Abstract
Numerous studies have reported task shifting and task sharing due to various reasons and with varied scopes of health services, either task-shifted or -shared. However, very few studies have mapped the evidence on task shifting and task sharing. We conducted a scoping review to synthesize evidence on the rationale and scope of task shifting and task sharing in Africa. We identified peer-reviewed papers from PubMed, Scopus, and CINAHL bibliographic databases. Studies that met the eligibility criteria were charted to document data on the rationale for task shifting and task sharing, and the scope of tasks shifted or shared in Africa. The charted data were thematically analyzed. Sixty-one studies met the eligibility criteria, with fifty-three providing insights on the rationale and scope of task shifting and task sharing, and seven on the scope and one on rationale, respectively. The rationales for task shifting and task sharing were health worker shortages, to optimally utilize existing health workers, and to expand access to health services. The scope of health services shifted or shared in 23 countries were HIV/AIDS, tuberculosis, hypertension, diabetes, mental health, eyecare, maternal and child health, sexual and reproductive health, surgical care, medicines’ management, and emergency care. Task shifting and task sharing are widely implemented in Africa across various health services contexts towards ensuring access to health services.
Keywords: task shifting, task sharing, rationale, scope, health service delivery, optimal utilization of health workers, access to health services
1. Introduction
Task shifting and task sharing are being implemented in several countries to efficiently utilize existing health workers to improve the access of the population to quality health services. Access of populations to quality healthcare is essential in achieving Universal Health Coverage (UHC) and the health and health-related Sustainable Development Goals (SDG) [1,2,3]. Task shifting is defined by the World Health Organization (WHO) as “the rational redistribution of tasks among health workforce teams”, from trained and qualified health workers to other health workers with shorter training duration to maximize the available health workforce [2]. In task shifting, tasks are delegated or transferred, and in task sharing, tasks are delivered collaboratively by different staff categories [3]. This approach is implemented in many countries globally, including Africa, where there remains a persistent health workforce shortage and deficient access to healthcare [4,5].
Africa faces numerous health workforce challenges that are contributing to the health indices and systems’ performance of countries in the continent [6]. These challenges are also impacting negatively on the functionality and the resilience of the health system [7,8], and the attainment of key population outcomes [9]. These challenges, which are quite broad and have contextual specificities, include weak health and health workforce leadership, governance and stewardship mechanisms, and management systems, as well as poor regulation, and evidence generation and use mechanisms [6,10]. Furthermore, there is a persistent low stock of qualified and skilled health workers, inequitable distribution of existing ones, marked inequalities in education, employment, and population needs, and poor work environments at various levels of the health system [6,11].
The impact of the aforementioned challenges includes a high deficit in the health workforce in most countries in Africa. The Africa Regional average density of doctors, nurses, and midwives per 1000 population in 2018 was 1.55, which is lower than the SDG index threshold of 4.45 [4]. Coping with the persistent deficit which has been ever-present over the years informed the implementation of formally task shifting and task sharing, and informally in levels of service delivery and programs. Its implementation varies widely, with several countries currently implementing the approach and others planning to commence implementation. For those implementing, in the early stages of implementation or planning to commence implementation, evidence on circumstances that should inform its implementation and the scopes of tasks that could be task shifted or shared is pertinent.
Numerous studies have reported task shifting and task sharing due to various reasons and with varied scopes of health services, either task-shifted or -shared. However, very few studies have holistically mapped the evidence on task shifting and task sharing, with most focusing on specific programs [12,13,14,15]. It is worth reviewing the evidence of task shifting and task sharing for integrated health service delivery, focusing on the rationale and scope of tasks. Therefore, this scoping review aimed to synthesize evidence on the rationale and scope of task shifting and task sharing in Africa.
2. Materials and Methods
This scoping review was conducted using the enhanced Arksey and O’Malley’s framework for scoping reviews [16,17]. The review questions were: (1) What are the documented rationales for task shifting and task sharing? (2) What scope of tasks were shifted or shared to improve the access of the population to health services in Africa? To answer these questions, the Joanna Briggs Institute’s population, concept, and context (PCC) framework presented in Table 1 was adopted.
Table 1.
Population, concept, and context (PCC) framework for the scoping review.
| Criteria | Component(s) | Explanation |
|---|---|---|
| Population (P) | Population Health workforce |
Everyone accessing health services. Healthcare workers such as physicians, nurses, midwives, and community health workers that are working as frontline contact in the healthcare system. |
| Concept (C) | Rationale Scope |
Usual reasons or the logical explanations for task shifting and task sharing. Extent or range of services that are task-shifted or -shared amongst various categories of health workers. |
| Context (C) | Healthcare services African countries |
Healthcare services within essential service packages that are either sought or received by the population at any healthcare service delivery level in both public and private sectors. Any country within the African continent. |
We identified relevant studies by applying the search strategy in Table 2 to obtain peer-reviewed papers from the PubMed, Scopus, and CINAHL bibliographic databases. We considered quantitative, qualitative, and mixed-methods studies, as well as review and perspective papers on task shifting or sharing for integrated health service delivery. We also considered articles published from 2010 to 2021 to obtain a wide range of contemporary information.
Table 2.
Search strategy.
| Source of Literature | Task Shifting/Sharing Terms | Health System/Services Terms | Africa Terms |
|---|---|---|---|
| PubMed | “task shifting” [Title/Abstract] OR “task sharing” [Title/Abstract] AND (“Africa”) [Mesh] | “health system*” [tiab] OR “healthcare system*” [tiab] OR “health care system*” [tiab] OR “healthcare sector*” [tiab] OR “healthcare industr*” [tiab] OR “health industr*” [tiab] OR “health facilit*” [tiab] OR “hospital*” [tiab] OR “healthcare” [tiab] OR “health care” [tiab] OR “health service*” [tiab] OR “healthcare service*” [tiab] OR “health cent*” [tiab] OR “care, health” [tiab] OR “system, health care” [tiab] OR “systems, health care” [tiab] OR “system, healthcare” [tiab] | Africa*[tiab] OR Algeria*[tiab] OR Angola*[tiab] OR Benin*[tiab] OR Botswana*[tiab] OR Burkina Faso [tiab] OR Burundi*[tiab] OR Cape Verde*[tiab] OR Cabo Verde [tiab] OR Cameron*[tiab] OR Cameroon*[tiab] OR Chad*[tiab] OR Comoros*[tiab] OR Congo*[tiab] OR Cote d’Ivoire[tiab] OR Ivory coast [tiab] OR Djibouti*[tiab] OR Egypt*[tiab] OR Eritrea*[tiab] OR Ethiopia*[tiab] OR Gabon*[tiab] OR Gambia*[tiab] OR Ghana*[tiab] OR Guinea*[tiab] OR Kenya*[tiab] OR Lesotho*[tiab] OR Liberia*[tiab] OR Libya*[tiab] OR Madagascar*[tiab] OR Malawi*[tiab] OR Mali*[tiab] OR Maurit*[tiab] OR Morocc*[tiab] OR Mozambiqu*[tiab] OR Namibia*[tiab] OR Niger*[tiab] OR Rwanda*[tiab] OR Senegal*[tiab] OR Seychelles[tiab] OR Sierra Leone*[tiab] OR Somalia*[tiab] OR South Africa*[tiab] OR Sudan*[tiab] OR Swaziland*[tiab] OR Tanzania*[tiab] OR Togo*[tiab] OR Tunisia*[tiab] OR Uganda*[tiab] OR Zambia*[tiab] OR Zimbabwe*[tiab] |
| CINHAL | TI “task shifting” OR AB “task shifting” OR TI “task sharing” OR AB “task sharing” OR MH “task shifting” OR MH “task sharing” | TI” health system*” OR AB “health system*” OR TI” healthcare system*” OR AB” healthcare system*” OR TI” health care system*” OR AB” health care system*” OR TI” healthcare sector*” OR AB” healthcare sector*” OR TI” health facilit*” OR AB” health facilit*” OR TI “hospital*” OR AB “hospital*” OR TI” healthcare” OR AB” healthcare” OR TI “health care” OR AB “health care” OR TI” health service*” OR AB” health service*” OR TI” healthcare service*” OR AB” healthcare service*” OR TI” health cent*” OR AB” health cent*” OR TI” care, health” OR AB” care, health” OR TI “system, health care” OR AB “system, health care” OR TI “systems, health care” OR AB “systems, health care” OR TI “system, healthcare” OR TI “system, healthcare” | MH Africa OR TI Africa* OR AB Africa* OR TI Algeria* OR AB Algeria* OR TI Angola*OR AB Angola* OR TI Benin*OR AB Benin* OR TI Botswana* OR AB Botswana OR TI “Burkina Faso*” OR AB “Burkina Faso*” OR TI Burundi* OR AB Burundi* OR TI “Cape Verde*” OR AB “Cape Verde*” OR TI Cameron* OR AB Cameron*OR TI Cameroon*OR AB Cameroon* OR TI Chad* OR AB chad* OR TI Comoros* OR AB Comoros* OR TI Congo* OR AB Congo* OR TI “Cote d’Ivoire” OR AB “Cote d’Ivoire” OR TI “Ivory coast” OR AB “Ivory coast” OR TI Djibouti* OR AB Djibouti* OR TI Egypt* OR AB Egypt* OR TI Eritrea* OR AB Eritrea* OR TI Ethiopia* OR AB Ethiopia* OR TI Gabon* OR AB Gabon* OR TI Gambia*OR AB Gambia* OR TI Ghana* OR AB Ghana OR TI Guinea* OR AB Guinea* OR TI Kenya* OR AB Kenya* OR TI Lesotho* OR Lesotho* OR TI Liberia* OR AB Liberia OR TI Libya* AB Libya* OR TI Madagascar* OR AB Madagascar* OR TI Malawi* OR AB Malawi* OR TI Mali* OR AB Mali* OR TI Maurit* OR AB Maurit* OR TI Morocc* OR AB Morocc* OR TI Mozambiqu* OR AB Mozambiqu* OR TI Namibia* OR AB Namibia* OR TI Niger* OR AB Niger* OR TI Rwanda* OR AB Rwanda* OR TI Senegal* OR AB Senegal* OR TI Seychelles* OR TI Seychelles* OR TI “Sierra Leone*” OR AB “Sierra Leone*” OR TI Somalia* OR AB Somalia” OR TI South Africa* OR AB South Africa* OR TI Sudan* OR AB Sudan* OR TI Swaziland* OR AB Swaziland* OR TI Tanzania* OR AB Tanzania* OR TI Togo* OR AB Togo* OR TI Tunisia* OR AB Tunisia OR TI Uganda* OR AB Uganda* OR TI Zambia* OR TI Zambia* OR TI Zimbabwe* OR AB Zimbabwe* |
| Scopus | “task shifting” OR “task sharing” | “health system*” OR “healthcare system*” [tiab] OR “health care system*” OR “healthcare sector*” OR “healthcare industr*” OR “health industr*” OR “health facilit*” OR “hospital*” OR “healthcare” OR “health care” OR “health service*” OR “healthcare service*” OR “health cent*” OR “care, health” OR “system, health care” OR “systems, health care” OR “system, healthcare” |
TITLE-ABS-KEY (“Africa” OR “Algeria*” OR “Angola*” OR “Benin*” OR “Botswana*” OR “Burkina Faso” OR “Burundi*” OR “Cape Verde*” OR “Cabo Verde” OR “Cameron*” OR “Cameroon*” OR “Chad*” OR “Comoros*” OR “Congo*” OR “Cote d’Ivoire” OR “Ivory coast” OR “Djibou*” OR “Egypt*” OR “Eritrea*” OR “Ethiopia*” OR “Gabon*” OR “Gambia*” OR “Ghana*” OR “Guinea*” OR “Kenya*” OR “Lesotho*” OR “Liberia*” OR “Libya*” OR “Madagascar*” OR “Malawi*” OR “Mali*” OR “Maurit*” OR “Morocc*” OR “Mozambiqu*” OR “Namibia*” OR “Niger*” OR “Rwanda*” OR “Senegal*” OR “Seychelles” OR “Sierra Leone*” OR “Somalia*” OR “South Africa*” OR “Sudan*” OR “Swaziland*” OR “Tanzania*” OR “Togo*” OR “Tunisia*” OR “Uganda*” OR “Zambia*” OR “Zimbabwe*”) |
All articles obtained from the literature search, which was conducted independently by the authors, were downloaded into the Mendeley reference manager, with duplicates removed. The title and abstract were screened independently by the authors, with discrepancies discussed and a consensus reached. Afterwards, the full text was reviewed based on the eligibility criteria for inclusion. The inclusion criteria were: (1) quantitative, qualitative, and mixed-methods studies on task shifting or sharing for integrated health service delivery in Africa, (2) review and perspective papers on task shifting or sharing for integrated health service delivery in Africa, (3) full-text articles are written in the English language and are accessible, and (4) articles were published from 2010 to 2021. The exclusion criteria were: (1) papers written in other languages, (2) full texts were not accessible, and (3) papers were news articles, editorials, commentaries, and letters to the editor that did not involve primary data and did not provide insights into the rationale, scope, and health professions education for task shifting and task sharing in Africa.
The first author (S.C.O.) used a data extraction matrix to extract information on the author and year of publication, country name, study design, study setting, and population. Additionally extracted were the key findings on the rationale and scope of task shifting and task sharing, health service context, and the level of care. As had been carried out in other studies, we extracted text verbatim on themes, concepts, and categories relevant to the research questions [18,19] into the extraction matrix for analysis using the thematic analysis approach. The second author randomly reviewed the charting for 50% of the studies, with an agreement reached on the charting output.
We analyzed the characteristics of the papers based on the extracts using descriptive statistics. We analyzed the qualitative content of the papers using thematic analysis [20,21], with synthesized information described narratively based on information on the rationale and scope of task shifting and task sharing in Africa. We reported the findings using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines Extension for Scoping Review reporting standards (Table A1).
3. Results
3.1. Description of Studies
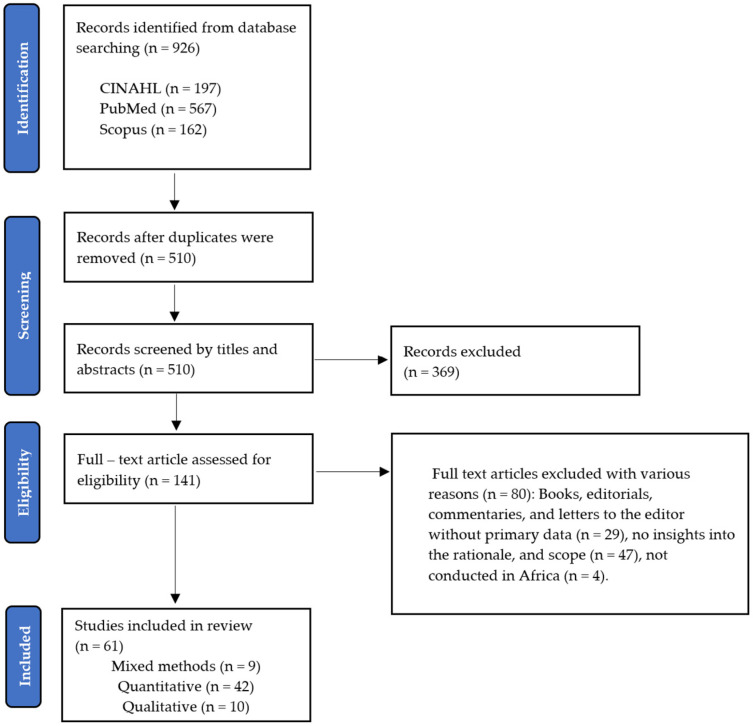
We identified 926 records from the databases CINAHL (n = 197), PubMed (n = 567), and Scopus (n = 162). After duplicates were removed, 510 records were screened by titles and abstracts, from which 141 articles’ full text were assessed for eligibility (Figure 1). Sixty-one original research papers were included in the final review, with nine (15%) mixed-methods studies, forty-two (69%) quantitative, and ten (16%) qualitative (Table 2). In all, 80 papers were excluded following the full-text review, with 29 being books, editorials, commentaries, and letters to the editor without primary data, 47 papers providing no insights on the rationale and scope of task shifting and task sharing, and 4 not being conducted in Africa.
Figure 1.
PRISMA-ScR flow diagram.
3.2. Characteristics of the Included Studies
The main characteristics of the included papers are presented in Table 3, with details in Table 4. The highest proportion of the papers was published in 2017 (18%), with the lowest proportion published in 2019 (3%). Of the included papers, 2 were multi-country, and 22 were conducted in different countries in Africa. Thirteen percent (n = 8) were conducted in Uganda, and ten percent (n = 6) were conducted in Ghana and Kenya. Of the reviewed papers, 87% (n = 53) provided insights on the rationale and scope of task shifting and task sharing, with 11% (n = 7) providing insights on scope only, and 2% (n = 1) on rationale only. Furthermore, 59% (n = 36) of the studies reported task shifting and task sharing practices at the community and primary level of care, with 3% (n = 2) of studies reporting practices at the tertiary level of care.
Table 3.
Main characteristics of the included papers.
| Paper Characteristics | Categories | Results | |
|---|---|---|---|
| n | % | ||
| Year of publication | 2010 | 4 | 7 |
| 2011 | 5 | 8 | |
| 2012 | 5 | 8 | |
| 2013 | 4 | 7 | |
| 2014 | 6 | 10 | |
| 2015 | 6 | 10 | |
| 2016 | 7 | 11 | |
| 2017 | 11 | 18 | |
| 2018 | 4 | 7 | |
| 2019 | 2 | 3 | |
| 2020 | 4 | 7 | |
| 2021 | 3 | 5 | |
| Country of study | Benin | 1 | 2 |
| Botswana | 1 | 2 | |
| Burkina Faso | 1 | 2 | |
| Cameroon | 3 | 5 | |
| Democratic Republic of the Congo | 1 | 2 | |
| Eswatini | 1 | 2 | |
| Ethiopia | 4 | 7 | |
| Ghana | 6 | 10 | |
| Kenya | 6 | 10 | |
| Madagascar | 1 | 2 | |
| Malawi | 5 | 8 | |
| Mozambique | 3 | 5 | |
| Namibia | 2 | 3 | |
| Nigeria | 4 | 7 | |
| Senegal | 1 | 2 | |
| Sierra Leone | 1 | 2 | |
| South Africa | 4 | 7 | |
| Swaziland | 1 | 2 | |
| Tanzania | 2 | 3 | |
| Uganda | 8 | 13 | |
| Zambia | 2 | 3 | |
| Zimbabwe | 1 | 2 | |
| Multi-country | 2 | 3 | |
| Type of article | Original research | 61 | 100 |
| Study design | Quantitative research | 42 | 69 |
| Qualitative research | 10 | 16 | |
| Mixed methods | 9 | 15 | |
| Main focus | Rationale | 1 | 2 |
| Scope | 7 | 11 | |
| Both | 53 | 87 | |
| Level of care | Community care level | 8 | 13 |
| Primary care level | 13 | 21 | |
| Primary and community care level | 15 | 25 | |
| Secondary and primary care level | 7 | 11 | |
| Secondary care level | 13 | 21 | |
| Secondary, primary, and community care level | 2 | 3 | |
| Tertiary care level | 2 | 3 | |
| All levels | 1 | 2 | |
Table 4.
Details on study characteristics.
| First Author (Year) |
Country | Study Title | Study Design and Population | Study Focus |
Level of Care |
|---|---|---|---|---|---|
| Bemelmans 2010 | Malawi | Providing universal access to antiretroviral therapy in Thyolo, Malawi through task shifting and decentralization of HIV⁄AIDS care | Design Cross-sectional study (descriptive) Population: People living with HIV/AIDS Health workers: Nurses to health surveillance assistant (HSA)/lay counsellor, medical doctors, clinical officer, medical assistant, and nurses. |
Rationale, Scope | Secondary and primary care level |
| Kosgei 2010 | Kenya | Task shifting in HIV clinics, Western Kenya | Design Cross-sectional study (descriptive) | Rationale, Scope | Primary care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Nurses and clinical officer. | |||||
| Labhardt 2010 | Cameroon | Task shifting to non-physician clinicians for integrated management of hypertension and diabetes in rural Cameroon: a programme assessment at two years | Design: Cross-sectional study (implementation) | Rationale, Scope | Primary care level |
| Population: People requiring hypertension and diabetes care | |||||
| Health workers: Non-physician clinician (NPC)—nurses | |||||
| Selke 2010 | Kenya | Task-Shifting of antiretroviral delivery from health care workers to persons living with HIV/AIDS: clinical outcomes of a community-based program in Kenya | Design: Prospective cluster-randomized controlled clinical trial Population: People living with HIV/AIDS Health workers: People living with HIV/AIDS (PLWAs) as community care coordinators (CCCs) |
Scope | Primary care level |
| De Wet 2011 | South Africa | Exploring task-shifting practices in antiretroviral treatment facilities in the Free State Province, South Africa | Design: Prospective cluster-randomized controlled clinical trial Population: People living with HIV/AIDS Health workers: Nurses and community health workers—‘lay workers’, ‘community care workers’, ‘home-based carers’, ‘directly observed treatment (DOT) supporters’, or ‘lay counselors. |
Rationale, Scope | Primary care level |
| Chibanda 2011 | Zimbabwe | Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV | Design: Cross-sectional study (implementation) | Scope | Primary care level |
| Population: General population with a high prevalence of people living with HIV | |||||
| Health workers: Lay workers (health promoters) | |||||
| Gessessew 2011 | Ethiopia | Task shifting and sharing in Tigray, Ethiopia, to achieve comprehensive emergency obstetric care | Design: Cross-sectional study (retrospective review of hospital records) | Scope | Secondary and primary care level |
| Population: Women of reproductive age receiving obstetric care | |||||
| Health workers: Non-physician clinicians (NPCs) | |||||
| Jennings 2011 | Benin | Task shifting in maternal and newborn care: a non-inferiority study examining delegation of antenatal counseling to lay nurse aides supported by job aids in Benin | Design: Non-inferiority quasi-experimental design | Rationale, Scope | Primary care level |
| Population: Women of reproductive age receiving maternal and newborn health service | |||||
| Health workers: Nurse-midwives and lay nurse aides | |||||
| Umar 2011 | Nigeria | Reduction of client waiting time using task shifting in an anti-retroviral clinic at Specialist Hospital Bauchi, Nigeria. | Design: Cross-sectional study (implementation) | Rationale, Scope | Secondary care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Doctors and nurses | |||||
| Tweya 2012 | Malawi | Task shifting’ in an antiretroviral clinic in Malawi: can health surveillance assistants manage patients safely? | Design: Cross-sectional study (implementation) | Rationale, Scope | Primary care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Health surveillance assistants (HSAs) | |||||
| Hoke 2012 | Madagascar | Community-based provision of injectable contraceptives in Madagascar: ‘task shifting’ to expand access to injectable contraceptives | Design: Cross-sectional study (implementation) | Rationale, Scope | Community care level |
| Population: Women of reproductive age requiring contraceptives | |||||
| Health workers: Community-based distribution (CBD) agents/community health workers | |||||
| Born 2012 | Zambia | Evaluation of a task-shifting strategy involving peer educators in HIV care and treatment clinics in Lusaka, Zambia | Design: Cross-sectional mixed-methods study | Rationale, Scope | Community care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Peer educators (PEs). | |||||
| Dambisya 2012 | Uganda | Policy and programmatic implications of task shifting in Uganda: a case study | Design: Cross-sectional, qualitative descriptive study | Rationale, Scope | Secondary, primary, and community care level |
| Population: General population, PLWHA, etc. | |||||
| Health workers: Clinical officers, nurses, midwives, and CHWs | |||||
| Mafigiri 2012 | Uganda | Task shifting for tuberculosis control: A qualitative study of community-based directly observed therapy in urban Uganda | Design Cross-sectional mixed-methods study | Rationale, Scope | Community care level |
| Population: People living receiving TB care | |||||
| Health workers: Laypersons | |||||
| Kiweewa 2013 | Uganda | Noninferiority of a task-shifting HIV care and treatment model using peer counselors and nurses among Ugandan women initiated on ART: evidence from a randomized trial | Design: Prospective randomized intervention trial study | Rationale, Scope | Secondary care level |
| Population: Women on ART | |||||
| Health workers: peer counselors and nurses | |||||
| Boullé 2013 | Cameroon | Task shifting HIV care in rural district hospitals in Cameroon | Design cohort study | Rationale, Scope | Secondary care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Nurses | |||||
| Ledikwe 2013 | Botswana | Evaluation of a well-established task-shifting initiative: The lay counselor cadre in Botswana | Design: Cross-sectional multi-method study | Rationale, Scope | Primary and community care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Lay Counselors | |||||
| Galukande 2013 | Uganda | Use of surgical task shifting to scale up essential surgical services: a feasibility analysis at facility level in Uganda | Design: Cross-sectional qualitative study | Rationale, Scope | Secondary care level |
| Population General population | |||||
| Health workers: surgical specialists | |||||
| Baine 2014 | Uganda | A scoping study on task shifting: the case of Uganda | Design: Cross-sectional qualitative study | Rationale, Scope | Secondary, primary, and community care levels |
| Population: General population | |||||
| Health workers: Clinical officers, nurses | |||||
| Asfaw 2014 | Ethiopia | Patient satisfaction with task shifting of antiretroviral services in Ethiopia: implications for universal health coverage | Design: Cross-sectional study | Scope | Secondary and primary care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Health officers and nurses | |||||
| Paul 2014 | Uganda | Barriers and facilitators in the provision of post-abortion care at district level in central Uganda—a qualitative study focusing on task sharing between physicians and midwives | Design: Cross-sectional qualitative study | Rationale, Scope | Secondary care level |
| Population: Women of reproductive health | |||||
| Health workers: Midwives | |||||
| O’Malley 2014 | Namibia | Nurse task shifting for antiretroviral treatment services in Namibia: implementation research to move evidence into action | Design: Cross-sectional study (implementation) | Rationale, Scope | Secondary and primary care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Nurses | |||||
| Andriamanjato 2014 | Madagascar, Malawi, and Rwanda | Task shifting in primary eye care: how sensitive and specific are common signs and symptoms to predict conditions requiring referral to specialist eye personnel? | Design: Cross-sectional study (implementation) | Rationale, Scope | Secondary care level |
| Population: General population | |||||
| Health workers: General primary healthcare (PHC) workers—ophthalmic clinical officers | |||||
| Eliah 2014 | Kenya, Malawi, and Tanzania | Task shifting for cataract surgery in eastern Africa: productivity and attrition of non-physician cataract surgeons in Kenya, Malawi, and Tanzania | Design: Cross-sectional study (implementation) | Rationale, Scope | Secondary care level |
| Population: General population | |||||
| Health workers: Non-physician cataract surgeons | |||||
| Wiedenmayer 2015 | Tanzania | The reality of task shifting in medicines management- a case study from Tanzania | Design: Cross-sectional study | Rationale, Scope | Secondary and primary care level |
| Population: General population | |||||
| Health workers: Nurses and medical attendants | |||||
| Mwangala 2015 | Zambia | Task-shifting and quality of HIV testing services: experiences from a National Reference Hospital in Zambia | Design: Cross-sectional qualitative study | Rationale, Scope | Secondary care level |
| Population: General population. | |||||
| Health workers: Lay counselors, nurses, and laboratory personnel | |||||
| Suzan-Monti 2015 | Cameroon | Benefits of task-shifting HIV care to nurses in terms of health-related quality of life in patients initiating antiretroviral therapy in rural district hospitals in Cameroon | Design: Cross-sectional study (implementation) | Rationale, Scope | Secondary care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Nurses | |||||
| Chamberlain 2015 | Uganda | Mortality related to acute illness and injury in rural Uganda: task shifting to improve outcomes | Design: Cross-sectional study (intervention) | Rationale, Scope | Secondary care level |
| Population: General population | |||||
| Health workers: Nurses | |||||
| Charyeva 2015 | Nigeria | Task shifting provision of contraceptive implants to community health extension workers: results of operations research in northern Nigeria | Design: Cross-sectional study (intervention) | Rationale, Scope | Community care level |
| Population: Women of reproductive age | |||||
| Health workers: Community health extension workers | |||||
| Agyapon 2015 | Ghana | Task shifting Ghana’s community mental health workers’ experiences and perceptions of their roles and scope of practice | Design: Cross-sectional study | Rationale, Scope | Community care level |
| Population: General population | |||||
| Health workers: Community mental health workers—community psychiatric nurses (CPNs), clinical psychiatric officers (CPOs), and community mental health officers (CMHOs) | |||||
| Akeju 2016 | Nigeria | Human resource constraints and the prospect of task-sharing among community health workers for the detection of early signs of pre-eclampsia in Ogun State, Nigeria | Design: Cross-sectional qualitative study | Rationale, Scope | Primary care level |
| Population: Women of reproductive age | |||||
| Health workers: Community health extension workers (CHEW) | |||||
| Wright 2016 | Malawi | Building capacity for community mental health care in rural Malawi: Findings from a district-wide task-sharing intervention with village-based health workers | Design: Cross-sectional study (intervention) | Rationale, Scope | Primary and community care level |
| Population: General population | |||||
| Health workers: Village-based health workers | |||||
| Gueye 2016 | Senegal | Mentoring, task sharing, and community outreach through the TutoratPlus approach: increasing use of long-acting reversible contraceptives in Senegal | Design: Cross-sectional study (intervention) | Rationale, Scope | Primary and community care level |
| Population: Women of reproductive age | |||||
| Health workers: Nurses, non-clinical family planning counselors, and community health workers | |||||
| Dos Santos 2016 | Mozambique | Overview of the mental health system in Mozambique: addressing the treatment gap with a task-shifting strategy in primary care | Design: Cross-sectional study (intervention) | Rationale, Scope | Primary and community care level |
| Population: General population | |||||
| Health workers: Psychiatric technicians | |||||
| Agyapong 2016a | Ghana | Improving Ghana’s mental healthcare through task-shifting psychiatrists’ and health policy directors’ perceptions about government’s commitment and the role of community mental health workers | Design: Cross-sectional study (mixed methods) | Rationale, Scope | Primary and community care level |
| Population: General population | |||||
| Health workers: Community mental health workers—community mental health officers (CMHOs), clinical psychiatric officers (CPOs), and clinical psychiatric nurses (CPNs) | |||||
| Some 2016 | Kenya | Task shifting the management of non-communicable diseases to nurses in Kibera, Kenya: does it work? | Design: Cross-sectional study (descriptive retrospective) | Rationale, Scope | Primary care level |
| Population: General population | |||||
| Health workers: Nurses | |||||
| Agyapong 2016b | Ghana | Task shifting perception of stake holders about adequacy of training and supervision for community mental health workers in Ghana | Design: Cross-sectional study (mixed methods) | Rationale, Scope | Primary and community care level |
| Population: General population | |||||
| Health workers: Community mental health workers—community mental health officers (CMHOs), clinical psychiatric officers (CPOs) and, clinical psychiatric nurses (CPNs) | |||||
| Landes 2017 | Malawi | Task shifting of triage to peer expert informal care providers at a tertiary referral HIV clinic in Malawi: a cross-sectional operational evaluation | Design Cross-sectional study (implementation) | Rationale, Scope | Tertiary care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Lay health cadre of expert patients (EPs) | |||||
| Okyere 2017 | Ghana | Is task-shifting a solution to the health workers’ shortage in Northern Ghana? | Design: Cross-sectional study (qualitative) | Rationale | All levels |
| Population: General population | |||||
| Health workers: Medical assistants (MA), midwives, general registered nurses (GRN), enrolled nurses (EN), community health officers (CHO), disease control officers (DCO), psychiatric nurses (PN), optometrist, and health nurse aides | |||||
| Tilahun 2017 | Ethiopia | Improving contraceptive access, use, and method mix by task sharing Implanon insertion to frontline health workers: the experience of the integrated family health program in Ethiopia | Design: Cross-sectional study (intervention) | Rationale, Scope | Primary and community care level |
| Population: Women of reproductive age | |||||
| Health workers: Health extension workers | |||||
| Bolkan 2017 | Sierra Leone | Safety, productivity and predicted contribution of a surgical task-sharing programme in Sierra Leone | Design: Prospective observational study | Rationale, Scope | Secondary care level |
| Population: General population | |||||
| Health workers: Associate clinicians/community health officers (CHOs) and junior doctors | |||||
| Farley 2017 | South Africa | Evaluation of a nurse practitioner–physician task-sharing model for multidrug-resistant tuberculosis in South Africa | Design: Prospective cohort study | Rationale, Scope | Secondary care level |
| Population: People with multidrug-resistant tuberculosis | |||||
| Health workers: Clinical nurse practitioner (CNP) and a medical officer (MO) | |||||
| Lulebo 2017 | Democratic Republic of the Congo | Task shifting in the management of hypertension in Kinshasa, Democratic Republic of Congo: a cross-sectional study | Design: Cross-sectional study | Rationale, Scope | Primary care level |
| Population: People with hypertension | |||||
| Health workers: Nurses | |||||
| Gyamfi 2017 | Ghana | Training nurses in task-shifting strategies for the management and control of hypertension in Ghana: a mixed-methods study | Design: Mixed-methods study | Rationale, Scope, | Secondary, and primary care level |
| Population: People with hypertension | |||||
| Health workers: Community health nurses (CHNs) and enrolled nurses (ENs) | |||||
| Dlamini-Simelane 2017 | Swaziland | Task shifting or shifting care practices? The impact of task shifting on patients’ experiences and health care arrangements in Swaziland | Design: Cross-sectional (qualitative—ethnographic) study | Rationale, Scope | Primary and community care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Lay counsellors and nurses | |||||
| Kaindjee-Tjituka 2017 | Namibia | Task-shifting point-of-care CD4+ testing to lay health workers in HIV care and treatment services in Namibia | Design: Cross-sectional study | Rationale, Scope | Primary and community care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Lay health workers and nurses | |||||
| Naburi 2017 | Tanzania | The potential of task-shifting in scaling up services for prevention of mother-to-child transmission of HIV: a time and motion study in Dar es Salaam, Tanzania | Design: Cross-sectional study (intervention) | Rationale, Scope | Primary and community care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Community health workers (CHWs) and nurses | |||||
| Naikoba 2017 | Uganda | Improved HIV and TB knowledge and competence among mid-level providers in a cluster-randomized trial of one-on-one mentorship for task shifting | Design: Cluster-randomized trial | Rationale, Scope | Secondary and primary care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Mid-level providers (MLPs)—clinical officers, registered nurses, and registered midwives | |||||
| Marotta 2018 | Mozambique | Pathways of care for HIV-infected children in Beira, Mozambique: pre–post intervention study to assess impact of task shifting | Design: Cross-sectional study (intervention) | Rationale, Scope | Primary and community care level |
| Population: People living with HIV/AIDS | |||||
| Health workers: Maternal and child nurses | |||||
| Davis 2018 | Malawi | Task shifting levonorgestrel implant insertion to community midwife assistants in Malawi: results from a non-inferiority evaluation | Design: Cross-sectional study (intervention) | Rationale, Scope | Primary and community care level |
| Population: Women of reproductive age requiring contraceptives | |||||
| Health workers: Community midwife assistants (CMAs) | |||||
| Awolude 2018 | Nigeria | Screen and triage by community extension workers to facilitate screen and treat: task-sharing strategy to achieve universal coverage for cervical cancer screening in Nigeria | Design: Cross-sectional study (intervention) | Rationale, Scope | Primary care level |
| Population: Women of reproductive age | |||||
| Health workers: CHEWs and CHOs | |||||
| Sayed 2018 | Kenya | Task Sharing and shifting to provide pathology diagnostic services: The Kenya fine-needle aspiration biopsy cytology and bone marrow aspiration and trephine biopsy training program | Design: Cross-sectional study (intervention) | Rationale, Scope | Tertiary care level |
| Population: General population | |||||
| Health workers: Pathologists, medical officers (MO), clinical officers (CO), and technologists | |||||
| Millogo 2019 | Burkina Faso | Task sharing for family planning services, Burkina Faso | Design: Cross-sectional study (intervention) | Rationale, Scope | Primary and community care level |
| Population: Women of reproductive age requiring contraceptives | |||||
| Health workers: Community health workers (CHWs), auxiliary nurses, and auxiliary midwives | |||||
| Tariku 2019 | Ethiopia | Surgical task shifting helps reduce neonatal mortality in Ethiopia: A retrospective cohort study | Design: Retrospective cohort study | Rationale, Scope | Secondary care level |
| Population: Women of reproductive age requiring contraceptives | |||||
| Health workers: Non-physician surgeons (NPS) | |||||
| Wall 2020 | Kenya | What about lay counselors’ experiences of task-shifting mental health interventions? Example from a family-based intervention in Kenya | Design: Cross-sectional study (mixed methods) | Scope | Community care level |
| Population: General population | |||||
| Health workers: Lay counselors | |||||
| Gbagbo 2020 | Ghana | Increasing access to intrauterine contraceptive device uptake in Ghana: stakeholders’ views on task sharing service delivery with community health nurses | Design: Cross-sectional qualitative study | Rationale, Scope | Community care level |
| Population: Women of reproductive age requiring contraceptives | |||||
| Health workers: Community health nurses | |||||
| Peresu 2020 | Eswatini | Task-shifting directly observed treatment and multidrug-resistant tuberculosis injection administration to lay health workers: stakeholder perceptions in rural Eswatini | Design: Mixed-methods study—cross-sectional survey and qualitative study | Rationale, Scope | Community care level |
| Population: People with tuberculosis | |||||
| Health workers: Lay health workers (LHWs)/community treatment supporter (CTS) | |||||
| Lund 2020 | South Africa | Task-sharing of psychological treatment for antenatal depression in Khayelitsha, South Africa: Effects on antenatal and postnatal outcomes in an individual randomized controlled trial | Design: Randomized controlled trial | Rationale, Scope | Primary and community care level |
| Population: Women of reproductive age | |||||
| Health workers: Non-specialist community health workers | |||||
| Sevene 2021 | Mozambique | Feasibility of task-sharing with community health workers for the identification, emergency management, and referral of women with pre-eclampsia, in Mozambique | Design: Mixed-methods study | Rationale, Scope | Primary and community care level |
| Population: Pregnant women | |||||
| Health workers: Community health workers | |||||
| Jacobs 2021 | South Africa | Task sharing or task dumping: counsellors experiences of delivering a psychosocial intervention for mental health problems in South Africa | Design: Cross-sectional qualitative study | Scope | Primary care level |
| Population: General population | |||||
| Health workers: Non-specialist—facility-based counsellors (FBCs), specific cadre of community health workers trained to deliver health promotion and HIV adherence counselling services | |||||
| Yator 2021 | Kenya | Task-sharing and piloting WHO group interpersonal psychotherapy (IPT-G) for adolescent mothers living with HIV in Nairobi primary health care centers: a process paper | Design: Cross-sectional study (intervention) | Scope | Primary care level |
| Population: Postpartum adolescent (PPA) mothers living with HIV | |||||
| Health workers: Community health workers (CHWs) |
3.3. Main Themes from the Included Studies
The main theme and subthemes are presented in Table 5 and described in subsequent sections.
Table 5.
Main theme and sub-themes.
| Main Theme | Sub-Themes |
|---|---|
| Rationale for task shifting and task sharing | Health worker shortages |
| Optimally utilize existing health workers | |
| Expand access to health services | |
| Scope of shifted and shared tasks | HIV/AIDS care |
| Hypertension management | |
| Diabetes management | |
| Mental health | |
| Maternal and child healthcare | |
| Sexual and reproductive health services | |
| Eye care | |
| Tuberculosis care | |
| Surgical care and procedures | |
| Medicines’ management | |
| Emergency care |
3.3.1. Rationale for Task Shifting and Task Sharing
Fifty-four studies [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74] included under this theme provided insights on the rationale for the implementation of task shifting and task sharing in Africa, as presented in Table 6.
Table 6.
Summary of key findings on rationale and scope of task shifting and task sharing in reviewed studies.
| First Author (Year) | Country | Health Services Context | Key Findings |
|---|---|---|---|
| Bemelmans 2010 | Malawi | Access to HIV⁄AIDS care | Rationale: Staff shortages in the levels of care and by location. Scope: HIV testing and counselling from nurses to health surveillance assistant (HSA)/lay counsellor, antiretroviral therapy (ART) initiations from medical doctors to non-physician clinicians—clinical officer, medical assistant, and nurse |
| Kosgei 2010 | Kenya | Access to HIV⁄AIDS care | Rationale: Scarcity of healthcare providers and the need to improve patient outcomes without increasing clinic human resources. Scope: ART care |
| Labhardt 2010 | Cameroon | Access to care for hypertension and type 2 diabetes care | Rationale: Majority of the rural population does not have access to adequate hypertension and diabetes care. Scope: Hypertension and diabetes care |
| Selke 2010 | Kenya | Access to HIV⁄AIDS care | Scope: Delivery of medications and provision of follow-up care to patients on ART in the community with support of an electronic decision tool, and 3 monthly visits to facilities compared to the usual monthly visit. |
| De Wet 2011 | South Africa | Access to HIV⁄AIDS care | Rationale: Shortage of health workers (physicians and nurses). Scope: Task shifting from nurses to community health workers for HIV treatment and care. HIV counselling, drug readiness training, distribution of nutritional supplements, and capturing and updating electronic information. |
| Chibanda 2011 | Zimbabwe | Access to mental health intervention/services | Scope: Depression and other common mental disorders (CMD)—screening and monitoring CMD and in delivering the intervention |
| Gessessew 2011 | Ethiopia | Access to comprehensive obstetric care | Rationale: Shortage of physicians in rural areas. Scope: Comprehensive emergency obstetric care (CEmOC) |
| Jennings 2011 | Benin | Access to maternal and newborn health services | Rationale: Need to expand the role of lay nurse aides. Scope: Counselling in maternal and newborn care. |
| Umar 2011 | Nigeria | Access to HIV⁄AIDS care | Rationale: Long waiting time of HIV/AIDS patients in the clinic due to the high workload of available doctors. Scope: Consultation for HIV patients presenting for routine refill and follow-up visits |
| Tweya 2012 | Malawi | Access to HIV⁄AIDS care | Rationale: Shortage of clinicians and nurses. Scope Provision of antiretroviral therapy (ART) to stable patients. |
| Hoke 2012 | Madagascar | Access to injectable contraceptives | Rationale Lack of access to health facilities. Scope: Injection (re-injection) and counselling of patients. |
| Born 2012 | Zambia | Access to HIV⁄AIDS care | Rationale: Rapid expansion of antiretroviral therapy (ART) using existing health workers. Scope: Provision of counselling, education talks, and adherence support to patients in HIV care. |
| Dambisya 2012 | Uganda | Access to HIV⁄AIDS care, maternal and child health, general healthcare, etc. | Rationale: Severe health worker shortage and a high demand for healthcare services. Scope: Community health workers (CHW) and PLWHA in care and support of AIDS patients, ophthalmic clinical officers conduct cataract surgery, psychiatric clinical officers cover the same scope as the psychiatrists, but are more community-oriented than the psychiatrists, who tend to be mainly hospital-based. Nurses set IV lines in upcountry due to lack of physicians, midwives conduct manual vacuum extraction, manual removal of the placenta, and manual vacuum aspiration due to shortage of doctors. CHWs and community members involved in delivery of expanded program on immunization (EPI) services, etc. |
| Mafigiri 2012 | Uganda | Access to TB care | Rationale: To address barriers to successful DOTS in rural areas. Scope: Directly observed treatment short course (DOTS) |
| Kiweewa 2013 | Uganda | Access to HIV⁄AIDS care | Rationale Shortage of physicians. Scope: ART follow-up care to postpartum women |
| Boullé 2013 | Cameroon | Access to HIV⁄AIDS care | Rationale Shortage of physicians |
| Ledikwe 2013 | Botswana | Access to HIV⁄AIDS care | Rationale: Shortage of health workers. Scope: HIV tests and related counselling at public health facilities |
| Galukande 2013 | Uganda | Access to surgical services | Rationale: Shortage and maldistribution of surgical specialists. Scope: Emergency and essential surgical care |
| Baine 2014 | Uganda | Access to health services | Rationale: Shortage of health workers in Uganda. Scope: Surgical care, sexual and reproductive health, HIV/AIDS, tuberculosis DOTS therapy. |
| Asfaw 2014 | Ethiopia | Access to HIV⁄AIDS care | Scope: Antiretroviral therapy |
| Paul 2014 | Uganda | Access to post-abortion care | Rationale Absence of physicians. Scope: Post-abortion care |
| O’Malley 2014 | Namibia | Access to HIV⁄AIDS care | Rationale: Shortage of physicians. Scope: Antiretroviral treatment services |
| Andriamanjato 2014 | Madagascar, Malawi, and Rwanda | Access to eye care | Rationale: Shortage of health workers trained in eye care. Scope: Primary eye care |
| Eliah 2014 | Kenya, Malawi, and Tanzania | Access to eye care | Rationale: Shortage and maldistribution of ophthalmologists. Scope: Cataract surgery |
| Wiedenmayer 2015 | Tanzania | Access to medicines | Rationale: Severe shortage of pharmaceutical staff. Scope: Pharmaceutical management |
| Mwangala 2015 | Zambia | Access to HIV testing | Rationale: Shortage of human resources. Scope: HIV testing services |
| Suzan-Monti 2015 | Cameroon | Access to HIV⁄AIDS care | Rationale: Shortage of physicians in rural areas. Scope: Initiating antiretroviral therapy (ART) |
| Chamberlain 2015 | Uganda | Access to emergency care services | Rationale: Critical shortages of acute care and healthcare workers in resource-limited settings. Scope: Emergency care services in a rural setting |
| Charyeva 2015 | Nigeria | Access to contraceptive implants | Rationale: Severe shortage of human resources. Scope: Provision of contraceptive implants |
| Agyapon 2015 | Ghana | Access to mental health services | Rationale: Inadequate numbers of psychiatrists. Scope: Mental healthcare |
| Akeju 2016 | Nigeria | Access to maternal health services | Rationale: Non-availability of health personnel at the primary healthcare level. Scope: Detection of early signs of pre-eclampsia |
| Wright 2016 | Malawi | Access to mental health services | Rationale: Improve access to primary mental healthcare. Scope: Primary mental healthcare |
| Gueye 2016 | Senegal | Access to family planning services | Rationale: To improve access to family planning in rural areas and improve contraceptive prevalence. Scope: Provision of family planning services—long-acting reversible contraceptives (LARC), specifically implants and the intrauterine device. |
| Dos Santos 2016 | Mozambique | Access to mental health services | Rationale: To expand access to primary mental healthcare due to low numbers of psychiatrists and psychologists Scope: Delivery of psychiatric care |
| Agyapong 2016a | Ghana | Access to mental health services | Rationale: Expand mental healthcare delivery due to shortage of psychiatrists. Scope: CPNs and CMHOs are primarily responsible for case detection in the community, referral of patients to CPOs and psychiatrists. CPOs are responsible for diagnosing and treating a range of common psychiatric conditions |
| Some 2016 | Kenya | Access to non-communicable diseases (NCDs) care | Rationale: Shortage of health workers at the primary level of care and need to increase access to NCD care in primary healthcare settings. Scope: Management of NCDs (hypertension, diabetes mellitus type 2, epilepsy, asthma, and sickle cell) |
| Agyapong 2016b | Ghana | Access to mental health services | Rationale: Shortage of psychiatrists. Scope: Case detection and referral, and diagnosis and treatment of common psychiatric conditions. |
| Landes 2017 | Malawi | Access to HIV⁄AIDS care | Rationale: Shortage of health workers Scope: Triaging of HIV/AIDS patients |
| Okyere 2017 | Ghana | Rationale: Insufficient health workers. | |
| Tilahun 2017 | Ethiopia | Access to family planning services | Rationale: To improve access to family planning in rural areas and improve contraceptive prevalence. Scope: Provision of long-acting contraceptive (Implanon) family planning services. |
| Bolkan 2017 | Sierra Leone | Access to emergency surgical care | Rationale: Shortage of surgical providers. Scope: Surgical and obstetric emergencies |
| Farley 2017 | South Africa | Access to TB treatment services | Rationale: Shortages of medical officers to implement decentralization of MDR-TB treatment service to outpatient settings/lower-level health facilities. Scope: Multidrug-resistant tuberculosis (MDR-TB) treatment |
| Lulebo 2017 | Democratic Republic of the Congo | Access to hypertension management services | Rationale: Shortage of health workers. Scope: Hypertension management |
| Gyamfi 2017 | Ghana | Access to hypertension management services | Rationale: To expand service delivery to lower levels. Scope: Hypertension management and control |
| Dlamini-Simelane 2017 | Swaziland | Access to HIV⁄AIDS care | Rationale: Decentralized ART provision to improve access. Scope: HIV counselling by lay counsellors (predominantly PLHIV), initiation of patients on ART by nurses |
| Kaindjee-Tjituka 2017 | Namibia | Access to CD4+ testing | Rationale: Roll-out and scale-up of POC CD4+ testing in HCT settings in public health facilities. Scope: Point-of-care (POC) CD4+ testing |
| Naburi 2017 | Tanzania | Access to HIV⁄AIDS care—PMTCT services | Rationale: Reduce nurses’ workload and health system costs. Scope: Prevention of mother-to-child transmission of HIV (PMTCT) service delivery |
| Naikoba 2017 | Uganda | Access to HIV/AIDS and TB services | Rationale: Health worker shortages. Scope: HIV care and treatment |
| Marotta 2018 | Mozambique | Access to HIV/AIDS services for children < 5 years | Rationale: To improve ART initiation and retention of HIV-infected children. Scope: Care for HIV-positive children < 5 years old |
| Davis 2018 | Malawi | Access to contraceptive implants | Rationale: Shortage of nurses/midwives. Scope: Long-acting reversible contraception (LARC) insertion (levonorgestrel (LNG) contraceptive implants) |
| Awolude 2018 | Nigeria | Access to cervical cancer screenings | Rationale: Shortage of doctors and nurses in rural areas. Scope: Screen for cervical cancer using visual inspection with acetic acid |
| Sayed 2018 | Kenya | Access to cancer screenings | Rationale: Scarcity of pathologists in Kenya. Scope: Fine-needle aspiration biopsy cytology and bone marrow aspiration and trephine biopsy |
| Millogo 2019 | Burkina Faso | Access to contraceptives | Rationale Shortage of qualified health staff. Scope: Community health workers (CHWs) to offer oral and injectable contraceptives to new users, and auxiliary nurses and auxiliary midwives to provide implants and intrauterine devices. |
| Tariku 2019 | Ethiopia | Access to contraceptives | Rationale: Shortage of physicians, improve access to surgical services and reduce neonatal mortality. Scope: Caesarean section |
| Wall 2020 | Kenya | Access to mental health services | Rationale: Improve access at the community level. Scope: Community-based family therapy mental health interventions |
| Gbagbo 2020 | Ghana | Access to intrauterine contraceptive device | Rationale: Addressing persistent human resources shortages. Scope: Intrauterine contraceptive device |
| Peresu 2020 | Eswatini | Access to multidrug-resistant tuberculosis (MDR-TB) treatment in rural areas | Rationale: Shortage of human resources for health (HRH) and limited access to multidrug-resistant tuberculosis (MDR-TB) treatment in rural areas. Scope: Directly observed treatment (DOT) supervision and administration of intramuscular MDR-TB injections |
| Lund 2020 | South Africa | Access to mental health services | Rationale: Dearth of mental health professionals. Scope: Psychological treatment for perinatal depression |
| Sevene 2021 | Mozambique | Access to hypertension services | Rationale: Delays in reaching health facilities and insufficient healthcare professionals. Scope: Initial screening and initiation of obstetric emergency care for pre-eclampsia/eclampsia |
| Jacobs 2021 | South Africa | Access to mental health services | Scope: Mental health counselling |
| Yator 2021 | Kenya | Access to HIV/AIDS care | Scope: Interpersonal psychotherapy (IPT-G) for adolescent mothers living with HIV |
Health Worker Shortages
Forty studies [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37] reported the rationale for task shifting and task sharing implementation to be due to a shortage of health workers. The cadres reported to be inadequate to inform task shifting and task sharing in the various countries included physicians [38,39,40,41,42,43], nurses [44,45,46], midwives [46], surgical specialists [47,48], eye care specialists [75,76], pharmaceutical staff [49], emergency care practitioners [27], psychiatrists [50,51,52,53], psychologists [51], and pathologists [54]. Insights on the reported shortages were provided in four studies. A study in Malawi [22] stated that the shortage was prominent by the level of care and geographical location. The studies in Cameroon [41], Ethiopia [55], and Nigeria [56] reported that the shortage of physicians and nurses was more prominent in rural areas. Two other Nigerian studies reported shortages being marked at the primary level of care [45,77]. Further insight on the impact on health services’ delivery was provided in two Ugandan studies [57,58]. These studies highlighted that the health worker shortage meant the high demand for health services could not be adequately met.
Optimally Utilize Existing Health Workers
Seven [22,59,60,61,62,63,64] studies reported the rationale for task shifting and sharing implementation to include the need to optimally utilize the available human resources within a health service level to deliver health services. The study in Benin [59] implemented task shifting to expand the role of existing lay nurse aides to conduct counselling in maternal and newborn care. In a study conducted in Kenya [60], task shifting was implemented in HIV/AIDS care to optimally utilize existing health workers to improve outcomes without increasing resources. A Nigerian study [61] reported the implementation of task shifting to reduce the waiting time for accessing services from doctors by expanding the role of existing nurses. In Zambia [62], the rationale for implementing task shifting and sharing was to utilize existing peer educators in expanding the delivery of health services. A study in Tanzania [63] reported a task shifting implementation in preventing mother-to-child transmission (PMTCT) service delivery to optimally utilize existing health workers by reducing nurses’ workload and health system costs.
Expand Access to Health Services
Twelve [22] studies reported the rationale for task shifting and sharing implementation to be to ensure increased access to health services at other levels of care and geographical locations, specifically, rural areas. The countries where an expansion of health services to other levels of care was reported include Ghana, Kenya, Madagascar, Malawi, Namibia, Swaziland, and Uganda. A study in Ghana [68] reported the implementation of task sharing to expand the service delivery of hypertension management and control to lower levels of care. In Kenya [45], the rationale for implementing task shifting was to increase access to non-communicable diseases (NCD) services (hypertension, diabetes mellitus type 2, epilepsy, asthma, and sickle cell) in primary healthcare settings. Another study in Kenya [74] reported implementing task shifting to improve access to mental health interventions at the community level. The study in Madagascar [66] reported that task shifting of the provision of contraceptives was implemented to expand access of community members through community health workers. A study in Malawi [67] reported task shifting of primary mental healthcare to the community level to improve the access of community members. In a Namibian study [73], task shifting was implemented to scale-up point-of-care CD4+ testing in HIV counselling and testing settings in public health facilities. A study in Swaziland [72] reported the implementation of task sharing to decentralize antiretroviral (ART) provision to improve access. A Ugandan study [71] reported the implementation of task shifting for tuberculosis to improve the access of community members to directly observed treatment short course (DOTS).
Studies from Cameroon, Eswatini, Ethiopia, and Senegal reported the implementation of task shifting and task sharing to expand health services to rural areas. In a study conducted in Cameroon [65], task shifting was implemented to increase the access of the rural population to adequate hypertension and diabetes care. A study in Eswatini [35] reported the implementation of task shifting tuberculosis management to improve access in rural areas. A study in Ethiopia [69] reported the task sharing implementation to improve access to family planning in rural areas. In a study in Senegal [70], task sharing to increase the use of long-acting reversible contraceptives was performed to improve the access to family planning in rural areas.
3.3.2. Scope of Shifted and Shared Tasks
Sixty reviewed studies reported a range of tasks that were either task-shifted or task-shared in various health services contexts in Africa (Table 6).
HIV/AIDS Care
Twenty-three studies reported task shifting and task sharing of HIV/AIDS services, as shown in Table 6. The HIV/AIDS service areas reported included HIV counselling and testing, ART, PMTCT, and care and support. Task shifting and sharing of HIV counselling and testing were reported in studies in Botswana [24], Malawi [22], Namibia [73], Swaziland [72], and Zambia [26]. The beneficiary cadres included laypersons [24], health surveillance assistant (HSA)/lay counsellor [22,26,72], nurses [26,73], and laboratory personnel [26]. ART-related task shifting and sharing were reported in Cameroon [41], Ethiopia [78], Kenya [60], and Malawi [22,44], with beneficiary cadres including nurses [22,41,60,78], health officers [78], clinical officers [22,60], medical assistants [22], and health surveillance assistants (HSAs) [44]. The task shifting and task sharing of care and support services by community health workers [79], people living with HIV/AIDS (PLWAs) as community care coordinators [80], laypersons [29], maternal and child nurses [64], and peer educators [62] was reported in Kenya [79,80], Malawi [29], Mozambique [64], and Zambia [62].
Hypertension Management
Five studies reported task shifting and task sharing in the management of hypertension. A study conducted in Cameroon [65] reported a task shifting of integrated management of hypertension to non-physician clinicians (nurses) in a rural setting to improve the access to care for hypertension. In Kenya [45], NCD service delivery, including hypertension, was task-shifted to nurses in primary healthcare settings. In a study conducted in the Democratic Republic of Congo (DRC) [31], hypertension management was task-shifted to nurses. In a Ghanian study [68], hypertension management was task-shifted to community health nurses (CHNs) and enrolled nurses (ENs). The study conducted in Mozambique [37] reported that initial screening and initiation of obstetric emergency care for pre-eclampsia/eclampsia was task-shifted to community health workers.
Diabetes Management
Two studies reported task shifting and task sharing in diabetes management. The first study from Cameroon [65] reported a task shifting of integrated management of diabetes to nurses in a rural setting to improve access to type 2 diabetes care. The second study, that was conducted in Kenya [45], reported task shifting of NCD services, including for diabetes mellitus, to nurses in primary healthcare settings.
Mental Health
Ten studies conducted in eight countries reported the scope of shifted or shared tasks to be within the delivery of the mental health services domain. Three studies in Ghana [50,52,53] reported the task shifting of mental healthcare to community mental health workers—community psychiatric nurses (CPNs), clinical psychiatric officers, (CPOs), and community mental health officers (CMHOs). A study in Malawi [67] reported task shifting of primary mental healthcare at the community level to village-based health workers. In a study conducted in Zimbabwe [81], delivery of depression and other common mental disorders (CMD) services, specifically screening and monitoring of CMD and delivery of interventions, were task-shifted to lay workers. The study in Uganda [57] reported task shifting and sharing practices to include psychiatric clinical officers covering the same scope as the psychiatrists. A study in Mozambique [51] reported task shifting of the delivery of psychiatric care to psychiatric technicians due to low numbers of psychiatrists and psychologists. A study in Kenya [74] reported implementing task shifting of community-based family therapy mental health interventions to lay counsellors. A study in South Africa [36] reported task shifting of psychological treatment for perinatal depression to non-specialist community health workers. Another study in South Africa [82] reported task sharing of mental health counselling to non-specialist facility-based counsellors (FBCs).
Maternal and Child Healthcare
In six studies from four countries, maternal and child health services were either task-shifted or task-shared. The study in Benin [59] implemented task shifting to expand the role of existing lay nurse aides to conduct counselling in maternal and newborn care. A study in Ethiopia [55] reported the task shifting of comprehensive emergency obstetric care (CEmOC) to non-physician clinicians (NPCs). In another study in Ethiopia [43], task shifting of the conduct of the caesarian section to non-physician surgeons (NPS) was reported. In a study in Nigeria [77], detection of early signs of pre-eclampsia was reported to be task-shifted, albeit informally, to community health extension workers. The study in Uganda [57] reported task shifting and task sharing practices to include midwives conducting manual vacuum extraction, manual removal of the placenta, and manual vacuum aspiration due to a shortage of doctors, and community health workers (CHWs) and community members were involved in the delivery of an expanded program on immunization (EPI) services. Another study in Uganda [39] highlighted that due to the absence of physicians in certain locations, midwives were often the main providers of post-abortion care services.
Sexual and Reproductive Health Services
Eight reviewed studies from seven countries reported the task shifting or task sharing of sexual and reproductive health services. A study in Burkina Faso [33] reported task shifting of the provision of oral and injectable contraceptives to community health workers, and implants and intrauterine devices to auxiliary midwives and nurses. A study in Ethiopia [69] reported the implementation of task sharing of the provision of long-acting contraceptive (Implanon) family planning services to health extension workers. A study in Ghana [34] reported the implementation of task sharing of the provision of an intrauterine contraceptive device to community health nurses. The study in Madagascar [66] task-shifted the provision of injectable contraceptives and counselling of patients to community health workers. In a study in Malawi [46], the task of long-acting reversible contraception (LARC) insertion was shifted to community midwife assistants (CMAs). In a study in Nigeria [28], the provision of contraceptive implants was task-shifted to community health extension workers. Another Nigerian study [56] reported the task shifting of the screening for cervical cancer using visual inspection with acetic acid to community health officers and community health extension workers. In a study in Senegal [70], task sharing of long-acting reversible contraceptives (LARC), specifically implants and intrauterine devices, was implemented for nurses, non-clinical family planning counsellors, and community health workers.
Eye Care
Task shifting of eye care services was reported in three studies conducted in six countries. A study in Uganda [57] reported task shifting and sharing practices to include ophthalmic clinical officers conducting cataract surgery. A study [75] in Madagascar, Malawi, and Rwanda reported task shifting of primary eye care service delivery to general primary healthcare (PHC) workers (ophthalmic clinical officers). A multi-country study [76] in Kenya, Malawi, and Tanzania also reported task shifting of cataract surgery to non-physician cataract surgeons.
Tuberculosis Care
The task shifting of tuberculosis-related care was reported in three studies. A Ugandan study reported the task shifting of directly observed treatment short course (DOTS) to laypersons [71] and nurses [25]. A study in South Africa [42] reported the task sharing of multidrug-resistant tuberculosis (MDR-TB) treatment between clinical nurse practitioners (CNPs) and medical officers (MO). A study in Eswatini [35] reported the task shifting of directly observed treatment (DOT) supervision and administration of intramuscular MDR-TB injections to lay health workers (LHWs)/community treatment supporters (CTS) to improve the access in rural areas.
Surgical Care and Procedures
For surgical care and procedures, three studies provided insights into task shifting and sharing practices. A study in Uganda [47] that explored surgical task shifting practices from surgical specialists to non-specialist physicians reported that the practice was already in place. A study in Sierra Leone [48] reported the implementation of task sharing of surgical and obstetric emergencies to associate clinicians/community health officers (CHOs) and junior doctors. In a Kenyan study [54], the conducting of fine-needle aspiration biopsy cytology, bone marrow aspiration, and trephine biopsy was shared by pathologists, medical officers (MO), clinical officers (CO), and technologists.
Medicines’ Management
One study from Tanzania [49] reported task shifting of pharmaceutical management to nurses and medical attendants. This was reported to be because of the shortage of pharmaceutical personnel in the country, which impacts negatively on service provision, especially in rural areas.
Emergency Care
One study reported task shifting of emergency care-related services. The study from Uganda [27] reported task shifting of acute care for emergency services in a rural setting to nurses. This was pertinent as 84% of the country’s population reside in rural areas and they require access to emergency care.
4. Discussion
This scoping review synthesized evidence on the rationale for task shifting and task sharing in Africa. The reported rationales in the reviewed papers were health worker shortages, the need to optimally utilize existing health workers, and the need to expand access to health services.
The health worker shortages were reported to be prominent by the level of care and geographical location, especially in rural areas. The finding on the shortage of health workers matches the reported global shortage of health workers, which is projected at 10 million by 2030 [83] and is more prominent in Africa [84] and rural and remote areas [85]. The implementation of task shifting and task sharing to cope with this is consistent with the literature. The suboptimal funding of public health [86], including service delivery and its impact on the quality of health infrastructure, the availability of health workers, and service delivery, is also reported in the literature. Similarly, the weak investment in HRH development has also been widely reported in Africa, and this is suggested to substantially contribute to the shortage of health workers [87]. Contributing to this is the dearth of attraction and retention strategies in countries, which is also compounding the shortages and resulting in poorly motivated health workers that are also inequitably distributed [85].
We also found that the need to optimally utilize existing health workers was another reported rationale for task shifting and task sharing. An important perspective gained in the study from Kenya [60] was task shifting being implemented to improve populations’ access to health services without increasing resource needs. This is recommended in instances where evidence exists of varied workloads and availability of certain cadres of health workers with low workloads that can take up additional tasks and relieve those with high workloads [88]. This should, however, be informed by an assessment of the workloads, use of the evidence to explore task shifting and task sharing possibilities [89], and adequate capacity building and provision of relevant incentives to beneficiary cadres, in order to ensure quality service delivery.
Another reported rationale for task shifting and task sharing was to expand access to health services to other levels of care and geographical locations, specifically, rural areas. The reported expansion of services to other levels of care and rural areas was implemented in scenarios where the primary cadres responsible for the service delivery were not typically available at the target level of care, based on the service delivery organization model. In the reviewed studies, the reported instances were expanding service delivery to primary [45] and community level settings [66,67,74] and rural areas [35,65,69], for improved access to NCD services, family planning services, and HIV/AIDS and tuberculosis services.
This scoping review also synthesized evidence on the scope of task shifting and task sharing implementation in Africa. Our findings indicate that the health services shifted or shared in 23 countries where reviewed papers emanated include communicable diseases (HIV/AIDS and tuberculosis), NCD (hypertension, diabetes, mental health, and eyecare), maternal and child health, sexual and reproductive health, surgical care, medicines’ management, and emergency care. In addition to these conditions and health services being those contributing to the burden of morbidity and mortality in Africa [90,91], some of these areas, especially HIV/AIDS, tuberculosis, maternal and child health, sexual and reproductive health, and medicines’ management, have received substantive investments from donors and partners in recent years. Perhaps, this investment promoted the task shifting and task sharing practices that were published in the reviewed studies across all levels of the health system, considering most of the studies were funded by projects.
4.1. Implications for Policy and Practice
The health system in Africa will likely continue to be faced with a shortage of health workers until urgent steps are taken. The aim should be to urgently strengthen the health system to become adequately resilient [92] and ensure universal access to qualified, skilled, and motivated health workers that are equitably distributed [93]. Until this is achieved, the persistent health worker shortages call for policies aimed at ensuring that adequate numbers of qualified, skilled, and motivated health workers are available to deliver quality health services at all levels of the system in Africa, based on population health needs. Achieving this also requires apposite contextual policies and interventions to attract and retain health workers, with emphasis given to rural and remote areas.
Task shifting and task sharing implementation to optimally utilize existing health workers or expand service delivery using cadres whose primary function differs should be implemented based on contextual needs. Furthermore, evidence from a needs assessment on scope and competencies should be documented [27] and used to inform the capacity building and the provision of necessary job aids [45,72]. These are pertinent in ensuring quality service delivery.
4.2. Limitations
The findings should not be considered to provide a complete view of the rationale and scope for task shifting and task sharing in Africa, as this review was based on peer-reviewed literature that met a set of criteria. There is a possibility that there are ongoing practices that either are not published in the peer-reviewed literature or did not meet the inclusion criteria for this review. Additionally, in alignment with the scoping review methodology, we did not critically appraise the evidence provided in this paper. We may have also missed out on task shifting and task sharing practices not published in English. Lastly, although we rigorously searched three databases, we may have missed out on studies that are available in other databases.
5. Conclusions
Task shifting and task sharing are widely implemented in Africa across various health services contexts, aimed towards ensuring access to health services. To guide its implementation, populations’ needs should be used to inform the capacity building of beneficiary cadres to ensure that they have the required knowledge, skills, competence, and job aids to guarantee quality service delivery.
Appendix A
Table A1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-SCR) Checklist.
| Section | Item | Prisma-ScR Checklist Item | Reported on Page # |
|---|---|---|---|
| TITLE | |||
| Title | 1 | Identify the report as a scoping review. | 1 |
| ABSTRACT | |||
| Structured summary | 2 | Provide a structured summary that includes (as applicable): background, objectives, eligibility criteria, sources of evidence, charting methods, results, and conclusions that relate to the review questions and objectives. | 1 |
| INTRODUCTION | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. Explain why the review questions/objectives lend themselves to a scoping review approach. | 2, 3 |
| Objectives | 4 | Provide an explicit statement of the questions and objectives being addressed with reference to their key elements (e.g., population or participants, concepts, and context) or other relevant key elements used to conceptualize the review questions and/or objectives. | 3 |
| METHODS | |||
| Protocol and registration | 5 | Indicate whether a review protocol exists, state if and where it can be accessed (e.g., a Web address), and if available, provide registration information, including the registration number. | - |
| Eligibility criteria | 6 | Specify characteristics of the sources of evidence used as eligibility criteria (e.g., years considered, language, and publication status), and provide a rationale. | 4 |
| Information sources | 7 | Describe all information sources in the search (e.g., databases with dates of coverage and contact with authors to identify additional sources), as well as the date the most recent search was executed. | 4 |
| Search | 8 | Present the full electronic search strategy for at least 1 database, including any limits used, such that it could be repeated. | 3 |
| Selection of sources of Evidence |
9 | State the process for selecting sources of evidence (i.e., screening and eligibility) included in the scoping review. | 4 |
| Data charting process | 10 | Describe the methods of charting data from the included sources of evidence (e.g., calibrated forms or forms that have been tested by the team before their use, and whether data charting was done independently or in duplicate) and any processes for obtaining and confirming data from investigators. | 4 |
| Data items | 11 | List and define all variables for which data were sought and any assumptions and simplifications made. | 3 |
| Critical appraisal of individual sources of evidence |
12 | If done, provide a rationale for conducting a critical appraisal of included sources of evidence. Describe the methods used and how this information was used in any data synthesis (if appropriate). | - |
| Synthesis of results | 13 | Describe the methods of handling and summarizing the data that were charted. | 4, 5 |
Author Contributions
Conception and design of the work, S.C.O. and C.D.C.; data collection, S.C.O. and C.D.C.; data analysis and interpretation, S.C.O. and C.D.C.; drafting the article, S.C.O.; critical revision of the article, C.D.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of North-West University Health Research Ethics Committee (NWU-00099-22-A1, 31 August 2022).
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.World Health Organization . WHO Recommendations: Optimizing Health Worker Roles to Improve Access to Key Maternal and Newborn Health Interventions through Task Shifting. World Health Organization; Geneva, Switzerland: 2012. [PubMed] [Google Scholar]
- 2.World Health Organization . Task Shifting: Rational Redistribution of Tasks among health Workforce Teams: Global Recommendations and Guidelines. World Health Organization; Geneva, Switzerland: 2007. [Google Scholar]
- 3.Orkin A.M., Rao S., Venugopal J., Kithulegoda N., Wegier P., Ritchie S.D., Vanderburgh D., Martiniuk A., Salamanca-Buentello F., Upshur R. Conceptual framework for task shifting and task sharing: An international Delphi study. Hum. Resour. Health. 2021;19:61. doi: 10.1186/s12960-021-00605-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . The State of the Health Workforce in the WHO African Region. World Health Organization; Brazzaville, Congo: 2021. [Google Scholar]
- 5.World Health Organization . The State of Health in the WHO African Region: An Analysis of the Status of Health, Health Services and Health Systems in the Context of the Sustainable Development Goals. World Health Organization; Brazzaville, Congo: 2018. [Google Scholar]
- 6.World Health Organization . Road Map for Scaling up the Human Resources for Health for Improved Health Service Delivery in the African Region 2012–2025: Adopted by the Sixty-Second Session of the Regional Committee. World Health Organization; Brazzaville, Congo: 2013. [Google Scholar]
- 7.World Health Organization . Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes: WHO’s Framework for Action. World Health Organization; Geneva, Switzerland: Brazzaville, Congo: 2007. [Google Scholar]
- 8.World Health Organization . The World Health Report 2006—Working Together for Health. World Health Organization; Geneva, Switzerland: 2006. [Google Scholar]
- 9.Russo G., Xu L., McIsaac M., Matsika-Claquin M.D., Dhillon I., Mcpake B., Campbell J. Health workers’ strikes in low-income countries: The available evidence. Bull. World Health Organ. 2019;97:460. doi: 10.2471/BLT.18.225755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization . Global Strategy on Human Resources for Health: Workforce 2030. World Health Organization; Geneva, Switzerland: 2016. [Google Scholar]
- 11.Esu E.B., Chibuzor M., Aquaisua E., Udoh E., Sam O., Okoroafor S., Ongom M., Effa E., Oyo-Ita A., Meremikwu M. Interventions for improving attraction and retention of health workers in rural and underserved areas: A systematic review of systematic reviews. J. Public Health. 2021;43:i54–i66. doi: 10.1093/pubmed/fdaa235. [DOI] [PubMed] [Google Scholar]
- 12.Orkin A.M., Venugopal J., Curran J.D., Fortune M.K., Mcarthur A., Mew E., Ritchie S.D., Drennan I.R., Exley A., Jamieson R., et al. Emergency care with lay responders in underserved populations: A systematic review. Bull. World Health Organ. 2021;99:514–528H. doi: 10.2471/BLT.20.270249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Federspiel F., Mukhopadhyay S., Milsom P.J., Scott J.W., Riesel J.N., Meara J.G. Global surgical, obstetric, and anesthetic task shifting: A systematic literature review. Surgery. 2018;164:553–558. doi: 10.1016/j.surg.2018.04.024. [DOI] [PubMed] [Google Scholar]
- 14.Zhao Y., Hagel C., Tweheyo R., Sirili N., Gathara D., English M. Task-sharing to support paediatric and child health service delivery in low- and middle-income countries: Current practice and a scoping review of emerging opportunities. Hum. Resour. Health. 2021;19:95. doi: 10.1186/s12960-021-00637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Polus S., Lewin S., Glenton C., Lerberg P.M., Rehfuess E., Gülmezoglu A.M. Optimizing the delivery of contraceptives in low- and middle-income countries through task shifting: A systematic review of effectiveness and safety. Reprod. Health. 2015;12:27. doi: 10.1186/s12978-015-0002-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arksey H., O’Malley L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 17.Colquhoun H.L., Levac D., O’Brien K.K., Straus S., Tricco A.C., Perrier L., Kastner M., Moher D. Scoping reviews: Time for clarity in definition, methods, and reporting. J. Clin. Epidemiol. 2014;67:1291–1294. doi: 10.1016/j.jclinepi.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 18.Cox R., Molineux M., Kendall M., Tanner B., Miller E. Co-produced capability framework for successful patient and staff partnerships in healthcare quality improvement: Results of a scoping review. BMJ Qual. Saf. 2022;31:134–146. doi: 10.1136/bmjqs-2020-012729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Majid U., Gagliardi A. Clarifying the degrees, modes, and muddles of “meaningful” patient engagement in health services planning and designing. Patient Educ. Couns. 2019;102:1581–1589. doi: 10.1016/j.pec.2019.04.006. [DOI] [PubMed] [Google Scholar]
- 20.Tessema G.A., Kinfu Y., Dachew B.A., Tesema A.G., Assefa Y., Alene K.A., Aregay A.F., Ayalew M.B., Bezabhe W.M., Bali A.G., et al. The COVID-19 pandemic and healthcare systems in Africa: A scoping review of preparedness, impact and response. BMJ Glob. Health. 2021;6:e007179. doi: 10.1136/bmjgh-2021-007179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tricco A.C., Lillie E., Zarin W., O’brien K., Colquhoun H., Kastner M., Levac D., NG C., Sharpe J.P., Wilson K. A scoping review on the conduct and reporting of scoping reviews. BMC Med. Res. Methodol. 2016;16:15. doi: 10.1186/s12874-016-0116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bemelmans M., van den Akker T., Ford N., Philips M., Zachariah R., Harries A., Schouten E., Hermann K., Mwagomba B., Massaquoi M. Providing universal access to antiretroviral therapy in Thyolo, Malawi through task shifting and decentralization of HIV/AIDS care. Trop. Med. Int. Health. 2010;15:1413–1420. doi: 10.1111/j.1365-3156.2010.02649.x. [DOI] [PubMed] [Google Scholar]
- 23.De Wet K., Wouters E., Engelbrecht M. Exploring task-shifting practices in antiretroviral treatment facilities in the Free State Province, South Africa. J. Public Health Policy. 2011;32:S94–S101. doi: 10.1057/jphp.2011.30. [DOI] [PubMed] [Google Scholar]
- 24.Ledikwe J.H., Kejelepula M., Maupo K., Sebetso S., Thekiso M., Smith M., Mbayi B., Houghton N., Thankane K., O’Malley G. Evaluation of a well-established task-shifting initiative: The lay counselor cadre in Botswana. PLoS ONE. 2013;8:e61601. doi: 10.1371/journal.pone.0061601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baine S.O., Kasangaki A. A scoping study on task shifting, the case of Uganda. BMC Health Serv. Res. 2014;14:184. doi: 10.1186/1472-6963-14-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mwangala S., Moland K.M., Nkamba H.C., Usonda K.G., Monze M., Musukwa K.K., Fylkesnes K. Task-shifting and quality of HIV testing services: Experiences from a national reference hospital in Zambia. PLoS ONE. 2015;10:e0143075. doi: 10.1371/journal.pone.0143075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chamberlain S., Stolz U., Dreifuss B., Elson S.W., Hammerstedt H., Andinda J., Maling S., Bisanzo M. Mortality related to acute illness and injury in rural Uganda: Task shifting to improve outcomes. PLoS ONE. 2015;10:e0122559. doi: 10.1371/journal.pone.0122559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Charyeva Z., Oguntunde O., Orobaton N., Otolorin E., Inuwa F., Alalade O., Abegunde D. Task shifting provision of contraceptive implants to community health extension workers: Results of operations research in northern Nigeria. Glob. Health Sci. Pract. 2015;3:382–394. doi: 10.9745/GHSP-D-15-00129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Landes M., Thompson C., Mwinjiwa E., Thaulo E., Gondwe C., Akello H., Chan A.K. Task shifting of triage to peer expert informal care providers at a tertiary referral HIV clinic in Malawi: A cross-sectional operational evaluation. BMC Health Serv. Res. 2017;17:341. doi: 10.1186/s12913-017-2291-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Okyere E., Mwanri L., Ward P. Is task-shifting a solution to the health workers’ shortage in Northern Ghana? PLoS ONE. 2017;12:e0174631. doi: 10.1371/journal.pone.0174631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lulebo A.M., Kaba D.K., Atake S.E.-H., Mapatano M.A., Mafuta E.M., Mampunza J.M., Coppieters Y. Task shifting in the management of hypertension in Kinshasa, Democratic Republic of Congo: A cross-sectional study. BMC Health Serv. Res. 2017;17:67–73. doi: 10.1186/s12913-017-2645-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Naikoba S., Senjovu K.D., Mugabe P., Mccarthy C.F., Riley P.L., Kadengye D.T., Dalal S. Improved HIV and TB knowledge and competence among mid-level providers in a cluster-randomized trial of one-on-one mentorship for task shifting. JAIDS J. Acquir. Immune Defic. Syndr. 2017;75:e120–e127. doi: 10.1097/QAI.0000000000001378. [DOI] [PubMed] [Google Scholar]
- 33.Millogo T., Kouanda S., Tran N.T., Kaboré B., Keita N., Ouedraogo L., Tall F., Kiarie J., Thatte N., Festin M. Task sharing for family planning services, Burkina Faso. Bull. World Health Organ. 2019;97:783. doi: 10.2471/BLT.19.230276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gbagbo F., Morhe E. Increasing access to intrauterine contraceptive device uptake in Ghana: Stakeholders views on task sharing service delivery with community health nurses. Ghana Med. J. 2020;54:114–120. doi: 10.4314/gmj.v54i2.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peresu E., Heunis J.C., Kigozi N.G., De Graeve D. Task-shifting directly observed treatment and multidrug-resistant tuberculosis injection administration to lay health workers: Stakeholder perceptions in rural Eswatini. Hum. Resour. Health. 2020;18:1–12. doi: 10.1186/s12960-020-00541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lund C., Schneider M., Garman E.C., Avies T., Munodawafa M., Honikman S., Bhana A., Bass J., Bolton P., Dewey M. Task-sharing of psychological treatment for antenatal depression in Khayelitsha, South Africa: Effects on antenatal and postnatal outcomes in an individual randomised controlled trial. Behav. Res. Ther. 2020;130:103466. doi: 10.1016/j.brat.2019.103466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sevene E., Boene H., Vidler M., Valá A., Macuacua S., Augusto O., Fernandes Q., Bique C., Macete E., Sidat M. Feasibility of task-sharing with community health workers for the identification, emergency management and referral of women with pre-eclampsia, in Mozambique. Reprod. Health. 2021;18:145. doi: 10.1186/s12978-021-01192-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boullé C., Kouanfack C., Laborde-Balen G., Carrieri M.P., Dontsop M., Boyer S., Aghokeng A.F., Spire B., Koulla-Shiro S., Delaporte E. Task shifting HIV care in rural district hospitals in Cameroon: Evidence of comparable antiretroviral treatment-related outcomes between nurses and physicians in the Stratall ANRS/ESTHER trial. J. Acquir. Immune Defic. Syndr. 2013;62:569–576. doi: 10.1097/QAI.0b013e318285f7b6. [DOI] [PubMed] [Google Scholar]
- 39.Paul M., Gemzell-Danielsson K., Kiggundu C., Kiggundu C., Namugenyi R., Klingberg-Allvin M. Barriers and facilitators in the provision of post-abortion care at district level in central Uganda–a qualitative study focusing on task sharing between physicians and midwives. BMC Health Serv. Res. 2014;14:28. doi: 10.1186/1472-6963-14-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.O’Malley G., Asrat L., Sharma A., Hamunime N., Stephanus Y., Brandt L., Ali D., Kaindjee-Tjituka F., Natanael S., Gweshe J. Nurse task shifting for antiretroviral treatment services in Namibia: Implementation research to move evidence into action. PLoS ONE. 2014;9:e92014. doi: 10.1371/journal.pone.0092014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Suzan-Monti M., Blanche J., Boyer S., Kouanfack C., Delaporte E., Bonono R.C., Carrieri P., Protopopescu C., Laurent C., Spire B. Benefits of task-shifting HIV care to nurses in terms of health-related quality of life in patients initiating antiretroviral therapy in rural district hospitals in C ameroon [Stratall Agence Nationale de Recherche sur le SIDA (ANRS) 12110/Ensemble pour une Solidarité Thérapeutique Hospitalière en Réseau (ESTHER) substudy] HIV Med. 2015;16:307–318. doi: 10.1111/hiv.12213. [DOI] [PubMed] [Google Scholar]
- 42.Farley J.E., Ndjeka N., Kelly A.M., Whitehouse E., Lachman S., Budhathoki C., Lowensen K., Bergren E., Mabuza H., Mlandu N. Evaluation of a nurse practitioner-physician task-sharing model for multidrug-resistant tuberculosis in South Africa. PLoS ONE. 2017;12:e0182780. doi: 10.1371/journal.pone.0182780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tariku Y., Gerum T., Mekonen M., Takele H. Surgical task shifting helps reduce neonatal mortality in Ethiopia: A retrospective cohort study. Surg. Res. Pract. 2019;2019:5367068. doi: 10.1155/2019/5367068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tweya H., Feldacker C., Ben-Smith A., Eigel R., Boxshall M., Phiri S., Jahn A. ‘Task shifting’ in an antiretroviral clinic in Malawi: Can health surveillance assistants manage patients safely? Public Health Action. 2012;2:178–180. doi: 10.5588/pha.12.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Some D., Edwards J.K., Reid T., Van Den Bergh R., Kosgei R.J., Wilkinson E., Baruani B., Kizito W., Khabala K., Shah S. Task shifting the management of non-communicable diseases to nurses in Kibera, Kenya: Does it work? PLoS ONE. 2016;11:e0145634. doi: 10.1371/journal.pone.0145634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Davis D.N., Lemani C., Kamtuwanje N., Phiri B., Masepuka P., Kuchawo S., Bhushan N.L., Tang J.H. Task shifting levonorgestrel implant insertion to community midwife assistants in Malawi: Results from a non-inferiority evaluation. Contracept. Reprod. Med. 2018;3:24. doi: 10.1186/s40834-018-0077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Galukande M., Kaggwa S., Sekimpi P., Kakaire O., Katamba A., Munabi I., Runumi F.M., Mills E., Hagopian A., Blair G. Use of surgical task shifting to scale up essential surgical services: A feasibility analysis at facility level in Uganda. BMC Health Serv. Res. 2013;13:292. doi: 10.1186/1472-6963-13-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bolkan H.A., Van Duinen A., Waalewijn B., Elhassein M., Kamara T., Deen G., Bundu I., Ystgaard B., Von Schreeb J., Wibe A. Safety, productivity and predicted contribution of a surgical task-sharing programme in Sierra Leone. J. Br. Surg. 2017;104:1315–1326. doi: 10.1002/bjs.10552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wiedenmayer K.A., Kapologwe N., Charles J., Chilunda F., Mapunjo S. The reality of task shifting in medicines management-a case study from Tanzania. J. Pharm. Policy Pract. 2015;8:13. doi: 10.1186/s40545-015-0032-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Agyapong V.I., Osei A., Farren C.K., Mcauliffe E. Task shifting–Ghana’s community mental health workers’ experiences and perceptions of their roles and scope of practice. Glob. Health Action. 2015;8:28955. doi: 10.3402/gha.v8.28955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dos Santos P.F., Wainberg M.L., Caldas-de-Almeida J.M., Saraceno B., Mari J.D.J. Overview of the mental health system in Mozambique: Addressing the treatment gap with a task-shifting strategy in primary care. Int. J. Ment. Health Syst. 2016;10:1–9. doi: 10.1186/s13033-015-0032-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Agyapong V.I.O., Farren C., McAuliffe E. Improving Ghana’s mental healthcare through task-shifting-psychiatrists and health policy directors perceptions about government’s commitment and the role of community mental health workers. Glob. Health. 2016;12:57. doi: 10.1186/s12992-016-0199-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Agyapong V.I., Osei A., Mcloughlin D.M., Mcauliffe E. Task shifting—Perception of stake holders about adequacy of training and supervision for community mental health workers in Ghana. Health Policy Plan. 2016;31:645–655. doi: 10.1093/heapol/czv114. [DOI] [PubMed] [Google Scholar]
- 54.Sayed S., Field A., Rajab J., Mutuiri A., Githanga J., Mungania M., Okinda N., Moloo Z., Abdillah A., Ayara B. Task sharing and shifting to provide pathology diagnostic services: The Kenya fine-needle aspiration biopsy cytology and bone marrow aspiration and trephine biopsy training program. J. Glob. Oncol. 2018;4:1–11. doi: 10.1200/JGO.18.00094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gessessew A., Barnabas G.A., Prata N., Weidert K. Task shifting and sharing in Tigray, Ethiopia, to achieve comprehensive emergency obstetric care. Int. J. Gynaecol. Obs. 2011;113:28–31. doi: 10.1016/j.ijgo.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 56.Awolude O.A., Oyerinde S.O., Akinyemi J.O. Screen and triage by community extension workers to facilitate screen and treat: Task-sharing strategy to achieve universal coverage for cervical cancer screening in Nigeria. J. Glob. Oncol. 2018;4:1–10. doi: 10.1200/JGO.18.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dambisya Y.M., Matinhure S. Policy and programmatic implications of task shifting in Uganda: A case study. BMC Health Serv. Res. 2012;12:61. doi: 10.1186/1472-6963-12-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kiweewa F.M., Wabwire D., Nakibuuka J., Mubiru M., Bagenda D., Musoke P., Fowler M.G., Antelman G. Noninferiority of a task-shifting HIV care and treatment model using peer counselors and nurses among Ugandan women initiated on ART: Evidence from a randomized trial. J. Acquir. Immune Defic. Syndr. 2013;63:e125–e132. doi: 10.1097/QAI.0b013e3182987ce6. [DOI] [PubMed] [Google Scholar]
- 59.Jennings L., Yebadokpo A.S., Affo J., Agbogbe M., Tankoano A. Task shifting in maternal and newborn care: A non-inferiority study examining delegation of antenatal counseling to lay nurse aides supported by job aids in Benin. Implement Sci. 2011;6:2. doi: 10.1186/1748-5908-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kosgei R.J., Wools-Kaloustian K.K., Braitstein P., Sidle J., Sang E., Gitau J., Sitienei J., Owino R., Mamlin J., Kimaiyo S. Task shifting in HIV clinics, Western Kenya. East Afr. Med. J. 2010;87:299–303. [PubMed] [Google Scholar]
- 61.Umar N.A., Hajara M.J., Khalifa M. Reduction of client waiting time using task shifting in an anti-retroviral clinic at Specialist Hospital Bauchi, Nigeria. J. Public Health Afr. 2011;2:e2. doi: 10.4081/jphia.2011.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Born L.J., Wamulume C., Neroda K.A., Quiterio N., Giganti M.J., Morris M., Bolton-Moore C., Baird S., Sinkamba M., Topp S.M., et al. Evaluation of a Task-Shifting Strategy Involving Peer Educators in HIV Care and Treatment Clinics in Lusaka, Zambia. J. Public Health Afr. 2012;3:e3. doi: 10.4081/jphia.2012.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Naburi H., Ekström A.M., Mujinja P., Kilewo C., Manji K., Biberfeld G., Sando D., Chalamila G., Bärnighausen T. The potential of task-shifting in scaling up services for prevention of mother-to-child transmission of HIV: A time and motion study in Dar es Salaam, Tanzania. Hum. Resour. Health. 2017;15:35. doi: 10.1186/s12960-017-0207-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Marotta C., Giaquinto C., Di Gennaro F., Chhaganlal K.D., Saracino A., Moiane J., Maringhini G., Pizzol D., Putoto G., Monno L. Pathways of care for HIV infected children in Beira, Mozambique: Pre-post intervention study to assess impact of task shifting. BMC Public Health. 2018;18:703. doi: 10.1186/s12889-018-5646-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Labhardt N.D., Balo J.R., Ndam M., Grimm J.J., Manga E. Task shifting to non-physician clinicians for integrated management of hypertension and diabetes in rural Cameroon: A programme assessment at two years. BMC Health Serv. Res. 2010;10:339. doi: 10.1186/1472-6963-10-339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hoke T.H., Wheeler S.B., Lynd K., Green M.S., Razafindravony B.H., Rasamihajamanana E., Blumenthal P.D. Community-based provision of injectable contraceptives in Madagascar: ‘task shifting’ to expand access to injectable contraceptives. Health Policy Plan. 2012;27:52–59. doi: 10.1093/heapol/czr003. [DOI] [PubMed] [Google Scholar]
- 67.Wright J., Chiwandira C. Building capacity for community mental health care in rural Malawi: Findings from a district-wide task-sharing intervention with village-based health workers. Int. J. Soc. Psychiatry. 2016;62:589–596. doi: 10.1177/0020764016657112. [DOI] [PubMed] [Google Scholar]
- 68.Gyamfi J., Plange-Rhule J., Iwelunmor J., Lee D., Blackstone S.R., Mitchell A., Ntim M., Apusiga K., Tayo B., Yeboah-Awudzi K. Training nurses in task-shifting strategies for the management and control of hypertension in Ghana: A mixed-methods study. BMC Health Serv. Res. 2017;17:104. doi: 10.1186/s12913-017-2026-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tilahun Y., Lew C., Belayihun B., Hagos K.L., Asnake M. Improving contraceptive access, use, and method mix by task sharing Implanon insertion to frontline health workers: The experience of the Integrated Family Health Program in Ethiopia. Glob. Health Sci. Pract. 2017;5:592–602. doi: 10.9745/GHSP-D-17-00215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gueye B., Wesson J., Koumtingue D., Stratton S., Viadro C., Talla H., Dioh E., Cissé C., Sebikali B., Daff B.M. Mentoring, task sharing, and community outreach through the TutoratPlus approach: Increasing use of long-acting reversible contraceptives in Senegal. Glob. Health Sci. Pract. 2016;4:S33–S43. doi: 10.9745/GHSP-D-15-00328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mafigiri D.K., McGrath J.W., Whalen C.C. Task shifting for tuberculosis control: A qualitative study of community-based directly observed therapy in urban Uganda. Glob. Public Health. 2012;7:270–284. doi: 10.1080/17441692.2011.552067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dlamini-Simelane T., Moyer E. Task shifting or shifting care practices? The impact of task shifting on patients’ experiences and health care arrangements in Swaziland. BMC Health Serv. Res. 2017;17:20. doi: 10.1186/s12913-016-1960-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kaindjee-Tjituka F., Sawadogo S., Lowrance D., Maher A., Salomo N., Mutandi G., Mbapaha C., Neo M., Beukes A., Gweshe J. Task-shifting point-of-care CD4+ testing to lay health workers in HIV care and treatment services in Namibia. Afr. J. Lab. Med. 2017;6:1–5. doi: 10.4102/ajlm.v6i1.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wall J.T., Kaiser B.N., Friis-Healy E.A., Ayuku D., Puffer E.S. What about lay counselors’ experiences of task-shifting mental health interventions? Example from a family-based intervention in Kenya. Int. J. Ment. Health Syst. 2020;14:1–14. doi: 10.1186/s13033-020-00343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Andriamanjato H.H., Mathenge W., Kalua K., Courtright P., Lewallen S. Task shifting in primary eye care: How sensitive and specific are common signs and symptoms to predict conditions requiring referral to specialist eye personnel? Hum. Resour. Health. 2014;12:S3. doi: 10.1186/1478-4491-12-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Eliah E., Lewallen S., Kalua K., Courtright P., Gichangi M., Bassett K. Task shifting for cataract surgery in eastern Africa: Productivity and attrition of non-physician cataract surgeons in Kenya, Malawi and Tanzania. Hum. Resour. Health. 2014;12:S4. doi: 10.1186/1478-4491-12-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Akeju D.O., Vidler M., Sotunsa J., Osiberu M., Orenuga E., Oladapo O.T., Adepoju A., Qureshi R., Sawchuck D., Adetoro O.O. Human resource constraints and the prospect of task-sharing among community health workers for the detection of early signs of pre-eclampsia in Ogun State, Nigeria. Reprod. Health. 2016;13:115–122. doi: 10.1186/s12978-016-0216-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Asfaw E., Dominis S., Palen J.G., Wong W., Bekele A., Kebede A., Johns B. Patient satisfaction with task shifting of antiretroviral services in Ethiopia: Implications for universal health coverage. Health Policy Plan. 2014;29:ii50–ii58. doi: 10.1093/heapol/czu072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yator O., Kagoya M., Khasakhala L., John-Stewart G., Kumar M. Task-sharing and piloting WHO group interpersonal psychotherapy (IPT-G) for adolescent mothers living with HIV in Nairobi primary health care centers: A process paper. AIDS Care. 2021;33:873–878. doi: 10.1080/09540121.2020.1801981. [DOI] [PubMed] [Google Scholar]
- 80.Selke H.M., Kimaiyo S., Sidle J.E., Vedanthan R., Tierney W.M., Shen C., Denski C.D., Katschke A.R., Wools-Kaloustian K. Task-shifting of antiretroviral delivery from health care workers to persons living with HIV/AIDS: Clinical outcomes of a community-based program in Kenya. J. Acquir. Immune Defic. Syndr. 2010;55:483–490. doi: 10.1097/QAI.0b013e3181eb5edb. [DOI] [PubMed] [Google Scholar]
- 81.Chibanda D., Mesu P., Kajawu L., Cowan F., Araya R., Abas M.A. Problem-solving therapy for depression and common mental disorders in Zimbabwe: Piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV. BMC Public Health. 2011;11:828. doi: 10.1186/1471-2458-11-828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jacobs Y., Myers B., van der Westhuizen C., Brooke-Sumner C., Sorsdahl K. Task sharing or task dumping: Counsellors experiences of delivering a psychosocial intervention for mental health problems in South Africa. Community Ment. Health J. 2021;57:1082–1093. doi: 10.1007/s10597-020-00734-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Boniol M., Kunjumen T., Nair T.S., Siyam A., Campbell J., Diallo K. The global health workforce stock and distribution in 2020 and 2030: A threat to equity and ‘universal’health coverage? BMJ Glob. Health. 2022;7:e009316. doi: 10.1136/bmjgh-2022-009316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.World Health Organization . Health Workforce Requirements for Universal Health Coverage and the Sustainable Development Goals. World Health Organization; Geneva, Switzerland: 2016. Human Resources for Health Observer, 17. [Google Scholar]
- 85.World Health Organization . WHO Guideline on Health Workforce Development, Attraction, Recruitment and Retention in Rural and Remote Areas: Web Annexes. World Health Organization; Geneva, Switzerland: 2021. [PubMed] [Google Scholar]
- 86.Malakoane B., Heunis J.C., Chikobvu P., Kigozi N.G., Kruger W.H. Public health system challenges in the Free State, South Africa: A situation appraisal to inform health system strengthening. BMC Health Serv. Res. 2020;20:58. doi: 10.1186/s12913-019-4862-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ahmat A., Okoroafor S.C., Kazanga I., Asamani J.A., Millogo J.J.S., Illou M.M.A., Mwinga K., Nyoni J. The health workforce status in the WHO African Region: Findings of a cross-sectional study. BMJ Glob. Health. 2022;7:e008317. doi: 10.1136/bmjgh-2021-008317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Okoroafor S., Ahmat A., Osubor M., Nyoni J., Bassey J., Alemu W. Assessing the staffing needs for primary health care centers in Cross River State, Nigeria: A workload indicators of staffing needs study. Hum. Resour. Health. 2022;19:108. doi: 10.1186/s12960-021-00648-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.World Health Organization . Workload Indicators of Staffing Need. World Health Organization; Geneva, Switzerland: 2010. User’s Manual. [Google Scholar]
- 90.Mudie K., Jin M.M., Kendall L., Addo J., Dos-Santos-Silva I., Quint J., Smeeth L., Cook S., Nitsch D., Natamba B. Non-communicable diseases in sub-Saharan Africa: A scoping review of large cohort studies. J. Glob. Health. 2019;9:020409. doi: 10.7189/jogh.09.020409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Vos T., Lim S.S., Abbafati C., Abbas K.M., Abbasi M., Abbasifard M., Abbasi-Kangevari M., Abbastabar H., Abd-Allah F., Abdelalim A. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Nuzzo J.B., Meyer D., Snyder M., Ravi S.J., Lapascu A., Souleles J., Andrada C.I., Bishai D. What makes health systems resilient against infectious disease outbreaks and natural hazards? Results from a scoping review. BMC Public Health. 2019;19:1310. doi: 10.1186/s12889-019-7707-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.World Health Organization . The African Regional Framework for the Implementation of the Global Strategy on Human Resources for Health: Workforce 2030. World Health Organization; Geneva, Switzerland: 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article.