Key Points
Question
What patient factors are associated with postoperative dysphagia following tracheal resection?
Findings
In this retrospective cohort study of 54 adults, increased age at time of operation was moderately associated with decreased functional oral intake scale scores postoperatively and delayed resolution of symptoms.
Meaning
When considering tracheal resection, older patients should be counseled to expect higher severity of dysphagia after surgery and a longer recovery before returning to their baseline swallowing function.
Abstract
Importance
Patients undergoing tracheal resection commonly experience dysphagia postoperatively, and the patient factors that predict severity and duration of symptoms are currently unclear.
Objective
To determine the association of patient and surgical factors on postoperative dysphagia in adult patients undergoing tracheal resection.
Design, Setting, and Participants
This was a retrospective cohort study of patients undergoing tracheal resection at 2 tertiary academic centers from February 2014 to May 2021. The centers included LAC+USC (Los Angeles County + University of Southern California) Medical Center and Keck Hospital of USC, both tertiary care academic institutions. Patients involved in the study underwent a tracheal or cricotracheal resection.
Exposures
Tracheal or cricotracheal resection.
Main Outcomes and Measures
The main outcome was dysphagia symptoms as measured by the functional oral intake scale (FOIS) on postoperative days (PODs) 3, 5, and 7, on the day of discharge, and at the 1-month follow-up visit. Demographics, medical comorbidities, and surgical factors were evaluated for association with FOIS scores at each time period using Kendall rank correlation and Cliff delta.
Results
The study cohort consisted of 54 patients, with a mean (SD) age of 47 (15.7) years old, of whom 34 (63%) were male. Length of resection segment ranged from 2 to 6 cm, with a mean (SD) length of 3.8 (1.2) cm. The median (range) FOIS score was 4 (1-7) on PODs 3, 5, 7. On the day of discharge and at 1-month postoperative follow-up, the median (range) FOIS score was 5 (1-7) and 7 (1-7), respectively. Increasing patient age was moderately associated with decreasing FOIS scores at all measured time points (τ = −0.33; 95% CI, −0.51 to −0.15 on POD 3; τ = −0.38; 95% CI, −0.55 to −0.21 on POD 5; τ = −0.33; 95% CI, −0.58 to −0.08 on POD 7; τ = −0.22; 95% CI, −0.42 to −0.01 on day of discharge; and τ = −0.31; 95% CI, −0.53 to −0.09 at 1-month follow-up visit). History of neurological disease, including traumatic brain injury and intraoperative hyoid release, was not associated with FOIS score at any of the measured time points (δ = 0.03; 95% CI, −0.31 to 0.36 on POD 3; δ = 0.11; 95% CI, −0.28 to 0.47 on POD 5, δ = 0.3; 95% CI, −0.25 to 0.70 on POD 7; δ = 0.15; 95% CI, −0.24 to 0.51 on the day of discharge, and δ = 0.27; 95% CI, −0.05 to 0.53 at follow-up). Resection length was also not correlated with FOIS score with τ ranging from −0.04 to −0.23.
Conclusions and Relevance
In this retrospective cohort study, most patients undergoing tracheal or cricotracheal resection experienced full resolution of dysphagia symptoms within the initial follow-up period. During preoperative patient selection and counseling, physicians should consider that older adult patients will experience greater severity of dysphagia throughout their postoperative course and delayed resolution of symptoms.
This cohort study assesses the association of patient and surgical factors on postoperative dysphagia in adult patients undergoing tracheal resection.
Introduction
Laryngotracheal stenosis is a narrowing of the upper airway in the larynx, subglottis, or trachea, most commonly caused by idiopathic or traumatic causes. Airway trauma includes prolonged intubation and postintubation and posttracheostomy-related injury,1 with a reported rate of stenosis in these patients ranging from 10% to 22%.2,3 Other causes include neoplastic compression or invasion, and autoimmune disorders.4 Treatment of laryngotracheal stenosis can involve endoscopic treatment with lysis of the stenosis and balloon dilation with various adjuvant medications or treatment. Stenosis which involves the cartilage with external collapse, existing tracheostomy, or failure of endoscopic management may require airway resection procedures such as tracheal or cricotracheal resection.5,6,7
As these open resection procedures involve disruption of the normal musculature and cartilaginous framework of the larynx and trachea, the nearby structures involved with swallowing can be affected, leading to dysphagia and an increased risk of aspiration encountered in the postoperative period.8,9 Longitudinal pharyngeal muscles help to expand and constrict the pharynx during swallowing and can be disrupted during airway resection, as well as pharyngeal constrictors. Other potentially affected muscles include suprahyoid muscles including the digastric, geniohyoid, stylohyoid, and mylohyoid, which are involved in elevating the hyoid during swallowing, as well as opposing infrahyoid muscles such as the omohyoid, sternohyoid and thyrohyoid, functioning to depress the hyoid. Intraoperative laryngeal release techniques often involve sectioning of the suprahyoid and infrahyoid muscles discussed previously and are sometimes necessary to allow a tension-free anastomosis and have been previously described to have an effect on dysphagia.10 Recently, studies have begun to investigate swallowing function as a primary outcome after open airway resection. Lennon et al11 described a series of 38 patients undergoing airway reconstruction procedures (25 patients undergoing tracheal or cricotracheal resection) and found that patients requiring temporary airway stent placement had a significantly longer duration of dysphagia symptoms compared with those without stents. While the effects of certain surgical factors on dysphagia following airway resection have been studied, there remains a lack of information on the individual patient factors that may predispose to postoperative dysphagia symptoms.12,13 Understanding the predictive patient factors for dysphagia is critical to guide appropriate patient selection and adequate counseling of patients on the risks and anticipated recovery following airway resection procedures.
The aim of the present study is to evaluate the outcomes of open airway resection on swallowing function in the postoperative period, and to identify patient and surgical factors that may be associated with the development of dysphagia following tracheal or cricotracheal resection in adult patients.
Methods
This retrospective cohort study was approved by the University of Southern California institutional review board. Informed consent was waived because all data were deidentified. A retrospective review of electronic medical records was conducted on consecutive patients who underwent tracheal or cricotracheal resection with subsequent end-to-end anastomosis at LAC+USC (Los Angeles County + University of Southern California) Medical Center and Keck Hospital of USC between February 2014 and May 2021.
Study Population
During the time period specified, all patients who underwent tracheal or cricotracheal resection with end-to-end anastomosis during the study period were eligible for inclusion in the study. Patients with tracheostomy at the time of surgery, as well as patients with stenosis of malignant origin, were eligible for inclusion. Exclusion criteria consisted of patients who underwent laryngotracheoplasty or posterior cricoid split with cartilage grafting.
Demographic characteristics including sex, age, ethnicity, and body mass index were collected. Medical comorbidities, prior history of traumatic brain injury, stroke, spinal cord injury, or other neurological disease were also reviewed. Preoperative information on gross deficits such as paraplegia, along with preoperative vocal fold abnormalities were noted. Surgical factors collected included cause, degree, length, and location of stenosis, length of resection, intraoperative laryngeal release technique, number of days required in the intensive care unit, and number of days until discharge. Dysphagia symptoms were measured as the primary outcome. Severity of dysphagia was quantified using the functional oral intake scale (FOIS)14 ranging from 1 to 7, with 1 representing no oral intake and 7 representing a full oral intake with a regular diet as categorized in the eTable in Supplement 1. The FOIS scores were recorded based on clinical evaluation preoperatively, and on postoperative days (PODs) 3, 5, and 7, on the day of discharge, and at the first follow-up appointment at the 1-month postoperative time point or later. Severe impairment of swallowing was defined as FOIS equal to or less than 3 in this present study. A FOIS score of 3 was chosen as it represents the cutoff for tube-dependent nutrition, a clinically significant measure for patients. As per our institutional protocol, all tracheal resection patients are evaluated by speech language pathology on POD 1, trialed with oral intake, and subsequently started on a clear liquid diet with advancement of diet as able with the goal of a regular diet by day of discharge.
Statistical Analysis
Summary statistics were presented using frequency (percentage) for categorical variables and mean (SD) or median (range) for continuous variables, dependent on distribution. Because of nonnormality, Kendall rank order correlation was performed to measure the monotonic association between continuous variables and FOIS scores at each time point.
Effect sizes were presented as Cliff delta or Kendall tau, as appropriate, along with corresponding 95% CIs. Values for Cliff delta vary between −1 and +1, and absolute values were interpreted as follows: 0 to 0.147 (negligible), 0.147 to 0.330 (small), 0.330 to 0.474 (medium), and values greater than 0.474 as (large). Kendall tau values range from −1 to +1, with 0 indicating no association and ±1 representing perfect association; absolute values were interpreted as follows: less than 0.10 (very weak), 0.10 to 0.19 (weak), 0.20 to 0.29 (moderate), and greater than or equal to 0.30 (strong). Normality was assessed using histograms and the Shapiro-Wilk test. All tests were 2-sided. All analyses were performed in R statistical software, version 4.2.1 (R Project for Statistical Computing).
Results
Fifty-four patients, consisting of 34 male adults and 20 female adults, underwent a tracheal or cricotracheal resection between February 2014 and May 2021 and were eligible for inclusion in this study (Table 1). The age at time of the procedure for participants ranged from 19 to 73 years, with a mean (SD) age of 47 (15.7) years. The indication for resection was tracheal stenosis due to prolonged intubation or tracheostomy-related trauma in 42 (78%) patients, papillary thyroid carcinoma involving the airway in 10 (19%) patients, and idiopathic stenosis in 2 (4%) patients. Fifteen (28%) patients had medical history significant for neurological disease including 7 with traumatic brain injury, 7 with stroke, 2 with aneurysm, and 5 with prior spinal cord injury. The mean (SD) time from surgery to postoperative follow-up visit was 47.4 (29.9) days.
Table 1. Description of the Study Population.
| Characteristic | Value, No. (%) |
|---|---|
| Sex | |
| Female | 20 (37) |
| Male | 34 (63) |
| Age, mean (SD) [range], y | 47 (15.7) [19-73] |
| Cause | |
| Intubation/tracheostomy trauma | 42 (78) |
| Papillary thyroid carcinoma | 10 (19) |
| Idiopathic | 2 (4) |
| Neurological history | |
| Yes | 15 (28) |
| No | 39 (72) |
| Procedure type | |
| Tracheal resection | 40 (74) |
| Cricotracheal resection | 14 (26) |
| Hyoid release (suprahyoid and infrahyoid) | |
| Yes | 36 (67) |
| No | 9 (17) |
| Unknown | 9 (17) |
| Length of resection, mean (SD) [range], cm | 3.8 (1.2) [2-6] |
Fourteen (26%) patients underwent cricotracheal resection while the remaining 40 (74%) patients underwent tracheal resection. The total length of resection segment ranged from 2 cm to 6 cm, with a mean (SD) length of 3.8 (1.2) cm. Thirty-six (67%) patients underwent both suprahyoid and infrahyoid laryngeal release techniques intraoperatively. Nine patients did not undergo laryngeal release, and the usage of release techniques was unable to be determined from the medical record for the remaining 9 patients. It is to be noted that the use of laryngeal release procedures was decided intraoperatively by the surgeon depending on the length of resection and the need to reduce tension on the anastomosis. All release procedures were performed by the senior author (K.O.) in the same manner. Suprahyoid and infrahyoid musculature are both removed from the hyoid between the lesser cornu and the contralateral lesser cornu, and a 1-cm middle segment of the hyoid bone was removed. All patients underwent blunt dissection of the anterior 180° portion of the trachea extending inferiorly to the level of the aortic arch. Patients were routinely extubated after surgery and T-tubes were not utilized in these cases.
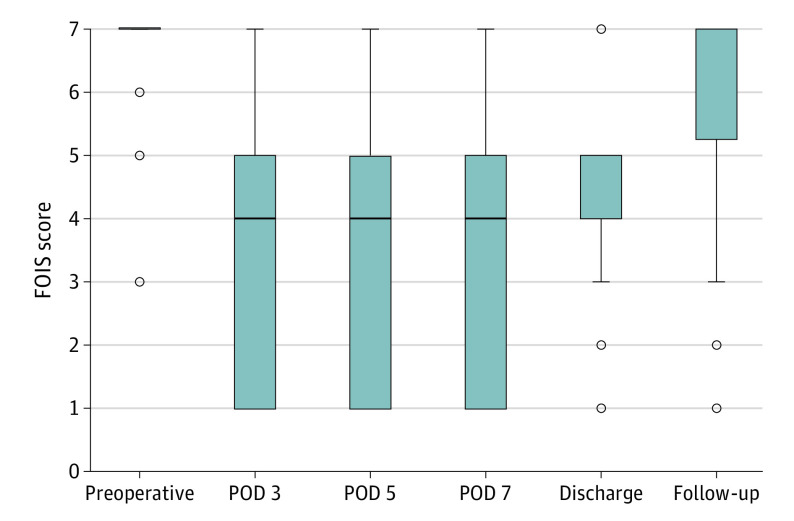
The FOIS scores were measured at various time points in the preoperative and postoperative course (Figure 1). The median (range) FOIS score for all patients preoperatively was 7 (3-7). In the immediate postoperative period, the FOIS score was 4 (1-7) on POD 3, POD 5, and POD 7. On the day of discharge, FOIS was 5 (1-7), and at the 1-month postoperative follow-up visit, it was 7 (1-7). Twenty-three (44.2%) of patients on POD 3, 20 (39.2%) on POD 5, 14 (45.2%) on POD 7, 12 (23.5%) on discharge, and 8 (15.7%) at follow-up visit had substantial limitations on oral intake with FOIS less than or equal to 3.
Figure 1. Postoperative Functional Oral Intake Scale (FOIS) Score.
Box plot of FOIS scores at varying time points including preoperatively, the immediate postoperative period by postoperative day (POD), and at 1-month follow-up for patients undergoing airway resection. The box represents the IQR. The top edge of the box is the upper quartile, the middle line in the box is the median, and the lower edge is the lower quartile. The connected lines on top of and underneath the box are the maximum and minimum, respectively. Outliers are represented as circle markers.
Increasing patient age showed a low-to-moderate strength of association with worse FOIS scores at all measured time points. These data (POD 3, POD 5, POD 7, and follow-up) are shown in Figure 2 (except day of discharge) (Kendall correlation coefficients: τ = −0.33; 95% CI, −0.51 to −0.15 on POD 3; τ = −0.38; 95% CI, −0.55 to −0.21 on POD 5; τ = −0.33; 95% CI, −0.58 to −0.08 on POD 7; τ = −0.22; 95% CI, −0.42 to −0.01 on day of discharge; and τ = −0.31; 95% CI, −0.53 to −0.09 at 1-month follow-up visit).
Figure 2. Correlation Between Age and Postoperative Functional Oral Intake Scale (FOIS) Score.
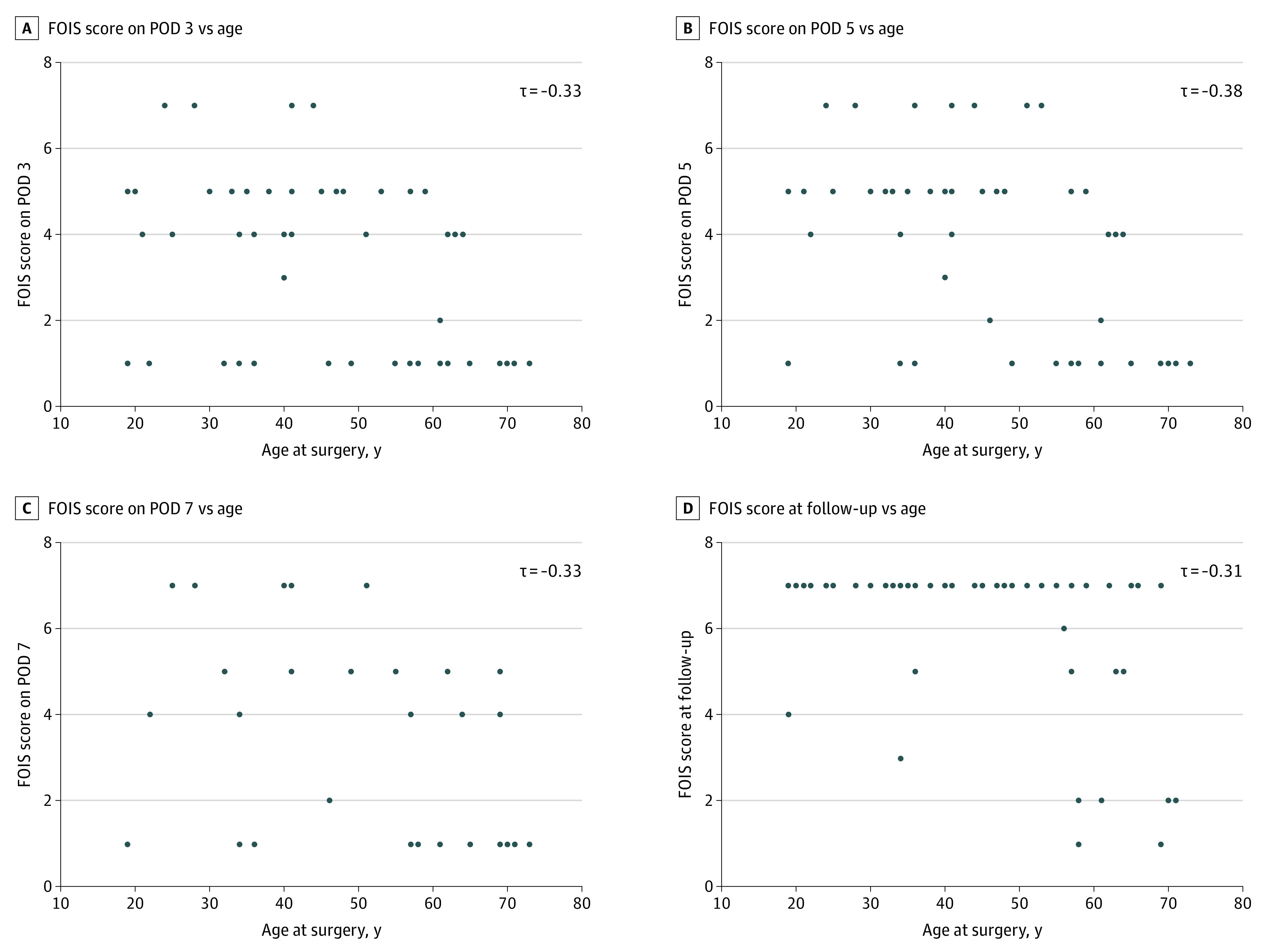
Correlation between age and FOIS score on (A) postoperative day (POD) 3, (B) POD 5, (C) POD 7, and (D) 1-month follow-up visit. Kendall tau is reported as the correlation coefficient. Each dot represents a single patient.
Procedure type showed a moderate association with FOIS score. Cricotracheal resection was moderately associated with lower FOIS score compared with tracheal resection alone on POD 3 (δ = −0.34; 95% CI, −0.59 to −0.03), POD 5 (δ = −0.32; 95% CI, −0.57 to −0.02), POD 7 (δ = −0.42; 95% CI, −0.59 to −0.03) and on the day of discharge (δ = −0.35; 95% CI, −0.60 to −0.04). There was a small difference in median scores between the 2 procedures at the 1-month follow-up visit (δ = −0.24; 95% CI, −0.56 to −0.11). A higher percentage of patients that underwent cricotracheal resection had severe impairment (FOIS score less than 3) compared with tracheal resection alone at 1-month follow-up visit (45.5% vs 7.7%; difference in proportion = 37.8%; 95% CI, 7.2%-68.4%).
The presence of prior traumatic brain injury or other neurological disease had a small to negligible difference in FOIS score as compared with no relevant injury or disease at any time point with Cliff delta (δ = 0.03; 95% CI, −0.31 to 0.36 on POD 3; δ = 0.11; 95% CI, −0.28 to 0.47 on POD 5, δ = 0.3; 95% CI, −0.25 to 0.70 on POD 7; δ = 0.15; 95% CI, −0.24 to 0.51 on the day of discharge, and δ = 0.27; 95% CI, −0.05 to 0.53 at follow-up). The correlation between resection length and FOIS score was weak at all measured time points with Kendall tau ranging from −0.04 to −0.23 (Table 2). There was a small to negligible difference in FOIS score between patients undergoing intraoperative laryngeal release compared with those who did not, with Cliff delta ranging from 0.02 to 0.32 (Table 3).
Table 2. Strength of Association Between Resection Length and Functional Oral Intake Scale Score at Each Time Period.
| Variable | Correlation coefficient (95% CI)a |
|---|---|
| FOIS Score | |
| POD 3 | −0.11 (−0.35 to 0.13) |
| POD 5 | −0.04 (−0.31 to 0.22) |
| POD 7 | −0.23 (−0.57 to 0.10) |
| At discharge | −0.19 (−0.43 to 0.09) |
| At follow-up | −0.09 (−0.35 to 0.17) |
Abbreviations: FOIS, functional oral intake scale; POD, postoperative day.
Kendall tau.
Table 3. Functional Oral Intake Scale Scores at Postoperative Time Points Stratified by the Usage of Laryngeal Release Techniques Intraoperatively.
| Variable | No. | Had intraoperative release, median (IQR) [range]a | Cliff delta (95% CI) | |
|---|---|---|---|---|
| No (n = 9) | Yes (n = 36) | |||
| FOIS Score | ||||
| POD 3 | 52 | 4 (4.5) [1 to 7] | 4 (4) [1 to 7] | 0.14 (−0.33 to 0.56) |
| POD 5 | 51 | 4.5 (4.5) [1 to 7] | 4 (4) [1 to 7] | 0.05 (−0.39 to 0.47) |
| POD 7 | 31 | 4 (4) [1 to 7] | 4 (4) [1 to 7] | 0.02 (−0.49 to 0.52) |
| At discharge | 51 | 6 (2.3) [2 to 7] | 5 (2.5) [1 to 7] | 0.32 (−0.13 to 0.66) |
| At follow-up | 51 | 7 (1) [2 to 7] | 7 (0) [1 to 7] | 0.03 (−0.31 to 0.35) |
Abbreviations: FOIS, functional oral intake scale; POD, postoperative day.
Nine patients were missing information on whether intraoperative release was performed.
Discussion
Dysphagia in the immediate period following tracheal resection procedures has commonly been discussed in the literature as a potential complication15,16; however, there have been few studies that aim to determine the underlying causes for adverse functional outcomes.12 While recent studies have identified various surgical factors that predispose to dysphagia following airway reconstruction including temporary stent placement11 and laryngeal release techniques,17 to our knowledge, the patient factors that predispose to dysphagia following open airway surgery have not yet been elucidated. The purpose of this retrospective cohort study was to analyze both patient and surgical factors that may predispose to swallowing difficulties and prolong the recovery period in adult patients undergoing tracheal resection with end-to-end anastomosis.
At every time point measured, increasing patient age had a low to moderate strength of association with lower FOIS scores, suggesting that age increases the severity of dysphagia experienced following tracheal resection and delays the return to normal preoperative diets. At baseline, the older adult population has a lower level of swallowing function.18 Disruption in the swallowing mechanism postoperatively may cause a greater functional deficit in older adults due to a lower baseline functional status, as evidenced by the worsened FOIS score at all time points with increasing age. Also, increased age and related measures of frailty have previously been associated with delayed recovery and adverse outcomes following surgery. A systematic review by Lin et al19 reported that across various studies using differing measures of frailty, there was strong evidence of increased mortality at 30 days, 90 days, and 1 year postoperatively, as well as an increase in postoperative complications and length of stay in the hospital. Given the existing literature, it is likely that delayed recovery from the disruption in soft tissues and cartilaginous structures involved in swallowing occurring during airway resection in patients of increased age contributes to greater severity and duration of dysphagia. Considering these findings, patient age should be carefully considered when choosing the appropriate treatment for tracheal stenosis, and patients of advanced age should be counseled to expect increased severity and duration of swallowing difficulties following tracheal resection.
In the literature, dysphagia is commonly observed in patients following traumatic brain injury20,21 and stroke.22 However, in the present study there was a small to negligible association between relevant neurological history and postoperative dysphagia at any time point when compared with patients without any neurological history. In the current study, the methods did not specify the timing and recovery of previous neurological injury, which could theoretically have an effect on the extent of postoperative dysphagia.
Cricotracheal resection in comparison to tracheal resection alone was moderately associated with increased FOIS scores in the postoperative period and throughout their hospital stay with the 95% CI not including 0. However, there was a small difference in median FOIS scores between the 2 procedures at the 1-month follow-up, giving evidence that patient recovery and long-term functional outcomes from both cricotracheal and tracheal resection are similar.
Although usage of laryngeal release is traditionally thought to cause greater severity of swallowing difficulties due to increased disruption of soft tissue and musculature during tracheal resection, the association was not supported by this study at any time point postoperatively. Similarly, we show that for the present cohort of patients, the length of trachea that was resected did not correlate to any change in dysphagia and diet after the surgery. Mohsen et al17 reported that for patients undergoing long-segment tracheal resection (>4 cm) with intraoperative laryngeal release procedures, only 17 of 52 patients experienced transient swallowing dysfunction, with the majority of those patients only experiencing mild grade 1 dysphagia symptoms. The results of our current study, along with the recent literature, suggest that longer segments of trachea can be resected, and laryngeal release maneuvers can be performed during tracheal resection without any association with postoperative swallowing difficulty, contrary to the traditional perspective on causes of dysphagia following open airway surgery in the literature. However, as the current study is an observational study and is limited to patients undergoing surgery at only 2 institutions, there may be significant interinstitutional differences in tracheal resection technique causing variable amounts of disruption to surrounding structures intraoperatively that may contribute to a wider range of swallowing outcomes after surgery than is observed in the present study’s data. Also, as both suprahyoid and infrahyoid release was conducted concurrently on the patients in this study and performed in the same manner by the senior author, the differences between each respective technique’s effect on postoperative dysphagia remains unclear.
Limitations
The current study was subject to several limitations. As this study is retrospective in nature, the present data collection was limited to the variables that have been previously recorded. As we investigated swallowing outcomes in the immediate postsurgical period up to the initial follow-up visit, typically conducted at 1 month after surgery, we are limited in our ability to observe dysphagia symptoms over the long-term recovery period. Given the long-term functional outcomes are still unclear in the literature, future studies should be performed with structured observation and follow-up over an extended length of time postoperatively, especially for patients with residual deficits after their 1-month follow-up. Another important limitation was the small sample size of this cohort of patients that were included in the present study. The small sample size led to imprecision in our estimates and limits our ability to make definitive conclusions on certain patient factors predictive of dysphagia. For example, while we hypothesized that relevant neurological history would predict postsurgical swallowing difficulty, no difference was identified in this study, with 15 patients meeting the relevant criteria. Future studies including a larger sample size would be helpful for more accurately assessing any potential relationship between neurological history and postsurgical swallowing difficulty. In the present cohort, 19% of patients preoperatively had airway obstruction secondary to papillary thyroid carcinoma that necessitated the procedure. None of these patients had been irradiated prior to surgery. It is important to note that it is possible that patients who receive treatment such as radiation therapy may experience greater difficulty swallowing postoperatively. The present study’s primary outcome was measured using FOIS, initially described by Crary et al14 to document the functional level of oral intake of food and nutrition and was strongly associated with dysphagia severity when cross-validated with videofluoroscopic examination. However, the use of FOIS still limits our ability to assess the subjective symptoms of swallowing difficulty that may possibly persist after surgery despite appropriate oral intake as measured by FOIS. Use of validated patient-reported outcomes (PRO) in dysphagia, such as the quality of life in swallowing disorders (SWAL-QOL), may better represent the patient perspective on complications and recovery following tracheal resection. Despite these limitations, this study serves to add to the growing body of literature focused on patient factors predictive of dysphagia after airway resection and can serve to generate other hypotheses regarding swallowing outcomes for future investigations.
Future directions include studying a larger sample of patients to detect other predictive patient-related factors of dysphagia and incorporating PRO measures both preoperatively and postoperatively to better understand the patient perspective on functional outcomes. This study identified factors that are predictive of dysphagia following tracheal resection and can help both the surgeon and patient to make a more informed decision regarding the potential complications and recovery when considering open airway resection.
Conclusions
This retrospective cohort study demonstrates that dysphagia is commonly encountered in the postoperative period following tracheal resection in adult patients, but recovery to baseline swallowing function and preoperative diet generally occurs within the first month following surgery. Increased age at the time of surgery was associated with increased dysphagia symptoms postoperatively and delayed return to baseline diet and swallowing. Understanding risk factors for postoperative dysphagia in tracheal resection is crucial for appropriate patient selection and to adequately counsel patients considering tracheal resection procedures.
eTable 1. Functional Oral Intake Scale
Data Sharing Statement
References
- 1.Grillo HC, Mark EJ, Mathisen DJ, Wain JC. Idiopathic laryngotracheal stenosis and its management. Ann Thorac Surg. 1993;56(1):80-87. doi: 10.1016/0003-4975(93)90406-8 [DOI] [PubMed] [Google Scholar]
- 2.Kastanos N, Estopá Miró R, Marín Perez A, Xaubet Mir A, Agustí-Vidal A. Laryngotracheal injury due to endotracheal intubation: incidence, evolution, and predisposing factors—a prospective long-term study. Crit Care Med. 1983;11(5):362-367. doi: 10.1097/00003246-198305000-00009 [DOI] [PubMed] [Google Scholar]
- 3.Dane TEB, King EG. A prospective study of complications after tracheostomy for assisted ventilation. Chest. 1975;67(4):398-404. doi: 10.1378/chest.67.4.398 [DOI] [PubMed] [Google Scholar]
- 4.Gelbard A, Francis DO, Sandulache VC, Simmons JC, Donovan DT, Ongkasuwan J. Causes and consequences of adult laryngotracheal stenosis. Laryngoscope. 2015;125(5):1137-1143. doi: 10.1002/lary.24956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wynn R, Har-El G, Lim JW. Tracheal resection with end-to-end anastomosis for benign tracheal stenosis. Ann Otol Rhinol Laryngol. 2004;113(8):613-617. doi: 10.1177/000348940411300803 [DOI] [PubMed] [Google Scholar]
- 6.Mansour KA, Lee RB, Miller JI. Tracheal resections: lessons learned. Ann Thorac Surg. 1994;57(5):1120-1125. doi: 10.1016/0003-4975(94)91340-4 [DOI] [PubMed] [Google Scholar]
- 7.Stoelben E, Aleksanyan A. Technique of laryngotracheal resection in subglottic stenosis. J Thorac Dis. 2020;12(10):6152-6162. doi: 10.21037/jtd.2020.04.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kane Miller C, Linck J, Willging JP. Duration and extent of dysphagia following pediatric airway reconstruction. Int J Pediatr Otorhinolaryngol. 2009;73(4):573-579. doi: 10.1016/j.ijporl.2008.12.024 [DOI] [PubMed] [Google Scholar]
- 9.Clunie GM, Belsi A, Roe JWG, Alexander CM, Sandhu G, McGregor A. Not just dyspnoea: swallowing as a concern for adults with laryngotracheal stenosis undergoing airway reconstruction. Dysphagia. 2022;37(2):365-374. doi: 10.1007/s00455-021-10287-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Biller HF, Munier MA. Combined infrahyoid and inferior constrictor muscle release for tension-free anastomosis during primary tracheal repair. Otolaryngol Head Neck Surg. 1992;107(3):430-433. doi: 10.1177/019459989210700315 [DOI] [PubMed] [Google Scholar]
- 11.Lennon CJ, Gelbard A, Bartow C, Garrett CG, Netterville JL, Wootten CT. Dysphagia following airway reconstruction in adults. JAMA Otolaryngol Head Neck Surg. 2016;142(1):20-24. doi: 10.1001/jamaoto.2015.2562 [DOI] [PubMed] [Google Scholar]
- 12.Clunie GM, Roe JWG, Alexander C, Sandhu G, McGregor A. Voice and swallowing outcomes following airway reconstruction in adults: a systematic review. Laryngoscope. 2021;131(1):146-157. doi: 10.1002/lary.28494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clunie GM, Kinshuck AJ, Sandhu GS, Roe JWG. Voice and swallowing outcomes for adults undergoing reconstructive surgery for laryngotracheal stenosis. Curr Opin Otolaryngol Head Neck Surg. 2017;25(3):195-199. doi: 10.1097/MOO.0000000000000362 [DOI] [PubMed] [Google Scholar]
- 14.Crary MA, Mann GDC, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86(8):1516-1520. doi: 10.1016/j.apmr.2004.11.049 [DOI] [PubMed] [Google Scholar]
- 15.Bibas BJ, Terra RM, Oliveira Junior AL, et al. Predictors for postoperative complications after tracheal resection. Ann Thorac Surg. 2014;98(1):277-282. doi: 10.1016/j.athoracsur.2014.03.019 [DOI] [PubMed] [Google Scholar]
- 16.El-Fattah AMA, Kamal E, Am HE, Fouda M, Elwahab AEMA, Tawfik A. Cervical tracheal resection with cricotracheal anastomosis: experience in adults with grade III-IV tracheal stenosis. J Laryngol Otol. 2011;125(6):614-619. doi: 10.1017/S0022215110002537 [DOI] [PubMed] [Google Scholar]
- 17.Mohsen T, Abou Zeid A, Abdelfattah I, Mosleh M, Adel W, Helal A. Outcome after long-segment tracheal resection: study of 52 cases. Eur J Cardiothorac Surg. 2018;53(6):1186-1191. doi: 10.1093/ejcts/ezx475 [DOI] [PubMed] [Google Scholar]
- 18.Thiyagalingam S, Kulinski AE, Thorsteinsdottir B, Shindelar KL, Takahashi PY. Dysphagia in older adults. Mayo Clin Proc. 2021;96(2):488-497. doi: 10.1016/j.mayocp.2020.08.001 [DOI] [PubMed] [Google Scholar]
- 19.Lin H-S, Watts JN, Peel NM, Hubbard RE. Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr. 2016;16(1):157. doi: 10.1186/s12877-016-0329-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Terré R, Mearin F. Prospective evaluation of oro-pharyngeal dysphagia after severe traumatic brain injury. Brain Inj. 2007;21(13-14):1411-1417. doi: 10.1080/02699050701785096 [DOI] [PubMed] [Google Scholar]
- 21.Howle AA, Baguley IJ, Brown L. Management of dysphagia following traumatic brain injury. Curr Phys Med Rehabil Rep. 2014;2:219-230. doi: 10.1007/s40141-014-0064-z [DOI] [Google Scholar]
- 22.Terré R, Mearin F. Oropharyngeal dysphagia after the acute phase of stroke: predictors of aspiration. Neurogastroenterol Motil. 2006;18(3):200-205. doi: 10.1111/j.1365-2982.2005.00729.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Functional Oral Intake Scale
Data Sharing Statement