Abstract
BACKGROUND AND OBJECTIVES:
Opioid related overdose among adolescents and young adults in the United States is rising. Medications for opioid use disorder (MOUD), including buprenorphine can reduce the risk of overdose, however they are underutilized. A better understanding of buprenorphine prescribing to youth will help inform interventions to expand access to treatment.
METHODS:
We used IQVIA data to examine buprenorphine dispensing trends among youth aged ≤19 years from 2015 to 2020. Dispensing was examined by prescriber specialty, age, and sex. Data were weighted to provide national estimates.
RESULTS:
The rate of buprenorphine dispensed to youth decreased 25% over the study period, from 0.84 to 0.63 prescriptions per 1000 youth per year. The proportion of youth dispensed buprenorphine also decreased 45%, from 7.6 to 4.2 persons per 100 000 per year. Over the same time, the proportion of adults aged ≥20 years dispensed buprenorphine increased 47%, from 378 to 593 persons per 100 000. Differences in dispensing by sex and temporal trends were also noted. Pediatricians accounted for less-than 2% of all prescriptions dispensed.
CONCLUSIONS:
Buprenorphine dispensing to youth is low and declining in recent years. Given rates of opioid use disorder among youth, these findings suggest that many youth who could benefit from MOUD are not receiving it. Pediatricians could play a role in expanding access to MOUD for this high-risk population. Efforts to expand access to MOUD for adolescents could include improving training in opioid use disorder treatment of pediatricians and encouraging all clinicians who care for adolescents and young adults to obtain waivers to prescribe buprenorphine for MOUD.
Drug overdose deaths in the United States have increased significantly in recent years, reaching the highest levels in history. During the 12-month period ending in January 2022, there were over 100 000 drug overdose deaths in the United States, with over 80 000 attributable to opioids.1 The rise in overdose deaths has largely been driven by increases in deaths associated with illicitly-manufactured fentanyl (IMF), with the proportion of IMF-associated deaths rising sharply from 2019 to 2020.2
Trends of opioid-associated mortality in adolescents mirrors that of the general population. The rate of opioid-involved overdose deaths in children and adolescents increased nearly four-fold from 2010 to 2021, with most of this increase driven by IMF.3 An analysis of data from 39 states and the District of Columbia identifying nearly 3000 opioid associated deaths in youth age 15 to 24 years in 2020 alone.2
Adolescents and young adults who use substances and who are diagnosed with substance use disorders including opioid use disorder (OUD) are at high risk for overdose death.4 From 2001 to 2014, diagnosis of OUD in adolescents and young adults increased nearly six-fold.5 Although reported lifetime use of opioids by adolescents has been falling in more recent years, the prevalence of use remains high.6 In 2019, 7.2% of high school students reported current prescription opioid misuse and that same year, an estimated 87 000 adolescents age 12 to 17 years reported an opioid use disorder.7,8 Identification of and initiating treatment in youth with substance use disorder could reduce their risk of overdose and overdose death.
Medications for opioid use disorder (MOUD), including buprenorphine, methadone, and naltrexone, are effective treatment of patients with OUD, and youth who receive MOUD are more likely to be retained in care.9,10 Multiple professional societies, including the American Academy of Pediatrics, American Society for Addiction Medicine, and the Society for Adolescent Health and Medicine, recommend that general pediatricians consider offering MOUD to at least some patients with OUD.11–13 The Society for Adolescent Health and Medicine recommends that all adolescents with OUD be offered medication management.12
Despite clear evidence of benefit in treatment of OUD and recommendations from professional organizations in support of its use in adolescents, MOUD in youth remains underutilized. One multistate study using Medicaid data found that less than a quarter of adolescents and young adults with OUD, and only 1-in-21 youth aged <18 years, received MOUD within 3 months of diagnosis.10 Another study found that only 1.9% of youth were prescribed pharmacotherapy within 30 days following a nonfatal overdose.14
Increasing access to evidence-based substance use disorder treatment including MOUD is a key component to improving outcomes for adolescents with OUD and reducing fatal and nonfatal overdoses. In 2000, Congress passed the Drug Addiction Treatment Act of 2000 (DATA 2000). This act requires clinicians seeking to administer or prescribe buprenorphine to seek a buprenorphine waiver. To obtain a waiver, clinicians must register a notification of intent with the Substance Abuse and Mental Health Services Administration. Since 2020, several changes have been enacted to facilitate greater prescribing of buprenorphine. Clinicians can now prescribe buprenorphine via telemedicine, and training requirements to obtain a DATA 2000 waiver have recently been eliminated for clinicians who may only prescribe to a limited number of patients. In theory, such flexibilities can pave the way for more clinicians to prescribe buprenorphine to adolescents. Buprenorphine is approved for use in children age ≥16 years and is frequently used off-label in younger adolescents. It has well-documented effectiveness, can be delivered in a primary care setting and has many advantages for use in adolescents.15–17 To date, no national estimates of buprenorphine dispensing have been published among youth. This study provides updated national estimates of buprenorphine dispensing among youth age ≤19 years among all payers. An improved understanding of national buprenorphine prescribing patterns among clinicians who treat adolescents with OUD could inform approaches to increasing access to buprenorphine and other MOUD services and linking adolescents to care after OUD diagnosis or an overdose event.
METHODS
We used IQVIA National Prescription Audit New to Brand and Total Patient Tracker data, which contains prescriptions dispensed from approximately 48 900 retail pharmacies, representing 92% of all prescriptions in the United States, to describe buprenorphine dispensing trends in youth from 2015 to 2020. These data are well suited for this analysis as it includes all payers and is projected to be nationally representative of all prescriptions dispensed from retail pharmacies in the United States. Youth was defined as individuals aged ≤19 years. For comparison purposes buprenorphine dispensing was also examined among adults aged ≥20 years. Buprenorphine products not approved for OUD were excluded and it was assumed that all prescriptions analyzed were for OUD treatment. Cross-sectional analyses were used to describe buprenorphine dispensing trends over time and by age, sex, and prescriber specialty. Monthly and annual dispensing rates of buprenorphine prescriptions per 1000 youth age ≤19 years and annual rates of all individuals dispensed at least 1 buprenorphine prescription per 100 000 US population were calculated by age group using annual population estimates from the US Census Bureau.18 Analysis was performed in Microsoft Excel (2017). This study was reviewed by the Centers for Disease Control and Prevention and it was determined that it met the definition of research as defined in HHS regulation 45 CFR 46.102(l) but did not involve human subjects as defined in 45 CFR 46.103(e). Thus, Institutional Review Board review was not required.
RESULTS
From 2015 to 2020, 347 905 buprenorphine prescriptions were dispensed to youth aged ≤19 years in the United States, an average of 57 984 prescriptions annually (0.71 prescriptions per 1000 US population). The annual rate of buprenorphine dispensing decreased 25%, from 0.84 to 0.63 prescriptions per 1000 persons between 2015 and 2020 (Table 1). A temporal pattern was observed, with buprenorphine dispensing lowest in the winter months and highest in the autumn months (Fig 1).
TABLE 1.
Annual Rate of Buprenorphine Prescriptions Dispensed to Youth Aged ≤19 y by Prescriber Specialty – United States, 2015 to 2020
| Specialty | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | % Change 2015–2020 % | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Ratea | N | Ratea | N | Ratea | N | Ratea | N | Ratea | N | Ratea | ||
| Total | 68 857 | 0.84 | 61 096 | 0.74 | 67 003 | 0.82 | 48 890 | 0.60 | 50 374 | 0.62 | 51 685 | 0.63 | −25 |
| N | % | N | % | N | % | N | % | N | % | N | % | ||
| Family medicine | 15 028 | 21.8 | 13 072 | 21.4 | 14 594 | 21.8 | 8879 | 18.2 | 8659 | 17.2 | 8715 | 16.9 | −42 |
| Psychiatry | 14152 | 18.9 | 11 523 | 18.9 | 12 205 | 18.2 | 7051 | 14.4 | 5656 | 11.2 | 5236 | 10.1 | −63 |
| General practice or unspecified specialtyb | 12 253 | 17.2 | 10 533 | 17.2 | 10 556 | 15.8 | 7036 | 14.4 | 6414 | 12.7 | 5508 | 10.7 | −55 |
| Internal medicine | 9394 | 14.7 | 8972 | 14.7 | 8912 | 13.3 | 6690 | 13.7 | 6214 | 12.3 | 4991 | 9.7 | −47 |
| Nurse practitioner | 214 | 0.2 | 146 | 0.2 | 1504 | 2.2 | 4225 | 8.6 | 8900 | 17.7 | 13 764 | 26.6 | 6332 |
| Surgical specialties | 3546 | 6.2 | 3771 | 6.2 | 4992 | 7.5 | 2614 | 5.3 | 2086 | 4.1 | 1765 | 3.4 | −50 |
| Anesthesia, pain, or PM and R | 3301 | 5.4 | 3272 | 5.4 | 3999 | 6.0 | 3375 | 6.9 | 2594 | 5.1 | 2036 | 3.9 | −38 |
| Emergency medicine | 2587 | 3.1 | 1920 | 3.1 | 2264 | 3.4 | 1506 | 3.1 | 1419 | 2.8 | 1172 | 2.3 | −55 |
| Other medical or pediatric subspecialitiesc | 2310 | 3.6 | 2180 | 3.6 | 2142 | 3.2 | 1480 | 3.0 | 1354 | 2.7 | 972 | 1.9 | −58 |
| Physician assistant | 79 | 0.2 | 108 | 0.2 | 595 | 0.9 | 1724 | 3.5 | 2747 | 5.5 | 3386 | 6.6 | 4186 |
| Addiction medicine | 1716 | 2.2 | 1339 | 2.2 | 1222 | 1.8 | 730 | 1.5 | 820 | 1.6 | 917 | 1.8 | −47 |
| Pediatrics (including MED-PEDS) | 889 | 2.1 | 1274 | 2.1 | 1116 | 1.7 | 825 | 1.7 | 436 | 0.9 | 541 | 1.0 | −39 |
| Other | 1373 | 1.6 | 970 | 1.6 | 885 | 1.3 | 737 | 1.5 | 1056 | 2.1 | 662 | 1.3 | −52 |
Data source: IQVIA National Prescription Audit (NPA) new to brand data (2015–2020). PM, physical medicine; R, rehabilitation.
Prescriptions per 1000 persons.
Includes general practice, general osteopathic medicine, and other unspecified specialty.
Does not include medicine-pediatrics.
FIGURE 1.
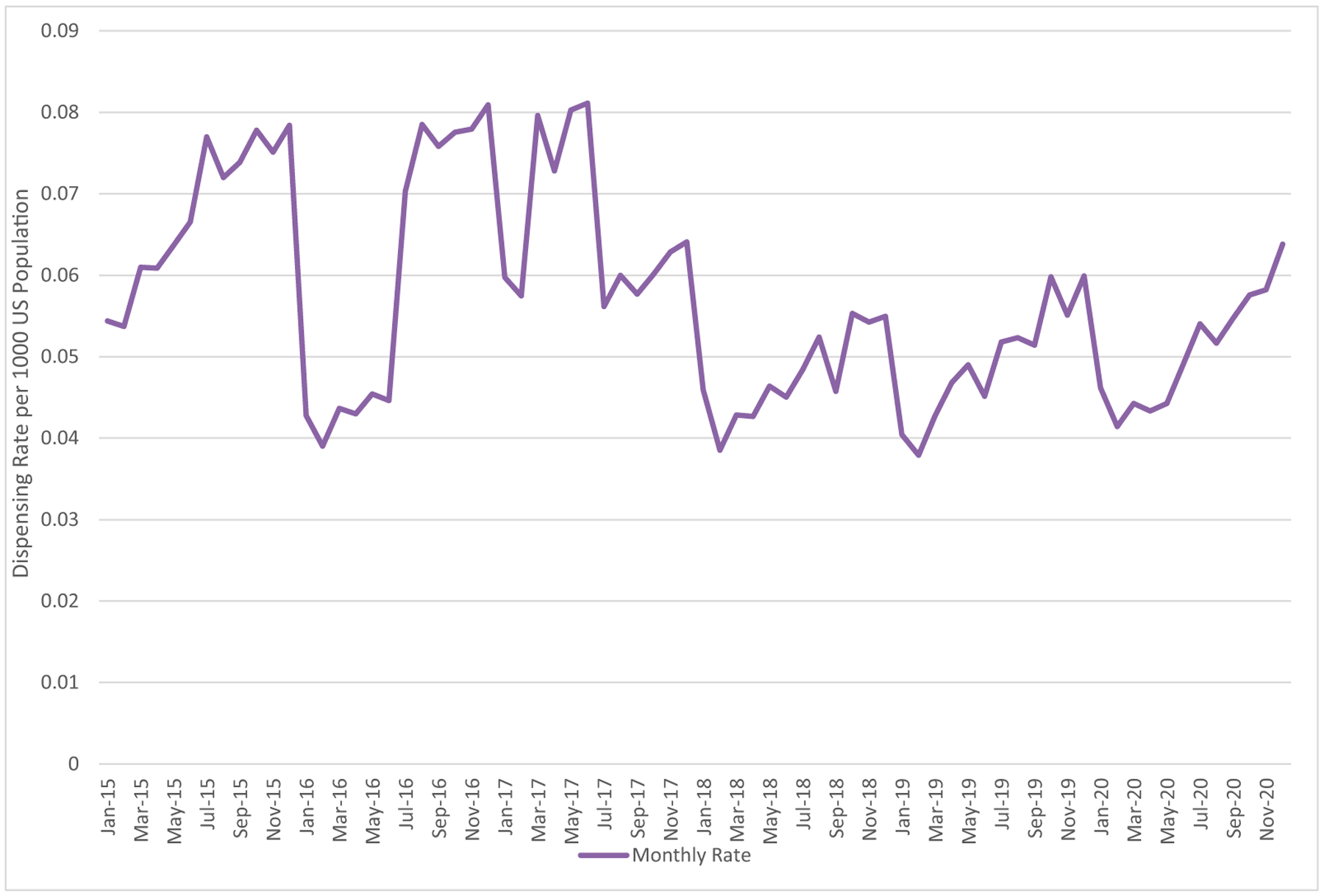
Buprenorphine prescription dispensing rates to youth aged 0 to 19 years, 2015 to 2020. Buprenorphine dispensing rates to youth varied over the calendar year. Average dispensing rates to youth declined from 2015 to 2020. Data source: IQVIA NPA data (2015–2020).
Buprenorphine dispensing to youth stratified by prescriber specialty is shown in Table 1. The number of buprenorphine prescriptions dispensed declined across all prescribing specialties except nurse practitioners and physician assistants. Pediatricians prescribed only a small fraction (1.0% to 2.1%) of all buprenorphine prescriptions dispensed. Prescriptions by pediatricians declined by 39% from 2015 to 2020. Among specialties with a decline, the decrease ranged from 38% to 63% (mean 50%), whereas prescriptions from nurse practitioners and physician assistants increased by 6332% and 4186%, respectively. The largest reductions were observed among general practice physicians or physicians with an unspecified specialty and psychiatrists with 55% and 63% reductions, respectively.
From 2015 to 2018, family medicine physicians were the largest prescribing specialty, followed by psychiatrists and general practitioners or nonspecialty trained physicians, prescribing approximately 18% to 21%, 14% to 18% and 14% to 17% respectively of prescriptions dispensed annually. In 2020, nurse practitioners were the leading prescribers (26.6%), followed by family medicine physicians (16.9%). Other subspecialties prescribing a small but notable proportion of buprenorphine prescriptions dispensed in 2020 are surgical subspecialities (3.4%), anesthesiology and pain specialists (3.9%), and addiction medicine specialists (1.8%).
Buprenorphine was dispensed to 22 393 (data not shown) unique youths from 2015 to 2020 (4169 annually; 5.1 of 100 000 persons-per-year). The proportion of youth receiving a prescription declined 45% over the same period (2015, 7.6 of 100 000 vs 2020, 4.17 of 100 000) (Table 2). Differences in dispensing to males versus females were noted. In 2015, the proportion of males and females receiving buprenorphine was similar (7.69 of 100 000 vs 7.63 of 100 000). However, from 2015 to 2020, a larger decrease in unique individuals was observed among females compared with males (54% decrease compared with 38%). By 2020, the proportion receiving a prescription among females was 26% less compared with males.
TABLE 2.
Annual Rate of Youth Aged ≤19 y Who Had at Least One Buprenorphine Prescription Tilled, by Age Group and Sex — United States, 2015–2020
| 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | Mean (Rate) | % Change 2015–2020 % | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Rateb | N | Rateb | N | Rateb | N | Rateb | N | Rateb | N | Rateb | |||
| Total adults (20+ years) | 904 796 | 379.3 | 1 001 783 | 416.0 | 1 104 775 | 454.8 | 1 177 558 | 481.0 | 1 292 018 | 523.9 | 1 327 100 | 538.1 | 1 134672 (465.5) | 47 |
| Total youth (0–19 y) | 6244 | 7.61 | 4941 | 6.02 | 4017 | 4.89 | 3316 | 4.05 | 3091 | 3.79 | 3405 | 4.17 | 4169 (5.09) | −45 |
| Annual prescriptions per youth | 11.0 | — | 12.4 | — | 16.7 | — | 14.7 | — | 16.3 | — | 16.3 | — | 15.2 | 38 |
| Sexa | ||||||||||||||
| Male | 3226 | 7.69 | 2467 | 5.88 | 1972 | 4.70 | 1604 | 3.83 | 1662 | 3.99 | 2013 | 4.83 | 2157 (5.15) | −38 |
| Female | 3061 | 7.63 | 2485 | 6.19 | 2035 | 5.07 | 1700 | 4.24 | 1416 | 3.55 | 1407 | 3.52 | 2019 (5.03) | −54 |
| Age (years) | ||||||||||||||
| 0–5 | 119 | 0.50 | 152 | 0.63 | 111 | 0.46 | 84 | 0.35 | 126 | 0.53 | 246 | 1.04 | 140 (0.59) | 109 |
| 6–11 | 23 | 0.09 | 47 | 0.19 | 48 | 0.20 | 40 | 0.16 | 37 | 0.15 | 59 | 0.24 | 46 (0.19) | 89 |
| 12–17 | 581 | 2.33 | 473 | 1.89 | 375 | 1.50 | 253 | 1.01 | 223 | 0.89 | 341 | 1.36 | 372 (1.49) | −41 |
| 18–19 | 5521 | 65.25 | 4269 | 50.48 | 3482 | 41.08 | 2938 | 34.30 | 2705 | 31.50 | 2758 | 32.12 | 3612 (42.39) | −51 |
Data source: IQVIA Total Patient Tracker (TPT) data (2015–2020). —, not applicable.
Number of patients do not add to the total because of a small number of individuals with unspecified sex.
Individuals per 100 000 with at least 1 buprenorphine prescription filled.
Among youth, buprenorphine dispensing also varied by age (Table 2). Most youth dispensed buprenorphine were aged 18 to 19 years (87%). The mean number of adolescents aged 12 to 17 years dispensed buprenorphine annually was 375 compared with 3612 among those aged 18 to 19 years. The number of unique youth aged 12 to 17 years and 18 to 19 years with a buprenorphine prescription declined by 41% and 51%, respectively from 2015 to 2020.
Although the number of children aged ≤12 years with a buprenorphine prescription increased, the absolute numbers were small (N = 1092). Most youth with a buprenorphine prescription in this age range were aged ≤5 years. The proportion of youth receiving buprenorphine was substantially lower than adults age ≥20 years. From 2015 to 2020, an average of 4169 unique youth (5.09 of 100 000) received a prescription annually compared with 1 134 672 adults age >20 years (465.5 of 100 000). From 2015 to 2020, the number of adults aged ≥ 20 years receiving a buprenorphine prescription increased 47% compared with a 45% reduction among youth age ≤19 years.
DISCUSSION
This study demonstrates that buprenorphine dispensing is low and declining in recent years among youth in the United States. Only 336 000 total prescriptions were dispensed to 22 000 youth age ≤19 years over the study period. However, an estimated 87 000 adolescents age 12 to 17 years and 227 000 young adults age 18 to 25 have OUD.7 These statistics likely under-estimate the national prevalence of OUD in both adolescents and young adults.19 With an average of only 4169 youth receiving buprenorphine annually, a relatively small proportion of youth with self-reported OUD are receiving buprenorphine from a retail pharmacy. Together these findings suggest that many youth with OUD who could benefit from MOUD are not receiving it. Most of these youth were not dispensed medication in more than 1 year during the study period, indicating poor retention in treatment, consistent with previous studies.10 Prescribing to youth was particularly low when compared with adults age ≥20 years. In 2020, the proportion of adults with dispensed buprenorphine was 128 times greater than youth aged ≤19 years and 17 times greater than youth aged 18 to 19 years. In addition, in contrast to the 45% decline in number of youth dispensed buprenorphine over the 6-year study period, the number of adults dispensed buprenorphine increased 47%.
Underutilization of buprenorphine in adolescent OUD treatment has been described previously, and our findings are consistent with these studies.5,10,14,20 Although underutilized, prior studies have shown a modest increase in MOUD provision to youth from 2000 to 2014.5 This more recent decline in buprenorphine dispensing is surprising, as is the relatively abrupt drop in 2018. The reason for this uneven decline is unclear and warrants further study. However, the very low dispensing rate is consistent with a recent study from the 2019 National Survey on Drug Use and Health that found 0 adolescents with OUD in the sample to have received MOUD within the past year.21 This decline in dispensing among youth is particularly striking in contrast to the 47% increase in dispensing observed among adults. As suggested in previous research examining buprenorphine dispensing trends, some of the specialty-specific changes are likely related to The Comprehensive Addiction and Recovery Act implemented in 2016.22 Expansion of prescribing authority to nurse practitioners and physician assistants is a contributing factor in the greater proportion of MOUD in primary care settings provided by these practitioners.23 Nurse practitioners and physician assistants can play an important role in expanding access to MOUD for youth. However, shifting prescribing patterns among specialties cannot account for the overall decline. Moreover, it cannot explain this decline at a time when buprenorphine prescribing for adults is increasing. Since 2020, multiple flexibilities for prescribing buprenorphine were introduced, including eliminating training requirements for DATA 2000 waivers to prescribe to a limited number of patients and allowing prescribing via telemedicine to expand access to MOUD for patients who might benefit. Despite these flexibilities, dispensing of buprenorphine to youth in 2020 was appreciably lower than that in 2015 to 2017. The observed decline across specialties, including pediatricians, underscores the work to be done to make MOUD more available.
Differences in prescribing by sex as well as temporal variations were also noted. Buprenorphine dispensing to young women and girls age ≤19 years declined by over 50% during the study period compared with 38% among young men and boys of the same age. The observed temporal variations in buprenorphine also could suggest uneven availability of MOUD and might reflect variation in access to pediatricians and school-based health programs before or at onset of the school year, relative to other times of the year. Dispensing might correlate with increases in OUD diagnoses during periods when youth substance use is more likely to be detected. Increasing screening for substance use disorders with referral to treatment in multiple settings could ensure youth have more consistent access to MOUD services when it is needed. Implementation of universal screening, brief intervention, and referral to treatment protocols in all pediatric primary care settings could boost overall substance use disorder diagnosis and ensure greater equity in access to appropriate treatment.24
Although not the primary focus of this analysis, a small but notable proportion of buprenorphine dispensed to youth aged ≤19 years was dispensed to children aged ≤5 years. There are no widely recognized indications for the use of buprenorphine in young children in outpatient settings and many of these prescriptions may represent idiosyncratic uses. However, buprenorphine can be used for treatment of neonatal opioid withdrawal syndrome. In one study, 20% of surveyed pediatric practitioners of 2 national clinical pharmacy associations indicated that infants with neonatal opioid withdrawal syndrome could be discharged from the hospital with pharmacotherapy; it is possible that prescription for a home-based taper of buprenorphine might account for some of that dispensed to these children.25,26 Further discussion on use of buprenorphine outside the context of MOUD is beyond the scope of this paper.
This study highlights a gap in access to recommended, evidence-based treatment of opioid use disorder among youth. Differences in dispensing buprenorphine by age and sex were noted, as was variation by time of year. Multiple factors might contribute to low prescribing, including a paucity of treatment facilities for adolescents and a shortage of physicians with DATA 2000 waivers to prescribe buprenorphine who treat children.21–23 Additional factors include potential high-levels of cost sharing required,30 stigma around OUD, and access to primary care and confidential services among youth.31
To close these gaps in care, MOUD treatment of adolescents could be made more readily available in primary care settings. One reason for lower dispensing to younger youth could be that buprenorphine and its various formulations are not approved for use in adolescents aged <16 years.32 Although off-label prescribing occurs, the lack of Food and Drug Administration approval might be a barrier to prescribing, particularly among clinicians with less experience in the management of substance use disorders. Training in managing OUD for youth-serving clinicians could be prioritized. Most children aged ≤18 years receive medical care from a pediatrician.33,34 However, in 2020, pediatricians prescribed only 1% of the buprenorphine dispensed. Treatment in pediatric clinics could be emphasized, including encouraging more general pediatricians to obtain DATA waivers. Prescriptions from addiction medicine specialists and emergency physicians were also low. One reason for the relatively few prescriptions originating from addiction medicine specialists is the scarcity of these clinicians overall, particularly those who care for adolescents.27 Training more clinicians in addiction medicine and adolescent psychiatry could be important in expanding access to MOUD for adolescents, particularly for individuals with complex histories and comorbid psychiatric disorders. Encouraging MOUD initiation in the emergency department following overdose events is also an important strategy for expanding MOUD access and linking these patients to care.35
There are also opportunities for public health practitioners to enhance access to MOUD for adolescents in the community. Innovative overdose surveillance, including linking emergency medical services and emergency medicine data on nonfatal overdoses with geographic data and MOUD prescriber locations could be used to identify “hot spots” for adolescent overdoses and to identify gaps in treatment availability. Public health programs to link youth experiencing homelessness or housing instability to care could also enhance access to MOUD for many youth with OUD. Strengthening recovery-oriented systems for adolescents in the community can facilitate referrals to behavioral health services and community and family outreach following nonfatal overdoses.36 Through enhanced surveillance and strengthening systems, communities can leverage their local data to ensure that children in need of services are identified early and available resources match local needs. Finally, examination of existing payor policies around cost-sharing might facilitate greater access to buprenorphine.37
LIMITATIONS
This study was subject to several limitations. Diagnoses are not associated with prescriptions in our dataset; thus, we were unable to determine the proportion of patients with OUD that were dispensed buprenorphine. We excluded buprenorphine formulations used for pain and assumed that all dispensed buprenorphine included in this study was for treatment of OUD. However, pain control may account for a limited portion of these prescriptions. This analysis relies on dispensing data, rather than prescribing data. Prescriptions not filled would not be reflected, resulting in lower rates than actually prescribed. Data on prescriptions filled outside of retail pharmacies, such as through mail order, the Indian Health System, Veterans Affairs, opioid treatment programs, or large health systems are not included in this data and are therefore not generalizable to populations served by such systems. In addition, medications administered directly in the office or emergency department are not reflected in this analysis. Finally, data from 2021 was not available at the time of analysis to further evaluate the effects of the coronavirus disease 2019 pandemic on buprenorphine dispensing. Data from 2020 do not appear to show any appreciable pandemic related effects. However, future analyses could further evaluate specific effects of the pandemic and pandemic related changes in buprenorphine prescribing requirements on dispensing to youth.
CONCLUSIONS
Despite increases in overdoses involving opioids in adolescents and young adults, barriers to widespread treatment with MOUD for youth with OUD remain and buprenorphine prescribing is low. Increased access to MOUD among adolescents and youth is an important strategy in addressing OUD among this population. Understanding barriers contributing to low prescribing rates by clinicians who treat youth can inform public health efforts to increase availability of MOUD in pediatric primary care settings as well as to improve linkage to care following OUD diagnosis and overdose events.
WHAT’S KNOWN ON THIS SUBJECT:
Prescription opioid misuse in adolescents and young adults is prevalent and opioid-involved overdose deaths in these populations are rising. Opioid agonists such as buprenorphine can reduce the risk of overdose death, but they are underutilized.
WHAT THIS STUDY ADDS:
This study updates the latest trends in dispensing buprenorphine to youth as well as provides insight into who is prescribing to youth. Understanding dispensing patterns can inform interventions to expand access to medications for opioid use disorder for adolescents.
ABBREVIATIONS
- IMF
illicitly-manufactured fentanyl
- OUD
opioid use disorder
- MOUD
medications for opioid use disorder
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
CONFLICT OF INTEREST DISCLOSURES: The authors have indicated they have no conflicts of interest relevant to this article to disclose.
REFERENCES
- 1.Ahmad FBRL, Sutton P. Provisional Drug Overdose Death Counts. Hyattsville, MD: National Center for Health Statistics; 2022 [Google Scholar]
- 2.O’Donnell J, Tanz LJ, Gladden RM, Davis NL, Bitting J. Trends in and characteristics of drug overdose deaths involving illicitly manufactured fentanyls — United States, 2019–2020. MMWR Morb Mortal Wkly Rep. 2021;70(50):1740–1746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedman J, Akre S. COVID-19 and the drug overdose crisis: uncovering the deadliest months in the United States, January–July 2020. Am J Public Health. 2021;111(7):1284–1291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frank D, Mateu-Gelabert P, Guarino H, et al. High risk and little knowledge: overdose experiences and knowledge among young adult nonmedical prescription opioid users. Int J Drug Policy. 2015;26(1):84–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hadland SE, Wharam JF, Schuster MA, Zhang F, Samet JH, Larochelle MR. Trends in receipt of buprenorphine and naltrexone for opioid use disorder among adolescents and young adults, 2001–2014. JAMA Pediatr. 2017;171(8): 747–755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Monitoring the Future. 1975–2021 data for in-school surveys of 8th, 10th, and 12th grade students. Available at: http://monitoringthefuture.org/data/21data.htm. Accessed August 31, 2022
- 7.Substance Abuse and Mental Health Administration. NSDUH detailed tabs 2019. [August 6, 2021]. Available at: https://www.samhsa.gov/data/sites/default/files/reports/rpt29394/NSDUHDetailedTabs2019/NSDUHDetTabsSect5pe2019.htm. Accessed.
- 8.Jones CM, Clayton HB, Deputy NP, et al. Prescription opioid misuse and use of alcohol and other substances among high school students - Youth Risk Behavior Survey, United States, 2019. MMWR Suppl. 2020;69(1):38–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) national practice guideline for the use of medications in the treatment of addiction involving opioid use. J Addict Med. 2015;9(5):358–367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hadland SE, Bagley SM, Rodean J, et al. Receipt of timely addiction treatment and association of early medication treatment with retention in care among youths with opioid use disorder. JAMA Pediatr. 2018;172(11):1029–1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Committee on Substance Use and Prevention. Medication-assisted treatment of adolescents with opioid use disorders. Pediatrics. 2016;138(3): e20161893. [DOI] [PubMed] [Google Scholar]
- 12.Society for Adolescent Health and Medicine. Medication for adolescents and young adults with opioid use disorder. J Adolesc Health. 2021;68(3):632–636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Society for Addiction Medicine. The ASAM national practice guideline for the treatment of opioid use disorder: 2020 focused update. J Addict Med. 2020;14(2S Suppl 1):1–91 [DOI] [PubMed] [Google Scholar]
- 14.Alinsky RH, Zima BT, Rodean J, et al. Receipt of addiction treatment after opioid overdose among Medicaid-enrolled adolescents and young adults. JAMA Pediatr. 2020;174(3): e195183–e195183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014;(2):CD002207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Borodovsky JT, Levy S, Fishman M, Marsch LA. Buprenorphine treatment for adolescents and young adults with opioid use disorders: a narrative review. J Addict Med. 2018;12(3): 170–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marsch LA, Moore SK, Borodovsky JT, et al. A randomized controlled trial of buprenorphine taper duration among opioid-dependent adolescents and young adults. Addiction. 2016;111(8): 1406–1415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.US Census Bureau. 2019. population estimates by age, sex, race and Hispanic origin. Available at: https://www.census.gov/newsroom/press-kits/2020/population-estimates-detailed.html. Accessed October 4, 2021
- 19.Keyes KM, Rutherford C, Hamilton A, et al. What is the prevalence of and trend in opioid use disorder in the United States from 2010 to 2019? Using multiplier approaches to estimate prevalence for an unknown population size. Drug Alcohol Depend Rep. 2022;3: 100052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feder KA, Krawczyk N, Saloner B. Medication-assisted treatment for adolescents in specialty treatment for opioid use disorder. J Adolesc Health. 2017;60(6):747–750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mauro PM, Gutkind S, Annunziato EM, Samples H. Use of medication for opioid use disorder among US adolescents and adults with need for opioid treatment, 2019. JAMA Netw Open. 2022; 5(3):e223821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roehler DR, Guy GP, Jones CM. Buprenorphine prescription dispensing rates and characteristics following federal changes in prescribing policy, 2017–2018: a cross-sectional study. Drug Alcohol Depend. 2020;213:108083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barnett ML, Lee D, Frank RG. In rural areas, buprenorphine waiver adoption since 2017 driven by nurse practitioners and physician assistants. Health Aff (Millwood). 2019;38(12):2048–2056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levy SJ, Williams JF; Committee on Substance Use and Prevention. Substance use screening, brief intervention, and referral to treatment. Pediatrics. 2016; 138(1):e20161211. [DOI] [PubMed] [Google Scholar]
- 25.Kraft WK, Adeniyi-Jones SC, Chervoneva I, et al. Buprenorphine for the treatment of the neonatal abstinence syndrome. N Engl J Med. 2017;376(24): 2341–2348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Byerley EM, Mohamed MW, Grindeland CJ, Muzzy Williamson JD. Neonatal abstinence syndrome practices in the United States. J Pediatr Pharmacol Ther. 2021;26(6):577–583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alinsky RH, Hadland SE, Matson PA, Cerda M, Saloner B. Adolescent-serving addiction treatment facilities in the United States and the availability of medications for opioid use disorder. J Adolesc Health. 2020;67(4):542–549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mericle AA, Arria AM, Meyers K, Cacciola J, Winters KC, Kirby K. National trends in adolescent substance use disorders and treatment availability: 2003–2010. J Child Adolesc Subst Abuse. 2015;24(5):255–263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Foti K, Heyward J, Tajanlangit M, et al. Primary care physicians’ preparedness to treat opioid use disorder in the United States: a cross-sectional survey. Drug Alcohol Depend. 2021;225:108811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saloner B, Feder KA, Krawczyk N. Closing the medication-assisted treatment gap for youth with opioid use disorder. JAMA Pediatr. 2017;171(8):729–731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Adams ZW, Taylor BG, Flanagan E, et al. Opioid use disorder stigma, discrimination, and policy attitudes in a national sample of U.S. young adults. J Adolesc Health. 2021;69(2):321–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Food US and Administration Drug. Subutex and suboxone drug approval package. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/022410Orig1s000TOC.cfm. Accessed July 1, 2022
- 33.Phillips RL Jr, Bazemore AW, Dodoo MS, Shipman SA, Green LA. Family physicians in the child health care workforce: opportunities for collaboration in improving the health of children. Pediatrics. 2006;118(3):1200–1206 [DOI] [PubMed] [Google Scholar]
- 34.Wasserman RC, Varni SE, Hollander MC, Harder VS. Change in site of children’s primary care: a longitudinal population-based analysis. Ann Fam Med. 2019;17(5): 390–395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Robinson CA, Wilson JD. Management of opioid misuse and opioid use disorders among youth. Pediatrics. 2020;145(Suppl 2): S153–S164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sheedy CK, Whitter M. Guiding principles and elements of recovery-oriented systems of care: what do we know from the research? J Drug Addict Educ Erad. 2013;9(4):225 [Google Scholar]
- 37.Reif S, Creedon TB, Horgan CM, Stewart MT, Garnick DW. Commercial health plan coverage of selected treatments for opioid use disorders from 2003 to 2014. J Psychoactive Drugs. 2017;49(2): 102–110 [DOI] [PMC free article] [PubMed] [Google Scholar]


