Abstract
Aim
Advanced life support courses have a clear educational impact; however, it is important to determine whether participation of one or more members of the resuscitation team in an accredited advanced life support course improves in-hospital cardiac arrest patient survival outcomes.
Methods
We searched EMBASE.com, Medline, Cochrane and CINAHL from inception to 1 November 2022. Included studies were randomised or non-randomised interventional studies assessing the impact of attendance at accredited life support courses on patient outcomes. Accredited life support courses were classified into 3 contexts: Advanced Life Support (ALS), Neonatal Resuscitation Training (NRT), and Helping Babies Breathe (HBB). Existing systematic reviews were identified for each of the contexts and an adolopment process was pursued. Appropriate risk of bias assessment tools were used across all outcomes. When meta-analysis was appropriate a random-effects model was used to produce a summary of effect sizes for each outcome.
Results
Of 2714 citations screened, 19 studies (1 ALS; 7 NRT; 11 HBB) were eligible for inclusion. Three systematic reviews which satisfied AMSTAR-2 criteria for methodological quality, included 16 of the studies we identified in our search. Among adult patients all outcomes including return of spontaneous circulation, survival to discharge and survival to 30 days were consistently better with accredited ALS training. Among neonatal patients there were reductions in stillbirths and early neonatal mortality.
Conclusion
These results support the recommendation that accredited advanced life support courses, specifically Advanced Life Support, Neonatal Resuscitation Training, and Helping Babies Breathe improve patient outcomes.
Keywords: Advanced life support, Course, Neonatal, Adult, Patient outcome
Introduction
Accredited advanced resuscitation training has existed since the 1970s when the Advanced Cardiac Life Support (ACLS) course (for adults) was developed by the American Heart Association (AHA).1, 2 This course paved the way for advanced life support (ALS) courses offered by other resuscitation councils. Resuscitation courses focusing on other patient populations, such as neonates and pediatrics, were subsequently developed in the 1980s. More recently, programs like Helping Babies Breathe (HBB), a simulation-based curriculum to facilitate resuscitation training for facility birth attendants from resource limited settings, were established to make high-priority resuscitation training concepts accessible to a global audience.3 Evaluations have confirmed the educational impact of these courses;4 however, a key question is whether attendance of healthcare personnel on such courses has an impact on survival of patients with cardiac arrest.
A 2018 systematic review identified very low certainty evidence that resuscitation team member completion of an adult ALS course improves patient outcomes after cardiac arrest.5 The primary limitation of this review was that it focused exclusively on courses intended to treat adult patients. Understanding whether completion of accredited advanced life support courses improves patient outcomes in populations other than adults or within other contexts was identified as a priority topic by the Education, Implementation and Teams (EIT) Task Force of the International Liaison Committee on Resuscitation (ILCOR).6
The objective of this systematic review was to determine if participation of one or more members of the resuscitation team in an accredited advanced life support course, including courses focused on the care of adult, paediatric, and neonatal patients improve patient outcomes.
Methods
This systematic review was commissioned by the ILCOR Education, Implementation and Teams (EIT) Task Force as part of a continuous evidence evaluation process. The study and protocol were registered with Prospero (registration number CRD42021253673).
Research question
To guide the systematic review, a research question using the PICOST (Population, Intervention, Control, Outcomes, Study design, and Timeframe)7 format was formulated, as follows: “In patients requiring in-hospital cardiac arrest resuscitation of any age (Population), does prior participation of one or more members of the resuscitation team in an accredited advanced life support course (Intervention), as opposed to no such participation (Control), affect return of spontaneous circulation (ROSC), survival to hospital discharge or to 30 days, survival to one year, survival with favorable neurological outcome, or specifically in neonatal studies: stillbirth rate, neonatal and perinatal mortality (Outcomes)?”
We defined ‘accredited life support course’ as structured advanced life support courses that have been approved by a professional organization (e.g., a resuscitation council) this includes Advanced Life Support (ALS), Advanced Cardiac Life Support (ACLS), Neonatal Resuscitation Program (NRP), Neonatal Life Support (NLS), Advanced Resuscitation of the Newborn Infant (ARNI), Pediatric Advanced Life Support (PALS), European Paediatric Advanced Life Support Course (EPALS), Helping Babies Breathe (HBB) and the European Paediatric Immediate Life Support (EPILS). Basic life support, trauma and First Aid courses were excluded.
Study eligibility
We included randomised and non-randomised interventional studies that specifically described the impact upon patient outcomes of attendance at an accredited life support course, including ALS, ACLS, PALS, EPALS, EPILS, NRT, NRP, HBB, NLS or ARNI by one or more of the healthcare personnel attending a patient requiring resuscitation. We excluded studies in trauma life support (as not primarily cardiac aetiology for cardiac arrest), and studies that only looked at the impact of individual components of a course (e.g., defibrillation, airway management, drug therapy). Studies written in any language were included if there was an English-language abstract.
Data sources
We searched EMBASE.com, Medline, Cochrane and CINAHL with the search date of 18 October 2021, but updated the search on 1 November 2022. The search strategy is described in Appendix 1.
Appraisal and update of existing systematic reviews
When existing systematic reviews addressing our PICOST question were identified, we pursued an adolopment process to update previous evidence. The adolopment process is based on the GRADE-ADOLOPMENT approach proposed by the GRADE working group8 and adopted by ILCOR.9 The steps of this process included (1) Determination of appropriate methodological rigour of the existing systematic review via the AMSTAR-2 criteria;10 (2) Review of the existing review’s literature search to determine if it was sufficiently recent (within the last 3 months) or needed to be repeated/revised; (3) Re-analysis of the data in light of any new literature identified. Components of the AMSTAR 2 checklist that were considered essential to pursue adolopment included published evidence of all the following: search strategy, inclusion/exclusion criteria, data extraction tables, bias assessment tables (including criteria used), GRADE Evidence Profile tables and meta-analysis.
Study selection
The titles and abstracts of all potentially eligible studies were screened for inclusion by four reviewers split into pairs. The included studies were independently screened in more detail for eligibility in these pairs based upon set inclusion and exclusion criteria. Any disagreements between the reviewers at either stage were resolved by discussion.
Data collection and quality assessment
Data from each study were independently extracted by each reviewer. Data were collated separately for each outcome, namely ROSC, survival to hospital discharge, survival to 30 days, survival to 1 year, and survival with favourable neurological outcome. We decided to combine survival to hospital discharge and survival to 30 days in the analysis.11 For neonatal studies we also recorded: stillbirth rate (deaths prior to complete expulsion or extraction of products of conception from its mother), fresh stillbirth rate (deaths with no signs of life at any time after birth and without any signs of maceration), 1-day neonatal mortality, 7-day neonatal mortality, 28-day neonatal mortality, and perinatal mortality (all deaths in the first week after birth, including intrapartum-related stillbirths).12
Two reviewers independently assessed the overall quality of evidence of individual studies using the GRADE approach (Grades of Recommendation, Assessment, Development and Evaluation).13 Where the adolopment process was used to update previously published systematic reviews, the same risk of bias tool was used as per the initial publication, for consistency. When available, we examined study protocols of included studies to assess for any reporting bias; and checked that our search of the literature did not identify studies that were missed or unreported by included systematic reviews. In case of disagreement, consensus was reached by discussion. An assessment of certainty of evidence was made using GRADE methodology.13
Analysis
We used both quantitative and narrative syntheses of evidence.
Considering the clinical and methodological heterogeneity of included studies, we used a random effects model for meta-analysis where indicated. Data were entered into Review Manager (RevMan5, The Cochrane Collaboration, Oxford, UK) to calculate the Odds ratio (OR) and risk difference (RD), 95% confidence intervals (CI) and statistical heterogeneity. Heterogeneity between studies was statistically assessed using the chi-squared test. The extent of heterogeneity among studies was expressed with I2, with I2 values > 50% indicating large inconsistency or heterogeneity.
In situations where it was deemed inappropriate to perform a meta-analysis (due to clinical or methodological heterogeneity), a narrative summary was provided.
Results
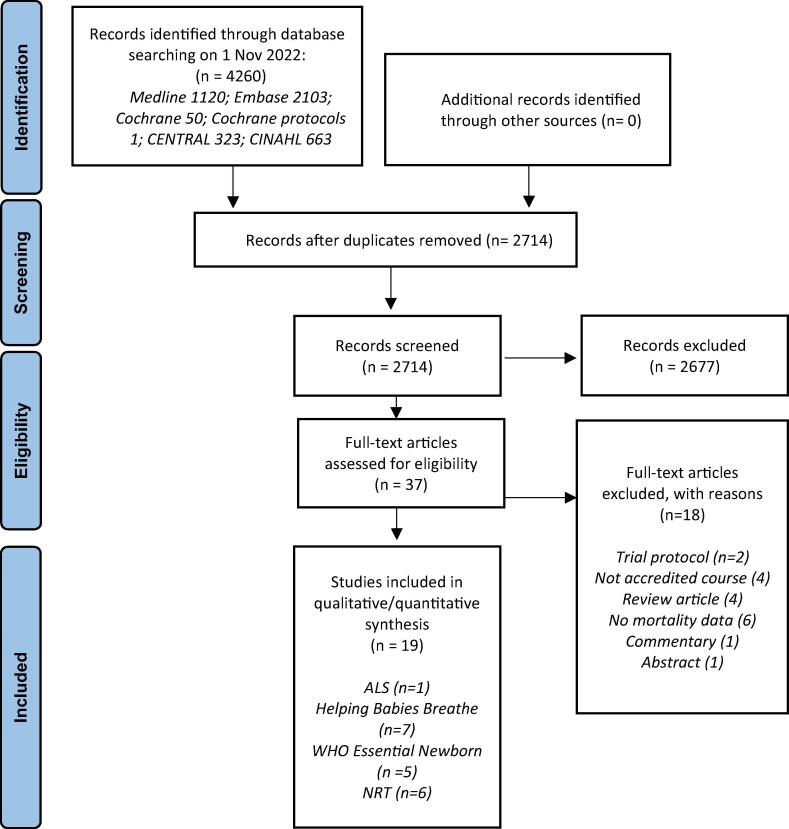
The search identified 2714 articles after duplicates were removed. Of these, 2677 articles were excluded during the title and abstract screen, leaving 37 full text articles to be screened for eligibility (see Fig. 1). Eighteen papers were excluded as shown in Fig. 1. Identified studies mapped to three separate contexts, namely adult Advanced Life Support (ALS), Neonatal Resuscitation Training (NRT), and Helping Babies Breathe (HBB). Three systematic reviews were identified which individually covered ALS,5 NRT,12 and HBB.14 These systematic reviews included sixteen of the identified studies. An additional three studies not included in the published systematic reviews were identified for inclusion from the search, comprising ALS (n = 1);15 and HBB (n = 2).16, 17 No studies were identified for other types of accredited advanced life support courses. Table 1 contains the characteristics of included studies.
Fig. 1.
Prisma flow diagram.
Table 1.
Characteristics of newly identified studies for ‘Advanced Life Support’, and ‘Helping Babies Breathe Training’ (characteristics of all included studies are listed in Appendix 1).
| Advanced life support studies | |||||
|---|---|---|---|---|---|
| Author Year Country |
Study design | Setting | Number of patients | Outcome measures | Results |
| Pareek15 2018 India |
Retrospective cohort study, pre- and post- AHA ACLS | 750 bed tertiary care hospital | 632 – 294 pre ACLS; 338 post ACLS; no data on age or sex | ROSC; Survival to hospital discharge | • ROSC increased from 19.7% to 30.1% (p = 0.003) |
| • Significant increase in survival to hospital discharge post-BLS/ACLS training (p < 0.0001) | |||||
| Helping babies breathe studies | |||||
| Innerdal17 2020 Mali |
Pre-post training | Local district hospital | 9769: 3125 pre-training; 6644 post-training | Fresh stillbirth rate, 1-day neonatal mortality, perinatal mortality | • Perinatal mortality rate (PMR) decreased from 21.7/1000 births to 6.0/1000 live births; RR 0.27, (95% CI 0.19–0.41; p < 0.0001). |
| • 1-day neonatal mortality rate decreased from 6.3/1000 to 0.8/1000 live births; RR 0.12 (95% CI 0.05–0.33; p = 0.0006). | |||||
| • Fresh stillbirth rate decreased from 15.7/1000 to 5.3/1000, RR 0.33 (95% CI 0.22–0.52; p < 0.0001) | |||||
| Patterson16 2021 Democratic Republic of Congo |
Pre-post training | Three health facilities | 24977: 13,840 pre-training; 11,137 post-training | Total stillbirth, fresh stillbirth, macerated stillbirth, neonatal death before discharge, perinatal death | • No change in total stillbirths following resuscitation training and continuous electronic HR monitoring of non-breathing newborns (aRR 1.15 [0.95, 1.39]). |
| • Increased rate of macerated stillbirth (aRR 1.58 [1.24, 2.02]), death before discharge (aRR 3.31 [2.41,4.54]), and perinatal death (aRR 1.61 [1.38, 1.89]) during the intervention period. | |||||
BLS- Basic Life Support; ACLS- Advanced Cardiac Life Support; HBB – Helping Babies Breath.
Risk of bias within studies
The risk of bias assessment is summarised in Table 2, Table 3, Table 4. The Risk of Bias In Non-randomised Studies of Interventions (ROBINS-I)18 tool was used for ALS studies, the criteria suggested by Cochrane Effective Practice and Organization of Care19 and criteria outlined in Chapter 8 of Cochrane Handbook for Systematic Reviews and interventions20 for NRT studies, and the McMaster critical review form for quantitative studies21 for HBB studies.
Table 2.
ROBINS-I risk of bias assessment for ‘Advanced Life Support’.
| Study | Year | Design | Total Patients | Population | Industry Funding | Eligibility Criteria | Exposure/Outcome | Confounding | Follow Up |
|---|---|---|---|---|---|---|---|---|---|
| Lowenstein39 | 1986 | Non-RCT | 90 | AHA ACLS | No | Low | Low | Low | Low |
| Sanders40 | 1994 | Non-RCT | 64 | AHA ACLS | No | Highb | Low | Low | Low |
| Makker41 | 1995 | Non-RCT | 225 | AHA ACLS | No | Unclearc | Low | Highd | Low |
| Camp42 | 1997 | Non-RCT | 236 | AHA ACLS | No | Highe | Low | Highd | Low |
| Pottle43 | 2000 | Non-RCT | 299 | RC(UK) ALS | No | Highf | Low | Highd | Low |
| Dane44 | 2000 | Non-RCT | 117 | AHA ACLS | Partiala | Low | Low | Highd | Low |
| Moretti45 | 2007 | Non-RCT | 156 | AHA ACLS | No | Low | Low | Low | Low |
| Sodhi46 | 2011 | Non-RCT | 627 | AHA ACLS | No | Low | Low | Highd | Low |
| Pareek15 | 2018 | Non-RCT | 632 | AHA BLS/ACLS | No | Low | Low | Highd | Low |
BLS- Basic Life Support; ACLS- Advanced Cardiac Life Support.
Portions of the research were funded by a Teaching Methods Grant from AHA to the first author.
Did not elaborate on exclusion criteria for cardiac arrest patients.
All incidents analysed but not clear how identified.
Prognostic factors not adjusted for in statistical analysis of most studies; considered low if they reported characteristics of patients in one group vs another and described p values.
Differing and unclear eligibility criteria for three periods of study.
Only those with completed audit form (86.5%) included.
Table 3.
Risk of bias assessment for ‘Neonatal Resuscitation Training’.
| Study | Incomplete outcome data addressed? | Free of selective reporting | Free of other bias? | Baseline outcomes similar? | Free of contamination? | Baseline characteristics similar? |
|---|---|---|---|---|---|---|
| Zhu30 | Unclear risk | Low risk | Low risk | Unclear risk | Low risk | Unclear risk |
| Deorari33 | Unclear risk | Low risk | Low risk | Unclear risk | Low risk | Unclear risk |
| Jeffery22 | Unclear risk | Low risk | Low risk | Unclear risk | Unclear risk | Unclear risk |
| Vakrilova31 | Low risk | Low risk | High risk | Unclear risk | High risk | Unclear risk |
| O’Hare23 | Low risk | Low risk | Unclear risk | Unclear risk | Low risk | Unclear risk |
| Opiyo24 | Unclear risk | Low risk | Unclear risk | Unclear risk | Low risk | Unclear risk |
| Boo25 | Low risk | Low risk | Unclear risk | Unclear risk | High risk | Low risk |
| Hole35 | High risk | Low risk | Unclear risk | Unclear risk | High risk | Unclear risk |
| Sorenson26 | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk |
| Patel 12 | Low risk | Low risk | Unclear risk | Unclear risk | Low risk | Low risk |
| Msemo28 | Unclear risk | Low risk | Low risk | Unclear risk | Low risk | Unclear risk |
| Bellad29 | Low risk | Low risk | Low risk | Unclear risk | Low risk | High risk |
| Ashish12 | Low risk | Low risk | Low risk | Unclear risk | Low risk | High risk |
| Goudar27 | Unclear risk | Low risk | Unclear risk | Unclear risk | Low risk | Low risk |
Risk of Bias assessed using the criteria suggested by Cochrane Effective Practice and Organization of Care19and criteria outlined in Chapter 8 of Cochrane Handbook for Systematic Reviews and interventions.
Table 4.
McMaster critical review form for quantitative studies Risk of bias assessment for ‘Helping Babies Breathe Training’.
| Arabi | Bellad | Goudar | KC | Mduma | Msemo | Wrammert | Innerdal | Patterson | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Study purpose | + | + | + | + | + | + | + | + | + | |
| Literature | + | + | + | - | +/- | + | + | + | + | |
| Sample | Description | + | + | + | + | +/- | + | +/- | + | + |
| Sample size justified | - | - | - | + | + | + | + | - | - | |
| Outcomes | Reliable | + | + | + | + | + | - | +/- | - | + |
| Valid | + | + | + | - | + | - | + | + | + | |
| Intervention | Description | + | - | + | + | + | + | - | + | - |
| Contamination | + | - | - | - | + | - | - | + | + | |
| Cointervention | + | - | - | - | + | + | - | - | + | |
| In terms of statistical significance | + | + | + | + | + | + | + | + | + | |
| Analysis appropriate | + | + | + | + | + | + | + | + | + | |
| Clinical importance | + | + | + | + | + | + | + | + | + | |
| Drop-outs reported | - | + | + | - | - | - | - | + | - | |
| Conclusions and implications | + | + | + | + | + | + | + | + | ||
| Score | 13 | 11 | 12 | 10 | 12 | 11 | 8 | 11 |
Advanced life support (ALS)
One systematic review including eight studies satisfied the AMSTAR-2 criteria for appropriate methodological quality.5 Our literature search identified one additional study for inclusion.15
The additional study within the ALS context for adults was a 2018 pre-post intervention study from India evaluating the impact of an AHA ACLS course on patient outcomes after in-hospital cardiac arrest.15 This additional study supported the association between course participation and ROSC and survival to hospital discharge identified in the previous systematic review.5
Results of the updated analysis (Table 5) of all nine studies including 2,445 patients continue to show an association between course participation and ROSC, pooled OR of 1.66 (95% CI 1.24–2.21). The certainty of evidence for ROSC remains very low. The previous systematic review15 showed a non-significant effect of course participation on patient survival to hospital discharge but a significant effect on course participation and patient survival to 30 days. In the updated analysis, these outcomes were combined and showed a significant association, OR 2.48 (95% CI 1.21–5.09). The updated analysis showed non-significant association between course participation and patient survival to 1 year pooled OR 3.61 (95% CI 0.11 to 119.42). The quality of the studies for these outcomes remains very low.
Table 5.
GRADE Summary of findings table for ‘Advanced life support’.
| No of patients |
Effect | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | ACLS/ ALS | No ACLS/ ALS | Relative (95% CI) | Certainty | Importance |
| ROSC | |||||||||||
| 7 | Observational studies | seriousa | seriousb | seriousc | seriousd | none | 480/ 1211 (39.6%) | 261/ 882 (29.6%) | OR 1.66 (1.24 to 2.21) |  |
CRITICAL |
| Survival to discharge and 30 days | |||||||||||
| 8 | Observational studies | seriousa | seriousb | seriousc | seriousd | none | 309/ 995 (31.1%) | 111/ 672 (16.5%) | OR 2.48 (1.21 to 5.09) |  |
CRITICAL |
| 1 year survival | |||||||||||
| 2 | Observational studies | seriousa | seriousb | seriousc | seriousd | none | 51/ 262 (19.5%) | 31/ 193 (16.1%) | OR 3.61 (0.11 to 119.42) |  |
CRITICAL |
Mixture of serious and low risk of bias studies.
Some studies showed significant improvement, and some showed no improvement.
Differences in patient type, hospital type, provider type and team composition, and nature of intervention.
Absence of confidence intervals.
Neonatal resuscitation training (NRT)
A summary of the studies for the NRT context is presented in Table 6.
Table 6.
Pooled risk ratios from hospital based Neonatal Resuscitation Courses.
| Outcome | Studies (n) | Participants (n) | RR | 95% CI |
|---|---|---|---|---|
| All stillbirths | 9 | 1,334,307 | 0.88 | 0.82 to 0.94 |
| Fresh stillbirths | 6 | 231,455 | 0.71 | 0.54 to 0.93 |
| 1-day neonatal mortality | 5 | 216,373 | 0.58 | 0.38 to 0.90 |
| 7-day neonatal mortality | 5 | 296,300 | 0.78 | 0.63 to 0.97 |
| 28-day mortality | 6 | 1,090,594 | 0.89 | 0.65 to 1.22 |
| Perinatal mortality | 4 | 1,178,446 | 0.78 | 0.70 to 0.87 |
One systematic review including fourteen community-based and in-hospital based interventions,12 satisfied the AMSTAR-2 criteria for appropriate methodological quality. Consistent with our PICOST question, we examined only in-hospital based studies for this review. Our literature search did not identify any new studies. We report a summary of the in-hospital based sub-group analysis.
The fourteen in-hospital studies including 1,531,254 patients were conducted from 1993 to 2009. All the studies were retrospective pre- and post- intervention studies from low to middle resource settings.
Nine studies with a total of 1,334,307 patients assessed the risk of stillbirths where one or more members of the team had undergone NRT.12, 22, 23, 24, 25, 26, 27, 28 The data showed a significant decrease in the risk of all stillbirths. Six studies with a total of 231,455 patients assessed fresh stillbirths.12, 24, 27, 28, 29 The data showed a significant decrease in the risk of fresh stillbirths where staff members had undertaken NRT. Five studies with a total of 216,373 patients assessed 1-day neonatal mortality.12, 28, 29, 30 The data showed a significant decrease in the risk of 1-day neonatal mortality. Five studies with a total of 296,300 patients assessed 7-day neonatal mortality.22, 29, 30, 31, 32 The data showed a significant decrease in the risk of 7-day neonatal mortality. Six studies with a total of 1,090,594 patients assessed 28-day neonatal mortality.24, 27, 29, 33, 34, 35 There was no difference in the risk of 28-day neonatal mortality. Four studies with a total of 1,178,446 patients assessed perinatal mortality.12, 22, 25, 29 The data showed a significant decrease in the risk of perinatal mortality when attending team members had undertaken NRT.
Helping Babies Breathe (HBB)
One systematic review14 satisfied the AMSTAR-2 criteria for appropriate methodological quality. Two additional studies16, 17 were identified in our search. These studies were appraised using the McMaster Critical Review form21 and found to be of moderate quality, similar to the other studies in the systematic review identified for this context.
The additional studies were both pre- and post- intervention studies evaluating the impact of a HBB course on neonatal outcomes in Mali17 and the Democratic Republic of Congo.16 The study by Innerdal et al. (2020) further supported the association between course participation and decreased perinatal mortality, fresh stillbirth rate, and 1-day neonatal mortality.17 The study by Patterson et al. (2021) found no difference in stillbirth rate but found increased perinatal mortality and death before discharge in the intervention group.16 Overall, two out of four studies demonstrate decreased perinatal mortality, five out of eight studies show decreased fresh stillbirth rate, with HBB training.
Due to substantial clinical and methodological heterogeneity between the studies, no meta-analysis was performed.
Discussion
Our systematic review supports the understanding that participation of one or more members of the resuscitation team in an accredited advanced life support course, particularly those focused on the care of adult and neonatal patients, improves patient outcomes. The additional identified studies strengthen the conclusions of previous systematic reviews and add to the growing body of evidence in favour of advanced life support training for both these age groups.
Although we only identified three new studies, this work is still important. By examining a wider range of courses and patient populations, we were able to address the PICOST question and overcome the limitation of the previous systematic review more comprehensively.
For adult patients, the additional study strengthened the association between survival outcomes and advanced life support training attendance with a similar odds ratio but tighter confidence intervals. Considered together, the evidence suggests that ROSC, survival to discharge and survival to 30 days are consistently better with accredited advanced life support training, whereas survival to 1 year is inconclusive due to limited data and wide confidence intervals.
While no new studies were identified for NRT, previous analyses have examined data from both the community and hospital-based implementations. Our new analysis of data from only hospital-based studies demonstrates an effect in favour of training. We suggest that this may be because hospital-based implementations allow more consistent provision of training and accurate data acquisition as compared to community settings. Given that neonatal survival rates are particularly poor in resource limited settings,36 it is even more important to clearly demonstrate improved outcomes from advanced life support training before diverting resources from other important public health interventions.
For HBB, one of the two new studies added further support for the association between training and reductions in stillbirths and early neonatal mortality.17 The other study, which showed no difference in stillbirth rate and greater perinatal mortality in the intervention group, may have been impacted by a less rigorous implementation of HBB (monthly practice without external training support vs weekly practice with external training support in previous studies) and their retrospective collection of pre-intervention data which may have underreported death.16 Furthermore, there is evidence to suggest that the women enrolled during the HBB intervention stage of this study may have included higher-risk pregnancies.16 Despite HBB studies having substantial variability in setting, duration of training, varying study designs and lack of consistent outcomes contributing to substantial heterogeneity, analyses seem to show a treatment effect in favour of training, regardless of setting. A separate cost effectiveness analysis based on the implementation of HBB in rural Tanzania also determined it to be a highly cost-effective intervention.32 Given that a quarter of global neonatal deaths are due to birth asphyxia,37 the potential for lives saved appears to outweigh the costs of providing these courses.
In addition to improvements in patient outcomes, complex interventions such as advanced life support training have other benefits, particularly as a means of providing the opportunity to update healthcare professions on changes as new evidence emerges and is integrated into guidelines, algorithms, and teaching. Furthermore, training is an important means through which updated guidelines are implemented and integrated into practice.38
Our use of adolopment, whereby we justify the inclusion of existing systematic reviews by applying a transparent three-step process of (1) determining methodological rigour, (2) reviewing and revising literature searches; and (3) re-analysing data, is novel and reduces duplication of efforts allowing the systematic review process to be more resource efficient (e.g., reviewer and information specialist time).
Knowledge gaps and future research
Given significant heterogeneity in the included studies, future studies need to establish the best combination of settings, trainee characteristics, and training frequency to sustain existing effects on patient outcomes in all contexts. The published evidence only covers three accredited life support courses, so further research is needed for other courses (e.g. paediatric / trauma courses). Despite this, it is reasonable to assume that advanced life support training may offer comparable outcomes in other courses. Studies addressing longer-term outcomes (including favourable neurological outcomes) would be helpful. The finding that NRT and HBB did not affect mortality from day 7 to 28 suggests that training may not have as significant an impact in the absence of appropriate ongoing care. Further cost-effectiveness analyses would also be helpful in addressing the cost benefit of advanced life support interventions particularly in low resource settings where such courses have the potential to divert resources away from other valuable public health initiatives.
Limitations
All studies included in this review were non-randomised, the majority of which were pre-post studies. Pre-post studies without concurrent control groups carry a large risk of bias. There was significant heterogeneity in the intervention group with regards to course length, content, setting, and timing of outcome measurement. There are also some limitations to the adolopment approach: existing systematic reviews must be methodologically rigorous and have published/ shared their search strategy (including date of last search), inclusion and exclusion criteria, data extraction tables, bias assessment tables (including criteria used), GRADE evidence profile tables and meta-analyses (where appropriate). Because of the stringent (≤3 months) cut-off for recency of the existing systematic reviews search strategy, most adolopment processes will at a minimum need to re-run the existing search strategy. Furthermore, if the existing systematic review only addresses a part of the new PICOST (as was the case in this study) a new search strategy may be required. Despite these limitations, adolopment is a reasonable tool to consider in situations where a question has a recently published systematic review identified. Many courses, especially neonatal and pediatric courses, also focus on prevention of cardia arrest rather than CPR only which may affect cardiac arrest incidence bu not cardiac arrest survival outcomes.
Conclusion
This review found additional evidence in support of health care personnel attendance of advanced life support courses. Studies demonstrate that accredited advanced life support courses, specifically ALS, NRT, and HBB training, improve patient survival outcomes in both adult and neonatal cardiac arrest patients.
Funding
None.
Conflicts of Interest
This systematic review was part of the ILCOR continuous evidence evaluation process, which is guided by a rigorous conflict of interest policy (see www.ilcor.org). Andrew Lockey is President of Resuscitation Council UK and a member of the ILCOR Task Force on Education, Implementation and Teams (EIT). Robert Greif is the European Resuscitation Council (ERC) Director of Guidelines and ILCOR, and ILCOR’s EIT Taskforce Chair. Catherine Patocka and Kasper G Lauridsen are members of ILCOR’s EIT Task Force.
CRediT authorship contribution statement
Catherine Patocka: Writing – original draft, Investigation. Andrew Lockey: Conceptualization, Investigation, Data curation, Writing – review & editing. Kasper G. Lauridsen: Investigation, Writing – review & editing. Robert Greif: Conceptualization, Investigation, Writing – review & editing.
Acknowledgement
The authors would like to thank Jenny Ring (information specialist) and Helen Curtis (information specialist) for their help with this review. The following ILCOR Education Implementation and Teams (EIT) Taskforce members are acknowledged as collaborators on this review: Cristian Abelairas-Gomez, Farhan Bhanji, Jan Breckwoldt, Adam Cheng, Kathryn Eastwood, Nino Fijačko, Elaine Gilfoyle, Ming-Ju Hsieh, Ying-Chih Ko, Yiqun Lin, Tasuku Matsuyama, Kevin Nation, Taylor Sawyer, Sebastian Schnaubelt, Chih-Wei Yang, Joyce Yeung, and Judith Finn for the SAC review of this manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2023.100389.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Carveth S. Standards for Cardiopulmonary Resuscitation and Emergency Cardiac Care. JAMA - J Am Med Assoc. 1974;227:796–797. doi: 10.1001/jama.1974.03230200054012. [DOI] [PubMed] [Google Scholar]
- 2.Carveth S.W., Burnap T.K., Bechtel J., et al. Training in Advanced Cardiac Life Support. JAMA - J Am Med Assoc. 1976;235:2311–2315. doi: 10.1001/jama.1976.03260470029021. [DOI] [PubMed] [Google Scholar]
- 3.Niermeyer S., Little G.A., Singhal N., Keenan W.J. A short history of helping babies breathe: Why and how, then and now. Pediatrics. 2020;146:101–111. doi: 10.1542/peds.2020-005637. [DOI] [PubMed] [Google Scholar]
- 4.Riggs M., Franklin R., Saylany L. Associations between cardiopulmonary resuscitation (CPR) knowledge, self-efficacy, training history and willingness to perform CPR and CPR psychomotor skills: A systematic review. Resuscitation. 2018;2019:259–272. doi: 10.1016/j.resuscitation.2019.03.019. [DOI] [PubMed] [Google Scholar]
- 5.Lockey A., Lin Y., Cheng A. Impact of adult advanced cardiac life support course participation on patient outcomes—A systematic review and meta-analysis. Resuscitation. 2018;129:48–54. doi: 10.1016/j.resuscitation.2018.05.034. [DOI] [PubMed] [Google Scholar]
- 6.Wyckoff MH, Singletary EM, Soar J, et al. 2021 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Vol 145.; 2022. doi:10.1161/CIR.0000000000001017.
- 7.Tricco A.C., Tetzlaff J., Moher D. In: Knowledge Translation in Health Care: Moving from Evidence to Practice. 2nd ed. Straus S.E., Tetroe J., Graham I.D., editors. John Wiley & Sons, Ltd; 2013. Knowledge synthesis; pp. 29–49. [Google Scholar]
- 8.Schünemann H.J., Wiercioch W., Brozek J., et al. GRADE Evidence to Decision (EtD) frameworks for adoption, adaptation, and de novo development of trustworthy recommendations: GRADE-ADOLOPMENT. J Clin Epidemiol. 2017;81:101–110. doi: 10.1016/j.jclinepi.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 9.ILCOR adolopment process. https://www.ilcor.org/uploads/Systematic-Review-Process-Adolopment-SAC-approved-v2.0-7-January-2022.docx.
- 10.Shea B.J., Reeves B., Wells G.A., et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studeis of healthcare interventions, or both. BMJ. 2017 doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Majewski D., Ball S., Bailey P., et al. Survival to hospital discharge is equivalent to 30-day survival as a primary survival outcome for out-of-hospital cardiac arrest studies. Resuscitation. 2021;166:43–48. doi: 10.1016/j.resuscitation.2021.07.023. [DOI] [PubMed] [Google Scholar]
- 12.Patel A., Khatib M., Kurhe K., Bhargava S., Bang A. Impact of neonatal resuscitation trainings on neonatal and perinatal mortality: a systematic review and meta-analysis. BMJ Paediatr Open. 2017;1 doi: 10.1136/bmjpo-2017-000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schünemann HJ, Brozek J, Guyatt GH, Oxman AD, eds. Chapter 5 Quality of evidence. In: GRADE Handbook. ; 20. https://gdt.gradepro.org/app/handbook/handbook.html.
- 14.Versantvoort J.M.D., Kleinhout M.Y., Ockhuijsen H.D.L., Bloemenkamp K., De Vries W.B., Van Den Hoogen A. Helping Babies Breathe and its effects on intrapartum-related stillbirths and neonatal mortality in low-resource settings: A systematic review. Arch Dis Child. 2020;105:127–133. doi: 10.1136/archdischild-2018-316319. [DOI] [PubMed] [Google Scholar]
- 15.Pareek M., Parmar V., Badheka J., Lodh N. Study of the impact of training of registered nurses in cardiopulmonary resuscitation in a tertiary care centre on patient mortality. Indian J Anaesth. 2018;62:381. doi: 10.4103/ija.IJA_17_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patterson J., Berkelhamer S., Ishoso D., et al. Effect of resuscitation training and implementation of continuous electronic heart rate monitoring on identification of stillbirth. Resuscitation. December 2021;2022:57–63. doi: 10.1016/j.resuscitation.2021.12.020. [DOI] [PubMed] [Google Scholar]
- 17.Innerdal M., Simaga I., Diall H., et al. Reduction in perinatal mortality after implementation of HBB training at a district hospital in Mali. J Trop Pediatr. 2020;66:315–321. doi: 10.1093/TROPEJ/FMZ072. [DOI] [PubMed] [Google Scholar]
- 18.Sterne J, Hernan M, McAleenan A, Reeves B, Higgins J. Assessing risk of bias in a non-randomized study. In: Higgins J, Thomas J, Chandler J, et al., eds. Cochrane Handbook for Systematic Reviews of Interventions. 6.3. ; 2022.
- 19.Cochrane Effective Practice and Organisation of Care. Suggested risk of bias criteria for EPOC reviews. https://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-for-authors2017/suggested_risk_of_bias_criteria_for_epoc_reviews.pdf. Accessed August 26, 2022.
- 20.Higgins J, Thomas J, eds. Cochrane Training. Cochrane Handbook for Systematic Reviews of Interventions. 6.3.; 2022. https://training.cochrane.org/handbook.
- 21.Law M., Stewart N., Pollock D., Letts L., Bosch J., Westmorland M. Guidelines for Critical Review Form - Quantitative Studies. Guidel Crit Rev Form - Quant Stud. 1998:1–11. [Google Scholar]
- 22.Jeffery H., Kocova M., Tozija F., et al. The impact of evidence-based education on perinatal capacity-building initiative in macedonia. Med Educ. 2004;38:435–447. doi: 10.1046/j.1365-2923.2004.01785.x. [DOI] [PubMed] [Google Scholar]
- 23.O’Hare B., Nakakeeto M., Southall D. A pilot study to determine if nurses trained in basic neonatal resuscitation would impact the outcome of neonates delivered in Kampala. Uganda J Trop Pediatr. 2006;52:376–379. doi: 10.1093/tropej/fml027. [DOI] [PubMed] [Google Scholar]
- 24.Opiyo N., Were F., Govedi F., Fegan G., Wasunna A., English M. Effect of newborn resuscitation training on health worker practices in Pumwani Hospital. PLoS One. 2008;3:e1599. doi: 10.1371/journal.pone.0001599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boo N. Neonatal resuscitation programme in Malaysia: an eight-year experience. Singapore Med J. 2009;50:152–159. [PubMed] [Google Scholar]
- 26.Sorenson B., Rasch V., Massawe S., Nyakina J., Elsass P., Nielsen B.B. Impact of ALSO training on the management of prolonged labor and neonatal care at kagera regional hospital tanzania. Int J Gynecol Obstet. 2010;111:8–12. doi: 10.1016/j.ijgo.2010.04.031. [DOI] [PubMed] [Google Scholar]
- 27.Goudar S., Somannavar M., Clark R., et al. Stillbirth and newborn mortality in India after helping babies breathe training. Pediatrics. 2013;131:e344–e352. doi: 10.1542/peds.2012-2112. [DOI] [PubMed] [Google Scholar]
- 28.Msemo G, Massawe A, Mmbando D, et al. Newborn mortality and fresh stillbirth rates in Tanzania after helping babies breathe training. [DOI] [PubMed]
- 29.Bellad R., Bang A., Carlo W., et al. A pre-post study of a multi-country scale up of resuscitation training of facility birth attendants: does Helping Babies Breathe training save lives? BMC Pregnancy Childbirth. 2016;16:1–10. doi: 10.1186/s12884-016-0997-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhu X., Fang H., Zeng S., Li Y., Lin H., Shi S. The impact of the neonatal resuscitation program guidelines (NRPG) on the neonatal mortality in a hospital in Zhuhai, China. Singapore Med J. 1997;38:485–487. [PubMed] [Google Scholar]
- 31.Vakrilova L., Elleau C., Sluncheva B. French-Bulgarian program “Resuscitation of the newborn in a delivery room” – results and perspectives. Akush Ginekol. 2005;44:35–40. [PubMed] [Google Scholar]
- 32.Vossius C., Lotto E., Lyanga S., et al. Cost-effectiveness of the “helping babies breathe” program in a missionary hospital in rural Tanzania. PLoS One. 2014;9:e102080. doi: 10.1371/journal.pone.0102080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Deorari A., Paul V., Singh M., Vidyasagar D. Impact of education and training on neonatal resuscitation practices in 14 teaching hospitals in India. Ann Trop Paediatr. 2001;21:29–33. [PubMed] [Google Scholar]
- 34.Dreyfus H.L. 2nd ed. Routledge; London: 2009. On the Internet: Thinking in Action. [Google Scholar]
- 35.Hole M., Olmsted K., Kiromera A., Chamberlain L. A neonatal resuscitation curriculum in Malawi, Africa: did it change in-hospital mortality? Int J Pediatr. 2012;2012 doi: 10.1155/2012/408689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.WHO neonatal mortality rates. https://www.who.int/news-room/fact-sheets/detail/levels-and-trends-in-child-mortality-report-2021. Accessed August 26, 2022.
- 37.Perinatal asphyxia. https://www.who.int/teams/maternal-newborn-child-adolescent-health-and-ageing/newborn-health/perinatal-asphyxia. Accessed November 15, 2022.
- 38.Stærk M., Lauridsen K.G., Mygind-Klausen T., Løfgren B. Differences in implementation strategies of the european resuscitation council guidelines 2015 in danish hospitals – A nationwide study. Open Access Emerg Med. 2018;10:123–128. doi: 10.2147/OAEM.S171250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lowenstein S., Sabyan E., Lassen C., Kern D. Benefits of training physicians in advanced cardiac life support. Chest. 1986;89:512–516. doi: 10.1378/chest.89.4.512. [DOI] [PubMed] [Google Scholar]
- 40.Sanders A., Berg R., Burress M., Genova R., Kern K., Ewy G. The efficacy of an ACLS training program for resuscitation from cardiac arrest in a rural community. Ann Emerg Med. 1994;23:56–59. doi: 10.1016/s0196-0644(94)70009-5. [DOI] [PubMed] [Google Scholar]
- 41.Makker R., Gray-Siracusa K., Evers M. Evaluation of advanced cardiac life support in a community teaching hospital by use of actual cardiac arrests. Hear Lung. 1995;24:116–120. doi: 10.1016/s0147-9563(05)80005-6. [DOI] [PubMed] [Google Scholar]
- 42.Camp B., Parish D., Andrews R. Effect of advanced cardiac life support training on resuscitation efforts and survival in a rural hospital. Ann Emerg Med. 1997;29:529–533. doi: 10.1016/s0196-0644(97)70228-2. [DOI] [PubMed] [Google Scholar]
- 43.Pottle A., Brant S. Does resuscitation training affect outcome from cardiac arrest? Accid Emerg Nurs. 2000;8:45. doi: 10.1054/aaen.1999.0089. [DOI] [PubMed] [Google Scholar]
- 44.Dane F., Russell-Lindgren K., Parish D., Durham M., Brown T., Jr In-hospital resuscitation: association between ACLS training and survival to discharge. Resuscitation2. 2000;47:83–87. doi: 10.1016/s0300-9572(00)00210-0. [DOI] [PubMed] [Google Scholar]
- 45.Moretti M., Cesar L., Nusbacher A., Kern K., Timerman S., Ramiers J. Advanced cardiac life support training improves long-term survival from in-hospital cardiac arrest. Resuscitation. 2007;72:458–465. doi: 10.1016/j.resuscitation.2006.06.039. [DOI] [PubMed] [Google Scholar]
- 46.Sodhi K., Singla M., Shrivastava A. Impact of advanced cardiac life support training program on the outcome of cardiopulmonary resuscitation in a tertiary care hospital. Indian J Crit Care Med. 2011;15:209–212. doi: 10.4103/0972-5229.92070. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.