Abstract
Background
The Covid-19 has made a huge impact on higher education. Online teaching and learning became essential to deliver educational activities in all areas including medical education. In this study, we aimed to investigate medical students’ perceptions on the role of online teaching and learning in facilitating medical education.
Material and Methods
A cross-sectional study using a self-administered online questionnaire was conducted. Students eligible were medical students across all years at Imam Abdulrahman Bin Faisal University, Saudi Arabia. Perceptions analysis was conducted using SPSS software.
Results
A total of 563 students participated in the study (prominent category female 64%, n = 361). There was a significant increase in the number of hours devoted to online learning during the pandemic. Live lectures/tutorials platform via zoom showed the highest rate of interaction compared to pre-recorded lectures and learning materials uploaded on blackboard. 50% of the students disagreed that online teaching is as effective as face-to-face teaching. The greatest perceived enjoyable aspect included the online accessibility of materials. Whereas the most frequent perceived barrier to online learning included internet connection. 17% of students reflected a poor understanding of scientific materials through online PBL. More than 50% of students revealed that online theoretical lectures are as good as classroom or better. Whereas the majority (70%) were unable to learn clinical skills online. The results indicated high impact on students’ physical activities (80%). Impacts were higher on pre-clinical students’ health and social life than on clinical students.
Conclusion
Our findings reported that during emergency situations due to the pandemic, online teaching enables the continuity of medical education and provides adequate efficiency. The use of live online platforms showed high level of interaction. However, some barriers need to be addressed especially at the clinical skills development level to maximize the benefit of online teaching and learning.
Keywords: COVID-19, medical education, social impact, remote learning, barriers
Introduction
In March 2020, the World Health Organization (WHO) declared Covid-19 a global pandemic following its worldwide spread.1 In response to Covid-19, the Government of Saudi Arabia set and enforced countrywide lockdown restrictions that put in place greatly impacted entire aspects of everyday life, and inevitably education.2,3 The pandemic had forced business meetings, all types of social and religious gatherings and education at all levels to be transformed virtually.4
In the College of Medicine at Imam Abdulrahman Bin Faisal University (IAU), Saudi Arabia, the Bachelor of Medicine and Bachelor of Surgery (MBBS) program incorporates innovative approaches in medical education including the use of online platforms such as blackboard, an online platform that allows students and faculty to use online materials and activities to complement face-to-face teaching.5 Prior to the Covid-19 pandemic, several techniques including e-learning were introduced to enhance teaching and consequently amplify high levels of engagement in medical education.2,6–8
Globally, as in Saudi Arabia due to the restrictions set by the government during the pandemic, solely online platforms are in use, becoming the primary source for teaching and learning.3,4,9,10
Consequently, many studies have explored the effect of shifting to online education during the pandemic, considering both the teachers and the students’ viewpoints. Entire aspects of medical education are addressed, including curriculum and course design, teaching and learning methods, learning environment and student engagement, examinations and assessment practices.
Adaptation to technically enhanced approaches has already been introduced since the last two decades, with perceived developments throughout the years.6 Advanced technologies make education and learning environment easy, efficient and accessible for the students and proven to have high-quality levels of engagement in medical education.2,6–8 Results of a latest systematic review have revealed equivalence between the traditional classroom teaching “offline teaching” and online teaching in terms of the assessment outcomes.11
Online teaching and learning play a key role in medical education and are known to have several benefits in fostering students’ learning.2 However, the impact of exclusive online education might vary across different academic years. Regarding the various components of the undergraduate curriculum, research has suggested that impacts of exclusive online anatomical teaching for example, are more beneficial if compared to clinical teaching and learning.12,13 Students of preclinical years have also reflected that online prerecorded videos are efficient for learning.14 Other practical and clinical components of the curriculum such as basic clinical exposure (like history taking),15 field trip, anatomy laboratory, small group discussions and library time9 are found to be adversely affected by the imposed shift online.
All through the clinical years, students learn through several modalities including attending clinical rotations, acting as members of health-care teams, working together within multidisciplinary teams, observing, and interviewing patients, preparing morning case reports for supervisors, and practicing newly learnt clinical skills under supervision.15 During the Covid-19 pandemic and due to the shift to exclusive online medical education, the practice and development of the required clinical competencies has been disrupted which might negatively impact the provision of patient care and professionalism.16,17 A recent study exploring the role of virtual mock Objective Structures Clinical Examinations (OSCEs) suggests that these have a role in preparing medical students for their summative exams. However, this role was not reflected in their confidence levels.18
Nevertheless, some potential benefits of online technologies are reported including easy and comfortable use, worldwide acceptability besides the reductions in cost and air pollution due to less need for transportation.2,7,19–22 On the other hand, significant issues have been pointed out about the use of entirely online education such as: physical and social isolation, increased use of emails, difficulty to keep boundaries between time at the workplace and at home, lack of interaction, disturbance and technical problems, deficiency in integrated teaching and bed-side teaching, inadequate teaching and learning in practical and clinical settings besides time constraints for effective implementation of online education.9,11,22
Effectiveness of online education is difficult to quantify because of different parameters and perceptions.6,23,24 Since undergraduate medical students have been entirely dependent on online education during this pandemic,22 their perceptions towards online teaching and learning will inform the evaluation of its effectiveness. Therefore, this study aims to investigate medical students’ perceptions on the role of online teaching and learning in facilitating their education during the Covid-19 pandemic.
Materials and Methods
Study Design
In response to the country’s lockdown, face-to-face teaching and learning at the College of Medicine at IAU were suspended. All educational activities were conducted online by using virtual platforms.
After three and a half semesters of online learning that started in March 2020, a cross-sectional study was conducted to investigate the students’ perceptions of online teaching and learning. All students who are currently enrolled in the College of Medicine at IAU were invited to participate in the current online anonymous questionnaire-based study. Our study participants included all students (1240 students, male 50.5% and female 49.5%) from the preclinical years (2nd–3rd) and the clinical years (4th–6th).
Sample
A minimum sample size (380) of participants was estimated using a confidence level of 95% and a 5% margin of error was respected. A total number of 563 students responded to the questionnaire. All the eligible participants were informed about the purpose of the current study as clarified by a brief description in the first page of the questionnaire. Each student could complete the survey only once. Participation was voluntary and participants were assured of anonymity and data confidentiality. To proceed, respondents were required to provide informed consent by clicking on a button at the end of the first page after having read all relevant information. To successfully submit the completed questionnaire, completing all responses was mandatory. No incentives were offered to the participants for completing the questionnaire.
Questionnaire Design
A self-administered questionnaire was developed by the authors using QuestionPro® software. A literature review was performed to identify existing relevant surveys, and accordingly, we adopted these previous studies to assist in developing our questionnaire.2,19,25–27 Academicians in medical education, academicians in research, and academicians in biostatistics reviewed the questionnaire for content validity and reliability. Further, their comments and suggestions were discussed among the authors and considered in the development of the final version of the questionnaire. The questionnaire was available in English only. It was distributed to all eligible students (2nd, 3rd, 4th, 5th, and 6th year) using online platforms.
The questionnaire consists of 7 sections covering different aspects: introduction and informed consent, background and demographic characteristics, platforms evaluation, students’ experience, role of online learning in clinical teaching, examination, and impacts. The introductory section described the objective of the study and required the consent of the respondent before proceeding and it is followed by the section on the basic demographic characteristics of the respondents such as gender and medical school year. The questionnaire stated the learning strategies used prior to the Covid-19 pandemic: whether online learning platforms such as pre-recorded lectures/tutorials, learning materials uploaded on blackboard, and live lectures/tutorials via Zoom were used or not, and how many hours per week were spent on online learning.
Similarly, the questionnaire reflected the average number of hours spent on online learning during the Covid-19 pandemic. In addition, the respondents evaluated the online platforms adopted by the College of Medicine at IAU during the Covid-19 pandemic. Effectiveness of each platform was assessed by using Likert scale (1–5) for ranking (least effective-most effective). For interaction-level assessment, a scale from 1 to 3 was used for ranking (not interactive–interactive).
Moreover, respondents were asked to evaluate their entire online learning experience during the Covid-19 pandemic by scoring 9 statements using 5-points Likert scale from 1 for strongly disagree to 5 for strongly agree. Also, they compared between online learning and actual classroom learning in terms of the scientific materials’ understanding in 3 areas: PBL, theoretical lectures, and clinical lectures. In addition, respondents were asked about the enjoyable aspects of and barriers to online learning and teaching they experienced during the Covid-19 pandemic.
The last section of the questionnaire covered the impact of online learning during the Covid-19 pandemic on the student’s health and social life. A range of elements were explored including health, level of anxiety, level of stress, physical activities, and personal connection.
Data Analysis
After 2 months of data collection, data gathered from the survey were exported to IBM SPSS Statistics 26.0 (IBM Corp. in Armonk, NY) and Microsoft Excel (Excel 2016). For quantifiable variables, a descriptive analysis using mean and Standard Deviation (SD), frequency and percentages was performed. To associate between different variables Chi-Square tests were used. p-value <0.05 was considered statistically significant.
Ethical Approval
Study approval was granted by the Institutional Review Board (IRB) (IRB-2021-01-360) of the Imam Abdulrahman Bin Faisal University. Information to identify the participants was not obtained.
Results
The demographical characteristics are summarized in Table 1. In this study, we included a target population from year 2 to year 6 medical undergraduates of both genders. At IAU, medical studies are divided into 2 phases: pre-clinical (2nd–3rd year) and clinical (4th–6th year). Table 1 shows that there were more females (64%) than males (36%) among 563 respondents and students’ participations in our survey from 2nd–6th year were distributed as follows: 28%, 30%, 12%, 17%, and 13%, respectively.
Table 1.
Demography and Characteristics of Participants
| Characteristics | Number of Students (n) | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 202 | 36% |
| Female | 361 | 64% |
| Total | 563 | 100% |
| Educational level (2nd–6th year students, 1st preparatory year students are excluded) | ||
| 2nd year | 160 | 28% |
| Male | 58 | 10% |
| Female | 102 | 18% |
| 3rd year | 171 | 30% |
| Male | 59 | 10% |
| Female | 112 | 20% |
| 4th year | 67 | 12% |
| Male | 25 | 4.5% |
| Female | 42 | 7.5% |
| 5th year | 93 | 17% |
| Male | 31 | 6% |
| Female | 62 | 11% |
| 6th year | 72 | 13% |
| Male | 29 | 5% |
| Female | 43 | 8% |
| Total (2nd–6th year) | 563 | 100% |
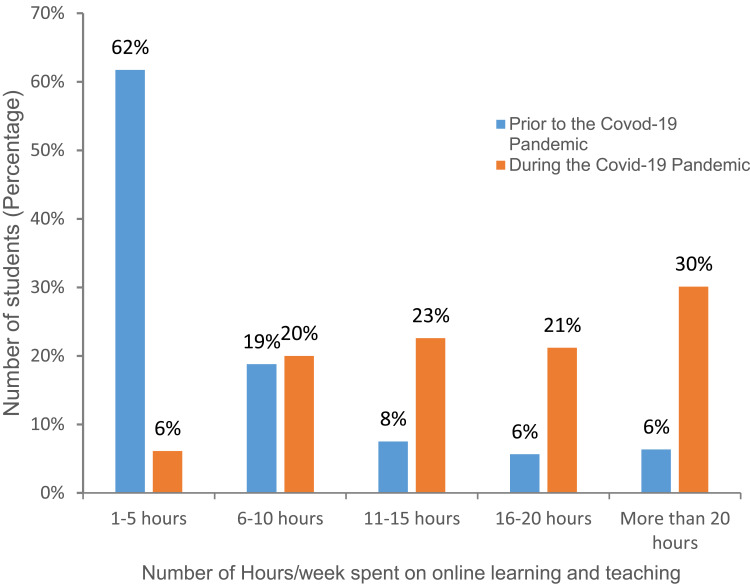
Our study found that there was a significant increase in the total number of hours’ students devoted to receiving instruction and learning online during the pandemic (Figure 1). Prior to the pandemic, 62% of the students (compared to 6% only during the pandemic) reported the use of online platforms for a maximum of up to just 5 hours per week. In addition, 19% of the students spent between 6 and up to 10 hours a week learning online, with 8%, 6% and 6% spending 11–15 hours, 16–20 hours and more than 20 hours, respectively. A significant difference was found between the time spent on online platforms before and during COVID-19, with 6% of students spending more than 20 hours learning online before the pandemic began, versus 30% of students spending >20 hours per week during the pandemic (P<0.001).
Figure 1.
Number of hours spent weekly on online learning and teaching prior and during the Covid-19 Pandemic. N = 425; P ‹ 0.01.
The study also showed that online platforms such as live lectures/tutorials via Zoom, pre-recorded lectures/tutorials and learning materials uploaded on blackboard were exclusively implemented for the delivery of lectures, practicals, clinical bedside teaching, for assignments submissions and course instructions. Results showed effectiveness of online teaching and learning methods. The majority of students considered online teaching and learning platforms are neutral, effective or most effective (Mean values vary between 3.2±1.25, 3.7±1.15 and 3.8±1.25). Students found live lectures/tutorials via zoom (61%) and pre-recorded lectures/tutorials (65%) are effective compared to 41% for learning materials uploaded on blackboard (P‹0.05) (Table 2).
Table 2.
Assessment of Platforms’ Effectiveness
| Effectiveness | N | 1 N (%) | 2 N (%) | 3 N (%) | 4 N (%) | 5 N (%) | Mean | SD |
|---|---|---|---|---|---|---|---|---|
| Live lectures/ tutorials via Zoom | 424 | 20 (5%) | 53 (13%) | 95 (22%) | 135 (32%) | 121 (29%) | 3.7 | 1.152 |
| Learning materials uploaded on Blackboard | 367 | 52 (14%) | 45 (12%) | 118 (32%) | 92 (25%) | 60 (16%) | 3.2 | 1.253 |
| Pre-recorded lectures/ tutorials | 375 | 25 (7%) | 42 (11%) | 64 (17%) | 96 (26%) | 148 (39%) | 3.8 | 1.256 |
Notes: Likert scale from 1–5 was used for ranking, where 1=Least effective and 5=most effective. Data are presented as numbers (N), percentages (%), and means and standard deviations (SD).
The majority of our students showed the highest rate of interaction for live lectures/tutorials via Zoom when compared with pre-recorded lectures or learning materials uploaded on blackboard. The mean of interaction level was 2.36±0.64 (interactive) for live lectures/tutorials via zoom compared to the mean of interaction level for the other platforms used where the mean varies between 1.48±0.72 and 1.66±0.79 (between no interaction and limited interaction). Only 9% of participants found live lectures/tutorials via zoom not interactive compared to learning materials uploaded on blackboard (54%) and pre-recorded lectures/tutorials (66%) (P‹0.05) (Table 3).
Table 3.
Assessment of Platforms’ Interaction Level
| Interaction | N | Not Interactive (1) N (%) | Interactive to Some Extent (2) N (%) | Interactive (3) N (%) | Mean | SD |
|---|---|---|---|---|---|---|
| Live lectures/ tutorials via Zoom | 418 | 37 (9%) | 194 (46%) | 187 (45%) | 2.36 | 0.639 |
| Learning materials uploaded on Blackboard | 305 | 165 (54%) | 80 (26%) | 60 (20%) | 1.66 | 0.788 |
| Pre-recorded lectures/ tutorials | 352 | 232 (66%) | 72 (20%) | 48 (14%) | 1.48 | 0.724 |
Notes: Scale from 1–3 was used for ranking, where 1 for not interactive and 3 for interactive. Data are presented as numbers (N), percentages (%), and means and standard deviations (SD).
Respondents’ perceptions towards online learning and teaching experiences were assessed for each of the nine statements rated on a scale of 5 points with 1 being strongly disagree and 5 being strongly agree (Table 4). 50% of the students disagree with the statement that online teaching is as effective as face-to-face teaching or enjoyable. On the other hand, 50% of the students would like the online teaching to be more interactive and found opportunities to ask questions are limited. Based on the mean value (2.77–3.50), neutral was the result of all the statements (Table 4).
Table 4.
Respondents’ Perceptions Towards Online Learning and Teaching Experiences
| Statements | Mean | ±SD |
|---|---|---|
| The teaching is often motivating | 2.96 | 1.189 |
| I find it easy to engage in the lesson | 2.98 | 1.334 |
| I feel able to ask questions | 3.28 | 1.259 |
| I enjoy the online teaching | 3.29 | 1.408 |
| I would like the online teaching to be more interactive | 3.50 | 1.098 |
| I feel that online teaching is as effective as face-to-face teaching | 2.77 | 1.481 |
| I prefer online teaching to face-to-face teaching | 3.07 | 1.526 |
| The teachers are well prepared for the online teaching sessions | 3.33 | 1.148 |
| I feel I am being well prepared for my profession | 3.17 | 1.246 |
Notes: Likert scale from 1–5 was used for ranking, where 1 = strongly disagree and 5 = strongly agree. Data are presented as means and standard deviations (SD). N = 394.
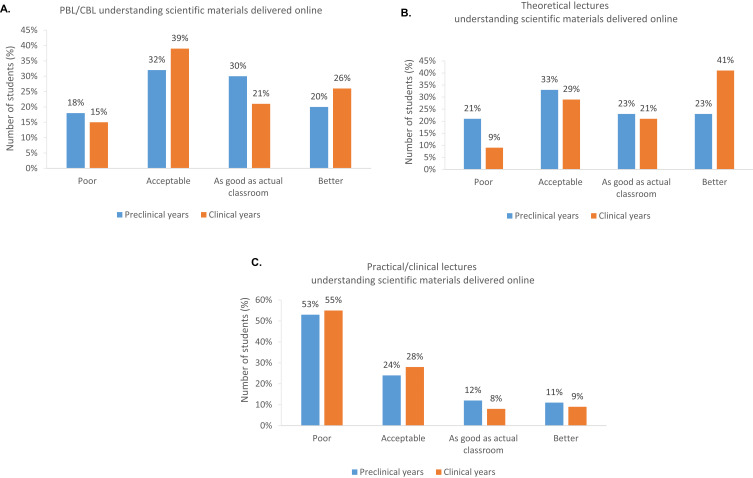
The College of Medicine revised MBBS curriculum has replaced the more traditional didactic lecture based curriculum with a more integrated model that introduces the concept of early clinical exposure. The reformed curriculum centers around the use of modern approaches in teaching and learning such as Problem-Based Learning (PBL) in second and third years and Case Based Learning (CBL) and Evidence Based Medicine (EBM) in fourth, fifth and sixth years emphasizing the use of self-directed learning to enhance the student’s engagement and foster achievement of the intended learning outcomes.5 About 50% of students perceived that understanding the scientific materials delivered through the online PBL sessions is as good as actual classroom PBL (25%) or even better (23%) while only 17% reflected is poor (Figure 2A). The majority of students revealed that understanding of scientific materials level for theoretical lectures delivered online are as good as actual classroom lectures or better (more than 50%) compared to 30% for acceptable and 16% for poor statements (Figure 2B). In addition, More than 50% of students agreed that the level of understanding the scientific materials was poor when practical/clinical lectures were delivered online compared to actual classroom. Only about 10% of the students found online clinical lectures better than actual classroom clinical lectures and 10% found both similar (Figure 2C). Only difference between results from students in preclinical years and students in clinical years for theoretical lectures delivered online was statistically significant (P‹0.001). Similarly to the results about understanding materials of clinical lectures delivered online, the majority of our students found poor the ability to learn clinical skills online (data not shown).
Figure 2.
(A–C) Understanding scientific materials delivered online vs actual classroom. Comparison 2nd–3rd (preclinical years) vs 4th–6th (clinical years) students. (A) PBL/CBL. (P=0.113) (B) Theoretical lectures. (P ‹ 0.001) (C) Practical/clinical lectures. (P = 0.449).
The main enjoyable aspects of online learning appeared to be the online accessibility of materials (73.2%) and the flexibility in time (69.7%) (Table 5). The highest frequencies of responses were 278, 265, or 248 for online accessibility of materials, flexibility in time, or more comfortable, while the lowest were 110, 86 or 21 for ability to ask questions, interactive, or others. Barriers to online learning were stated also (Table 5) and the frequencies of responses vary between 234 (61.6%) and 47 (12.4%) where internet connection is the most frequent and lack of devices is the least. Lack of effective communication compared to face-to-face interaction 185 (48.7%), family distractions 184 (48.4%), lack of self-discipline 158 (41.6%), lack of time management 132 (34.7%), anxiety 106 (27.9%), and stress 104 (27.4%) were considered barriers to online learning. In addition to timing of the lectures/tutorials 95 (25%), lack of virtual student support services 79 (20.8%), lack of space 73 (19.2%), and lack of technical support 70 (18.4%), students stated lack of contact with others and weakness at the team work level as further barriers to online learning.
Table 5.
Enjoyable Aspects of and Barriers to Online Learning and Teaching
| Enjoyable Aspects of Online Learning and Teaching | Frequency of Responses (%) |
|---|---|
| 1) Online accessibility of materials | 278 (73.2%) |
| 2) Flexibility in time | 265 (69.7%) |
| 3) More comfortable | 248 (65.3%) |
| 4) No travel | 236 (62.1%) |
| 5) Ability to learn at own pace | 215 (56.6%) |
| 6) Cost saving | 212 (55.8%) |
| 7) Ability to ask questions | 110 (28.9%) |
| 8) Interactive | 86 (22.6%) |
| 9) Others | 21 (5.5%) |
| Barriers to Online Learning and Teaching | Frequency of Responses (%) |
| 1) Internet connection | 234 (61.6%) |
| 2) Lack of effective communication compared to face-to-face interaction | 185 (48.7%) |
| 3) Family distractions | 184 (48.4%) |
| 4) Lack of self-discipline | 158 (41.6%) |
| 5) Lack of time management | 132 (34.7%) |
| 6) Anxiety | 106 (27.9%) |
| 7) Stress | 104 (27.4%) |
| 8) Timing of the lectures/tutorials | 95 (25%) |
| 9) Lack of virtual student support services | 79 (20.8%) |
| 10) Lack of space | 73 (19.2%) |
| 11) Lack of technical support | 70 (18.4%) |
| 12) Lack of devices | 47 (12.4%) |
| 13) Others | 23 (6.1%) |
Note: Number of students N = 380.
Students’ perceptions on the impacts of online teaching and learning on their health and social life are illustrated in Table 6. We compared the results as perceived by students from pre-clinical years vs clinical years. The majority of the students from preclinical (84%) and clinical (75%) years agreed on lack of physical activities due to online teaching and learning (P=0.027). Likewise, the majority of preclinical students found that online learning has a big impact on health (71%), social isolation (67%), and personal connection (59%) aspects. The clinical students’ perceptions of online teaching and learning impact on these aspects were equally divided between yes and no (around 50%). Similarly, more than 50% of preclinical students found online learning stressful compared to clinical students (36%). The anxiety level was also higher for preclinical students (52%) versus 35% for clinical students. The results revealed that during the pandemic when the online teaching and learning was implemented, the impact was higher on students from pre-clinical years than on students from clinical years with statistical significance (P‹0.05) (Table 6).
Table 6.
Impacts of Online Learning and Teaching on Students’ Health and Social Life Comparison 2nd–3rd vs 4th–6th Students
| Impacts of Online Learning and Teaching on Students | P value | |
|---|---|---|
| Headache/ vision problems or other medical conditions | ||
| 2nd–3rd (Pre-clinical) | 146 (71%) | P‹0.001 |
| 4th–6th (Clinical) | 78 (53%) | |
| Anxiety | ||
| 2nd–3rd (Pre-clinical) | 121 (52%) | P=0.001 |
| 4th–6th (Clinical) | 51 (35%) | |
| Stress | ||
| 2nd–3rd (Pre-clinical) | 132 (57%) | P‹0.001 |
| 4th–6th (Clinical) | 52 (36%) | |
| Social isolation | ||
| 2nd–3rd (Pre-clinical) | 155 (67%) | P‹0.001 |
| 4th–6th (Clinical) | 70 (48%) | |
| Lack of physical activities | ||
| 2nd–3rd (Pre-clinical) | 195 (84%) | P=0.027 |
| 4th–6th (Clinical) | 110 (75%) | |
| Personal connection | ||
| 2nd–3rd (Pre-clinical) | 138 (59%) | P=0.028 |
| 4th–6th (Clinical) | 71 (48%) |
Discussion
During the early phase of the Covid-19 pandemic, the College of Medicine IAU adopted various new and pre-existing online platforms and switched totally, then partially to online learning and teaching to preserve the continuity of medical studies. A significant increase in the total number of hours’ students devoted to receiving instruction and learning online during the pandemic compared to prior to the pandemic (P‹0.01) (Figure 1). These findings compare favorably to other studies published by other groups.2 The increase of number of hours spent weekly on online learning is expected, since online learning became the primary method used by students to continue their studies, when in person class attendance had been suspended.
The effectiveness of e-learning can be increased by making the e-learning system easy for application.28 In addition, the main enablers of online learning were motivation, interaction and user-friendly technologies.29 Our study revealed high effectiveness level of online teaching and learning methods. Comparable to our study, different studies showed that an online teaching and learning method was better or as effective as offline methods with a high level of acceptance of e-learning.11,30,31 On the other hand, and in contrast to our study, results from other studies reported unsatisfactory or very unsatisfactory the experience of the E-learning.25,32 These results might be explained by the fact that online platforms in the form of video lectures using YouTube® and blackboard were previously applied for years at IAU.5
A recently published study from Jeddah KSA, done at King Abdulaziz University reported that medical students moderately accepted online learning during the pandemic lockdowns and about half of the respondents in the study rated online learning as better or similar to face-to-face learning.30 For our students at IAU, the percentage was somewhat less, with 42% either strongly agreeing or agreeing that online learning was better or similar to face-to-face learning with 22% remaining neutral.
Similarly to other studies,2,19,32 only 34% agreed that online teaching and learning are equally effective when compared to face to face. However, our students prefer to engage in face-to-face learning instead of solo online learning. This is aligned with the results from the study conducted at Alfaisal University in KSA, concluding that the level of satisfaction in fully online learning during the Covid-19 pandemic remained low especially among high achieving students.33
Despite the highest rate of interaction for live lectures/tutorials via Zoom when compared with video lectures or learning materials uploaded on blackboard, very few students showed interaction as the advantage of online teaching.19,34,35 Psychological closeness for the students with the instructors due to instructors’ nonverbal clues seen in campus teaching is an advantageous factor of face-to-face teaching and learning.36,37 Similarly, negative attitudes of the students towards online learning in regards to critical thinking, brainstorming, teamwork and collaborations with students and learning recognition in terms of social nearness, social interaction, access to support services, and fulfillment are favoring face-to-face teaching and learning.38–40 To provide opportunities for peers’ interaction and to augment medical students’ education, study sessions and virtual group clinical opportunities are recommended.40
Previous studies have reported that online teaching and learning can cover practical lessons, allow interactive constructive discussions and can be effective in terms of achieving learning outcomes.2,26,41 Generally, the modern online study during the COVID-19 pandemic has demonstrated a largely positive impact on online medical teaching and learning with significant and promising potential for the future of medical education.2,36,42 In the current study, only 17% of the students reflected the understanding of scientific materials through online PBL is poor while the majority found it as good as or better than in actual classroom (Figure 2A). These results might not be aligned with some other studies where the students reflected that online teaching and learning are not suitable for medical studies in general.26 Further studies might be needed to compare the students’ actual performance in online PBL and CBL versus classroom sessions. Aligned with other studies, our results showed that clinical skills which are best learned in clinics and laboratories remain a pertinent barrier to online teaching.2,18,25,40,43–45
Similarly to other studies, the most enjoyable aspects of online learning appeared to be the online accessibility of materials, flexibility of the time, ability to learn at own pace and cost saving.2,42 Post pandemic recommendations suggested to maintain flexibility and accessibility to educational resources.45 20% of respondents found interaction and ability to ask questions are enjoyable aspects of online learning. As suggested in previous studies, students who have difficulties to interact and to engage in a live lecture are encouraged to participate and interact more in online class.2,46 However, this advantage is applicable only when interaction is permitted as in live lectures online.47
On the other hand, online learning is dependent on the accessibility, functionality of electronic devices, and on excellent incessant internet connection.32,43 In line with these findings, internet connection (43%) is the main barrier revealed in the current study. Lack of devices and lack of technical support appeared to be less effective as barriers to online teaching and learning as reported also in another study.42 Further barriers to online learning that contribute to low effectiveness were identified as lack of effective communication compared to face-to-face interaction, family distractions, lack of self-discipline, and lack of time management.2
Results illustrating the students’ perceptions on the impacts of online teaching and learning on their health and social life showed that it has a high impact on physical activities. These findings are supported by a national study conducted across the Kingdom of Saudi Arabia, which reported the negative impact on physical activity in more than 50% of respondents resulting from the imposed strict hygiene and national lockdown measures.48 A significant reduction in the amount of time spent in physical activity levels was also reported during the Covid-19 lockdown compared to before the lockdown period.49
Recent studies have signified the impact of online teaching and learning in some medical conditions such as headache, eye strain, computer vision syndrome (CVS), neck pain and sleep disturbances reporting a highly significant correlation with online class duration of more than 4 hours, each class is more than 40 minutes and associated pre-existing medical issues.50,51
Moreover, pandemic-related stress or anxiety were also considered as a challenge reported by a considerable number of students (48%).40,42,52 Anxiety might be related to the lack of social interaction with friends and colleagues and to the lack of physical activities due to online teaching and learning as found in our study; however, exam anxiety might be decreased due to the nature of unrestricted online exams.2 Students reporting an impact on their personal connections and experiencing social isolation can have a negative impact on their learning experiences.53 In addition, the results are comparable to other studies showing that health-related issues, anxiety symptoms, stress and depressive symptoms are higher among pre-clinical students as compared to clinical years’ students.41,52 Comparison studies to elaborate the difference between preclinical and clinical students’ perceptions and to compare between genders will support our findings.
Limitations
In this study, we noticed that medical students’ knowledge, attitudes, and practice regarding online learning vary. Therefore, the results may not be generalized to other universities in Saudi Arabia, and further studies in other universities to obtain an overview of the online learning platforms use must be done. In addition, attention should be directed to survey responses for possible students recall bias. Another limitation is the self-administered nature of the study design. In addition to the low responses rate, it limited our ability to quantify effectiveness of online platforms. All our results are based exclusively on the students’ perceptions. To build on the results of our study, future research should focus on a quantitative study reflecting the impact of online teaching and learning on students’ performance.
Conclusion
In conclusion, online teaching and learning during Covid-19 pandemic affects students’ physical, social and mental wellbeing besides their intellectual ability to learn. Students showed predominantly positive perspective on online learning and teaching. However, improvement needs to be applied, especially at the clinical skills development level, to enhance the effectiveness of the online approach. A blended format of online learning and traditional methods will be beneficial as suggested in other studies.6,33,45,54 Moreover, a continuous training for our faculty to enhance their online teaching skills will improve online teaching and learning implementation. Comparing the students’ actual performance in online PBL and CBL versus classroom sessions will provide robust evidence on the benefit of online team-based learning.55
Despite the barriers of online learning and teaching, the experience students have had during the pandemic has increased their perspectives toward the effectiveness of online platforms. This will support the use of online approaches in medical education in the future.
Acknowledgments
The authors would like to acknowledge all the medical students who participated in this survey and to thank Dr Moataza M Abdel Wahab, Family and community medicine, College of Medicine, IAU for her guidance in statistical analysis.
Data Sharing Statement
Data of this study are available upon request from the corresponding author.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Kaur N, Dwivedi D, Arora J, Gandhi A. Study of the effectiveness of e-learning to conventional teaching in medical undergraduates amid COVID-19 pandemic. Natl J Physiol Pharm Pharmacol. 2020;10(7):563–567. [Google Scholar]
- 2.Dost S, Hossain A, Shehab M, Abdelwahed A, Al-Nusair L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ open. 2020;10(11):e042378. doi: 10.1136/bmjopen-2020-042378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.AlQhtani A, AlSwedan N, Almulhim A, et al. Online versus classroom teaching for medical students during COVID-19: measuring effectiveness and satisfaction. BMC Med Educ. 2021;21(1):1–7. doi: 10.1186/s12909-021-02888-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adedoyin OB, Soykan E. Covid-19 pandemic and online learning: the challenges and opportunities. Interact Learn Environ. 2020;3:1–3. [Google Scholar]
- 5.MBBS Revised Study Plan, 2014–2015. College of Medicine, Imam Abdulrahman Bin Faisal University. Unpublished; 2015.
- 6.Gormley GJ, Collins K, Boohan M, Bickle IC, Stevenson M. Is there a place for e-learning in clinical skills? A survey of undergraduate medical students’ experiences and attitudes. Med Teach. 2009;31(1):e6–e12. doi: 10.1080/01421590802334317 [DOI] [PubMed] [Google Scholar]
- 7.Sandhu P, de Wolf M. The impact of COVID-19 on the undergraduate medical curriculum. Med Educ Online. 2020;25(1):1764740. doi: 10.1080/10872981.2020.1764740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kay D, Pasarica M. Using technology to increase student (and faculty satisfaction with) engagement in medical education. Adv Physiol Educ. 2019;43(3):408–413. doi: 10.1152/advan.00033.2019 [DOI] [PubMed] [Google Scholar]
- 9.Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323(21):2131–2132. doi: 10.1001/jama.2020.5227 [DOI] [PubMed] [Google Scholar]
- 10.Evans DJ, Bay BH, Wilson TD, Smith CF, Lachman N, Pawlina W. Going virtual to support anatomy education: a STOPGAP in the midst of the Covid‐19 pandemic. Anat Sci Educ. 2020;13(3):279–283. doi: 10.1002/ase.1963 [DOI] [PubMed] [Google Scholar]
- 11.Pei L, Wu H. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Med Educ Online. 2019;24(1):1666538. doi: 10.1080/10872981.2019.1666538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barry DS, Marzouk F, Chulak-Oglu K, et al. Anatomy education for the YouTube generation. Anat Sci Educ. 2016;9:90–96. doi: 10.1002/ase.1550 [DOI] [PubMed] [Google Scholar]
- 13.Longhurst GJ, Stone DM, Dulohery K, et al. Strength, weakness, opportunity, threat (SWOT) analysis of the adaptations to anatomical education in the United Kingdom and Republic of Ireland in response to the Covid-19 pandemic. Anat Sci Educ. 2020;13:301–311. doi: 10.1002/ase.1967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Emanuel EJ. The inevitable reimagining of medical education. JAMA. 2020;323(12):1127–1128. doi: 10.1001/jama.2020.1227 [DOI] [PubMed] [Google Scholar]
- 15.Hilburg R, Patel N, Ambruso S, Biewald MA, Farouk SS. Medical education during the coronavirus disease-2019 pandemic: learning from a distance. Adv Chronic Kidney Dis. 2020;27(5):412–417. doi: 10.1053/j.ackd.2020.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller DG, Pierson L, Doernberg S. The role of medical students during the COVID-19 pandemic. Ann Intern Med. 2020;173(2):145–146. doi: 10.7326/M20-1281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huddart D, Hirniak J, Sethi R, et al. #MedStudentCovid: how social media is supporting students during COVID‐19. Med Edu. 2020;54(10):951. doi: 10.1111/medu.14215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guan Hui Tricia Lim, Ritika Devendra Gera, Fady Hany Kamel, Vikram Ajit Rajan Thirupathirajan, Somar Albani, Rima Chakrabarti. “We Need More Practice”: evaluating the role of virtual mock OSCEs in the undergraduate programme during the COVID pandemic. Adv Med Educ Pract. 2023;28(14):157–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bączek M, Zagańczyk-Bączek M, Szpringer M, Jaroszyński A, Wożakowska-Kapłon B. Students’ perception of online learning during the COVID-19 pandemic: a survey study of Polish medical students. Medicine. 2021;100(7):e24821. doi: 10.1097/MD.0000000000024821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salem AH. Randomized controlled trial of simulation-based teaching versus traditional clinical instructions in nursing: a pilot study among critical care nursing students. Int J Nurs Educ. 2015;7(1):277. [Google Scholar]
- 21.Chumley-Jones HS, Dobbie A, Alford CL. Web-based learning: sound educational method or hype? A review of the evaluation literature. Acad Med. 2002;77:86–93. doi: 10.1097/00001888-200210001-00028 [DOI] [PubMed] [Google Scholar]
- 22.Verma A, Verma S, Garg P, Godara R. Online teaching during COVID-19: perception of medical undergraduate students. Indian J Surg. 2020;82(3):299–300. doi: 10.1007/s12262-020-02487-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cook DA. Web-based learning: pros, cons and controversies. Clin Med. 2007;7(1):37. doi: 10.7861/clinmedicine.7-1-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Workforce Group. Modernizing healthcare training: E‐learning in health‐care services. e-mpirical Ltd; 2006. [Google Scholar]
- 25.Al-Balas M, Al-Balas HI, Jaber HM, et al. Distance learning in clinical medical education amid COVID-19 pandemic in Jordan: current situation, challenges, and perspectives. BMC Med Educ. 2020;20(1):341. doi: 10.1186/s12909-020-02257-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Al Zahrani EM, Al Naam YA, AlRabeeah SM, et al. E-Learning experience of the medical profession’s college students during COVID-19 pandemic in Saudi Arabia. BMC Med Educ. 2021;21(1):1. doi: 10.1186/s12909-021-02860-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shawaqfeh MS, Al Bekairy AM, Al-Azayzih A, et al. Pharmacy students perceptions of their distance online learning experience during the Covid-19 pandemic: a cross-sectional survey study. J Med Educ Curric Dev. 2020;7:1–9. doi: 10.1177/2382120520963039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen WS, Yao AYT. An empirical evaluation of critical factors influencing learner satisfaction in blended learning: a pilot study. Univers J Educ Res. 2016;4(7):1667–1671. doi: 10.13189/ujer.2016.040719 [DOI] [Google Scholar]
- 29.Regmi K, Jones L. A systematic review of the factors – enablers and barriers – affecting e-learning in health sciences education. BMC Med Educ. 2020;20(1):1–18. doi: 10.1186/s12909-020-02007-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ibrahim NK, Al Raddadi R, AlDarmasi M, et al. Medical students’ acceptance and perceptions of e-learning during the Covid-19 closure time in King Abdulaziz University, Jeddah. J Infect Public Health. 2021;14(1):17–23. doi: 10.1016/j.jiph.2020.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Costa A, Costa A, Olsson IAS. Students’ acceptance of e-learning approaches in laboratory animal science training. Lab Anim. 2019;0023677219879170. [DOI] [PubMed] [Google Scholar]
- 32.Barakat M, Abu Farha R, Muflih S, et al. The era of E-learning from the perspectives of Jordanian medical students: a cross-sectional study. Heliyon. 2022;8(7):e09928. doi: 10.1016/j.heliyon.2022.e09928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arain SA, Ali M, Arbili L, et al. Medical students and faculty perceptions about online learning during Covid-19 pandemic: alfaisal university experience. Front Public Health. 2022;10(1–8):880835. doi: 10.3389/fpubh.2022.880835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cook D, Steinert Y. Online learning for faculty development: a review of the literature. Med Teach. 2013;35:930–937. doi: 10.3109/0142159X.2013.827328 [DOI] [PubMed] [Google Scholar]
- 35.Shaiba LA, Alnamnakani MA, Temsah MH, et al. Medical faculty’s and students’ perceptions toward pediatric electronic OSCE during the COVID-19 pandemic in Saudi Arabia. Healthcare. 2021;9(8):950. doi: 10.3390/healthcare9080950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khalil R, Mansour AE, Fadda WA, et al. The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia: a qualitative study exploring medical students’ perspectives. BMC Med Educ. 2020;20(1):285. PMID: 32859188; PMCID: PMC7453686. doi: 10.1186/s12909-020-02208-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Manusov V. A history of research on nonverbal communication: our divergent pasts and their contemporary legacies. In: Matsumoto D, Hwang HC, Frank MG, editors. APA Handbook of Nonverbal Communication. Washington, DC: American Psychological Association; 2016:3–15. [Google Scholar]
- 38.Hanafy SM, Jumaa MI, Arafa MA. A comparative study of online learning in response to the coronavirus disease 2019 pandemic versus conventional learning. Saudi Med J. 2021;42(3):324–331. doi: 10.15537/smj.2021.42.3.20200741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bali S, Liu MC. Students’ perceptions toward online learning and face-to-face learning courses2018. Conf Series. 2018;1108:012094. doi: 10.1088/1742-6596/1108/1/012094 [DOI] [Google Scholar]
- 40.Walters M, Alonge T, Zeller M. Impact of Covid-19 on medical education: perspectives from students. Acad Med. 2022;97(3):S40–S48. doi: 10.1097/ACM.0000000000004525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Alsoufi A, Alsuyihili A, Msherghi A, et al. Impact of the COVID-19 pandemic on medical education: medical students’ knowledge, attitudes, and practices regarding electronic learning. PLoS One. 2020;15(11):e0242905. doi: 10.1371/journal.pone.0242905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rajab MH, Gazal AM, Alkattan K. Challenges to online medical education during the COVID-19 pandemic. Cureus. 2020;12(7). doi: 10.7759/cureus.8966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abbasi MS, Ahmed N, Sajjad B, et al. E-Learning perception and satisfaction among health sciences students amid the COVID-19 pandemic. Work. 2020;67(3):549–556. doi: 10.3233/WOR-203308 [DOI] [PubMed] [Google Scholar]
- 44.Schlenz MA, Schmidt A, Wöstmann B, Krämer N, Schulz-Weidner N. Students’ and lecturers’ perspective on the implementation of online learning in dental education due to SARS-CoV-2 (COVID-19): a cross-sectional study. BMC Med Educ. 2020;20(1):1–7. doi: 10.1186/s12909-020-02266-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Samannodi M, Bulkhi A, Alwafi H, et al. Impact of Covid-19 pandemic on medical education: a cross-sectional study in the western region of Saudi Arabia. AMEP. 2022;13:741–754. doi: 10.2147/AMEP.S369213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ni AY, Ya NA. Comparing the effectiveness of classroom and online learning: teaching research methods. J Public Aff Educ. 2013;19:199–215. doi: 10.1080/15236803.2013.12001730 [DOI] [Google Scholar]
- 47.Keis O, Grab C, Schneider A, et al. Online or face to face instruction? A qualitative study on the electrocardiogram course at the University of Ulm to examine why students choose a particular format. BMC Med Educ. 2017;17:194. doi: 10.1186/s12909-017-1053-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bakhsh MA, Khawandanah J, Naaman RK, Alashmali S. The impact of COVID-19 quarantine on dietary habits and physical activity in Saudi Arabia: a cross-sectional study. BMC Public Health. 2021;21(1):1. doi: 10.1186/s12889-021-11540-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barwais FA. Physical activity at home during the COVID-19 pandemic in the two Most-affected cities in Saudi Arabia. Open Public Health J. 2020;13:1. doi: 10.2174/1874944502013010470 [DOI] [Google Scholar]
- 50.Singh HK, Joshi A, Malepati RN, et al. A survey of E-learning methods in nursing and medical education during COVID-19 pandemic in India. Nurse Educ Today. 2021;99:104796. doi: 10.1016/j.nedt.2021.104796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Altalhi A, Khayyat W, Khojah O, Alsalmi M, Almarzouki H. Computer vision syndrome among health sciences students in Saudi Arabia: prevalence and risk factors. Cureus. 2020;12(2):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Abdulghani HM, Sattar K, Ahmad T, Akram A. Association of COVID-19 pandemic with undergraduate medical students’ perceived stress and coping. Psychol Res Behav Manag. 2020;13:871. doi: 10.2147/PRBM.S276938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kaufmann R, Vallade JI. Exploring connections in the online learning environment: student perceptions of rapport, climate, and loneliness. Interact Learn Environ. 2020;9:1–5. [Google Scholar]
- 54.Maertens H, Madani A, Landry T, Vermassen F, Van Herzeele I, Aggarwal R. Systematic review of e-learning for surgical training. B J Surg. 2016;11:1428–1437. doi: 10.1002/bjs.10236 [DOI] [PubMed] [Google Scholar]
- 55.Foo CC, Cheung B, Chu KM. A comparative study regarding distance learning and the conventional face-to-face approach conducted problem-based learning tutorial during the COVID-19 pandemic. BMC Med Educ. 2021;21(1):1–6. doi: 10.1186/s12909-021-02575-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data of this study are available upon request from the corresponding author.