Abstract
Nurses, as the largest forces in the health system, are always challenged with various work responsibilities such as long working hours, lack of manpower and death of patients. This study aimed at providing a model of the relationship between workload and physical and mental health, sleep disorders, and individual and family problems by the mediation role of job stress. The present study is a cross-sectional study that was conducted on 300 nurses in a specialty and sub-specialty hospital in Tehran. For this reason, various questionnaires including demographic, survey of shift workers (SOS) and job stress questionnaires were used to collect the desired data. The proposed model was presented using structural equation modeling method based on Smart-PLS and SPSS-20 software. The results show that workload has an effect on job stress (β=0.747), mental health (β=-0.291), Physical health (β=-0.253), sleep quality (β=-0.234) and personal and family problems (β=-0.206). Also the results of this study show that job stress has an effect on mental health (β=-0.295), Physical health (β=-0.349), sleep quality (β=-0.295) and Personal and family problems (β=-0.441). In conclusion, results showed that the data fitted well with the model and that workload is associated with physical and mental problems, sleep disorders and individual and family problems both directly and indirectly through job stress mediation.
Key Words: Shift work, workload, job stress, shift disorders
Ethical Publication Statement
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Providing 24-h services is an inevitable part of thehealth care system which has led to the introduction of the shift work phenomenon.1 Shift work is a continuous or non-continuous rotational pattern during the day or week and refers to anything that is done outside the time period of 7 am to 6 pm.2 In developed countries, about 20% of the workforce works in shifts, and one third of the workforce work night shifts.3 Shift work is one of the most important challenges of the health system, and nurses as the main force of this system face many complications caused by work shifts.4,5
Long and non-standard working hours, lack of manpower and work shifts caused increased work accidents and human errors, anxiety, sleep disorders, increased smoking, decreased immune function, digestive problems, cardiovascular disease, and musculoskeletal complications.6-8 The workload of a nurse is defined based on the number of patients, workplace situation and facilities, and their performance in providing services,9,10 which includes the qualitative and quantitative workload. The quantitative workload refers to a condition in which individuals are required to perform more tasks that are higher than their capacity.11 A sharp increase in workload can results in several physical and mental consequences for nurses.12 Job stress is considered as one of the most important consequences of long working hours and work over-load in nurses.13 It is defined as an unfavorable mental state in response to workplace pressure.14 According to the National Institute for Occupational Safety & Health (NIOSH) definition, when there is no harmony between job needs and abilities, capabilities and desires, a person experiences job stress.15 Therefore, job stress is associated with the imbalance between a person's capacity and the job tasks.16,17
Researches have shown that workload, as one of the most important causes of job stress, endangers the physical and mental health of nurses.12,18 In this regard, in Shaw et al. study,11 it was found that the qualitative workload could increase stress, anxiety, and depression, however, this association was not significant. Angermeyer et al. reported that nurses are always in the process of stress and psychological damage due to the workload and shift work.19 Numerous stressors can lead to job stress for nurses, such as work over-load, lack of manpower, low freedom of action, patient death, sleep disturbance, long working hours and suffering of patients, physical injuries such as cardiovascular, gastrointestinal and musculoskeletal disorders and individual and family problems.5,20-25 On the other hand, it can be stated that the shift work-related problems are attributed to their job stress. Previous studies have demonstrated that job stress can negatively affect nurses' performance.18,26,27Therefore, the conceptual model of this study is in accordance to the importance of shift problems and nurses' physical and mental health, considering that job stress can act as a mediator between shift work and its complications. Until now, few studies have focused on investigation of stress as a mediator to shift work and its complications. No model-based study has investigated the effect of such variables in Iran. Therefore, the present study aimed to design and present a conceptual model on the effects of workload and job stress on the shift work disorders among nurses. For this reason, the workload was considered as an independent variable, physical health, mental health, sleep quality, individual problems, and family problems were considered as the dependent variables. The job stress was considered as a mediator variable. Figure 1 shows the proposed conceptual model of this study.
Fig 1.
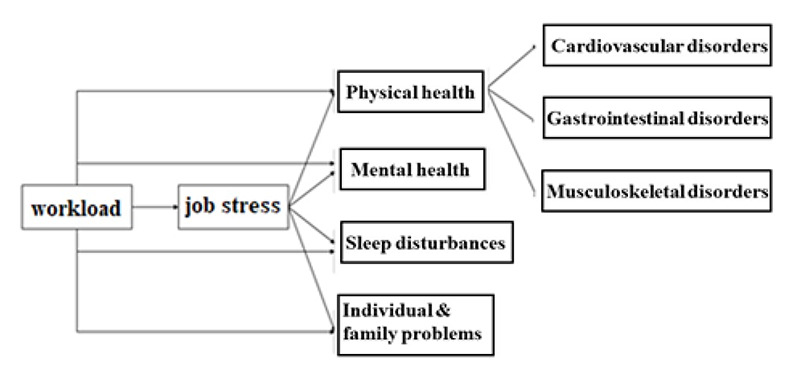
The proposed conceptual model
Materials and Methods
The aim of this study was to present a conceptual model through structural equation modeling in 2021. The research population included all nurse staffs in a specialty and sub-specialty hospital in Tehran. According to the statistics provided by vice-chancellorship for treatment, the total number of employed nurses in this hospital was estimated to be about 1000 individuals. Based on Krejcie and Morgan's Table according to Osipow,28 278 individuals were selected, and finally, 310 individuals were selected as the study population considering 10% of the possible fall. Inclusion criteria included having at least a bachelor's degree, at least one year of work experience and not having a second job. Moreover, the nurses with a history of severe personal stress and those who did not tend to cooperate in the study were excluded from the study. Finally, 300 questionnaires were analyzed. The protocol of the present study was approved by the Baqiyatallah University of Medical Sciences. The stratified random sampling was used for collecting the samples. In this study, various questionnaires were used for collecting the data including demographic characteristic, job stress and survey of shift workers (SOS) questionnaires. Demographic questionnaire consisted of questions regarding demographic variables such as gender, age, level of education, and work experience. Osipow Occupational Stress Inventory was developed in 1987 by Osipow et al.28 to assess individual stress in six dimensions including role overload, role insufficiency, role ambiguity, role boundary, role responsibility and work environment. This questionnaire consisted of 60 questions, which each of them are assessed using 10 questions. The scoring of this questionnaire is based on the Likert scale which includes never (number1) to most of the time (number 5). Some of the questions in this questionnaire have a reverse scoring range. This questionnaire measures the stress level of individuals based on their gender. The scale of assessment based on gender is presented in Table 1. This questionnaire was calculated by 89% in Iranian society by Komeili-Sani et al. using Cronbach's alpha coefficient.29 The SOS questionnaire was first introduced by Barton et al. based on the standard shift work index.30 This questionnaire has three sections of general information, individual differences and tolerance of shift work, and consists of questions related to the population and individual characteristics (11 questions), type of shift system (3 questions), job satisfaction (5 questions), mental - psychological problems (10 questions), gastrointestinal problems (8 questions), cardiovascular problems (5 questions), sleep disturbances (4 questions), musculoskeletal disorders (4 questions), and the adverse effects of shift work on individual and family life (4 questions). Scoring of this questionnaire is graded as a 4-point Likert scale from never (1 point) to always (4). The validity of this questionnaire was confirmed by Choobineh et al. using content and structural validity.31 Kuder-Richardson method was also used for the reliability, which was obtained to be about 81%.30 Pordanjani et al. determined the reliability of this questionnaire using Cronbach's alpha coefficient, which was calculated to be 0.67, 0.86, 0.87, 0.85, 0.79 and 0.87 for workload, cardiovascular, gastrointestinal, musculoskeletal, general health and sleep disorders, respectively.31Preliminary analyses such as mean, standard deviation and data normality test were performed using SPSS software. Then, the validity analysis of the variables was observed using Smart-PLS software, and finally, the research hypotheses were examined according to the research objectives using the Structural Equation Modeling (SEM) and given to the results of path coefficients.32 SEM is a method of multivariate statistical analysis and a combination of factor analysis, path analysis and regression, and is a comprehensive statistical approach to identify hidden variables related to an index.33 In order to evaluate the normality of the variables distribution, kurtosis and skewness tests were used. The measurement model was evaluated in two stages using first-order confirmatory factor analysis and second-order confirmatory factor analysis. Cronbach's alpha (α) and composite reliability (CR) were used to evaluate the reliability. Finally, two criteria of convergent validity and divergent validity were used to evaluate the validity of the model. In order to evaluate the convergent and divergent validity, the extracted mean variance index and Fornell-Larcker and HTMT ratio methods were used, respectively.
Table 1.
Scale of Osipow questionnaire based on gender
| Stress | Questionnaire Score | |
|---|---|---|
| Female | Male | |
| No Stress | 60-107 | 60-133 |
| Normal | 108-203 | 134-216 |
| Medium | 204-251 | 217-258 |
| Severe | 252-300 | 259-300 |
Table 2.
Results of descriptive statistics of demographic variables
| Variable | Item | Number | Frequency |
|---|---|---|---|
| Male | 116 | 38.7 | |
| Gender | |||
| Female | 184 | 61.3 | |
| < 25 | 87 | 29.0 | |
| 25-35 | 91 | 30.3 | |
| Age | 36-45 | 83 | 27.7 |
| >45 | 39 | 13.0 | |
| Educationnel | Under graduate | 215 | 71.6 |
| Level | Graduate | 85 | 28.3 |
| < 10 | 125 | 41.7 | |
| Work Exprience | 10-20 | 143 | 47.7 |
| > 20 | 32 | 10.7 |
Results
The study population consisted of 300 nurses from a specialty and sub-specialty hospital in Tehran. Of them, 61.3% were female and 38.7% male. Most participants (30.3%) were in the age range 25-35 years. Table 2 shows that 215 participants had a bachelor's degree and 85 had a postgraduate degree. Therefore, most of the participants in this project (71.6%) had a bachelor's degree. Table 2 presents the demographic variables.
As all statistical tests, the normality of the variables distribution should be tested in SEM.34 In this study, kurtosis and skewness test were used to investigate the claim about the distribution of a quantitative variable data. According to the suggestion of George and Mahler,35 the acceptable range of skewness and kurtosis is +2 and -2. The results showed that the amount of skewness and kurtosis of all items was in the range of +2 and -2. Therefore, no violation of data normality was observed, As a result, it can be stated that all items were normal. The measurement model was evaluated in two steps. In the first stage, the results of the first-order confirmatory factor analysis were performed for all research items and related variables, and in the second stage, second-order confirmatory factor analysis was performed due to the fact that the variables of job stress, mental and physical health have dimensions.
Factor loading coefficients of items (questions) are the first factor to be considered in reflective models. According to Chin,34 the standardized factor loading of each item should be greater than 0.5; at this stage, two indices of Cronbach's alpha coefficient (α) and composite reliability criterion (CR) were used to evaluate the reliability of the research items, in which values above 0.7 are acceptable for the reliability of the measurement model.35 To evaluate the validity of the model, two criteria of convergent validity and divergent validity were used. In order to evaluate the convergent validity, the extracted mean variance index (2) was used, which should ≥0.5 according to Fornell-Larcker.36 In order to evaluate the divergent validity, Fornell-Larcker and HTMT ratio methods were used. The results showed that the values of all factor loadings are greater than 0.5 and the observable variables are a reliable scale for calculating the latent variables of the model. Table 3 shows the fitting results of the proposed conceptual model.
Table 3.
Results of factor loadings and convergent validity and reliability coefficients
| Main variables (latent) | Cronbach's alpha (α) | CR | Extracted Mean variance | |
|---|---|---|---|---|
| Occupational Stress Inventory | Loading role | 0.965 | 0.965 | 0.733 |
|
|
Insufficiency role | 0.955 | 0.956 | 0.69 |
|
|
Ambiguity role | 0.969 | 0.969 | 0.756 |
|
|
Boundary role | 0.959 | 0.958 | 0.697 |
|
|
Responsibility | 0.957 | 0.958 | 0.697 |
|
|
Physical environment | 0.936 | 0.934 | 0.59 |
|
|
Physical symptoms | 0.937 | 0.938 | 0.658 |
| survey of shift workers questionnaire | Social function | 0.942 | 0.942 | 0.701 |
|
|
Anxiety symptoms | 0.947 | 0.72 | 0.947 |
|
|
Depression Symptoms | 0.914 | 0.914 | 0.605 |
|
|
Cardiovascular complications | 0.905 | 0.905 | 0.704 |
|
|
Skeletal and muscular complications | 0.934 | 0.934 | 0.779 |
|
|
Gastrointestinal complications | 1 | 1 | 1 |
|
|
Workload | 0.856 | 0.856 | 0.665 |
|
|
sleep quality | 0.823 | 0.827 | 0.706 |
|
|
Individual and family problems | 0.900 | 0.900 | 0.751 |
Table 4.
Divergent validity matrix by Fornell -Locker method (second order structure)
| variables | Job stress | Physical health | Individual and family problems | Sleep quality | Mental health | Workload |
|---|---|---|---|---|---|---|
| Job stress | 0.784 | |||||
| Physical health | -0.538 | 0.794 | ||||
| Individual and family problems | -0.594 | 0.298 | 0.866 | |||
| Sleep quality | -0.47 | 0.462 | 0.347 | 0.84 | ||
| Mental health | -0.513 | 0.385 | 0.304 | 0.428 | 0.771 | |
| Workload | 0.747 | -0.514 | -0.535 | -0.455 | -0.511 | 0.815 |
Table 5.
Divergent validity matrix using HTMT index method (second order structure)
| Variables | Job stress | Physical health | Individual and family problems | Sleep quality | Mental health |
|---|---|---|---|---|---|
| Job stress | |||||
| Physical health | 0.538 | ||||
| Individual and family problems | 0.588 | 0.299 | |||
| Sleep quality | 0.469 | 0.498 | 0.346 | ||
| Mental health | 0.512 | 0.412 | 0.308 | 0.433 | |
| Workload | 0.737 | 0.522 | 0.536 | 0.456 | 0.512 |
According to Table 3, CR results were between 0.934 and 0.969, which showed that CR obtained for all variables was higher than 0.7, which is acceptable.35 Cronbach's alpha results showed that the values of all variables are higher than 0.7. All extracted mean variances are greater than 0.5, and between 0.590 and 0.756, indicating that convergent validity is confirmed for the variables in this study. According to the above results, it can be stated that the convergent reliability and validity of all variables are acceptable.
For divergent validity, Fornell-Larcker and HTMT ratio methods were used. In Fornell-Larcker method, the relationship between the extracted squares of variance and the mean correlation was used to show the divergent validity. According to Fornell-Larcker, the extracted square of variance should be greater than the mean correlation of the variables. HTMT criterion measures the ratio of multiple attributes of observed variables to their single attributes. If this ratio is less than 0.9, the measurement model has validity conditions. Table 4 shows the divergent validity matrix by Fornell-Locker method. The correlation between the structures is less than the mean square of the extracted variance of each structure, which shows that no two variables are completely correlated with each other. The composition of the items indicates that the structures are well separated from each other. Therefore, the measurement tool has a divergent validity.
Table 5 shows the results of HTMT index survey. All values are less than 0.9 and show that the measurement tool is divergent according to this criterion.37
The evaluation results of the second-order measurement model are shown in Figure 2. According to Table 6, the values of R2 are calculated for the endogenous structures of the research and confirm the suitability of the structural model fitting according to the criterion value. According to Cohen,38 three values of 0.02, 0.16 and 0.26 are considered as the criterion values for weak, medium and strong. Therefore, the effect of independent variables on the dependent variables of this research was desirable and strong.
Fig 2.
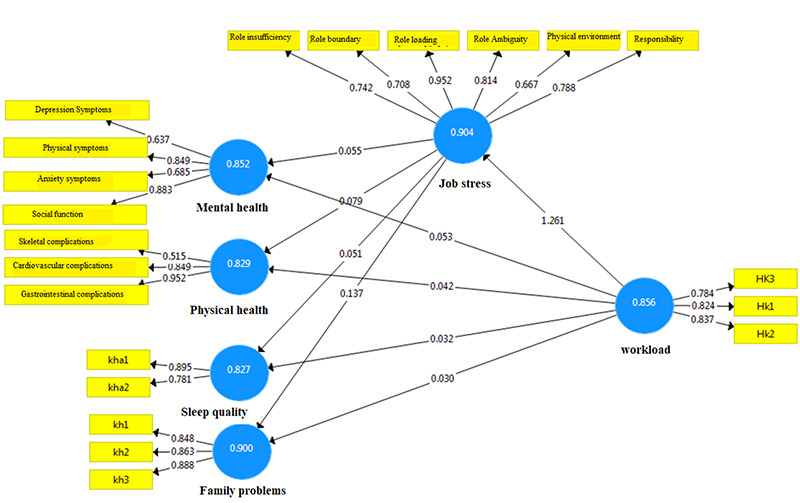
Evaluation of the measurement model (second order).
Table 6.
Results of determination coefficient of R2 and redundancy validity (CV Red)
| Endogenous latent variables | Determination coefficient of R2 0.558 | Redundancy validity (CV Red) 0.283 |
|---|---|---|
| Job stress |
|
|
| Physical health | 0.318 | 0.182 |
| Individual and family problems | 0.372 | 0.258 |
| Sleep quality | 0.245 | 0.153 |
| Mental health | 0.300 | 0.161 |
In this study, in order to evaluate the quality or validity of the model, the validity index of redundancy was used. According to Table 6, the redundancy index for all endogenous variables was more than zero, so it can be concluded that the structural model of this study has the appropriate predictive power for endogenous variables.
The effect size criterion (f2), introduced by Cohen,38 determines the intensity of the relationship between model structures. The effect size criterion uses R2 index to analyze the relationship between structures. The values of 0.02, 0.15 and 0.35 indicate the small, medium and large effect size of one structure on another, respectively. According to the mentioned values, the effect of workload on job stress, mental health, physical health, sleep quality and individual and family problems are equal to 1.261, 0.053, 0.042, 0.32 and 0.30, respectively. The effect size of workload on job stress is "large" and on other quality-dependent variables is "small". The effect of job stress on mental health, physical health, sleep quality and individual and family problems were 0.055, 0.079, 0.051 and 0.137, respectively. The effect size of job stress on the variables depended to this variable was "small".
In this study, the relevant hypotheses were tested based on bootstrap (value 10,000). The level of error defined in this study was obtained to be 0.05, and t-value was higher than 1.96, indicating the hypothesis acceptance. The final model is shown in Figure 3.
The investigation of the results of testing the hypotheses showed that the path of "workload to job stress" was significant at the level of 0.01 and the critical value of 14.428. The amount of factor loading was equal to 0.747. According to the obtained values, the hypothesis that "workload has an effect on job stress" was confirmed. The results of the path "workload to mental health" showed that the p-value was less than 0.05, and also the critical ratio value (2.251) for this path was more than 1.96. So, the effect of workload on mental health was significant at the level of 95%. It should be noted that the open value of the standardized factor for this path was 1.291, which indicated the effect of workload on mental health. The results showed that the path of "workload to physical health" was significant at the level of 95% (significant value was equal to 0.014 and < 0.05) and the amount of standardized factor loading (-0.253) for this path showed the negative impact of "workload" on "physical health". The results confirmed the hypothesis that "workload has an effect on physical health". In relation to the hypothesis of “workload to sleep quality”, given that p-value was less than 0.05, it can be claimed that this hypothesis is confirmed by an error coefficient of 5%. Therefore, it can be claimed that workload affects the sleep quality. The results showed that the path of "workload to individual and family problems" was significant at the level of 95% (significant value is equal to 0.038 and less than 0.05), and the amount of standardized factor loading (-0.206) for this path shows the negative impact of "workload" on "individual and family problems". The results confirm the hypothesis that "workload has an effect on physical health". The results of the path of "job stress on mental health" show that p-value is less than 0.01 and the value of the critical ratio (2.670) for this path is more than 1.96, which indicates the effect of job stress on mental health is significant at 99%. The relationship between job stress and physical health was calculated to be equal to -0.349, and the critical ratio value was 3.534, which was greater than t-critical value (1.96) and shows that the observed relationship is significant. Therefore, it can be said that job stress affects physical health by a confidence level of 95%. The results of the path of “job stress to sleep quality” showed that the standardized factor loading for this path was -0.295 and the significance level was equal to 0.0011, which was less than 0.05. According to the results, the hypothesis that "Job stress has an effect on sleep quality" was confirmed at a confidence level of 95%. The results of the hypothesis that job stress affects individual and family problems showed that p-value was less than 0.001, which confirmed the hypothesis by 1% level. The results of hypothesis testing are shown in Table 8.
Table 7.
Effect size results (f2)
| Path | The effect size criterion (f2) |
|---|---|
| Workload->job stress | 1.261 |
| Workload->mental health | 0.053 |
| Workload->physical health | 0.042 |
| Workload->sleep quality | 0.032 |
| Workload-> individual& family problems | 0.030 |
| Job stress->mental health | 0.055 |
| Job stress-> physical health | 0.079 |
| Job stress-> sleep quality | 0.051 |
| Job stress-> individual & family problems | 0.137 |
Fig 3.
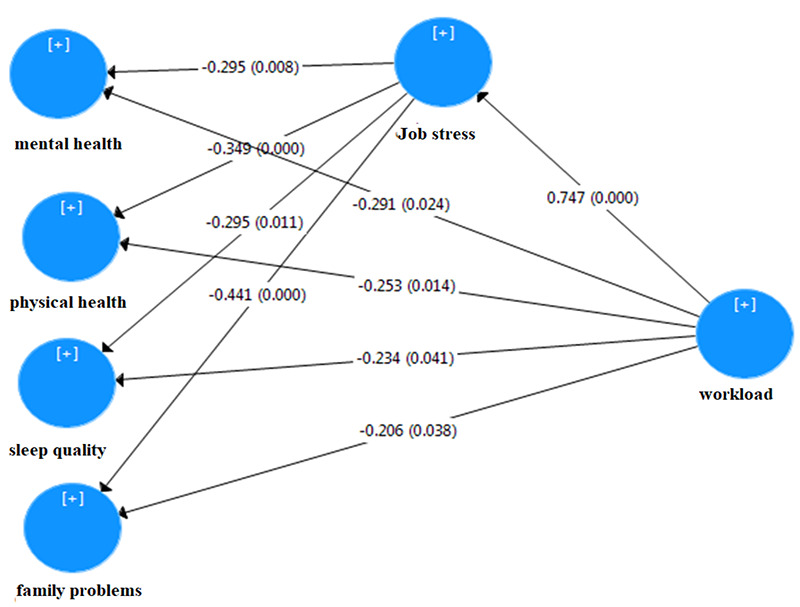
Evaluation of the measurement model (second order)
Discussion
The aim of this study was to present a model of the workload and job stress effect on shift work-related disorders in nurses. The proposed model provided an appropriate summary of the research background about the mediation role of job stress and shift work complications that can be used in future studies. The overall results of the conceptual model showed that the proposed model had acceptable convergent and divergent validity and reliability, so it had sufficient credibility. The calculated R2 values for the endogenous structures of the research confirmed the proposed conceptual model fitting. The effect of independent variables on the dependent variables of this research was estimated to be desirable and strong. Finally, the redundancy index was used to check the validity of the model, which showed that the proposed model had a good predictive power for endogenous variables.
Table 8.
Hypothesis test results
| Hypothes is | Path | Coefficient of path (β) | Critical value (t) | Significan ce level | Conclusion |
|---|---|---|---|---|---|
| 1 | Workload->job stress | 0.747 | 14.428 | 0.001 | Significant |
| 2 | Workload->mental health | -0.291 | 2.251 | 0.024 | Significant |
| 3 | Workload->physicalhealth | -0.253 | 2.446 | 0.014 | Significant |
| 4 | Workload->sleepquality | -0.234 | 2.044 | 0.041 | Significant |
| 5 | Workload->individual&familypro blems | -0.206 | 2.073 | 0.038 | Significant |
| 6 | Job stress->mental health | -0.295 | 2.67 | 0.008 | Significant |
| 7 | Job stress->physicalhealth | -0.349 | 3.534 | 0.001 | Significant |
| 8 | Job stress-> sleep quality | -0.295 | 2.545 | 0.011 | Significant |
| 9 | Job stress-> individual & family problems | -0.441 | 4.823 | 0.001 | Significant |
The results of the model evaluation showed that workload both directly and indirectly has an effect on physical and mental health, sleep quality and individual and family problems through job stress mediation. Work over-load, lack of manpower, low freedom of action, long working hours always cause stress and fatigue in nurses and endanger their physical health. Previous studies have shown that work over-load is the main cause of job stress.39-41
The results of the present study showed that workload and job stress can endanger people's physical health. Accordance to the results of this study, other studies have shown that job stress along with a work over-load acts as an important factor in reducing the life quality of nurses and creating health problems for them. It has been also reported that stress is significantly associated with many physical problems such as migraine, muscle pain, back and joints pain, hypertension, acute myocardial infarction, irritable bowel syndrome, duodenal ulcer, immune system and endocrine diseases. Quantitative and qualitative work overload can lead to physiological changes, increased blood cholesterol and increased heart beat.42-46
The conceptual model of the present study demonstrated that workload and job stress increase people's mental health problems and disorders. In accordance with the present study, the results of other studies also showed a significant relationship between stress levels and psychological problems such as anxiety, low self-esteem, depression and feelings of inadequacy.47-50 In another study, the researchers stated that the quantitative workload is an external factor imposed on people through the work environment and cannot lead to psychological problems; however, it leads to time limitation and mental pressure in the person. While the qualitative workload has an internal and mentality aspect in which the person does not see himself adequate and suitable for his job and this feeling of inadequacy leads to depression, hostility, anxiety and job stress.11
The results of the present study indicated that workload directly or indirectly leads to sleep disorders in nurses through the mediation role of job stress. Previous studies have shown that workload had a direct negative effect on sleep quality.5,11,13,20 Moreover, several studies have reported that work over-load had a negative effect on sleep by increasing job stress leading to suppression of sleepiness, sleep related respiratory disorders, lack of sleep and reduced sleep hours.32 Shift work is an integral part of the health system and poses many complications to nurses. It is noteworthy that effective strategies can be used to reduce job stress, and consequently mental and physical disorders, sleep disorders, and individual and family life problems in nurses. Since the sampling was performed during COVID 19 pandemic, the nurses possibly were affected by the disease, and hence more extensive and detailed studies are needed to confirm our findings.
One of the most important limitations of this study was the lack of generalizability of its results to all healthcare workers due to the use of information from only one hospital, and it is necessary to conduct this study in other hospitals with a larger population.
In general, the results of the present study show that job stress caused by work over-load among nurses can lead to physical and mental health problems, sleep disorders and individual and family problems. Therefore, in order to minimize the medical errors and accidents, to improve the health and safety of nurses, the economic and productivity of the health system, more studies are required to be conducted on control job stress and its complications in nurses.
Acknowledgments
The authors would like to state their gratitude to all the nurses who participated in this study. We would like to thanks the valuable tips and advice of the Clinical Research Development Unit of Baqiyatallah Hospital (Ethics code: IR.BMSU.REC.1399.258, project code: 98000079).
List of acronyms
- CR
composite reliability
- f2
effect size criterion
- R2
size criterion uses
- SEM
Structural Equation Modeling
- SOS
survey of shift workers
Funding Statement
Funding: The authors received no specific funding for this work.
Contributor Information
Keivan Saedpanah, Email: Keivan.Saedpanah@gmail.com.
Mohammad Ghasemi, Email: Ghasemi:mghmed@yahoo.com.
Hesam Akbari, Email: hesam120@yahoo.com.
Amir Adibzadeh, Email: adibzadeh_251@yahoo.com.
References
- 1.Moreno CR, Louzada FM. What happens to the body when one works at night? Cad SaudePublica. 2004. Nov-Dec;20(6):1739-45. doi: 10.1590/s0102-311x2004000600034. Epub 2004. Dec 8. [DOI] [PubMed] [Google Scholar]
- 2.Esquirol Y, Perret B, Ruidavets JB, Marquie JC, Dienne E, Niezborala M, Ferrieres J. Shift work and cardiovascular risk factors: new knowledge from the past decade. Arch Cardiovasc Dis. 2011. Dec;104(12):636-68.doi: 10.1016/j.acvd.2011.09. 004. Epub 2011. Nov 21. [DOI] [PubMed] [Google Scholar]
- 3.Rouch I, Wild P, Ansiau D, Marquié JC. Shiftwork experience, age and cognitive performance. Ergonomics. 2005. Aug 15;48(10):1282-93. doi: 10.1080/00140130500241670. [DOI] [PubMed] [Google Scholar]
- 4.Ruiz-Fernández MD, Pérez-García E, Ortega-Galán ÁM. Quality of Life in Nursing Professionals: Burnout, Fatigue, and Compassion Satisfaction. Int J Environ Res Public Health. 2020. Feb 15;17(4):1253. doi: 10.3390/ijerph17041253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saksvik-Lehouillier I, Bjorvatn B, Hetland H, Sandal GM, Moen BE, Magerøy N, Akerstedt T, Pallesen S. Individual, situational and lifestyle factors related to shift work tolerance among nurses who are new to and experienced in night work. J AdvNurs. 2013. May;69(5):1136-46. doi: 10.1111/j.1365-2648.2012.06105.x. Epub 2012. Jul 31. [DOI] [PubMed] [Google Scholar]
- 6.Carayon P, Gürses AP. A human factors engineering conceptual framework of nursing workload and patient safety in intensive care units. Intensive Crit Care Nurs. 2005. Oct;21(5):284-301. doi: 10.1016/j.iccn.2004.12. 003. Epub 2005. Feb 24. [DOI] [PubMed] [Google Scholar]
- 7.Suzuki K, Ohida T, Kaneita Y, Yokoyama E, Uchiyama M. Daytime sleepiness, sleep habits and occupational accidents among hospital nurses. J AdvNurs. 2005. Nov;52(4):445-53. doi: 10.1111/j.1365-2648.2005.03610.x. [DOI] [PubMed] [Google Scholar]
- 8.Wong IS, Dawson D, VAN Dongen HPA. International consensus statements on non-standard working time arrangements and occupational health and safety. Ind Health. 2019;57(2):135-138. doi: 10.2486/indhealth. 57_202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ulrich B, Barden C, Cassidy L, Varn-Davis N. Critical Care Nurse Work Environments 2018: Findings and Implications. Crit Care Nurse. 2019. Apr;39(2):67-84. doi: 10.4037/ccn2019605. Epub 2019. Feb 6. [DOI] [PubMed] [Google Scholar]
- 10.Aiken LH, Sloane DM, Ball J, Bruyneel L, Rafferty AM, Griffiths P. Patient satisfaction with hospital care and nurses in England: an observational study. BMJ Open. 2018. Jan 11;8(1):e019189. doi: 10.1136/bmjopen-2017-019189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shaw JB, Weekley JA. The effects of objective work-load variations of psychological strain and post-work-load performance. J Manag. 1985. Apr;11(1):87-98. doi: 10.1177/01492063850110 0108 [Google Scholar]
- 12.Dall'Ora C, Ball J, Reinius M, Griffiths P. Burnout in nursing: a theoretical review. Hum Resour Health. 2020. Jun 5;18(1):41. doi: 10.1186/s12960-020-00469-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.D'Ettorre G, Pellicani V, Caroli A, Greco M. Shift work sleep disorder and job stress in shift nurses: implications for preventive interventions. Med Lav. 2020. Jun 26;111(3):195-202. doi: 10.23749/mdl.v111i3.9197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bardhan R, Heaton K, Davis M, Chen P, Dickinson DA, Lungu CT. A Cross Sectional Study Evaluating Psychosocial Job Stress and Health Risk in Emergency Department Nurses. Int J Environ Res Public Health. 2019. Sep 4;16(18):3243. doi: 10.3390/ijerph16183243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van der Wal RAB, Wallage J, Bucx MJL. Occupational stress, burnout and personality in anesthesiologists. Curr Opin Anaesthesiol. 2018. Jun;31(3):351-356. doi: 10.1097/ACO.00000000 00000587. [DOI] [PubMed] [Google Scholar]
- 16.Järvelin-Pasanen S, Sinikallio S, Tarvainen MP. Heart rate variability and occupational stress-systematic review. Ind Health. 2018. Nov 21;56(6):500-511. doi: 10.2486/indhealth.2017-0190. Epub 2018. Jun 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clough BA, March S, Chan RJ, Casey LM, Phillips R, Ireland MJ. Psychosocial interventions for managing occupational stress and burnout among medical doctors: a systematic review. Syst Rev. 2017. Jul 17;6(1):144. doi: 10.1186/s13643-017-0526-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jasiński AM, Derbis R, Walczak R. Workload, job satisfaction and occupational stress in Polish midwives before and during the COVID-19 pandemic. Med Pr. 2021. Dec 22;72(6):623-632. doi: 10.13075/mp.5893.01149. Epub 2021. Oct 12. [DOI] [PubMed] [Google Scholar]
- 19.Angermeyer MC, Bull N, Bernert S, Dietrich S, Kopf A. Burnout of caregivers: a comparison between partners of psychiatric patients and nurses. Arch Psychiatr Nurs. 2006. Aug;20(4):158-65. doi: 10.1016/j.apnu.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Gander P, van den Berg M, Signal L. Sleep and sleepiness of fishermen on rotating schedules. Chronobiol Int. 2008. Apr;25(2):389-98. doi: 10.1080/07420520802106728. [DOI] [PubMed] [Google Scholar]
- 21.Books C, Coody LC, Kauffman R, Abraham S. Night Shift Work and Its Health Effects on Nurses. Health Care Manag (Frederick). 2017. Oct/Dec;36(4):347-353. doi: 10.1097/HCM.000 0000000000177. [DOI] [PubMed] [Google Scholar]
- 22.Ribet C, Derriennic F. Age, working conditions, and sleep disorders: a longitudinal analysis in the French cohort E.S.T.E.V. Sleep. 1999. Jun 15;22(4):491-504. [PubMed] [Google Scholar]
- 23.Shader K, Broome ME, Broome CD, West ME, Nash M. Factors influencing satisfaction and anticipated turnover for nurses in an academic medical center. J Nurs Adm. 2001. Apr;31(4):210-6. doi: 10.1097/00005110-200104000-00010. [DOI] [PubMed] [Google Scholar]
- 24.Stevens RG. Light-at-night, circadian disruption and breast cancer: assessment of existing evidence. Int J Epidemiol. 2009. Aug;38(4):963-70. doi: 10.1093/ije/dyp178. Epub 2009. Apr 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lunde LK, Skare Ø, Mamen A, Sirnes PA, Aass HCD, Øvstebø R, Goffeng E, Matre D, Nielsen P, Heglum HSA, Hammer SE, Skogstad M. Cardiovascular Health Effects of Shift Work with Long Working Hours and Night Shifts: Study Protocol for a Three-Year Prospective Follow-Up Study on Industrial Workers. Int J Environ Res Public Health. 2020. Jan 16;17(2):589. doi: 10.3390/ijerph17020589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khamisa N, Oldenburg B, Peltzer K, Ilic D. Work related stress, burnout, job satisfaction and general health of nurses. Int J Environ Res Public Health. 2015. Jan 12;12(1):652-66. doi: 10.3390/ijerph120100652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rasool SF, Wang M, Zhang Y, Samma M. Sustainable Work Performance: The Roles of Workplace Violence and Occupational Stress. Int J Environ Res Public Health. 2020. Feb 1;17(3):912. doi: 10.3390/ijerph17030912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Osipow SH. Occupational stress inventory, revised edition (OSI-R). Psychological Assessment Resources, Incorporated; 1998. [Google Scholar]
- 29.Komeili-Sani M, Etemadi A, Boustani H, Bahreini M, Hakimi A. The relationship between nurses' clinical competency and job stress in Ahvaz university hospital. Journal of clinical nursing and midwifery. 2015;4. [Google Scholar]
- 30.Barton J, Spelten E, Totterdell P, Smith L, Folkard S, Costa G. The Standard Shiftwork Index: a battery of questionnaires for assessing shiftwork-related problems. Work & Stress. 1955;9(1):4-30. [Google Scholar]
- 31.Choobineh A, Soltanzadeh A, Tabatabai S, Jahangiri M, Khavvaji S. Comparison of shift work-related health problems in 12-hour shift schedules of petrochemical industries. Iran Occupational Health. 2010;7(4). 49-54. [Google Scholar]
- 32.Stein CM, Morris NJ, Hall NB, Nock NL. Structural Equation Modeling. Methods Mol Biol. 2017;1666:557-580. doi: 10.1007/978-1-4939-7274-6_28. [DOI] [PubMed] [Google Scholar]
- 33.George D. SPSS for windows step by step: A simple study guide and reference, 17. update, 10/e: Pearson Education India; 2011 [Google Scholar]
- 34.Chin WW. The partial least squares approach to structural equation modeling. Modern methods for business research. 1998;295(2). 295-336. [Google Scholar]
- 35.Nunnally JC. Psychometric theory 3E: Tata McGraw-hill education; 1994 [Google Scholar]
- 36.Fornell C, Larcker DF. Structural equation models with unobservable variables and measurement error: Algebra and statistics. Sage Publications Sage CA: Los Angeles, CA; 1981. [Google Scholar]
- 37.Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. Journal of the academy of marketing science. 2015;43(1)35-115. doi: 10.1007/s11747-014-0403-8 [Google Scholar]
- 38.Cohen J. Statistical power analysis Jbr the behavioral. Sciences Hillsdale (NJ): Lawrence Erlbaum Associates.1988.18-74. [Google Scholar]
- 39.Chang EM, Daly J, Hancock KM, Bidewell JW, Johnson A, Lambert VA, Lambert CE. The relationships among workplace stressors, coping methods, demographic characteristics, and health in Australian nurses. J Prof Nurs. 2006;22(1):30-8. doi: 10.1016/j.profnurs.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 40.Kokoroko E, Sanda MA. Effect of Workload on Job Stress of Ghanaian OPD Nurses: The Role of Coworker Support. Saf Health Work. 2019. Sep;10(3):341-346. doi: 10.1016/j.shaw.2019.04. 002. Epub 2019. Apr 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McNeely E. The consequences of job stress for nurses' health: time for a check-up. Nurs Outlook. 2005. Nov-Dec;53(6):291-9. doi: 10.1016/j. outlook.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 42.Wilson CB. Safer handling practice for nurses: a review of the literature. Br J Nurs. 2001. Jan 25-Feb 7;10(2):108-14. doi: 10.12968/bjon.2001.10.2. 5393. [DOI] [PubMed] [Google Scholar]
- 43.de Gaudemaris R, Levant A, Ehlinger V, Hérin F, Lepage B, Soulat JM, Sobaszek A, Kelly-Irving M, Lang T. Blood pressure and working conditions in hospital nurses and nursing assistants. The ORSOSA study. Arch Cardiovasc Dis. 2011. Feb;104(2):97-103. doi: 10.1016/j.acvd.2010. 12.001. Epub 2011. Jan 22. [DOI] [PubMed] [Google Scholar]
- 44.Mönnikes H, Tebbe JJ, Hildebrandt M, Arck P, Osmanoglou E, Rose M, Klapp B, Wiedenmann B, Heymann-Mönnikes I. Role of stress in functional gastrointestinal disorders. Evidence for stress-induced alterations in gastrointestinal motility and sensitivity. Dig Dis. 2001;19(3):201-11. doi: 10.1159/000050681. [DOI] [PubMed] [Google Scholar]
- 45.Chandola T, Brunner E, Marmot M. Chronic stress at work and the metabolic syndrome: prospective study. BMJ. 2006. Mar 4;332(7540):521-5. doi: 10.1136/bmj.38693.435301.80. Epub 2006. Jan 20. PMID: 16428252; PMCID: PMC1388129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Huang Y, Hu Y, Mai W. Stress and sleep disturbance--a connection in CVD. Nat Rev Cardiol. 2012. Oct;9(10):598; author reply 598. doi: 10.1038/nrcardio.2012.45-c1. Epub 2012. Aug 14. [DOI] [PubMed] [Google Scholar]
- 47.Olofsson B, Bengtsson C, Brink E. Absence of response: a study of nurses' experience of stress in the workplace. J Nurs Manag. 2003. Sep;11(5):351-8. doi: 10.1046/j.1365-2834.2003. 00384.x. [DOI] [PubMed] [Google Scholar]
- 48.Tennant C. Work-related stress and depressive disorders. J Psychosom Res. 2001. Nov;51(5):697-704. doi: 10.1016/s0022-3999(01)00255-0. [DOI] [PubMed] [Google Scholar]
- 49.Mealer ML, Shelton A, Berg B, Rothbaum B, Moss M. Increased prevalence of post-traumatic stress disorder symptoms in critical care nurses. Am J RespirCrit Care Med. 2007. Apr 1;175(7):693-7. doi: 10.1164/rccm.200606-735OC. Epub 2006. Dec 21. [DOI] [PubMed] [Google Scholar]
- 50.Arora VM, Georgitis E, Siddique J, Vekhter B, Woodruff JN, Humphrey HJ, Meltzer DO. Association of workload of on-call medical interns with on-call sleep duration, shift duration, and participation in educational activities. JAMA. 2008. Sep 10;300(10):1146-53. doi: 10.1001/jama.300. 10.1146. [DOI] [PubMed] [Google Scholar]


