Abstract
In ovarian cancer patients, the 5-year survival rate is 90% for stages I and II, but only 30% for stages III and IV. Unfortunately, as 75% of the patients are diagnosed at stages III and IV, many experience a recurrence. To ameliorate this, it is necessary to develop new biomarkers for early diagnosis and treatment. The ubiquitin–proteasome system is a post-translational modification that plays an important role in regulating protein stability through ubiquitination. In particular, deubiquitinating enzymes (DUBs) regulate protein stability through deubiquitinating substrate proteins. In this review, DUBs and substrates regulated by these enzymes are summarized based on their functions in ovarian cancer cells. This would be useful for the discovery of biomarkers for ovarian cancer and developing new therapeutic candidates.
Keywords: deubiquitinating enzyme, epithelial ovarian cancer, ubiquitin–proteasome system
1. Introduction
1.1. Ovarian Cancer
Ovarian cancer is the 7th most frequent cancer in women globally [1]. As the rates of ovarian cancer diagnosis rate per 100,000 people per year and the death rate of patients are consistently decreasing, the 5-year related survival rate increased to 54.31% in 2020 from 34.38% in 1975 [1,2]. However, 233,565 newly diagnosed patients are in U.S [1]. The 5-year survival rate for stages I and II ovarian cancers, according to the International Federation of Gynecology and Obstetrics (FIGO) staging system, is between 80 and 90%, but that for stages III and IV is only 30% [1,3,4]. This is because stage I and II ovarian cancers localize near the ovaries or fallopian tubes, while stages III and IV cancers invade nearby organs, such as the lymph nodes, abdomen, omentum, liver, spleen, and lung [5,6]. Moreover, 75% of ovarian cancer patients are diagnosed in advanced stages (stage III and IV), due to a deficiency of screening for early prognosis and the absence of precise pelvic or abdominal symptoms [7,8].
1.1.1. Subtypes
Ovarian cancer is subdivided into epithelial and non-epithelial cancer. Epithelial ovarian cancer (EOC) accounts for over 90% of ovarian cancer and has four histological subtypes: serous, endometrioid, clear cell, and mucinous [1,9]. EOC has two categories: type I and type II. Type I EOC has mild symptoms, grows slowly, has a clear borderline, is diagnosed in the early stage, and includes low-grade serous, low-grade endometrioid, mucinous, and clear cell carcinomas. Type II EOC is highly lethal, invasive, grows rapidly, and contains high-grade serous and high-grade endometrioid carcinomas (Table 1) [9,10,11].
Table 1.
Subtypes of ovarian cancer and characteristics of each.
| Cancer | Type | Subtype | Grade | Characteristics | References |
|---|---|---|---|---|---|
| Ovarian cancer | Epithelial | Serous | High-grade | 90% of serous ovarian cancer | [10,12,13,14,15] |
| Generally diagnosed in older women | |||||
| Present at advanced stages | |||||
| Have poor prognosis (10-year survival rate of 30%) | |||||
| Originates in the ovary, fallopian tube, and others | |||||
| Have TP53 and BRCA mutation | |||||
| 50% of tumors have homologous recombination deficiencies | |||||
| Low-grade | Usually diagnosed in younger women | [10,12,14,16,17] | |||
| Grow slowly | |||||
| Have a better prognosis than high-grade serous carcinoma | |||||
| Originates in ovary | |||||
| Endometrioid | Low-grade | Chemosensitive | [10,18,19] | ||
| Generally diagnosed in the early stage | |||||
| Originates in endometriosis | |||||
| Has better prognosis | |||||
| Mucinous | Low-grade | Most uncommon cancer in epithelial ovarian cancer | [10,19,20,21] | ||
| Associated with metastasis from the gastrointestinal tract | |||||
| Most patients are diagnosed with stage I | |||||
| Clear cell | Low-grade | Relatively have a good prognosis | [1,10,19,22] | ||
| Generally diagnosed in the early stage | |||||
| Have resistance to platinum-based chemotherapy in advanced stage | |||||
| Non-epithelial | Germ cell | - | 3% of ovarian cancer | [1,10,23,24] | |
| Have obvious makers of tumor | |||||
| Diagnosed at a young age (10~30 years old) | |||||
| Histologically like men’s germ cell tumors in the testes | |||||
| Sex cord-stromal | - | Under 2% of ovarian cancer | [25,26] | ||
| Generally diagnosed in the early stage | |||||
| Smoking decreases the risk of the tumor | |||||
| Rarely have malignance |
1.1.2. Risk Factors
Ovarian cancer involves various risk factors, such as gene mutations, ovulation, dietary factors, and ethnical groups [1]. Some factors increase the risk, while others decrease it. For example, early menarche and late menopause are associated with an increased risk of ovarian cancer, because they cause an inflammatory reaction through the course of many ovulations [27,28]. Moreover, germline mutations in BRCA1 or BRCA2 increase the incidence of ovarian cancer. Older age and endometriosis are also risk factors for ovarian cancer [29]. Endometriosis is related to endometriosis-associated EOC [30]. In contrast, early menopause, late menarche, hysterectomy, high levels of vitamin D, and the use of oral contraceptives lead to a decreased incidence of ovarian cancer [1,8,31].
1.1.3. Diagnosis and Screening
Three methods are used for ovarian cancer screening: (i) monitoring biomarkers, (ii) scanning with radiological methods, and (iii) performing cancer tissue biopsy. Cancer antigen 125 (carbohydrate antigen, mucin-16, CA125) is one of the most frequently used biomarkers for ovarian cancer. However, CA125 is inadequate for the early diagnosis of ovarian cancer because of its low sensitivity [32]. To improve the sensitivity of screening ovarian cancers, new biomarkers such as human epididymis protein 4 (HE4), are identified [33]. Monitoring the expression of HE4 is a more sensitive screening method than monitoring CA125, but it is still inadequate [34]. For these reasons, screening algorithms, such as the risk of malignancy index (RMI) and risk of ovarian malignancy algorithms (ROMA), have been developed [34,35].
Among radiological scans, transvaginal sonography (TVS) is more sensitive to detecting ovarian cancer than computed axial tomography (CT) or other radiological methods [36,37]. Finally, ovarian cancer is definitively diagnosed by biopsy during surgery or core-needle biopsy [1]. However, the core–needle biopsy is not recommended because of the risk of metastasis [38].
1.1.4. Treatments
Standard treatments for ovarian cancer are chemotherapy and surgery. Currently, there are two types of chemotherapy (platinum-containing drugs and taxane) and two types of targeted treatments which are poly ADP-ribose polymerase (PARP) inhibitors (PARPi) and vascular endothelial growth factor (VEGF) inhibitors (VEGFi) for ovarian cancer, depending on their anti-tumor mechanism or material [1]. First, platinum-containing drugs (including cisplatin, carboplatin, oxaliplatin, picoplatin, and satraplatin) cause DNA damage and induce apoptotic cell death by binding to the N7 of guanine bases, resulting in intrastrand adduction and interstrand crosslinks [11,39]. Cisplatin was first used in 1971 and was the first platinum-based drug approved by the Food and Drug Administration (FDA) in 1978 [40]. However, patients resistant to platinum therapy have lower median survival rates. The median survival of platinum-sensitive patients is two years, but that of platinum-resistant ovarian cancer is 9–12 months [41]. Second, taxanes, including paclitaxel and docetaxel, target microtubules to inhibit cell division [42,43]. Unlike other microtubule-targeted drugs, taxanes stabilize microtubules and repress the microtubule dynamics [44]. In 1992, the FDA approved taxol for the treatment of ovarian cancer [45].
As targeted treatments, PARPi has been suggested as the mechanism of synthetic lethality that BRCA-deficient tumor cells become sensitive to PARPi [46]. In 2014, olaparib was approved by the FDA for the treatment of ovarian cancer. Talazoparib, niraparib, and rucaparib have also been approved by the FDA as PARPis [47,48]. Moreover, angiogenesis-targeted drugs inhibit angiogenesis by inhibiting VEGF, mainly using monoclonal VEFG antibodies, bevacizumab, and VEGF receptor tyrosine kinase inhibitor (VEGF RTKi) [9]. The FDA approved bevacizumab for the treatment of advanced-stage ovarian cancer in 2018 [49]. Additionally, VEGF RTKi, cediranib, and nintedanib have been studied for use in patients with ovarian cancer [50,51].
Ovarian cancer treatment depends on several conditions, such as stage, BRCA mutation, and platinum sensitivity of the patients [1,9]. A combination of appropriate drugs was selected for each patient, and intraperitoneal chemotherapy and neoadjuvant chemotherapy were also considered [52].
The surgery for the treatment of ovarian cancer patients varies according to the stage of ovarian cancer [5]. Total abdominal hysterectomy and salpingo-oophorectomy are the most commonly used methods; however, surgery such as infracolic omentectomy, selective lymphadenectomy, and cytoreductive surgery can be performed [5,53].
1.2. Ubiquitin, Ubiquitin–Proteasome System (UPS), and Deubiquitinating Enzymes (DUBs)
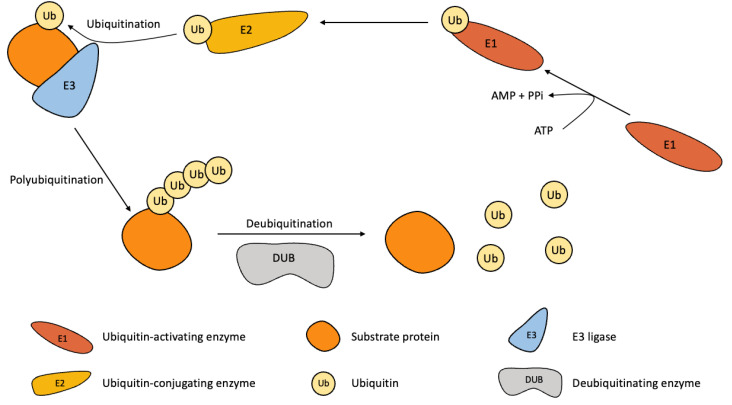
Ubiquitin, composed of 76 amino acids, binds with substrate and forms chains by forming covalent bonds in Lys and Met residues [54,55,56]. Attaching ubiquitin itself is a mechanism known as polyubiquitination. Polyubiquitination is associated with seven lysine residues (Lys6, Lys11, Lys 27, Lys29, Lys33, Lys48, and Lys63) and one methionine residue (Met1) [57,58]. Ubiquitination is mediated by three enzymes: E1 ubiquitin-activating enzyme, E2 ubiquitin-conjugating enzyme, and E3 ubiquitin ligase. Firstly, E1 binds to ubiquitin using ATP, and through the E2, E3 ligase attaches ubiquitin to its substrate protein (Figure 1) [57,59,60].
Figure 1.
A mechanism of the ubiquitination and deubiquitination. The substrate is ubiquitinated by the E1 ubiquitin-activating enzyme, E2 ubiquitin-conjugating enzyme, and E3 ligase. The polyubiquitin chain is formed by successive mechanisms. A substrate with polyubiquitin chains regulates various cellular functions. Conversely, the polyubiquitin chain of the substrate is cleaved by the DUB.
1.2.1. Ubiquitination
Ubiquitination or polyubiquitination is a post-translational modification (PTM). The subtypes of ubiquitin modifications are monoubiquitination, multi-monoubiquitination, polyubiquitination, mixed-polyubiquitination, and branched polyubiquitination [61,62]. Ubiquitination affects many cellular functions, such as protein degradation, DNA damage response (DDR), cell cycle control, apoptosis, autophagy, endocytosis, and cellular signaling [62,63,64,65,66], and each ubiquitin residue plays different roles in cells. For instance, Met1-linked ubiquitination regulates NF-κB signaling pathway, anti-apoptosis, and hypoxic stress; Lys6-linked polyubiquitin is associated with mitophagy; Lys11-linked ubiquitin chain regulates cell division; Lys27-linked polyubiquitination blocks the activation of the inflammasome; Lys29-linked diubiquitin regulates the cell cycle and proteotoxic stress; Lys33-linked polyubiquitination is associated with DNA methylation; Lys48-, branched Lys63 and Lys48-linked polyubiquitin chains are related to proteasomal degradation; and Lys63-linked polyubiquitination regulates DNA damage repair and PI3K/Akt signaling [67,68,69,70,71,72,73,74,75,76].
1.2.2. UPS
UPS is composed of ubiquitin E1, E2, E3, and 26S proteasomes. Through this mechanism, substrate proteins, which have a polyubiquitin chain, are degraded through the 26S proteasome using ATPs [77,78]. The proteasome is composed of the 20S proteasome, which is the core of proteolysis, and various proteasome regulators (e.g., PA700, PA28αβ, PA28γ, P200, ECM29, and PSMF1) [79]. UPS dysfunction occurs in many diseases, such as neurodegenerative diseases, autoimmune diseases, diabetes, and cancer [80,81]. Thus, UPS components are a target of diseases, specifically cancers that induce apoptosis and cell cycle arrest [82,83].
1.2.3. DUBs
DUBs detach ubiquitin from substrate proteins, and proteins that lose the polyubiquitin chain (Figure 1) [84,85]. DUBs are regulated by PTM such as phosphorylation, ubiquitination, SUMOylation, lipid modification, and O-glycosylation. These PTMs regulate the stability, interaction affinity, localization, and catalytic activity of DUBs [86]. There are nine subfamilies divided by structural fold, the process of action, and sequence motifs [87]. These nine subfamilies are subdivided into eight Cys proteases and one metalloprotease, where protease targets proteolysis [88]. The eight Cys protease subfamilies are ubiquitin-specific proteases (USP), ovarian tumor proteases (OTU), ubiquitin C-terminal hydrolases (UCH), Machado-Josephin domain proteases (MJD), monocyte chemotactic protein-induced protease (MCPIP), permuted papin fold-peptidase of dsDNA and eukaryotes (PPPDE), motifs interacting with Ub-containing novel DUB family (MINDY), and zinc finger with UFM1-specific peptidase domain protein (ZUFSP). One metalloprotease subfamily is the JAB1/MPN/MOV34 metalloenzymes (JAMM) [87,89,90,91].
1.2.4. UPS and DUBs in Cancer
DUBs and the UPS are related to several diseases, such as neurodegeneration, developmental disorders, and cancers [65]. Specifically, ubiquitination of oncoproteins and deubiquitination of tumor suppressor proteins may lead to tumorigenesis suppression, tumor progression, cancer metabolism, and chemotherapy or radiotherapy resistance, whereas deubiquitination of oncoproteins causes cancer by prolonging the half-life of oncoproteins [62,89,92]. For instance, deubiquitination of FOXM1 induces cancer progression and chemoresistance through the DUB UCHL3; OTUD1 reduces the pro-oncogenic TGF-β signaling mediated by SMAD7 to suppress the metastasis in breast cancer [93,94].
2. DUBs in Ovarian Cancer
Fifteen different DUBs and their 17 substrates have been investigated in ovarian cancer (Table 2). Most DUBs have been studied in high-grade serous and endometrioid carcinomas, while non-epithelial, mucinous, and clear cell carcinomas have rarely been studied. Surprisingly, all DUBs related to ovarian cancer were overexpressed and seemed to act like an oncoprotein. Therefore, mechanistic studies of these DUBs, their substrates, and intracellular functions could be the basis for EOC treatment.
Table 2.
List of DUBs, substrates, and functions which are associated with ovarian cancer.
| DUBs | Subtypes of Cancer | Substrates | Functions | Proteins Related to Function | Expression in Cancer | Level of Expression | References |
|---|---|---|---|---|---|---|---|
| USP5 | Serous, endometrioid | HDAC2 | Cell cycle arrest, chemoresistance, apoptosis | p21, p27 | Up | mRNA, protein | [95] |
| USP14 | Serous, endometrioid | BCL-XL | Apoptosis, cell cycle arrest | PCNA, Cyclin A, Cyclin D1 | Up | Protein | [96] |
| Serous, endometrioid | BCL-6 | Chemoresistance apoptosis, | Not determined | Up | Protein | [97] | |
| USP15 | Serous, endometrioid | p53 (R175H) | Tumor cell death | Not determined | Up | mRNA | [98] |
| USP13 | Serous | ACLY, OGDH | Glutaminolysis, mitochondrial dysfunction, lipid synthesis | Not determined | Up | Copy number | [99] |
| Serous, clear cell | MCL-1 | Apoptosis | Not determined | Up | Protein | [100] | |
| Serous, mucinous | RAP80 | DNA damage response, chemoresistance | BRCA1, CCDC98 | Up | mRNA, protein | [101] | |
| USP10 | Serous, endometrioid | G3BP1 | Cell proliferation, migration, invasion | Not determined | Up | mRNA | [102] |
| USP32 | Serous, endometrioid | FDFT1 | Tumor sphere formation (invasion) | ZEB1, FN1, CDH1, CDH2, Snail 1 | Up | Protein | [103] |
| COPS5 | Serous, endometrioid | p27 | Cell proliferation, apoptosis | Akt | Up | mRNA, protein | [104,105] |
| PSMD14 | Serous, endometrioid | PKM2 | Cell viability, migration, invasion | Not determined | Up | mRNA, protein | [106] |
| USP17 | Serous, clear cell, endometrioid | MCL-1 | Chemoresistance, apoptosis | MGMT | Up | Protein | [107] |
| USP36 | Serous, endometrioid | PrimPol | Chemoresistance, DNA replication stress | Not determined | Up | Protein | [108] |
| OTUB1 | Serous, endometrioid | FOXM1 | Cell cycle arrest, invasion | Snail, CDC25B, Cyclin B | Up | Protein | [109] |
| UCHL3 | Serous, endometrioid | TRAF2 | Inflammatory response, tumorigenesis, migration | NF-κB1 | Up | mRNA, protein | [110] |
| USP11 | Serous | Snail | Cell proliferation, migration, invasion, | E-cadherin, N-cadherin, Fibronectin | Up | mRNA, protein | [111] |
| USP1 | Serous, clear cell, endometrioid | Snail | Invasion, metastasis | ATM, ATR | Up | Protein | [112] |
| USP35 | Serous | STING | Chemoresistance | TBK, IRF3, IFN-β | Up | Protein | [113] |
2.1. DUBs Associated with Cell Cycle Arrest
The cell cycle in cancer cells is unscheduled because of the scarcity of checkpoints, owing to chromosomal and genomic instability [114]. Cell cycle arrest and control by checkpoints are important for cancer growth control. Cell cycle checkpoints are regulated by various cyclin-dependent kinase (CDK) and cyclin families. The G1/S checkpoint is activated by certain stimuli (such as hormones, ultraviolet (UV), replicative senescence, and growth factors) which inhibit the CDK4/CDK6/Cyclin D complex or CDK2/Cyclin E complex through p15, p16, p18, p19, and p27 [114,115,116,117]. The G2/M checkpoint is activated by DNA damage such as UV radiation, platinum-based therapy, or infrared radiation (IR) [118]. CDC2/Cyclin B complex promotes the cell cycle from the G2 phase to the M phase. This complex is inhibited by p53 via p21 and GADD45 [119,120]. However, when DNA damage could not be repaired appropriately, programmed cell death would be induced by checkpoint signaling [115].
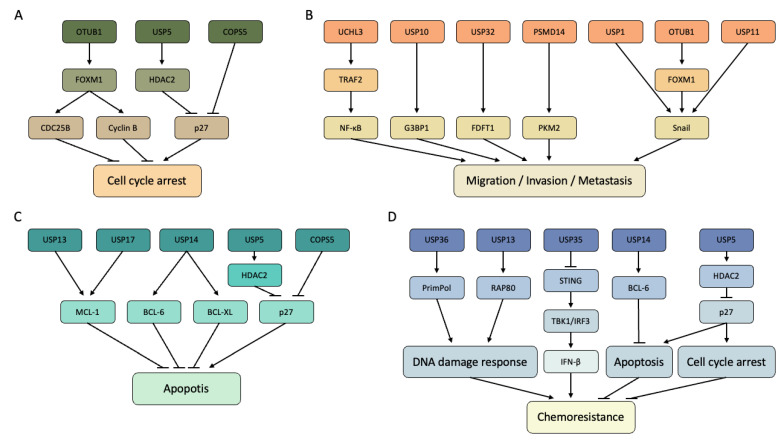
COPS5 and USP5 negatively regulate the stability of p27 (Figure 2A) [95,104,105]. p27 induces cell cycle arrest by inhibiting the CDK2/Cyclin E complex at the G1/S checkpoint [119]. Moreover, USP5 positively regulates the stability and deubiquitinates HDAC2, of which the mutation or loss of function acts as an oncogene (Figure 2A) [95,121]. OTUB1 positively regulated CDC25B and Cyclin B via the control of FOXM1 (Figure 2A) [109]. FOXM1 promotes the transcription of both genes to their target promoters [122,123]. Moreover, FOXM1 promotes the E2F pathway by regulating CDC25B gene transcription [122]. Between CDC25B and Cyclin B, CDC25B dephosphorylates CDK1/Cyclin B to induce the cell cycle from G2 to M [124,125].
Figure 2.
DUBs, substrates, and their functions. (A) DUBs and substrates associated with cell cycle arrest. (B) DUBs and substrates associated with migration, invasion, and metastasis. (C) DUBs and substrates associated with apoptosis. (D) DUBs and substrates associated with DNA damage response and chemoresistance. The arrows from the DUBs to the substrates indicate that the binding between them is confirmed, and the stability of the substrate is controlled by DUBs.
2.2. DUBs Associated with Migration, Invasion, and Metastasis
Metastasis in cancer is a critical event that affects the survival of patients and is one of the standards of cancer progression. In EOC, there are three ways for metastasis in ovarian cancer: transcoelomic, hematogenous, and lymphatic routes, of which hematogenic, motility, and lethal routes are the most common [126]. Metastasis occurs through epithelial–mesenchymal transition (EMT) in cancer cells through the exchange of cadherin and integrin expression levels [127]. To investigate cancer metastasis in vitro, migration assay and invasion assay were performed, and the EMT-associated markers, such as E-cadherin, N-cadherin, ZEB, Snail, and Twist were verified [128,129].
USP1, OUTB1, and USP11 induced migration, invasion, and metastasis through Snail (Figure 2B) [109,111,112]. OTUB1 positively regulates FOXM1, a transcription factor that promotes Snail transcription. FOXM1 regulates EMT, cell migration, and drug resistance [130]. Snail is also a transcription factor that promotes EMT and motility of cells [131]. Snail regulates the expression of E-cadherin, N-cadherin, fibronectin, and vimentin to induce EMT [132]. As Snail is usually overexpressed in cancer tissue and especially metastatic tissue, patients with the highly expressed Snail exhibited the short survival expectancy [133,134].
TRAF2 was deubiquitinated and positively regulated by UCHL3 (Figure 2B) [110]. NF-κB which is regulated by TRAF2, belongs to a family of five master transcription factors. Twist, adhesion molecules, and other EMT-associated molecules are the targets of NF-κB [135]. USP10 regulates GTPase-activating protein SH3 domain-binding protein 1 (G3BP1) (Figure 2B) [102]. G3BP1 is an RNA-binding protein that affects the stability of mRNA in response to extracellular stimuli. G3BP1 responds to cellular stress and activates the STING pathway by binding to dsDNA and RNA in the cytosol [136]. In addition to inducing metastasis in EOC, G3BP1 induces metastasis through IL-6/G3BP1/STAT3 signaling in renal cell carcinoma [137]. FDFT1 stability is regulated by USP32, and this mechanism is associated with mesenchymal markers, such as FN1, ZEB1, Snail, and CDH2 (Figure 2B) [103]. In various cancers, including ovarian cancer, FDFT1 is associated with invasion and activates cancer cell metastasis through MMP1, CD44, and AKT/mTOR/HIF1α signaling [138]. PSMD14 deubiquitinated PKM2 and positively regulated the PKM2 monomer (Figure 2B) [106]. PKM2 promotes EMT by inhibiting E-cadherin expression and cancer metastasis along with PAK2 and HSP90 [139].
2.3. DUBs Associated with Apoptosis
Apoptosis is a caspase-dependent programmed cell death promoted by reactive oxygen species (ROS), UV radiation, chemotherapy, and other stimuli [140,141]. In ovarian cancer, patients are treated by radio and chemotherapy, which induce apoptosis. Specifically, radiotherapy and platinum-based therapies induce DNA damage [41]. DNA damage, one of the causes of the intrinsic apoptotic pathway, promotes p53 overexpression [39]. Overexpression of p53 activates the p53-dependent apoptotic pathway, which activates BAX, BAK, mitochondrial outer membrane permeabilization (MOMP), apoptotic protease activating factor 1 (APAF1), caspase-9 to form an apoptosome and cause apoptosis [141,142]. Moreover, taxane causes cell cycle arrest by blocking the cell division and promotes apoptosis through the abnormal activity of c-Jun N-terminal kinase/stress-activated protein kinase (JNK/SAPK), BCL-2, and p53 pathway [143,144].
In ovarian cancer, USP13, USP17, and USP14 positively regulate the stability of MCL-1 and BCL-XL, which are members of the anti-apoptotic BCL-2 family (Figure 2C) [96,100,107]. As MCL-1 and BCL-XL suppress BAX and BAK to inhibit the intrinsic apoptosis pathway, the expression levels of USP13, USP17, and USP14 are important. Therefore, it is predicted that upregulation of MCL-1 and BCL-XL would result in poor treatment because of inhibiting apoptosis in cancer cells [145]. USP14 also positively regulates the stability of BCL-6, a proto-oncogene that inhibits the expression of p53; consequently, p53-dependent apoptosis is suppressed (Figure 2C) [97,146,147]. USP5 negatively regulated the stability of p27 by modulating the HDCA2 expression (Figure 2C) [95]. HDAC2 and COPS5 downregulate p27, a regulator of CDK/Cyclin, which is associated with apoptosis via cell cycle arrest [148].
2.4. DUBs Associated with DNA Damage and Chemoresistance
DDR occurs when cells experience DNA dagame through stimuli, and the repair mechanism of DDR varies depending on which damage occurs. There are five main DDR mechanisms: homologous recombination (HR), base excision repair (BER), mismatch repair (MMR), nucleotide excision repair (NER), and nonhomologous end joining (NHEJ) [149]. In the course of ovarian cancer treatment, cisplatin leads to the induction of BER, NER, HR, and NHEJ through the DNA adduction, DNA crosslinking, and the production of reactive oxygen species [150,151,152,153,154,155].
USP13 regulates and deubiquitinates RAP80, which regulates HR through BRCA1, BRCC46, and Abraxas (Figure 2D) [101,156]. USP36 deubiquitinates and regulates the stability of PrimPol, a DNA damage-tolerant polymerase (Figure 2D) [108]. PrimPol synthesizes the DNA primers to restart and reprime DNA replication during replication stress [108,157]. PrimPol is also involved in DDR as the component of the Fanconi anemia pathway to repair DNA by intra-strand crosslink [158].
Chemoresistance could be caused by a combination of several complex factors. In this review, we focused on the combination of DUBs and their substrates that leads to chemoresistance (Figure 2D). USP14 inhibits apoptosis by deubiquitinates BCL-6. USP5 inhibits cell cycle arrest by deubiquitinates HDAC2. PrimPol which is deubiquitinated by USP36 increases DNA replication. RAP80 deubiquitinated by USP13 promotes DDR through BRCA1. These studies have also shown that chemoresistance could be induced by overexpression of these DUBs and their substrates [95,97,101,108]. Lastly, USP35 suppressed anti-tumor immunity of type I interferon through the STING/TBK1/IRF3 pathway and as a result, chemoresistance was induced [113,159,160,161].
2.5. Other DUBs
Mutated p53 promotes EMT, receptor tyrosine kinase signaling, and interactions with the extracellular matrix [162]. In particular, the p53 (R175H) cancer cell growth through the GEF-H1 pathway and cell cycle in EOC [163,164]. Mutated p53 (R157H) is deubiquitinated by USP15 [98]. The half-life of deubiquitinated p53 (R175H) increases and aggregates to show a gain of functions.
USP13 regulates the stability of oxoglutarate dehydrogenase (ODGH) and ATP citrate lyase (ACLY) through deubiquitination [99]. ODGH mediates the conversion of decarbonized α-ketoglutaric acid to fumarate and ACLY lysis of citrate to acetyl-CoA. USP13 knockdown inhibits both mechanisms, resulting in mitochondrial and lipogenic dysfunctions. Therefore, USP13 suppression decreases ATP production by repressing the TCA cycle and inhibiting de novo lipogenesis [99].
3. Discussions
Early diagnosis of ovarian cancer is critical for patient survival. The survival rates of patients with stage I and II cancer were high, but the survival rates of patients with stage III and IV cancer were low. However, most patients were diagnosed with stages III and IV [165]. Therefore, diagnosis through serum tests, such as CA125 and HE4, is important. TVS often needs to be performed for accurate examination; however, because it has some limitations, it is quicker and more convenient to detect cancers during a blood test. The diagnostic rate of serum tests based on CA125, HE4, and ROMA is quite high, but it is still necessary to develop biomarkers that could reliably detect cancer in serum [166]. Because DUBs showed elevated expression in several cancers, they may be used as biomarkers. Mainly USP4, USP7, USP22, UCHL1, UCHL5, and OTUB1 could be used as biomarkers for each type of cancer such as EOC, breast cancer, melanoma, cervical cancer, and colorectal cancer [167]. The DUBs in Table 2 could be used as biomarkers for ovarian cancer; however, serum detection is required. This is because core-transvaginal needle biopsy is not commonly used because of the risk of metastasis [38]. In addition, identifying biomarkers to predict diagnosis or targeted therapy through postoperative patient sample analysis is also very important for improving patient survival.
All DUBs listed in this review (Table 2) are elevated in cancer; therefore, DUB inhibitors could be used to treat patients. Many DUB inhibitors, such as P5091, inhibits USP7, Sputin1, which inhibits USP10 and USP13, and LDN-57444, which inhibits UCHL1 and UCHL3 [167]. In addition, the DUB inhibitor VLX1570, which inhibits USP14 and UCHL5, has undergone phase 1 clinical trials in multiple melanoma patients [168]. However, because the characteristic of DUB inhibitors is that one DUB should regulate multiple substrates, side effects could be severe when drugs targeting DUB are treated. To overcome this limitation, DUB-tailored inhibitor synthesis based on ultra-high throughput screening technology has been suggested as an innovative method for finding selective DUB inhibitors [169].
As well as finding selective DUB inhibitors, research has focused on the development of proteolysis-targeting chimera (PROTAC) and deubiquitinase-targeting chimera (DUBTAC), to reduce their side effects. PROTAC or DUBTAC is composed of a ligand of E3 ligase or DUB, a linker, and a ligand of the substrate. These molecules promote the binding and activity of E3 ligases or DUBs to substrates [170,171]. One of the PROTAC, ARV-110, which targets androgen receptors in prostate cancer, completed phase 2 clinical trials, and ARV-471, which targets estrogen receptor in breast cancer, also completed phase 2 clinical trials [172]. Based on this notion, it could be used as an adjuvant drug by reducing the half-life of the targeted oncoprotein or increasing the stability of the anti-cancer protein. In addition, it might be possible to make cells chemosensitive by targeting proteins related to chemoresistance. Therefore, it would be effective to develop PROTAC and DUBTAC as well as DUB inhibitors because they could reduce side effects and target multiple proteins with similar functions by targeting a specific domain.
This review has several limitations. Firstly, we summarized only DUBs with their known substrates in ovarian cancers. There are more studies on identifying important DUBs such as USP8 and USP19 in ovarian cancers [173,174]. However, in this paper, we could not include them, as their target substrates and underlying mechanism were unknown. In addition, we could not include well-known mechanisms of DUBs in other cancers. For example, USP1 deubiquitinates FANCD2/FANCI or PCNA to prevent the recruitment of interstrand crosslink repair proteins and translesion DNA polymerase to inhibit DNA repair; USP7 regulates lung squamous cell carcinoma cell proliferation through MEK/ERK signaling by deubiquitinates the Raf-1 [175,176]. These well-known DUBs could also have key roles in ovarian cancers through these mechanisms, but it further needs to be confirmed experimentally.
4. Conclusions
In this review, we have organized 15 DUBs, 17 substrates, and their functions in EOC. This could support the development of biomarkers or the search for therapeutic targets. The functions of DUBs via regulating substrates, which are oncoproteins or anti-cancer proteins, are indispensable for revealing the mechanisms in ovarian cancer cells. Among the 100 DUBs that were identified, only 15 have been investigated in EOC. Therefore, further research is needed to overcome EOC.
Author Contributions
Writing original draft preparation, Y.M. and H.-B.P.; writing review and editing, S.H. and K.-H.B.; visualization, Y.M.; supervision, S.H. and K.-H.B.; funding acquisition, S.H. and K.-H.B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was funded by a grant (No. HI16C1559) from the Korea Health Technology R&D Project through The Korea Health Industry Development Institute (KHIDI); the Basic Science Research Program through the National Research Foundation of Korea (NRF) with a grant (No. NRF-2019R1A6A1A03032888) funded by the Ministry of Education; and supported by the NRF grant (No. 2022R1A2C109179712) funded by the Ministry of Science and ICT (MSIT).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Stewart C., Ralyea C., Lockwood S. Ovarian Cancer: An Integrated Review. Semin. Oncol. Nurs. 2019;35:151–156. doi: 10.1016/j.soncn.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Ovarian Cancer—Cancer Stat Facts. [(accessed on 14 November 2022)]; Available online: https://seer.cancer.gov/statfacts/html/ovary.html.
- 3.SEER*Explorer Application. [(accessed on 14 November 2022)]; Available online: https://seer.cancer.gov/statistics-network/explorer/application.html?site=61&data_type=4&graph_type=5&compareBy=stage&chk_stage_104=104&chk_stage_105=105&chk_stage_106=106&chk_stage_107=107&series=age_range&chk_age_range_1=1&chk_age_range_9=9&chk_age_range_141=141&chk_age_range_157=157&hdn_sex=3&race=1&advopt_precision=1&advopt_show_ci=on&hdn_view=0&advopt_display=2#graphArea.
- 4.Webb P.M., Jordan S.J. Epidemiology of Epithelial Ovarian Cancer. Best Pract. Res. Clin. Obstet. Gynaecol. 2017;41:3–14. doi: 10.1016/j.bpobgyn.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 5.Berek J.S., Renz M., Kehoe S., Kumar L., Friedlander M. Cancer of the Ovary, Fallopian Tube, and Peritoneum: 2021 Update. Int. J. Gynecol. Obstet. 2021;155:61–85. doi: 10.1002/ijgo.13878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ovarian Epithelial, Fallopian Tube, and Primary Peritoneal Cancer Treatment (PDQ®)–Patient Version-NCI. [(accessed on 14 November 2022)]; Available online: https://www.cancer.gov/types/ovarian/patient/ovarian-epithelial-treatment-pdq#_104.
- 7.Baek S.-J., Park J.-Y., Kim D.-Y., Kim J.-H., Kim Y.-M., Kim Y.-T., Nam J.-H. Stage IIIC Epithelial Ovarian Cancer Classified Solely by Lymph Node Metastasis Has a More Favorable Prognosis than Other Types of Stage IIIC Epithelial Ovarian Cancer. J. Gynecol. Oncol. 2008;19:223–228. doi: 10.3802/jgo.2008.19.4.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roett M.A., Evans P. Ovarian cancer: An overview. Am. Fam. Physician. 2009;80:609–616. [PubMed] [Google Scholar]
- 9.Jayson G.C., Kohn E.C., Kitchener H.C., Ledermann J.A. Ovarian Cancer. Lancet. 2014;384:1376–1388. doi: 10.1016/S0140-6736(13)62146-7. [DOI] [PubMed] [Google Scholar]
- 10.Matulonis U.A., Sood A.K., Fallowfield L., Howitt B.E., Sehouli J., Karlan B.Y. Ovarian Cancer. Nat. Rev. Dis. Prim. 2016;2:16061. doi: 10.1038/nrdp.2016.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Zyl B., Tang D., Bowden N.A. Biomarkers of platinum resistance in ovarian cancer: What can we use to improve treatment. Endocr.-Relat. Cancer. 2018;25:r303–r318. doi: 10.1530/ERC-17-0336. [DOI] [PubMed] [Google Scholar]
- 12.McCluggage W.G. My Approach to and Thoughts on the Typing of Ovarian Carcinomas. J. Clin. Pathol. 2008;61:152–163. doi: 10.1136/jcp.2007.049478. [DOI] [PubMed] [Google Scholar]
- 13.Bowtell D.D., Böhm S., Ahmed A.A., Aspuria P.-J., Bast R.C., Beral V., Berek J.S., Birrer M.J., Blagden S., Bookman M.A., et al. Rethinking ovarian cancer II: Reducing mortality from high-grade serous ovarian cancer. Nat. Rev. Cancer. 2015;15:668–679. doi: 10.1038/nrc4019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morphologic, Immunophenotypic, and Molecular Features of Epithelial Ovarian Cancer. [(accessed on 18 November 2022)]. Available online: https://www.cancernetwork.com/view/morphologic-immunophenotypic-and-molecular-features-epithelial-ovarian-cancer.
- 15.Vang R., Levine D.A., Soslow R.A., Zaloudek C., Shih Ie M., Kurman R.J. Molecular Alterations of TP53 are a Defining Feature of Ovarian High-Grade Serous Carcinoma: A Rereview of Cases Lacking TP53 Mutations in The Cancer Genome Atlas Ovarian Study. Int. J. Gynecol. Pathol. 2016;35:48–55. doi: 10.1097/PGP.0000000000000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kurman R.J. Origin and Molecular Pathogenesis of Ovarian High-Grade Serous Carcinoma. Ann. Oncol. 2013;24:x16–x21. doi: 10.1093/annonc/mdt463. [DOI] [PubMed] [Google Scholar]
- 17.O’Neill C.J., Deavers M.T., Malpica A., Foster H., McCluggage W.G. An Immunohistochemical Comparison Between Low-Grade and High-Grade Ovarian Serous Carcinomas: Significantly Higher Expression of P53, MIB1, BCL2, HER-2/Neu, and C-KIT in High-Grade Neoplasms. Am. J. Surg. Pathol. 2005;29:1034–1041. doi: 10.1097/01.pas.0000166367.68459.7d. [DOI] [PubMed] [Google Scholar]
- 18.Crispens M.A. Endometrial and Ovarian Cancer in Lynch Syndrome. Clin. Colon Rectal Surg. 2012;25:97–102. doi: 10.1055/s-0032-1313780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vargas A.N. Natural History of Ovarian Cancer. Ecancermedicalscience. 2014;8:465. doi: 10.3332/ecancer.2014.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brown J., Frumovitz M. Mucinous tumors of the ovary: Current thoughts on diagnosis and management. Curr. Oncol. Rep. 2014;16:389. doi: 10.1007/s11912-014-0389-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ryland G.L., Hunter S.M., Doyle M.A., Caramia F., Li J., Rowley S.M., Christie M., Allan P.E., Stephens A.N., Bowtell D.D., et al. Mutational landscape of mucinous ovarian carcinoma and its neoplastic precursors. Genome Med. 2015;7:87. doi: 10.1186/s13073-015-0210-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tan D.S., Kaye S. Ovarian clear cell adenocarcinoma: A continuing enigma. J. Clin. Pathol. 2007;60:355–360. doi: 10.1136/jcp.2006.040030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gershenson D.M., Morris M., Cangir A., Kavanagh J.J., Stringer C.A., Edwards C.L., Silva E.G., Wharton J.T. Treatment of malignant germ cell tumors of the ovary with bleomycin, etoposide, and cisplatin. J. Clin. Oncol. 1990;8:715–720. doi: 10.1200/JCO.1990.8.4.715. [DOI] [PubMed] [Google Scholar]
- 24.Tschernichovsky R., Goodman A. Risk-Reducing Strategies for Ovarian Cancer in BRCA Mutation Carriers: A Balancing Act. Oncologist. 2017;22:450–459. doi: 10.1634/theoncologist.2016-0444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Horta M., Cunha T.M. Sex Cord-Stromal Tumors of the Ovary: A Comprehensive Review and Update for Radiologists. Diagn. Interv. Radiol. 2015;21:277–286. doi: 10.5152/dir.2015.34414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schultz K.A.P., Harris A.K., Schneider D.T., Young R.H., Brown J., Gershenson D.M., Dehner L.P., Hill D.A., Messinger Y.H., Frazier A.L. Ovarian Sex Cord-Stromal Tumors. J. Oncol. Pract. 2016;12:940–946. doi: 10.1200/JOP.2016.016261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walker J.L., Powell C.B., Chen L., Carter J., Bae Jump V.L., Parker L.P., Borowsky M.E., Gibb R.K. Society of Gynecologic Oncology Recommendations for the Prevention of Ovarian Cancer. Cancer. 2015;121:2108–2120. doi: 10.1002/cncr.29321. [DOI] [PubMed] [Google Scholar]
- 28.Mallen A., Soong T.R., Townsend M.K., Wenham R.M., Crum C.P., Tworoger S.S. Surgical Prevention Strategies in Ovarian Cancer. Gynecol. Oncol. 2018;151:166–175. doi: 10.1016/j.ygyno.2018.08.005. [DOI] [PubMed] [Google Scholar]
- 29.Stone R.L., Nick A.M., McNeish I.A., Balkwill F., Han H.D., Bottsford-Miller J., Rupairmoole R., Armaiz-Pena G.N., Pecot C.V., Coward J., et al. Paraneoplastic thrombocytosis in ovarian cancer. N. Engl. J. Med. 2012;366:610–618. doi: 10.1056/NEJMoa1110352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Králíčková M., Laganà A.S., Ghezzi F., Vetvicka V. Endometriosis and Risk of Ovarian Cancer: What Do We Know? Arch. Gynecol. Obstet. 2020;301:1–10. doi: 10.1007/s00404-019-05358-8. [DOI] [PubMed] [Google Scholar]
- 31.Wang L., Zhou S., Guo B. Vitamin D Suppresses Ovarian Cancer Growth and Invasion by Targeting Long Non-Coding RNA CCAT2. Int. J. Mol. Sci. 2020;21:2334. doi: 10.3390/ijms21072334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang M., Cheng S., Jin Y., Zhao Y., Wang Y. Roles of CA125 in Diagnosis, Prediction, and Oncogenesis of Ovarian Cancer. Biochim. Biophys. Acta (BBA)—Rev. Cancer. 2021;1875: 188503. doi: 10.1016/j.bbcan.2021.188503. [DOI] [PubMed] [Google Scholar]
- 33.Hellström I., Raycraft J., Hayden-Ledbetter M., Ledbetter J.A., Schummer M., McIntosh M., Drescher C., Urban N., Hellström K.E. The HE4 (WFDC2) Protein Is a Biomarker for Ovarian Carcinoma. Cancer Res. 2003;63:3695–3700. [PubMed] [Google Scholar]
- 34.Dochez V., Caillon H., Vaucel E., Dimet J., Winer N., Ducarme G. Biomarkers and Algorithms for Diagnosis of Ovarian Cancer: CA125, HE4, RMI and ROMA, a Review. J. Ovarian Res. 2019;12:28. doi: 10.1186/s13048-019-0503-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim B., Park Y., Kim B., Ahn H.J., Lee K.-A., Chung J.E., Han S.W. Diagnostic Performance of CA 125, HE4, and Risk of Ovarian Malignancy Algorithm for Ovarian Cancer. J. Clin. Lab. Anal. 2019;33:e22624. doi: 10.1002/jcla.22624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Valentin L., Ameye L., Testa A., Lécuru F., Bernard J.-P., Paladini D., Van Huffel S., Timmerman D. Ultrasound Characteristics of Different Types of Adnexal Malignancies. Gynecol. Oncol. 2006;102:41–48. doi: 10.1016/j.ygyno.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 37.Timmerman D., Valentin L., Bourne T.H., Collins W.P., Verrelst H., Vergote I. Terms, Definitions and Measurements to Describe the Sonographic Features of Adnexal Tumors: A Consensus Opinion from the International Ovarian Tumor Analysis (IOTA) Group. Ultrasound Obstet. Gynecol. 2000;16:500–505. doi: 10.1046/j.1469-0705.2000.00287.x. [DOI] [PubMed] [Google Scholar]
- 38.Yousefi Z., Frazestanian M., Davachi B., Saeed S., Azad A., Tavakoli Khorasani S. Is Transvaginal Core Needle Biopsy A Safe Method in Diagnosis of Ovarian Cancer? Int. J. Cancer Manag. 2017:11. doi: 10.5812/ijcm.8121. [DOI] [Google Scholar]
- 39.Dasari S., Tchounwou P.B. Cisplatin in Cancer Therapy: Molecular Mechanisms of Action. Eur. J. Pharmacol. 2014;740:364–378. doi: 10.1016/j.ejphar.2014.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kelland L. The Resurgence of Platinum-Based Cancer Chemotherapy. Nat. Rev. Cancer. 2007;7:573–584. doi: 10.1038/nrc2167. [DOI] [PubMed] [Google Scholar]
- 41.Davis A., Tinker A.V., Friedlander M. “Platinum resistant” ovarian cancer: What is it, who to treat and how to measure ben-efit? Gynecol. Oncol. 2014;133:624–631. doi: 10.1016/j.ygyno.2014.02.038. [DOI] [PubMed] [Google Scholar]
- 42.Singla A.K., Garg A., Aggarwal D. Paclitaxel and its formulations. Int. J. Pharm. 2002;235:179–192. doi: 10.1016/S0378-5173(01)00986-3. [DOI] [PubMed] [Google Scholar]
- 43.Verweij J., Clavel M., Chevalier B. Paclitaxel (Taxol) and docetaxel (Taxotere): Not simply two of a kind. Ann. Oncol. 1994;5:495–505. doi: 10.1093/oxfordjournals.annonc.a058903. [DOI] [PubMed] [Google Scholar]
- 44.Shi X., Sun X. Regulation of Paclitaxel Activity by Microtubule-Associated Proteins in Cancer Chemotherapy. Cancer Chemother. Pharmacol. 2017;80:909–917. doi: 10.1007/s00280-017-3398-2. [DOI] [PubMed] [Google Scholar]
- 45.Weaver B.A. How Taxol/paclitaxel kills cancer cells. Mol. Biol. Cell. 2014;25:2677–2681. doi: 10.1091/mbc.e14-04-0916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.D’Andrea A.D. Mechanisms of PARP inhibitor sensitivity and resistance. DNA Repair. 2018;71:172–176. doi: 10.1016/j.dnarep.2018.08.021. [DOI] [PubMed] [Google Scholar]
- 47.Weil M.K., Chen A. PARP Inhibitor Treatment in Ovarian and Breast Cancer. Curr. Probl. Cancer. 2011;35:7–50. doi: 10.1016/j.currproblcancer.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Melnichenko I., Sargsyan L., Bedirian K., Dallakyan D., Gevorgyan A., Aloyan G., Harutyunyan A., Davtyan L., Lazaryan A., Manukyan N., et al. How to Treat Metastatic Malignant Triton Tumor in an Adolescent. Oncology. 2022;33:674–677. doi: 10.46883/2022.25920979. [DOI] [PubMed] [Google Scholar]
- 49.FDA . FDA Approves Bevacizumab in Combination with Chemotherapy for Ovarian Cancer. FDA; Silver Spring, MD, USA: 2019. [Google Scholar]
- 50.Khalique S., Banerjee S. Nintedanib in Ovarian Cancer. Expert Opin. Investig. Drugs. 2017;26:1073–1081. doi: 10.1080/13543784.2017.1353599. [DOI] [PubMed] [Google Scholar]
- 51.Orbegoso C., Marquina G., George A., Banerjee S. The Role of Cediranib in Ovarian Cancer. Expert Opin. Pharmacother. 2017;18:1637–1648. doi: 10.1080/14656566.2017.1383384. [DOI] [PubMed] [Google Scholar]
- 52.Padmakumar S., Parayath N., Leslie F., Nair S.V., Menon D., Amiji M.M. Intraperitoneal Chemotherapy for Ovarian Cancer Using Sustained-Release Implantable Devices. Expert Opin. Drug Deliv. 2018;15:481–494. doi: 10.1080/17425247.2018.1446938. [DOI] [PubMed] [Google Scholar]
- 53.Hacker N.F., Rao A. Surgery for Advanced Epithelial Ovarian Cancer. Best Pract. Res. Clin. Obstet. Gynaecol. 2017;41:71–87. doi: 10.1016/j.bpobgyn.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 54.Akutsu M., Dikic I., Bremm A. Ubiquitin Chain Diversity at a Glance. J. Cell Sci. 2016;129:875–880. doi: 10.1242/jcs.183954. [DOI] [PubMed] [Google Scholar]
- 55.Randles L., Walters K.J. Ubiquitin and Its Binding Domains. Front. Biosci. 2012;17:2140–2157. doi: 10.2741/4042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ciechanover A., Stanhill A. The Complexity of Recognition of Ubiquitinated Substrates by the 26S Proteasome. Biochim. Biophys. Acta (BBA)-Mol. Cell Res. 2014;1843:86–96. doi: 10.1016/j.bbamcr.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 57.Nandi D., Tahiliani P., Kumar A., Chandu D. The Ubiquitin-Proteasome System. J. Biosci. 2006;31:137–155. doi: 10.1007/BF02705243. [DOI] [PubMed] [Google Scholar]
- 58.Swatek K.N., Komander D. Ubiquitin Modifications. Cell Res. 2016;26:399–422. doi: 10.1038/cr.2016.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Do H.-A., Baek K.-H. Cellular Functions Regulated by Deubiquitinating Enzymes in Neurodegenerative Diseases. Ageing Res. Rev. 2021;69:101367. doi: 10.1016/j.arr.2021.101367. [DOI] [PubMed] [Google Scholar]
- 60.Leestemaker Y., Ovaa H. Tools to Investigate the Ubiquitin Proteasome System. Drug Discov. Today Technol. 2017;26:25–31. doi: 10.1016/j.ddtec.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 61.French M.E., Koehler C.F., Hunter T. Emerging Functions of Branched Ubiquitin Chains. Cell Discov. 2021;7:6. doi: 10.1038/s41421-020-00237-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Varshavsky A. Regulated Protein Degradation. Trends Biochem. Sci. 2005;30:283–286. doi: 10.1016/j.tibs.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 63.Schwertman P., Bekker-Jensen S., Mailand N. Regulation of DNA Double-Strand Break Repair by Ubiquitin and Ubiquitin-like Modifiers. Nat. Rev. Mol. Cell Biol. 2016;17:379–394. doi: 10.1038/nrm.2016.58. [DOI] [PubMed] [Google Scholar]
- 64.Oh E., Akopian D., Rape M. Principles of Ubiquitin-Dependent Signaling. Annu. Rev. Cell Dev. Biol. 2018;34:137–162. doi: 10.1146/annurev-cellbio-100617-062802. [DOI] [PubMed] [Google Scholar]
- 65.Rape M. Ubiquitylation at the Crossroads of Development and Disease. Nat. Rev. Mol. Cell Biol. 2018;19:59–70. doi: 10.1038/nrm.2017.83. [DOI] [PubMed] [Google Scholar]
- 66.Damgaard R.B. The Ubiquitin System: From Cell Signalling to Disease Biology and New Therapeutic Opportunities. Cell Death Differ. 2021;28:423–426. doi: 10.1038/s41418-020-00703-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wickliffe K.E., Williamson A., Meyer H.-J., Kelly A., Rape M. K11-Linked Ubiquitin Chains as Novel Regulators of Cell Division. Trends Cell Biol. 2011;21:656–663. doi: 10.1016/j.tcb.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ohtake F., Tsuchiya H., Saeki Y., Tanaka K. K63 ubiquitylation triggers proteasomal degradation by seeding branched ubiquitin chains. Proc. Natl. Acad. Sci. USA. 2018;115:E1401–E1408. doi: 10.1073/pnas.1716673115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Durcan T.M., Tang M.Y., Pérusse J.R., Dashti E.A., Aguileta M.A., McLelland G.-L., Gros P., Shaler T.A., Faubert D., Coulombe B., et al. USP8 Regulates Mitophagy by Removing K6-Linked Ubiquitin Conjugates from Parkin. EMBO J. 2014;33:2473–2491. doi: 10.15252/embj.201489729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wang D., Zhang Y., Xu X., Wu J., Peng Y., Li J., Luo R., Huang L., Liu L., Yu S., et al. YAP Promotes the Activation of NLRP3 Inflammasome via Blocking K27-Linked Polyubiquitination of NLRP3. Nat. Commun. 2021;12:2674. doi: 10.1038/s41467-021-22987-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu X., Xu B., Yang J., He L., Zhang Z., Cheng X., Yu H., Liu X., Jin T., Peng Y., et al. UHRF2 Commissions the Completion of DNA Demethylation through Allosteric Activation by 5hmC and K33-Linked Ubiquitination of XRCC1. Mol. Cell. 2021;81:2960–2974. doi: 10.1016/j.molcel.2021.05.022. [DOI] [PubMed] [Google Scholar]
- 72.Yu Y., Zheng Q., Erramilli S.K., Pan M., Park S., Xie Y., Li J., Fei J., Kossiakoff A.A., Liu L., et al. K29-Linked Ubiquitin Signaling Regulates Proteotoxic Stress Response and Cell Cycle. Nat. Chem. Biol. 2021;17:896–905. doi: 10.1038/s41589-021-00823-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhang H., Zhao X., Guo Y., Chen R., He J., Li L., Qiang Z., Yang Q., Liu X., Huang C., et al. Hypoxia regulates overall mRNA homeostasis by inducing Met(1)-linked linear ubiquitination of AGO2 in cancer cells. Nat. Commun. 2021;12:5416. doi: 10.1038/s41467-021-25739-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cao L., Liu X., Zheng B., Xing C., Liu J. Role of K63-Linked Ubiquitination in Cancer. Cell Death Discov. 2022;8:410. doi: 10.1038/s41420-022-01204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tang Y., Joo D., Liu G., Tu H., You J., Jin J., Zhao X., Hung M.-C., Lin X. Linear Ubiquitination of CFLIP Induced by LUBAC Contributes to TNFα-Induced Apoptosis. J. Biol. Chem. 2018;293:20062–20072. doi: 10.1074/jbc.RA118.005449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Aalto A., Martínez-Chacón G., Kietz C., Tsyganova N., Kreutzer J., Kallio P., Broemer M., Meinander A. M1-Linked Ubiquitination Facilitates NF-ΚB Activation and Survival during Sterile Inflammation. FEBS J. 2022;289:5180–5197. doi: 10.1111/febs.16425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sommer T., Wolf D.H. The Ubiquitin–Proteasome-System. Biochim. Biophys. Acta (BBA)-Mol. Cell Res. 2014;1843:1. doi: 10.1016/j.bbamcr.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 78.Bard J.A.M., Goodall E.A., Greene E.R., Jonsson E., Dong K.C., Martin A. Structure and Function of the 26S Proteasome. Annu. Rev. Biochem. 2018;87:697–724. doi: 10.1146/annurev-biochem-062917-011931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Albornoz N., Bustamante H., Soza A., Burgos P. Cellular Responses to Proteasome Inhibition: Molecular Mechanisms and Beyond. Int. J. Mol. Sci. 2019;20:3379. doi: 10.3390/ijms20143379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rousseau A., Bertolotti A. Regulation of Proteasome Assembly and Activity in Health and Disease. Nat. Rev. Mol. Cell Biol. 2018;19:697–712. doi: 10.1038/s41580-018-0040-z. [DOI] [PubMed] [Google Scholar]
- 81.Gilda J.E., Gomes A.V. Proteasome Dysfunction in Cardiomyopathies. J. Physiol. 2017;595:4051–4071. doi: 10.1113/JP273607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Guo N., Peng Z. MG132, a Proteasome Inhibitor, Induces Apoptosis in Tumor Cells. Asia-Pac. J. Clin. Oncol. 2013;9:6–11. doi: 10.1111/j.1743-7563.2012.01535.x. [DOI] [PubMed] [Google Scholar]
- 83.Kito Y., Matsumoto M., Hatano A., Takami T., Oshikawa K., Matsumoto A., Nakayama K.I. Cell Cycle–Dependent Localization of the Proteasome to Chromatin. Sci. Rep. 2020;10:5801. doi: 10.1038/s41598-020-62697-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Amerik A.Y., Hochstrasser M. Mechanism and Function of Deubiquitinating Enzymes. Biochim. Biophys. Acta (BBA)-Mol. Cell Res. 2004;1695:189–207. doi: 10.1016/j.bbamcr.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 85.Pickart C.M. Mechanisms Underlying Ubiquitination. Annu. Rev. Biochem. 2001;70:503–533. doi: 10.1146/annurev.biochem.70.1.503. [DOI] [PubMed] [Google Scholar]
- 86.Das T., Shin S.C., Song E.J., Kim E.E. Regulation of Deubiquitinating Enzymes by Post-Translational Modifications. Int. J. Mol. Sci. 2020;21:4028. doi: 10.3390/ijms21114028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kumar P., Kumar P., Mandal D., Velayutham R. The Emerging Role of Deubiquitinases (DUBs) in Parasites: A Foresight Review. Front. Cell. Infect. Microbiol. 2022;12:985178. doi: 10.3389/fcimb.2022.985178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Park H.-B., Baek K.-H. E3 Ligases and Deubiquitinating Enzymes Regulating the MAPK Signaling Pathway in Cancers. Biochim. Biophys. Acta (BBA)-Rev. Cancer. 2022;1877:188736. doi: 10.1016/j.bbcan.2022.188736. [DOI] [PubMed] [Google Scholar]
- 89.Kim S.-H., Baek K.-H. Regulation of Cancer Metabolism by Deubiquitinating Enzymes: The Warburg Effect. Int. J. Mol. Sci. 2021;22:6173. doi: 10.3390/ijms22126173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Xie X., Wang X., Jiang D., Wang J., Fei R., Cong X., Wei L., Wang Y., Chen H. PPPDE1 Is a Novel Deubiquitinase Belonging to a Cysteine Isopeptidase Family. Biochem. Biophys. Res. Commun. 2017;488:291–296. doi: 10.1016/j.bbrc.2017.04.161. [DOI] [PubMed] [Google Scholar]
- 91.Jin Z., Zheng E., Sareli C., Kolattukudy P.E., Niu J. Monocyte Chemotactic Protein-Induced Protein 1 (MCPIP-1): A Key Player of Host Defense and Immune Regulation. Front. Immunol. 2021;12:727861. doi: 10.3389/fimmu.2021.727861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sun T., Liu Z., Yang Q. The role of ubiquitination and deubiquitination in cancer metabolism. Mol. Cancer. 2020;19:146. doi: 10.1186/s12943-020-01262-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Song Z., Li J., Zhang L., Deng J., Fang Z., Xiang X., Xiong J. UCHL3 Promotes Pancreatic Cancer Progression and Chemo-Resistance through FOXM1 Stabilization. Am. J. Cancer Res. 2019;9:1970. [PMC free article] [PubMed] [Google Scholar]
- 94.Zhang Z., Fan Y., Xie F., Zhou H., Jin K., Shao L., Shi W., Fang P., Yang B., van Dam H., et al. Breast Cancer Metastasis Suppressor OTUD1 Deubiquitinates SMAD7. Nat. Commun. 2017;8:2116. doi: 10.1038/s41467-017-02029-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Du Y., Lin J., Zhang R., Yang W., Quan H., Zang L., Han Y., Li B., Sun H., Wu J. Ubiquitin Specific Peptidase 5 Promotes Ovarian Cancer Cell Proliferation through Deubiquitinating HDAC2. Aging. 2019;11:9778–9793. doi: 10.18632/aging.102425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wang Y., Wang J., Zhong J., Deng Y., Xi Q., He S., Yang S., Jiang L., Huang M., Tang C., et al. Ubiquitin-Specific Protease 14 (USP14) Regulates Cellular Proliferation and Apoptosis in Epithelial Ovarian Cancer. Med. Oncol. 2014;32:379. doi: 10.1007/s12032-014-0379-8. [DOI] [PubMed] [Google Scholar]
- 97.Shen J., Hong L., Chen L. Ubiquitin-Specific Protease 14 Regulates Ovarian Cancer Cisplatin-Resistance by Stabilizing BCL6 Oncoprotein. Biochem. Biophys. Res. Commun. 2020;524:683–688. doi: 10.1016/j.bbrc.2020.01.150. [DOI] [PubMed] [Google Scholar]
- 98.Padmanabhan A., Candelaria N., Wong K.K., Nikolai B.C., Lonard D.M., O’Malley B.W., Richards J.S. USP15-dependent lysosomal pathway controls p53-R175H turnover in ovarian cancer cells. Nat. Commun. 2018;9:1270. doi: 10.1038/s41467-018-03599-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Han C., Yang L., Choi H.H., Baddour J., Achreja A., Liu Y., Li Y., Li J., Wan G., Huang C., et al. Amplification of USP13 Drives Ovarian Cancer Metabolism. Nat. Commun. 2016;7:13525. doi: 10.1038/ncomms13525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zhang S., Zhang M., Jing Y., Yin X., Ma P., Zhang Z., Wang X., Di W., Zhuang G. Deubiquitinase USP13 Dictates MCL1 Stability and Sensitivity to BH3 Mimetic Inhibitors. Nat. Commun. 2018;9:215. doi: 10.1038/s41467-017-02693-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Li Y., Luo K., Yin Y., Wu C., Deng M., Li L., Chen Y., Nowsheen S., Lou Z., Yuan J. USP13 Regulates the RAP80-BRCA1 Complex Dependent DNA Damage Response. Nat. Commun. 2017;8:15752. doi: 10.1038/ncomms15752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Li M., Tang Y., Zuo X., Meng S., Yi P. Loss of Ras GTPase-activating protein SH3 domain-binding protein 1 (G3BP1) inhib-its the progression of ovarian cancer in coordination with ubiquitin-specific protease 10 (USP10) Bioengineered. 2022;13:721–734. doi: 10.1080/21655979.2021.2012624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Nakae A., Kodama M., Okamoto T., Tokunaga M., Shimura H., Hashimoto K., Sawada K., Kodama T., Copeland N.G., Jenkins N.A., et al. Ubiquitin specific peptidase 32 acts as an oncogene in epithelial ovarian cancer by deubiquitylating farnesyl-diphosphate farnesyltransferase 1. Biochem. Biophys. Res. Commun. 2021;552:120–127. doi: 10.1016/j.bbrc.2021.03.049. [DOI] [PubMed] [Google Scholar]
- 104.Zhang H., Zhong A., Sun J., Chen M., Xie S., Zheng H., Wang Y., Yu Y., Guo L., Lu R. COPS5 Inhibition Arrests the Proliferation and Growth of Serous Ovarian Cancer Cells via the Elevation of P27 Level. Biochem. Biophys. Res. Commun. 2017;493:85–93. doi: 10.1016/j.bbrc.2017.09.070. [DOI] [PubMed] [Google Scholar]
- 105.Wang Y., Wang Y., Cheng C., Ji Y., Zhao Y., Zou L., Shen A. Expression of Jun Activation Domain-Binding Protein 1 and Ser10 Phosphorylated P27 Protein in Human Epithelial Ovarian Carcinoma. J. Cancer Res. Clin. Oncol. 2009;135:951–959. doi: 10.1007/s00432-008-0531-y. [DOI] [PubMed] [Google Scholar]
- 106.Sun T., Liu Z., Bi F., Yang Q. Deubiquitinase PSMD14 promotes ovarian cancer progression by decreasing enzymatic activity of PKM2. Mol. Oncol. 2021;15:3639–3658. doi: 10.1002/1878-0261.13076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wu X., Luo Q., Zhao P., Chang W., Wang Y., Shu T., Ding F., Li B., Liu Z. MGMT-Activated DUB3 Stabilizes MCL1 and Drives Chemoresistance in Ovarian Cancer. Proc. Natl. Acad. Sci. USA. 2019;116:2961–2966. doi: 10.1073/pnas.1814742116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yan Y., Xu Z., Huang J., Guo G., Gao M., Kim W., Zeng X., Kloeber J.A., Zhu Q., Zhao F., et al. The Deubiquitinase USP36 Regulates DNA Replication Stress and Confers Therapeutic Resistance through PrimPol Stabilization. Nucleic Acids Res. 2020;48:12711–12726. doi: 10.1093/nar/gkaa1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wang Y., Zhou X., Xu M., Weng W., Zhang Q., Yang Y., Wei P., Du X. OTUB1-Catalyzed Deubiquitination of FOXM1 Facilitates Tumor Progression and Predicts a Poor Prognosis in Ovarian Cancer. Oncotarget. 2016;7:36681–36697. doi: 10.18632/oncotarget.9160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhang M.H., Zhang H.H., Du X.H., Gao J., Li C., Shi H.R., Li S.Z. UCHL3 promotes ovarian cancer progression by stabilizing TRAF2 to activate the NF-κB pathway. Oncogene. 2020;39:322–333. doi: 10.1038/s41388-019-0987-z. [DOI] [PubMed] [Google Scholar]
- 111.Wang W., Wang J., Yan H., Zhang K., Liu Y. Upregulation of USP11 Promotes Epithelial-to-mesenchymal Transition by Deubiquitinating Snail in Ovarian Cancer. Oncol. Rep. 2019;41:1739–1748. doi: 10.3892/or.2018.6924. [DOI] [PubMed] [Google Scholar]
- 112.Sonego M., Pellarin I., Costa A., Vinciguerra G.L.R., Coan M., Kraut A., D’Andrea S., Dall’Acqua A., Castillo-Tong D.C., Califano D., et al. USP1 Links Platinum Resistance to Cancer Cell Dissemination by Regulating Snail Stability. Sci. Adv. 2019;5:eaav3235. doi: 10.1126/sciadv.aav3235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zhang J., Chen Y., Chen X., Zhang W., Zhao L., Weng L., Tian H., Wu Z., Tan X., Ge X., et al. Deubiquitinase USP35 Restrains STING-Mediated Interferon Signaling in Ovarian Cancer. Cell Death Differ. 2021;28:139–155. doi: 10.1038/s41418-020-0588-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Malumbres M., Barbacid M. Cell Cycle, CDKs and Cancer: A Changing Paradigm. Nat. Rev. Cancer. 2009;9:153–166. doi: 10.1038/nrc2602. [DOI] [PubMed] [Google Scholar]
- 115.Pietenpol J.A., Stewart Z.A. Cell Cycle Checkpoint Signaling: Cell Cycle Arrest versus Apoptosis. Toxicology. 2002;181–182:475–481. doi: 10.1016/S0300-483X(02)00460-2. [DOI] [PubMed] [Google Scholar]
- 116.Musgrove E.A., Caldon C.E., Barraclough J., Stone A., Sutherland R.L. Cyclin D as a Therapeutic Target in Cancer. Nat. Rev. Cancer. 2011;11:558–572. doi: 10.1038/nrc3090. [DOI] [PubMed] [Google Scholar]
- 117.Goel S., DeCristo M.J., McAllister S.S., Zhao J.J. CDK4/6 Inhibition in Cancer: Beyond Cell Cycle Arrest. Trends Cell Biol. 2018;28:911–925. doi: 10.1016/j.tcb.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Al-Ejeh F., Kumar R., Wiegmans A., Lakhani S.R., Brown M.P., Khanna K.K. Harnessing the Complexity of DNA-Damage Response Pathways to Improve Cancer Treatment Outcomes. Oncogene. 2010;29:6085–6098. doi: 10.1038/onc.2010.407. [DOI] [PubMed] [Google Scholar]
- 119.Besson A., Dowdy S.F., Roberts J.M. CDK Inhibitors: Cell Cycle Regulators and Beyond. Dev. Cell. 2008;14:159–169. doi: 10.1016/j.devcel.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 120.Abbas T., Dutta A. P21 in Cancer: Intricate Networks and Multiple Activities. Nat. Rev. Cancer. 2009;9:400–414. doi: 10.1038/nrc2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ropero S., Esteller M. The Role of Histone Deacetylases (HDACs) in Human Cancer. Mol. Oncol. 2007;1:19–25. doi: 10.1016/j.molonc.2007.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Sullivan C., Liu Y., Shen J., Curtis A., Newman C., Hock J.M., Li X. Novel Interactions between FOXM1 and CDC25A Regulate the Cell Cycle. PLoS ONE. 2012;7:e51277. doi: 10.1371/journal.pone.0051277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Leung T.W.C., Lin S.S.W., Tsang A.C.C., Tong C.S.W., Ching J.C.Y., Leung W.Y., Gimlich R., Wong G.G., Yao K.-M. Over-Expression of FoxM1 Stimulates Cyclin B1 Expression. FEBS Lett. 2001;507:59–66. doi: 10.1016/S0014-5793(01)02915-5. [DOI] [PubMed] [Google Scholar]
- 124.Lindqvist A., Källström H., Lundgren A., Barsoum E., Rosenthal C.K. Cdc25B Cooperates with Cdc25A to Induce Mitosis but Has a Unique Role in Activating Cyclin B1–Cdk1 at the Centrosome. J. Cell Biol. 2005;171:35–45. doi: 10.1083/jcb.200503066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Donzelli M., Draetta G.F. Regulating Mammalian Checkpoints through Cdc25 Inactivation. EMBO Rep. 2003;4:671–677. doi: 10.1038/sj.embor.embor887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Tan D.S., Agarwal R., Kaye S.B. Mechanisms of Transcoelomic Metastasis in Ovarian Cancer. Lancet Oncol. 2006;7:925–934. doi: 10.1016/S1470-2045(06)70939-1. [DOI] [PubMed] [Google Scholar]
- 127.Lengyel E. Ovarian Cancer Development and Metastasis. Am. J. Pathol. 2010;177:1053–1064. doi: 10.2353/ajpath.2010.100105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kramer N., Walzl A., Unger C., Rosner M., Krupitza G., Hengstschläger M., Dolznig H. In Vitro Cell Migration and Invasion Assays. Mutat. Res./Rev. Mutat. Res. 2013;752:10–24. doi: 10.1016/j.mrrev.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 129.Thiery J.P., Acloque H., Huang R.Y.J., Nieto M.A. Epithelial-Mesenchymal Transitions in Development and Disease. Cell. 2009;139:871–890. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 130.Raychaudhuri P., Park H.J. FoxM1: A master regulator of tumor metastasis. Cancer Res. 2011;71:4329–4333. doi: 10.1158/0008-5472.CAN-11-0640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Villarejo A., Cortés-Cabrera A., Molina-Ortíz P., Portillo F., Cano A. Differential role of Snail1 and Snail2 zinc fingers in E-cadherin repression and epithelial to mesenchymal transition. J. Biol. Chem. 2014;289:930–941. doi: 10.1074/jbc.M113.528026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kang Y., Massagué J. Epithelial-mesenchymal transitions: Twist in development and metastasis. Cell. 2004;118:277–279. doi: 10.1016/j.cell.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 133.Taki M., Abiko K., Baba T., Hamanishi J., Yamaguchi K., Murakami R., Yamanoi K., Horikawa N., Hosoe Y., Nakamura E., et al. Snail promotes ovarian cancer progression by recruiting myeloid-derived suppressor cells via CXCR2 ligand upregulation. Nat. Commun. 2018;9:1685. doi: 10.1038/s41467-018-03966-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Blechschmidt K., Sassen S., Schmalfeldt B., Schuster T., Höfler H., Becker K.-F. The E-Cadherin Repressor Snail Is Associated with Lower Overall Survival of Ovarian Cancer Patients. Br. J. Cancer. 2008;98:489–495. doi: 10.1038/sj.bjc.6604115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Xia Y., Shen S., Verma I.M. NF-ΚB, an Active Player in Human Cancers. Cancer Immunol. Res. 2014;2:823–830. doi: 10.1158/2326-6066.CIR-14-0112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Wiser C., Kim B., Ascano M. G3BP1 Enhances Cytoplasmic DNA Pattern Recognition. Nat. Immunol. 2019;20:5–7. doi: 10.1038/s41590-018-0279-8. [DOI] [PubMed] [Google Scholar]
- 137.Wang Y., Fu D., Chen Y., Su J., Wang Y., Li X., Zhai W., Niu Y., Yue D., Geng H. G3BP1 Promotes Tumor Progression and Metastasis through IL-6/G3BP1/STAT3 Signaling Axis in Renal Cell Carcinomas. Cell Death Dis. 2018;9:501. doi: 10.1038/s41419-018-0504-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ha N.T., Lee C.H. Roles of Farnesyl-Diphosphate Farnesyltransferase 1 in Tumour and Tumour Microenvironments. Cells. 2020;9:2352. doi: 10.3390/cells9112352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Chen X., Chen S., Yu D. Protein kinase function of pyruvate kinase M2 and cancer. Cancer Cell Int. 2020;20:523. doi: 10.1186/s12935-020-01612-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Mohammad R.M., Muqbil I., Lowe L., Yedjou C., Hsu H.Y., Lin L.T., Siegelin M.D., Fimognari C., Kumar N.B., Dou Q.P., et al. Broad targeting of resistance to apoptosis in cancer. Semin. Cancer Biol. 2015;35:S78–S103. doi: 10.1016/j.semcancer.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Codispoti B., Makeeva I., Sied J., Benincasa C., Scacco S., Tatullo M. Should We Reconsider the Apoptosis as a Strategic Player in Tissue Regeneration? Int. J. Biol. Sci. 2019;15:2029–2036. doi: 10.7150/ijbs.36362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Singh R., Letai A., Sarosiek K. Regulation of Apoptosis in Health and Disease: The Balancing Act of BCL-2 Family Proteins. Nat. Rev. Mol. Cell Biol. 2019;20:175–193. doi: 10.1038/s41580-018-0089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Mosca L., Ilari A., Fazi F., Assaraf Y.G., Colotti G. Taxanes in Cancer Treatment: Activity, Chemoresistance and Its Overcoming. Drug Resist. Updates. 2021;54:100742. doi: 10.1016/j.drup.2020.100742. [DOI] [PubMed] [Google Scholar]
- 144.Wang T.-H., Wang H.-S., Soong Y.-K. Paclitaxel-Induced Cell Death. Cancer. 2000;88:2619–2628. doi: 10.1002/1097-0142(20000601)88:11<2619::AID-CNCR26>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 145.Youle R.J., Strasser A. The BCL-2 protein family: Opposing activities that mediate cell death. Nat. Rev. Mol. Cell Biol. 2008;9:47–59. doi: 10.1038/nrm2308. [DOI] [PubMed] [Google Scholar]
- 146.Jardin F., Ruminy P., Bastard C., Tilly H. The BCL6 proto-oncogene: A leading role during germinal center development and lymphomagenesis. Pathol Biol. 2007;55:73–83. doi: 10.1016/j.patbio.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 147.Phan R.T., Dalla-Favera R. The BCL6 Proto-Oncogene Suppresses P53 Expression in Germinal-Centre B Cells. Nature. 2004;432:635–639. doi: 10.1038/nature03147. [DOI] [PubMed] [Google Scholar]
- 148.Abbastabar M., Kheyrollah M., Azizian K., Bagherlou N., Tehrani S.S., Maniati M., Karimian A. Multiple functions of p27 in cell cycle, apoptosis, epigenetic modification and transcriptional regulation for the control of cell growth: A double-edged sword protein. DNA Repair. 2018;69:63–72. doi: 10.1016/j.dnarep.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 149.Chatterjee N., Walker G.C. Mechanisms of DNA Damage, Repair, and Mutagenesis. Environ. Mol. Mutagen. 2017;58:235–263. doi: 10.1002/em.22087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Rocha C.R.R., Silva M.M., Quinet A., Cabral-Neto J.B., Menck C.F.M. DNA Repair Pathways and Cisplatin Resistance: An Intimate Relationship. Clinics. 2018;73:e478s. doi: 10.6061/clinics/2018/e478s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Lord C.J., Ashworth A. The DNA Damage Response and Cancer Therapy. Nature. 2012;481:287–294. doi: 10.1038/nature10760. [DOI] [PubMed] [Google Scholar]
- 152.Pilié P.G., Tang C., Mills G.B., Yap T.A. State-of-the-Art Strategies for Targeting the DNA Damage Response in Cancer. Nat. Rev. Clin. Oncol. 2019;16:81–104. doi: 10.1038/s41571-018-0114-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Bouberhan S., Philp L., Hill S., Al-Alem L.F., Rueda B. Exploiting the Prevalence of Homologous Recombination Deficiencies in High-Grade Serous Ovarian Cancer. Cancers. 2020;12:1206. doi: 10.3390/cancers12051206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kiss R.C., Xia F., Acklin S. Targeting DNA Damage Response and Repair to Enhance Therapeutic Index in Cisplatin-Based Cancer Treatment. Int. J. Mol. Sci. 2021;22:8199. doi: 10.3390/ijms22158199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Lee T.-H., Kang T.-H. DNA Oxidation and Excision Repair Pathways. Int. J. Mol. Sci. 2019;20:6092. doi: 10.3390/ijms20236092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Hu Y., Scully R., Sobhian B., Xie A., Shestakova E., Livingston D.M. RAP80-directed tuning of BRCA1 homologous recombination function at ionizing radiation-induced nuclear foci. Genes Dev. 2011;25:685–700. doi: 10.1101/gad.2011011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Guilliam T.A., Doherty A.J. PrimPol—Prime Time to Reprime. Genes. 2017;8:20. doi: 10.3390/genes8010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.González-Acosta D., Blanco-Romero E., Ubieto-Capella P., Mutreja K., Míguez S., Llanos S., García F., Muñoz J., Blanco L., Lopes M., et al. PrimPol-mediated repriming facilitates replication traverse of DNA interstrand crosslinks. EMBO J. 2021;40:e106355. doi: 10.15252/embj.2020106355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Crow Y.J., Casanova J.L. STING-associated vasculopathy with onset in infancy—A new interferonopathy. N. Engl. J. Med. 2014;371:568–571. doi: 10.1056/NEJMe1407246. [DOI] [PubMed] [Google Scholar]
- 160.Konno H., Konno K., Barber G.N. Cyclic dinucleotides trigger ULK1 (ATG1) phosphorylation of STING to prevent sustained innate immune signaling. Cell. 2013;155:688–698. doi: 10.1016/j.cell.2013.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Blaauboer A., Sideras K., van Eijck C.H.J., Hofland L.J. Type I Interferons in Pancreatic Cancer and Development of New Therapeutic Approaches. Crit. Rev. Oncol./Hematol. 2021;159:103204. doi: 10.1016/j.critrevonc.2020.103204. [DOI] [PubMed] [Google Scholar]
- 162.Tang Q., Su Z., Gu W., Rustgi A.K. Mutant p53 on the Path to Metastasis. Trends Cancer. 2020;6:62–73. doi: 10.1016/j.trecan.2019.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Soragni A., Janzen D.M., Johnson L.M., Lindgren A.G., Thai-Quynh Nguyen A., Tiourin E., Soriaga A.B., Lu J., Jiang L., Faull K.F., et al. A Designed Inhibitor of P53 Aggregation Rescues P53 Tumor Suppression in Ovarian Carcinomas. Cancer Cell. 2016;29:90–103. doi: 10.1016/j.ccell.2015.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Chiang Y.-T., Chien Y.-C., Lin Y.-H., Wu H.-H., Lee D.-F., Yu Y.-L. The Function of the Mutant P53-R175H in Cancer. Cancers. 2021;13:4088. doi: 10.3390/cancers13164088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Doubeni C.A., Doubeni A.R.B., Myers A.E. Diagnosis and Management of Ovarian Cancer. Am. Fam. Physician. 2016;93:937–944. [PubMed] [Google Scholar]
- 166.Ortiz-Muñoz B., Aznar-Oroval E., García A.G., Peris A.C., Ballestero P.P., Yepes M.S., Lozano T.G., Ballester C.I., Garcia E.G. HE4, Ca125 and ROMA Algorithm for Differential Diagnosis between Benign Gynaecological Diseases and Ovarian Cancer. Tumor Biol. 2014;35:7249–7258. doi: 10.1007/s13277-014-1945-6. [DOI] [PubMed] [Google Scholar]
- 167.Poondla N., Chandrasekaran A.P., Kim K.-S., Ramakrishna S. Deubiquitinating Enzymes as Cancer Biomarkers: New Therapeutic Opportunities? BMB Rep. 2019;52:181–189. doi: 10.5483/BMBRep.2019.52.3.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Rowinsky E.K., Paner A., Berdeja J.G., Paba-Prada C., Venugopal P., Porkka K., Gullbo J., Linder S., Loskog A., Richardson P.G., et al. Phase 1 study of the protein deubiquitinase inhibitor VLX1570 in patients with relapsed and/or refractory multiple myeloma. Investig. New Drugs. 2020;38:1448–1453. doi: 10.1007/s10637-020-00915-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Chan W.C., Liu X., Magin R.S., Girardi N.M., Ficarro S.B., Hu W., Tarazona Guzman M.I., Starnbach C.A., Felix A., Adelmant G., et al. Accelerating Inhibitor Discovery for Deubiquitinating Enzymes. Nat. Commun. 2023;14:686. doi: 10.1038/s41467-023-36246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Henning N.J., Boike L., Spradlin J.N., Ward C.C., Liu G., Zhang E., Belcher B.P., Brittain S.M., Hesse M.J., Dovala D., et al. Deubiquitinase-Targeting Chimeras for Targeted Protein Stabilization. Nat. Chem. Biol. 2022;18:412–421. doi: 10.1038/s41589-022-00971-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Li X., Song Y. Proteolysis-Targeting Chimera (PROTAC) for Targeted Protein Degradation and Cancer Therapy. J. Hematol. Oncol. 2020;13:50. doi: 10.1186/s13045-020-00885-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Qi S.-M., Dong J., Xu Z.-Y., Cheng X.-D., Zhang W.-D., Qin J.-J. PROTAC: An Effective Targeted Protein Degradation Strategy for Cancer Therapy. Front. Pharmacol. 2021;12:692574. doi: 10.3389/fphar.2021.692574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Corno C., D’Arcy P., Bagnoli M., Paolini B., Costantino M., Carenini N., Corna E., Alberti P., Mezzanzanica D., Colombo D., et al. The Deubiquitinase USP8 Regulates Ovarian Cancer Cell Response to Cisplatin by Suppressing Apoptosis. Front. Cell Dev. Biol. 2022;10:1–17. doi: 10.3389/fcell.2022.1055067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Kang H., Choi M.C., Kim S., Jeong J.-Y., Kwon A.-Y., Kim T.-H., Kim G., Joo W.D., Park H., Lee C., et al. USP19 and RPL23 as Candidate Prognostic Markers for Advanced-Stage High-Grade Serous Ovarian Carcinoma. Cancers. 2021;13:3976. doi: 10.3390/cancers13163976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Park H.-B., Hwang S., Baek K.-H. USP7 Regulates the ERK1/2 Signaling Pathway through Deubiquitinating Raf-1 in Lung Adenocarcinoma. Cell Death Dis. 2022;13:698. doi: 10.1038/s41419-022-05136-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.García-Santisteban I., Peters G.J., Giovannetti E., Rodríguez J.A. USP1 Deubiquitinase: Cellular Functions, Regulatory Mechanisms and Emerging Potential as Target in Cancer Therapy. Mol. Cancer. 2013;12:91. doi: 10.1186/1476-4598-12-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created in this study. Data sharing is not applicable to this article.