Abstract
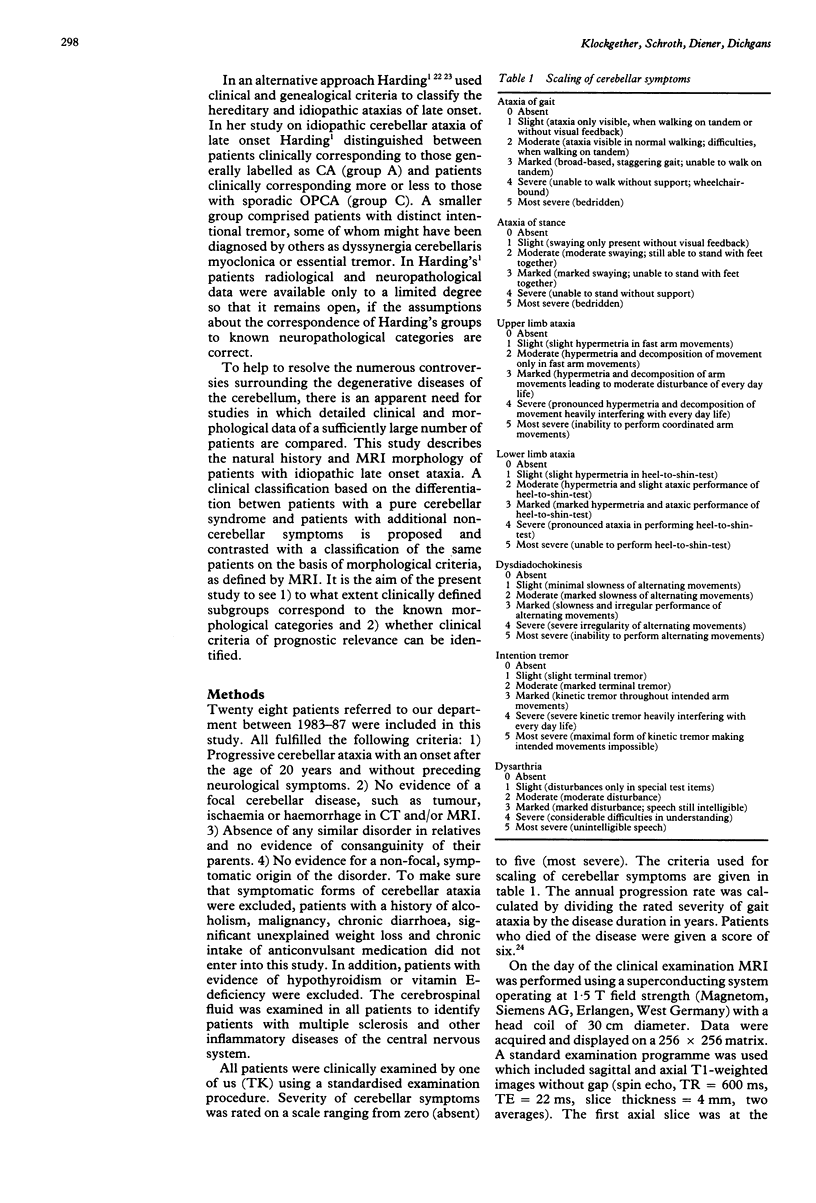
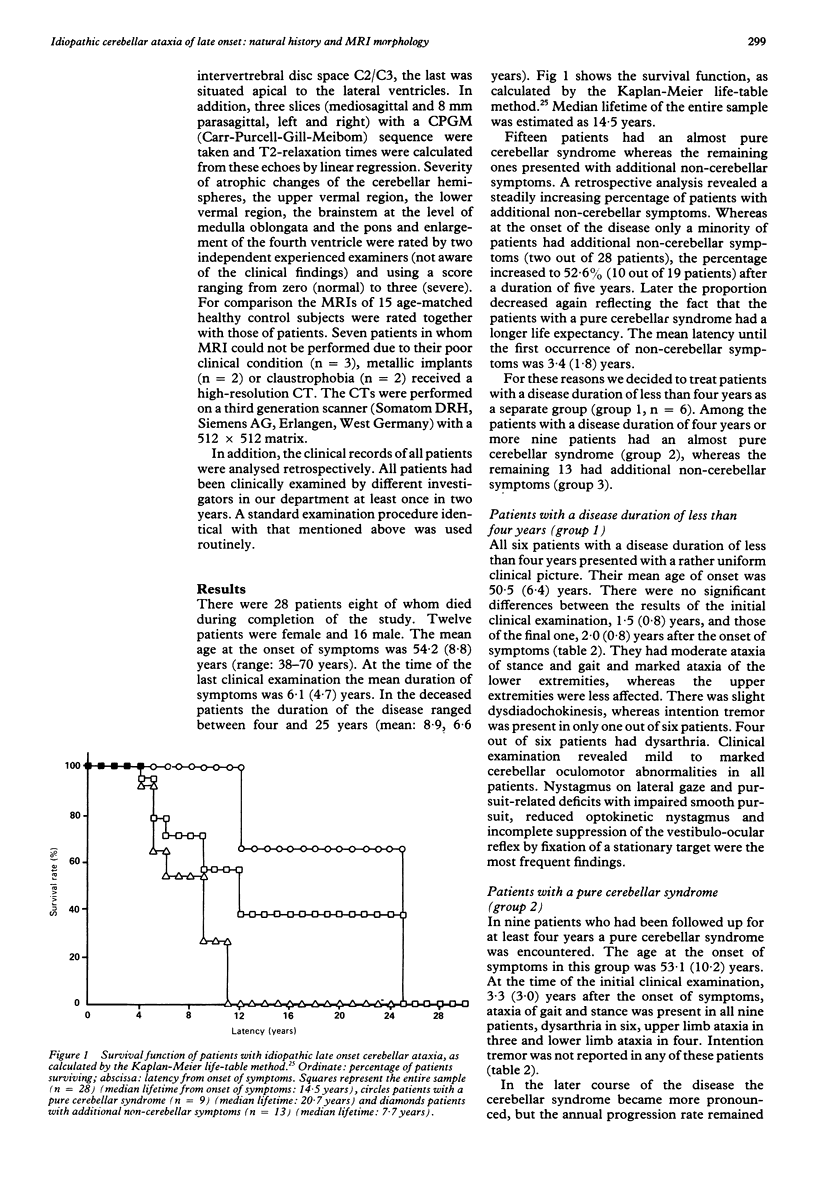
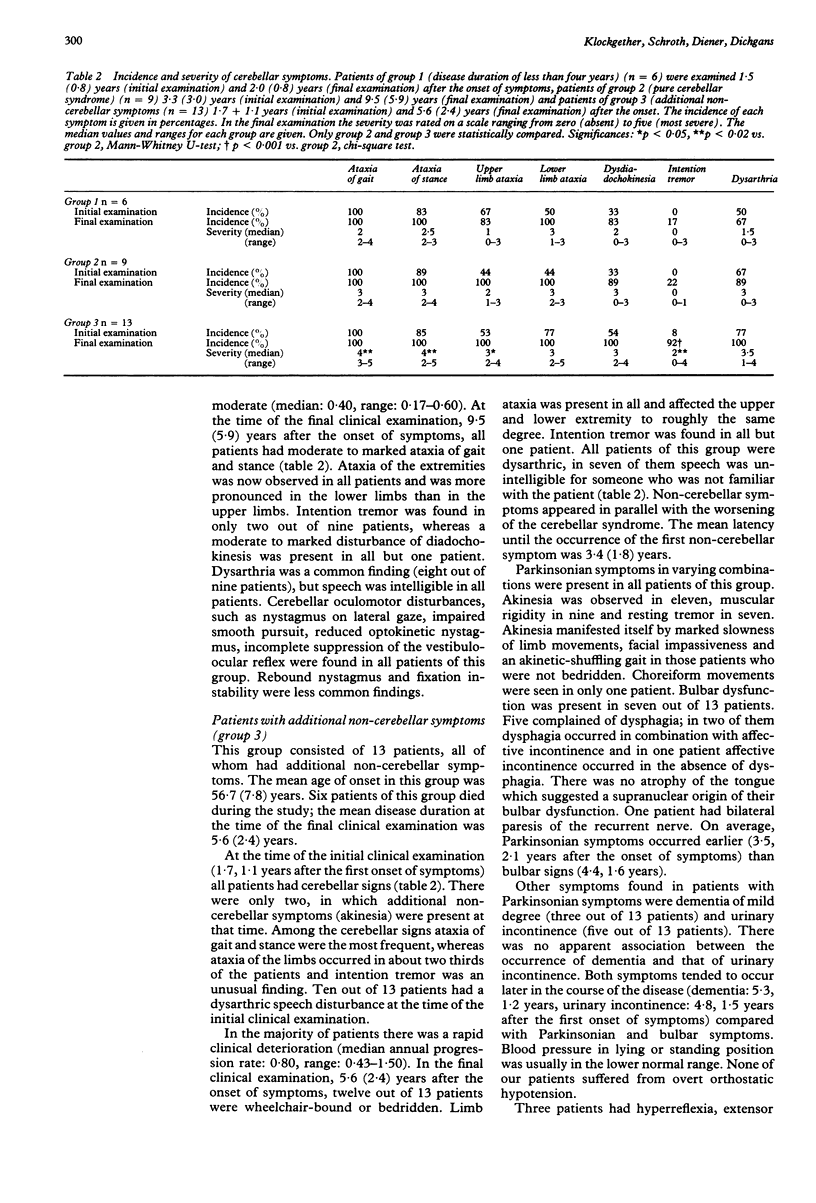
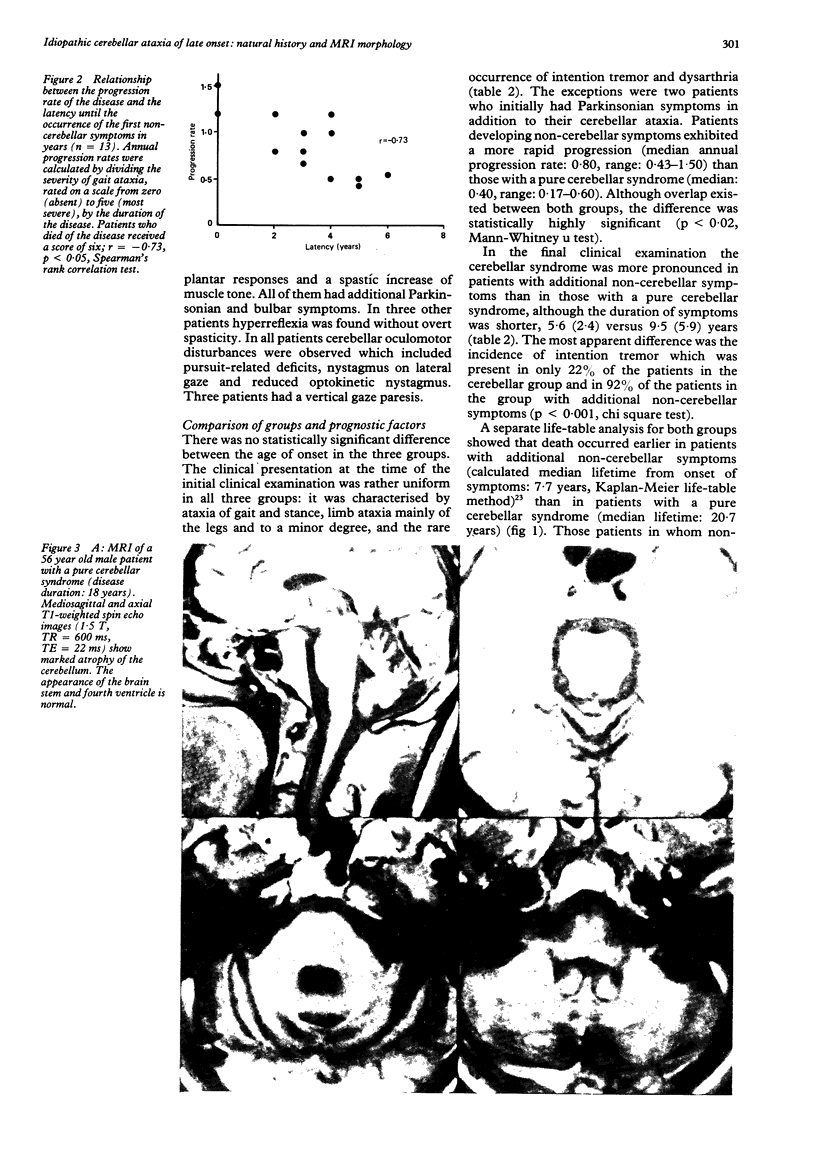
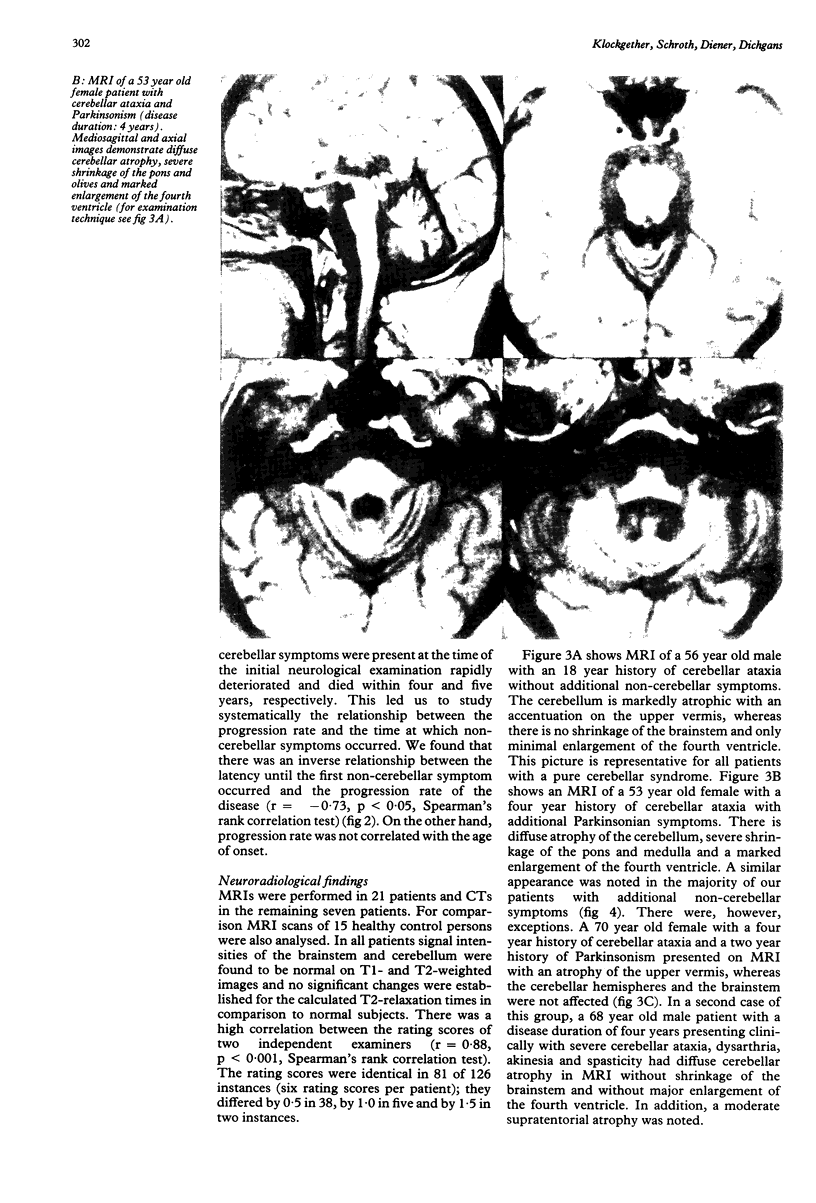
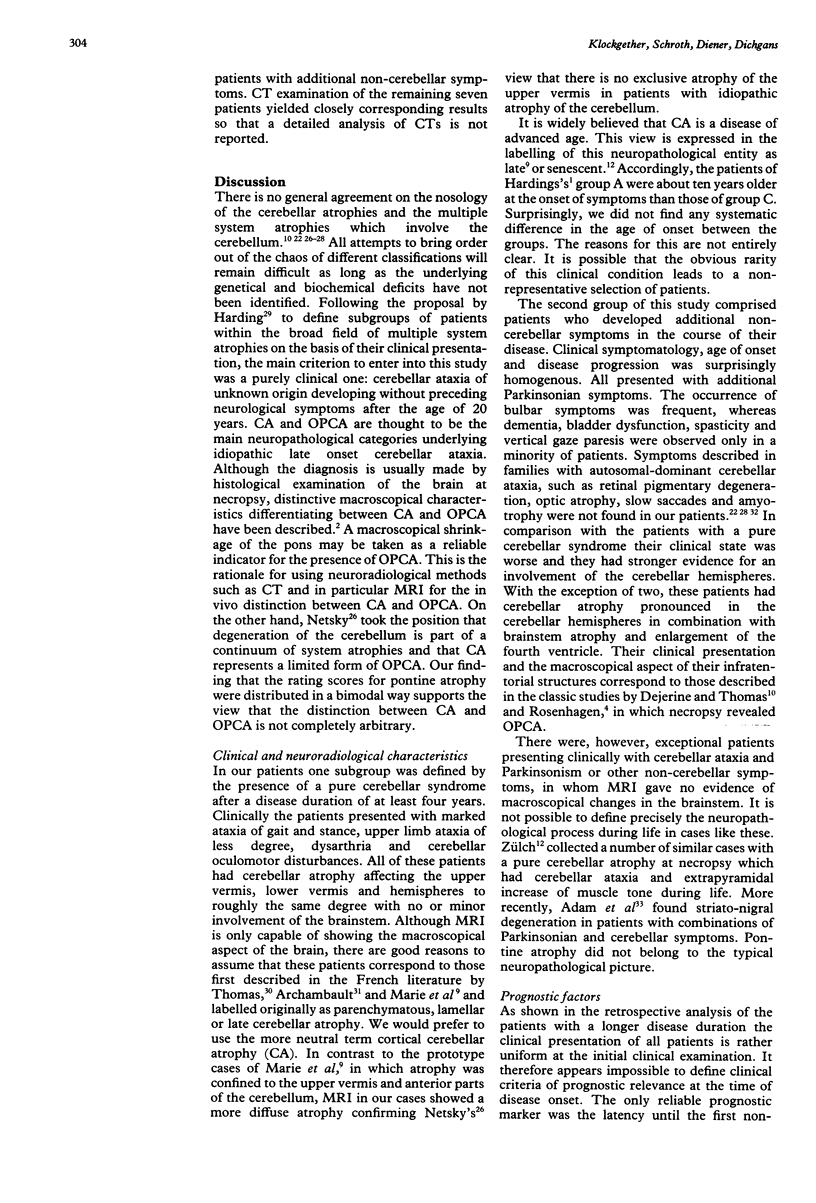
Twenty eight patients with the clinical diagnosis of idiopathic late onset cerebellar ataxia were examined clinically and by magnetic resonance imaging (MRI) or computed tomography (CT). In addition, the clinical records of all patients were analysed retrospectively. On the basis of their clinical presentation they were subdivided into patients with a pure cerebellar syndrome (n = 9) and patients with a cerebellar syndrome and additional non-cerebellar symptoms (n = 13). No attempts were made to classify patients with a disease duration of less than four years (n = 6) because the retrospective analysis showed that the disease started almost invariably with a pure cerebellar syndrome and additional symptoms came later. Patients with a lasting pure cerebellar syndrome had a significantly better prognosis than patients with additional non-cerebellar involvement (annual progression rate rate: 0.40 versus 0.80). Calculated median lifetime from onset of symptoms was 20.7 years in patients with a pure cerebellar syndrome and 7.7 years in patients with additional non-cerebellar symptoms. Among the latter, disease progression was faster the earlier non-cerebellar symptoms occurred. All of them presented with Parkinsonian symptoms, whereas bulbar symptoms, vertical gaze paresis, pyramidal deficits, dementia and urinary incontinence were encountered less frequently. MRI or CT showed cerebellar atrophy without apparent involvement of brainstem structures in all patients with a pure cerebellar syndrome suggesting the diagnosis of cerebellar cortical atrophy (CA). The majority of the patients with additional non-cerebellar symptoms had evidence of an atrophy of the cerebellum and the brainstem suggesting the presence of olivo-ponto-cerebellar atrophy (OPCA). In two of them, however, MRI morphology was not compatible with the diagnosis of OPCA.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Allen J. H., Martin J. T., McLain L. W. Computed tomography in cerebellar atrophic processes. Radiology. 1979 Feb;130(2):379–382. doi: 10.1148/130.2.379. [DOI] [PubMed] [Google Scholar]
- Berciano J. Olivopontocerebellar atrophy. A review of 117 cases. J Neurol Sci. 1982 Feb;53(2):253–272. doi: 10.1016/0022-510x(82)90011-9. [DOI] [PubMed] [Google Scholar]
- CARTER H. R., SUKAVAJANA C. Familial cerebello-olivary degeneration with late development of rigidity and dementia. Neurology. 1956 Dec;6(12):876–884. doi: 10.1212/wnl.6.12.876. [DOI] [PubMed] [Google Scholar]
- Coutinho P., Andrade C. Autosomal dominant system degeneration in Portuguese families of the Azores Islands. A new genetic disorder involving cerebellar, pyramidal, extrapyramidal and spinal cord motor functions. Neurology. 1978 Jul;28(7):703–709. doi: 10.1212/wnl.28.7.703. [DOI] [PubMed] [Google Scholar]
- Currier R. D., Jackson J. F., Meydrech E. F. Progression rate and age at onset are related in autosomal dominant neurologic diseases. Neurology. 1982 Aug;32(8):907–909. doi: 10.1212/wnl.32.8.907. [DOI] [PubMed] [Google Scholar]
- García de la Rocha M. L., Moreno Martínez J. M., Garrido Carrión A., Fernández P. M., Martín Araguz A. Present criteria for the diagnosis of in vivo of olivopontocerebellar atrophy. Acta Neurol Scand. 1988 Mar;77(3):234–238. doi: 10.1111/j.1600-0404.1988.tb05901.x. [DOI] [PubMed] [Google Scholar]
- Gilroy J., Lynn G. E. Computerized tomography and auditory-evoked potentials. Use in the diagnosis of olivopontocerebellar degeneration. Arch Neurol. 1978 Mar;35(3):143–147. doi: 10.1001/archneur.1978.00500270025006. [DOI] [PubMed] [Google Scholar]
- Harding A. E. "Idiopathic" late onset cerebellar ataxia. A clinical and genetic study of 36 cases. J Neurol Sci. 1981 Aug;51(2):259–271. doi: 10.1016/0022-510x(81)90104-0. [DOI] [PubMed] [Google Scholar]
- Harding A. E. The clinical features and classification of the late onset autosomal dominant cerebellar ataxias. A study of 11 families, including descendants of the 'the Drew family of Walworth'. Brain. 1982 Mar;105(Pt 1):1–28. doi: 10.1093/brain/105.1.1. [DOI] [PubMed] [Google Scholar]
- Huang Y. P., Plaitakis A. Morphological changes of olivopontocerebellar atrophy in computed tomography and comments on its pathogenesis. Adv Neurol. 1984;41:39–85. [PubMed] [Google Scholar]
- Jellinger K., Tarnowska-Dziduszko E. Die ZNS-Veränderungen bei den olivo-ponto-cerebellaren Atrophien. Z Neurol. 1971;199(3):192–214. [PubMed] [Google Scholar]
- Koller W. C., Glatt S. L., Perlik S., Huckman M. S., Fox J. H. Cerebellar atrophy demonstrated by computed tomography. Neurology. 1981 Apr;31(4):405–412. doi: 10.1212/wnl.31.4.405. [DOI] [PubMed] [Google Scholar]
- Nabatame H., Fukuyama H., Akiguchi I., Kameyama M., Nishimura K., Nakano Y. Spinocerebellar degeneration: qualitative and quantitative MR analysis of atrophy. J Comput Assist Tomogr. 1988 Mar-Apr;12(2):298–303. [PubMed] [Google Scholar]
- Puska P., Iacono J. M., Nissinen A., Korhonen H. J., Vartianinen E., Pietinen P., Dougherty R., Leino U., Mutanen M., Moisio S. Controlled, randomised trial of the effect of dietary fat on blood pressure. Lancet. 1983 Jan 1;1(8314-5):1–5. doi: 10.1016/s0140-6736(83)91556-8. [DOI] [PubMed] [Google Scholar]