Abstract
Importance: Some autistic adults experience depression and anxiety related to their social relationships. There is a need for evidence-based occupational therapy interventions that decrease depression and anxiety and improve the health of social relationships for autistic adults.
Objective: To determine the feasibility and preliminary effectiveness of the Healthy Relationships on the Autism Spectrum (HEARTS) intervention, a six-session, group-based psychoeducational intervention for the improvement of relationship health.
Design: One-group pretest–posttest design with a 3-mo follow-up after baseline.
Setting: United States; online intervention through community organization.
Participants: Fifty-five adults, ages 20 to 43 yr, with a professional or self-diagnosis of autism and the capacity to independently participate in an online, group-based, participatory class.
Intervention: Participants received 6 90-min weekly sessions that addressed healthy relationship topics, including recognizing abuse, meeting people, maintaining relationships, setting interpersonal boundaries, neurohealth for relationships, and ending relationships. A psychoeducational approach that provided education and involved guided discovery and strategy acquisition was used.
Outcomes and Measures: All measures were self-administered through an online survey. Depression and anxiety were assessed using instruments from the Patient-Reported Outcomes Measurement Information System.
Results: Fifty-five participants completed the intervention. Postintervention scores revealed statistically significant improvements in depression and anxiety.
Conclusions and Relevance: HEARTS is a promising intervention for improving depression and anxiety among autistic adults and should be investigated further.
What This Article Adds: HEARTS offers a potentially effective, nonpharmacological, psychoeducational group-based intervention option to promote healthy relationships for autistic adults.
Positionality Statement: This article uses identity-first language (autistic person) in accordance with the preference of autistic self-advocates (Autistic Self Advocacy Network, 2020; Kenny et al., 2016; Lord et al., 2022).
Healthy Relationships on the Autism Spectrum (HEARTS) offers a potentially effective, nonpharmacological, psychoeducational group-based intervention option to promote healthy relationships for autistic adults.
Autism is a developmental difference, often characterized as a disability, that affects how people experience the world around them (Autistic Self Advocacy Network, 2022). Many autistic people experience atypical social cognition and social perception, executive function differences, and atypical sensory and other information processing, and some may have repetitive behaviors or a small set of intense interests (Centers for Disease Control and Prevention, 2018; Harrington & Allen, 2014; Lai et al., 2014; Lord et al., 2022). There is a diversity of preferences among autistic people about terminology, but in this article, we use identity-first language (i.e., “autistic person”) rather than person-first language (i.e., “person with autism), in accordance with the preference of autistic self-advocates (Autistic Self Advocacy Network, 2020; Kenny et al., 2016; Lord et al., 2022). There are approximately 78 million autistic people worldwide (Lord et al., 2022), and it is estimated that one in 45 U.S. children are autistic (Centers for Disease Control and Prevention, 2020). The identification of autistic people is expanding, and estimates suggest that more than 70,000 autistic adolescents enter adulthood every year (Shattuck et al., 2012).
Autistic people are substantially more likely than nonautistic people to experience depression and anxiety. The results of a recent meta-analysis suggest that autistic people are 4 times more likely to experience depression in their lifetime than nonautistic people (Hudson et al., 2019). A recent comparison study of autistic and nonautistic adults found that autistic adults were more than twice as likely to be living with an anxiety disorder (relative risk of 2.62) and that autistic adults without intellectual disability (ID) were at increased risk for anxiety compared with autistic adults with ID (Nimmo-Smith et al., 2020).
Among nonautistic youths, research has identified risk factors for depression and anxiety in both individual domains (e.g., genetics, neurobiological stress response) and contextual domains (e.g., parenting, stressful life events, social relationships; Klein et al., 2013). For autistic people, depression and anxiety can be affected by social factors such as loneliness and peer rejection. Social skills interventions have been found to reduce depression for autistic adolescents (Schiltz et al., 2018). Autistic people are at acute risk of experiencing social disconnectedness, even compared with people with other types of disabilities. For example, autistic people, compared with people with other disabilities, are significantly more likely to never see friends, never get called by friends, never be invited to activities, and be socially isolated (Orsmond et al., 2013). Many autistic people have had negative social experiences, such as being bullied, rejected, or excluded, which makes them reluctant to initiate social interactions, increases their fear of rejection, and causes negative automatic thoughts about their own social abilities or others’ intentions toward them, contributing to greater social withdrawal (Adams et al., 2017; Humphrey & Symes, 2011; Schiltz et al., 2018; Smith & White, 2020). Social isolation and loneliness are linked with anxiety and the development of depressive symptoms among autistic people (Gotham et al., 2014; Han et al., 2019; Umagami et al., 2022).
There is an urgent need to develop public health and occupational therapy strategies to reduce depression, anxiety, and social disconnectedness for autistic people. Being friendless, having low-quality or short-lived friendships, and lacking social support predict academic, behavioral, and social–emotional problems (Rose & Asher, 2000) and reduced quality of life (Lord et al., 2022) and have been associated with depression and suicidality among autistic people (Hedley et al., 2017; Hedley, Uljarević, Foley, et al., 2018; Hedley, Uljarević, Wilmot, et al., 2018). Moreover, depression, anxiety, and social disconnectedness are negatively associated with activities of daily living and instrumental activities of daily living (Brenes et al., 2005; Kivelä & Pahkala, 2001; Na & Streim, 2017; Ormel et al., 2002; Penninx et al., 1999; Tomioka et al., 2018). Because depression and anxiety may contribute to social disconnectedness (Santini et al., 2020) by causing people to withdraw or pull away from friends, intimate partners, family, and community, interventions that reduce depression and anxiety for autistic people may also improve their social well-being.
In 2020, our research team conducted formative research with 25 autistic people and 7 autism service providers to create a new six-session, online, group-based psychoeducational intervention for autistic adults designed to improve their social connectedness (Rothman & Graham Holmes, 2021). The intervention, Healthy Relationships on the Autism Spectrum (HEARTS), was subsequently feasibility tested through a study using a one-group pretest–posttest design. HEARTS is a psychoeducational intervention that draws from psychoeducation and peer support approaches (Dennis, 2003) and is delivered through facilitated discussions about didactic content, role-playing with feedback, and peer modeling. The HEARTS intervention is unique in that it was codesigned by a collaborative group of nonautistic researchers and autistic advisors, and it was codelivered by teams of nonautistic and autistic interventionists when it was feasibility tested. Drawing on the strengths of grassroots peer-helping movements such as the domestic violence and sexual assault movements, where it has been demonstrated that peers can help peers, the HEARTS intervention was designed to be delivered by laypeople or by social workers, occupational therapists, or anyone with basic training in group intervention skills (Lawson & Anselmo, 1981; Shaw, 1979). The co-interventionists, who included Laura Graham Holmes and Emily F. Rothman, negotiated the roles that each would play in delivering the intervention during weekly debriefing and planning meetings. For some classes, the autistic interventionist chose to deliver the content and lead the discussion, whereas for others, they preferred to monitor and read text from the lively chat discussions and contribute their perspective or experiences relevant to the class content.
HEARTS uses a neurodiversity framework rather than a deficit model and, therefore, does not view the way that an autistic person communicates or socializes as inherently in need of remediation. Instead, the philosophical underpinning is that differences in social communication, executive function, and sensory processing can and should be accepted without judgment and that support can and should be provided for each person to set and strive for their own personal goals related to healthier relationships. To give a concrete example, rather than teaching participants that they should make eye contact with other people or that they should rehearse small talk to start conversations (i.e., things that nonautistic people tend to value), HEARTS encourages participants to identify how they prefer to communicate with others and how they can express their needs, boundaries, and desires to someone whom they are getting to know in a manner consistent with the relationship continuing in a way that is pleasurable for both people.
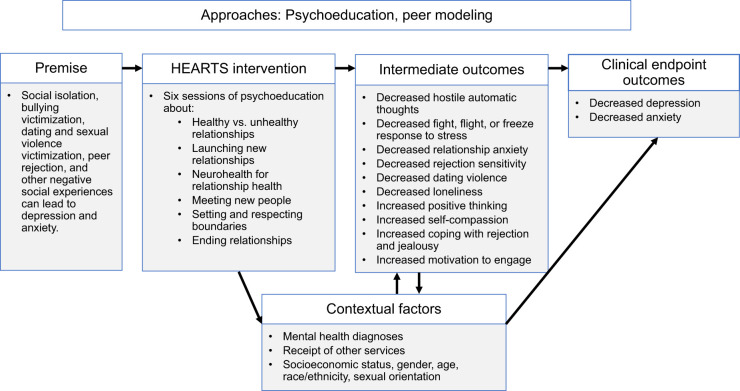
The HEARTS intervention addressed theoretical mechanisms at multiple levels—cognitive (e.g., hostile automatic thoughts, rejection sensitivity, positive thinking), behavioral (e.g., involvement in abusive dating relationships, improving self-care), and emotional (e.g., coping with rejection and jealousy, self-compassion, motivation to engage with others for socializing)—to target anxiety and depression as clinical endpoints (Rothman, Graham Holmes, et al., 2022). This intervention aims to improve correlates of social well-being to decrease depression and anxiety, the clinical endpoints (see Figure 1). Initial feasibility test results, published previously (Rothman, Graham Holmes, et al., 2022), revealed that HEARTS participants experienced increases in coping skills, social motivation, and flourishing and decreases in hostile automatic thoughts, dating abuse, emotional dysregulation, and rejection sensitivity from baseline to 3 mo postbaseline. The present study examined the preliminary effectiveness of HEARTS in improving depression and anxiety. We hypothesized that notable improvements would be found in depression and anxiety at the 3-mo follow-up.
Figure 1.
HEARTS conceptual model diagram.
Note. HEARTS = Healthy Relationships on the Autism Spectrum.
Method
Research Design
This intervention study used a one-group pretest– posttest design with a 3-mo postbaseline follow-up.
Participants
To be eligible for research, participants had to (1) be adults (ages 18–44 yr), (2) be able to communicate in English, (3) state that they had one or more relationships (e.g., with a friend, romantic partner, coworker, or family member) that they wanted to improve, (4) have access to a computer with the Zoom platform and a private space where they could participate in class, (5) state that they were autistic (either formally or self- diagnosed), and (6) be responsive to interviewer questions. A rating scale was created for the purpose of assessing participants’ responsiveness to interviewer questions; for details, see Rothman, Graham Holmes, et al. (2022).
Procedures
All procedures were reviewed and approved by the Boston University Institutional Review Board. Participants were recruited through advertisements sent to them from the Asperger/Autism Network, the autism self-advocacy organization, and through social media. Potentially interested participants emailed the study team. The team emailed a research consent form back and scheduled a brief Zoom meeting with each potential participant to explain what the HEARTS intervention would be like and to invite them to consider participating in research. Those who consented to participate in research were then emailed a link to the baseline assessment, which was a self-report survey. The survey also included measures related to flourishing and positive thinking, interpersonal competence, dating abuse, hostile automatic thoughts, coping with rejection and jealousy, rejection sensitivity, motivation for social engagement, and loneliness. For results from the full baseline surveys, see Rothman, Graham Holmes, et al. (2022). Study participants received up to $200, including $40 for completing the baseline survey, $40 for completing the postintervention survey, and $20 for each class that they attended.
Of 84 people who were screened for eligibility, 90% (n = 76) were eligible for research. Of those who were not eligible, 4 did not qualify on the basis of responsiveness to interviewer questions, 2 were older than 44 yr of age, and 2 were repeat students who had already participated in the study. Of the 76 eligible people, 95% (n = 72) consented to participate in the research. Interested people who chose not to participate in the research study were still able to attend the class. Reasons for discontinuing the class included schedule changes at work and being unable to attend sessions, hospital stays, and emotional burnout. One person who consented did not complete the baseline survey in time to be included in the research study, 4 attended most sessions but did not complete the postintervention survey, and 2 completed both the baseline and postintervention surveys but attended too few sessions (less than four) to be included in data analyses.
The HEARTS intervention was delivered by teaching pairs of two. Each teaching team included one autistic person and one nonautistic person. In total, three autistic people and two nonautistic people delivered the HEARTS sessions during the pilot phase. The median HEARTS session size was 20 people (range = 16–23 participants). HEARTS classes began within 2 wk of study enrollment. All classes took place online via Zoom. The content of all classes was documented using a fidelity tracking form that was completed at the end of each class by the nonautistic interventionist. Fidelity was further verified during a weekly debriefing and planning meeting between the autistic and nonautistic co-interventionists.
Participants completed the pretest survey before attending the first class. Each week, they were emailed a survey with depression and anxiety measures (discussed in the “Instruments” section) and open-ended questions about their use of skills that week. Finally, participants were emailed a link to the postintervention survey 6 wk after the final HEARTS class (i.e., 12 wk after baseline).
Intervention
The participants attended 6 90-min weekly classes. HEARTS is a manualized intervention and consists of six class sessions, with each session comprising three to four activities. (Table A.1 in the Supplemental Appendix, available online with this article at https://research.aota.org/ajot, provides a description of HEARTS class sessions.) Formative research for the content of HEARTS was conducted by interviewing 25 autistic people about what they would want to learn in a healthy relationships class (Rothman & Graham Holmes, 2021). Participants attended class from a private space in their home, without other people present. Accessibility was emphasized. For example, attendees were told that it was acceptable to participate with cameras on or off and verbally or exclusively using the type-to-chat function and that they could use assistive communication devices if desired. At the outset of the first class, all participants introduced themselves and talked briefly about relationships that they were planning to work on over the course of the intervention. Instructions for this activity were sent by email before the first class so that people could think about what they wanted to say ahead of time. At the beginning of each class session, participants discussed whether they had completed the previous week’s homework practice and what they had learned. Next, facilitators presented information in interactive presentations or activities (e.g., card sorting, role play). Finally, two or more optional homework practice assignments were offered for the week addressing skills discussed in class. Examples of homework practice assignments included using what was learned about healthy and unhealthy relationships to analyze a relationship that participants observed in media (e.g., in a television or book; Class 1, Defining Healthy Relationships) and to use the Healthy Goals worksheet to improve how they took care of themselves (e.g., sleep, physical activity, other healthy habits) for a week and reflect on whether they noticed a difference (Class 3, Neurohealth for Relationships). To assess whether participants were engaged in the lessons and give them an opportunity to engage with content privately or by typing rather than verbally asking questions, the interventionists conducted weekly online surveys that were completed at the participants’ convenience. Participants responded to questions about their week (e.g., whether they felt that they were coping with feelings in a healthy way, whether they did something to improve one of their relationships) and whether they had any thoughts about class or any questions or topics they wanted to bring up in class.
Instruments
PROMIS Depression–Short Form 4a, Version 1.0
The Patient-Reported Outcomes Measurement Information System (PROMIS) Depression measure (Pilkonis et al., 2011, 2014) assesses symptoms of depression in adults and has been previously validated for use with autistic adults (Graham Holmes et al., 2020). The short-form scale consists of four items rated on a 5-point Likert-style scale for frequency of symptom occurrence, ranging from never (1) to always (5). Raw scores were converted to a t score with a mean of 50 (SD = 10). A higher score represents more of the construct measured; that is, a higher frequency of depressive symptoms. The scale has good internal consistency for autistic adults (α = .95; Graham Holmes et al., 2020). A minimal important change (MIC) criteria means how much scores need a within-patient change over time for patients to consider an intervention meaningful. A review of the literature provided a MIC range of 1.5 to 3.7 points on the PROMIS Depression t score scale (Terwee et al., 2021).
PROMIS Anxiety–Short Form 4a, Version 1.0
The PROMIS Anxiety measure (Pilkonis et al., 2011) assesses symptoms of anxiety in adults and has previously been validated for use with autistic adults (Graham Holmes et al., 2020). The short-form scale consists of four items rated on a 5-point Likert-style scale for frequency of symptom occurrence, ranging from never (1) to always (5). Raw scores are converted to a t score with mean of 50 (SD = 10). A higher score represents more of the construct measured, that is, a higher frequency of anxiety symptoms. The scale has good internal consistency for autistic adults (α = .94; Graham Holmes et al., 2020). A review of the literature provided a MIC range of 2.3 to 3.5 points on the PROMIS Anxiety t-score scale (Terwee et al., 2021).
Hostile Automatic Thoughts Scale
The Hostile Automatic Thoughts Scale (Snyder et al., 1997) instructs respondents to consider how often they had various thoughts in the past week about other people. Sample items include “I hate this person so much I could kill them” and “I’ll show this person!” The original scale was modified for this study by eliminating four items and expanding response options from two to five categories. For this study, response options were on a 5-point Likert-type scale ranging from 1 (not at all) to 5 (all the time) and were summed for analysis. A high score represents a person with frequent hostile automatic thoughts. Cronbach’s α in this sample was .95.
Measures of Adolescent Relationship Harassment and Abuse
The Measures of Adolescent Relationship Harassment and Abuse (Rothman, Cuevas, et al., 2022) were completed only by people who had a casual sexual encounter, intimate relationship, or romantic relationship in the past year. Respondents answered seven dating abuse victimization questions and seven dating abuse perpetration questions. Sample items included “I slapped, pushed, shoved or shook them” and “They hit, punched, kicked or choked me.” Response options were “yes,” “no,” and “prefer not to answer.” A total scale score was calculated by summing across items. Higher scores represented more dating abuse. The number of items endorsed by participants ranged from 0 to 5, with a median of 1.
Coping With Rejection and Jealousy
This measure was an original, 16-item instrument. Sample items included “I am so afraid of rejection that I don’t try to meet new people” and “I’ve been bullied in the past, so I get anxious about making friends.” Response options were on a 5-point Likert scale ranging from totally disagree (1) to totally agree (5). All responses were summed for a total score. Higher scores indicated better coping with rejection and jealousy. Cronbach’s α in this sample was .56.
Motivation to Engage With Others
This was an original 16-item instrument that measured motivation to socialize in the past month. Respondents were asked how motivated they felt in response to 16 items on a scale ranging from 1 (not at all motivated) to 5 (very motivated). Sample items included “send a text message or email to a friend” and “talk to someone that I don’t already know.” Responses were summed, with a higher score indicating more motivation to engage with others. Cronbach’s α in this sample was .92. Participants could elect to skip questions that did not apply to them (e.g., “ask a co-worker to get together outside of work”), and if they skipped more than two questions, their score was not summed.
Positive Thinking Scale
The Positive Thinking Scale (Diener et al., 2010) is a 22-item self-report instrument. A sample item is “I am optimistic about my future.” Two modifications were made to the original version: The word salient was changed to memorable, and the word shortcomings was changed to faults. Response options were “yes” and “no.” A scale score was derived by assigning a value of 1 to each response of “yes” and summing across all items. Higher scores represent more positive thinking. Cronbach’s α in this sample was .42.
Predominant Response Questionnaire
We used a modified version of the 20-item Predominant Response Questionnaire (Jones et al., n.d.) to measure how people respond to stressful situations. Respondents were asked to reflect on any fight- or-flight moments they had in the past week and rate whether the items were true for them. Items from this questionnaire began with the stem “This week, something(s) happened and.” Sample items included “my heart rate increased,” “I acted without thinking rationally (lashing out),” “I mis-read events because I expected the worst,” and “I felt frozen or stuck (in terms of decisions).” Response options were “yes” or “no.” A scale score was created by assigning a value of 1 to each response of “yes” and summing across items. Higher score indicates greater likelihood of having a fight, flight, or freeze response. Cronbach’s α in this sample was .88.
Rejection Sensitivity
This 10-item instrument was inspired by an existing instrument but rewritten to reflect contemporary modes of socializing (Downey & Feldman, 1996). Respondents consider scenarios in which people might find themselves and imagine whether they would be worried that they had done something wrong and whether they would expect the other person in the scenario to want to stop socializing with them. Worry is scored on a 6-point Likert scale; expectation that the other person will stop talking to them is also scored on a 6-point Likert scale. For example, respondents are asked to imagine the following: “I ask a friend to get together and hang out, but they say that they are too busy.” They then rate how worried they are that it is their fault on a scale ranging from 1 (not at all worried) to 6 (very concerned). Respondents are then asked to rate how likely they would be to expect that the friend does not like them anymore on a scale ranging from 1 (very unlikely) to 6 (very likely). Responses were summed, with higher scores representing more rejection sensitivity. Cronbach’s α in this sample was .96. The mean score on the scale was used for analytic purposes.
State Self-Compassion Scale
On the six-item State Self-Compassion Scale (Neff et al., 2021), response options were modified to be “yes,” “sort of,” and “no.” A sample item is “I feel intolerant and impatient toward myself.” Responses were summed, with higher scores representing more self-compassion. Cronbach’s α in this sample was .50. The total scale score was used for analytic purposes.
The UCLA Loneliness Scale
The 20-item UCLA Loneliness Scale (Russell, 1996) asks respondents to rate how often a series of statements is descriptive of them, such as “How often do you feel alone?” Response options are on a 4-point Likert scale ranging from 1 (never) to 4 (often). Responses were summed, with higher scores representing more loneliness. Cronbach’s α in this sample was .34.
Statistical Analysis
We analyzed baseline depression and anxiety scores for participants who completed four or more HEARTS sessions and the postintervention survey. We fit linear mixed-effect models for repeated measures over time with individual random effects to assess how depression and anxiety t scores changed throughout the 6-wk intervention. This kind of model takes into account the similarities within participants when measures are repeated over time (e.g., when different people have different baseline t scores). The model covariates are the week of the intervention, gender, whether the participant reported that they were diagnosed with depression, whether the participant reported that they were diagnosed with an anxiety disorder, and interaction terms for gender and diagnosis of depression or anxiety by week of the intervention. Finally, correlation analyses were run for outcomes (baseline depression and anxiety), measures of relationship and other skills or thought patterns that changed over the course of the intervention, and between change in outcomes and change in measures of relationship and thought patterns from baseline to postintervention survey.
Results
Study Population
The sample consisted of 55 participants, with an average age of 28 yr (range = 20–43 yr; Table 1 includes a summary of participant characteristics). More than half were cisgender female (55%), 31% were cisgender male, and 15% were nonbinary or another gender. Forty-one participants (76%) reported having been diagnosed with depression, and 45 (82%) reported having been diagnosed with an anxiety disorder. Approximately 25% of participants (n = 14) were self-diagnosed with autism, whereas 75% had a written report from a doctor or other health care professional indicating that they had a diagnosis of autism, Asperger’s, or pervasive developmental disorder–not otherwise specified.
Table 1.
Participant Demographics
| Demographic | n (%) |
| Gender | |
| Cisgender male | 17 (31) |
| Cisgender female | 30 (55) |
| Nonbinary | 6 (11) |
| Other | 2 (4) |
| Race | |
| Asian | 3 (6) |
| Black | 3 (6) |
| White | 44 (80) |
| Multiracial | 4 (7) |
| Unknown or other | 1 (2) |
| Ethnicity | |
| Hispanic | 4 (7) |
| Non-Hispanic | 51 (93) |
| Sexual orientation | |
| Heterosexual or straight | 29 (53) |
| Bisexual, gay, lesbian, or pansexual | 21 (38) |
| Asexual | 2 (4) |
| Other | 3 (6) |
| Ever been diagnosed with | |
| Autism, Asperger’s syndrome, or PDD–NOS | 41 (75) |
| Intellectual disability | 5 (9) |
| ADD or ADHD | 25 (46) |
| Depression | 41 (76) |
| Anxiety disorder, including OCD | 45 (82) |
| Substance use or alcohol use disorder | 4 (7) |
| Schizophrenia | 3 (6) |
| Bipolar disorder | 3 (6) |
| Eating disorder | 7 (13) |
| Oppositional defiant disorder or conduct disorder | 4 (7) |
| Posttraumatic stress disorder | 14 (26) |
| Currently has a spouse, dating, or intimate partner | 21 (38) |
| Currently resides with parents | 26 (47) |
| Ever received free or reduced-price meals at school | 13 (24) |
| Employed full-time | 19 (35) |
| Employed part-time | 14 (25) |
Note. N = 55. Mean age = 28 yr (SD = 7). ADD = attention deficit disorder; ADHD = attention deficit hyperactivity disorder; PDD–NOS = pervasive developmental disorder, not otherwise specified. OCD = obsessive–compulsive disorder.
Completion and Attrition Rates
In total, 98 people enrolled in the HEARTS intervention. Of these 98, 81 were screened for research eligibility, and 75 were eligible. Of these, 69 consented and 67 completed the baseline survey required to enroll in the study. Of the 67 who were enrolled in the study, 57 completed the postintervention survey. Of these, 55 had attended four or more HEARTS classes and are included in the data analysis.
Preliminary Effect on Depression and Anxiety
In terms of fidelity to the original curriculum plan, ≥90% fidelity was achieved for each class session. The findings were produced on the basis of data from the 55 participants who completed four or more sessions and the postintervention survey.
The mixed-effects model shows that, on average, depression t scores decreased by 1.39 points per wk, 95% confidence interval (CI) [−1.94, −0.84]; and anxiety t scores decreased by 0.99 per wk, 95% CI [−1.64, −0.34] (Tables 2 and 3). According to the fitted models with depression score as outcome, participants who were diagnosed with depression had depression t scores that were 8.24 points higher on average, 95% CI [−14.41, −2.07]), compared with those who were not diagnosed with depression. For both models, interactions between gender and week in the intervention were apparent. The models indicate that cisgender women may have benefited more from the intervention than cisgender men or people who identified as other genders (e.g., nonbinary, transmasculine).
Table 2.
Results of a Mixed-Effects Model for PROMIS Depression t Scores
| Variable | Coefficient | 95% CI | p |
|---|---|---|---|
| Intercept | 62.32 | [58.22, 66.42] | <.001*** |
| Week | −1.39 | [−1.94, −0.84] | <.001*** |
| Gender | |||
| Cisgender male | −1.34 | [−7.35, 4.67] | .661 |
| Nonbinary or other gender | −0.79 | [−8.71, 7.14] | .845 |
| Anxiety disorder diagnosis (no) | 0.62 | [−6.34, 7.58] | .862 |
| Depression diagnosis (no) | −8.24 | [−14.41, −2.07] | .009** |
| Week × Gender (cisgender male) | 1.05 | [0.24, 1.87] | .012* |
| Week × Gender (other) | 0.85 | [−0.24, 1.94] | .126 |
| Week × Anxiety (no) | −0.47 | [−1.42, 0.48] | .334 |
| Week × Depression (no) | 0.16 | [−0.70, 1.01] | .718 |
Note. R2 = 0.828. CI = confidence intervals; PROMIS = Patient-Reported Outcomes Measurement Information System.
p < .05.
p < .01.
p < .001.
Table 3.
Results of a Mixed-Effects Model for PROMIS Anxiety t Scores
| Variable | Coefficient | 95% CI | p |
|---|---|---|---|
| Intercept | 65.59 | [61.37, 69.82] | <.001*** |
| Week | −0.99 | [−1.64, −0.34] | .003** |
| Gender | |||
| Cisgender male | −1.78 | [−7.96, 4.41] | .572 |
| Nonbinary or other gender | −2.77 | [−10.93, 5.38] | .504 |
| Anxiety diagnosis (no) | −2.30 | [−9.45, 4.85] | .528 |
| Depression diagnosis (no) | −5.67 | [−12.02, 0.68] | .080 |
| Week × Gender: Cisgender male | 0.39 | [−0.57, 1.35] | .424 |
| Week × Gender: Other | 1.44 | [−0.15, 2.72] | .028* |
| Week × Anxiety Diagnosis: No | −0.12 | [−1.24, 0.99] | .830 |
| Week × Depression diagnosis: No | −0.20 | [−1.21, 0.80] | .690 |
Note. R2 = .830. CI = confidence intervals; PROMIS = Patient-Reported Outcomes Measurement Information System.
p < .05.
p < .01.
p < .001.
There were moderate correlations between relationship skills or thought patterns and anxiety and depression at baseline (Table A.2 in the Supplemental Appendix). Anxiety was significantly correlated with the tendency to have a fight, flight, or freeze response to a stressful incident (r = .224, p < .001), positive thinking (r = −.332, p = .018), and self-compassion (r = −.328, p = .020). Depression was significantly correlated with having a fight, flight, or freeze response to stressful incidents (r = .577, p < .001), coping with rejection and jealousy (r = −.343, p = .015), rejection sensitivity (r = .445, p = .001), positive thinking (r = −.456, p < .001), and loneliness (r = .458, p < .001). Decreased anxiety over the course of the intervention was significantly correlated with a decreased tendency to have a fight, flight, or freeze response to a stressful incident (r = .355, p = .011) and increased positive thinking (r = −.390, p = .005). Decreased depression over the course of the intervention was significantly correlated with increased positive thinking (r = −.401, p = .004) and decreased loneliness (r = .315, p = .026).
Discussion
In this study, we measured the preliminary effect of HEARTS on depression and anxiety in autistic adults. The results suggest that there was a low attrition rate and moderate improvements in depression and anxiety. Cisgender women appeared to have the strongest improvements in depression and anxiety over the course of the intervention. Improvements in other outcomes, including coping skills, social motivation, and rejection sensitivity, were also observed (Rothman, Graham Holmes, et al., 2022); therefore, investment in a larger scale, randomized controlled trial test of HEARTS is warranted.
Given the high rates of depression and anxiety among autistic people, and the high impacts of depression and anxiety on functioning, adult outcomes, and quality of life, it is critical that we offer evidence-based interventions to address depression and anxiety that are low cost and easily accessible. HEARTS was designed to be delivered by any person with training in group therapy and relationship skills interventions, such as clinical psychologists, social workers, and occupational therapists, as well as laypeople who receive training and supervision in psychoeducational group facilitation skills (Case-Smith & Arbesman, 2008; Weissman et al., 2006) to increase access for autistic adults. The rationale for developing an intervention that can be delivered by a wide range of interventionists is that there are too few licensed mental health providers in the United States (Substance Abuse and Mental Health Services Administration, 2020). Autistic adults, in particular, may have difficulty accessing mental health services, because many do not have an intellectual disability diagnosis that would qualify them for state-administered services (which may still be difficult to access even for those with ID), and outpatient providers may be reluctant to provide care for this clinically distinct population if they have not been trained to do so (Kerns et al., 2016). Approximately 34% of autistic adults report unmet mental health needs (Nicolaidis et al., 2013), and the lack of providers trained to provide services for autistic adults is a major contributor (Bruder et al., 2012). HEARTS is an intervention that may be effective if provided by a variety of professionals and laypeople to autistic adults online, which can help address the unmet need for more and better service availability to adults on the autism spectrum.
Our findings are consistent with other research showing that group-based interventions can have a positive effect on depression and anxiety for autistic people (Reaven et al., 2012; White et al., 2013). Although the majority of interventions for anxiety and depression in autism have used a cognitive–behavioral approach (S. W. White et al., 2018), interventions focused on building skills for employment or relationships have recently been found to have a positive effect on mental health. For example, group psychosocial interventions targeting social exclusion by building neurotypical social skills (e.g., the PEERS intervention) have been shown to reduce depression and suicidality among autistic teens (Schiltz et al., 2018) and social anxiety among autistic young adults (McVey et al., 2017); note, however, that teaching neurotypical social skills is not aligned with the HEARTS model. Because most depression and anxiety intervention studies for autism focus on children (Menezes et al., 2020; S. W. White et al., 2018), HEARTS has the potential to fill a critical service gap in addressing mental health for autistic adults.
Results of the primary outcomes for HEARTS were reported in a previous article, including findings related to hostile automatic thoughts; the tendency to have a fight, flight, or freeze response to stress; relationship anxiety and rejection sensitivity; coping with rejection and jealousy; dating violence; loneliness; and some positive outcomes such as positive thinking, self-compassion, and motivation to engage (Rothman, Graham Holmes, et al., 2022). We found that participants who reported a decreased tendency to have an intense reaction to stressors and increased positive thinking over the intervention period had a greater decrease in anxiety by the postintervention survey. People who reported increased positive thinking and decreased loneliness over the course of the intervention had greater decreases in depression by the postintervention survey. Although this pilot feasibility trial was not designed to test mechanisms of intervention effect or causal relationships between these variables, future evaluations of the HEARTS intervention should explore the hypothesis that positive thinking and loneliness may influence depression and anxiety, as well as the extent to which HEARTS can influence those clinical endpoints.
There are multiple group-based, psychoeducational, and skills-building occupational therapy interventions that have had positive effects on depression or anxiety (Kirsh et al., 2019). One of the strengths of the HEARTS intervention is that it can be easily disseminated to occupational therapy practitioners. Occupational therapists who are interested in delivering HEARTS can email the principal investigator (Emily F. Rothman) to request the HEARTS materials.
Limitations
This study provides preliminary evidence related to the feasibility and effectiveness of HEARTS on reducing depression and anxiety. It was a nonexperimental study, and as such, changes in depression and anxiety cannot be attributed to HEARTS. It is possible that other aspects of the experience played a role in the effects, such as participation in a social group, the opportunity to discuss personal challenges, or meeting people in similar situations. Indeed, interpersonal functioning and support is one factor that has been shown to predict the course of depression, and group therapy modalities have the potential to address those factors because of the interpersonal focus and psychosocial support provided in most group interventions (McDermut et al., 2001). In addition, we did not learn whether participants were receiving other therapies during the course of the study, and receiving other interventions or supports may moderate the effects of this intervention. It is also possible that external factors decreased all participants’ depression and anxiety unrelated to their participation in HEARTS. However, HEARTS was pilot tested during the coronavirus disease 2019 pandemic of 2020. Some autistic adults saw improvements in anxiety and stress in the beginning of the pandemic, but participants overall reported a loss of important supports and declines in mental health (Bundy et al., 2022; Pellicano et al., 2022), particularly those who had previous anxiety or depression diagnoses (Bal et al., 2021). It therefore seems unlikely that external factors would have improved depression and anxiety among the 55-person sample, but controlled studies are required to determine whether HEARTS is effective.
A second limitation is that because HEARTS was delivered online, it is unknown whether it would have the same effect had it been delivered in person, and it would be helpful in future research to compare these two delivery modalities. A third limitation is that the sample was small, and we were therefore unable to undertake stratified analyses to assess whether observed changes in depression and anxiety were enhanced in demographic subgroups such as women, men, or nonbinary people, or by age group. Furthermore, participants in this sample were primarily White; a more ethnically and racially diverse sample would benefit future evaluations of HEARTS. Larger studies are also needed to assess the generalizability of these findings to the broader autistic population; for example, people with varying levels of cognitive or communication ability.
Implications for Occupational Therapy Practice
The HEARTS intervention may have potential to facilitate benefits if larger studies using an experimental design confirm that it affects depression, anxiety, or other outcomes. If practitioners choose to implement HEARTS in clinical settings, they need to carefully document intervention content, client responses to the intervention, and changes in client functioning (or occupational engagement) from start to termination.
Conclusions
This study found preliminary support for the effectiveness of HEARTS on depression and anxiety. HEARTS is a novel six-session online intervention codesigned and cotaught with autistic people. HEARTS can serve to empower autistic people to have control over their relationships in a climate where autistic people (and disabled people, in general) are often made to feel powerless. Interventions that support a person’s ability to set and achieve their own goals contribute to well-being for autistic people (K. White et al., 2018). These results contribute to the evidence base of interventions on which occupational therapists, social workers, public health practitioners, psychologists, and others have to draw when considering how to support the development of healthy relationship skills for autistic adults.
Supplementary Material
Acknowledgments
We acknowledge the participants in the HEARTS intervention, Nancy Schwartz, and the staff of Asperger/Autism Network. The research reported in this publication was supported by Award K18MH12291 from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Adams, R., Bishop, S., & Taylor, J. L. (2017). Negative peer experiences in adolescents with autism spectrum disorders. In Fisher M. H. (Ed.), International review of research in developmental disabilities (Vol. 52, pp. 75–107). Academic Press. [Google Scholar]
- Autistic Self Advocacy Network. (2020). Identify-first language. https://autisticadvocacy.org/about-asan/identity-first-language/
- Autistic Self Advocacy Network. (2022). About autism. https://autisticadvocacy.org/about-asan/about-autism/
- Bal, V. H., Wilkinson, E., White, L. C., Law, J. K., The SPARK Consortium, Feliciano, P., & Chung, W. K. (2021). Early pandemic experiences of autistic adults: Predictors of psychological distress. Autism Research , 14, 1209–1219. 10.1002/aur.2480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenes, G. A., Guralnik, J. M., Williamson, J. D., Fried, L. P., Simpson, C., Simonsick, E. M., & Penninx, B. W. J. H. (2005). The influence of anxiety on the progression of disability. Journal of the American Geriatrics Society , 53, 34–39. 10.1111/j.1532-5415.2005.53007.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruder, M. B., Kerins, G., Mazzarella, C., Sims, J., & Stein, N. (2012). Brief report: The medical care of adults with autism spectrum disorders: Identifying the needs. Journal of Autism and Developmental Disorders , 42, 2498–2504. 10.1007/s10803-012-1496-x [DOI] [PubMed] [Google Scholar]
- Bundy, R., Mandy, W., Crane, L., Belcher, H., Bourne, L., Brede, J., . . . Cook, J. (2022). The impact of early stages of COVID-19 on the mental health of autistic adults in the United Kingdom: A longitudinal mixed-methods study. Autism , 26, 1765–1782. 10.1177/13623613211065543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case-Smith, J., & Arbesman, M. (2008). Evidence-based review of interventions for autism used in or of relevance to occupational therapy. American Journal of Occupational Therapy , 62, 416–429. 10.5014/ajot.62.4.416 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2018). Prevalence of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2014. MMWR: Morbidity and Mortality Weekly Report , 67(6), 1–23. https://www.cdc.gov/mmwr/volumes/67/ss/ss6706a1.htm?s_cid=ss6706a1_w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). Key findings: CDC releases first estimates of the number of adults living with autism spectrum disorder in the United States. https://www.cdc.gov/ncbddd/autism/features/adults-living-with-autism-spectrum-disorder.html
- Dennis, C.-L. (2003). Peer support within a health care context: A concept analysis. International Journal of Nursing Studies , 40, 321–332. 10.1016/S0020-7489(02)00092-5 [DOI] [PubMed] [Google Scholar]
- Diener, E., Wirtz, D., Tov, W., Kim-Prieto, C., Choi, D., Oishi, S., & Biswas-Diener, R. (2010). New well-being measures: Short scales to assess flourishing and positive and negative feelings. Social Indicators Research , 97, 143–156. 10.1007/s11205-009-9493-y [DOI] [Google Scholar]
- Downey, G., & Feldman, S. I. (1996). Implications of rejection sensitivity for intimate relationships. Journal of Personality and Social Psychology , 70, 1327–1343. 10.1037/0022-3514.70.6.1327 [DOI] [PubMed] [Google Scholar]
- Gotham, K., Bishop, S. L., Brunwasser, S., & Lord, C. (2014). Rumination and perceived impairment associated with depressive symptoms in a verbal adolescent-adult ASD sample. Autism Research , 7, 381–391. 10.1002/aur.1377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham Holmes, L., Zampella, C. J., Clements, C., McCleery, J. P., Maddox, B. B., Parish-Morris, J., . . . Miller, J. S. (2020). A lifespan approach to patient-reported outcomes and quality of life for people on the autism spectrum. Autism Research , 13, 970–987. 10.1002/aur.2275 [DOI] [PubMed] [Google Scholar]
- Han, G. T., Tomarken, A. J., & Gotham, K. O. (2019). Social and nonsocial reward moderate the relation between autism symptoms and loneliness in adults with ASD, depression, and controls. Autism Research , 12, 884–896. 10.1002/aur.2088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington, J. W., & Allen, K. (2014). The clinician’s guide to autism. Pediatrics in Review , 35, 62–78, quiz 78. 10.1542/pir.35.2.62 [DOI] [PubMed] [Google Scholar]
- Hedley, D., Uljarević, M., Foley, K.-R., Richdale, A., & Trollor, J. (2018). Risk and protective factors underlying depression and suicidal ideation in autism spectrum disorder. Depression and Anxiety , 35, 648–657. 10.1002/da.22759 [DOI] [PubMed] [Google Scholar]
- Hedley, D., Uljarević, M., Wilmot, M., Richdale, A., & Dissanayake, C. (2017). Brief report: Social support, depression and suicidal ideation in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders , 47, 3669–3677. 10.1007/s10803-017-3274-2 [DOI] [PubMed] [Google Scholar]
- Hedley, D., Uljarević, M., Wilmot, M., Richdale, A., & Dissanayake, C. (2018). Understanding depression and thoughts of self-harm in autism: A potential mechanism involving loneliness. Research in Autism Spectrum Disorders , 46, 1–7. 10.1016/j.rasd.2017.11.003 [DOI] [Google Scholar]
- Hudson, C. C., Hall, L., & Harkness, K. L. (2019). Prevalence of depressive disorders in individuals with autism spectrum disorder: A meta-analysis. Journal of Abnormal Child Psychology , 47, 165–175. 10.1007/s10802-018-0402-1 [DOI] [PubMed] [Google Scholar]
- Humphrey, N., & Symes, W. (2011). Peer interaction patterns among adolescents with autistic spectrum disorders (ASDs) in mainstream school settings. Autism , 15, 397–419. 10.1177/1362361310387804 [DOI] [PubMed] [Google Scholar]
- Jones, L., Field, T., Beeson, E., & Miller, R.. (n.d.). Predominant Response Questionnaire (PRQ) (Version 6). Neuroscience-Informed Cognitive–Behavior Therapy. https://www.n-cbt.com/uploads/7/8/1/8/7818585/predominantresponsequestionnaire_v6.pdf
- Kenny, L., Hattersley, C., Molins, B., Buckley, C., Povey, C., & Pellicano, E. (2016). Which terms should be used to describe autism? Perspectives from the UK autism community. Autism , 20, 442–462. 10.1177/1362361315588200 [DOI] [PubMed] [Google Scholar]
- Kerns, C. M., Roux, A. M., Connell, J. E., & Shattuck, P. T. (2016). Adapting cognitive behavioral techniques to address anxiety and depression in cognitively able emerging adults on the autism spectrum. Cognitive and Behavioral Practice , 23, 329–340. 10.1016/j.cbpra.2016.06.002 [DOI] [Google Scholar]
- Kirsh, B., Martin, L., Hultqvist, J., & Eklund, M. (2019). Occupational therapy interventions in mental health: A literature review in search of evidence. Occupational Therapy in Mental Health , 35, 109–156. 10.1080/0164212X.2019.1588832 [DOI] [Google Scholar]
- Kivelä, S.-L., & Pahkala, K. (2001). Depressive disorder as a predictor of physical disability in old age. Journal of the American Geriatrics Society , 49, 290–296. 10.1046/j.1532-5415.2001.4930290.x [DOI] [PubMed] [Google Scholar]
- Klein, D., Kujawa, A., Black, S., & Pennock, A. (2013). Depressive disorders. In Beauchaine T. P. & Hinshaw S. P. (Eds.), Child and adolescent psychopathology (2nd ed., pp. 543–575). Wiley. [Google Scholar]
- Lai, M.-C., Lombardo, M. V., & Baron-Cohen, S. (2014). Autism. Lancet , 383, 896–910. 10.1016/S0140-6736(13)61539-1 [DOI] [PubMed] [Google Scholar]
- Lawson, K., & Anselmo, E. (1981). Sexual assault intervention manual. Rape Information and Counseling Service. https://www.nlm.nih.gov/exhibition/confrontingviolence/assets/transcripts/OB12007_200_dpi.pdf
- Lord, C., Charman, T., Havdahl, A., Carbone, P., Anagnostou, E., Boyd, B., . . . McCauley, J. B. (2022). The Lancet Commission on the future of care and clinical research in autism. Lancet , 399, 271–334. 10.1016/S0140-6736(21)01541-5 [DOI] [PubMed] [Google Scholar]
- McDermut, W., Miller, I. W., & Brown, R. A. (2001). The efficacy of group psychotherapy for depression: A meta-analysis and review of the empirical research. Clinical Psychology: Science and Practice , 8, 98–116. 10.1093/clipsy.8.1.98 [DOI] [Google Scholar]
- McVey, A. J., Schiltz, H., Haendel, A., Dolan, B. K., Willar, K. S., Pleiss, S., . . . Van Hecke, A. V. (2017). Brief report: Does gender matter in intervention for ASD? Examining the impact of the PEERS® social skills intervention on social behavior among females with ASD. Journal of Autism and Developmental Disorders , 47, 2282–2289. 10.1007/s10803-017-3121-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menezes, M., Harkins, C., Robinson, M. F., & Mazurek, M. O. (2020). Treatment of depression in individuals with autism spectrum disorder: A systematic review. Research in Autism Spectrum Disorders , 78, 101639. 10.1016/j.rasd.2020.101639 [DOI] [Google Scholar]
- Na, L., & Streim, J. E. (2017). Psychosocial well-being associated with activity of daily living stages among community-swelling older adults. Gerontology and Geriatric Medicine , 3, 2333721417700011. 10.1177/2333721417700011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff, K. D., Tóth-Király, I., Knox, M. C., Kuchar, A., & Davidson, O. (2021). The development and validation of the State Self-Compassion Scale (Long- and Short Form). Mindfulness , 12, 121–140. 10.1007/s12671-020-01505-4 [DOI] [Google Scholar]
- Nicolaidis, C., Raymaker, D., McDonald, K., Dern, S., Boisclair, W. C., Ashkenazy, E., & Baggs, A. (2013). Comparison of healthcare experiences in autistic and non-autistic adults: A cross-sectional online survey facilitated by an academic-community partnership. Journal of General Internal Medicine , 28, 761–769. 10.1007/s11606-012-2262-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nimmo-Smith, V., Heuvelman, H., Dalman, C., Lundberg, M., Idring, S., Carpenter, P., . . . Rai, D. (2020). Anxiety disorders in adults with autism spectrum disorder: A population-based study. Journal of Autism and Developmental Disorders , 50, 308–318. 10.1007/s10803-019-04234-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormel, J., Rijsdijk, F. V., Sullivan, M., van Sonderen, E., & Kempen, G. I. J. M. (2002). Temporal and reciprocal relationship between IADL/ADL disability and depressive symptoms in late life. Journals of Gerontology: Series B , 57, 338–347. 10.1093/geronb/57.4.P338 [DOI] [PubMed] [Google Scholar]
- Orsmond, G. I., Shattuck, P. T., Cooper, B. P., Sterzing, P. R., & Anderson, K. A. (2013). Social participation among young adults with an autism spectrum disorder. Journal of Autism and Developmental Disorders , 43, 2710–2719. 10.1007/s10803-013-1833-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellicano, E., Brett, S., den Houting, J., Heyworth, M., Magiati, I., Steward, R., . . . Stears, M. (2022). COVID-19, social isolation and the mental health of autistic people and their families: A qualitative study. Autism , 26, 914–927. 10.1177/13623613211035936 [DOI] [PubMed] [Google Scholar]
- Penninx, B. W., Leveille, S., Ferrucci, L., van Eijk, J. T., & Guralnik, J. M. (1999). Exploring the effect of depression on physical disability: Longitudinal evidence from the established populations for epidemiologic studies of the elderly. American Journal of Public Health , 89, 1346–1352. 10.2105/AJPH.89.9.1346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilkonis, P. A., Choi, S. W., Reise, S. P., Stover, A. M., Riley, W. T., & Cella, D.; PROMIS Cooperative Group. (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, anxiety, and anger. Assessment , 18, 263–283. 10.1177/1073191111411667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilkonis, P. A., Yu, L., Dodds, N. E., Johnston, K. L., Maihoefer, C. C., & Lawrence, S. M. (2014). Validation of the depression item bank from the Patient-Reported Outcomes Measurement Information System (PROMIS) in a three-month observational study. Journal of Psychiatric Research , 56, 112–119. 10.1016/j.jpsychires.2014.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reaven, J., Blakeley-Smith, A., Leuthe, E., Moody, E., & Hepburn, S. (2012). Facing your fears in adolescence: Cognitive–behavioral therapy for high-functioning autism spectrum disorders and anxiety. Autism Research and Treatment , 2012, 423905. 10.1155/2012/423905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose, A. J., & Asher, S. (2000). Children’s friendships. In Hendrick C. E. & Hendrick S. S. (Eds.), Close relationships: A sourcebook (pp. 47–58). Sage. 10.4135/9781452220437.n4 [DOI] [Google Scholar]
- Rothman, E. F., Cuevas, C. A., Mumford, E. A., Bahrami, E., & Taylor, B. G. (2022). The psychometric properties of the Measure of Adolescent Relationship Harassment and Abuse (MARSHA) with a nationally representative sample of U.S. youth. Journal of Interpersonal Violence , 37, NP9712–NP9737. 10.1177/0886260520985480 [DOI] [PubMed] [Google Scholar]
- Rothman, E. F., & Graham Holmes, L. (2021). Using formative research to develop HEARTS: A curriculum-based healthy relationships promoting intervention for individuals on the autism spectrum. Autism , 26, 160–168. 10.1177/13623613211024521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman, E. F., Graham Holmes, L., Caplan, R., Chiang, M., Haberer, B., Gallop, N., . . . Wharmby, P. (2022). Healthy Relationships on the Autism Spectrum (HEARTS): A feasibility test of an online class co-designed and co-taught with autistic people. Autism , 26, 690–702. 10.1177/13623613211069421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell, D. W. (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment , 66, 20–40. 10.1207/s15327752jpa6601_2 [DOI] [PubMed] [Google Scholar]
- Santini, Z. I., Jose, P. E., York Cornwell, E., Koyanagi, A., Nielsen, L., Hinrichsen, C., . . . Koushede, V. (2020). Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health , 5, e62–e70. 10.1016/S2468-2667(19)30230-0 [DOI] [PubMed] [Google Scholar]
- Schiltz, H. K., McVey, A. J., Dolan, B. K., Willar, K. S., Pleiss, S., Karst, J. S., . . . Van Hecke, A. V. (2018). Changes in depressive symptoms among adolescents with ASD completing the PEERS® social skills intervention. Journal of Autism and Developmental Disorders , 48, 834–843. 10.1007/s10803-017-3396-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shattuck, P. T., Roux, A. M., Hudson, L. E., Taylor, J. L., Maenner, M. J., & Trani, J.-F. (2012). Services for adults with an autism spectrum disorder. Canadian Journal of Psychiatry , 57, 284–291. 10.1177/070674371205700503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw, L. (1979). Counseling the abuse victim. Pennsylvania Coalition Against Domestic Violence. https://www.nlm.nih.gov/exhibition/confrontingviolence/assets/transcripts/OB12009_200_dpi.pdf
- Smith, I. C., & White, S. W. (2020). Socio-emotional determinants of depressive symptoms in adolescents and adults with autism spectrum disorder: A systematic review. Autism , 24, 995–1010. 10.1177/1362361320908101 [DOI] [PubMed] [Google Scholar]
- Snyder, C. R., Crowson, J. J., Houston, B. K., Kurylo, M., & Poirier, J. (1997). Assessing hostile automatic thoughts: Development and validation of the HAT Scale. Cognitive Therapy and Research , 21, 477–492. 10.1023/A:1021988511695 [DOI] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2020). SAMHSA releases Behavioral Health Workforce Report. https://annapoliscoalition.org/samhsa-releases-behavioral-health- workforce-report/
- Terwee, C. B., Peipert, J. D., Chapman, R., Lai, J.-S., Terluin, B., Cella, D., . . . Mokkink, L. B. (2021). Minimal important change (MIC): A conceptual clarification and systematic review of MIC estimates of PROMIS measures. Quality of Life Research , 30, 2729–2754. 10.1007/s11136-021-02925-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomioka, K., Kurumatani, N., & Saeki, K. (2018). The differential effects of type and frequency of social participation on IADL declines of older people. PLoS One , 13, e0207426. 10.1371/journal.pone.0207426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umagami, K., Remington, A., Lloyd-Evans, B., Davies, J., & Crane, L. (2022). Loneliness in autistic adults: A systematic review. Autism , 26, 2117–2135. 10.1177/13623613221077721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman, M. M., Verdeli, H., Gameroff, M. J., Bledsoe, S. E., Betts, K., Mufson, L., . . . Wickramaratne, P. (2006). National survey of psychotherapy training in psychiatry, psychology, and social work. Archives of General Psychiatry , 63, 925–934. 10.1001/archpsyc.63.8.925 [DOI] [PubMed] [Google Scholar]
- White, K., Flanagan, T. D., & Nadig, A. (2018). Examining the relationship between self-determination and quality of life in young adults with autism spectrum disorder. Journal of Developmental and Physical Disabilities , 30, 735–754. 10.1007/s10882-018-9616-y [DOI] [Google Scholar]
- White, S. W., Ollendick, T., Albano, A. M., Oswald, D., Johnson, C., Southam-Gerow, M. A., . . . Scahill, L. (2013). Randomized controlled trial: Multimodal Anxiety and Social Skill Intervention for adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders , 43, 382–394. 10.1007/s10803-012-1577-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- White, S. W., Simmons, G. L., Gotham, K. O., Conner, C. M., Smith, I. C., Beck, K. B., & Mazefsky, C. A. (2018). Psychosocial treatments targeting anxiety and depression in adolescents and adults on the autism spectrum: Review of the latest research and recommended future directions. Current Psychiatry Reports , 20, 82. 10.1007/s11920-018-0949-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.