Abstract
Positive psychological interventions (PPIs), which aim to cultivate psychological well-being, have the potential to improve health behavior adherence. This systematic review summarized the existing literature on PPI studies with a health behavior outcome to examine study methodology, quality, and efficacy. Of the 27 identified studies, 20 measured physical activity, eight measured medication adherence, seven measured diet, and three measured smoking (eight targeted multiple behaviors). Twenty studies were randomized controlled trials (RCTs; 13 fully powered), and seven had a single-arm design. Study samples were usually adults (n = 21), majority non-Hispanic white (n = 15) and female (n = 14), and with a specific disease (e.g., diabetes, n = 16). Most interventions combined a PPI with health behavior-focused content (n = 17), used a remote delivery method (n = 17), and received a moderate or low study quality rating. Overall, 19/27 studies found a health behavior improvement of at least medium effect size, while six of the 13 studies powered to detect significant effects were statistically significant. Of the behaviors measured, physical activity was most likely to improve (14/20 studies). In summary, PPIs are being increasingly studied as a strategy to enhance health behavior adherence. The existing literature is limited by small sample size, low study quality and inconsistent intervention content and outcome measurement. Future research should establish the most effective components of PPIs that can be tailored to different populations, use objective health behavior measurement, and robustly examine the effects of PPIs on health behaviors in fully powered RCTs.
Introduction
Many chronic diseases require ongoing engagement in health behaviors to delay progression or prevent onset of further disease. These behaviors vary depending on the disease, but can include medication adherence, diet, physical activity, and abstinence from nicotine use. Adhering to these behaviors is often challenging. At least 35% of US adults do not meet national physical activity guidelines,1 and most individuals struggle to achieve a healthy diet (e.g., high consumption of fruits and vegetables).2 For chronic conditions such as hypertension, medication adherence is critical but remains challenging for many people.3,4 Interventions to modify these health behaviors can improve disease control, reduce mortality, and lower healthcare costs.5
Improving psychological well-being is a strategy that may assist with health behavior adherence.6 Positive psychological well-being is a broad construct encompassing factors such as positive affect, optimism, life purpose, personal growth, life satisfaction, and happiness.7 Importantly, it is not simply the absence of psychological distress. People with greater positive psychological well-being have been shown to engage in more healthy behaviors,8 independent of negative psychological states such as depression and anxiety that can impede disease management.9 Positive psychological interventions (PPIs) are a type of psychosocial intervention that aim to increase positive emotions, thoughts, and behaviors via completing specific, purposeful activities.10 PPIs typically require participants to complete and incorporate simple activities (e.g., acts of kindness, gratitude for daily events, self-affirmations, imagining a best possible future) into their daily lives to learn how to self-generate and increase focus on positive experiences. Because they do not target a specific negative construct as do most psychological interventions, they are broadly applicable to people with and without psychopathology.
While the majority of studies of PPIs examine psychological outcomes such as improved well-being or reduced depressive symptoms,11,12 researchers have begun to explore the effects of PPIs on health behaviors and associated physical health outcomes.13 Established behavior change methods (e.g., self-monitoring, goal-setting) can be effective, but do not target emotional correlates of behavior that can impede successful behavior change. PPIs could be an effective adjunctive strategy to improve the efficacy of behavior change techniques. Multiple meta-analyses have examined the effectiveness of PPIs on psychological outcomes in medical and general populations,12,14 but their effects on health behavior outcomes have not been reviewed to our knowledge. Specific applications of PPIs vary widely based on the targeted health behavior and population of interest. We conducted this review to provide an overview of the similarities and differences of these approaches, and to provide insight into their effectiveness on health behavior change.
Hence the primary aim of this study was to systematically review the extant literature on PPIs that assessed a health behavior outcome to shed light on the scope of such studies, specifically to understand in whom these PPIs have been tested, the format and content of the PPIs, what behaviors were measured, the rigor of existing studies, and whether PPIs appear to have efficacy regarding behavior change. Given that this is a relatively understudied topic, we included both randomized trials and single-arm studies, and included studies with the health behavior as a primary or secondary outcome.
Methods
Guidance and registration
This systematic review was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.15 It was registered on the international Prospective Register of Systematic Reviews (PROSPERO) on May 29, 2021 (CRD42021227969).
Study eligibility
To be included, studies were required to be clinical trials of interventions including a positive psychological component, defined as promoting positive emotions, thoughts, or behaviors, to increase the well-being of an individual or a group.16 Trials needed to include a health behavior (defined initially as physical activity, diet, medication adherence, tobacco use, or sleep) as an outcome. These behaviors were chosen as health-promoting acts over which an individual has direct control. We considered alcohol and other substance use, but ultimately chose to exclude them due to the strong addictive component. We retained tobacco use as it is highlighted as a key cardiac health behavior by the American Heart Association’s Life’s Simple 7.17 After review of included articles, we chose to exclude sleep as a health behavior because it was not conceptualized in the studies as a volitional behavior. Eligible study designs included randomized controlled trials (RCTs) and nonrandomized trials, as well as single-arm trials without a control condition. Study protocols, dissertations, unpublished studies, and pre-published or incomplete data (i.e., conference abstracts) were excluded. We limited our search to articles written in English or Spanish. While observational studies of psychological well-being constructs and health behaviors also provide useful information as to the potential role of PPIs, we chose not to include observational studies in the present review given that these data have been synthesized previously18 and we wanted to focus on intervention effects.
Search strategy
This review included searches of Pubmed, PsycINFO, and EMBASE from database inception until December 2020. References of included studies were also reviewed. The search strategy aimed to identify the targeted studies by requiring at least one positive psychology-related term, one intervention-related term, and one health behavior-related term. Terms related to positive psychology included: positive psycho*, resilience, positive affect, optimism, happiness, happy, gratitude, kindness, joy, and forgive*. Intervention-related terms included: intervention, treatment, program, trial, therapy, and randomly assigned. Finally, terms related to health behaviors included: health behavior, healthy behavior, physical activity, exercise, diet, eating, medication, smok*, sleep, tobacco, sedentar*, and sitting.
Study Selection Process
Eligible studies were imported into Covidence online software (https://www.covidence.org), and duplicates were removed. All titles and abstracts (n=863) and all full texts (n=126) were screened twice by a group of five independent reviewers (EF, EM, HA, JZ, RM). Disagreements were adjudicated by an independent reviewer (CC).
Data extraction
Data were extracted independently by four reviewers (EF, EM, JZ, RM; two reviewers extracted data from each study) with disagreements resolved through discussion to achieve consensus. Data extracted from each study included: sample size, study design, participant characteristics and demographics (age, gender, race/ethnicity, population type/medical diagnosis), intervention details (content of intervention and control group, length, delivery method), outcome measurement (health behavior(s), primary outcome, timing of measurements, measurement type), and results.
Risk of bias and quality assessment
Risk of bias was judged by the same independent reviewers as for data extraction (EF, EM, JZ, RM; two reviewers rated each study) using the Effective Public Health Practice Project (EPHPP) Quality Assessment Tool for Quantitative Studies.19,20 This tool assesses risk of bias on eight domains: selection bias; study design; confounders; blinding; data collection methods; withdrawals and drop-outs; intervention integrity; analyses. Ratings on these domains generate a global score (weak, moderate, or strong). Disagreements on each domain were resolved through discussion to achieve consensus.
Data analysis and synthesis
Due to the presence of substantial heterogeneity in study outcome and measurement of outcomes, performing a systematic review, rather than a quantitative meta-analysis, was deemed to be more appropriate. In order to summarize and synthesize the interventions, we created categories based on their structure, content, and delivery methods. We identified the specific positive psychological techniques used, any additional content of the interventions, the content and structure of control conditions when relevant, and the intensity of the intervention delivery.
Results
Study selection
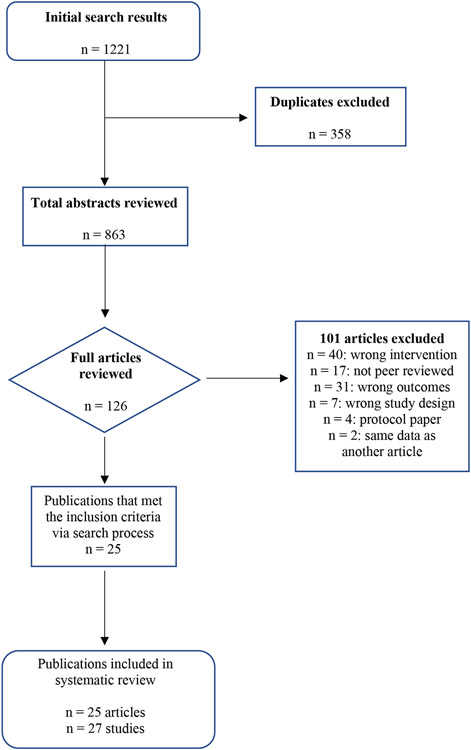
Figure 1 displays the PRISMA flow diagram for study inclusion. During the review process, the decision was made to exclude sleep as a health behavior, as the studies that measured sleep (n = 11) did so more as a well-being outcome rather than a volitional behavior.21,22 We also chose to exclude several studies of a school-based intervention that included aspects of positive psychology but was delivered in a much larger scale, programmatic way than the more individualistic interventions studied in the rest of the articles (n = 4; e.g., Kolle et al., 2020).23
Figure 1.
Search results and articles selection procedures
After these exclusions, this review included 27 studies in total, extracted from 25 articles published between 2001 and 2020. The most targeted health behavior was physical activity (20 studies) followed by medication adherence (eight studies), diet (seven studies), and smoking cessation (three studies). Eight studies targeted multiple health behaviors. While most studies (n = 20) were RCTs, seven were single-arm studies measuring pre-post changes. Only 13 of the RCTs were powered to detect significantly significant intervention effects.24-34 The remaining 14 studies were designed as feasibility and/or pilot studies.
Participant characteristics
Participant characteristics are detailed in Table 1. Participants in 21 of the studies were adults, with mean age ranging from 36 to 71.24-27,29-45 Five studies targeted young adults (usually college students) specifically,26,28,46,47 and one enrolled adolescents.48 In terms of race and ethnicity, more than half of the studies (n = 15) included a majority of non-Hispanic white participants.25,27,30,33,35-42,44,47,48 Six studies had a majority of racial/ethnic minority (e.g., Black, Hispanic) participants.24,31,32,34,43,45 One was conducted in Taiwan with Taiwanese participants,29 and the other 5 studies did not report race/ethnicity.26,28,46 Fourteen studies had a majority (>60%) of female participants,24-27,29,30,32,34,41,45-47 five had majority of male participants,31,33,35,38,43 and eight had between 40 and 60% female participants.28,36,37,39,40,42,44,48 Sixteen studies24-26,30-33,35-40,42,45,48 were designed for participants with a specific disease (most commonly diabetes and heart disease, less frequently hypertension, HIV, asthma, and neuromuscular disease) whereas the others included a broader population.26-29,34,41,43,44,46,47
Table 1.
Intervention and participant characteristics of included studies
| Study | N | Population | Race/Ethnicity | Agea | Gender | Intervention delivery mode |
Intervention duration |
|---|---|---|---|---|---|---|---|
| Randomized controlled trials | |||||||
| Boutin-Foster et al., 201624 | 177 | African American or black adults with hypertension | 100% African American or Black | 57 (10) | 69% F | Individual telephone calls plus written workbook | 12 months of phone calls every other month |
| Bradshaw et al., 200725 | 54 | Adults with type 2 diabetes | 92% White, 2% Hispanic, 0% Black, 4% Asian | 59 (11) | 65% F | In-person groups at diabetes center | 5 weeks of 90-minute meetings offered twice per week |
| Celano et al., 202035 | 45 | Adults with heart failure and suboptimal adherence to health behaviors | 87% White | 71 (10) | 27% F | Individual telephone calls plus written workbook | Initial in-person session plus 11 weeks of weekly 30-minute calls |
| Chandler et al., 201547 | 28 | Undergraduate students | 75% White, 4% Black, 14% Asian, 4% Hispanic, 4% Other | NR | 100% F | In-person groups | 4 weeks of weekly in-person groups |
| Emmons et al., 2003a26 | 192 | Undergraduate students | NR | NR | 73% F | Written exercises completed independently and turned in weekly | 10 weeks of weekly writing prompts |
| Emmons et al., 2003b26 | 157 | Undergraduate students | NR | NR | 75% F | Written exercises completed independently and turned in weekly | 2 weeks of daily writing prompts |
| Emmons et al., 2003c26 | 65 | Adults with neuromuscular disorders (e.g., post-polio, charco-marie-tooth, fascioscapulohumeral) | NR | 49 (NR) | 68% F | Written exercises completed independently and mailed in weekly | 3 weeks of daily writing prompts |
| Huffman et al., 201938 | 47 | Adults with acute coronary syndrome and low health behavior adherence | 92% White | 61 (11) | 33% F | Individual telephone calls plus written workbook | Initial in-person session plus 11 weeks of weekly 30-minute calls |
| Huffman et al., 202036 | 60 | Adults with type 2 diabetes and low physical activity | 75% Non-Hispanic White | 64 (10) | 52% F | Individual telephone calls plus written workbook | 12 weeks of weekly 30-minute calls |
| Jaser et al., 201448 | 39 | Adolescents with type 1 diabetes | 77% White | 15 (NR) | 51% F | Individual telephone calls | 8 weeks of phone calls every 2 weeks |
| Joutsenniemi et al., 201427 | 3274 | Finnish community sample | NR | 42 (NR) | 83% F | Individual emails | 4 months of emails delivered every 4-5 days |
| Kahler et al., 201544 | 66 | Community sample of smokers who want to quit | 81% White, 14% Black, 3% Hispanic, 5% Other | 46 (13) | 50% F | Individual in-person | 6 sessions over 7 weeks |
| Kersten et al., 201628 | 58 | Undergraduate students | NR | 19 (NR) | 57% F | Individual in-person | 4 sessions over 2 weeks |
| Lee et al., 201929 | 150 | Retired community-dwelling older adults in Taiwan | NR | 61 (7) | 79% F | In-person group sessions | 12 weeks of walking sessions with a trainer 3 times/week, plus 6 45-minute positive education group sessions |
| Mancuso et al., 201230 | 258 | Adults in New York City with mild-moderate asthma | 54% White, 22% Black, 31% Latino, 24% Other | 42 (12) | 75% F | Individual telephone calls plus written workbook | 12 months of phone calls every other month |
| Mann et al., 200145 | 40 | Women being treated for HIV | 35% Hispanic, 40% Black, 25% White | 39 (8) | 100% F | Individual in-person initial session with instruction to complete writing task at home | 4 weeks; instructed to write twice a week for 10 minutes at a time |
| Moskowitz et al., 201731 | 159 | People who had received HIV diagnosis in the past 3 months | 21% Black, 21% Latino, 3% Latino/Black, 45% White, 8% Asian/Pacific Islander, 1% Amer Indian | 36 (10) | 7% F | Individual in-person and telephone | 6 weeks of weekly sessions |
| Ogedegbe et al., 201232 | 256 | Black/African American adults with a diagnosis of hypertension | 100% Black | 58 (12) | 79% F | Individual telephone calls plus written workbook | 12 months of phone calls every other month |
| Peterson et al., 201233 | 242 | Adults who recently underwent percutaneous coronary intervention | 81% White, 11% Black, 4% Asian, 4% Multiracial, 13% Hispanic | 63 (11) | 30% F | Individual telephone calls plus written workbook | 12 months of phone calls every other month |
| Phillips et al., 201734 | 405 | Black or Hispanic adults with body mass index of 25-50 | 52% Black, 42% Hispanic, 5% Both | 48 (14) | 89% F | Individual in-person sessions | 1 year of sessions (weekly for months 1-3, biweekly for months 4-9, once monthly for months 10-12) |
| Single-arm studies | |||||||
| Celano, Freedman et al., 201839 | 11 | Adults with mild to moderate heart failure and suboptimal adherence to health behaviors | 90% White | 67 (11) | 40% F | Individual telephone calls plus written workbook | Initial in-person session plus 9 weeks of weekly 30-minute calls |
| Celano, Albanese et al., 201840 | 128 | Adults with an acute coronary syndrome and suboptimal adherence to health behaviors | 73% White | 63 (12) | 59% F | Individual telephone calls plus written workbook | Initial in-person session plus 7 weeks of weekly 30-minute calls |
| Celano et al., 201937 | 12 | Adults with non-insulin dependent type 2 diabetes and suboptimal physical activity | 83% White | 59 (11) | 42% F | Individual telephone calls plus written workbook | Initial in-person session plus 13 weeks of weekly 30-minute calls |
| DuBois et al., 201642 | 15 | Adults with type 2 diabetes and suboptimal health behavior adherence | 100% White | 61 (7) | 58% F | Individual telephone calls plus written workbook | 7 phone calls; weekly for 4 weeks, bi-weekly for 6 weeks |
| Hoeppner et al., 201943 | 30 | Adult nondaily smokers with current quit intention | 40% White, 43% Black, 17% Other, 7% Hispanic | 45 (14) | 27% F | Individual smartphone app | 3 weeks (1 week before and 2 weeks after quit day) of weekly sessions |
| Millstein et al., 202041 | 8 | Suboptimally active adults at risk of developing chronic diseases | 85% White | 63 (4) | 100% F | In-person group walking sessions plus written workbook | 8 weeks of weekly 90-minute in-person group sessions |
| O'Brien et al., 202046 | 134 | Higher education students in Ireland | NR | NR | 71% F | In-person group sessions (up to 150 students per session) | 2 90-minute sessions across 2 weeks |
NR = Not reported.
Age reported as M (SD).
Intervention characteristics
Intervention characteristics are detailed in Table 1. Interventions ranged in length from two weeks26,46 to one year.24,30,32-34 Delivery methods were most commonly remote (phone: n = 12,24,30,32,33,35-40,42,48 paper and/or online: n = 5).26,27,43 Eight interventions were delivered completely in-person,25,28,29,34,41,44,46,47 and two used a combination of in-person and remote delivery.31,45 Most interventions involved some sort of repeated contact with a study interventionist, typically on a weekly or bi-weekly basis.25,27-29,31,34-44,46-48 Several took a different approach, providing the majority of interventionist contact at the outset of the study, with instruction to continue activities independently for the duration of the study (sometimes with additional brief check-ins).24,26,30,32,33,45
Intervention Content
Positive psychological content
See Table 2 for detailed descriptions of interventions and comparators. While the specific content of the interventions varied, there were groupings of studies with similar interventions in terms of content and delivery. The first group was of six RCTs that used a positive affect induction approach.24,30,32-34,48 This involved teaching participants to think of things they perceived as positive or were proud of to increase positive affect and self-affirmation. All but one34 of these interventions also included mailing participants small gifts to increase positive affect. The next group with similar interventions included 10 studies that taught a series of positive psychology skills aimed at enhancing gratitude, personal strengths, and meaning in life.31,35-42,44 An interventionist taught each skill verbally in a given study session, and participants were given activities to practice the skill on their own between sessions. One other intervention utilized similar content as this group but was delivered via an app that prompted participants daily to use one of three randomly selected skills.43 Several interventions were focused on building resiliency more specifically, although they included components that were similar to other positive psychology programs (e.g., building personal strengths and psychosocial enrichment).25,47
Table 2.
Detailed description of interventions
| Study | Intervention Description | Comparator Description | HBa Focus |
|---|---|---|---|
| Randomized controlled trials | |||
| Boutin-Foster et al., 201624 | Positive affect induction. In addition to comparator content, received the positive affect and self-affirmation induction protocol and motivational interviewing. Positive affect strategy included focusing on positive thoughts that made them feel good throughout the day and receipt of unexpected gifts on a bimonthly basis. Self-affirmation strategy included instructing participants to think of core values that made them proud whenever they encountered a situation that would make it difficult to adhere to medications. Motivational interviewing for medication adherence was also provided. | Provided with educational workbook about hypertension and asked to develop a behavior contract that specified steps they would take to adhere to hypertension medications. Follow-up calls checked in on adherence to contract. | Yes |
| Bradshaw et al., 200725 | Building resiliency. The Resiliency Training Approach for Diabetes is an educational/experiential intervention intended to assist people with diabetes to initiate and develop self-directed behavior change. Approach focused on the psychosocial enrichment of the individual and the supportive relationship between the individual and their environment. Modules reinforced diabetes education literature and built on the concept of resiliency. | Treatment as usual from the Diabetes Center plus pedometer provision | Yes |
| Celano et al., 202035 | Enhancing gratitude, personal strengths, and meaning in life. The positive psychology-motivational interviewing intervention included provision of a treatment manual, a copy of the Learning to Live with Heart Failure guide, and a pedometer. Each phone session included a positive psychology exercise and discussion of a health behavior goal using motivational interviewing. Positive psychology exercises were grouped into three modules: gratitude (gratitude for positive events, expressing gratitude, capitalizing on positive events), strengths (remembering past successes, using personal strengths), and meaning (acts of kindness, the good life, enjoyable and meaningful activities). Motivational interviewing focused on adherence to physical activity, a low sodium diet, and medications. |
Active control: motivational interviewing alone. Participants received a treatment manual, the Learning to Live with Heart Failure guide, and a pedometer plus weekly phone calls about heart failure-specific health behaviors and identified potential behavior change. Treatment as usual: no phone sessions or treatment manual. |
Yes |
| Chandler et al., 201547 | Building resiliency. The Empower Resilience Intervention is a psycho-educational intervention that applies the ABCs of resilience (Active coping, Building strength, Cognitive flexibility, and Social support) using mindfulness-based stress reduction, education, structured writing, and social support with peer and facilitator interaction. Weekly topics included personality assets, resilience, adverse childhood experiences, physical health, preferred future, and social support. Each session included a brief guided mindfulness meditation, reviewing homework, learning about a topic, and freewriting on that topic. | Not clearly specified. Most likely not provided any intervention. | No |
| Emmons et al., 2003a26 | Targeting gratitude. Participants were prompted to write about up to 5 things in their lives they are grateful or thankful for that week. | In the "hassles" condition, participants were provided with a prompt to think back over today and list up to 5 hassles in their lives. In the "events" condition, participants were provided with a prompt to write up to 5 events in the last week that had an impact on them. | No |
| Emmons et al., 2003b26 | Targeting gratitude. Participants were prompted to write about up to 5 things in their lives they are grateful or thankful for that day. | In the "hassles" condition, participants were provided with a prompt to think back over today and list up to 5 hassles in their lives. In the "downward social comparison" condition, participants were provided with a prompt about comparing oneself to others and asked to write down ways in which one is better off than others. | No |
| Emmons et al., 2003c26 | Targeting gratitude. Participants were prompted to write about up to 5 things in their lives they are grateful or thankful for that day. | No writing assignment provided | No |
| Huffman et al., 201938 | Enhancing gratitude, personal strengths, and meaning in life. The positive psychology-motivational interviewing intervention included provision of a treatment manual and a pedometer. Each phone session included a positive psychology exercise and discussion of physical activity promotion using motivational interviewing. Positive psychology exercises were grouped into three modules: gratitude (gratitude for positive events, expressing gratitude, capitalizing on positive events), strengths (remembering past successes, using personal strengths), and meaning (acts of kindness, enjoyable and meaningful activities, the good life). | Motivational interviewing and health education: participants received a treatment manual and a pedometer plus weekly phone calls about cardiac-specific health behaviors and identified potential behavior change. | Yes |
| Huffman et al., 202036 | Enhancing gratitude, personal strengths, and meaning in life. The positive psychology-motivational interviewing intervention included provision of a treatment manual and a pedometer. Each phone session included a positive psychology exercise and discussion of a physical activity goal using motivational interviewing. Positive psychology exercises included: gratitude for positive events, gratitude letter, enjoyable and meaningful activities, recalling past successes, using personal strengths, and acts of kindness. | Motivational interviewing-enhanced behavioral counseling: time- and attention-matched control that focused on diabetes self-care behaviors (diet, physical activity, medication adherence, overall diabetes self-care). Participants received a treatment manual and a pedometer plus weekly phone calls about diabetes-specific health behaviors and identified potential behavior change. | Yes |
| Jaser et al., 201448 | Positive affect induction. The positive affect intervention was designed to increase positive affect through gratitude, self-affirmation, small gifts, and parental affirmations. Participants’ parents were instructed to provide weekly affirmations to participants on topics other than diabetes self-care by writing a short note or sending a text message. Participants were instructed to take a moment to notice things that made them happy (gratitude) and to remember something that they were proud of (self-affirmation) when it was time to check their blood sugar. They were reminded to use gratitude and self-affirmation during follow-up phone calls. Participants were also mailed a small gift every 2 weeks. | Mailed diabetes education materials every 2 weeks. | No |
| Joutsenniemi et al., 201427 | Enhancing happiness. Participants received emails every 4-5 days that included short texts that gave general information about happiness. The emails also included one of 4 different happiness exercises: good deeds, gratitude, optimism, and reducing rumination. | Received emails every 4-5 days that included short texts that gave general information about happiness. | No |
| Kahler et al., 201544 | Enhancing gratitude, personal strengths, and meaning in life. Standard smoking cessation as in control plus positive psychotherapy. At each session, positive psychology exercises were introduced, and participants were given related homework assignments. Exercises included Three Good Things, a Gratitude Letter, Savoring, Active-Constructive Responding, Savoring Acts of Kindness, and utilize their personal “Signature Strengths” (e.g., bravery, curiosity)—as assessed via the Values in Action Survey—to help them during their quit attempt. | Standard smoking cessation focused on problem solving regarding high-risk situations for smoking relapse, providing support, and encouraging participants to seek outside social support for quitting smoking. All participants received transdermal nicotine patch beginning on their scheduled quit date. Sessions also included 20-30 min of progressive muscle relaxation. | Yes |
| Kersten et al., 201628 | Targeting optimism. Participants were instructed to write about a past event that makes them feel nostalgic. | Write about an ordinary life event. | No |
| Lee et al., 201929 | Building social support. Attended pedometer walking exercise training sessions, plus received 6 positive education sessions designed based on self-determination theory and broaden-and-build theory to enhance positive self, emotion, motivation and self-efficacy to walk at least 30 min per day at least five times per week with family support and walking exercise companions. Sessions focused on instilling competency and self-efficacy of walking exercise, networking and becoming acquainted with other participants; gaining familiarity with communication skills required for positive support, sharing positive emotions associated with successful walking exercise to enhance partnership, increasing autonomy in walking exercise every day and building a healthy lifestyle. | In the pedometer walking exercise control, participants were encouraged to walk for at least 30 minutes 5 times/week and were given a booklet to write down pedometer readings each day. They walked on their own without any training. The pedometer walking exercise training control attended 30-minute walking exercise training sessions with a coach 3 times/week where heartrate was monitored and gradually increased throughout the intervention. | Yes |
| Mancuso et al., 201230 | Positive affect induction. In addition to comparator content, participants received the positive affect and self-affirmation induction protocol. Positive affect strategy included focusing on positive thoughts throughout the day and receipt of unexpected gifts on a bimonthly basis. Self-affirmation strategy instructed participants to think of things they were proud of when fulfilling the physical activity contract. Follow-up calls assessed adherence to the physical activity contract and how they applied positive affect and self-affirmation skills. | Provided with educational workbook about asthma, a pedometer, and asked to develop a behavior contract that specified the physical activity they would do. Follow-up calls checked in on adherence to contract. | Yes |
| Mann et al., 200145 | Targeting optimism. Instructed to write about a positive future where they only must take 1 pill each day for HIV. Told to write twice a week for 4 weeks for at least 10 minutes each time in provided journal. | Not asked to write in journals or imagine an optimistic future. Tried to time match first session with longer consent process | No |
| Moskowitz et al., 201731 | Enhancing gratitude, personal strengths, and meaning in life. Taught 8 empirically supported behavioral and cognitive skills for increasing positive affect: noting daily positive events, capitalizing on positive events, gratitude, mindfulness, positive reappraisal, focusing on personal strengths, setting and working toward attainable goals, and small acts of kindness | Also had 5 in-person sessions followed by 6th session by phone. Time/attention matched, consisted of an interview about different topics | No |
| Ogedegbe et al., 201232 | Positive affect induction. Educational workbook included an additional chapter about benefits of positive moments in overcoming obstacles to medication adherence. Positive affect strategy included focusing on positive thoughts that made them feel good throughout the day and receipt of unexpected gifts on a bimonthly basis. Self-affirmation strategy instructed participants to think of things they were proud of when fulfilling the physical activity contract. Follow-up calls assessed adherence to the medication contract and how they applied positive affect and self-affirmation skills. | Provided with culturally tailored educational workbook designed to (1) enhance knowledge about hypertension, (2) improve self-management behaviors, and (3) support goal-setting. Participants also signed a behavioral contract where they committed to taking medications as prescribed. Follow-up calls assessed behavioral contract adherence and confidence to take meds. | Yes |
| Peterson et al., 201233 | Positive affect induction. In addition to comparator content, participants received the positive affect and self-affirmation induction protocol. Positive affect strategy included focusing on positive thoughts throughout the day and receipt of unexpected gifts on a bimonthly basis. Self-affirmation strategy instructed participants to think of things they were proud of when fulfilling the physical activity contract. Follow-up calls assessed adherence to the physical activity contract and how they applied positive affect and self-affirmation skills. | Provided with culturally tailored educational workbook called "Living with Heart Disease: Taking Control after Angioplasty", a pedometer, and asked to develop a behavioral contract for self-selected physical activity. Follow-up calls checked in on adherence to contract. | Yes |
| Phillips et al., 201734 | Positive affect induction. In addition to comparator content, participants received the positive affect and self-affirmation induction protocol. They were instructed to identify small things that made them feel good and to think about those things when they first woke up and throughout their day. For the self-affirmation component, participants were asked to think of a proud moment in their lives and to remember that moment when faced with barriers to their new behavior goals | Small changes to eating: participants were guided to select one of 10 small change eating strategies to address their eating challenges (e.g., prepare main meal at home). They also set self-selected physical activity goals and made behavioral contract to adhere to goals at least 6 days/week. | Yes |
| Single-arm studies | |||
| Celano, Freedman et al., 201839 | Enhancing gratitude, personal strengths, and meaning in life. The positive psychology-motivational interviewing intervention included provision of a treatment manual, a copy of the Learning to Live with Heart Failure guide, and a pedometer. Each phone session included a positive psychology exercise and discussion of a health behavior goal using motivational interviewing. Positive psychology exercises were grouped into three modules: gratitude (gratitude for positive events, expressing gratitude), strengths (remembering past successes, using personal strengths), and meaning (acts of kindness, enjoyable and meaningful activities). Motivational interviewing focused on adherence to physical activity, a low sodium diet, and medications. | Yes | |
| Celano, Albanese et al., 201840 | Enhancing gratitude, personal strengths, and meaning in life. The positive psychology intervention included provision of a treatment manual. At each session, a new positive psychology exercise was introduced, and participants were encouraged to complete it during the week. Their practice was then reviewed the following week. Exercises included: enhancing gratitude for positive events, using personal strengths, expressing gratitude, capitalizing on positive events, remembering successes, performing enjoyable and meaningful activities, identifying humor in everyday life, and performing acts of kindness. This factorial trial compared effects of three treatment components: completing positive psychology exercises weekly vs. daily, inclusion/exclusion of motivational interviewing for a health behavior goal, and presence/absence of booster sessions after the core intervention. Therefore, participants were randomized on all three of these factors. For participants who received it, motivational interviewing focused mainly on physical activity though participants could choose another health behavior goal once they completed their activity goal. Booster sessions focused on ongoing use of positive psychology skills in everyday life and ongoing physical activity goal progress. | Yes | |
| Celano et al., 201937 | Enhancing gratitude, personal strengths, and meaning in life. The positive psychology-motivational interviewing intervention included provision of a treatment manual and a pedometer. Each phone session included a positive psychology exercise and discussion of physical activity promotion using motivational interviewing. Positive psychology exercises were grouped into three modules: gratitude (gratitude for positive events, expressing gratitude, capitalizing on positive events), strengths (remembering past successes, using personal strengths, using perseverance, humor in everyday life), and meaning (acts of kindness, enjoyable and meaningful activities, the good life). | Yes | |
| DuBois et al., 201642 | Enhancing gratitude, personal strengths, and meaning in life. The positive psychology intervention included provision of a treatment manual which described 6 positive psychology exercises that were also taught during treatment sessions. These included gratitude for positive events, personal strengths, gratitude letter, enjoyable and meaningful activities, recalling past successes, and acts of kindness. Participants were taught the skill, asked to practice it over the week and write about it, and then their practice was reviewed the following week. | No | |
| Hoeppner et al., 201943 | Enhancing gratitude, personal strengths, and meaning in life. The Smiling Instead of Smoking (SiS) app engages participants in daily positive psychology exercises over three weeks and provides behavioral support via three app-delivered sessions and ad lib user-initiated tools. One of three exercises is selected at random by the app each day. These include three good things, savoring, and experiencing kindness. Behavioral sessions assess smoking amount and triggers, advise quitting, assess readiness to quit and barriers, assist in setting a quit day, and provide support during quit attempt. Users could choose to monitor cigarette use, specify reasons for quitting, set reminders, enlist social support, view information on benefits of quitting, and address common concerns about quitting. | Yes | |
| Millstein et al., 202041 | Enhancing gratitude, personal strengths, and meaning in life. The positive psychology-motivational interviewing intervention included provision of a treatment manual and a Fitbit. Each group session included physical activity education and goal-setting using a motivational interviewing approach, plus a positive psychology exercise introduced each week paired with a relevant physical activity topic. Positive psychology exercises included: gratitude for health, perseverance, personal strengths, enjoyable and meaningful activities, remembering past successes, capitalizing on goals and health, and the good life. Group sessions ended with a group walk around the neighborhood. | Yes | |
| O'Brien et al., 202046 | Positive affirmations and building resiliency. State of Mind Ireland-Higher Education aims to develop knowledge and application of positive mental health strategies, increase well-being and prevent ill mental health, reduce mental health stigma and promote help-seeking behavior, and increase physical activity. Positive psychology components include discussing resilience to stress and positive affirmations. The intervention also includes education and goal-setting around physical activity. | Yes | |
HB: health behavior
Some of the interventions targeted gratitude or optimism specifically. The series of three studies reported by Emmons and colleagues26 asked participants to write down five things from the past week for which they were grateful. The optimism-focused interventions included writing about a positive future related to disease management (i.e., taking only 1 pill each day for HIV) twice per week for at least 10 minutes each time,45 and writing about a nostalgic event.28 The other interventions included unique “packages” of positive psychological tools. Joutsenniemi and colleagues sent emails that included readings from a book about happiness in addition to exercises aimed at increasing happiness.27 Lee and colleagues focused on building social support to promote walking.29 Finally, O’Brien and colleagues delivered an intervention to students including positive psychological components related to positive affirmations and building resilience to stress.46
Additional intervention content
While a subset of interventions included only psychological approaches (n = 10),26-28,31,42,45,47,48 most interventions combined the positive psychological content with a behavior change component directly addressing the health behavior being measured, such as motivational interviewing, goal-setting, or self-monitoring (n = 17).24,25,29,30,32-41,43,44,46
Comparator characteristics
Of the 20 studies that included control conditions, two had a control group that received no intervention.26,47 The rest provided some sort of active comparator intervention. Ten comparator conditions included behavior change techniques targeting the health behavior(s) being measured (e.g., motivational interviewing, goal-setting).24,29,30,32-36,38,44 Two included educational content about that health behavior48 or provision of a pedometer25 and the other six involved an attention-matched activity that was unrelated to the health behavior.26-28,31,45
Outcome characteristics and measurement
Table 3 details outcome measurement for each study. Physical activity was the most commonly measured health behavior outcome, with 20 studies including it either alone or in combination with other health behaviors. Most studies (n = 11) measured it via self-report;25-27,30,33,34,42,46,47 seven studies used a gold standard objective accelerometer measurement,35-41 and two used other objective step counters.28,29 There was significant variability among the self-report measures used. Two studies used the validated Paffenbarger Physical Activity and Exercise Index30,33,49 while the others used single-item or self-generated questions about physical activity amount. Two of the studies did not assess actual physical activity level, rather they asked about barriers to physical activity25 or meeting a self-identified physical activity goal.34
Table 3.
Health behavior outcome measurement and intervention effect.
| Study | Health Behavior (primary/ secondary) |
Measurement Type | Effect |
|---|---|---|---|
| Randomized controlled trials | |||
| Boutin-Foster et al., 201624 | Medication adherence (secondary) | Morisky Adherence Scale: 4-item well-validated scale | Medication adherence: -- |
| Bradshaw et al., 200725 | Physical activity, diet (not defined) | Questionnaire developed for the study. Physical activity item asked, "how many days per week do you exercise?" Diet item asked, "how do you decide what to eat?" with 4 response options. | Physical activity: -- Diet: 3 months ↑*; 6 months -- |
| Celano et al., 202035 | Physical activity, medication adherence, diet (secondary) | Physical activity: MVPA (minutes/day), overall physical activity (steps/day) using Actigraph accelerometer. Medication adherence: Self-Report Medication Adherence. Diet: sodium intake (Scored Sodium Questionnaire). |
Physical activity: 12-week MVPA ↑; 24-week MVPA ↑; 12-week steps --; 24-week steps -- Medication adherence: 12-week ↑; 24-week ↑ Diet: 12-week --; 24-week -- |
| Chandler et al., 201547 | Smoking cessation, physical activity (secondary) | Health Behavior Questionnaire (consists of 5 items assessing cigarette use, alcohol use, drug use, sexual activity, and physical activity). | Physical activity: ↑* Cigarette use: -- |
| Emmons et al., 2003a26 | Physical activity (secondary) | Self-report of hours of exercise for the week | Physical activity: ↑* compared to "hassles" control; --compared to "events" control. |
| Emmons et al., 2003b26 | Physical activity (secondary) | Self-report of minutes of exercise per day | Physical activity: -- |
| Emmons et al., 2003c26 | Physical activity (secondary) | Yes/no question if they had exercised that day | Physical activity: -- |
| Huffman et al., 201938 | Physical activity (secondary) | MVPA and steps per day measured with Actigraph accelerometer, and self-reported MET minutes/week measured with IPAQ. | Physical activity: 12-week MVPA ↑; 24-week MVPA ↑*; 12-week steps ↑*; 24-week steps ↑ |
| Huffman et al., 202036 | Physical activity (secondary) | MVPA (minutes/day), overall physical activity (steps/day) using Actigraph accelerometer | Physical activity: 8-week MVPA ↑*; 16-week MVPA ↑; 8-week steps ↑*; 16-week steps ↑ |
| Jaser et al., 201448 | Blood glucose monitoring frequency (primary) | Blood glucose meter downloads, self-report via the Self Care Inventory | Blood glucose monitoring adherence: meter downloads --; self-report ↑* |
| Joutsenniemi et al., 201427 | Physical activity (secondary) | Single item about leisure time physical activity: “How much do you exercise and strain yourself physically in your leisure time?” | Physical activity: -- |
| Kahler et al., 201544 | Smoking cessation (primary) | Seven-day point-prevalence smoking abstinence was assessed 8, 16, and 26 weeks after quit date via self-report and biochemical verification. | Smoking cessation: ↑* |
| Kersten et al., 201628 | Physical activity (not defined) | Fitbit steps | Physical activity: ↑* |
| Lee et al., 201929 | Physical activity (primary) | Self-reported steps from provided pedometer | Physical activity: ↑* |
| Mancuso et al., 201230 | Physical activity (primary) | Self-report via Paffenbarger Index | Physical activity: -- |
| Mann et al., 200145 | Medication adherence (secondary) | 5-item general measure of adherence from RAND Medical Outcomes Study with 3 additional items added to assess HIV medication regimen specifically. | Medication adherence: -- |
| Moskowitz et al., 201731 | Medication adherence (secondary) | Self-reported number of doses of antiretroviral therapy missed in the past 6 days (dichotomized into any vs none) | Medication adherence: -- |
| Ogedegbe et al., 201232 | Medication adherence (primary) | Electronic pill monitors counted the number of times the pill bottle was opened each day compared to the number of times they were supposed to take medications each day. | Medication adherence: ↑* |
| Peterson et al., 201233 | Physical activity (primary) | Self-report via Paffenbarger Index | Physical activity: ↑* |
| Phillips et al., 201734 | Diet, physical activity (secondary) | Diet: Behavioral Risk Factor Surveillance System to measure fruit and vegetable consumption Physical activity: adherence to self-chosen goals |
Diet: -- Physical activity: -- |
| Single-arm studies | |||
| Celano, Freedman et al., 201839 | Physical activity, medication adherence, diet (secondary) | Physical activity: MVPA (minutes/day), overall physical activity (steps/day) using Actigraph accelerometer. Medication adherence: Self-Report Medication Adherence. Diet: sodium intake (Scored Sodium Questionnaire). |
Physical activity: MVPA --; steps ↑
Medication adherence: ↑* Diet: ↑ |
| Celano, Albanese et al., 201840 | Physical activity (secondary) | Self-reported with single physical activity item of the Medical Outcomes Study Specific Adherence Scale (MOS) | Physical activity: ↑* |
| Celano et al., 201937 | Physical activity, medication adherence, diet (secondary) | Physical activity: MVPA and steps per day measured with Actigraph accelerometer, and self-reported MET minutes/week measured with International Physical Activity Questionnaire (IPAQ). Adherence to T2D medications: percent-based self-report measure. Diet: dietary items from the 11-item Summary of Diabetes Self-Care Activities. |
Physical activity: MVPA --; self-report ↑* Medication adherence: ↑ Diet: ↑* |
| DuBois et al., 201642 | Physical activity, diet (secondary) | Single items from the Summary of Diabetes Self-Care Activities (SDSCA) to assess diet and physical activity. | Physical activity: ↑* Diet: ↑ |
| Hoeppner et al., 201943 | Smoking cessation (secondary) | Self-report of smoking abstinence. 2 weeks post-quit, abstinence self-reports were biochemically verified with saliva cotinine. | Smoking cessation: ↑ |
| Millstein et al., 202041 | Physical activity, diet (secondary) | Physical activity: MVPA and steps per day measured with Actigraph accelerometer, and self-reported MET minutes/week measured with IPAQ. Diet: Behavioral Risk Factor Surveillance System Fruit and Vegetable Module to measure fruit and vegetable intake and fat intake measured with The National Cancer Institute's Percentage Energy from Fat Screener. |
Physical activity: MVPA ↑; steps; self-report ↑*
Diet: fruit/vegetable consumption ↑; energy from fat -- |
| O'Brien et al., 202046 | Physical activity (not defined) | Patient-Centered Assessment and Counselling for Exercise Plus Nutrition (PACE+ Physical Activity Measure)- 2-item screening tool used for adolescents in primary care that asks how many days of, (a) the past week and (b) a typical week, participants are active for at least 30 minutes; items are averaged together. | Physical activity: ↑* |
= improvement with at least a medium effect size (for studies with a comparator refers to intervention compared to control; for single-arm studies refers to pre-post change).
= Statistical significance (p<0.05). -- = no effect
Medication adherence was measured in eight studies. For the purposes of this review, we chose to include one study that measured blood glucose monitoring frequency within the medication section, as this is a key health behavior for type 1 diabetes management that informs medication use.48 Several validated self-report measures were used for medication adherence including the Morisky Adherence Scale,24,50 and the Self-Report Medication Adherence scale.35,39 Some studies used unvalidated self-report questions,31,37,45 and two used objective measures of adherence (e.g., electronic pill monitors, blood glucose monitor readings).32,48
While measurement of diet was conducted via self-report for all studies, there was wide variety in the aspects of diet measured and in the types of questions asked. Diet aspect depended on the study population; for example, in studies of patients with heart failure, the Scored Sodium Questionnaire was used to measure this clinically relevant aspect of diet.35,39 In studies of patients with diabetes, two used the dietary items from the Summary of Diabetes Self-Care Activities measure,37,42,51 and the third used questions on healthy eating from their clinic intake form which were not described in detail.25 The other two studies that measured diet were in populations without a specific chronic disease but with or at risk for obesity.34,41 These both used the Centers for Disease Control’s Behavioral Risk Factor Surveillance System fruit and vegetable module to assess fruit and vegetable consumption. Millstein and colleagues also assessed fat intake with the National Cancer Institute’s percentage energy from fat screener.52
Finally, of the three studies that assessed cigarette smoking, one used a single-item question about cigarette use as part of the broader Health Behavior Questionnaire.47 The other studies assessed smoking abstinence via self-report and confirmed reports of abstinence biochemically with saliva cotinine or by alveolar carbon monoxide.43,44
Intervention effects
Overall changes.
Effects of the interventions on health behavior outcomes were mixed (see Table 3 for details). Of the 13 studies powered to detect significant effects, six found a statistically significant improvement in at least one health behavior. Considering effect sizes across all studies, 19 found at least one health behavior improvement of medium or large effect size.
Physical activity studies.
Of the 20 studies examining physical activity as an outcome, 10 were powered to detect significant effects compared to a control condition.25-30,33,34 Of those, five found a significant improvement in physical activity with the intervention compared to the control.25,26,28,29,33 Three of the significant studies had health behavior components in both the intervention and control, while the other two only included positive psychological elements. Of the studies with non-significant effects, two had health behavior components in the intervention and control. Four other RCTs were underpowered to find significant effects compared to a control; of these, one, which included health behavior components in the intervention and control, found non-significant medium-to-large effect size effects of the intervention35 and the other three, two of which had health behavior components, found significant effects.36,38,47 The remaining six studies were single-arm pre-post studies. Of these, five found a statistically significant improvement in at least one measure of physical activity, although, notably, significant changes were only seen in self-reported physical activity.37,40-42,46 In the three single-arm studies that measured physical activity objectively, none found significant pre-post changes, with effect sizes ranging from small to large.37,39,41 All but one of the single-arm studies included health behavior components in the intervention.
Medication adherences studies.
Five of the eight studies that examined medication adherence were powered to detect significant effects.24,31,32,45,48 Of these, two found significant improvements in medication adherence in populations with hypertension and type 1 diabetes, although Jaser and colleagues saw improvements only in self-reported blood glucose monitoring frequency, not in objective monitor download data.32,48 One of the significant studies and one of the non-significant studies included a medication-focused health behavior component in the intervention and control. The nonsignificant studies included participants with hypertension and HIV. One pilot RCT that was underpowered to detect significant effects did find a medium effect-size improvement in self-reported medication adherence in the PPI compared to control, both of which included health behavior components, in adults with heart failure.35 Finally, there were two single-arm studies that measured pre-post change in medication adherence, both of which include health behavior intervention components. One found a significant improvement in patients with heart failure, and the other did not find improvements in a sample with type 2 diabetes.37,39
Diet studies.
Seven studies in total examined dietary change as an outcome. Two were well-powered RCTs which both included health behavior components in the intervention and control; of these, one found significant improvements in diet.25,34 The third RCT, which also included health behavior components, was underpowered to find significant results and did not find dietary changes.35 The other four studies were pilot studies examining pre-post changes in a very small sample (N ≤ 12). One of these studies, which included physical activity-focused content in the intervention and control, found a statistically significant improvement in dietary intake.37 The others, of which one included diet-focused content, one physical activity-focused, and one only positive psychological content, found nonsignificant medium effect-size improvements.39,41,42
Smoking studies.
Only three studies examined effects of positive psychology on smoking cessation. One fully powered study of an intervention that did not focus directly on smoking and measured smoking via a self-report risky behavior questionnaire and found no significant effects.47 The other two pilot studies measured smoking abstinence objectively and had interventions that included behavioral smoking cessation components. One of these found that 30% of participants demonstrated seven-day abstinence at the end of the study; this feasibility study did not include a control group for comparison.43 The other study found no significant effects of the intervention compared to a behavioral smoking cessation control, although when they analyzed the data using a more powerful longitudinal model they did find that participants in the positive psychology had a higher odds of abstinence compared to standard behavioral treatment.44
Risk of bias and study quality
We considered quality ratings of RCTs and single-arm studies separately, as two of the rating domains were not relevant to a single-arm design. Of the studies with comparators, three received a strong rating,25,30,36 eight received a moderate rating,24,29,31,33-35,38,48 and the rest were rated as weak.26-28,32,44,45,47 Lack of blinding (n = 10), risk of selection bias (n = 7), and uncontrolled confounders (n = 5) were the most common concerns that lowered ratings. Among single-arm studies, we did not penalize studies based on confounders and lack of blinding as they were not relevant to the study design. With this modified system, one received a strong rating46 and the rest received moderate ratings.37,39-43 Of the single-arm studies, selection bias (n = 5) was the most common concern leading to a moderate rating.
Discussion
This systematic review summarized the extant literature on PPIs targeting a health behavior (e.g., physical activity, diet, medication adherence, and/or smoking cessation). We found 27 eligible studies, with physical activity as the most frequently measured behavioral outcome. Effects of PPIs on a health behavior outcome have mostly been examined in adults, although several studies targeted young adults or adolescents. Most studies focused on a specific disease population, typically diabetes or heart disease, while others targeted broader samples.
PPIs are heterogeneous, including many techniques aimed at increasing a variety of positive psychological constructs including positive affect, optimism, or life purpose.11 Accordingly, PPI content, duration, and intensity varied considerably between studies. Commonalities across most interventions included providing participants with activities to complete on their own to increase these positive psychological constructs. Gratitude-based exercises were common, encouraging people to notice and appreciate positive things in their lives, as were exercises based on self-affirmation or personal strengths, where participants were instructed to identify the characteristics that make them successful. Most interventions were multifaceted, combining a PPI with other approaches, most commonly focused more directly on the health behaviors being targeted (e.g., goal-setting). There were no clear patterns in terms of intervention components and efficacy; those that directly targeted the health behavior in combination with a PPI did not have consistently different effects than those that used PPIs alone. As the controlled studies that included content related to the health behavior also had content relevant to the health behavior in the control condition, any effects seen were in theory caused by the inclusion of the PPI, rather than the behavioral elements exclusively. The interventions were largely feasible and well-accepted, based on low withdrawal rates and, when measured, high acceptability ratings. There is a rationale for tailoring interventions to the unique needs of different populations. However, too much heterogeneity makes it difficult to establish a strong evidence base for PPI components that consistently improve psychological and behavioral outcomes.
In terms of intervention efficacy on health behaviors, results were highly mixed across the behaviors measured. This is not surprising given the high variability in type and quality of outcome measurement, sample size, and intervention intensity and content. Of all health behaviors examined, physical activity was measured most frequently and showed the most promise in terms of statistically significant and/or large effect size improvements. Medication adherence was the second most commonly measured outcome with moderate validity in terms of measurement, but most studies did not find significant intervention effects. Measurement of diet was so variable across studies that results cannot be meaningfully summarized. PPIs for smoking cessation show promise based on the two studies that measured cigarette use comprehensively, but low power and lack of control for one study limit definitive conclusions.
This review highlights several important considerations for future research. First, accurate measurement of health behaviors is critical. While objective measurement was used in some studies (e.g., accelerometer, electronic pill bottles, biochemical verification of nicotine use), most relied on self-report which is typically less valid, and further, methods of self-report were highly variable, sometimes including unvalidated or single-item measures. In terms of intervention content, establishing the most effective PPI components – both in terms of positive psychology exercises utilized, and combinations of PPIs with other behavioral health intervention methods (e.g., goal-setting) – will be needed to build the evidence base necessary to support integration of PPIs into clinical care. Methodologies such as the multifactorial optimization strategy (MOST) can be applied to examine which PPI components are most efficacious and whether this is consistent across different populations and outcomes.53 While some studies delivered the intervention in-person, most were able to use remote methods feasibly, which may make such interventions more broadly applicable and more widely scalable. Most remote PPIs were delivered by phone. Future research should explore whether other remote delivery methods that take advantage of recent technological advancements (e.g., videoconference, mobile apps, text messaging) are similarly or more feasible and effective.
Strengths of this review include a comprehensive examination of the existing literature across multiple populations and health behavior outcomes, use of PRISMA guidelines, prospective trial registration, and use of multiple reviewers to select articles and extract data. Limitations include lack of meta-analysis to quantitatively summarize findings due to the wide variety in outcome measurement, and risk of omitted studies due to the wide variety of naming and describing PPIs in the literature. The studies included in this review commonly had limitations such as oversampling of non-Hispanic white participants which limits generalizability of findings, and pilot study designs that lacked power to consistently detect significant effects.
In sum, PPIs are being used to target multiple health behaviors in a variety of medical and healthy populations. As they relate to health behavior outcomes, PPIs appear to hold some promise, although the literature remains mixed and of intermittent quality, with many studies at early pilot and feasibility stages of development. Due to the heterogeneity of the types of PPIs studied and the populations in whom they have been examined, there is not yet a clear consensus on whether and for whom PPIs are effective in terms of changing health behaviors. This is in line with several analyses that have suggested demographics do not predict outcome during a PPI.54,55 While more high-quality research is needed to determine the optimal intervention content, dosage, and delivery method to affect sustainable health behavior change, PPIs remain a viable option that is typically well-received for promoting health behavior change.
Funding:
This work was supported by the National Institutes of Health [grant numbers K23HL148017 (PI: Feig), K23HL135277 (PI: Millstein), K08CA251653 (PI: Amonoo), R21NR018738 (PI: Huffman), and R01HL155301 (PI: Celano)].
Abbreviations
- PPI
positive psychology intervention
- RCT
randomized controlled trial
- HB
health behavior
Footnotes
Conflict of interest statement: The authors declare no conflicts of interest.
References
- 1.Du Y, Liu B, Sun Y, Snetselaar LG, Wallace RB, & Bao W (2019). Trends in Adherence to the Physical Activity Guidelines for Americans for Aerobic Activity and Time Spent on Sedentary Behavior Among US Adults, 2007 to 2016. JAMA Network Open, 2(7), e197597–e197597. 10.1001/JAMANETWORKOPEN.2019.7597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hiza HAB, Casavale KO, Guenther PM, & Davis CA (2013). Diet Quality of Americans Differs by Age, Sex, Race/Ethnicity, Income, and Education Level. Journal of the Academy of Nutrition and Dietetics, 113(2), 297–306. 10.1016/J.JAND.2012.08.011 [DOI] [PubMed] [Google Scholar]
- 3.Youn B, Shireman TI, Lee Y, Galárraga O, & Wilson IB (2019). Trends in medication adherence in HIV patients in the US, 2001 to 2012: an observational cohort study. Journal of the International AIDS Society, 22(8), e25382. 10.1002/JIA2.25382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uchmanowicz B, Jankowska EA, Uchmanowicz I, & Morisky DE (2019). Self-Reported Medication Adherence Measured With Morisky Medication Adherence Scales and Its Determinants in Hypertensive Patients Aged ≥60 Years: A Systematic Review and Meta-Analysis. Frontiers in Pharmacology, 0, 168. 10.3389/FPHAR.2019.00168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kontis V, Cobb LK, Mathers CD, Frieden TR, Ezzati M, & Danaei G (2019). Three Public Health Interventions Could Save 94 Million Lives in 25 Years. Circulation, 140(9), 715–725. 10.1161/CIRCULATIONAHA.118.038160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Cappellen P, Rice EL, Catalino LI, & Fredrickson BL (2018). Positive affective processes underlie positive health behaviour change. Psychology & Health, 33(1), 77–97. 10.1080/08870446.2017.1320798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boehm JK, & Kubzansky LD (2012). The heart’s content: The association between positive psychological well-being and cardiovascular health. Psychological Bulletin, 138(4), 655–691. 10.1037/a0027448 [DOI] [PubMed] [Google Scholar]
- 8.Kim ES, Kubzansky LD, Soo J, & Boehm JK (2017). Maintaining healthy behavior: A prospective study of psychological well-being and physical activity. Annals of Behavioral Medicine, 51(3), 337–347. 10.1007/s12160-016-9856-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huffman JC, Beale EE, Celano CM, Beach SR, Belcher AM, Moore SV, Suarez L, Motiwala SR, Gandhi PU, Gaggin HK, & Januzzi JL (2016). Effects of optimism and gratitude on physical activity, biomarkers, and readmissions after an acute coronary syndrome: The Gratitude Research in Acute Coronary Events study. Circulation: Cardiovascular Quality and Outcomes, 9(1), 55–63. 10.1161/CIRCOUTCOMES.115.002184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seligman MEPP, Steen TA, Park N, & Peterson C (2005). Positive psychology progress: Empirical validation of interventions. The American Psychologist, 60(5), 410–421. 10.1037/0003-066X.60.5.410 [DOI] [PubMed] [Google Scholar]
- 11.Sin NL, & Lyubomirsky S (2009). Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. Journal of Clinical Psychology, 65(5), 467–487. 10.1002/jclp.20593 [DOI] [PubMed] [Google Scholar]
- 12.Chakhssi F, Kraiss JT, Sommers-Spijkerman M, & Bohlmeijer ET (2018). The effect of positive psychology interventions on well-being and distress in clinical samples with psychiatric or somatic disorders: a systematic review and meta-analysis. BMC Psychiatry, 18(1), 211. 10.1186/s12888-018-1739-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kubzansky LD, Huffman JC, Boehm JK, Hernandez R, Kim ES, Koga HK, Feig EH, Lloyd-Jones DM, Seligman MEP, & Labarthe DR (2018). Positive Psychological Well-Being and Cardiovascular Disease: JACC Health Promotion Series. Journal of the American College of Cardiology, 72(12), 1382–1396. 10.1016/j.jacc.2018.10.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carr A, Cullen K, Keeney C, Canning C, Mooney O, Chinseallaigh E, & O’Dowd A (2021). Effectiveness of positive psychology interventions: a systematic review and meta-analysis. The Journal of Positive Psychology, 16(6), 749–769. 10.1080/17439760.2020.1818807 [DOI] [Google Scholar]
- 15.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, & PRISMA-P Group. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4, 1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schueller SM, Kashdan TB, & Parks AC (2014). Synthesizing positive psychological interventions: Suggestions for conducting and interpreting meta-analyses. International Journal of Wellbeing, 4(1), 91–98. 10.5502/ijw.v4i1.5 [DOI] [Google Scholar]
- 17.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, … Rosamond WD (2010). Defining and Setting National Goals for Cardiovascular Health Promotion and Disease Reduction. Circulation, 121(4), 586–613. 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 18.Boehm JK, Chen Y, Koga H, Mathur MB, Vie LL, & Kubzansky LD (2018). Is Optimism Associated With Healthier Cardiovascular-Related Behavior? Circulation Research, 122(8), 1119–1134. 10.1161/CIRCRESAHA.117.310828 [DOI] [PubMed] [Google Scholar]
- 19.Jackson N, Waters E, & Guidelines for Systematic Reviews in Health Promotion and Public Health Taskforce. (2005). Criteria for the systematic review of health promotion and public health interventions. Health Promotion International, 20(4), 367–374. 10.1093/heapro/dai022 [DOI] [PubMed] [Google Scholar]
- 20.Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, & Cummings GG (2012). Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. Journal of Evaluation in Clinical Practice, 18(1), 12–18. 10.1111/j.1365-2753.2010.01516.x [DOI] [PubMed] [Google Scholar]
- 21.Milbury K, Engle R, Liao ZX, Tsao AS, Owens A, Bruera E, & Cohen L (2017). Couple-based mind-body intervention for patients with metastatic lung cancer and their spouses. Journal of Clinical Oncology, 35(31_suppl), 179–179. 10.1200/JCO.2017.35.31_suppl.179 [DOI] [Google Scholar]
- 22.Southwell S, & Gould E (2017). A randomised wait list-controlled pre–post–follow-up trial of a gratitude diary with a distressed sample. The Journal of Positive Psychology, 12(6), 579–593. 10.1080/17439760.2016.1221127 [DOI] [Google Scholar]
- 23.Kolle E, Solberg RB, Säfvenbom R, Dyrstad SM, Berntsen S, Resaland GK, Ekelund U, Anderssen SA, Steene-Johannessen J, & Grydeland M (2020). The effect of a school-based intervention on physical activity, cardiorespiratory fitness and muscle strength: the School in Motion cluster randomized trial. International Journal of Behavioral Nutrition and Physical Activity, 17(1), 1–14. 10.1186/S12966-020-01060-0/TABLES/6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boutin-Foster C, Offidani E, Kanna B, Ogedegbe G, Ravenell J, Scott E, Rodriguez A, Ramos R, Michelen W, Gerber LM, & Charlson M (2016). Results from the trial using motivational interviewing, positive affect, and self-affirmation in African Americans with hypertension (TRIUM PH). Ethnicity and Disease, 26(1), 51–60. 10.18865/ed.26.1.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bradshaw BG, Richardson GE, Kumpfer K, Carlson J, Stanchfield J, Overall J, Brooks AM, & Kulkarni K (2007). Determining the efficacy of a resiliency training approach in adults with type 2 diabetes. Diabetes Educator, 33(4), 650–659. 10.1177/0145721707303809 [DOI] [PubMed] [Google Scholar]
- 26.Emmons RA, & McCullough ME (2003). Counting blessings versus burdens: An experimental investigation of gratitude and subjective well-being in daily life. Journal of Personality & Social Psychology, 84(2), 377–389. 10.1037//0022-3514.84.2.377 [DOI] [PubMed] [Google Scholar]
- 27.Joutsenniemi K, Kaattari C, Härkänen T, Pankakoski M, Langinvainio H, Lönnqvist J, Mattila AS, & Mustonen P (2014). E-mail-based exercises in happiness, physical activity and readings: A randomized trial on 3274 finns. African Journal of Psychiatry (South Africa), 17(5). 10.4172/Psychiatry.1000140 [DOI] [Google Scholar]
- 28.Kersten M, Cox CR, & van Enkevort EA (2016). An exercise in nostalgia: Nostalgia promotes health optimism and physical activity. Psychology and Health, 31(10), 1166–1181. 10.1080/08870446.2016.1185524 [DOI] [PubMed] [Google Scholar]
- 29.Lee TSH, Hung CC, Lin CK, & Chiang HH (2019). Controlled randomized trial of walking exercise with positive education on cardiovascular fitness and happiness in retired older adults. Geriatrics and Gerontology International, 19(9), 879–884. 10.1111/ggi.13733 [DOI] [PubMed] [Google Scholar]
- 30.Mancuso CA, Choi TN, Westermann H, Wenderoth S, Hollenberg JP, Wells MT, Isen AM, Jobe JB, Allegrante JP, & Charlson ME (2012). Increasing physical activity in patients with asthma through positive affect and self-affirmation: A randomized trial. Archives of Internal Medicine, 172(4), 337–343. 10.1001/archinternmed.2011.1316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moskowitz JT, Carrico AW, Duncan LG, Cohn MA, Cheung EO, Batchelder A, Martinez L, Segawa E, Acree M, & Folkman S (2017). Randomized controlled trial of a positive affect intervention for people newly diagnosed with HIV. Journal of Consulting and Clinical Psychology, 85(5), 409–423. 10.1037/ccp0000188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ogedegbe GO, Boutin-Foster C, Wells MT, Allegrante JP, Isen AM, Jobe JB, & Charlson ME (2012). A randomized controlled trial of positive-affect intervention and medication adherence in hypertensive African Americans. Archives of Internal Medicine, 172(4), 322–326. 10.1001/archinternmed.2011.1307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peterson JC, Charlson ME, Hoffman Z, Wells MT, Wong SC, Hollenberg JP, Jobe JB, Boschert KA, Isen AM, & Allegrante JP (2012). A randomized controlled trial of positive-affect induction to promote physical activity after percutaneous coronary intervention. Archives of Internal Medicine, 172(4), 329–336. 10.1001/archinternmed.2011.1311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Phillips EG, Wells MT, Winston G, Ramos R, Devine CM, Wethington E, Peterson JC, Wansink B, & Charlson M (2017). Innovative approaches to weight loss in a high-risk population: The small changes and lasting effects (SCALE) trial. Obesity, 25(5), 833–841. 10.1002/oby.21780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Celano CM, Freedman ME, Harnedy LE, Park ER, Januzzi JL, Healy BC, & Huffman JC (2020). Feasibility and preliminary efficacy of a positive psychology-based intervention to promote health behaviors in heart failure: The REACH for Health study. Journal of Psychosomatic Research, 139, 110285. 10.1016/J.JPSYCHORES.2020.110285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Huffman JC, Golden J, Massey CN, Feig EH, Chung WJ, Millstein RA, Brown L, Gianangelo T, Healy BC, Wexler DJ, Park ER, & Celano CM (2020). A Positive Psychology-Motivational Interviewing Intervention to Promote Positive Affect and Physical Activity in Type 2 Diabetes: The BEHOLD-8 Controlled Clinical Trial. Psychosomatic Medicine, 82(7), 641–649. 10.1097/PSY.0000000000000840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Celano CM, Gianangelo TA, Millstein RA, Chung W-J, Wexler DJ, Park ER, & Huffman JC (2019). A positive psychology–motivational interviewing intervention for patients with type 2 diabetes: Proof-of-concept trial. The International Journal of Psychiatry in Medicine, 54(2), 97–114. 10.1177/0091217418791448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huffman JC, Feig EH, Millstein RA, Freedman M, Healy BC, Chung WJ, Amonoo HL, Malloy L, Slawsby E, Januzzi JL, & Celano CM (2019). Usefulness of a positive psychology-motivational interviewing intervention to promote positive affect and physical activity after an acute coronary syndrome. American Journal of Cardiology, 123(12), 1906–1914. 10.1016/j.amjcard.2019.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Celano CM, Freedman ME, Beale EE, Gomez-Bernal F, & Huffman JC (2018). A positive psychology intervention to promote health behaviors in heart failure: A proof-of-concept trial: The REACH for Health study. Journal of Nervous and Mental Disorders, 206(10), 800–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Celano CM, Albanese AM, Millstein RA, Mastromauro CA, Chung W-J, Campbell KA, Legler SR, Park ER, Healy BC, Collins LM, Januzzi JL, & Huffman JC (2018). Optimizing a positive psychology intervention to promote health behaviors following an acute coronary syndrome: The Positive Emotions after Acute Coronary Events-III (PEACE-III) randomized factorial trial. Psychosomatic Medicine, 80(6), 526–534. 10.1097/PSY.0000000000000584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Millstein RA, Thorndike AN, Kim S, Park ER, & Huffman JC (2020). A community-based positive psychology group intervention to promote physical activity among people with metabolic syndrome: Proof of concept results to inform a pilot randomized controlled trial protocol. Contemporary Clinical Trials Communications, 19. 10.1016/j.conctc.2020.100626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dubois CM, Millstein RA, Celano CM, Wexler DJ, & Huffman JC (2016). Feasibility and acceptability of a positive psychological intervention for patients with type 2 diabetes. Primary Care Companion to the Journal of Clinical Psychiatry, 18(3). 10.4088/PCC.15m01902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hoeppner BB, Hoeppner SS, Carlon HA, Perez GK, Helmuth E, Kahler CW, & Kelly JF (2019). Leveraging positive psychology to support smoking cessation in nondaily smokers using a smartphone app: Feasibility and acceptability study. JMIR MHealth and UHealth, 7(7). 10.2196/13436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kahler CW, Spillane NS, Day AM, Cioe PA, Parks A, Leventhal AM, & Brown RA (2015). Positive Psychotherapy for Smoking Cessation: A Pilot Randomized Controlled Trial. Nicotine and Tobacco Research, 17(11), 1385–1392. 10.1093/ntr/ntv011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mann T (2001). Effects of future writing and optimism on health behaviors in HIV-infected women. Annals of Behavioral Medicine, 23(1), 26–33. 10.1207/S15324796ABM2301_5 [DOI] [PubMed] [Google Scholar]
- 46.O’Brien N, Lawlor M, Chambers F, & O’brien W (2020). State of mind ireland-higher education: A mixed-methods longitudinal evaluation of a positive mental health intervention. International Journal of Environmental Research and Public Health, 17(15), 1–23. 10.3390/ijerph17155530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chandler GE, Roberts SJ, & Chiodo L (2015). Resilience Intervention for Young Adults With Adverse Childhood Experiences. Journal of the American Psychiatric Nurses Association, 21(6), 406–416. 10.1177/1078390315620609 [DOI] [PubMed] [Google Scholar]
- 48.Jaser SS, Patel N, Rothman RL, Choi L, & Whittemore R (2014). Check it!: A randomized pilot of a positive psychology intervention to improve adherence in adolescents with type 1 diabetes. The Diabetes Educator, 40(5), 659–667. 10.1177/0145721714535990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Paffenbarger RS, Blair SN, Lee IM, & Hyde RT (1993). Measurement of physical activity to assess health effects in free-living populations. Medicine and Science in Sports and Exercise, 25(1), 60–70. 10.1249/00005768-199301000-00010 [DOI] [PubMed] [Google Scholar]
- 50.Morisky DE, Green LW, & Levine DM (1986). Concurrent and predictive validity of a self-reported measure of medication adherence. Medical Care, 24(1), 67–74. 10.1097/00005650-198601000-00007 [DOI] [PubMed] [Google Scholar]
- 51.Toobert DJ, Hampson SE, & Glasgow RE (2000). The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care, 23(7), 943–950. 10.2337/diacare.23.7.943 [DOI] [PubMed] [Google Scholar]
- 52.Thompson FE, Midthune D, Subar AF, Kipnis V, Kahle LL, & Schatzkin A (2007). Development and Evaluation of a Short Instrument to Estimate Usual Dietary Intake of Percentage Energy from Fat. Journal of the American Dietetic Association, 107(5), 760–767. 10.1016/j.jada.2007.02.006 [DOI] [PubMed] [Google Scholar]
- 53.Collins LM, Murphy SA, & Strecher V (2007). The Multiphase Optimization Strategy (MOST) and the Sequential Multiple Assignment Randomized Trial (SMART). American Journal of Preventive Medicine, 32(5), S112–S118. 10.1016/j.amepre.2007.01.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Campbell KA, Healy BC, Celano CM, Albanese A, Millstein RA, & Huffman JC (2018). Predictors of completion of a psychological-behavioral intervention in acute coronary syndrome patients. Journal of Psychosomatic Research, 112, 9–12. 10.1016/j.jpsychores.2018.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Feig E, Healy B, Celano C, Nikrahan G, Miskowitz J, & Huffman J (2019). Positive psychology interventions in patients with medical illness: What predicts improvement in psychological state? International Journal of Wellbeing, In press. [Google Scholar]