Abstract
Introduction and importance
Anorectal malformation is associated with congenital anomalies affecting other body systems, including vertebral, anorectal, cardiac, tracheoesophageal, renal and limb defects. Mayer-Rokitansky-Küster-Hauser syndrome is a collection of several congenital defects in the female reproductive system, including congenital agenesis of the uterus, cervix, and upper two-thirds of the vagina, that could be associated with anorectal malformation.
Case presentation
A 3-year old female initially treated for vestibular fistula as she had only two orifices, who intra-operatively was discovered to have Mayer–Rokitansky–Küster–Hauser syndrome associated with cardiac, skeletal (foot), and anorectal anomalies.
Clinical discussion
The diagnosis Mayer-Rokitansky-Küster-Hauser syndrome should be considered in a female patient presenting with anorectal malformation especially when two orifices are encountered in the perineum. Mayer-Rokitansky-Küster-Hauser syndrome can be associated with vestibular or rectovaginal fistula, of which the former is the most common type that coexists. Treatment involves surgical and nonsurgical approaches, Surgically a new cavity is created to replace the vagina with a mucous membrane lined canal such as a bowel segment.
Conclusion
This case demonstrates that anorectal malformation with Mayer–Rokitansky–Küster–Hauser syndrome can be mistaken for a vestibular fistula, even in specialized centers like ours. Therefore, a high index of suspicion should be noted especially when examination under anesthesia confirms only two orifices in the perinium.
Keywords: Anorectal malformation, Mayer; Rokitansky; Küster; Hauser syndrome
Highlights
-
•
In resource-limited settings evaluation of the associated VACTERL anomalies in Anorectal malformation (ARM) can be a challenge.
-
•
Mayer–Rokitansky–Küster–Hauser syndrome (MRKH) can easily be confused with vestibular or rectovaginal fistula.
-
•
MRKH should be suspected when clinical findings demonstrate two orifices with an absent vagina.
1. Introduction
Anorectal malformation (ARM) is associated with congenital anomalies affecting other body systems including vertebral, anorectal, cardiac, tracheoesophageal, renal and limb defects (VACTERL) [1], [2].
The resources needed to evaluate for these anomalies can be limited in our setting by constrained investigative capabilities in most of our health care facilities, limited pediatric surgeons and unmet surgical needs [3], [4], [5].
The relevance of assessment and identification of associated anomalies in ARM in the first 24 h, especially those that are life threatening such as cardiac defects cannot be underestimated [6]. Once the child is stable particularly in resource-limited settings, less attention maybe paid to these associated VACTERL anomalies. Mayer–Rokitansky–Küster–Hauser syndrome (MRKH) should be evaluated as an associated anomaly with ARM, especially in girls presentsing with two openings in the perineum that are not in the normal position instead of three. Mayer-Rokitansky-Küster-Hauser syndrome can associated with vestibular or rectovaginal fistula, the former being the commonest type that coexists.
MRKH is distinguished by normal female external genitalia with a short, blind-ending vagina, normal ovaries and fallopian tubes and uterus which maybe underdeveloped. Patients are usually seen at puberty with primary amenorrhea or cyclical pain [6]. Additionally, MRKH is associated with other malformations such as renal, skeletal, cardiac and auditory defects.
This case highlights the frequently emphasized importance of history taking and clinical examination of patients to make appropriate diagnosis. It further demonstrates how ARM is often missed even in specialized centre [7], [8], [9].
We present a case of a 3-year old female who presented with two perineal orifices and was initially thought to have a vestibular fistula. However, intraoperatively she was discovered to have MRKH. The case has been reported in line with the SCARE 2020 guidelines [10].
2. Presentation of case
A 3-year-old female presented with a sigmoid colostomy and an unrecognized MRKH syndrome. Colostomy was placed when she was 1 week old after presenting to a peripheral hospital with complaint of passing stool via the vagina. Intra-operatively, she experienced cardiac arrest, cardiopulmonary resuscitation (CPR) was performed and she was transferred to the intensive care unit (ICU). She was managed for post cardiac arrest care in ICU, and referred to investigate the cause of the arrest at the Uganda Heart Institute (UHI) the only specialized cardiac centre for the entire country located in the capital city. Echocardiography at UHI showed partial atrioventricular (AV) canal-common atrium, moderate right atrioventricular valve regurgitation (AVVR) and left superior vena cava (LSVC) with unroofed coronary sinus. After stabilization, with support from a non-governmental organization (NGO) she was ultimately referred for surgery in India at 2-years-2-months of age.
She presented to our centre at 3-years of age for anal repair. She was a well-nourished toddler, weighing 12 kg. Abdominal examination was normal with a well-functioning divided sigmoid colostomy. Her blood work-up was all within normal ranges. She was initially noted on perineal exam to have a vestibular fistula – no recognition of MRKH was made. She also had deformity on the left foot (Fig. 1). A pediatric cardiology review with repeat echocardiography cleared her for surgery.
Fig. 1.
Left foot deformity.
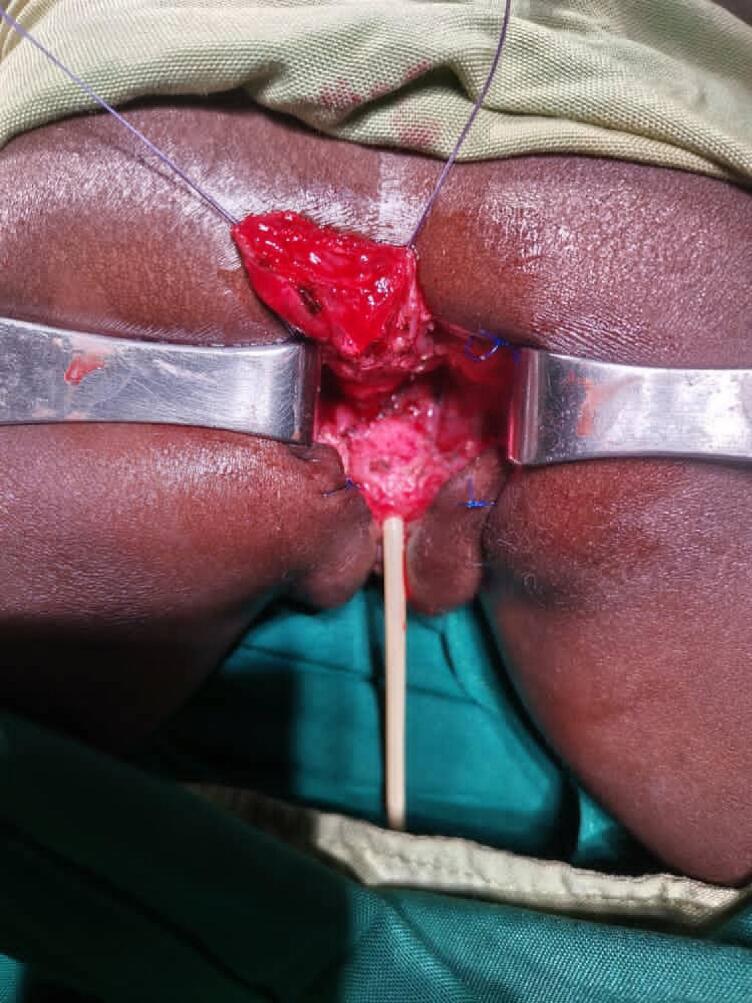
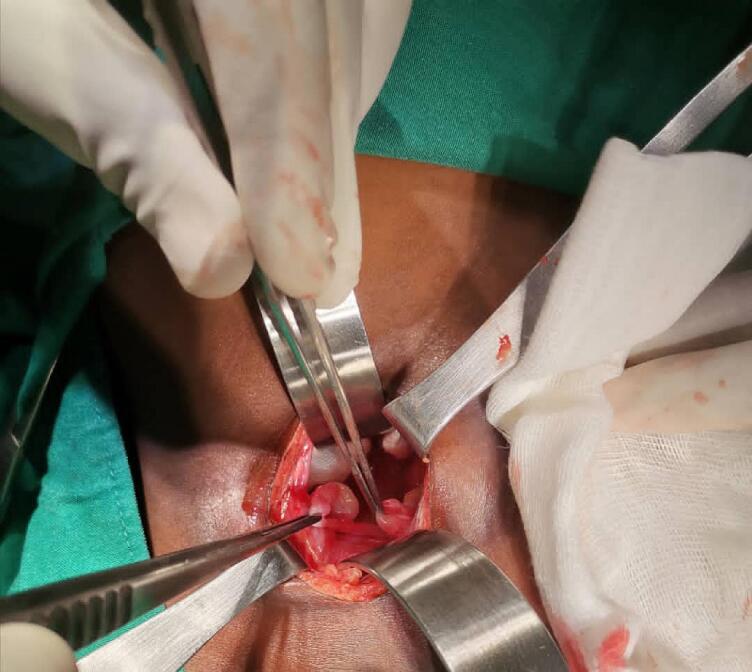
Based on the above findings the team elected to proceed with posterior sagittal anorectoplasty (PSARP). Surgery commenced through a posterior sagittal incision in jerk knife position. Intra operative findings demonstrated two orifices with an absent vagina (Fig. 2). A full abdominal preparation was done, and laparotomy was performed. She was found to have normal kidneys and ovaries, but no uterus (Fig. 3). At this point a diagnosis of MRKHS was made and discussed with the family who agreed to proceed with the PSARP. The PSARP was performed with vaginal reconstruction. The neo-anus was calibrated to 14 mm at the end of repair. After consultation with our adult gynecologist (we do not have pediatric gynecologist) together with a visiting adult gynecologist, given the vaginal agenesis and absent uterus coupled with an already mobilized rectum, the team concluded that the best option was to create a neo-vagina using the distal end of the rectum. Approximately 6 cm of the distal rectum was retained as a neo-vagina, and the proximal rectum was brought down posteriorly within the limits of the sphincter complex marked previously using electrocoagulation (Fig. 2, Fig. 4) to complete the PSARP.
Fig. 2.
Absent vagina, mobilized rectum.
Fig. 3.
Normal ovaries, no uterus.
Fig. 4.
PSARP completed.
She underwent serial anal dilatation according to our ward protocol and achieved anal size for age calibrated at 15 mm Hegar. Six weeks later the colostomy was taken down. She is being followed in the clinic by a multidisciplinary team including pediatric surgeons, cardiologists, gynecologists, orthopedic surgeons and urologists. At her three months follow-up she had normal functional outcome. Her abdominal ultrasound scan showed normal kidneys and her karyotype is XX.
Ethical approval wasn't necessary from our ethical review committee for this case report. The family verbally consented for this publication.
3. Discussion
The diagnosis of MRKH should be considered in a female patient presenting with ARM, especially when two orifices are encountered in the perineum [11]. A careful history and clinical examination should be complete in these children. MRKH can easily be confused with vestibular or rectovaginal fistula, of which the former is the commonest type that coexists with MRKH [12], [13].
MRKH is associated with other malformations such as renal, skeletal, cardiac and auditory defects [14], [15]. Our patient presented with cardiac, skeletal (foot) and anorectal anomalies, with MRKH discovered intra-operatively. MRKH may also present with as hernia uterii ovarii which is presence of the uterus in inguinal hernia [16].
Patients are commonly seen at puberty with primary amenorrhea or cyclical pain [14]. Our patient presented at 3-years of age as a case of ARM with associated cardiac, skeletal (foot) anomalies during anoplasty [17]. This case further illustrates the relevance of assessing other anomalies once a single anomaly is identified.
If MRKH is potentially suspected, the commonly performed investigations are transabdominal ultrasonography and/or Magnetic resonance imaging (MRI) [14]. Ultrasound has the advantage of being readily available and cheap in our setting. In MRKH ultrasound may reveal an absence of the uterus and status of the kidneys. MRI is more sensitive and specific than ultrasonography but this is not readily available and expensive in our setting. MRI usually performed when ultrasonographic findings are equivocal, since failure to identify the uterus or ovaries does necessarily guarantee their absence. Laparoscopy is a good alternative which can be both diagnostic and therapeutic [18]. Our patient didn't have any of these investigations. Additionally laparoscopy could have saved the patient from laparotomy in this case which isn't available at our facility.
Karyotypye evaluation is an important part of MRKH work-up and usually reveals 46, XX [6], [14]. This must be performed for proper assignment of gender, and to direct treatment in cases of disorders of sex differentiation (DSD), that is a multidisciplinary team (MDT) management.
To evaluate for associated anomalies, these patients should undergo spine radiography, cardiac echocardiography, and audiogram. All these were evaluated in our patient by a MDT.
A diagnosis of MRKH syndrome also poses substantial psychosocial stress to the patient and their families. [14], [19]
Treatment for MRKH involves both surgical and nonsurgical approaches. Nonsurgical procedure utilizes regular dilatation using Hegar dilators when the vaginal dimple is deep enough (2–4 cm). Surgical approach employs different techniques with the ultimate goal of creating a new cavity and replacing the vagina with a mucous membrane lined canal such as a segment of bowel [6], [12], [13], [14], [20]. Via posterior sagittal approach we performed vaginal reconstruction and the anoplasty with the neoanus calibrated to 14 mm at the end of repair.
4. Conclusion
This case demonstrates that anorectal malformation with Mayer–Rokitansky–Küster–Hauser syndrome can be mistaken for a vestibular fistula, even in specialized centers like ours. Therefore, a high index of suspicion should be noted especially when examination reveals only two orifices in the perinium.
Consent for publication
Written informed consent was obtained from the patient's legal guardian(s) for publication of this case report and any accompanying images.
Ethical approval
Ethical approval was waived by the authors' institution.
Funding
No external funding.
Author contribution
Conception and design - Felix Oyania, Martin Situma.
Acquisition of data or analysis and interpretation of data - Felix Oyania, Martin Situma, Sarah Jane Commander.
Drafting the article or revising it critically for important intellectual content - Felix Oyania, Robert Mugarura, Sarah Jane Commander.
Final approval of the version published - Felix Oyania, Sarah Jane Commander, Martin Situma.
Agreement to be accountable for the article and to ensure that all questions regarding the accuracy or integrity of the article are investigated and resolved - Felix Oyania, Martin Situma.
Guarantor
Felix Oyania, Martin Situma.
Research registration number
Not applicable.
Availability of supporting data
Supporting data is available upon request.
Parental consent for minors
Written informed consent was obtained from the patient's parents/legal guardian for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Declaration of competing interest
All authors declared no conflict of interest.
Acknowledgements
Patient and her family, Sarah Jane Commander, Stephen Trinidad, Martin Situma.
Contributor Information
Felix Oyania, Email: oyafel@icloud.com.
Sarah Jane Commander, Email: Sarah.commander@duke.edu.
Robert Mugarura, Email: rmugarura@kab.ac.ug.
References
- 1.Nah S.A., Ong C.C.P., Lakshmi N.K., et al. Anomalies associated with anorectal malformations according to the krickenbeck anatomic classification. J. Pediatr. Surg. 2012 doi: 10.1016/j.jpedsurg.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 2.Rintala R.J., Lindahl H.G., Rasanen M. Do children with repaired low anorectal malformations have normal bowel function? J Pediatr Surg. 1997 doi: 10.1016/S0022-3468(97)90628-X. Published Online First. [DOI] [PubMed] [Google Scholar]
- 3.Ozgediz D., Poenaru D. The burden of pediatric surgical conditions in low and middle income countries: a call to action. J. Pediatr. Surg. 2012 doi: 10.1016/j.jpedsurg.2012.09.030. [DOI] [PubMed] [Google Scholar]
- 4.Yousef Y., Lee A., Ayele F., et al. Delayed access to care and unmet burden of pediatric surgical disease in resource-constrained African countries. J. Pediatr. Surg. 2019 doi: 10.1016/j.jpedsurg.2018.06.018. [DOI] [PubMed] [Google Scholar]
- 5.Meara J.G., Leather A.J.M., Hagander L., et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015:386. doi: 10.1016/S0140-6736(15)60160-X. [DOI] [PubMed] [Google Scholar]
- 6.Holcomb G.W., Murphy J.P. Ashcraft's pediatric. Surgery. 2010 doi: 10.1016/B978-1-4160-6127-4.X0001-8. [DOI] [Google Scholar]
- 7.Sinha S.K., Kanojia R.P., Wakhlu A., et al. Delayed presentation of anorectal malformations. J. Indian Assoc. Pediatr. Surg. 2008;13:64. doi: 10.4103/0971-9261.43023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haider N., Fisher R. Mortality and morbidity associated with late diagnosis of anorectal malformations in children. Surgeon. 2007;5:327–330. doi: 10.1016/s1479-666x(07)80083-7. [DOI] [PubMed] [Google Scholar]
- 9.Wilson B.E., Etheridge C.E., Soundappan S.V.S., et al. Delayed diagnosis of anorectal malformations: are current guidelines sufficient? J. Paediatr. Child Health. 2010;46:268–272. doi: 10.1111/j.1440-1754.2009.01683.x. [DOI] [PubMed] [Google Scholar]
- 10.Agha R.A., Franchi T., Sohrabi C., The S.C.A.R.E., et al. Guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;2020:84. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 11.Sarin Y.K. Mayer-Rokitansky syndrome and anorectal malformation. Indian J. Pediatr. 2005;72:803. doi: 10.1007/BF02734160. [DOI] [PubMed] [Google Scholar]
- 12.Adejuyigbe O., Sowande O.A., Olayinka O.S., et al. Rectovestibular fistula with absent distal vagina in an adolescent nigerian girl. J. Pediatr. Surg. 2002;37:1479–1480. doi: 10.1053/jpsu.2002.35419. [DOI] [PubMed] [Google Scholar]
- 13.Patankar J.Z., Mali V.P., Yashpal R., et al. Anorectal malformation with congenital absence of vagina: a case report and review of the literature. Pediatr. Surg. Int. 2004;20:295–297. doi: 10.1007/s00383-003-1130-2. [DOI] [PubMed] [Google Scholar]
- 14.Morcel K., Camborieux L., Guerrier D. Mayer-rokitansky-Küster-Hauser (MRKH) syndrome. Orphanet. J. Rare Dis. 2007;2:1–9. doi: 10.1186/1750-1172-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rahayatri T.H., Pramudito B.C., Soedibyo S. Vaginal reconstruction using ileum segment and posterior sagittal anorectoplasty in a patient with Mayer–Rokitansky–Küster–Hauser syndrome with anorectal malformations: a case report. Int. J. Surg. Case Rep. 2021;79:76–83. doi: 10.1016/j.ijscr.2020.12.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taher H., Azzam A., Kamal A., et al. Hernia uteri inguinale in an 18 months old female infant: a case report. Int. J. Surg. Case Rep. 2021:78. doi: 10.1016/j.ijscr.2020.11.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pandya K.A., Koga H., Okawada M., et al. Vaginal anomalies and atresia associated with imperforate anus: diagnosis and surgical management. J. Pediatr. Surg. 2015;50:431–437. doi: 10.1016/j.jpedsurg.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 18.Taher H.M.A., Fares A., Wishahy A.M.K. Laparoscopic resurrection of an old technique: a new approach for total urogenital separation and rectal pull-through in patients with long common channel cloacal malformation. J. Endourol. 2022;36:1177–1182. doi: 10.1089/end.2021.0724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Folch M., Pigem I., Konje J.C. Müllerian agenesis: etiology, diagnosis, and management. Obstet Gynecol Surv. 2000;55:644–649. doi: 10.1097/00006254-200010000-00023. [DOI] [PubMed] [Google Scholar]
- 20.Levitt M.A., Stein D.M., Peña A. Rectovestibular fistula with absent vagina: a unique anorectal malformation. J. Pediatr. Surg. 1998;33:986–990. doi: 10.1016/s0022-3468(98)90519-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Supporting data is available upon request.