Abstract
Background
Concentration and physical strength are essential for the long duration of hair transplant surgery. Because both the patient and the doctor must maintain certain postures for long periods, the importance of ergonomics cannot be understated.
Aims
To review the devices, instruments, and techniques developed for ergonomic follicular unit excision surgery, to present our experience with various ergonomic modifications, and to evaluate the effectiveness of the related devices, novel concepts, and methods.
Methods
We evaluated the scientific evidence supporting the ideas, methods, devices, and systems to help create a better ergonomic environment, and we investigated how these elements can be fine‐tuned to improve efficiency when performing follicular unit excision graft harvesting.
Results
Through innovative methods, ideas, devices, and instruments, the authors achieved a high‐quality ergonomic environment for performing follicular unit excision.
Conclusion
Follicular unit excision is a widely used technique in hair restoration surgery. However, follicular unit excision is a very laborious and time‐consuming procedure and mandates the best ergonomic conditions for both the surgeon and the patient. Therefore, it is crucial that the physician understands and appropriately adopts the various means and techniques to provide an ergonomic environment.
Keywords: follicle, hair follicles, hair transplant, hair transplantation, hairloss
1. INTRODUCTION
Hair transplant surgery is one of the longest duration surgeries in the field of dermatology and plastic surgery. Furthermore, high‐magnification loupes and microscopes are used to perform micro‐level manipulations and meticulous procedures. As a result, hair surgeons suffer from exhaustion and chronic pain in the neck, shoulders, and wrists. 1 This initiates a vicious cycle in which fatigue and pain disturb not only with the surgeon's concentration but also the surgery quality and results. The operation time consequently lengthens, causing the surgeon to experience even more pain in the neck and the shoulders. 2 Recently, hair transplant surgeries are requiring a higher level of expertise and detailed procedures. After the introduction by Rassman and Bernstein in 2002, follicular unit excision (FUE) has made developmental leaps to FUE megasessions, then to non‐shaven FUE (NS‐FUE), and recently to long‐hair FUE. 3 , 4 , 5 The importance of ergonomics has increased proportionately.
The key to ergonomics in surgery is allowing the surgeon to work in the most anatomical position in a relaxed manner while making only minimal and the most effective movements. In accordance with these concerns and concepts, we report how the authors have applied various intraoperative methods to achieve better ergonomics when performing FUE.
2. VARIOUS POSITIONS IN FUE
There are generally three positions when performing FUE. The first position is during graft punching, with the surgeon sitting beside the patient who is in the prone position. The second position is graft punching at the patient's head with the patient in the prone position. The third position is with the surgeon standing or sitting behind the patient who is in the sitting position. Having the patient in the sitting position is superior to the prone position in terms of the angle and directional alignment, graft centering, and acquiring a better surgical view, even more so in performing NS‐FUE. 5 However, the biggest drawback of the sitting position is when harvesting from donor areas below the occipital protuberance, where the hair exit angle tends to be very acute. In this situation, the patient's neck must be bent during effective harvesting, and maintaining such a posture for a prolonged period can be unbearable or even impossible. 5 , 6
3. MOTORIZED FOREHEAD‐SUPPORTING FUE CHAIR SYSTEM
A motorized forehead‐supporting FUE chair system to firmly fix the patient’s head is very useful. 5 These systems ease the harvesting process and enable the patient to maintain certain postures, such as flexing or tilting the neck. There are three methods of controlling the system: a footswitch for the surgeon, another footswitch for the scrub nurse, and a remote control for the circulating assistant that does not require using sterile gloves. Both the forehead fixture and the chair can be moved forward and backward as well as upward and downward (Figure 1). Using a chair system with forehead support not only easily fixes the head but also allows upward traction. Upward traction of the scalp has numerous merits, one of which is tensing the scalp and erecting the hair follicles to be closer to a vertical angle. 7 , 8 , 9
FIGURE 1.

A motorized forehead‐supporting Follicular Unit Excision chair system
4. TRANSFORMATION (CHAIR TO BED, BED TO CHAIR)
The motorized forehead‐supporting FUE surgical chair system transforms into a surgical bed. The chair is used without the head rest for harvesting with the patient in the sitting position and does not require that the patient move from the chair to a surgical table; the chair system turns into a surgical bed simply by adding the head rest (Figure 2).
FIGURE 2.

Position changes (chair to bed, bed to chair) the apparatus transforms from a chair to a surgical bed, and vice versa. (A). Sitting position for follicular unit excision harvesting. (B). Head‐rest assembly for transformation to a surgical bed. (C). Surgical bed format for graft implantation
5. FINGERTIP TOUCH SENSOR
Until now, the motorized FUE punch machines have mostly been controlled by a foot pedal. With every change in the surgery position or location, the surgeon must realign his/her posture and foot pedal after locating the foot pedal, inevitably looking away from the surgical field. Additionally, when the surgeon is in the sitting position, it is easier to press the foot pedal with most of the weight shifted to the hips (ischium). However, in the standing position, one has to load body weight onto the other foot, shifting the body to one side, leading to physical discomfort in the weight‐bearing lateral ankle, knee, and pelvis. The spine also takes on an abnormal curvature. Maintaining this static posture for prolonged periods exerts stress on the ankles, knees, pelvis, and the spine, resulting in fatigue and joint and muscle pain. A fingertip touch sensor is a good solution to the aforementioned ergonomic problem. This switch provides both stability and accuracy when performing surgery. When the patient is seated with the surgeon standing behind the patient, the sensor allows an ergonomic posture; without having to stand on one foot, the surgeon's weight is evenly divided on both feet, allowing good posture and providing better ergonomics.
Each surgeon has a unique style when performing surgery, and each has different hand sizes, postures, and habits. Therefore, the handpiece must be adjustable to provide balance in each surgeon's hand irrespective of their posture, habits, or hand size. The lever principle is applied to activate the handpiece that we use, which is long and up to 29 mm in length. A nudge anywhere on the button starts the machine by exerting pressure on the rear part of the button, which springs back up owing to its elastic recoil mechanism, enabling reactivation with another soft touch (Figure 3).
FIGURE 3.

Fingertip touch sensor. Fingertip touch sensor: the long extension of the button is convenient as it is activated sensitively by touching anywhere on the rod using the lever principle. For the surgeon using traditional foot pedal switch, standing on one foot induces a non‐ergonomic and unstable posture. Using a fingertip touch switch evenly disperses the surgeon's weight and reduces muscle fatigue
Despite the scientific and ergonomic design of the fingertip sensor, a foot pedal can be alternatively chosen if muscle and joint fatigue presents in the fingers. Both the fingertip sensor and the foot pedal or either can be selectively switched on depending on the patient's position and the location of the recipient site. For instance, the foot pedal is superior to the fingertip sensor when harvesting from the beard.
6. 360° ULTRATHIN FOOT PEDAL
A footswitch is usually used when harvesting with a motorized FUE punching machine. The authors used a three‐dimensional (3D) scanner to manufacture a foot pedal switch that is ultrathin compared with conventional foot pedals. Additionally, the foot pedal is round in design, with no sides, to eliminate having to check the foot position on the pedal with each use (Figure 4). When harvesting at the patient's back, a foot pedal that is too thick and high and requires that the surgeon flex their ankle to a higher degree, inevitably necessitates putting more weight on the opposite leg. The waist is also bent, and it is not easy to maintain this posture for long periods (Figure 5). Eventually, this posture strains the back, hips, knees, and ankles.
FIGURE 4.
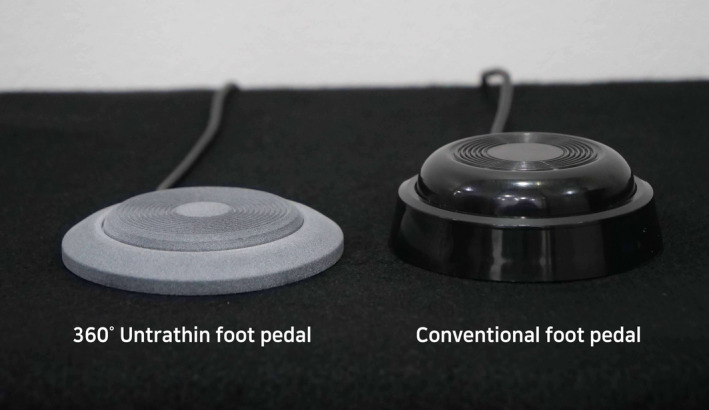
360° ultrathin foot pedal versus a conventional foot pedal. The ultrathin foot pedal minimizes musculoskeletal pain in the ankle and the knees. The foot pedal is activated by pressing anywhere over a full 360 degrees
FIGURE 5.

Dissecting the donor grafts with the patient in surgeon on standing position. (A). Using a traditional foot pedal with a substantial height. (B). Ergonomic improvement using a 360° ultrathin foot pedal
7. BLUETOOTH‐BASED FUE PUNCHING MACHINE
Currently, most of the motorized FUE machines operated by a main control box are available. However, there is no main hardware control body for the FUE punch device that we use; a tablet PC is all that is required. By downloading an application, every function of the FUE punch is controlled via Bluetooth connections. More delicate and complicated software programming is possible, and it is also possible to upgrade functions using only software upgrades without having to replace the device or purchase additional equipment. The device is also easy to carry and repair.
8. MAGNIFYING LOUPE
The patient is positioned in the sitting position for FUE punching and in the supine position for graft placement. Having the patient in a sitting position is beneficial for aligning the surgeon's eyes with the punch tip and the target graft for accurate excision, similar to the aiming technique when shooting a shotgun. In contrast, when the patient is in the supine position for the graft placement process, the surgical field is located lower than the surgeon's eye level. Therefore, when harvesting the donor hair under magnifying loupes, the surgeon's neck is bent backward, which tenses the neck and causes neck and shoulder pain (Figure 6). If one lowers the height of the chair in an attempt to alleviate the pain, the surgical field and the surgeon's hands are now located noticeably below eye level. It is then difficult to read the hair exit angle and direction and increases the risk of follicular injury. As a solution, the authors alternately use two different loupes, one for harvesting and one for graft placement; both loupes provide 5.5× magnification. Lenses are customized to be attached at different angles to ease the working posture, with the ultimate purpose of reducing neck and shoulder pain. Generally, the angle at which the oculars are placed in the frame is approximately 33–34 degrees. The loupes that the authors use for graft placement (with the patient in the supine position) have a similar declination angle. However, during harvesting (with the patient in the sitting position) we use custom‐made loupes that provide approximately 23 more degrees in the horizontal angle at which the oculars are attached to the frame.
FIGURE 6.

Magnifying loupe. (A). Loupes customized to provide a more horizontal declination angle vs. loupes with a larger declination angle. (B). Graft harvesting using conventional magnifying loupes. With the patient in the sitting position, the surgeon may feel discomfort in the neck from tilting back. (C). Using loupes with a reduced declination angle for graft harvesting allows an ergonomic neck posture
9. MICROSCOPIC GRAFT INSPECTION AND DISSECTION
A very high definition (HD) microscope with high magnification is connected to a full HD monitor (Figure 7). Binocular microscopes are not used because they lower efficiency from maintaining a fixed position for long periods. When preparing grafts, curved forceps are held in one hand and a #20 scalpel blade is held in the other hand (Figure 8). Slivering boards made of birch wood are used for their durability and firmness, and these measure 5.5 × 8.3 cm in width and length and 1.3 cm in height. These dimensions have been derived after many years of adjustment. Thicker, slimmer, or smaller boards cause the assistants discomfort.
FIGURE 7.

Graft preparation using a high‐magnifying microscope connected to a full HD monitor
FIGURE 8.

Two‐hand dissection on slivering boards made of birch wood
10. ENTERTAINMENT AND GRAFT MONITORING SYSTEM VIA A BLUETOOTH‐CONNECTED MICROSCOPE
The patient can watch a movie, listen to music, or use the internet with a tablet PC during harvesting. The patient can also check the progress of graft preparation by sharing, via Bluetooth, the assistant's screen showing dissecting, trimming, or sorting the grafts. Being able to check the condition of the donor hair in real‐time allows the patient to have more trust in the surgery (Figure 9).
FIGURE 9.
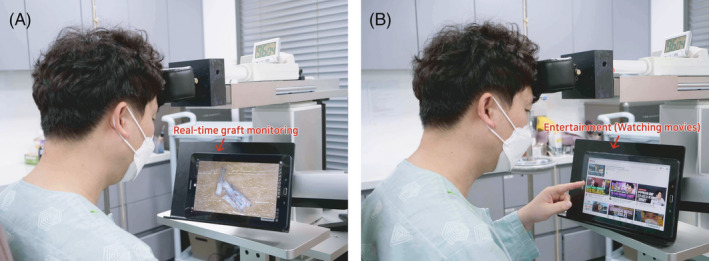
Entertainment and graft monitoring system for the patient. The patient may use a tablet PC to freely check the process of graft dissection by the assistants, or watch a movie. (A) Real‐time graft monitoring. (B) Entertainment (watching movies)
11. IMPLANTATION SYSTEM
We use sharp implanters for graft placement, and we follow certain principles during surgery: keeping the surgery time as short as possible and making the inserting movements as relaxed as possible. These two efforts minimize graft popping and bleeding, reduce soft tissue trauma, promote circulation recovery, prevent scarring, and increase graft survival rates. These principles also greatly reduce physical stress.
This system requires two to three loaders and one passer. The passer retrieves the implanter immediately after graft placement and hands over an implanter loaded with a graft. 10 the surgeon's hand moves only minimally within a 5‐cm distance, vertically (Figure 10). Both elbows are fixed, which permits only slight movements of the wrist joint. The left hand holds the micro‐forceps, while the right hand holds the implanter. These chairs should not be difficult to purchase as many manufacturers produce surgical chairs of this kind. When there is a dislodged or misplaced graft to be reloaded, it is picked up by the forceps in the left hand and immersed into a bowl with storage solution placed on a chairside table. Here, the elbow of the left arm remains on the elbow rest, and minimal movements are made during the surgery.
FIGURE 10.

Ergonomic graft implantation system. Two to three loaders and a passer form a team. The surgeon's eyes are fixed at the recipient area, and the graft placing process is efficiently performed with the hand moving within a 2–3‐cm radius
A soft and easy grip is important. Stiff or tight gripping causes extreme fatigue for the surgeon and prevents smooth and gradual penetration of the skin, causing abrupt and deeper insertions with additional soft tissue trauma.
12. THE SURGEON'S EYES ARE FIXED
The above‐mentioned methods provide the surgeon with excellent eye‐hand coordination, speed, and accuracy; the surgeon's eyes do not leave the surgical field throughout the entire graft insertion process. Expeditious graft transfer not only reduces fatigue for the surgeon, patient, and assistant, but also increases the chances of graft survival.
13. IMPLANTER
The authors use sharp implanters for graft insertion to accurately and swiftly transfer donor grafts and to accomplish a high density. High magnification loupes are used to readily recognize the size and the bevel face of the implanter and to make only minimal movements to reduce soft tissue damage or graft popping. Rainbow™ implanters (Seson Medical Company, Seoul, Korea) are specifically designed for this purpose. The device has numerous break‐lines at the body that allow for a soft and light grip. The black line and the round protruding structure on the body are aligned with the bevel, allowing the surgeon and the assistant to read the direction of the bevel tip with touch, only (Figure 11).
FIGURE 11.
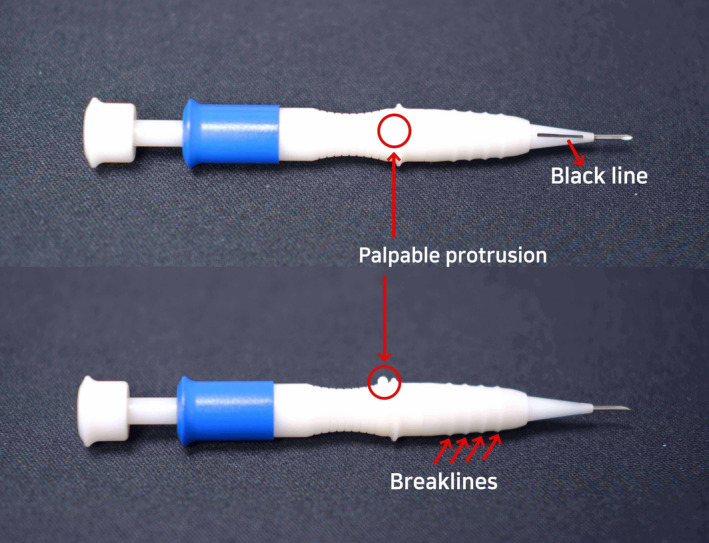
Ergonomic design of the Rainbow™ implanter. Numerous break‐lines on the body of the implanter make a soft and light grip feasible. The black line and the round protruding structure on the body are aligned with the bevel, which allow the surgeon and the assistant to read the direction of the bevel tip using only touch
14. SATISFACTION SURVEY
We asked 10 hair surgeons who had applied the ergonomic concepts, instruments, and devices described in this paper for more than 6 months on the degree of symptom improvement and satisfaction. Hair transplant surgery experience ranged from 2 to 17 years at most with an average of 7.6 years.
Prior to application, a questionnaire was conducted about the area and degree of discomfort and pain, as well as improvement of symptoms and satisfaction after application. Severity of symptoms was described as 0 (none), 1 (mild), 2 (moderate), and 3 (severe) using the Likert Scale (Table 1).
TABLE 1.
Frequency and severity of symptoms by region before ergonomic improvement (duplicate selection allowed)
| Area of discomfort | Frequency number | Severity (average score) |
|---|---|---|
| Neck | 9 | 2.2 |
| Shoulder | 10 | 2.6 |
| Back | 5 | 2.1 |
| Pelvis | 1 | 1 |
| Knee | 2 | 1 |
| Ankle | 3 | 1.5 |
| Wrist | 5 | 1.8 |
| Elbow | 4 | 1.6 |
| Overall discomfort and pain | 10 | 2.3 |
The surgeon scored the results in terms of degree of symptom improvement and subjective satisfaction using a 5‐point Likert scale (1 point, very dissatisfied; 2 points, dissatisfied; 3 points, neither satisfied nor dissatisfied; 4 points, satisfied; and 5 points, very satisfied).
All surgeons experienced significant improvement in musculoskeletal discomfort and pain and described that the surgical procedure became very comfortable. The mean satisfaction score was 4.8. Symptom improvement by region and overall satisfaction were very high (Table 2).
TABLE 2.
Frequency and severity of symptoms by region after ergonomic improvement (duplicate selection allowed)
| Area of discomfort | Frequency number | Severity (average score) |
|---|---|---|
| Neck | 8 | 1.2 |
| Shoulder | 9 | 1.3 |
| Back | 1 | 1 |
| Pelvis | 0 | – |
| Knee | 0 | – |
| Ankle | 0 | – |
| Wrist | 3 | 1.3 |
| Elbow | 2 | 1 |
| Overall discomfort and pain | 10 | 1.1 |
In particular, improvement of symptoms in the neck and shoulder was evident, and pain or discomfort was greatly reduced overall.
However, the number of surgeons who fully applied this system, equipment, and ergonomic concept was small, so only 10 surgeons were surveyed. It is thought that further research with more surgeons will be helpful in the future.
15. CONCLUSION
In this study, multiple methods of achieving the best ergonomics throughout FUE surgery effectively raised efficiency and reduced the degree of fatigue for both the surgeon and the patient.
ETHICAL STATEMENT
All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki (as was revised in 2013). All patients provided informed consent for the case details and images to be published in this report.
CONFLICT OF INTEREST
Dr. J.H. Park has patents and ownership interest of Seson medical company. For the remaining authors, none were declared. No funding was received for this article.
ACKNOWLEDGMENTS
We thank Jane Charbonneau, DVM, from Edanz Group (https://en‐author‐services.edanz.com/ac) for editing a draft of this manuscript.
Park JH, Kim NR, Manonukul K. Ergonomics in follicular unit excision surgery. J Cosmet Dermatol. 2022;21:2146–2152. 10.1111/jocd.14376
DATA AVAILABILITY STATEMENT
In addition to photographic evidence showing interval changes that appear in the manuscript, complete medical records of the presented cases are stored in the treating clinic, in line with the standard of care.
REFERENCES
- 1. Williams KL Jr, Gupta AK, Schultz H. Ergonomics in hair restoration surgeons. J Cosmet Dermatol. 2016;15(1):66‐71. doi: 10.1111/jocd.12188. [DOI] [PubMed] [Google Scholar]
- 2. Ahmad M, Mohmand MH. Effect of surgeon's workload on rate of transection during follicular unit excision/extraction (FUE). J Cosmet Dermatol. 2020;19(3):720‐724. doi: 10.1111/jocd.13078. [DOI] [PubMed] [Google Scholar]
- 3. Rassman WR, Bernstein RM. Follicular unit extraction: minimally invasive surgery for hair transplantation. Dermatol Surg. 2002;28(8):720‐728. [DOI] [PubMed] [Google Scholar]
- 4. Park JH, You SH, Kim NR. Nonshaven follicular unit extraction: personal experience. Ann Plast Surg. 2019;82(3):262‐268. doi: 10.1097/SAP.0000000000001679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gupta AK, Bruce A, Trivellini R, et al. Innovations hair restoration surgeons have made to adapt to the challenges of follicular unit excision. J Cosmet Dermatol. 2020;19(8):1883‐1891. doi: 10.1111/jocd.13506. [DOI] [PubMed] [Google Scholar]
- 6. Park JH, You SH, Kim N. Forehead‐supporting chair system for follicular unit extraction hair transplantation. Arch Aesthetic Plast Surg. 2019;25(1):42‐44. [Google Scholar]
- 7. Miao Y, Fan ZX, Jiang W, Hu ZQ. Patient in the sitting position to improve comfort in follicular unit extraction. Plast Reconstr Surg Glob Open. 2016;4(11):e1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rose PT, Canales M, Zontos M. Examination of the exit angle of hair at the skin surface versus the internal angle of hair as it relates to the FUE/FIT harvesting method. Hair Forum Int'l. 2017;27(1):8‐10. [Google Scholar]
- 9. Zontos G, Williams KL Jr, Nikiforidis G. Minimizing injury to the donor area in follicular unit extraction (FUE) harvesting. J Cosmet Dermatol. 2017;16(1):61‐69. [DOI] [PubMed] [Google Scholar]
- 10. Park JH. Novel Implanter technique that enables more than 1,600 grafts in 1 hour with dense packing. ISHRS Video. Library. 2013.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
In addition to photographic evidence showing interval changes that appear in the manuscript, complete medical records of the presented cases are stored in the treating clinic, in line with the standard of care.


