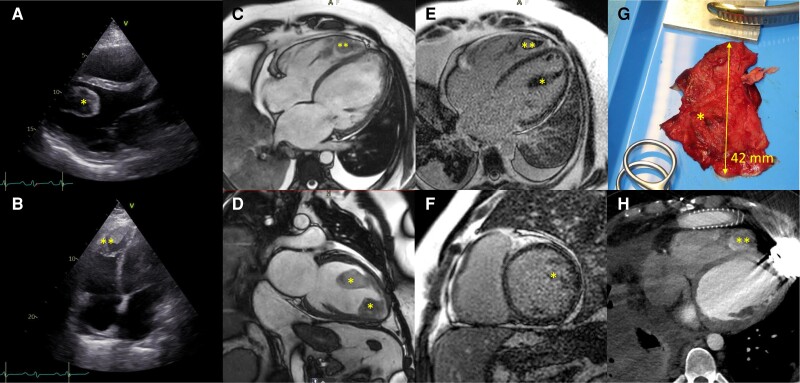
A 39-year-old male patient, known with morbid obesity [body mass index (BMI) 45 kg/m²], was referred with progressive shortness of breath over the last 2 years. He reported acute worsening over the past 3 weeks and malleolar oedema and haemoptysis over the past 3 days. No fever was recorded. Electrocardiogram showed sinus tachycardia with SIQIIITIII sign, and troponins (78 ng/L, reference < 14 ng/L), D-dimers (>4400 µg/L, reference < 550 µg/L), N-terminal pronatriuretic peptide (8370 ng/L, reference < 125 ng/L), and lactate levels (9.1 mmol/L) were markedly elevated. COVID polymerase chain reaction (PCR) on admission was positive (3–5 log copies). Pulmonary computed tomography (CT) showed bilateral embolism in segmental pulmonary arteries with accompanying infarctions. Furthermore, intracardiac biventricular masses were noted, which were identified as intraventricular thrombi on cardiac ultrasound due to low flow (Panels A and B). The left and right ventricles were largely dilated [left ventricular end-diastolic diameter (LVEDD) 7.5 cm] with severely impaired systolic function [left ventricular ejection fraction (LVEF) 11%; right ventricular ejection fraction (RVEF) 12%]. On cardiac magnetic resonance imaging (MRI), T1 and T2 values and extracellular volume were elevated, suggesting either myocardial oedema or inflammation. There was no focal late gadolinium enhancement (LGE) (Panels C and D showing cine images, Panels E and F showing LGE images; see Supplementary material online, Videos S1–S4). The patient was admitted to the cardiac intensive care unit because of rapid progression to stage D cardiogenic shock according to the Society for Cardiovascular Angiography and Interventions (SCAI) score and was promptly started on therapeutic unfractionated heparin infusion, inotropes (milrinone), and intravenous diuretics. After 11 days of highly intensive medical treatment, including administration of levosimendan and achieving 10 L of fluid loss, the patient remained in refractory cardiogenic shock (SCAI-C), still requiring high doses of inotropes. The case was discussed in the multidisciplinary heart team, and a left ventricular assist device (LVAD) was implanted as a ‘Bridge-to-Decision’ strategy with resection of the left ventricular (LV) thrombus (Panel G: LV thrombus surgical specimen, Panel H: postoperative CT). Postoperatively, he had a rapid recovery, and vitamin K antagonists, as standard therapy in LVAD-supported patients, were initiated as long-term anticoagulation therapy. Three weeks after surgery, the patient was discharged home. Six months after discharge, he is doing quite well and his weight has dropped to a BMI of 34 kg/m². Ahead of a heart transplant, additional bariatric surgery will presumably be provided before active listing.
Left ventricular (*) and right ventricular (**) thrombi on cardiac ultrasound (panels A and B), cardiac MRI (panels C and D showing cine images; panels E and F showing LGE images), postoperative resection specimen (panel G) in postoperative CT images with LVAD in situ.
Supplementary Material
Contributor Information
Matthias Verbesselt, Department of Cardiovascular Diseases, University Hospital Leuven, Herestraat 49, 3000 Leuven, Belgium.
Jan Bogaert, Department of Radiology, University Hospital Leuven, Leuven, Belgium.
Thomas Castelein, Department of Cardiology, Cardiovascular Center Aalst, OLV Clinic Aalst, Aalst, Belgium.
Bernard Stockman, Department of Cardiovascular Surgery, Cardiovascular Center Aalst, OLV Clinic Aalst, Aalst, Belgium.
Bart Meyns, Department of Cardiovascular Surgery, University Hospital Leuven, Leuven, Belgium.
Christophe Vandenbriele, Department of Cardiovascular Diseases, University Hospital Leuven, Leuven, Belgium; Department of Critical Care, Royal Brompton & Harefield Hospitals, Guy’s and St Thomas’ NHS Foundation Trust, London, UK.
Supplementary material
Supplementary material is available at European Heart Journal – Case Reports.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for the submission and publication of this case report, including images and associated text, has been obtained from the patient in line with COPE guidance.
Funding: None declared.
Data availability: No new data were generated or analysed in support of this research.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.