INTRODUCTION
Cerebral palsy (CP) is the most common physical disability in children.1 Children with CP receive physical therapy services across the lifespan to address motor and functional impairments.2 Understanding the optimal dose of physical therapy needed for positive outcomes is a national priority.3 Kolobe and colleagues define dose according to the American College of Sports Medicine as including frequency, intensity, time and type.4 A framework for evaluating how physical therapy dose impacts outcomes begins with understanding the type of therapy intervention delivered.5 A systematic review delineates types of interventions for CP into 4 grades of recommendations based on evidence to support or refute them: green ‘do it’, yellow ‘probably should do it’, yellow ‘probably should not do it’, and red ‘do not do it’.6,7 Although more is known about which types of therapy interventions are evidence based, details about the delivery of these interventions in clinical settings are limited.
The literature provides some information about the focus of interventions preferred or provided by pediatric therapists. In 2 studies8,9 therapists responded to what they would do but this may not reflect what they actually do in practice. Others9,10 examined limited types of interventions and did not include the wide spectrum of physical therapy interventions provided to children with CP. In other studies,9,11,12 families completed questionnaires about the focus of therapy services provided to children. Together, these studies are limited by narrow age ranges and limited detail on intervention type; however, we can infer that therapy provided to children with CP focuses on primary and secondary impairments and may not represent the most evidence-informed practice.
Much less is known about specific types of physical therapy intervention actually delivered across wide age ranges for children with CP. Using billing information from the electronic health record (EHR), our group examined physical therapy intervention according to the International Classification of Function, Disability and Health delivered in a hospital based outpatient setting for 1 year with over 400 children with CP across all ages.13 The largest category of intervention addressed activity (47%), followed by body structure and function (25%), environment (21%), and examination (7%). While this study included a wide age range of individuals with CP (1–33 years), results were limited to billing information.
The CP intervention studies previously cited,8–13 lack detailed information about specific intervention types delivered to individuals with CP. More recently, using practice-based evidence methods, the PTCOUNTS study14,15 provided greater detail about the types of physical therapy delivered to school-age (5–12 years) children (primarily with CP) in the United States. The most frequent interventions over the academic year were in the categories of neuromuscular, mobility and musculoskeletal; and the least frequent interventions were positioning, equipment, cardiopulmonary, sensory and integumentary. There was limited use of evidence-based interventions in the school setting, such as constraint induced movement therapy, body weight supported treadmill training, and cardiopulmonary/fitness interventions. Encouragingly, therapists were not using interventions known to lack evidence (e.g., neurodevelopmental treatment and passive range of motion). The type of intervention delivered varied by functional level but not by age. The school based PTCOUNTS study provided greater detail about therapy type than previous studies, but it was limited by age and setting.
The efficacy of evidence-based intervention (EBI) delivery in hospital-based outpatient clinical settings across all ages of children with CP is unknown. The studies cited above provide only a partial view of current therapy provision for children with CP. Understanding how typical therapy interventions vary from EBI practice facilitates efforts to increase adherence with EBI and maximize outcomes for children. This information would also support education and training of providers and identify future research directions. The purpose of this study was to characterize the type of physical therapy intervention delivered in routine clinical care in a large sample of children with CP, and to examine variation by age, Gross Motor Function Classification System (GMFCS),16 race, and insurance type.
METHODS
Design
This study used a retrospective cohort design Using the EHR from a tertiary medical center.
Procedures
Cincinnati Children’s Hospital Medical Center Institutional Review Board approval was obtained for retrospective data collection from the EHR (EPIC) between November 1, 2017- October 31, 2018 at a tertiary care pediatric outpatient therapy division where approximately 50 physical therapists deliver care to individuals with CP. Demographic information and physical therapy treatment data were extracted from EPIC. As part of clinical practice, therapists select details of intervention type delivered at each treatment session using a standardized EHR documentation form adapted from PTCOUNTs and posted as a common data element form for CP (PT individual session case report form found at https://commondataelements.ninds.nih.gov/cerebral%20palsy). A previous publication17 describes development and testing of the form in the EHR and includes the form and training materials as supplemental digital materials one [available at: http://links.lww.com/PPT/A251] and two [available at: http://links.lww.com/PPT/A252].
Data were checked for accuracy and completeness. Eighty-two treatment interventions were grouped under the categories of neuromuscular, musculoskeletal, modalities, adaptive equipment/orthotic management, orthoses, equipment, positioning, assistive technology, cardiopulmonary, integumentary, education/training and other. For each category, the therapist selected any number of intervention types delivered during that session (e.g., discrete intervention types under the neuromuscular category include motor control, repetitive task specific training, balance, facilitation, and postural control). The flowsheet was used when documenting physical therapy treatment visits. Therapy visits that did not include discrete treatment data included visits that addressed screening, multidisciplinary clinic evaluations, new visit evaluations, gait laboratory visits, or other non-treatment visits.
Once the population of children with CP was identified, the EHR records were explored, including the content of therapy visits to determine inclusion for analysis. Individuals remained in the cohort if 75% or more of outpatient therapy visits included details on treatment interventions delivered at that visit. For all qualifying individuals, therapist-selected intervention categories and specific types were extracted from the therapy flowsheet. Sessions that were missing treatment intervention type data were excluded. Intervention types were summarized as continuous variables based on counts per session and mapped to the 4 grades of recommendation based on evidence to support or refute them: green ‘do it’, yellow ‘probably should do it’, yellow ‘probably should not do it’, and red ‘do not do it’.7 (Table 3). Frequency and percentages were reported for each graded category and a category for intervention not graded. Green ‘do it’ and yellow ‘probably should do it’ interventions were combined into an EBI category and produced a raw count and a percentage of EBI for each individual across all sessions.
TABLE 3.
Description of Physical Therapy Interventions Grouped by Evidence Grade Delivered to Individuals in the Year (4335 Treatment Sessions)
| Interventions by Evidence Grade | Documentation Flowsheet Intervention Category | Documentation Flowsheet Intervention Type | Counts for Intervention Type n (%) |
|---|---|---|---|
| Green ‘do it’ | 13549 (48) | ||
| Home program | Education | Caregiver education /home program | 3552 (12.5) |
| Goal directed training/functional training | Neuromuscular | Motor control | 2443 (9) |
| Strength training | musculoskeletal | Functional strengthening | 2359 (8) |
| Goal directed training/functional training | Neuromuscular | Repetitive task specific training | 2069 (7) |
| Home program | Education | Patient education /home program | 1942 (7) |
| Strength Training | Musculoskeletal | Strength progressive resistive exercises | 717 (2.5) |
| Fitness training | Cardiopulmonary | Aerobic conditioning | 225 <1 (1) |
| Casting | Musculoskeletal | Serial cast ankle | 242 <1 (1) |
| Yellow ‘probably should it’ | 5168 (18) | ||
| Orthotics | Orthotics | Ankle foot orthosis | 1163 (4) |
| Treadmill training | Equipment | Treadmill | 794 (3) |
| Assistive tech/equipment | Adaptive Equipment | Fit adjust | 631 (2) |
| Assistive tech/equipment | Equipment | Body weight support | 497 (2) |
| Assistive tech/equipment | Equipment | Walker | 424 (1) |
| Assistive tech/equipment | Equipment | Gait trainer | 237 (*) |
| Assistive tech/equipment | Adaptive Equipment | Prescription | 252 (*) |
| Assistive tech/equipment | Equipment | Robotic | 203 (*) |
| Electrical stimulation | Modalities | Neuromuscular electrical stimulation | 215 (*) |
| Assistive tech/equipment | Adaptive Equipment | Training | 194 (*) |
| Assistive technology/equipment | Equipment | Manual wheelchair | 137 (*) |
| Assistive tech/equipment | Adaptive Equipment | Fabrication | 140 (*) |
| Hydrotherapy | Modalities | Aquatics | 120 (*) |
| Assistive tech/equipment | Adaptive Equipment | Maintenance/repair | 57 (*) |
| Assistive tech/equipment | Equipment | Stander | 35 (*) |
| Orthotics | Orthotics | Taping | 21 (*) |
| Biofeedback | Modalities | Biofeedback | 15 (*) |
| Assistive tech/equip | Equipment | Power wheelchair | 13 (*) |
| Orthotics | Orthotics | Shoe inserts | 18 (*) |
| Orthotics | Orthotics | Functional electrical stimulation neuroprosthesis | 15 (*) |
| Assistive tech/equipment | Adaptive equipment | Ergo universal | 1 (*) |
| Assistive tech/equipment | Assistive technology | Switch | 3 (*) |
| Assistive techno/equipment | Assistive technology | Virtual reality | 1 (*) |
| Yellow ‘probably should not do it’ | 564 (2) | ||
| Stretching manual | Musculoskeletal | Passive range of motion | 539 (2) |
| Massage | Musculoskeletal | Massage | 25 (*) |
| Red ‘do not do’ | 948 (3) | ||
| NDT handling | Neuromuscular | Facilitation | 948 (3) |
| Ungraded | 8560 (30) | ||
| Ungraded | Neuromuscular | Postural Control | 2494 (9) |
| Ungraded | Neuromuscular | Balance | 2317 (8) |
| Ungraded | Integumentary | Skin check | 718 (3) |
| Ungraded | Equipment | Bench | 584 (2) |
| Ungraded | Musculoskeletal | Weight bearing | 530 1.8 (2) |
| Ungraded | Musculoskeletal | Stretch prolonged | 518 1.8 (2) |
| Ungraded | Orthotics | Knee immobilizer | 183 (*) |
| Ungraded | Equipment | Therapy ball | 128 (*) |
| Ungraded | Equipment | Wall rail furniture | 115 (*) |
| Ungraded | Equipment | Balance beam | 89 (*) |
| Ungraded | Musculoskeletal | Manual therapy | 79 (*) |
| Ungraded | Orthotics | Supramalleolar | 71 (*) |
| Ungraded | Assistive technology | Electronic device | 60 (*) |
| Ungraded | Equipment | Stationary bike | 30 (*) |
| Ungraded | Equipment | Elliptical | 26 (*) |
| Ungraded | Orthotics | Foot orthosis | 34 (*) |
| Ungraded | Equipment | Push toy | 22 (*) |
| Ungraded | Integumentary | Pressure relief | 15 (*) |
| Ungraded | Integumentary | Position changes | 17 (*) |
| Ungraded | Assistive technology | Pictures | 12 () |
| Ungraded | Assistive technology | Video gaming | 12 (*) |
| Ungraded | Assistive technology | Adaptive toy | 13 (*) |
| Ungraded | Cardiopulmonary | Breathing | 10 (*) |
| Ungraded | Assistive technology | Pet therapy | 6 (*) |
| Ungraded | Equipment | Upper extremity ergometer | 5 (*) |
| Ungraded | Musculoskeletal | Serial cast knee | 4 (*) |
| Ungraded | Cardiopulmonary | Energy conservation | 2 (*) |
| Ungraded | Equipment | Parallel bars | 1 (*) |
| Ungraded | Equipment | Seated stepper | 1 (*) |
| Ungraded | Modalities | Hot Cold | 1 (*) |
| TOTAL n (%) | 28,344 (100) | ||
Less than 1%
Age was grouped into 4 categories <5, 5–12, 12– 18 and >18 as these represent meaningful transition points for individuals with CP when a change in service delivery might occur. Gross Motor Function Classification System (GMFCS) level16 is documented in each treatment note and was assigned based on the most frequent rating for children 2 years and older, and type/topography of CP was assigned based on information in the EHR problem list. Because the GMFCS is less reliable in younger children we did not assign a GMFCS level for children less than 2 years. Insurance type was recorded for insurance the child had during the study year and categorized as public, private, both, or other/none.
R software version 3.5.3 was used to analyze data. Parametric tests were used for data with a normal distribution and nonparametric tests for data without a normal distribution. Mean, standard deviation, median and interquartile range were calculated for continuous variables and frequencies and percentages for categorical variables. The Chi square test was used to compare the rates between independent groups. Two-sided independent t test and Fisher exact test were used for categorical variables. Pairwise comparisons with Benjamini-Hochberg (BH) adjustment were used to examine variation by age, GMFCS, race and insurance type. Statistical results were interpreted at 95% confidence interval with statistical significance set at P < .05 (2-tailed).
RESULTS
Participants
A total of 618 children were seen in the outpatient physical therapy department during the study period, with 465 children (mean age 9.5 years, SD 7) meeting criteria to be included in the analysis. There was a significant difference (p<0.01) in mean age between individuals included (n =465, 9.5 years (sd 7) and individuals not included (n= 153, 11 years (sd 6.4). In addition, the mean number of visits was significantly different (p< 0.001) between the groups (11 versus 6 respectively) (Table 1)
TABLE 1.
Characteristics of Individuals Seen in Outpatient Physical Therapy Division During the Study Period
| N=618 | N= 465 included | N=153 excluded | |
|---|---|---|---|
| Age (years)* | |||
| Mean (sd) | 10 (6.6) | 9.5 (sd 7) | 11 (6) |
| Median (Range) | 8.5 (5, 14) | 8 (5, 13) | 11 (6, 16) |
| Age groupings n (%) | |||
| Below 5 | 163 (27) | 131 (28) | 32 (21) |
| 5-<12 | 260 (42) | 205 (44) | 55 (36) |
| 12 -<18 | 121 (20) | 74 (16) | 47 (31) |
| 18 and Over | 74 (12) | 55 (12) | 19 (12) |
| Gender Male n (%) | 357 (58) | 270 (58) | 87 (57) |
| Race n (%) | |||
| White | 458 (74) | 340 (73) | 118 (77) |
| African American | 89 (14) | 68 (15) | 21 (14) |
| Other | 71 (11) | 57 (12) | 14 (9) |
| Ethnicity n (%) | |||
| Non-Hispanic | 578 (94) | 437 (94) | 141 (92) |
| Hispanic | 39 (6) | 27 (6) | 12 (8) |
| Patient Refused | 1 (0) | 1 (0) | 0 (0) |
| Number of visits* | |||
| Mean n (%) | 9.8 (11) | 11 (sd12) | 6 (7) |
| Median (Range) | 7 (3,13) | 8, (4, 15) | 3 (2, 7) |
| GMFCS n (%) | |||
| I | 158 (26) | 113 (24) | 45 (29) |
| II | 137 (22) | 95 (20) | 42 (28) |
| III | 85 (14) | 71 (15) | 14 (9) |
| IV | 106 (17) | 84 (18) | 22 (14) |
| V | 80 (13) | 59 (13) | 21 (14) |
| Less than 2 years old | 52 (8) | 43 (9) | 9 (6) |
| Type of cerebral palsy n (%) | |||
| Spastic hemiplegia | 149 (31) | 114 (30) | 35 (38) |
| Spastic diplegia | 89 (19) | 75 (19) | 14 (15) |
| Spastic quadriplegia | 143 (30) | 116 (30) | 27 (29) |
| Ataxic | 3 (1) | 3 (1) | 0 (0) |
| Athetoid | 5 (1) | 4 (1) | 1 (1) |
| Other unspecified | 95 (20) | 78 (20) | 17 (18) |
| Insurance n (%) | |||
| Private | 111 (18) | 79 (17) | 32 (21) |
| Public | 297 (49) | 229 (50) | 68 (44) |
| Both | 195 (32) | 146 (32) | 49 (32) |
| Other/None/self-pay | 15 (2) | 11 (2) | 4 (3) |
Abbreviation: GMFCS, Gross Motor Function Classification System.
Significant difference between included and excluded groups for the variables of age (p<0.01) and number of visits (p< 0.001) Percentages do not equal 100 due to rounding.
Interventions delivered
A total of 28,344 physical therapy interventions were delivered over 4335 treatment visits. Each individual received a median of 34 (range 11–81) total interventions during the year. The interventions delivered represent 10 of the 11 possible intervention categories (Table 2). The largest percentage of interventions selected by therapists were in the neuromuscular category (36%) and no interventions were selected from the positioning category.
TABLE 2.
Description of the Number of Interventions Delivered for Each Category Type
| Intervention Categories | Number of Selections (% of total) |
|---|---|
| Neuromuscular | 10,271 (36) |
| Musculoskeletal | 5013 (18) |
| Education | 5494 (19) |
| Equipment | 3341 (12) |
| Orthotics | 1505 (5) |
| Adaptive equipment/orthotic management | 1275 (4) |
| Integumentary | 750 (3) |
| Modalities | 351 (1) |
| Cardiopulmonary | 237 (1) |
| Assistive technology | 107 (<1) |
| Positioning | 0 (0) |
| Total | 28,344 |
Evidence-based grades of intervention types
Overall, 13,549 (48%) intervention type selections were green ‘do it’, 5168 (18%) yellow ‘probably should do’, 564 (2%) yellow ‘probably should not do’, 948 (3%) red ‘do not do it’, and 8560 (30%) not graded. Figure 1 graphs the percentage of intervention delivered per individual by the graded intervention category. Violin plots in Figure 1 depict the median, interquartile range, and density distribution (width of each violin plot) for each graded category. The shape of the distribution indicates the green interventions are more normally distributed than other categories and that the percent of yellow ‘probably should not do’ and red ‘do not do’ interventions are highly concentrated around the median with clusters (double humps) in the distribution of the data.18
Figure 1.
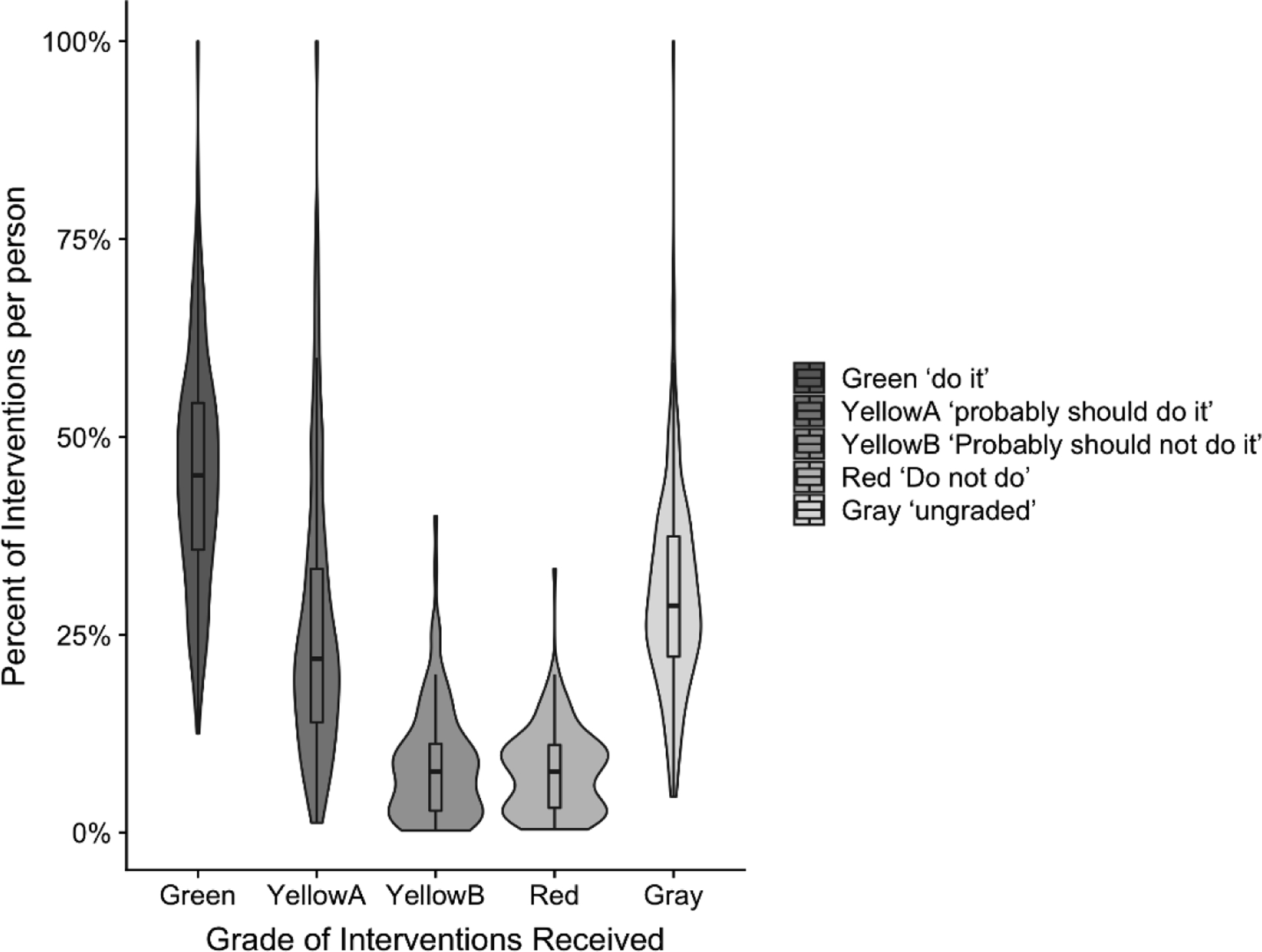
Percent of interventions per individual for the evidence grades, green ‘do it’, yellow ‘probably should do it’, yellow ‘probably should not do it’, red ‘do not do it’ and ungraded.
Violin plots indicate the percent of interventions per individual for each category. The box and whisker plots indicate median score (middle line), bars show interquartile ranges, and violin width represents the density distribution of the data. Wider sections of the violin plot represent a higher probability that members of the population will take on the given value; the narrower sections represent a lower probability.
The most frequently delivered green ‘do it’ interventions were motor control (9%), functional strengthening (8%) and caregiver education (2.5%). The most frequently delivered yellow ‘probably should do’ interventions were ankle foot orthoses (4%), treadmill training (3%) and fit or adjustment of adaptive equipment (2%). The only yellow ‘probably should not do’ interventions were manual stretching/passive range of motion and massage; and red ‘do not do’ was facilitation. Postural control, balance, and skin check were the most frequently delivered ungraded interventions (Table 3).
Total count of interventions per individual for each graded category
Across the 1 year period, each individual received a median of 16 (range 5–40) green ‘do it’ interventions, 7 (range 3–16) yellow ‘probably should do’ interventions, 3 (range 1–6) yellow ‘probably should not do’ interventions, 4 (range 2–8) red ‘do not do’ interventions, and 11 (range 4–27) ungraded interventions.
Variation in amount of EBI (green ‘do it’ + yellow ‘probably should do’) by child characteristics
When examining variation in EBI (green ‘do it’ and yellow ‘probably should do’) by GMFCS level, age group, race, gender and type of insurance, significant variation was demonstrated only across GMFCS levels. Significant differences were found between GMFCS levels V and most other levels (V and I (p=0.04), V and II (p=0.04), V and III (p<0.001), V and IV (p<0.001)) and between GMFCS level III and most other levels (III and I (p<0.001), III and II (p<0.001) III and V (p<0.001), III and <2 not classified (p=.003) (Table 4).
TABLE 4.
Variation in Evidence Based Intervention (EBI)^ Delivery by Gross Motor Function Classification System (GMFCS), Age Group, Race, Gender and Type of Insurance
| Variable | Participants n=465 | Raw count interventions (all grades) | Raw count of EBI^ | Median count EBI per individual (Range) |
|---|---|---|---|---|
| GMFCS * | ||||
| I | 113 | 6075 | 3968 | 25 (9–46) |
| II | 95 | 4891 | 3405 | 20 (7.5–52) |
| III | 71 | 6710 | 4713 | 55 (12–94.5) |
| IV | 84 | 6458 | 4206 | 26 (7–74) |
| V | 59 | 1638 | 949 | 8 (4–19) |
| Under 2 | 43 | 2572 | 1476 | 21 (11–48.5) |
| Age Group | ||||
| Below 5 years | 131 | 8507 | 5276 | 27 (10.5–60) |
| 5- <12 years | 205 | 12761 | 8601 | 24 (9–55) |
| 12- <18 years | 74 | 4443 | 3043 | 12.5 (5–52) |
| 18 and older | 55 | 2633 | 1797 | 12 (4.5–41) |
| Race | ||||
| Non white | 125 | 6125 | 4095 | 19 (7–40) |
| White | 340 | 22219 | 14622 | 23 (8–61.5) |
| Gender | ||||
| Female | 195 | 11966 | 7991 | 21 (7–57.5) |
| Male | 270 | 16378 | 10726 | 23 (7–54) |
| Type of Insurance | ||||
| Private | 79 | 4789 | 3148 | 29 (13–53) |
| Public | 229 | 12480 | 8012 | 17 (7–45) |
| Both | 146 | 10788 | 7353 | 23 (6–71) |
| Other | 11 | 287 | 204 | 17 (3.5–25.5) |
Abbreviations: GMFCS, Gross Motor Function Classification System; EBI, Evidence based intervention.
EBI includes green ‘do it’ and yellow ‘probably should do it’ interventions
Significant differences between Levels V and I (p=0.04), V and II (p=0.04), V and III (p<0.001), V and IV (p<0.001), and between III and I (p<0.001), III and II (p<0.001) III and V (p<0.001), III and Under 2 not classified (p=.003).
DISCUSSION
This study characterized physical therapy interventions delivered routinely during hospital-based outpatient clinical care by graded EBI (green ‘do it’ or yellow ‘probably should do’) and examined the variation by age, GMFCS Level, race and insurance type. Over 60 % of all interventions delivered were evidence-based in a large sample of children with CP. Green ‘do it’ interventions made up a majority of provided therapies at 48% and the percentage of provided therapy interventions decreased as the strength of evidence also decreased from green to yellow ‘probably should do’ to yellow ‘probably should not do’ to red ‘do not do’ In addition, the amount of EBI provided per person varied based on GMFCS level but not by age, gender, race or insurance type. Children classified as GMFCS Level III received the most EBI while GMFCS Level V received the least. The top 3 categories of intervention delivered were neuromuscular, musculoskeletal and education. The least common intervention categories were positioning, assistive technology and cardiopulmonary. These results identify where therapists at 1 institution are integrating evidence-based treatments into their sessions and identify areas for improvement.
When comparing our findings to other studies, there were similarities in predictors of variation in services delivered and differences in GMFCS grouping assignments, measurement strategies, and findings. Similarities include reporting variation in the amount of services delivered between GMFCS levels. Palisano and Jeffries measured amount of services in minutes and collapsed GMFCS levels using parent reports for information,11,15 while McCoy measured amount as the number of sessions, kept GMFCS levels separate, and used therapist documentation as we did.12 All 3 studies found more severely involved children received more sessions or minutes than other children. Our results demonstrated the opposite with the most severely involved (GMFCS V) receiving lower counts of EBI. We did not report minutes or number of sessions. Moreover, we found that children in GMFCS IV received more EBI than GMFCS V, but not different than other GMFCS levels. The prior studies11,12,15 found those at GMFCS I received the least amount of intervention. It seems logical that children at GMFCS I would receive the lowest count of interventions in the school setting.15 This is because children at GMFCS I can negotiate their educational environment and are less likely to qualify for therapy to meet educational needs. Children at level I demonstrate impairments in balance, coordination and speed19 which our results suggest may be more likely to be addressed by hospital based outpatient therapists. In our study, children classified as GMFCS III received the most EBI. There are potentially various explanations for this. Children classified as GMFCS III can use multiple methods for mobility and may require more intervention to address their varying mobility needs. However, future research is needed to understand this difference.
Results from the current study are consistent with our prior work20 describing total amount of therapy units billed differing by children’s GMFCS level. In both studies, children classified as GMFCS III received the most units or counts of intervention, and those classified as GMFCS V received the fewest. Furthermore, both studies examined hospital-based outpatient clinic therapy which may explain this relationship between severe motor impairment and reduced EBI, as children classified as GMFCS V may use more school-based services. Another explanation may be the limited range of EBI for more severely involved children. This is supported by a recent research agenda created by stakeholders rating the development and testing of effective interventions for children classified as GMFCS IV and V as a top ranked research priority.21
In contrast to our previous study that found younger children received more therapy units than older children,20 we did not find a difference in EBI by age groups. Both studies included wide age ranges, used the same age categories, and had similar age distribution. Current findings may reflect a change in practice at our institution as we have transitioned to intensive and episodic care for older children to address specific functional goals, possibly resulting in greater service delivery. Using a narrower age group, neither Palisano11 nor Jeffries15 found a difference in total amount of services received by age, while McCoy12 did not assess effects of age on number of sessions.
With regard to comparing type of intervention delivered in the present study to others, only the school based PTCOUNTS15 study provided similar details on intervention type and described total counts per student by broad intervention category (e.g., neuromuscular, musculoskeletal). Our study provided greater detail regarding the type of intervention within categories to examine against EBI grades. Similar to the school based PTCOUNTS study, we also report the neuromuscular category as the most frequent interventions selected. In addition, we described greater details about the frequency of individual neuromuscular interventions (e.g., motor control (9%), postural control (9%), balance (8%), and repetitive task specific practice (7%)) while the school based PTCOUNTS study, reported the use of primarily balance interventions with limited detail of other neuromuscular interventions. We replicated findings of a large number of musculoskeletal interventions including strengthening.
The amount of education/home program in the school-based PT COUNTS study and the present study suggests therapists are involving families and individuals in the rehabilitation process. Another commonality was the low frequency of cardiopulmonary and positioning interventions. We agree with previous authors15 that increasing the delivery of cardiopulmonary /fitness interventions is an area for improvement, especially given the sedentary lifestyles for individuals with CP as they age.22–24 It is possible that individuals in this study were participating in cardiopulmonary activities outside of therapy, but this information was not collected. With regard to our lack of selected interventions in the positioning category, our therapists felt this intervention was focused on the classroom setting and not necessarily applicable to outpatient treatment sessions. Following this study, we removed the positioning category from our documentation.
Another similarity between our results and the school based PTCOUNTS study is that therapists rarely use interventions that lack evidence including passive range of motion or facilitation/handling. Feedback from therapists in our study stated facilitation/handling was thought to be included during functional task practice and functional strengthening activities that required hand placements to aid in movements and not traditional neurodevelopmental therapy. In summary, both in the school setting and outpatient clinic, therapists deliver a majority of neuromuscular, musculoskeletal, and education interventions and spend relatively little time on positioning and cardiopulmonary interventions.
Different than the school based PTCOUNTS study, we report greater use of treadmill training in our setting. Equipment such as treadmills may be more available in the hospital-based outpatient environment. Treadmills can be expensive and require sufficient space to house, in addition to extra personnel and set up time which may not be available in a school setting. Our findings report higher rates of integumentary interventions than delivered in the school based PTCOUNTS study likely reflecting the amount of bracing and orthotic interventions provided in our hospital-based outpatient setting requiring skin checks.
Treatment environments in a school differ than the hospital-based outpatient clinic setting and may explain these observations. These differences contribute to our understanding of care across settings and highlight the contextual differences of service delivery in the 2 settings. School based services more often occur in natural environments such as the classroom, hallways, lunch room, stairs playground or even school bus.25 Differences between the environments also highlight the important need for therapists to coordinate and communicate across settings. One example to illustrate this would be a school aged child with CP who is walking but whose walking is contributing to difficulty keeping up with peers at school. One evidence based intervention to improve walking capacity is short burst interval treadmill training.26 Our results suggest this intervention is more likely to be delivered in the hospital-based outpatient setting where there is equipment, space and personnel to deliver the required intervention at the required frequency, but carryover to the child’s more natural environment (e.g., school) would be necessary to make a difference in the child’s performance/what the child actually does. The recent growth of telehealth services may provide a creative option to enhance coordination between settings. Studies that follow children across both the school and hospital-based outpatient clinic setting would render a more comprehensive picture of the child’s receipt of therapy services.
Other green ‘do it’ and yellow ‘probably should do’ interventions according to EBI grades, including early intervention, constraint therapy, vibration, and hippo therapy, were not captured in this study for various reasons. Early intervention is the term used to describe publicly funded state run programs that offer the services and supports that are available to babies and young children with delays and disabilities and their families (https://www.cdc.gov/ncbddd/actearly/parents/states.html) and is not delivered in the hospital based outpatient clinic setting. Constraint therapy is delivered by occupational therapists in our institution and was not assessed in this study. A similar method for documenting occupational therapy sessions will allow us to capture this information in future studies. Vibration is not an intervention provided at our institution perhaps due to lack of knowledge regarding its benefits and need for special equipment. Provision of vibration intervention has been identified as an area for improvement at our institution. Lastly, hippotherapy is available in our community and not accounted for during hospital-based outpatient clinic sessions.
Strengths and Limitations
Strengths of this study were inclusion of a large sample of children across all ages and GMFCS levels, novel use of a standardized flowsheet allowing for data harvesting from EPIC, and the level of detail about delivered intervention type. Moreover, this study ranked therapy based on EBI to facilitate a more nuanced understanding of what interventions were provided. Results from this institution cannot necessarily be generalized to other hospital-based outpatient clinic settings. The institution’s culture of continuous learning and improvement27 may have contributed to outcomes in the present study. A limitation of this study was not including other types of therapy visits (e.g., evaluation visits, gait analysis, and interdisciplinary clinic visit), visits with providers in other settings (private clinics, home, school), or the amount of practice or completion of therapy activities at home. Future studies should consider services provided in other settings, as well as, tracking therapy activities at home.
Type of intervention delivered is only 1 component of therapy dose as described by Kolobe et al.3 The present study did not report on intensity (how hard the child worked in the session), time spent during session, or frequency of visits. The standardized documentation flowsheet used in the current study includes these components of dose and will be explored in future publications. We were not able to assess the relationship between EBI and outcomes due to the variety of outcome measures administered to children with CP and time points throughout the year. Prospectively designed studies to allow for standardized outcome administration along with detailed treatment dose data from the EHR are needed. While statistically significant variation in EBI provision was noted, we are unsure if this difference is clinically meaningful. Other important questions that should be explored include understanding if there is a threshold amount of specific EBI that produces meaningful outcomes, if provision of ineffective therapy can dilute or eliminate the benefits of EBI, or how each component of dose (frequency, intensity, time and type) contributes to outcomes. These queries will require sophisticated analyses because in real-world practice, most therapy sessions are eclectic and include multiple interventions. Looking ahead, strategies from this study may inform work to combine data from multiple institutions for large pragmatic trials.
In conclusion, discrete documentation of intervention type in a flowsheet enabled us to understand what specific interventions therapists are delivering in a hospital-based outpatient setting, examine delivered intervention against evidence grades and define relationships between GMFCS and therapy provision. Further work is needed to determine if amount of EBI is related to better outcomes. Combining type of therapy intervention with other aspects of dose available from the flowsheet (intensity, time, and frequency) to create a multifactorial model may be useful in future studies to elucidate the role of each component of dose. We urge other centers to adopt a similar documentation system to support multi-site studies that advance our understanding of therapy dose and outcomes in children with CP.
Supplementary Material
Acknowledgements:
Julie Badylak PT for her technical assistance with data extraction and data base creation.
Grant Support:
This project was partially supported by grants from Research in Patient Services and the Academic Research Committee Cincinnati Children’s Hospital Medical Center
References
- 1.Christensen D, Van Naarden Braun K, Doernberg NS, et al. Prevalence of cerebral palsy, co-occurring autism spectrum disorders, and motor functioning - Autism and Developmental Disabilities Monitoring Network, USA, 2008. Dev Med Child Neurol. 2014;56(1):59–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Palisano RJ, Murr S. Intensity of therapy services: what are the considerations? Phys Occup Ther Pediatr. 2009;29(2):107–112. [DOI] [PubMed] [Google Scholar]
- 3.Kolobe TH, Christy JB, Gannotti ME, et al. Research summit III proceedings on dosing in children with an injured brain or cerebral palsy: executive summary. Phys Ther. 2014;94(7):907–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Medicine ACoS. ACSM’s guidelines for exercise testing and prescription. Tenth ed: Wolters Kluwer; 2018. [Google Scholar]
- 5.Gannotti ME, Christy JB, Heathcock JC, Kolobe TH. A path model for evaluating dosing parameters for children with cerebral palsy. Phys Ther. 2014;94(3):411–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Novak I, McIntyre S, Morgan C, et al. A systematic review of interventions for children with cerebral palsy: state of the evidence. Dev Med Child Neurol. 2013;55(10):885–910. [DOI] [PubMed] [Google Scholar]
- 7.Novak I, Morgan C, Fahey M, et al. State of the evidence traffic lights 2019: systematic review of interventions for preventing and treating children with cerebral palsy. Curr Neurol Neurosci Rep. 2020;20(2):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saleh MN, Korner-Bitensky N, Snider L, et al. Actual vs. best practices for young children with cerebral palsy: a survey of paediatric occupational therapists and physical therapists in Quebec, Canada. Dev Neurorehabil. 2008;11(1):60–80. [DOI] [PubMed] [Google Scholar]
- 9.Rackauskaite G, Uldall PW, Bech BH, Ostergaard JR. Impact of child and family characteristics on cerebral palsy treatment. Dev Med Child Neurol. 2015;57(10):948–954. [DOI] [PubMed] [Google Scholar]
- 10.Kruijsen-Terpstra AJ, Ellens M, Ketelaar M, et al. Child-focused and context-focused behaviors of physical and occupational therapists during treatment of young children with cerebral palsy. Phys Occup Ther Pediatr. 2016;36(4):363–375. [DOI] [PubMed] [Google Scholar]
- 11.Palisano RJ, Begnoche DM, Chiarello LA, Bartlett DJ, McCoy SW, Chang HJ. Amount and focus of physical therapy and occupational therapy for young children with cerebral palsy. Phys Occup Ther Pediatr. 2012;32(4):368–382. [DOI] [PubMed] [Google Scholar]
- 12.McCoy SW, Palisano R, Avery L, et al. Physical, occupational, and speech therapy for children with cerebral palsy. Dev Med Child Neurol. 2020;62(1):140–146. [DOI] [PubMed] [Google Scholar]
- 13.Bailes AF, Gannotti M, Fenchel M. Using the electronic medical record to study the association of child and environmental characteristics on the type of physical therapy services delivered to individuals with cerebral palsy. Physiotherapy Theory & Practice. 2017;33(8):644–652. [DOI] [PubMed] [Google Scholar]
- 14.Effgen SK, McCoy SW, Chiarello LA, Jeffries LM, Bush H. Physical therapy-related child outcomes in school: an example of practice-based evidence methodology. Pediatr Phys Ther. 2016;28(1):47–56. [DOI] [PubMed] [Google Scholar]
- 15.Jeffries LM, McCoy SW, Effgen SK, Chiarello LA, Villasante Tezanos AG. Description of the services, activities, and interventions within school-based physical therapist practices across the United States. Phys Ther. 2019;99(1):98–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39(4):214–223. [DOI] [PubMed] [Google Scholar]
- 17.Bailes AF, Strenk ML, Quatman-Yates C, Hobart J, Furnier A. Documenting physical therapy dose for individuals with cerebral palsy: a quality improvement initiative. Pediatr Phys Ther. 2019;31(3):234–241. [DOI] [PubMed] [Google Scholar]
- 18.Hintze JL, Nelson RD. Violin plots: a box plot density trace synergism. The American Statistician. 1998;52(2):181–184. [Google Scholar]
- 19.Glazebrook CM, Wright FV. Measuring advanced motor skills in children with cerebral palsy: further development of the Challenge module. Pediatr Phys Ther. 2014;26(2):201–213. [DOI] [PubMed] [Google Scholar]
- 20.Bailes AF, Succop P. Factors associated with physical therapy services received for individuals with cerebral palsy in an outpatient pediatric medical setting. Phys Ther. 2012;92(11):1411–1418. [DOI] [PubMed] [Google Scholar]
- 21.Gross PH, Bailes AF, Horn SD, et al. Setting a patient‐centered research agenda for cerebral palsy: a participatory action research initiative. Dev Med Child Neurol. 2018;60(12):1278–1284. [DOI] [PubMed] [Google Scholar]
- 22.Morgan P, McGinley J. Gait function and decline in adults with cerebral palsy: a systematic review. Disabil Rehabil. 2014;36(1):1–9. [DOI] [PubMed] [Google Scholar]
- 23.Ryan JM, Forde C, Hussey JM, Gormley J. Comparison of patterns of physical activity and sedentary behavior between children with cerebral palsy and children with typical development. Phys Ther. 2015;95(12):1609–1616. [DOI] [PubMed] [Google Scholar]
- 24.Nooijen CF, Slaman J, Stam HJ, Roebroeck ME, Berg-Emons RJ, Learn2Move Research G. Inactive and sedentary lifestyles amongst ambulatory adolescents and young adults with cerebral palsy. J Neuroeng Rehabil. 2014;11:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaminker MK, Chiarello LA, O’Neil ME, Dichter CG. Decision making for physical therapy service delivery in schools: a nationwide survey of pediatric physical therapists. Phys Ther. 2004;84(10):919–933. [PubMed] [Google Scholar]
- 26.Bjornson KF, Moreau N, Bodkin AW. Short-burst interval treadmill training walking capacity and performance in cerebral palsy: a pilot study. Dev Neurorehabil. 2019;22(2):126–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quatman-Yates CC, Paterno MV, Strenk ML, et al. A Model for Cultivating a Culture of Continuous Learning and Improvement: An Ethnographic Report. Adv Health Care Manag. 2019;18. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


