ATCC 25923, KWIK-STIK™ Microbiologics, Argenta, Poznan, Poland) and an S. pseudintermedius ED99 type strain (lab collection) were used as an internal control of the entire study. For the purposes of the research presented in the manuscript, the strains were revived onto blood agar, mannitol salt agar (Oxoid, Argenta, Poznan, Poland), and STAPH chromagar (GRASO, Starogard Gdanski, Poland) and incubated overnight at 37 °C.
After bacterial growth, isolates were identified on the basis of their ability to ferment mannitol (GRASO, Starogard Gdanski, Poland), Polymyxin B resistance, and ability to form fibrin clots in rabbit plasma (Biomed, Cracow, Poland). The Staphaurex™ Plus Latex Agglutination Test (Remel, ThermoFisher Scientific, Waltham, MA, USA) was also performed. After initial selection, a multiplex polymerase chain reaction (M-PCR) method described by Sasaki et al. [16] was performed to differentiate of coagulase-positive staphylococci (CoPS). By using this method, seven species of CoPS were preliminary differentiated based on the size of the PCR product after amplification of the conserved regions of the thermonuclease (nuc) gene. In addition, the presence of the mecA and blaZ genes were also tested according to Ruzauskas et al. [17]. In this case, the major genetic determinants of resistance to ß-lactam antibiotics were tested.
2.2. Antimicrobial Susceptibility Testing
The disk diffusion method was used to determine which antimicrobial agent will inhibit the growth of the selected staphylococci according to the CLSI M100 31st ed. [18] and VET01S 5th ed. [19] recommendations. The following commercial disks (OXOID, Argenta, Poznan, Poland) were used: penicillin G (5 μg), amoxicillin (10 μg), amoxicillin with clavulanic acid (20 + 10 μg), cefalexin (30 μg), doxycycline (30 μg), oxytetracycline (30 μg), trimethoprim/sulfamethoxazole (1:19; 25 μg), neomycin (30 μg), gentamicin (10 μg), amikacin (30 μg), enrofloxacin (5 μg), marbofloxacin (5 μg), ciprofloxacin (10 μg), and polymyxin B (300 U). In order to estimate potential methicillin resistance, an oxacillin disk (1 μg; resistance with the zone of inhibition ≤17 mm recommended for S. pseudintermedius) and a cefoxitin disk (30 μg; a surrogate for oxacillin recommended for S. aureus with the zone of inhibition ≤21 mm in regard to resistance) were used.
2.3. Antibiotics and Essential Oils Analysis
A freeze-dried gentamicin (OXOID, ThermoFisher Scientific, Waltham, MA, USA) was dissolved in deionized water to a final concentration of 256 mg/mL, becoming the basis for the appropriate two-fold dilutions in Mueller–Hinton broth (MHB) (GRASO, Gdansk, Poland) to achieve a final concentration ranging from 2.56 mg/mL to 0.01 μg/mL.
Enrofloxacin, as a ready-to-use solution for injection (Baytril™ One, 100 mg/mL suspended in 30 mg n-Butanol; Bayer Animal Health, UK), was purchased from Medivet (Szczecin, Poland). Similarly to above, the solution was initially diluted to concentration of 2.56 mg/mL, and then, two-fold dilutions were prepared.
Commercial essential oils (Organique/Avicenna, Wroclaw, Poland) from patchouli (Pogostemon cablin; PcEO) and tea tree (Melaleuca alternifolia; MaEO) were used in the study. Only to control the content of patchouli alcohol, a sample of Tisserand Aromatherapy brand of patchouli oil (First Natural Brands Ltd., Sayers Common, West Sussex, United Kingdom) was used in the HPLC-MS study as an internal control. Vials were stored at 4 °C in dark glass bottles. Dimethyl sulfoxide (DMSO) (Avantor, Gliwice, Poland) was used as an organic solvent for essential oils (twofold dilutions expressed as % v/v and mg/mL). A stock solution of the tested oils was prepared in a final concentration ranging from 10% to 0.001% v/v. The concentration was expressed in mg/mL depending on the individual density of the EO batch. In order to exclude an inhibitory effect of DMSO on growth of staphylococci, a concentration gradient of DMSO alone ranging from 0% to 50% (increase by 5%) was performed, and the survival of each staphylococci strain in this gradient was evaluated.
2.4. Activity of Antibiotics and Essential Oils against Staphylococci
2.4.1. Individual MIC
To assess the sensitivity of each staphylococci strain to the antimicrobial agents under study, the minimum inhibitory concentration (MIC) of gentamicin, enrofloxacin, and both essential oils (PcEO and MaEO) against all S. pseudintermedius and S. aureus strains was individually determined via the serial dilution method using sterile 96-well plates (Wuxi Nest Biotechnology, Wuxi, China). Briefly, a decreasing concentration of antibiotics was successively added in the amount of 10 µL to each well containing 85 µL MHB in the rows of the 96-well microplate (causing an additional dilution of 1:10). In the case of EOs, 10 µL of decreasing-concentration, previously prepared stock solution of EOs was used in a similar arrangement as above (1:10; max DMSO content ≤ 10%). Next, the bacterial suspension (5 µL) at a concentration of 2.0 × 107 CFU/mL (DEN-1 densitometer, BioSan, Józefów, Poland) was added to each well (final concentration approx. 1.0 × 106 CFU/mL per well). The MIC was estimated after 24 h of incubation at 37 ± 1 °C. To avoid a false reading (especially at EO with artificial turbidity at the highest concentrations), a 10 µL of 0.01% resazurin (POL-AURA, Olsztyn, Poland) was added to each well. The color changed from blue to pink after an additional 3 h of incubation with resazurin at 37 ± 1 °C, indicating the presence of live bacteria in the well (which means that the antimicrobial agent was ineffective at the concentration tested). MIC was determined on the basis of the dark blue color appearance in the first well after any pink wells (corresponding to the smallest concentration of an antimicrobial agent capable of eliminating staphylococci). All experiments were performed in triplicate.
2.4.2. Checkerboards
Knowing the individual effective concentrations of gentamicin, enrofloxacin and EOs, we extended our investigation to study the potential synergistic or antagonistic effect between those antimicrobial agents in the following four combinations: PcEO × gentamicin, PcEO × enrofloxacin, MaEO × gentamicin, and MaEO × enrofloxacin in the 96-well checkerboard.
Briefly, a mix of seven serial twofold dilutions of EO in rows (10 µL/well; horizontal orientation) and ten serial twofold dilutions of antibiotics in columns (10 µL/well; vertical orientation) was added to 75 µL/well of MHB for different oil × antibiotic combinations/well. The last row and penultimate column always contained only a single antimicrobial agent supplemented with the pure lacking opposite diluent (DMSO or ddH2O). The last column was reserved for positive and negative controls (wells contain only MHB and both diluents). Then, 5 µL of the particular bacterial suspension at a final concentration of 2.0 × 107 CFU/mL was added to each well (final concentration approx. 1.0 × 106 CFU/mL per well with the exclusion of negative controls which control the purity of MHB and diluents). Positive control confirms the vitality of the strain under conditions of maximum DMSO concentration in MHB. Incubation and readings were similar to the individual MIC. If there was an interaction, the best well was selected. Each checkerboard was performed in triplication.
2.4.3. Fractional Inhibitory Concentrations
To determine possible interactions between antimicrobial agents, fractional inhibitory concentrations (FICs) were calculated according to van Vuuren and Viljoen [15] as follows:
| FIC(OxA) = MIC(OxA)/MIC(O) |
| FIC(AxO) = MIC(AxO)/MIC(A) |
where:
| OxA—oil in combination with antibiotics O—oil alone |
| AxO—antibiotics in combination with oil A—antibiotics alone |
The ΣFIC was then calculated for each test sample independently as the sum of the FIC:
| ΣFIC = FIC(OxA) + FIC(AxO) |
The interpretation of possible interactions in vitro between antimicrobial agents was described as synergistic (ΣFIC ≤ 0.5), additive (0.5 < ΣFIC ≤ 1.0), noninteractive (1.0 < ΣFIC ≤ 4.0), or antagonistic (ΣFIC > 4.0).
2.5. Qualitative Analysis of the Composition of Essential Oils
Composition of both commercial essential oils were analyzed via high-performance liquid chromatography–mass spectrometry (HPLC-MS) technique. A reversed-phase Zorbax 2.1 × 50 mm Eclipse Plus C18 column (Agilent, Santa Clara, CA, USA) equipped with a guard column was used for the chromatographic separation. An Ultivo G6465B mass spectrometer (Agilent, USA) coupled to a chromatograph (1260 Infinity II Series Liquid Chromatograph, Agilent, USA) was used to detect and identify the constitutes according to mass-to-charge ratio (m/z) working in scanning mode (SCAN) followed by multiple reaction monitoring (MRM) mode.
The patchouli oil and tea tree oil were diluted using HPLC hypergrade acetonitrile—ACN (Supelco, Sigma Aldrich, Burlington MA, USA)—to prepare a concentration of 100 mg/mL. Then, the concentration of the oil was further rediluted to obtain lower dilutions for injection into the mass spectrometer (injection volume 1 μL). Mobile phase A was ddH2O containing 0.1% HCOOH (Formic Acid 98–100%, Suprapur, Merck, Germany), whereas mobile phase B was 100% ACN, also containing 0.1% HCOOH.
The source of electrospray ionization (ESI) operated in positive (M+H+ and other) and negative (M-H+ and other) modes. The triple quadrupole (QQQ) instrument operated under the following conditions: column temperature 25 °C, flow rate 0.3 mL/min, scan time (0.100 s to 0.500 s), fragmentator 5–120 V, collision energy interval (5.00–50.00 eV), and scanning range (100–750 m/z).
Whole system control and data acquisition were performed using MassHunter Acquisition Software ver. C.01.00 (Agilent, Santa Clara, CA, USA). The data obtained were analyzed using Qualitative Analysis Software ver. B.08.00 (Agilent, Santa Clara, CA, USA).
3. Results
The results of the drug resistance, tests, and PCR analysis of 21 strains under study are summarized in Table 1.
Table 1.
Susceptibility testing (the disk diffusion method) and other differentiation tests for all staphylococci strains under study.
| Antimicrobial Agents or Tests | Staphylococci | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sa ATCC 25923 | Sa 1 | Sa 2 | Sa 3 | Sa 4 | Sa 5 | Sa 6 | Sa 7 | Sps ED99 | Sps 1 | Sps 2 | Sps 3 | Sps 4 | Sps 5 | Sps 6 | Sps 7 | Sps 8 | Sps 9 | Sps 10 | Sps 11 | Sps 12 | |
| Penicillins (penicillin G, amoxicillin) |
S | R | R | R | S | S | S | S | S | R | R | R | R | R | R | R | R | R | S | S | S |
| amoxicillin potentiated with clavulanic acid | S | R | R | R | S | S | S | S | S | R | R | R | R | R | R | R | R | S | S | S | S |
| Cephalosporins (cefalexin) |
S | R | R | R | S | S | S | S | S | R | R | R | R | R | R | R | R | S | S | S | S |
| tetracyclines (doxycycline, oxytetracycline) |
S | R | I | S | S | S | S | S | S | R | R | R | I | I | R | S | I | S | S | S | S |
| sulfamethoxazole potentiated with trimethoprim | S | R | I | I | S | S | S | S | S | R | R | I | R | R | R | R | I | I | S | S | S |
| Aminoglycosides (neomycin, gentamicin, amikacin) |
S | S | S | R | S | S | S | S | S | R | R | R | R | R | R | R | R | R | S | S | R |
| Quinolones (enrofloxacin, marbofloxacin, ciprofloxacin) |
S | R | I | R | S | S | S | S | S | R | R | R | R | R | R | R | R | S | R | S | S |
| polymyxins (polymyxin B) | R | R | R | R | R | R | R | R | S | S | S | S | S | S | S | S | S | S | S | S | S |
| cefoxitin (disk diffusion method) | S | R | R | R | S | S | S | S | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| oxacillin (disk diffusion method) | [S] | [R] | [R] | [R] | [S] | [S] | [S] | [S] | S | R | R | R | R | R | R | R | R | S | S | S | S |
| M-PCR (bp) |
359 | 359 | 359 | 359 | 359 | 359 | 359 | 359 | 926 | 926 | 926 | 926 | 926 | 926 | 926 | 926 | 926 | 926 | 926 | 926 | 926 |
| mecA | - | + | + | + | - | - | - | - | - | + | + | + | + | + | + | + | + | - | - | - | - |
| blaZ | - | + | + | + | - | - | - | - | - | + | + | + | + | + | + | + | + | + | - | - | - |
| coagulase (rabbit serum) |
+ | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Latex Agglutination Test | + | + | + | + | + | + | + | + | - | ± | ± | ± | ± | ± | ± | ± | ± | - | - | - | - |
| mannitol (anaerobic) | + | + | + | + | + | + | + | + | - | - | - | - | - | - | - | - | - | - | - | - | - |
Sa—Staphylococcus aureus; Sps—Staphylococcus pseudintermedius; R—resistant; I—intermediate; S—susceptible; [S] or [R]—only in disk diffusion method, the results for oxacillin are based on the results for cefoxitin; bp—base pairs; n/a—not applicable; +—positive result; (-)—negative result; ±—trace granularity.
All coagulase-positive staphylococcal strains met the required criteria. Staphylococcus aureus ATCC 25923 and Sa 1–Sa 7 isolates have characteristics common to S. aureus, e.g., an immediate reaction in a high-specific latex test capability of fermenting mannitol. A typical PCR band of 359 bp fragment of the nuc gene was also obtained. On the contrary, other strains (Sps 1–Sps 12 and ED99) have always yielded a PCR band of 926 bp (according to Sasaki et al. [16], this fragment of the nuc gene is specific only to S. pseudintermedius) and negative results for the abovementioned tests. They also had quite a characteristic double hemolysis. Additionally, all the isolates were further identified via matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF-MS) (AniCon Labor GmbH, Germany) due to the collection of strains for autovaccines. Third-party test reports confirmed the species affiliation of all staphylococci under study.
Screening for drug resistance also revealed some patterns. Both reference strains, as well as Sa 4–Sa 7 and Sps 11, were susceptible to all antibiotics tested (except Polymyxin B, because S. aureus is naturally resistant to this antibiotic) and were mecA- and blaZ negative. Sps 9, Sps 10, and Sps 12 strains showed resistance only to single antibiotics (also mecA-negative; Sps 9 was blaZ-positive with resistance only to penicillins). In contrast, the remaining isolates (Sa1–Sa 3 and Sps 1–Sps 8) were resistant to the majority of antimicrobial agents examined, including cefoxitin/oxacillin. Moreover, only these isolates were simultaneously positive for the presence of the mecA gene (527 bp) and the blaZ gene (772 bp). Compiling this information, it can be concluded that isolates Sa1–Sa3 can be considered to represent a methicillin-resistant S. aureus (MRSA), whereas Sps 1–Sps 8 are considered methicillin-resistant S. pseudintermedius (MRSP). However, further in-depth studies are needed to confirm this hypothesis.
After preliminary analyses, the first dilution of essential oils was determined at levels of 1% (patchouli; density 0.966 g/mL) and 10% (tea tree; density 0.895 g/mL). A detailed susceptibility analysis to selected antibiotics (gentamicin, enrofloxacin) and essential oils (patchouli, tea tree) using the MIC method is summarized in Table 2.
Table 2.
Minimum inhibitory concentrations (MICs) of gentamicin, enrofloxacin, and both essential oils (PcEO and MaEO) against all S. pseudintermedius and S. aureus strains.
| Strain | MIC | |||
|---|---|---|---|---|
| Gentamicin | Enrofloxacin | Patchouli | Tea Tree | |
| μg/mL | μg/mL | % v/v (mg/mL) |
% v/v (mg/mL) |
|
| Reference strain: Staphylococcus aureus ATCC 25923 |
0.5 ÷ 1 | ≤0.125 | 0.125 ÷ 0.25 (1.2 ÷ 2.4) |
1.25 ÷ 2.5 (11.2 ÷ 22.4) |
|
Staphylococcus aureus isolate Sa 1 |
0.5 ÷ 2 | 4 ÷ 8 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
2.5 ÷ 5 (22.4 ÷ 44.8) |
|
Staphylococcus aureus isolate Sa 2 |
0.5 ÷ 1 | 2 ÷ 4 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
5 ÷ 10 (44.8 ÷ 89.6) |
|
Staphylococcus aureus isolate Sa 3 |
8 ÷ 16 | 16 ÷ 32 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
2.5 ÷ 5 (22.4 ÷ 44.8) |
|
Staphylococcus aureus isolate Sa 4 |
0.5 ÷ 1 | 0.125 ÷ 0.25 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
1.25 ÷ 2.5 (11.2 ÷ 22.4) |
|
Staphylococcus aureus isolate Sa 5 |
0.25 ÷ 0.5 | 0.5 ÷ 1 | 0.125 ÷ 0.25 (1.2 ÷ 2.4) |
1.25 ÷ 2.5 (11.2 ÷ 22.4) |
|
Staphylococcus aureus isolate Sa 6 |
0.125 ÷ 0.25 | 0.125 ÷ 0.25 | 0.125 ÷ 0.25 (1.2 ÷ 2.4) |
0.625 ÷ 1.25 (5.6 ÷ 11.2) |
|
Staphylococcus aureus isolate Sa 7 |
0.0625 ÷ 0.125 | 0.032 ÷ 0.125 | 0.125 ÷ 0.25 (1.2 ÷ 2.4) |
0.625 ÷ 1.25 (5.6 ÷ 11.2) |
| Type strain: Staphylococcus pseudintermedius ED99 |
0.5 ÷ 1 | 0.125 ÷ 0.25 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
1.25 ÷ 2.5 (11.2 ÷ 22.4) |
|
Staphylococcus pseudintermedius isolate Sps 1 |
32 ÷ 64 | 32 ÷ 64 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
1.25 ÷ 5 (11.2 ÷ 44.8) |
|
Staphylococcus pseudintermedius isolate Sps 2 |
32 ÷ 64 | 32 ÷ 64 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
1.25 ÷ 2.5 (11.2 ÷ 22.4) |
|
Staphylococcus pseudintermedius isolate Sps 3 |
64 ÷ 128 | 32 ÷ 64 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
1.25 ÷ 2.5 (11.2 ÷ 22.4) |
|
Staphylococcus pseudintermedius isolate Sps 4 |
32 ÷ 64 | 32 ÷ 64 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
0.625 ÷ 1.25 (5.6 ÷ 11.2) |
|
Staphylococcus pseudintermedius isolate Sps 5 |
128 ÷ 256 | 32 ÷ 64 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
1.25 ÷ 5 (11.2 ÷ 44.8) |
|
Staphylococcus pseudintermedius isolate Sps 6 |
64 ÷ 128 | 32 ÷ 64 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
2.5 ÷ 5 (22.4 ÷ 44.8) |
|
Staphylococcus pseudintermedius isolate Sps 7 |
32 ÷ 128 | 64 ÷ 128 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
0.625 ÷ 1.25 (5.6 ÷ 11.2) |
|
Staphylococcus pseudintermedius isolate Sps 8 |
64 ÷ 128 | 32 ÷ 64 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
1.25 ÷ 2.5 (11.2 ÷ 22.4) |
|
Staphylococcus pseudintermedius isolate Sps 9 |
32 ÷ 64 | ≤0.125 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
1.25 ÷ 5 (11.2 ÷ 44.8) |
|
Staphylococcus pseudintermedius isolate Sps 10 |
0.0625 ÷ 0.125 | 32 ÷ 64 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
1.25 ÷ 2.5 (11.2 ÷ 22.4) |
|
Staphylococcus pseudintermedius isolate Sps 11 |
0.125 ÷ 0.5 | ≤0.125 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
0.625 ÷ 2.5 (5.6 ÷ 22.4) |
|
Staphylococcus pseudintermedius isolate Sps 12 |
8 ÷ 32 | 0.25 ÷ 0.5 | 0.25 ÷ 0.5 (2.4 ÷ 4.8) |
1.25 ÷ 5 (11.2 ÷ 44.8) |
In general, the MIC results for antibiotics were in agreement with the disk diffusion method. A group of staphylococci is especially notable for their high MIC values (high resistance) for both antibiotics (Sps 1 to Sps 8). The Sa3 staphylococcus strain was also characterized by significant dual resistance. One-way moderate or high resistance was also noted in the case of Sps 9 and Sps 12 (gentamicin) as well as Sa 1, Sa 2 and Sps 10 (enrofloxacin). The MIC values are also in agreement with the standards [18,19]. In the case of EOs, definitely more balanced results were obtained. For PcEO, MIC values ranging from 0.25 to 0.5% v/v (2.4–4.8 mg/mL) were recorded most often (81%; all S. pseudintermedius and antibiotic-resistant strains of S. aureus) followed by 0.125–0.25% v/v, which corresponds to a PcEO concentration of 1.2–2.4 mg/mL (19%; only for antibiotic-sensitive strains of S. aureus). The activity of MaEO was more varied regardless of drug resistance. Most often, the MIC ranged from 1.25–2.5% v/v (38% of cases; concentration 11.2–22.4 mg/mL) followed by 0.625–1.25% v/v (19%; 5.6–11.2 mg/mL), 1.25–5% v/v (19%; 11.2 ÷ 44.8 mg/mL) and 2.5–5 (14%; 22.4 ÷ 44.8 mg/mL). In summary, a tenfold stronger effect of PcEO than MaEO was noted. The DMSO content in the wells did not exceed 10%. However, our strains were still able to survive in 15–20% DMSO. This is consistent with the general knowledge of DMSO activity that the content of DMSO should not be more than 10–15%, while DMSO in amounts of 5–7.5% had no effect on MICs [20].
The essential oils were tested in combination with antimicrobial drugs against resistant (11 strains) and susceptible bacteria (10 strains), in order to check for their possible synergistic or antagonistic interactions using checkerboard method. Results can be seen in Table 3. For comparison, Table S1 (in the supplementary section) presents the corresponding results when considering the concentration of EOs expressed in mg/mL instead of % v/v. Regardless of the unit chosen, identical interactions were obtained.
Table 3.
Checkerboard analysis with final interactions (best match within triplicate).
| Antimicrobial Agent | Patchouli Oil | Tea Tree Oil | ||||||
|---|---|---|---|---|---|---|---|---|
| MICi | MICc | FIC | ∑FIC [Interaction] |
MICi | MICc | FIC | ∑FIC (Interaction) |
|
| Staphylococcus aureus ATCC 25923 | ||||||||
| oil (% v/v) | 0.25 | 0.008 | 0.032 | 0.282 synergy |
2.5 | 0.08 | 0.032 | 0.282 synergy |
| gentamicin (μg/mL) | 1 | 0.25 | 0.25 | 1 | 0.25 | 0.25 | ||
| oil (% v/v) | 0.125 | 0.125 | 1 | 2.0 none |
1.25 | 1.25 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 0.125 | 0.125 | 1 | 0.125 | 0.125 | 1 | ||
| Staphylococcus aureus Sa 1 | ||||||||
| oil (% v/v) | 0.5 | 0.125 | 0.25 | 0.75 additive |
5 | 1.25 | 0.25 | 0.5 synergy |
| gentamicin (μg/mL) | 2 | 1 | 0.5 | 0.5 | 0.125 | 0.25 | ||
| oil (% v/v) | 0.5 | 0.25 | 0.5 | 1.0 additive |
5 | 1.25 | 0.25 | 0.375 synergy |
| enrofloxacin (μg/mL) | 8 | 4 | 0.5 | 8 | 1 | 0.125 | ||
| Staphylococcus aureus Sa 2 | ||||||||
| oil (% v/v) | 0.5 | 0.125 | 0.25 | 0.75 additive |
10 | 1.25 | 0.125 | 0.25 synergy |
| gentamicin (μg/mL) | 1 | 0.5 | 0.5 | 0.5 | 0.0625 | 0.125 | ||
| oil (% v/v) | 0.25 | 0.25 | 1 | 2.0 none |
5 | 5 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 4 | 4 | 1 | 4 | 4 | 1 | ||
| Staphylococcus aureus Sa 3 | ||||||||
| oil (% v/v) | 0.5 | 0.125 | 0.25 | 0.5 synergy |
2.5 | 0.625 | 0.25 | 0.5 synergy |
| gentamicin (μg/mL) | 16 | 4 | 0.25 | 8 | 2 | 0.25 | ||
| oil (% v/v) | 0.25 | 0.25 | 1 | 2.0 none |
5 | 5 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 32 | 32 | 1 | 32 | 32 | 1 | ||
| Staphylococcus aureus Sa 4 | ||||||||
| oil (% v/v) | 0.25 | 0.125 | 0.5 | 0.625 additive |
2.5 | 0.32 | 0.128 | 0.253 synergy |
| gentamicin (μg/mL) | 0.5 | 0.0625 | 0.125 | 0.5 | 0.0625 | 0.125 | ||
| oil (% v/v) | 0.25 | 0.25 | 1 | 2.0 none |
1.25 | 1.25 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 0.25 | 0.25 | 1 | 0.125 | 0.125 | 1 | ||
| Staphylococcus aureus Sa 5 | ||||||||
| oil (% v/v) | 0.25 | 0.0625 | 0.25 | 0.75 additive |
2.5 | 0.625 | 0.25 | 0.378 synergy |
| gentamicin (μg/mL) | 0.25 | 0.125 | 0.5 | 0.25 | 0.032 | 0.128 | ||
| oil (% v/v) | 0.25 | 0.25 | 1 | 2.0 none |
1.25 | 1.25 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 1 | 1 | 1 | 0.5 | 0.5 | 1 | ||
| Staphylococcus aureus Sa 6 | ||||||||
| oil (% v/v) | 0.125 | 0.016 | 0.128 | 0.384 synergy |
1.25 | 0.16 | 0.128 | 0.256 synergy |
| gentamicin (μg/mL) | 0.125 | 0.032 | 0.256 | 0.125 | 0.016 | 0.128 | ||
| oil (% v/v) | 0.125 | 0.032 | 0.256 | 0.756 additive |
1.25 | 0.625 | 0.5 | 1.0 additive |
| enrofloxacin (μg/mL) | 0.125 | 0.0625 | 0.5 | 0.125 | 0.0625 | 0.5 | ||
| Staphylococcus aureus Sa 7 | ||||||||
| oil (% v/v) | 0.25 | 0.0625 | 0.25 | 0.506 additive |
1.25 | 0.32 | 0.256 | 0.768 additive |
| gentamicin (μg/mL) | 0.125 | 0.032 | 0.256 | 0.0625 | 0.032 | 0.512 | ||
| oil (% v/v) | 0.125 | 0.0625 | 0.5 | 1.012 additive |
0.625 | 0.625 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 0.0625 | 0.032 | 0.512 | 0.125 | 0.125 | 1 | ||
| Staphylococcus pseudintermedius ED99 | ||||||||
| oil (% v/v) | 0.25 | 0.032 | 0.128 | 0.192 synergy |
2.5 | 0.32 | 0.128 | 0.256 synergy |
| gentamicin (μg/mL) | 0.5 | 0.032 | 0.064 | 0.5 | 0.064 | 0.128 | ||
| oil (% v/v) | 0.125 | 0.008 | 0.064 | 0.564 additive |
1.25 | 1.25 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 0.25 | 0.125 | 0.5 | 0.125 | 0.125 | 1 | ||
| Staphylococcus pseudintermedius Sps 1 | ||||||||
| oil (% v/v) | 0.5 | 0.0625 | 0.125 | 0.375 synergy |
5 | 0.625 | 0.125 | 0.375 synergy |
| gentamicin (μg/mL) | 64 | 16 | 0.25 | 32 | 8 | 0.25 | ||
| oil (% v/v) | 0.25 | 0.016 | 0.064 | 0.564 additive |
1.25 | 0.08 | 0.064 | 0.314 synergy |
| enrofloxacin (μg/mL) | 32 | 16 | 0.5 | 64 | 16 | 0.25 | ||
| Staphylococcus pseudintermedius Sps 2 | ||||||||
| oil (% v/v) | 0.5 | 0.125 | 0.25 | 0.75 additive |
1.25 | 0.16 | 0.128 | 0.378 synergy |
| gentamicin (μg/mL) | 64 | 32 | 0.5 | 32 | 8 | 0.25 | ||
| oil (% v/v) | 0.25 | 0.016 | 0.064 | 0.564 additive |
1.25 | 1.25 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 64 | 32 | 0.5 | 64 | 64 | 1 | ||
| Staphylococcus pseudintermedius Sps 3 | ||||||||
| oil (% v/v) | 0.5 | 0.25 | 0.5 | 0.625 additive |
1.25 | 0.16 | 0.128 | 0.191 synergy |
| gentamicin (μg/mL) | 128 | 16 | 0.125 | 64 | 4 | 0.0625 | ||
| oil (% v/v) | 0.5 | 0.032 | 0.064 | 0.564 additive |
1.25 | 1.25 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 64 | 32 | 0.5 | 64 | 64 | 1 | ||
| Staphylococcus pseudintermedius Sps 4 | ||||||||
| oil (% v/v) | 0.5 | 0.125 | 0.25 | 0.5 synergy |
0.625 | 0.16 | 0.256 | 0.381 synergy |
| gentamicin (μg/mL) | 64 | 16 | 0.25 | 32 | 4 | 0.125 | ||
| oil (% v/v) | 0.5 | 0.5 | 1 | 2.0 none |
1.25 | 1.25 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 32 | 32 | 1 | 64 | 64 | 1 | ||
| Staphylococcus pseudintermedius Sps 5 | ||||||||
| oil (% v/v) | 0.5 | 0.125 | 0.25 | 0.5 synergy |
5 | 1.25 | 0.25 | 0.281 synergy |
| gentamicin (μg/mL) | 256 | 64 | 0.25 | 128 | 4 | 0.031 | ||
| oil (% v/v) | 0.5 | 0.032 | 0.064 | 0.564 additive |
1.25 | 0.625 | 0.5 | 1.0 additive |
| enrofloxacin (μg/mL) | 64 | 32 | 0.5 | 64 | 32 | 0.5 | ||
| Staphylococcus pseudintermedius Sps 6 | ||||||||
| oil (% v/v) | 0.5 | 0.25 | 0.5 | 0.75 additive |
2.5 | 0.32 | 0.128 | 0.159 synergy |
| gentamicin (μg/mL) | 128 | 32 | 0.25 | 64 | 2 | 0.031 | ||
| oil (% v/v) | 0.5 | 0.5 | 1 | 2.0 none |
2.5 | 2.5 | 1 | 3.0 none |
| enrofloxacin (μg/mL) | 32 | 32 | 1 | 64 | 128 | 2 | ||
| Staphylococcus pseudintermedius Sps 7 | ||||||||
| oil (% v/v) | 0.5 | 0.25 | 0.5 | 1 additive |
0.625 | 0.16 | 0.256 | 0.381 synergy |
| gentamicin (μg/mL) | 128 | 64 | 0.5 | 32 | 4 | 0.125 | ||
| oil (% v/v) | 0.5 | 0.008 | 0.016 | 0.516 additive |
1.25 | 0.625 | 0.5 | 1.0 additive |
| enrofloxacin (μg/mL) | 64 | 32 | 0.5 | 128 | 64 | 0.5 | ||
| Staphylococcus pseudintermedius Sps 8 | ||||||||
| oil (% v/v) | 0.5 | 0.125 | 0.25 | 0.75 additive |
1.25 | 0.16 | 0.128 | 0.191 synergy |
| gentamicin (μg/mL) | 128 | 64 | 0.5 | 64 | 4 | 0.0625 | ||
| oil (% v/v) | 0.5 | 0.5 | 1 | 2.0 none |
1.25 | 1.25 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 64 | 64 | 1 | 64 | 64 | 1 | ||
| Staphylococcus pseudintermedius Sps 9 | ||||||||
| oil (% v/v) | 0.5 | 0.125 | 0.25 | 0.375 synergy |
5 | 1.25 | 0.25 | 0.375 synergy |
| gentamicin (μg/mL) | 64 | 8 | 0.125 | 32 | 4 | 0.125 | ||
| oil (% v/v) | 0.5 | 0.5 | 1 | 2.0 none |
1.25 | 1.25 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 0.125 | 0.125 | 1 | 0.125 | 0.125 | 1 | ||
| Staphylococcus pseudintermedius Sps 10 | ||||||||
| oil (% v/v) | 0.5 | 0.125 | 0.25 | 0.506 additive |
1.25 | 0.32 | 0.256 | 0.512 additive |
| gentamicin (μg/mL) | 0.125 | 0.032 | 0.256 | 0.0625 | 0.016 | 0.256 | ||
| oil (% v/v) | 0.5 | 0.5 | 1 | 2.0 none |
1.25 | 1.25 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 64 | 64 | 1 | 32 | 32 | 1 | ||
| Staphylococcus pseudintermedius Sps 11 | ||||||||
| oil (% v/v) | 0.5 | 0.25 | 0.5 | 0.75 additive |
2.5 | 0.625 | 0.25 | 0.378 synergy |
| gentamicin (μg/mL) | 0.5 | 0.125 | 0.25 | 0.125 | 0.016 | 0.128 | ||
| oil (% v/v) | 0.5 | 0.5 | 1 | 2.0 none |
0.625 | 0.625 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 0.125 | 0.125 | 1 | 0.125 | 0.125 | 1 | ||
| Staphylococcus pseudintermedius Sps 12 | ||||||||
| oil (% v/v) | 0.5 | 0.25 | 0.5 | 0.75 additive |
5 | 1.25 | 0.25 | 0.5 synergy |
| gentamicin (μg/mL) | 32 | 8 | 0.25 | 8 | 2 | 0.25 | ||
| oil (% v/v) | 0.5 | 0.5 | 1 | 2.0 none |
1.25 | 1.25 | 1 | 2.0 none |
| enrofloxacin (μg/mL) | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 1 | ||
Sa—Staphylococcus aureus; Sps—Staphylococcus pseudintermedius; MICi: MIC individually as MIC(O) or MIC(A); MICc: MIC in combination as MIC(OxA) or MIC(AxO); FIC: fractional inhibitory concentrations; none = noninteractive.
Gentamicin appears to be highly prone to interacting with EOs. In 53.4% of cases, the PcEO had additive effects on S. aureus and S. pseudintermedius while synergism was observed for MaEO. There was also a significant percentage of dual synergy results (38.1%). Even the worst synergy (∑FIC = 0.5) indicates that four-fold reduction in MICs of antibiotic and EO were observed. In the case of stronger synergies, a remarkable decrease in the MIC values of EOs was observed (e.g., Sps 3/tea tree eight-fold of tea tree and up to sixteen-fold of gentamicin). A double additive effect was noted for only two staphylococci (Sa 7 and Sps 10, however near synergy), probably by the fact that these two staphylococci were the most sensitive to gentamicin (MIC 0.0625–0.125 μg/mL), which may have limited the margin for possible interaction. There were no cases with neutral or negative interaction (even within triplicates).
Enrofloxacin in combination with patchouli or tea tree oil mostly acted independently and neutrally—no interactions were observed in 57.1% of cases. Other staphylococci reacted with little reproducibility. However, the PcEO had always an additive affect whereas MaEO acted quite randomly with enrofloxacin (synergy 9.5%, additive 14.3%, noninteractive 19.1%, respectively). Among them, two staphylococci (Sa 1 and Sps 1) are worthy of extra comment because of their origin: both are isolated from the most severe cases of canine pyoderma, and, surprisingly, the best combination of interaction was obtained for them: additive (PcEO) and synergy (MaEO).
HPLC-MS Analysis
Commercial EOs are available in diluted, highly concentrated, and—rarely—in undiluted forms. Often the price of such specifics reveals its level of purity or adulteration. An attempt was therefore made to make a preliminary assessment of the composition of the oils used in the study. The volume equivalent to a concentration of 0.1% v/v of each essential oil in the MIC was examined.
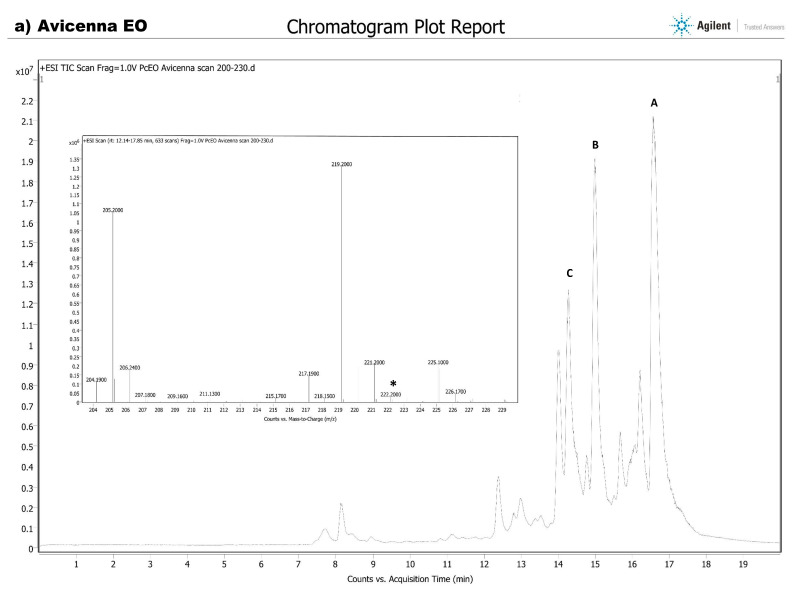
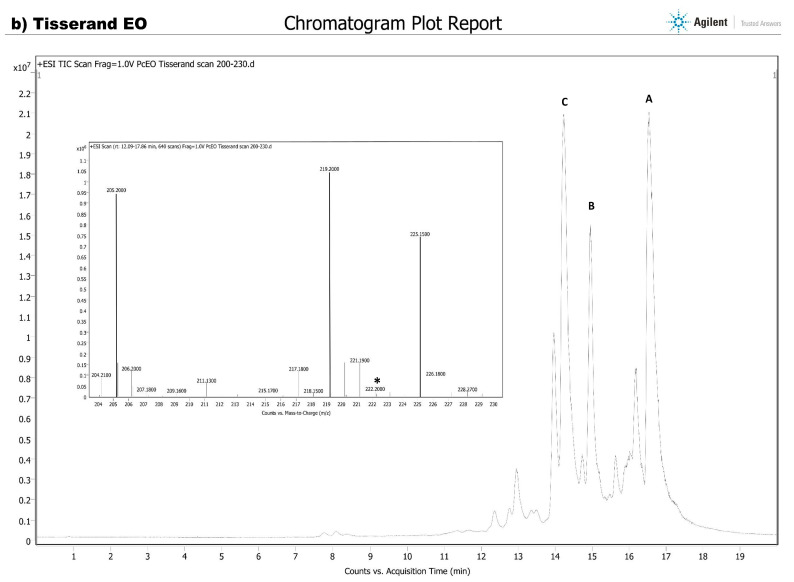
According to available gas chromatography–mass spectroscopy (GS-MS) analysis of patchouli oil, the presence of up to 30 volatile substances was identified but the main components are: patchouli alcohol (average 20–45% but sometimes up to 72%; molar mass 222.4 g/mol), followed by pogostol (222.4 g/mol; 0.2–6%), pogostone (224.3 g/mol; specific to P. cablin 0.1–27%), norpatchoulenol (206.3 g/mol; 0.1–4%), patchoulene (~8%), seychellene (~6%), α- and δ-guaiene (~18% of each), caryophellene (~8%) and bulnesene (3–23%) (204.4 g/mol of each) [21,22,23]. The nonvolatile chemical profile of PcEO was revealed for the first time using HPLC-Q-TOF-MS by Xie et al. [24], by whom an additional 73 nonvolatile constituents (i.e., 33 flavonoids, 21 organic acids, 9 phenylpropanoids, 4 sesquiterpenes, 3 alkaloids, and 3 other types of compounds) were identified and characterized (pachypodol was most abundant at 344.3 g/mol; other compounds have a molar masses usually greater than 300). In this manuscript, the scan range of patchouli oil was set from m/z 200 to 230 (covering the aforementioned volatile components), and the result is presented in Figure 1.
Figure 1.
Chromatograms and mass spectra for the patchouli oils under study: Avicenna EO (a) and Tisserand EO (b). A—major peak for mass 205.2 m/z, B—major peak for mass 219.2 m/z, C—major peak for mass 225.2 m/z. *—potential position of nonmodified patchouli alcohol—patchoulol (222.4 m/z).
To quantify patchoulol using GC-MS, m/z = 41, 55, 83, 98, 125, 138, 161, 179, 189, 207, and 222 were usually selected as the diagnostic ions (major ions are underlined; [23,25,26]. However, there are no significant data on how patchouli alcohol behaves in the mobile phase using liquid chromatography–mass spectroscopy (LC-MS) studies. Of some surprise in the presented study was the fact that there were no clear peaks, with masses ranging from 221–223 m/z, which should correspond to patchouli alcohol [222 ± H] (marked with an asterisk in Figure 1). For this purpose, the Avicenna EO was compared to a sample of some other essential oil from a highly acclaimed brand—Tisserand EO, an expert in sourcing and blending 100% natural pure essential oils since 1974. As can be seen in Figure 1, both chromatograms and mass spectra are almost identical. In both cases, the most abundant is the peak at m/z 219.2 (100% of both abundance, 1.35 × 106 and 1.05 × 106, respectively), which may be a sought-after oxygenated sesquiterpene: patchouli alcohol. Some of the PcEO sesquiterpene hydrocarbons (SQHCs), e.g., α-patchoulene and β-patchoulene are suspected to be artifacts formed through the dehydration of patchoulol and subsequent Wagner–Meerwein rearrangements during steam distillation [27]. When patchoulol is dehydrated ([M+H-H2O]+ resulted in mass m/z 205), depending on the conditions, various mixtures of patchoulenes and other rearranged hydrocarbons may be obtained (e.g., resulted in m/z 219.2). The neutral loss of -CO, H2O, -OCH3, or -CH3 was commonly observed in MS spectra. The nature of the patchoulol changes that are occurring during LC-MS remains to be explained. The second-most frequently recorded peak was m/z 205.2 (chromatogram abundance 1.05 × 106 with Abund % at 81.1 and 0.95 × 106 with Abund % at 91.25, respectively), which corresponds to an extensive and diverse group of sesquiterpenes of equal mass 204.36 g/mol ([M+H]+), including patchoulenes, guaienes, seychellenes, and bulnesenes, although a certain percentage here may be dehydrated patchoulol. Both essential oils noticeably vary in the third peak: m/z 225.2—it most likely refers to pogostone ([M+H]+). The Tisserand EO seems to be richer in this component compared to the Avicenna EO, but this observation can only be confirmed by a quantitative study. Pachypodol (m/z 343.3, [M-H]+) and several other components were also detected at a low level, which may indicate the natural origin of the essential oils.
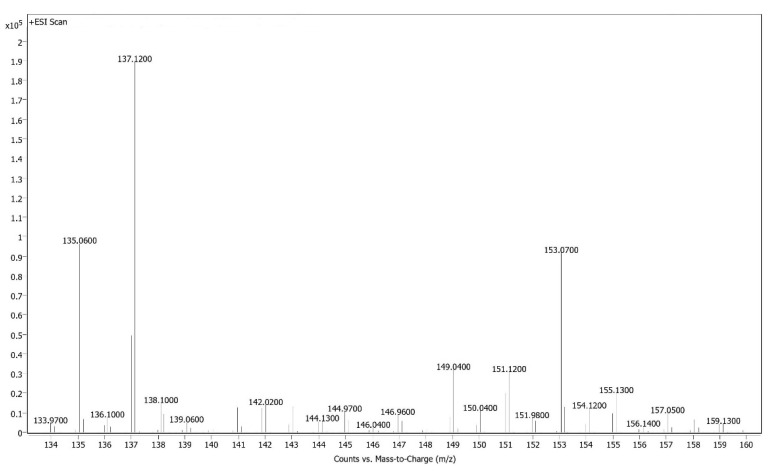
In the case of tea tree essential oil, the chemical composition of MaEO may be extremely variable, e.g., depending on chemotype (this means that several groups exist within a population of one plant species with the same morphological features differing in compositions of their products), and over 220 chemicals have been identified [28]. Essential oil of Melaleuca terpinen-4-ol type is predominant, whereas in the composition, it should have terpinen-4-ol (35–48%; 154.25 g/mol), γ-terpinene (14–28%; 136.23 g/mol), α-terpinene (6–12%; 136.23 g/mol), 1,8-Cineole/eucalyptol (0.01–10%; 154.25 g/mol), α-pinene (1–4%; 136.23 g/mol), p-cymene (0.5–8%; 134.22 g/mol), terpinolene (1.5–5%; 136.23 g/mol), α-terpineol (2–5%; 154.25 g/mol), sabinene (0.01–3.5%; 136.23 g/mol) (according to ISO 4730:2017-02 [29]). Mass spectra (range from 133 to 160, extremely specific) for the tea tree essential oil used for research (MIC and checkerboards) are summarized in Figure 2.
Figure 2.
Mass spectra for the Avicenna tea tree essential oil under study.
A high abundance of compounds with a mass-to-charge of 137 m/z was observed, which corresponds to a group of several monoterpenes with a mass of 136.23 g/mol ([M+H]+; abundance greater than 1.9 × 105). A two-fold lower abundance (approx. 1.0 × 105) was observed for compounds with a mass of 153 m/z, which probably corresponds to the neutral loss of hydrogen in terpinen-4-ol, eucalyptol, or—less possibly—α-terpineol (154.25 g/mol; [M-H]+). In contrast, the third peak (135 m/z; abundance approx. 1.0 × 105) can be either p-cymene ([M+H]+ from 134.22 g/mol) in lesser amounts or cases of hydrogen loss in a monoterpenes group. The presence of other compounds that are not natively present in MaEO (e.g., sesquiterpenes) and adulteration with fragrance compositions of synthetic origin (linalool, citronellol, etc.) were not found. In conclusion, the presence of the main MaEO-specific compounds (terpinen-4-ol and monoterpenes) was confirmed.
4. Discussion
Long-term antibiotic treatments may increase the risk of selecting for multidrug-resistant bacteria, one of the most relevant current threats to public health. Antimicrobial-resistant organisms can be transmitted to humans and other animals in the European Union and other countries through the consumption of products of animal origin, by direct contact with animals or humans, or by other means (Regulation EU No 2019/6) [30]. Alternative therapies, including essential oils (EOs), have become very popular as natural remedies in veterinary medicine. The objective of this study was the establishment of novel approaches to conventional therapies using selected EOs for the treatment of canine skin disorders. The efficacy of EOs in inhibiting a variety of classical and opportunistic pathogens depends on the plant part (e.g., leaf, flower, or bark), origin (e.g., country), seasonal variations, the method of extraction of the essential oil, the procedure used in the antimicrobial assays (e.g., different broth), and the target microbial isolate [31]. Different staphylococcal species (incl. S. pseudintermedius) isolated from canine dermatitis were examined in study by Ebani et al. [32]. Among them, oregano (Origanum vulgare L.) and thyme (Thymus vulgaris L.) EOs resulted highly active against all staphylococcal strains tested. The research conducted by Nocera et al. [7] aimed to test in vitro the antimicrobial activity of 11 EOs (e.g., cinnamon or eucalyptus) against four methicillin-resistant Staphylococcus pseudintermedius (MRSP) and four methicillin-susceptible S. pseudintermedius (MSSP) pyoderma-associated clinical isolates. The obtained findings demonstrated a clear in vitro efficacy of some tested EOs against both MRSP and MSSP strains isolated from dogs. Unfortunately, neither study included both PcEO and MaEO.
Patchouli essential oil (PcEO) is obtained by steam distillation or hydrodistillation of the dried leaves of Pogostemon cablin (Blanco) Benth. (Lamiaceae). It has a unique woody odor—utilized in high-end fragrances and cosmetics [27]. This plant originated in Southeast Asia, Madagascar, India, Brazil, Japan, and China, but 90% of patchouli oil around the world is supplied from Indonesia [21]. Given its multicomponent nature, PcEO is also a part of a traditional Chinese medicine that has been used for the treatment of many ailments for centuries, e.g., to treat colds, nausea, fever, headache, and diarrhea [24,33]. Biofilms formed by bacteria are associated with highly enhanced resistance against antimicrobial agents, resulting in therapy failure. However, the PcEO may significantly inhibited the initial adherence phase of S. aureus biofilm development [34].
Using the disk diffusion method, Karimi [35] revealed that freshly hydrodistilated Philippine patchouli oil was found to be active only against the Gram-positive bacteria (Staphylococcus aureus ATCC 25923 and other Staphylococcus sp., Bacillus sp., and Streptococcus species). Moreover, both hospital and community clinical human isolates of methicillin-sensitive (MSSA) and methicillin-resistant (MRSA) S. aureus were sensitive to an MIC range of 0.03–0.06% v/v. High antistaphylococcal potential of PcEO has been confirmed for the group of 31 strains isolated from cases of bovine mastitis (MIC ranging from 0.01% v/v to 0.312% v/v) and the reference strain S. aureus PCM 2051 (0.625% v/v) using commercial oil (Pollena Aroma, Poland) [36]. The results of MICs performed by Yang et al. [37] showed that patchouli oil and its main components (patchouli alcohol and pogostone) have good antibacterial activities against Staphylococcus aureus ATCC2925 (MIC at the level of 4.5 mg/mL, 2 mg/mL and 1 mg/mL, respectively). Other studies showed that pure PcEO at > 40 μL/mL concentration reduced the growth of Staphylococcus aureus ATCC 6538 reference strain [38]. The high efficacy of PcEO against staphylococci (even multidrug-resistant ones) is also confirmed by the results in the presented manuscript, where the MIC ranged from 0.125 to 0.5% v/v that correspond to average PcEO concentrations of 1.2–4.8 mg/mL. To our knowledge, we also present the first study of the in vitro activity of PcEO against S. pseudintermedius.
Tea tree essential oil (MaEO) is the volatile oil obtained by distillation from the leaves and terminal branchlets of Melaleuca alternifolia (Maiden et Betche) Cheel [29]. As mentioned previously, the chemical composition of MaEO may be extremely variable depending on multiple parameters, such as biomass used (from wild or cultivated trees; only leaves or leaves plus terminal branchlets); chemotype (according to ISO 4730:2017-02); and mode of production (steam distillation versus hydrodistillation) [28].
The activity of tea tree oil against S. aureus is definitely better documented in the scientific literature. May et al. [39] reported MaEO MICs and minimum bactericidal concentrations (MBCs) of 0.12–0.5% for S. aureus (including MRSA) as well as time-kill studies in which essential oil with increased concentration of terpinen-4-ol displayed enhanced antimicrobial activity (4 h instead of 6 h for standard tea tree oil). The mechanisms of action of MaEO and three of its components—1,8-cineole, terpinen-4-ol, and α-terpineol—against Staphylococcus aureus ATCC 9144 were also investigated by Carson et al. [40]. At inocula of 5.0 × 105 and 5.0 × 107 CFU/mL, the MICs and MBCs were both 0.25% and 0.5% v/v, respectively. At an inoculum of 5.0 × 109 CFU/mL, the MIC was 0.5% v/v and the MBC was 1% v/v. An identical result was obtained by Nelson [41], while similar results (0.12–0.5% v/v) against various methicillin resistant strains of seven species of Staphylococcus, including S. aureus were reported by Harkenthal et al. [42]. A slightly higher value for MSSA and MRSA was reported by Oliva et al. [43]—0.5–2% v/v. In our study, at inocula of approx. 1.0 × 106 CFU/mL per well, the MIC ranged from 0.625 to 1.25% or 5.6–11.2 mg/mL (susceptible strains of S. aureus) and 2.5 to 10% v/v (multidrug-resistant strains), which refers to the MaEO concentration range of 22.4–89.6 mg/mL. A similarly high MIC (5 ÷ 10%) was reported by De Martini et al. [44] for 17 coagulase-positive Staphylococci (CoPS) isolated from canine otitis externa cases. In contrast to all the above results, extremely low MIC values were also reported. Mann and Markham [45] and Kumari et al. [46] reported an MIC value of 0.02–0.04% v/v of tea tree oil against S. aureus.
In a study performed by Meroni et al. [47], a total of 23 S. pseudintermedius strains were collected from clinical samples (pyoderma) from different dogs. The majority of them (61%) were resistant to more than three pharmacological categories and were classified as multidrug-resistant. These authors reported slightly higher or similar MICs (7.6 ± 3.2% v/v) to those presented in this manuscript (0.625 ÷ 5% v/v). In the study of Valentine et al. [48], a total of 25 MRSP and 25 MSSP isolates from dogs with skin and soft tissue infections were included. Tea tree oil has been shown to inhibit the growth of both types of S. pseudintermedius strains, with MICs ranging from 0.12 to 0.96% v/v and from <0.03 to 0.96% v/v, respectively. In an experiment by Han et al. [49], the antimicrobial effects of a topical skin cream (Korean Dara cream®) consisting of four natural oils (emu oil, jojoba oil, avocado oil, and tea tree oil) were evaluated through measurements of MIC (0.23% v/v) against three S. pseudintermedius isolates obtained from the nostrils of healthy dogs.
The antibacterial activity of pure terpinen-4-ol on S. aureus reference strains (ATCC 25923, ATCC 13150, NCTC 6571 and NCTC 29213) and clinical isolates was assessed by determining the MIC (0.25% v/v in most cases) and MBC (mostly 0.5 % v/v) in few studies in the scientific literature [50,51,52]. In the presented manuscript, the MIC values were 5–10-fold higher when a commercial MaEO was used instead of terpinen-4-ol. Probably the low content of terpinen-4-ol in Avicenna essential oil caused this result. According to Avicenna Oil’s official certificate of laboratory analysis (batch no. 27947), the terpinen-4-ol content was at the level of 40.4% (2.5 times lower than the pure reagent). The strong antibiofilm activity of terpinen-4-ol against S. aureus was found in the study by Cordeiro et al. [52] in a concentration-dependent manner even at sub-MIC concentrations. Moreover, in silico molecular docking analysis showed a possible interaction between terpinen-4-ol and penicillin-binding protein 2a (PBP2a), which is one of the main molecules involved in staphylococci resistance to beta-lactam drugs. Apart from beta-lactamases being used to inactivate the antibiotic, MRSA and MRSP strain resistance is mediated through the acquisition of a gene cassette containing the mecA gene, which encodes the low-affinity altered transpeptidase PBP2a [53]. Thus, the effective binding of terpinen-4-ol to the PBP2a protein and the consequent inhibition of its activity can be an effective adjuvant tool in the treatment of resistant strains [52]. These observations are in agreement with our study, as the presence of this gene was confirmed in many of the multidrug-resistant strains studied in this manuscript (Sa1–Sa3 and Sps1–Sps8). In addition, resistance to penicillins in staphylococci is also mediated by β-lactamases encoded by the blaZ gene [17]. Unfortunately, only interactions with the main representatives of aminoglycosides and fluoroquinolones (without identifying their individual resistance genes) but not beta-lactam drugs have been studied, so this may be a goal for future studies.
Essential oils, due to the small scale on which they are obtained, sometimes have a high price, which encourages dishonest manufacturers and distributors to adulterate them. The main methods of adulterating EOs are to dilute them with vegetable fat, mix them with cheaper EOs, or to add synthetic components to mimic the olfactory properties or the composition of the chemotype [54,55]. While in the first case, the natural fragrance bouquet does not change (it is only less intense), when other compounds are introduced (e.g., various terpenes), the fragrance impression is significantly modified. Such modifications can also affect the antimicrobial activity of EOs [56]. In our study, both commercial Avicenna-brand EOs tested via HPLC-MS were characterized by an appropriate composition that does not vary from the literature data. There was also no adulteration with additional fragrance compounds, such as linalool, citronellol, or limonene, which could alter their properties. Furthermore, the Avicenna patchouli oil had a similar composition to an essential oil from an established brand that was more expensive.
5. Conclusions
Both commercial EOs were characterized by natural composition without artificial adulteration. Patchouli and tea tree oils can be good alternatives for treating severe cases of pyoderma in dogs, especially when dealing with multidrug-resistant strains. Gentamicin, in comparison to enrofloxacin, appears to be highly prone to interacting with EOs. It is noticeable that patchouli oil had several times stronger of an effect on staphylococci compared to tea tree oil. However, tea tree oil is characterized by a stronger synergistic effect, having great potential as long as the natural products contain predominantly terpinen-4-ol. In the future, it is advisable to conduct tests with several oils from different manufacturers (and, e.g., variable chemotypes) as well as their interaction with beta-lactams to confirm the observations obtained.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ani13081279/s1, Table S1. Checkerboard analysis with final interactions when the essential oil concentration is expressed in mg/mL instead % v/v (best match within triplicate; differences to Table 3. are highlighted in bold and red).
Author Contributions
Conceptualization, M.A.S. and S.Z.; data curation, S.Z.; dormal analysis, M.A.S., S.Z., and N.O.; investigation, M.A.S., S.Z., and N.O.; methodology, M.A.S. and S.Z.; resources, J.K.; software, S.Z.; validation, S.Z.; writing—original draft, S.Z. and N.O.; writing—review and editing, M.A.S. and J.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable (only bacterial strains were used; no animals were used in the study).
Informed Consent Statement
Not applicable.
Data Availability Statement
All data generated or analyzed during the study are included in this published article. The datasets used and/or analyzed in the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Loeffler A., Lloyd D.H. What has changed in canine pyoderma? A narrative review. Vet. J. 2018;235:73–82. doi: 10.1016/j.tvjl.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Seckerdieck F., Mueller R.S. Recurrent pyoderma and its underlying primary diseases: A retrospective evaluation of 157 dogs. Vet. Rec. 2018;182:434. doi: 10.1136/vr.104420. [DOI] [PubMed] [Google Scholar]
- 3.Mesman M.L., Kirby A.L., Rosenkrantz W.S., Griffin C.E. Residual antibacterial activity of canine hair treated with topical antimicrobial sprays against Staphylococcus pseudintermedius in vitro. Vet. Dermatol. 2016;27:261-e61. doi: 10.1111/vde.12318. [DOI] [PubMed] [Google Scholar]
- 4.Löwenstein C. Pyoderma in dogs. Tierärztl. Prax. 2011;39:405–417. [PubMed] [Google Scholar]
- 5.Szewczuk M.A., Zych S., Sablik P. Participation and drug resistance of coagulase-positive staphylococci isolated from cases of pyoderma and otitis externa in dogs. Slov. Vet. Res. 2020;57:33–43. [Google Scholar]
- 6.Beco L., Guaguère E., Lorente Méndez C., Noli C., Nuttall T., Vroom M. Suggested guidelines for using systemic antimicrobials in bacterial skin infections: Part 2-antimicrobial choice, treatment regimens and compliance. Vet. Rec. 2013;172:156–160. doi: 10.1136/vr.101070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nocera F.P., Mancini S., Najar B., Bertelloni F., Pistelli L., De Filippis A., Fiorito F., De Martino L., Fratini F. Antimicrobial activity of some essential oils against methicillin-susceptible and methicillin-resistant Staphylococcus pseudintermedius-associated pyoderma in dogs. Animals. 2020;10:1782. doi: 10.3390/ani10101782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Börjesson S., Gómez-Sanz E., Ekström K., Torres C., Grönlund U. Staphylococcus pseudintermedius can be misdiagnosed as Staphylococcus aureus in humans with dog bite wounds. Eur. J. Clin. Microbiol. Infect. Dis. 2015;34:839–844. doi: 10.1007/s10096-014-2300-y. [DOI] [PubMed] [Google Scholar]
- 9.Tongnuanchan P., Benjakul S. Essential oils: Extraction, bioactivities, and their uses for food preservation. J. Food Sci. 2014;79:R1231–R1249. doi: 10.1111/1750-3841.12492. [DOI] [PubMed] [Google Scholar]
- 10.Masyita A., Mustika Sari R., Dwi Astuti A., Yasir B., Rahma Rumata N., Emran T.B., Nainu F., Simal-Gandara J. Terpenes and terpenoids as main bioactive compounds of essential oils, their roles in human health and potential application as natural food preservatives. Food Chem. X. 2022;13:100217. doi: 10.1016/j.fochx.2022.100217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chouhan S., Sharma K., Guleria S. Antimicrobial activity of some essential oils—Present status and future perspectives. Medicines. 2017;4:58. doi: 10.3390/medicines4030058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaloustian J., Chevalier J., Mikail C., Martino M., Abou L., Vergnes M.F. Étude de six huiles essentielles composition chimique et activité antibactérienne. Phytothérapie. 2008;6:160–164. doi: 10.1007/s10298-008-0307-1. [DOI] [Google Scholar]
- 13.Devi K.P., Nisha S.A., Sakthivel R., Pandian S.K. Eugenol (an essential oil of clove) acts as an antibacterial agent against Salmonella Typhi by disrupting the cellular membrane. J. Ethnopharmacol. 2010;130:107–115. doi: 10.1016/j.jep.2010.04.025. [DOI] [PubMed] [Google Scholar]
- 14.Stefanakis M.K., Touloupakis E., Anastasopoulos E., Ghanotakis D., Katerinopoulos H.E., Makridis P. Antibacterial activity of essential oils from plants of the genus Origanum. Food Control. 2013;34:539–546. doi: 10.1016/j.foodcont.2013.05.024. [DOI] [Google Scholar]
- 15.Van Vuuren S., Viljoen A. Plant-based antimicrobial studies—Methods and approaches to study the interaction between natural products. Planta Med. 2011;77:1168–1182. doi: 10.1055/s-0030-1250736. [DOI] [PubMed] [Google Scholar]
- 16.Sasaki T., Tsubakishita S., Tanaka Y., Sakusabe A., Ohtsuka M., Hirotaki S., Kawakami T., Fukata T., Hiramatsu K. Multiplex-PCR method for species identification of coagulase-positive staphylococci. J. Clin. Microbiol. 2010;48:765–769. doi: 10.1128/JCM.01232-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ruzauskas M., Couto N., Pavilonis A., Klimiene I., Siugzdiniene R., Virgailis M., Vaskeviciute L., Anskiene L., Pomba C. Characterization of Staphylococcus pseudintermedius isolated from diseased dogs in Lithuania. Pol. J. Vet. Sci. 2016;19:7–14. doi: 10.1515/pjvs-2016-0002. [DOI] [PubMed] [Google Scholar]
- 18.Clinical and Laboratory Standards Institute (CLSI) Performance Standards for Antimicrobial Susceptibility Testing, M100. 31st ed. Clinical and Laboratory Standards Institute; Wayne, PA, USA: 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clinical and Laboratory Standards Institute (CLSI) Performance Standards for Antimicrobial Disk and Dilution Susceptibility Tests for Bacteria Isolated from Animals, VET01S. 5th ed. CLSI Supplement; Wayne, PA, USA: 2020. [Google Scholar]
- 20.Mi H., Wang D., Xue Y., Zhang Z., Niu J., Hong Y., Drlica K., Zhao X. Dimethyl sulfoxide protects Escherichia coli from rapid antimicrobial-mediated killing. Antimicrob. Agents Chemother. 2016;60:5054–5058. doi: 10.1128/AAC.03003-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ermaya D., Sari S.P., Patria A., Hidayat F., Razi F. Identification of patchouli oil chemical components as the results on distillation using GC-MS. IOP Conf. Ser. Earth Environ. Sci. 2019;365:012039. doi: 10.1088/1755-1315/365/1/012039. [DOI] [Google Scholar]
- 22.Santos L.L., Brandão B.L., Martins L.R., Rabelo M.E., Rodrigues L.A.B., Araújo C.V.C.M., Sobral F.T., Galardo R.A.K., Ameida M.S.S.S. Evaluation of the larvicidal potential of the essential oil Pogostemon cablin (Blanco) Benth in the control of Aedes aegypti. Pharmaceuticals. 2019;12:53. doi: 10.3390/ph12020053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Souhoka F.A., Al Aziz A.Z., Nazudin N. Patchouli oil isolation and identification of chemical components using GC-MS. Indo. J. Chem. Res. 2020;8:108–113. doi: 10.30598//ijcr.2020.8-fas. [DOI] [Google Scholar]
- 24.Xie B., Wu X.F., Luo H.T., Huang X.L., Huang F., Zhang Q.Y., Zhou X., Wu H.Q. Chemical profiling and quality evaluation of Pogostemon cablin Benth by liquid chromatography tandem mass spectrometry combined with multivariate statistical analysis. J. Pharm. Biomed. Anal. 2022;209:114526. doi: 10.1016/j.jpba.2021.114526. [DOI] [PubMed] [Google Scholar]
- 25.Deguerry F., Pastore L., Wu S., Clark A., Chappell J., Schalk M. The diverse sesquiterpene profile of patchouli, Pogostemon cablin, is correlated with a limited number of sesquiterpene synthases. Arch. Biochem. Biophys. 2006;454:123–136. doi: 10.1016/j.abb.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Y., Zhou L., Tang K., Xu M., Miao Z. Matching is the key factor to improve the production of patchoulol in the plant chassis of Marchantia paleacea. ACS Omega. 2020;51:33028–33038. doi: 10.1021/acsomega.0c04391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Van Beek T.A., Joulain D. The essential oil of patchouli, Pogostemon cablin: A review. Flavour Fragr. J. 2018;33:6–51. doi: 10.1002/ffj.3418. [DOI] [Google Scholar]
- 28.De Groot A.C., Schmidt E. Tea tree oil: Contact allergy and chemical composition. Contact Dermat. 2016;75:129–143. doi: 10.1111/cod.12591. [DOI] [PubMed] [Google Scholar]
- 29.Essential Oil of Melaleuca Terpinen-4-ol Type (Tea Tree Oil) International Organisation for Standardisation; Geneva, Switzerland: 2017. [Google Scholar]
- 30.Regulation (EU) 2019/6 of the European Parliament and of the Council of 11 December 2018 on Veterinary Medicinal Products and Repealing Directive 2001/82/EC. Official Journal of the European Union; Luxembourg: 2018. [Google Scholar]
- 31.Lima C.O., Barreto H.M., de Oliveira Lima E., de Souza E.L., de Siqueira J.P., Jr. Antimicrobial effect of the essential oil from Rosmarinus officinalis L. against Staphylococcus pseudintermedius isolated from dogs. Rev. Bras. Biocienc. 2013;11:280–283. [Google Scholar]
- 32.Ebani V.V., Bertelloni F., Najar B., Nardoni S., Pistelli L., Mancianti F. Antimicrobial activity of essential oils against Staphylococcus and Malassezia strains isolated from canine dermatitis. Microorganisms. 2020;8:252. doi: 10.3390/microorganisms8020252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Junren C., Xiaofang X., Mengting L., Qiuyun X., Gangmin L., Huiqiong Z., Guanru C., Xin X., Yanpeng Y., Fu P., et al. Pharmacological activities and mechanisms of action of Pogostemon cablin Benth: A review. Chin. Med. 2021;16:5. doi: 10.1186/s13020-020-00413-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bilcu M., Grumezescu A.M., Oprea A.E., Popescu R.C., Mogoșanu G.D., Hristu R., Stanciu G.A., Mihailescu D.F., Lazar V., Bezirtzoglou E., et al. Efficiency of vanilla, patchouli and ylang essential oils stabilized by iron oxide@C14 nanostructures against bacterial adherence and biofilms formed by Staphylococcus aureus and Klebsiella pneumoniae clinical strains. Molecules. 2014;19:17943–17956. doi: 10.3390/molecules191117943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karimi A. Characterization and antimicrobial activity of patchouli essential oil extracted from Pogostemon cablin [Blanco] Benth. [lamiaceae] Adv. Environ. Biol. 2014;8:2301–2309. [Google Scholar]
- 36.Szweda P., Zalewska M., Pilch J., Kot B., Milewski S. Essential oils as potential anti-staphylococcal agents. Acta Vet. Beogr. 2018;68:95–107. [Google Scholar]
- 37.Yang X., Zhang X., Yang S.P., Liu W.Q. Evaluation of the antibacterial activity of patchouli oil. Iran J. Pharm. Res. 2013;12:307–316. [PMC free article] [PubMed] [Google Scholar]
- 38.Tadtong S., Puengseangdee C., Prasertthanawut S., Hongratanaworakit T. Antimicrobial constituents and effects of blended eucalyptus, rosemary, patchouli, pine, and cajuput essential oils. Nat. Prod. Commun. 2016;11:267–270. doi: 10.1177/1934578X1601100234. [DOI] [PubMed] [Google Scholar]
- 39.May J., Chan C.H., King A., Williams L., French G.L. Time-kill studies of tea tree oils on clinical isolates. J. Antimicrob. Chemother. 2000;45:639–643. doi: 10.1093/jac/45.5.639. [DOI] [PubMed] [Google Scholar]
- 40.Carson C.F., Mee B.J., Riley T.V. Mechanism of action of Melaleuca alternifolia (tea tree) oil on Staphylococcus aureus determined by time-kill, lysis, leakage, and salt tolerance assays and electron microscopy. Antimicrob. Agents Chemother. 2002;46:1914–1920. doi: 10.1128/AAC.46.6.1914-1920.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nelson R.R.S. In vitro activities of five plant essential oils against methicillin–resistant Staphylococcus aureus and vancomycin—Resistant Enterococcus faecium. J. Antimicrob. Chemother. 1997;40:305–306. doi: 10.1093/jac/40.2.305. [DOI] [PubMed] [Google Scholar]
- 42.Harkenthal M., Reichling J., Geiss H.K., Saller R. Comparative study on the in vitro antibacterial activity of Australian tea tree oil, niaouli oil, manuka oil, kanuka oil, and eucalyptus oil. Pharmazie. 1999;54:460–463. [PubMed] [Google Scholar]
- 43.Oliva A., Costantini S., De Angelis M., Garzoli S., Božović M., Mascellino M.T., Vullo V., Ragno R. High potency of Melaleuca alternifolia essential oil against multi-drug resistant Gram-negative bacteria and methicillin-resistant Staphylococcus aureus. Molecules. 2018;23:2584. doi: 10.3390/molecules23102584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.De Martini M.C.A., Suthovski G., Catarina A.S., Fagundes K.R., Giotto C.C., Schmitz E.P.S., Gallina A.L., Azevedo M.G.B., Starikoff K.R., Champion T., et al. Antimicrobial activity of essential oils against positive coagulase Staphylococcus isolated from external canine otitis cases. Rev. Agric. Acad. 2021;4:43–52. doi: 10.32406/v4n2/2021/43-52/agrariacad. [DOI] [Google Scholar]
- 45.Mann M.C., Markham L.J. A new method for determining the minimum inhibitory concentration of essential oils. J. Appl. Microbiol. 1998;84:538–544. doi: 10.1046/j.1365-2672.1998.00379.x. [DOI] [PubMed] [Google Scholar]
- 46.Kumari P., Benjamin J.C., Lawrence R. Antibacterial activity of tea tree (Melaleuca alternifolia) oil against methicillin resistant Staphylococcus aureus. Int. J. Curr. Microbiol. App. Sci. 2018;7:1116–1123. [Google Scholar]
- 47.Meroni G., Cardin E., Rendina C., Herrera Millar V.R., Soares Filipe J.F., Martino P.A. In vitro efficacy of essential oils from Melaleuca alternifolia and Rosmarinus officinalis, Manuka honey-based gel, and Propolis as antibacterial agents against canine Staphylococcus pseudintermedius strains. Antibiotics. 2020;9:344. doi: 10.3390/antibiotics9060344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Valentine B.K., Dew W., Yu A., Weese J.S. In vitro evaluation of topical biocide and antimicrobial susceptibility of Staphylococcus pseudintermedius from dogs. Vet. Dermatol. 2012;23:493-e95. doi: 10.1111/j.1365-3164.2012.01095.x. [DOI] [PubMed] [Google Scholar]
- 49.Han J.I., Park S.J., Kim S.G., Park H.M. Antimicrobial effects of topical skin cream containing natural oil mixtures against Staphylococcus pseudintermedius and Malassezia pachydermatis. Vet. Med. 2015;60:202–207. doi: 10.17221/8108-VETMED. [DOI] [Google Scholar]
- 50.Loughlin R., Gilmore B.F., McCarron P.A., Tunney M.M. Comparison of the cidal activity of tea tree oil and terpinen-4-ol against clinical bacterial skin isolates and human fibroblast cells. Lett. Appl. Microbiol. 2008;46:428–433. doi: 10.1111/j.1472-765X.2008.02334.x. [DOI] [PubMed] [Google Scholar]
- 51.Hammer K.A., Carson C.F., Riley T.V. Effects of Melaleuca alternifolia (tea tree) essential oil and the major monoterpene component terpinen-4-ol on the development of single-and multistep antibiotic resistance and antimicrobial susceptibility. Antimicrob. Agents Chemother. 2012;56:909–915. doi: 10.1128/AAC.05741-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cordeiro L., Figueiredo P., Souza H., Sousa A., Andrade-Júnior F., Medeiros D., Nóbrega J., Silva D., Martins E., Barbosa-Filho J., et al. Terpinen-4-ol as an antibacterial and antibiofilm agent against Staphylococcus aureus. Int. J. Mol. Sci. 2020;21:4531. doi: 10.3390/ijms21124531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shalaby M.A.W., Dokla E.M., Serya R.A., Abouzid K.A. Penicillin binding protein 2a: An overview and a medicinal chemistry perspective. Eur. J. Med. Chem. 2020;199:112312. doi: 10.1016/j.ejmech.2020.112312. [DOI] [PubMed] [Google Scholar]
- 54.Jentzsch P.V., Ramos L.A., Ciobota V. Detection of essential oils adulteration: A quick overview and current challenges. Am. J. Biomed. Sci. Res. 2019;15:10–11. doi: 10.34297/AJBSR.2019.04.000746. [DOI] [Google Scholar]
- 55.Pierson M., Fernandez X., Antoniotti S. Type and magnitude of non-compliance and adulteration in neroli, mandarin and bergamot essential oils purchased on-line: Potential consumer vulnerability. Sci. Rep. 2021;11:11096. doi: 10.1038/s41598-021-90307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Capetti F., Marengo A., Cagliero C., Liberto E., Bicchi C., Rubiolo P., Sgorbini B. Adulteration of essential oils: A multitask issue for quality control. Three case studies: Lavandula angustifolia Mill., Citrus limon (L.) Osbeck and Melaleuca alternifolia (Maiden & Betche) Cheel. Molecules. 2021;26:5610. doi: 10.3390/molecules26185610. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during the study are included in this published article. The datasets used and/or analyzed in the current study are available from the corresponding author on reasonable request.