Abstract
Health disparities by socioeconomic status (SES) have been extensively documented, but less is known about the physical health implications of achieving upward mobility. This article critically reviews the evolving literature in this area, concluding that upward mobility is associated with a trade-off, whereby economic success and positive mental health in adulthood can come at the expense of physical health, a pattern termed skin-deep resilience. We consider explanations for this phenomenon, including prolonged high striving, competing demands between the environments upwardly mobile individuals seek to enter and their environments of origin, cultural mismatches between adaptive strategies from their childhood environments and those that are valued in higher-SES environments, and the sense of alienation, lack of belonging, and discrimination that upwardly mobile individuals face as they move into spaces set up by and for high-SES groups. These stressors are hypothesized to lead to unhealthy behaviors and a dysregulation of biological systems, with implications for cardiometabolic health.
Keywords: upward mobility, socioeconomic status, biological processes, health behaviors, cardiovascular health
INTRODUCTION
The American dream promises that any child, regardless of their family or origin, can ascend the socioeconomic ladder and enjoy the benefits of high status. For upwardly mobile individuals, those benefits include material wealth, prestige, power, and well-being. But what about physical health?
One might assume that the answer to this question is simple. There is an extensive literature documenting health disparities by socioeconomic status (SES). Individuals of lower SES are at increased risk for chronic diseases, functional disability, and premature mortality (Adler & Stewart 2010, Braveman et al. 2010, Williams et al. 2010). These disparities are evident from early childhood through older adulthood (Adler & Stewart 2010, Schreier & Chen 2013).
Given this backdrop, one might assume that upward mobility is beneficial for physical health. But as it turns out, surprisingly little is known about the health of individuals who live the American dream and achieve SES that is higher than the status of their family of origin. Moreover, evidence has accrued in recent years to suggest that upward mobility may even impose costs to physical health, particularly for Americans of color.
The goal of this article is to take stock of what is known about the health consequences of upward mobility. We focus on intergenerational mobility, whereby individuals transition from lower (childhood) SES to higher (adulthood) SES. We first review the empirical evidence regarding the links between upward mobility and physical health. Finding an association, we then consider mechanisms that might explain it, providing a theoretical overview of the unique psychological experiences of upwardly mobile individuals and the resulting pathways to health.
UPWARD MOBILITY AND PHYSICAL HEALTH: EMPIRICAL EVIDENCE
Different theoretical accounts exist about expected effects of social mobility on health (Kuh & Ben Shlomo 2004). One theory is that it is possible to mitigate or reverse the effects of early economic hardship, and that therefore those who achieve upward mobility will have better health than those who remain low in SES. This is because achieving higher SES will allow individuals access to better health care and greater opportunities for healthier lifestyles (Pudrovska & Anikputa 2013, Savelieva et al. 2017). A second, though not inconsistent, theory is that the health of those who achieve upward mobility will be somewhere in between the health of those who stay persistently low in SES and that of those who have consistently high SES (Hogberg et al. 2012, Pollitt et al. 2005). Finally, a third theory is that achieving upward mobility is associated with worse health compared to having a stable SES, because the experience of upward mobility causes stress and disruption of social connections, both of which have detrimental effects on health (Hogberg et al. 2012, Prag & Richards 2019).
Empirical Studies on Upward Mobility and Physical Health
Below we review empirical studies that have examined the association between upward mobility and physical health. Given that a review paper on this topic was published in 2005 (Pollitt et al. 2005), we first summarize its conclusions and then focus on studies published since. The 2005 review addressed life-course SES and cardiovascular outcomes and found mixed evidence for social mobility hypotheses. A number of studies included in the review found that cardiovascular health for the upward mobility group was in between, and not significantly different from, the health of the persistently low- and persistently high-SES groups. There were a roughly equivalent number of studies, however, that found some differences between the upwardly mobile group and one of the stable-SES groups.
Below we focus on post-2005 articles that contained both measures of childhood and adult SES and evaluated change across these two periods. We focus on studies with objective health outcomes—usually, physician diagnoses of disease or biomarkers. We searched for articles containing specific terms, including life-course socioeconomic, socioeconomic trajectory, childhood socioeconomic, socioeconomic change, health, mortality, cardiovascular, and biological. We reviewed the abstracts of the articles returned from these searches that were published between 2006 and February 2020. Articles were excluded if they did not contain at least one childhood SES measurement point and at least one adult SES measurement point; if the outcomes did not include objective health data (e.g., focused instead on self-reported health or quality of life); and if studies were published outside the United States or Western Europe (to avoid mixing effects from developing countries or countries with potentially large cultural differences from the United States and Europe). The majority of articles divided participants into groups based on childhood versus adult SES (low-low, low-high, high-low, high-high), and hence we summarize comparisons specifically between the low-high group and the others.
Of studies that observed differences in the upwardly mobile group, three focused on low-grade inflammation, a process that contributes to multiple health problems, including diabetes, heart disease, and stroke. These studies found that participants with upward mobility (low-high group) had higher levels of inflammation on at least some markers compared to those who had high SES in childhood and adulthood (high-high) (Castagne et al. 2016, Loucks et al. 2010, Na-Ek & Demakakos 2017). Three other studies found that the low-high group had significantly greater risk of experiencing cardiovascular disease or events than the high-high group (Kittleson et al. 2006, Tiikkaja & Hemstrom 2008, Tiikkaja et al. 2009). Finally, one study found that Black women from the low-high group had a higher risk of type 2 diabetes than those in the high-high group (Beckles et al. 2019).
Of studies that made comparisons with a low-low group, two focused on hypertension. One observed that upward mobility was associated with a lower risk of hypertension compared to a stable low-SES group, whereas the other reported a higher risk (Glover et al. 2020b, Hogberg et al. 2012). One study of obesity did not report statistical comparisons, but the figures depicted similar obesity rates for the low-high group and the low-low group, and higher rates compared to the high-high group (Heraclides & Brunner 2010).
One study of mortality reported a statistically significant difference across the four groups but no specific group comparisons. Based on the figure, the low-high group appeared to fall in between the high-high and low-low groups in risk for mortality (Pudrovska & Anikputa 2013). Finally, one study found that those with upward mobility had more ideal cardiovascular health than those who were stable in SES across childhood and adulthood (however, stable high and stable low participants were combined into one group, complicating interpretations) (Savelieva et al. 2017).
Of studies that observed null findings, two found no differences between the low-high and the high-high group in terms of mortality (Melchior et al. 2006, Stringhini et al. 2018), and three found no differences in terms of type 2 diabetes incidence (Lidfeldt et al. 2007, Smith et al. 2011, Stringhini et al. 2013). One study reported a 55% higher odds of obesity for the low-high than for the high-high group; however, this was not significant because the low-high group sample size was very small (James et al. 2006). One study focused on allostatic load, an aggregate of biomarkers associated with disease risk. Here the upward mobility group had allostatic load levels in between those of the stable low and stable high groups (with no additional effects of mobility on allostatic load after controlling for childhood and adult SES) (Prag & Richards 2019). Another study compared the upward mobility group to a stable low group and found no differences (after including demographic covariates) in the likelihood of having a high-risk health trajectory (defined as a physician diagnosis of chronic illness across multiple years) (Wilson & Shuey 2016).
All the studies reviewed above used observational designs, which makes causality difficult to infer, as there could be selection effects, such that earlier health predisposes individuals to a certain socioeconomic attainment in adulthood, or residual confounding, such that third variables (e.g., genetic factors) predispose individuals to both certain health outcomes and a certain socioeconomic attainment in adulthood. Experimental manipulations would provide stronger evidence but are challenging to implement with respect to SES. One study used a natural experiment and evaluated the health impact of an increase in required years of schooling. The researchers compared the adult health of individuals born right after the institution of a national education reform (which increased the minimum school leaving age in France from 14 to 16 years) with those who had just missed the cutoff. They found that blood pressure was higher in those born after, relative to before, the schooling mandate went into effect. This pattern was observed for individuals who came from low social class backgrounds. Among those from high social class backgrounds, the additional required years of schooling had no impact on blood pressure. These results suggested that upward mobility—or at least increasing one’s educational attainment—increased blood pressure in later adulthood for those who grew up low in SES (Courtin et al. 2019).
Summary
Taken together, these more recent studies lead to several conclusions. First, the health of upwardly mobile individuals tended to be worse than that of their counterparts who had consistently high SES. This pattern was evident for multiple biomarkers and for cardiovascular outcomes, though not for mortality. However, it is possible that longer follow-ups into older age are needed for mortality differences to be seen. Where there were mixed findings—e.g., in studies of diabetes—associations between upward mobility and worse health tended to be present in populations of color. These results suggest that not all currently high-SES individuals are the same, and that the process of achieving upward mobility may have some negative implications for adult health.
A second conclusion is that the health of those who are upwardly mobile is sometimes better than, but sometimes equivalent to, the health of those who are consistently low in SES. This pattern might suggest that moving up in SES has relatively weak effects on health, given that individuals who achieve high SES in adulthood do not always appear markedly different from their counterparts who remain low in SES throughout their lives.
Upward Mobility and Health: Patterns in the United States
One limitation of the studies reviewed above, at least for understanding health disparities in the United States, is that many of them did not address the overlap between SES and race/ethnicity because they were conducted in Europe. In the United States, SES patterns vary by race/ethnicity, such that Black and Latinx individuals have 2–3 times the poverty level of Whites, as well as lower college graduation rates and lower earnings and wealth (Williams et al. 2010, 2016). A second limitation is that many European studies utilize occupational class to measure SES. In the United States, SES and mobility may be better represented by markers such as income and wealth. A final issue is that physical and mental health are seldom considered in the same study; instead, they are the focus of distinct literatures.
Our group has addressed these issues across three studies. These studies have consistently observed that upward mobility has divergent associations with mental and physical health, particularly among individuals of color, a phenomenon we have termed skin-deep resilience. For instance, in a longitudinal study of Black youth, neighborhood poverty was characterized in adolescence. Youths were followed over time to determine who attended college. In young adulthood, we measured allostatic load (a multisystem indicator of health risk, including blood pressure, obesity, and stress hormones) and mental health (substance use, specifically tobacco, alcohol, and drug use). Among youths from high-poverty neighborhoods, those who made it to college showed lower levels of substance use, but at the same time higher levels of allostatic load, compared both to youths from high-poverty neighborhoods who did not make it to college and to youths from low-poverty neighborhoods who were in college (Chen et al. 2015).
A national longitudinal study of US youth assessed SES during adolescence in terms of household and neighborhood education, income, and employment. Youths were followed over time and assessed on college attendance. In young adulthood, measures of metabolic syndrome (a cluster of conditions including high blood pressure, obesity, and high glucose levels that increases risk for heart disease and diabetes) and mental health (depression) were obtained. Young adults who grew up low in SES but finished college had lower levels of depression, but a higher likelihood of metabolic syndrome, compared to young adults who grew up low in SES but did not go to college and to young adults from high-SES backgrounds who finished college. These patterns were evident among Black and Latinx participants but not Whites (Gaydosh et al. 2018).
A third study investigated the effects of upward mobility in two US national longitudinal samples. SES was largely defined by income. In adulthood, physical health (metabolic syndrome) and mental health (depression, perceived stress) were measured. The upwardly mobile group had better mental health profiles compared to the persistently low-SES group, and sometimes comparable to those of the persistently high-SES group. For example, the low-high group was less likely to have significant depression than the low-low group, and it was not different in depression from the high-high group across both samples. In contrast, in terms of physical health, the upwardly mobile group was more similar to the low-low group. That is, the low-high group had rates of metabolic syndrome that were significantly higher than those of the high-high group and not statistically different from those of the low-low group across both samples. In addition, a “trade-off” score was created, defined as the absence of significant depression plus the presence of metabolic syndrome within one person. The upwardly mobile group was significantly more likely to display this trade-off pattern compared to both the persistently high- and the persistently low-SES groups across both samples (Miller et al. 2020).
Summary
The results of these studies suggest that upward mobility is associated with a trade-off, whereby economic success and good mental health come at the expense of physical health. We refer to this pattern as skin-deep resilience because it suggests that above the skin, upwardly mobile youths appear to be doing well and achieving success by many external metrics (e.g., going to college, earning good incomes, having positive mental health). However, below the skin, they appear to be struggling physiologically in terms of their physical health, thus displaying resilience that is only skin-deep.
It is important to be cautious in interpreting these results. Because of their observational designs and the lack of childhood health measures, they do not allow us to infer causality. It is possible that early childhood health, or other genetic or environmental factors (e.g., genes or exposures that influence both health and one’s likelihood of upward mobility), drove the findings. The natural experiment of schooling in France described above (Courtin et al. 2019) suggests that a causal interpretation is plausible. From a replicability standpoint, the fact that the trade-off study replicated the same pattern of findings across two different national samples is encouraging. Finally, there is also evidence supporting a causal interpretation from a recent monozygotic twin study of low-grade inflammation. The study found that after accounting for potential genetic and environmental confounds, skin-deep resilience patterns were still evident (Chen et al. 2020). In addition, alternative explanations, while certainly possible, are somewhat difficult to envision, because they would have to involve a confounding variable that leads to upward mobility at the same time that it leads to poor adult health.
SES AND RACE/ETHNICITY
One question that arises in reviewing this literature is who experiences the health costs of mobility: Is it any low-SES individual who has ascended the socioeconomic ladder? What about individuals who are members of underrepresented, marginalized racial/ethnic groups, who in the United States share many experiences with low-SES individuals? Extensive research has documented that those from underrepresented racial/ethnic groups (particularly Blacks) are at greater risk of infant mortality, cardiovascular diseases, respiratory diseases, and all-cause mortality (Williams et al. 2010, 2016). Both SES and race/ethnicity are important determinants of health: Racial/ethnic disparities in health exist at all levels of SES, and SES disparities in health are observed within racial/ethnic groups (Williams et al. 2010, 2016). Therefore, are the costs of upward mobility most apparent at the intersection of identities related to both race and class?
Indeed, to date, mobility costs have been most frequently demonstrated among low-SES individuals of color (Brody et al. 2013, Chen et al. 2019, Gaydosh et al. 2018, Miller et al. 2016a). However, some recent studies have observed health costs across all upwardly mobile individuals, regardless of race/ethnicity (Chen et al. 2020, Miller et al. 2020). We also note that the COVID-19 pandemic has highlighted the increased risk of infection among populations of color in the United States. Though no research has been conducted linking COVID-19 outcomes to skindeep resilience, previous research has demonstrated the skin-deep resilience phenomenon with respect to the risk of upper respiratory infection after exposure to a rhinovirus among low-SES African Americans (Miller et al. 2016a), suggesting that the pandemic might further highlight disparities related to skin-deep resilience.
Throughout this review, we focus primarily on findings related to low SES, given our central interest in upward mobility. However, where data exist, we present evidence that addresses the intersectionality of race/ethnicity and SES. In some cases, we also refer to literature on race/ethnicity mechanisms when we believe it is germane to the discussion of upward mobility.
PSYCHOLOGICAL MECHANISMS EXPLAINING HEALTH DISPARITIES
The question that arises from these findings—assuming they are causal—is how and why upward mobility could have negative health effects. To provide background for this discussion, we begin this section with a brief overview of psychosocial mechanisms that have been proposed to explain the SES and physical health gradient (see Figure 1 for a graphical depiction).
Figure 1.
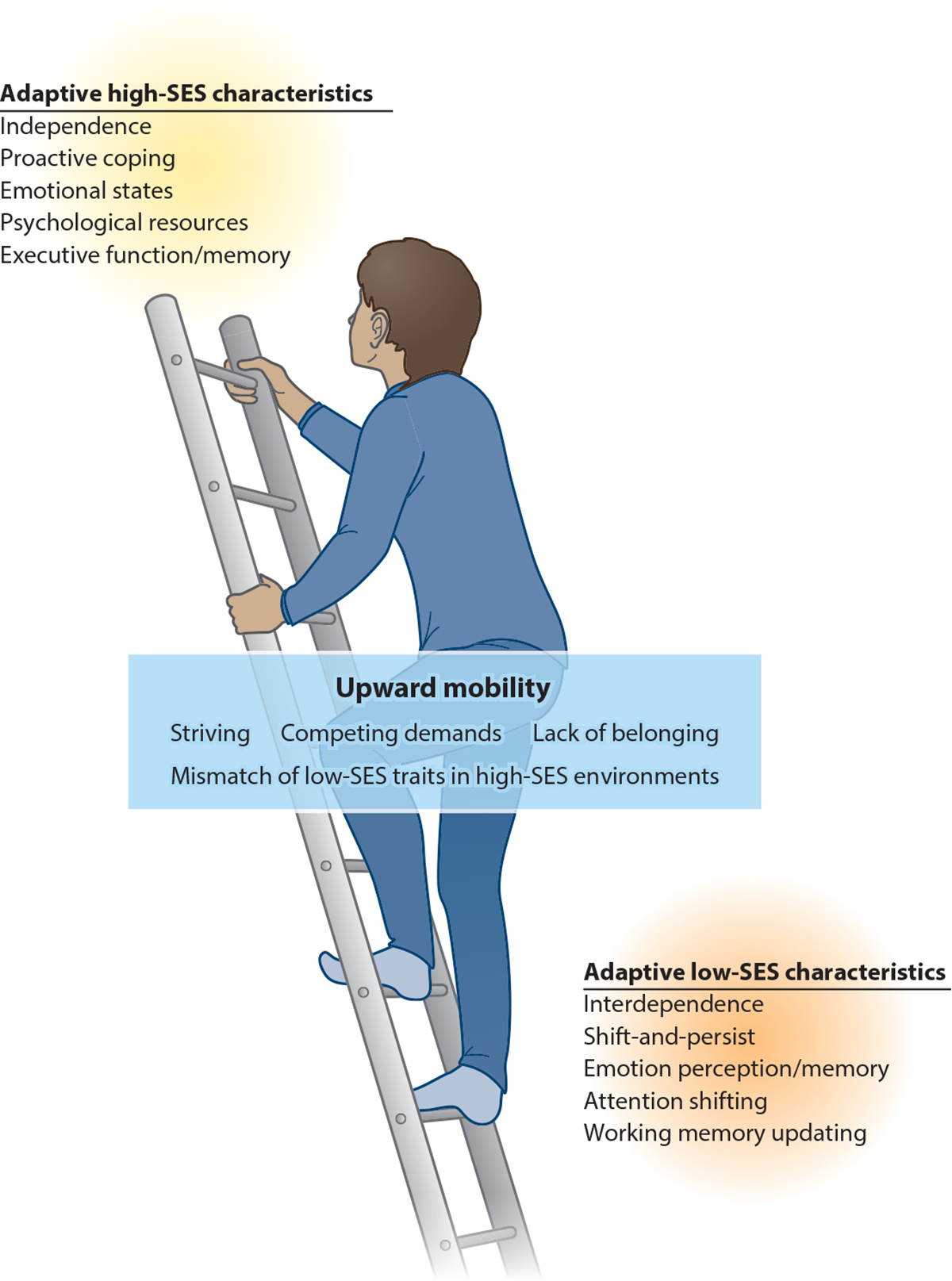
Model depicting psychological mediators associated with both low SES and high SES that explain SES disparities in physical health. The upwardly mobile group is depicted in between the low- and high-SES groups, experiencing pulls toward each. The upwardly mobile group is hypothesized to have its own set of unique psychological experiences that have implications for physical health. Abbreviation: SES, socioeconomic status.
It is important to acknowledge that low- and high-SES individuals experience vastly different contexts and structural conditions that shape their day-to-day lives and contribute to health disparities. There are differential exposures in terms of physical environmental conditions (e.g., pollution, housing conditions) (Diez Roux & Mair 2010, Hajat et al. 2015), access to resources (e.g., high-quality health care, healthy food options) (Diez Roux & Mair 2010, Smedley et al. 2003), and social environment conditions (e.g., exposure to violence) (Wright & Steinbach 2001) in low- and high-SES environments that play an important role in shaping how health outcomes can diverge between these two groups (Schreier & Chen 2013).
Characteristics of High-SES Individuals
Many of the above structural conditions also play a role in shaping psychological experiences within an individual that are thought to be important contributors to health disparities (Adler & Snibbe 2003). For example, one commonly discussed pathway is that high-SES individuals might experience better mental health—that is, fewer negative mood states such as depression, anger, and anxiety (Gallo & Matthews 2003). In turn, a large literature has linked these negative emotions to cardiovascular disease, all-cause mortality, and other health outcomes (see Everson-Rose & Lewis 2005, Gallo & Matthews 2003 for reviews).
A second commonly discussed pathway is that high-SES individuals could possess more psychological resources—higher mastery or self-esteem, perceived control, and optimism—that help protect them from adverse health outcomes (Finkelstein et al. 2007, Matthews & Gallo 2011). Evidence that psychological resources act as a mediator of the relationship between SES and health appears to be relatively strong (Matthews et al. 2010).
In addition, some researchers have posited that high-SES individuals are more likely to engage in proactive coping behaviors—that is, actions that prevent stressors or diminish their impact (Aspinwall & Taylor 1997)—and that proactive coping promotes better health behaviors and health (Aspinwall 2011, Finkelstein et al. 2007). In terms of cognition, an emerging literature suggests that there are robust differences by SES in executive functioning and working memory (Farah 2017), which could have implications for future health behaviors and health.
Overlaying these differences is the idea that cultural contexts can help explain differences in thoughts, emotions, and behaviors between groups (Markus et al. 2004). In US society, high-SES individuals are thought to value independence and a focus on the self (Markus et al. 2004). These values may explain why perceived control and proactive coping increase in tandem with SES. Furthermore, emerging data suggest that among higher-SES individuals, holding beliefs related to independence is associated with lower allostatic load (Levine et al. 2016), though more work is needed to substantiate this finding.
In sum, higher-SES individuals in the United States exhibit a constellation of characteristics revolving around autonomy and independence. These include psychological resources, such as mastery, control, and optimism, as well as proactive coping tendencies. These characteristics are thought to underlie the SES variations in negative mood (depression, anxiety, anger), executive function, and working memory, which in turn relate to health behaviors and disease outcomes.
Characteristics Engendered by Low-SES Environments
Because low-SES individuals are at risk for a number of poor health outcomes, mechanistic explanations have often been framed in terms of the deficits or negative characteristics that low-SES individuals might possess. However, more nuanced perspectives are emerging, which emphasize that the characteristics more often found among low-SES individuals can be viewed as adaptive within their contexts (Ellis et al. 2017, Frankenhuis & Nettle 2020) (see Figure 1).
In terms of cognition, research indicates that low-SES individuals are better at certain types of attention and memory tasks. Low-SES individuals are more adept at attending to cues of threat, which presumably has adaptive value in the environments in which they live (Frankenhuis & de Weerth 2013, Frankenhuis & Nettle 2020). Additionally, individuals who grow up in chaotic households are cognitively more efficient at shifting between tasks during laboratory conditions of uncertainty, compared to those who grew up in stable households (Mittal et al. 2015). The ability to shift between goals and strategies may be particularly adaptive within frequently changing low-SES environments. Furthermore, low-SES individuals are also better at updating working memory (i.e., changing and updating what they remember in the face of changing information), particularly during laboratory conditions of uncertainty (Young et al. 2018). Again, it would appear to be particularly advantageous to track and rapidly update information about one’s environment when that environment is unpredictable.
One can see how these strategies would be adaptive in many aspects of the daily lives of low-SES individuals. However, these benefits may come at a cost to physical health. For example, vigilance for threat has been linked to increases in cardiovascular reactivity during laboratory stressors (Smith et al. 2000). Threat vigilance also statistically mediates associations between low SES and acute stressor cardiovascular reactivity and the expression of genes that regulate inflammatory processes (Chen et al. 2004, 2009).
Emotionally, low-SES individuals are better at recognizing negative emotions and have better memories for negatively valenced emotional information (Frankenhuis & de Weerth 2013, Pollak & Kistler 2002). Low-SES individuals are also better at reading others’ emotions and have greater empathic accuracy than high-SES individuals (Kraus et al. 2012). Being able to perceive and remember emotion-relevant information may be adaptive for responding quickly to situations that could involve potential danger.
Despite their adaptive value in low-SES contexts, these traits may nonetheless entail a health cost. Recognizing negative emotions in faces elicits greater autonomic reactivity than perceiving threats in other sources (e.g., pictures of snakes) (Hariri et al. 2002). In addition, high levels of empathy have been associated with more low-grade inflammation in healthy individuals (Manczak et al. 2016).
When managing life stressors, low-SES individuals are also more likely to use disengagement coping strategies (e.g., distraction, denial) and less likely to use active coping strategies (e.g., problem solving) (Finkelstein et al. 2007).In terms of health, problem-focused coping is associated with better outcomes, whereas avoidance-type strategies are associated with poorer outcomes (Penley et al. 2002).
However, research indicates that there is a set of coping strategies that can be beneficial to health among lower-SES individuals. These strategies have been termed shift-and-persist, and they refer to the combination of adjusting the self to stressors by changing one’s thoughts and feelings (shifting) and taking a broader outlook on life that entails finding meaning and maintaining optimism (persisting) (Chen & Miller 2012). Among low-SES individuals, those who shift-and-persist have better health, as reflected in less obesity and better asthma outcomes (Chen et al. 2011, Kallem et al. 2013). Furthermore, high-SES individuals who shift-and-persist do not show health benefits.
These patterns can also be understood through a cultural lens (Markus et al. 2004). Lower-SES individuals in the United States value interdependence and social connections with others (Markus et al. 2004). This may explain why they are more attuned to the thoughts and feelings of others and more likely to value adjusting themselves in interpersonal situations. Moreover, among lower-SES individuals, holding beliefs related to interdependence is associated with lower allostatic load (Levine et al. 2016).
In sum, lower-SES individuals possess characteristics related to interdependence and a focus on their external environments. These include attending to and remembering the emotions of others and the details of changing circumstances as well as adjusting to situational demands. These characteristics have adaptive value in the contexts in which low-SES individuals live, but they may also have negative implications for health behaviors and health profiles.
THE PSYCHOLOGICAL EXPERIENCES OF UPWARD MOBILITY: A THEORETICAL ACCOUNT
What are the psychological experiences of someone pursuing upward mobility? We theorize that upward mobility involves simultaneous pulls toward the higher-SES environments that one is seeking to enter and pushes back toward one’s family/neighborhood environment of origin. Figure 1 depicts key factors that we propose characterize the upwardly mobile, with a focus on defining qualities (striving for success), environmental demands, and environmental fit (mismatch of traits and lack of belonging).
Striving
Youths seeking upward mobility often exhibit a hard-driving work ethic that includes high levels of prolonged striving and efforts at self-control. These qualities help them achieve successes in life, but over time they can take a cumulative toll on them physically, taxing physiological systems that contribute to later health problems (Brody et al. 2013). In particular in resource-poor environments that have insufficient supports, low-SES youths must put in disproportionately large amounts of effort to achieve similar academic outcomes as their more privileged counterparts. Low-SES youths may have to expend these efforts independently because their families do not have as much available time or personal experience with college to help them with schoolwork and future academic plans as high-SES caregivers do (Duncan & Murnane 2011). In addition, many schools in low-SES neighborhoods do not have the resources to provide the level of college preparation and advanced academic opportunities that higher-SES schools do, constraining students’ options for academic achievement (Duncan & Murnane 2011). More broadly, low-income youths need to mobilize self-control in order to avoid peer influences and behaviors related to crime, violence, and substance use that are more prevalent in low-SES neighborhoods (Sampson et al. 2019). Thus, to achieve success, low-SES youths may have to exhibit high levels of independent striving, with few resources and supports, and simultaneously maintain high levels of self-control to stay on track with their long-term goals. Over time, we postulate that these sustained efforts create wear and tear on youths’ physiological systems.
Empirically, the evidence for this wear-and-tear scenario emerges in statistical interactions between family SES and variables reflecting striving and self-control. These interactions show that for high-SES youths, striving is associated with better outcomes across multiple domains. In contrast, for low-SES youths, there appears to be a trade-off, with striving presaging more academic success and better well-being in tandem with worse physical health (skin-deep resilience). For example, a prospective analysis found that low-SES Black adolescents who engaged in high striving were more likely to finish college, earn higher incomes, and have less depression in young adulthood compared to low-SES Black individuals with low striving. However, these same youths were also more likely to develop diabetes by age 29 compared to their counterparts who were also low in SES but had low levels of striving. In contrast, among high-SES Black youths, striving was beneficial for both life outcomes and diabetes (Brody et al. 2016). Similarly, other prospective studies found that low-SES Black youths who showed high self-control had lower levels of internalizing and externalizing problems but higher levels of allostatic load and faster epigenetic aging of immune cells (based on DNA methylation patterns that reflect the discrepancy between a person’s biological and chronological age) compared to low-SES Black youths who had low self-control. In contrast, among high-SES Black youths, self-control was either beneficial or unrelated to mental and physical health (Brody et al. 2013, Miller et al. 2015). Similarly, in chronically ill populations, Black and Latinx youths with asthma who exhibited high self-control under stressful school conditions had better mental health (less anxiety and depression) but worse asthma inflammatory profiles compared to those who showed low self-control under stressful school conditions (Chen et al. 2019).
Studies that have investigated related constructs find similar patterns. For example, conscientiousness is a personality trait that overlaps with striving and self-control and interacts with SES in the same manner. In one study, Blacks who had low childhood SES, but were high in conscientiousness, reported more educational attainment and fewer depressive symptoms as adults (compared to those low in conscientiousness). However, after being administered an experimental virus, they were more likely to develop a verified respiratory infection. The opposite pattern was observed among Black adults with high childhood SES: Conscientiousness was protective against viral infection (Miller et al. 2016a). In another study, low-SES Black men high in conscientiousness had better psychological well-being but also higher metabolic syndrome scores than Black men who were low in SES and low in conscientiousness (Duggan et al. 2019). Furthermore, a monozygotic twin study found that conscientiousness was associated with higher educational attainment, fewer depressive symptoms, and less problematic alcohol use across all twins. However, discordance analyses revealed that among low-SES twin pairs, the one with higher conscientiousness had more low-grade inflammation [higher C-reactive protein (CRP)] in adulthood relative to their less conscientious twin. In contrast, among high-SES twins, the twin with higher conscientiousness had lower CRP levels, thus bolstering evidence for skin-deep resilience through a twin design that reduced the possibility of genetic and environmental confounds (Chen et al. 2020). In related studies, low-SES Black adults who showed high levels of high-effort coping, hard work, and a single-minded determination to succeed (i.e., John Henryism) exhibited higher blood pressure and a greater risk of hypertension compared to those with low levels of John Henryism (James et al. 1987, 1992). Lastly, we note that conceptually, constructs such as striving, self-control, and conscientiousness all overlap with the construct of grit. Grit has been studied largely in the educational domain (Duckworth 2016), with very little data linking grit to physical health outcomes (see Pena et al. 2019 for an exception). However, we would hypothesize that such studies might reveal similar skin-deep resilience patterns as observed with striving.
More generally, research points to the idea that prolonged high levels of effort/striving have physiological costs. The literature on effort-reward imbalance indicates that when people exert high levels of effort at work (including having an excessive overcommitment) and do not feel appropriately rewarded for their efforts, they experience an increased risk of cardiovascular disease, myocardial infarction, and diabetes as well as elevated levels of ambulatory blood pressure, stress hormones, and biomarkers of inflammation (see Siegrist 2010, Siegrist & Li 2016 for reviews). There is also evidence of physiological consequences of goal-striving stress (i.e., the discrepancy between one’s aspirations and one’s achievements). Higher levels of goal-striving stress predict increased risks of obesity, hypertension, and coronary heart disease (Glover et al. 2020a, Sellers et al. 2012). Goal-striving stress may be more evident in lower-SES youths, given the additional barriers and constraints they face in their academic pursuits.
Taken together, this research suggests a scenario where the high levels of sustained effort that lower-SES students exert to achieve academic successes—combined with the weaker support and fewer resources they receive relative to higher-SES students—contribute to a skin-deep resilience pattern. Skin-deep resilience fosters success throughout life but simultaneously takes a toll on physiological processes and physical health in upwardly mobile individuals.
Competing Demands
As youths are striving for upward mobility through educational efforts, they are often being pulled back toward their home environments through competing demands. For example, low-SES families often need youths to work and contribute to family finances, creating competing demands between school and work (Fuligni & Pedersen 2002). Efforts to balance school, work, and home demands may create additional pressures that many higher-SES youths do not have to face. For example, lower-SES individuals are more likely to report having multiple roles that conflict with one another (Stephens et al. 2001). Many low-SES youths have obligations around the house, such as care of younger siblings and meal preparation (Fuligni & Pedersen 2002), particularly when low-SES parents have to work multiple jobs or nontraditional shifts. Additionally, some low-SES youths may feel pressures to succeed in order to not to disappoint family members who take pride in and derive self-esteem from their accomplishments (Tesser 1988). Moreover, when success happens, these individuals may feel obligated to give back by taking care of family members and their communities of origin (Cole & Omari 2003), creating an additional layer of demands that many higher-SES individuals do not have to shoulder.
In turn, these competing demands are theorized to be detrimental to health because of the ways they drain time, energy, and resources (Martire & Stephens 2003). For example, experiencing high demands at work—such as an excessive workload and conflicting demands—combined with having low control is associated with an increased risk for cardiovascular diseases (myocardial infarction, stroke, and hypertension), as well as higher blood pressure (see Backe et al. 2012, Gilbert-Ouimet et al. 2014 for reviews). Other studies have found that related constructs, including role overload (having too many demands, for example, in one’s job), are associated with greater health problems (Shultz et al. 2010). Furthermore, both vital exhaustion (the experience of being excessively fatigued) and burnout (a chronic state of emotional exhaustion and physical fatigue) are associated with an increased risk of coronary heart disease and cardiovascular-related events (Frestad & Prescott 2017, Melamed et al. 2006).
In adolescence, one daily diary study found that adolescents who spent more time helping their family (e.g., cooking, cleaning, caring for siblings) had higher levels of low-grade inflammation (higher CRP) (Fuligni et al. 2009). Moreover, a second daily diary study demonstrated that adolescents who both experienced a high frequency of daily demands from family and who spent a lot of time (>1 hour/day) helping their family had the highest levels of low-grade inflammation and the largest proinflammatory cytokine responses to an in vitro bacterial challenge, compared to those who experienced fewer demands or provided less help (Levine et al. 2017).
Thus, while most students in high-achieving schools have to work hard for academic success, low-SES students must juggle academic demands with numerous other challenges in their lives. Work demands and family/home life demands also necessitate their attention, meaning that academic success has to be achieved while also successfully managing and balancing other life demands. This creates a greater overall burden of persistent competing demands, leading to insufficient time for leisure or restorative activities and taking a physiological toll on the health of low-SES youths.
Mismatches: Carryover of Earlier Strategies for Success
Low- and high-SES youths adopt different strategies for dealing with demands based on what is adaptive within the environments they grow up in. However, difficulties may arise if low-SES youths continue to utilize the strategies they developed in childhood once they enter higher-SES settings (e.g., high-achieving schools).
Within educational settings, the phenomenon of low-SES students using strategies that are not adaptive in their current environment has been termed cultural mismatch (Stephens et al. 2014, 2019). In such settings, higher-SES students have been described as typically exhibiting expressive independence, which includes a focus on expressing the self’s desires and goals, influencing situations, and assuming equality with others. These qualities are conveyed as valued in the school setting by reinforcing students who speak up in class, who pose questions to teachers, and who approach teachers for help (Stephens et al. 2014). Lower-SES students, in contrast, have been described as exhibiting hard interdependence, which includes a focus on adjusting to situations, being connected to others in part through an awareness of the social hierarchy, and staying tough in the face of challenges. This manifests in the form of lower-SES students being more deferential to authorities, being less likely to speak up in class or when they need help, and prioritizing following rules over asking questions (Stephens et al. 2014). These traits are not typically reinforced in higher education settings, leading lower-SES students to potentially feel disadvantaged. The implications of this cultural mismatch have been examined primarily within the educational domain, with research consistently demonstrating that cultural mismatches are associated with worse academic performance throughout the college years (Phillips et al. 2020).
However, though not yet well studied, cultural mismatch could also plausibly have implications for health. That is, the mismatch between one’s traits and one’s environment creates additional stress as students realize that the traits they learned to exhibit in their childhood environments are not as valued in their new environment and may be detrimental to their academic success in high-achieving settings. The struggles these students experience with cultural mismatches may add to the physiological toll of striving for success. For example, one study found that first-generation students showed greater cortisol increases in response to an acute stressor task consisting in giving a speech about their college goals compared to continuing-generation students, particularly when information was conveyed that emphasized typical norms expressed in college environments (e.g., encouraging students to explore personal interests and express their ideas and opinions) (Stephens et al. 2012). These findings suggest that the experience of cultural mismatch could bring about physiological changes that increase vulnerability to later-life health problems (Adam et al. 2017). Further evidence supporting the cultural mismatch hypothesis comes from another study documenting that when students of color attend schools that emphasize the value of diversity, they have lower levels of inflammation and fewer signs of metabolic syndrome compared to those who attend schools that do not explicitly acknowledge diversity values (Levine et al. 2019).
There is also evidence of the health consequences of environmental mismatch from animal studies (Bateson et al. 2014).The idea is that cues from the environment calibrate the phenotype of developing organisms to match their anticipated ecological demands. Numerous examples abound whereby different species evolve different phenotypes (e.g., fur or shell color/thickness, tendencies toward shelter-seeking behaviors, thrifty metabolic phenotype), depending on the environmental conditions in which they were born. These phenotypes are adaptive for their initial environmental conditions and persist even if environmental conditions change later in life. When later environmental conditions are different from what an organism prepared for, this mismatch can have detrimental consequences, for example, leading to being more vulnerable to predation, being less likely to reproduce, and having poor health outcomes such as obesity (Bateson et al. 2014).
In humans, there is evidence from prospective studies that mismatches between child and adult environments forecast increased risk of later-life health problems (Bateson et al. 2014). During gestation, mothers are thought to signal expected environmental conditions (e.g., nutritional scarcity) to the developing fetus. If the environment the child is raised in turns out to be different (e.g., nutritional abundance), poor health outcomes later in life, including obesity, diabetes, and cardiovascular disease, are more likely to occur (Bateson 2007), because the child’s metabolism was calibrated for nutrient scarcity. For example, those who were born during the famine known as the Dutch Hunger Winter of World War II were more likely to have impaired glucose tolerance in adulthood compared to those born right before or right after the famine period (Ravelli et al. 1998). Because nutrition improved after the famine, this is taken to be an example of how the mismatch between an earlier and a later environment can be detrimental to health.
Lack of Belonging
Cultural mismatch can also contribute to feelings of a lack of belonging in higher education settings. As low-SES youths strive for upward mobility, they may experience a lack of belonging in two ways. The first one is with their new academic environment. As they progress into high-achieving environments, low-SES youths may see fewer and fewer students who come from similar backgrounds as they do. The sense of being different from their peers in turn contributes to feeling a lack of belonging, questioning their belonging, and experiencing a stigmatized identity in these contexts (Johnson et al. 2011, Ostrove & Long 2007). For example, low-SES students may experience lifestyles that are very different from the ones they were brought up with (e.g., in terms of wealth) and that make them feel out of place (Browman & Destin 2016, Cole & Omari 2003). Furthermore, these feelings are experienced not only upon college entry but persist throughout the college years (Pascarella et al. 2004). In addition, low-SES students of color experience discrimination and microaggressions relatively frequently in higher education settings (Cole & Omari 2003). One study found that as education increased, instances of racial microaggressions increased, such that among college graduates of color, racial microaggressions comprised ~40% of the stress they experienced (Smith et al. 2011). Another study revealed that among a general sample of college students at a wealthy, elite private school, over 50% reported experiencing discrimination, including disparaging comments about the poor and dismissiveness about one’s social class (Langhout et al. 2007).
A second way that low-SES students striving for upward mobility may experience a sense of alienation is with regard to their neighborhood of origin. As they move into different educational spaces, these youths may experience a weakening of connections with their communities of origin (Destin et al. 2017, Van Laar et al. 2014). They may start to be treated differently by peers and be perceived as having adopted different characteristics associated with their higher-SES contexts (Destin et al. 2017). These students may begin to feel a disconnect between their communities of origin and their environments in college (Cole & Omari 2003, Destin & Debrosse 2017). This can create identity pressures on upwardly mobile youths: Continuing to associate with their group of origin may lead to rejection in their new context, but disassociating from it may lead to a loss of important sources of support (Van Laar et al. 2014). As a result, these youths may experience a growing sense of social isolation (not fitting with their neighborhood of origin, but also not fitting in their new academic environments). Or these students may have to work especially hard to effectively switch identities between school and home, acting one way in their neighborhoods and a different way at school (Cole & Omari 2003), which may create additional sources of stress.
In turn, experiences with discrimination, microaggressions, and a lack of belonging or social isolation all have implications for health. Discrimination has been associated with risk for a number of physical health problems (Williams & Mohammed 2009), and it is thought to be a significant contributor to explaining both racial and socioeconomic disparities in health (Myers 2009). Chronic or lifetime discrimination has been associated with coronary artery calcification (Lewis et al. 2006), new-onset cardiovascular events (e.g., heart attacks) in those initially free of cardiovascular disease (Everson-Rose et al. 2015), and diabetes onset over a 10-year follow-up period (Whitaker et al. 2017). Everyday discrimination has been associated with markers of low-grade inflammation (Kershaw et al. 2016) and with increases in blood pressure over a 10-year follow-up period (Moody et al. 2019). Discrimination is also consistently associated with poor sleep (Slopen et al. 2016). Among younger populations, one daily diary study of adolescents found that acts of discrimination were associated with greater self-reported health complaints (Huynh & Fuligni 2010). Further, an experimental study of college students of color found that those who were assigned to write about experiences of discrimination produced significantly fewer antibodies in response to a flu vaccine compared to students of color who wrote about a neutral topic (Stetler et al. 2006). It has been argued that experiences with discrimination elicit physiological responses that over time create challenges for biological systems, resulting in increased allostatic load and greater risk for chronic diseases in the long term (Mays et al. 2007). Further, the effects of discrimination are not limited to race/ethnicity, as effects of SES-based discrimination have also been documented on markers of inflammation (Van Dyke et al. 2017).
There is also a voluminous literature demonstrating the health consequences of social isolation. One meta-analysis concluded that social isolation, both objectively defined and subjectively experienced, is associated with an increased risk for early mortality (Holt-Lunstad et al. 2015). Subjectively experienced social isolation is conceptually related to lack of belonging. Moreover, social isolation effects are strongest among those who live in poverty and people of color (Cacioppo & Hawkley 2003). Social isolation has detrimental effects on both stress physiology and restorative processes such as sleep (Cacioppo & Cacioppo 2014, Cacioppo & Hawkley 2003). Furthermore, loneliness uniquely predicts health above and beyond other social relationship characteristics, such as social connections (Cacioppo & Cacioppo 2014). Finally, among college students, a sense of belonging, more so than other types of social support (e.g., tangible support, social intimacy), predicts self-reported physical health (Hale et al. 2005).
Thus, the experience of striving for upward mobility can lead to feelings of alienation, lack of belonging, and social isolation, with evidence that these types of social experiences are associated with poorer health. Further compounding these difficulties are the structural contexts that shape experiences with discrimination and microaggressions as upwardly mobile individuals enter spaces that were set up by and for those high in SES, and in turn, these experiences are linked to detrimental health effects.
Summary
In sum, we theorize that upwardly mobile individuals have a set of experiences that are distinct from the experiences of those who are stably high or low in SES and that have implications for physical health (Figure 1). Psychologically, upwardly mobile individuals are more likely to exhibit prolonged high levels of striving and self-control. These determined, persistent efforts are hypothesized to result in a trade-off, whereby academic successes come at a cost to physical health, a pattern termed skin-deep resilience. From a replicability standpoint, the findings about striving are strengthened by the fact that similar patterns have emerged consistently across multiple study samples. Environmentally, upwardly mobile individuals experience a larger set of competing demands from both the higher-SES context they seek to enter and their families and communities of origin. The combination of school, work, and home demands means that academic successes have to be achieved over and above other life demands, which creates a greater overall burden and less time for restorative activities and, we suggest, results in wear and tear on physiological systems. Culturally, upwardly mobile individuals are more likely to experience a mismatch between the adaptive strategies they learned to exhibit in their childhood environments and the strategies that are valued in higher-SES environments, creating added struggles that are presumed to affect physiological systems. Finally, structurally, the experience of moving into high-SES spaces set up by and for majority groups results in upwardly mobile individuals’ experiencing discrimination, microaggressions, and a sense of alienation and lack of belonging, all of which have associations with physical health.
In addition, it is important to note that financially, upwardly mobile individuals do not have the same wealth profiles as stably high-SES individuals (Cole & Omari 2003). Because of student loan debt, a lack of family wealth, and limited savings, their financial situations are often quite tenuous, even once they enter high-earning professions. Additionally, feelings of obligation to help family members and communities of origin place a greater financial strain on the wealth that they do have. This can result in economic stressors, even among individuals who are currently high in SES, that take an additional toll on their health.
Finally, one question that might arise is why, given all the challenges identified above, upwardly mobile individuals would not experience worse (rather than better) mental health. We hypothesize that this is in part because these upwardly mobile individuals are achieving a multitude of successes in their lives in terms of education, occupations, and incomes. These successes make them and their families proud. We speculate that the praise from others and boosts to self-esteem that result from these successes help foster positive mental health profiles. In addition, the idea that exposure to numerous environmental adversities might not necessarily result in poorer mental health can be seen in the literature, whereby Blacks have lower levels of major depression than Whites, despite the greater stress exposure, marginalized status, and fewer resources they typically experience (Barnes & Bates 2017). This may also be due in part to protective factors such as religiosity, self-esteem, or coping behaviors (Barnes & Bates 2017).
PATHWAYS TO HEALTH
Next we address the mechanistic question of how the stressful psychological experiences related to upward mobility come to affect physical health. We focus this discussion on cardiometabolic health, because nearly all of the literature on upward mobility and skin-deep resilience is in that domain. In health psychology, there are two pathways commonly proposed as mechanisms. One is an effect of stress on physiological systems, and the second is an effect of stress on health behaviors (see Figure 2).
Figure 2.
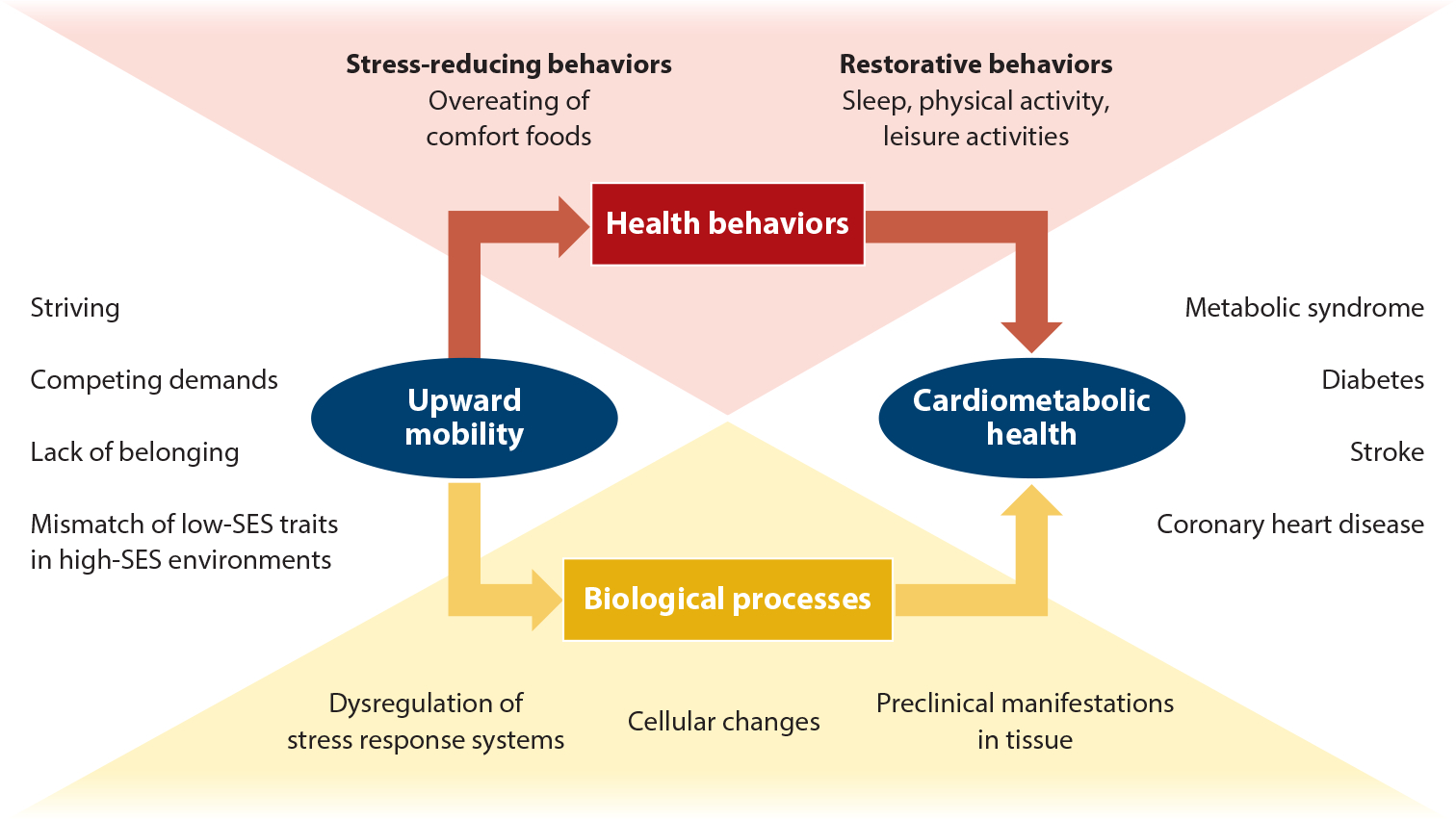
Model of pathways connecting the psychological experiences of upwardly mobile individuals to physical health. These pathways include health behaviors (both behaviors that help to reduce stress and restorative health behaviors) and biological processes (acute dysregulation of the autonomic nervous system and hypothalamic pituitary adrenal axis; cellular changes, such as epigenetic aging; and preclinical manifestations over time of disease in tissues) that have implications for cardiometabolic health in adulthood. Abbreviation: SES, socioeconomic status.
There are two categories of stressors relevant to upward mobility that likely affect biological and behavioral pathways. The first is a general set of chronic stressors that occur more frequently in the low-SES contexts that upwardly mobile individuals come from, including economic hardship, community disadvantage, and discrimination (Brody et al. 2010). The second is the specific stressors described above experienced by those pursuing upward mobility. Below we provide an overview of how these stressors affect both health behaviors and physiological systems.
Health Behaviors
Health behaviors such as exercise, diet, and sleep are shaped in part by the contexts in which individuals reside. For example, the lack of green spaces and sidewalks as well as the violence found in many low-SES communities constrain the options for physical activity (Boone-Heinonen & Gordon-Larsen 2011, Coombes et al. 2010). Food deserts, with a lack of healthy food options and an abundance of high-calorie, energy-dense foods, are more prominent in low-SES neighborhoods (Walker et al. 2010). In addition, physical and social environmental conditions such as noise and density, as well as violence, can disrupt sleep for those in low-SES neighborhoods (Johnson et al. 2018).
At the individual level, these contextual factors contribute to the general chronic stress that upwardly mobile individuals experience. These and other upward mobility–specific stressors are then hypothesized to have direct effects on the health behaviors that individuals practice. In turn, patterns of diet, physical activity, and sleep have consistent associations with longer-term cardiometabolic outcomes ranging from diabetes to cardiovascular disease to mortality (Gallicchio & Kalesan 2009, Itani et al. 2017, Loef & Walach 2012, Warburton et al. 2006).
Stress-Reducing Health Behaviors
Broadly speaking, we hypothesize that stressors that are uncontrollable will trigger behaviors such as unhealthy eating as one means of relieving the negative emotions associated with uncontrollable stress. Uncontrollable stressors include the contextual stressors associated with poverty and racism, which have many structural and societal root causes. In addition, the upward mobility–specific stressors of social exclusion, lack of belonging, and mismatches in fit, and the accompanying experiences with discrimination and microaggressions, are also hypothesized to be stressors outside of upwardly mobile individuals’ control, given that they stem from interactions with higher-SES individuals and the cultural norms found within higher-SES settings.
When one cannot mitigate a stressor, the best one can do is to alleviate one’s emotional reactions, in part through behaviors that are pleasurable in the moment and stress relieving. The overeating of comfort foods (i.e., foods high in refined sugars and fat or foods that are highly processed) represents one socially sanctioned way to do this (Jackson et al. 2010). Chronic stress is associated with snacking, as well as with craving and consuming foods that are high in sugar and fat (Araiza & Lobel 2018, Torres & Nowson 2007), in both children and adults (Hill et al. 2018). These patterns are thought to arise in part because stress triggers the release of cortisol, which stimulates hunger and feeding behaviors, increases the drive toward pleasurable activities, and leads to an increase in visceral fat storage (Adam & Epel 2007, Sominsky & Spencer 2014). In response to high-calorie food images, individuals high in chronic stress show greater activity in reward and motivation regions of the brain, and decreased activity in executive control regions, compared to individuals low in chronic stress (Tryon et al. 2013). Eating in response to stress is thought to occur for a number of reasons: because it helps to alleviate negative emotions, because it serves as an emotion-focused coping approach, and because the burdens on cognitive load imposed by stress decrease one’s ability to engage in self-restraint when it comes to food (Araiza & Lobel 2018).
These patterns may also be more prevalent in certain groups that are more likely to experience uncontrollable stressors, such as individuals of color and those low in SES (Jackson et al. 2010). For example, Blacks have been theorized to use coping strategies for dealing with chronic environmental stressors that preserve mental health at the expense of physical health (Jackson et al. 2010). Thus, life stress is associated with depression only among Blacks who do not engage in unhealthy behaviors; in contrast, stress is not associated with depression among Blacks who do engage in unhealthy behaviors. Furthermore, these patterns are specific to Blacks and not found among Whites (Jackson et al. 2010, Mezuk et al. 2010). In addition, epidemiological research has documented that Black/White disparities in obesity are greatest among high-SES adults (Gordon-Larsen et al. 2003). This is consistent with skin-deep resilience patterns, whereby achieving mobility (i.e., high adult SES) for individuals of color comes at a cost to physical health, and it suggests that unhealthy eating may be one pathway explaining skin-deep resilience effects. Taken together, these studies suggest that comfort eating may represent a good fit as a coping strategy for the numerous uncontrollable stressors associated with upward mobility, but with consequences for obesity and related chronic diseases down the line.
We note that previous literature has also shown that Blacks are more likely to engage in substance use as a way of coping with contextual stressors (Jackson et al. 2010, Mezuk et al. 2010). The use of substances may also help alleviate stress and negative emotions in the short term (Jackson et al. 2010); however, we hypothesize that individuals pursuing upward mobility gravitate toward the overeating of comfort foods, rather than substance use, as a more socially sanctioned way of dealing with stress. For example, low-SES individuals who make it to college show lower levels of substance use compared to those who do not go to college (Chen et al. 2015). Similarly, low-SES individuals who have high self-control show lower levels of substance use than those who are low in self-control (Miller et al. 2015). Thus, while substance use as a coping strategy may be used by some, it appears to be less likely as a health behavior pathway among low-SES individuals of color who are pursuing upward mobility.
Lack of Restorative Health Behaviors
Health behaviors can also serve a second function, that of restoring physical and mental wellbeing. Behaviors such as adequate sleep, physical activity, and other leisure activities can help individuals maintain good health despite stress in their lives. Here, we suspect that upwardly mobile individuals are less likely to engage in restorative health behaviors because of the frequency (rather than controllability) of life stressors. That is, the high number of competing demands that upwardly mobile individuals have to balance between school, work, family responsibilities, and financial needs consume time and energy in ways that leave little room for engaging in restorative health behaviors. In addition, the disproportionately large amounts of effort that upwardly mobile individuals must expend in striving for similar academic outcomes as their more privileged counterparts mean that restorative health behaviors often have to be sacrificed to achieve academic success.
In general, the literature shows that those who experience high levels of competing demands have less time for exercise and leisure pursuits (Nomaguchi & Bianchi 2004, Pearson 2008). Lack of time is one of the principal reasons for not engaging in sufficient physical activity, and it represents a more influential factor for low-SES than for high-SES individuals (Chinn et al. 1999). A review found that among Black women, lack of time is a key barrier to physical activity and is primarily due to the competing demands and fatigue that these women experience as they balance multiple roles related to work and family caretaking (Joseph et al. 2015). Furthermore, when work and family demands are high and in conflict with one another, people often sacrifice sleep in order to manage their obligations (Barnes et al. 2012). For example, those who work longer hours report shorter sleep durations (Akerstedt 2006, Jackson et al. 2015). High demands, particularly in terms of being overcommitted, being preoccupied with demands, and suffering from burnout, are all associated with greater sleep disturbances (Akerstedt 2006). Finally, frequent life stressors have been theorized and found to contribute to SES disparities in sleep (Jackson et al. 2015).
Furthermore, certain groups that experience more frequent life stressors are also less likely to engage in restorative health behaviors. For example, both low-SES individuals and individuals of color experience more negative life events than high-SES or White individuals (Hatch & Dohrenwend 2007). In turn, low-SES individuals are less likely to engage in vigorous activity or to achieve recommended levels of physical activity compared to high-SES individuals (Delva et al. 2006), both adults and adolescents (Hanson & Chen 2007a). Those who are upwardly mobile have physical activity levels in between those of the stable low- and stable high-SES groups (Elhakeem et al. 2017). Using accelerometry, Blacks were found to engage in less moderate-to-vigorous physical activity compared to Whites (Tucker et al. 2011). Black and Latinx women also reported exercising less frequently (Delva et al. 2006) and showed greater declines in exercise over time compared to White women (Clarke et al. 2009). Finally, in adolescents, lower levels of physical activity mediated race differences in obesity (Hanson & Chen 2007b).
With respect to sleep, reviews have found that both low SES and racial/ethnic minority status are associated with higher rates of sleep disturbances, shorter sleep duration, and poorer sleep quality (Grandner et al. 2016, Jackson et al. 2015). Both lower-SES adults and women of color show greater declines in adequate sleep over time (Clarke et al. 2009). In addition, Black/White disparities in the occurrence of short sleep are greatest in high-SES adults: That is, the likelihood of regularly experiencing short sleep decreased as SES increased among Whites, but it increased as SES increased among Blacks (Jackson et al. 2013). This is consistent with other skin-deep resilience patterns and suggests that inadequate sleep may serve as one pathway explaining skindeep resilience effects.
Summary
In sum, individuals pursuing upward mobility experience two types of stressors that have implications for health behaviors (see Figure 2). The first is uncontrollable stressors stemming from upward mobility–specific experiences with mismatches in fit and lack of belonging as well as discrimination. We postulate that uncontrollable stressors lead to engagement in unhealthy behaviors, such as the overeating of comfort foods, as a way to relieve stress and negative emotions. The second is the high frequency of stressors that upwardly mobile individuals experience in terms of the competing demands in their lives and their prolonged, effortful striving, both of which leave little time for restorative health behaviors, such as physical and leisure activities and sleep. In turn, unhealthy eating, physical inactivity, and inadequate sleep are key lifestyle contributors to cardiometabolic health problems (Itani et al. 2017, Torres & Nowson 2007, Warburton et al. 2006) and explain a substantial fraction of racial and economic health disparities in the United States (Bancks et al. 2017, Krishnan et al. 2010).
Biological Pathways
The final portion of our model depicts biological mechanisms that might explain how upward mobility comes to affect physical health (see Figure 2). Again, we focus on health problems in the cardiometabolic realm, as they have been the focus of upward mobility research to date. Because research on biological pathways is just emerging, we keep this section intentionally brief, and we acknowledge that much of it is speculative. Still, we believe it is useful to offer some general hypotheses, which can function as a roadmap for future hypothesis testing around skin-deep resilience mechanisms.
What are the plausible biological mechanisms through which achieving upward mobility could undermine cardiometabolic health? To answer this question, we draw upon the handful of studies reviewed above that measured biological processes and integrate their findings with more general knowledge of the mechanisms by which early experiences come to affect these conditions (Danese & McEwen 2012, Miller et al.2009, Suglia et al. 2018). This synthesis suggests a scenario whereby the challenges, struggles, and behaviors associated with upward mobility dysregulate activity of the body’s primary stress response systems, the autonomic nervous system and the hypothalamic pituitary adrenocortical axis (Brody et al. 2013, Chen et al. 2015). Persistent changes in the outflow of these axes’ hormonal products—epinephrine, norepinephrine, and cortisol—should alter the behavior of target cells in many tissues and organs, including the heart, lungs, blood vessels, immune system, and skeletal muscle, to name a few.
The nature of these changes will likely differ somewhat by tissue and will also depend on host genetics, other exposures, and additional factors. However, based on the available evidence, we would hypothesize that upward mobility accelerates the epigenetic aging of immune cells (Miller et al. 2015) and alters the way that immune cells respond to and recover from challenges (McEwen & Seeman 1999). In cells of the innate immune system, this would likely involve exaggerated cytokine responses to threats—both microbial and sterile—which contribute to chronic low-grade inflammatory processes (Irwin & Cole 2011). In cells of the adaptive immune system, research suggests that chronic stress would likely entail weaker cellular and humoral responses to pathogens, lowering host resistance to infectious diseases and reducing the protective value of vaccinations (Glaser & Kiecolt-Glaser 2005). In cells that comprise the vascular system, excessive hormonal stimulation might compromise the vessel’s elasticity to dilate when blood flow increases, an early sign of cardiovascular risk known as endothelial dysfunction (Harris & Matthews 2004). And in cells that make up adipose tissue and skeletal muscle, persistent hormonal and inflammatory exposures would presumably decrease sensitivity to insulin, impairing in the process the metabolism of fats and the regulation of glucose (Sjostrand & Eriksson 2009). These processes, if sustained, would increase the subsequent risk of diabetes, coronary heart disease, and stroke, among other cardiometabolic health problems.
Besides altering the way that cells function, variations in stress hormone outflow might also be expected to change the composition of tissues. There are two tissues where this seems particularly likely to occur, according to the broader literature: the gut, where initial evidence suggests that adversities reduce the diversity of the microbial population (He et al. 2018, Miller et al. 2016b), with implications for microbiome-immune communication (Cruz-Pereira et al.2020) and increasing risk for a variety of chronic health problems involving dysbiosis (Gilbert et al. 2018); and in the immune system, where hormones can selectively mobilize immature myeloid cells that have a strong proinflammatory skew into circulation (Miller et al. 2008, Powell et al. 2013). In animal models, these cells migrate into developing atherosclerotic plaques, accelerating the progression of heart disease (Heidt et al. 2014).
CONCLUSIONS
The physical health of individuals who achieve upward mobility from childhood to adulthood is often not equivalent to that of their peers who have had consistently high SES. In fact, upward mobility appears to be associated with a trade-off whereby economic success and good mental health come at the expense of physical health, a pattern we have termed skin-deep resilience. We hypothesize that skin-deep resilience emerges from a set of psychological experiences that are distinct from the experiences of individuals who are stably high or low in SES. These experiences include prolonged high levels of striving; competing demands between the environments upwardly mobile individuals seek to enter and their environments of origin; mismatches between the adaptive strategies these individuals learned to exhibit in their childhood environments and those that are valued in higher-SES environments; and the sense of alienation, lack of belonging, and experiences with discrimination that upwardly mobile individuals face as they move into high-SES spaces set up by and for majority groups. In turn, stressors that are uncontrollable lead upwardly mobile individuals to engage in unhealthy behaviors, such as the overeating of comfort foods, as a way to relieve negative emotions. Further, the high frequency of stressors that upwardly mobile individuals experience leaves little time for physical and leisure activities or sleep. These health behaviors are key contributors to cardiometabolic health problems. Biologically, these stressors contribute to the dysregulation of stress response systems, which over time alters the behaviors of target cells in many tissues and organs and eventually leads to preclinical manifestations and subsequent risks of diabetes, coronary heart disease, and stroke, among other cardiometabolic health problems.
Moving forward, there is a need for additional studies that can ascertain mechanisms and causality. Longitudinal studies are needed to determine when skin-deep resilience emerges during development, what mechanisms drive its development, and whether effects can be demonstrated above and beyond baseline health measures. Natural experiments (where possible) that take advantage of the rollout of new federal or state programs that could affect mobility would help answer questions about causality. Additional twin studies would also be helpful in this regard, as they can minimize genetic and environmental confounding.
Even more definitive would be experiments that manipulate potential skin-deep resilience mechanisms. These could take the form of interventions designed to mitigate the physical health costs of skin-deep resilience by addressing targeted mechanisms. For example, at the individual level, teaching coping strategies for dealing with the uncontrollable stressors that individuals seeking upward mobility confront could help reduce their health effects (Antoni 2012). At the interpersonal level, interventions that provide social support might help mitigate the health consequences related to alienation and perceived lack of belonging for low-SES individuals striving for success (Chen et al. 2021). At the structural level, interventions that seek to change the climate of higher education institutions to be more inclusive of lower-SES students could have health benefits as well (Browman & Destin 2016, Stephens et al. 2014). Finally, future interventions that seek to improve students’ academic outcomes in educational settings (Harackiewicz & Priniski 2018) may want to be mindful of potential physical health consequences.
If successful, these approaches could lead to new programs that consider youth more holistically, supporting academic endeavors and pathways to successful lives at the same time as they monitor and consider the physical well-being of youths. Programs could be designed at the individual, family, and/or school level that would provide additional resources and support for youths who are striving for upward mobility, with the hope that in the future, achieving the American dream will not have to come at the cost of one’s health.
SUMMARY POINTS.
Upward mobility, particularly in low-income individuals of color, is associated with atrade-off, whereby individuals achieve economic success, good mental health, and other positive life outcomes but are more likely to have poor physical health. This pattern has been termed skin-deep resilience.
Psychological explanations include the role of striving—that is, the idea that the high levels of sustained effort that lower-SES individuals exert to achieve their academic successes lead to positive life outcomes but at the same time take a physiological toll on their health.
Low-SES students striving for academic success often have to juggle academic demands with numerous other work and family demands. Balancing these competing demands creates an overall higher burden that contributes to the physiological health costs.
Culturally, upwardly mobile individuals are more likely to experience a mismatch between the adaptive strategies they learned to exhibit in their childhood environments and the strategies that are valued in higher-SES environments; this creates additional stress for these individuals, with potential physiological implications.
As low-SES individuals striving for upward mobility move into new spaces, they often experience both a lack of belonging with peers in their new environments (e.g., college, workplace) and greater alienation from their families and neighborhoods of origin. In turn, experiences with lack of belonging, social isolation, and discrimination are all linked to poor physical health.
Pathways to health include health behaviors; that is, upwardly mobile individuals experience uncontrollable stressors (e.g., lack of belonging) that predispose them toward unhealthy behaviors (e.g., comfort eating) in an effort to cope with these stressors. In addition, the high frequency of stressors that upwardly mobile individuals experience (e.g., competing demands) make it difficult for them to engage in restorative health behaviors such as exercise and adequate sleep.
A second pathway to health is biological; that is, the stressors associated with upward mobility dysregulate the activity of the body’s stress response systems, and persistent changes in these systems alter the behaviors of target cells in tissues and organs, leading eventually to preclinical manifestations and subsequent risk of cardiometabolic diseases.
FUTURE DIRECTIONS.
Additional studies are needed to determine the boundaries or parameters around skindeep resilience—that is, when it emerges during development and which demographic groups are at greatest risk for skin-deep resilience.
Future longitudinal studies are needed to test the specific psychological and biological mechanisms theorized in this review.
Natural experiment studies of skin-deep resilience—for example, testing programs orpolicies that promote upward mobility—would allow researchers to gain a better handle on causality.
Experimental studies are also needed that focus on interventions designed to mitigate the physical health costs of skin-deep resilience by addressing targeted mechanisms.
ACKNOWLEDGMENTS
Support for the writing of this manuscript was provided by NIH grants HD093718, HL136676, MD011749, and P50DA051361. The authors thank Rebekah Siliezar for the production of the figures.
Footnotes
DISCLOSURE STATEMENT
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
LITERATURE CITED
- Adam EK, Quinn ME, Tavernier R, McQuillan MT, Dahlke KA, Gilbert KE. 2017. Diurnal cortisol slopes and mental and physical health outcomes: a systematic review and meta-analysis. Psychoneuroendocrinology 83:25–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adam TC, Epel ES. 2007. Stress, eating, and the reward system. Physiol. Behav. 91:449–58 [DOI] [PubMed] [Google Scholar]
- Adler NE, Snibbe AC. 2003. The role of psychosocial processes in explaining the gradient between socioeconomic status and health. Curr. Dir. Psychol. Sci. 12:119–23 [Google Scholar]
- Adler NE, Stewart J. 2010. Health disparities across the lifespan: meaning, methods, and mechanisms. Ann. N. Y. Acad. Sci. 1186:5–23 [DOI] [PubMed] [Google Scholar]
- Akerstedt T 2006. Psychosocial stress and impaired sleep. Scand. J. Work Environ. Health 32:493–501 [PubMed] [Google Scholar]
- Antoni MH. 2012. Stress management, PNI, and disease. In The Oxford Handbook of Psychoneuroimmunology, ed. Segerstrom SC, pp. 385–420. New York: Oxford Univ. Press [Google Scholar]
- Araiza AM, Lobel M. 2018. Stress and eating: definitions, findings, explanations, and implications. Soc. Pers. Psychol. Compass 12:e12378 [Google Scholar]
- Aspinwall LG. 2011. Future-oriented thinking, proactive coping, and the management of potential threats to health and well-being. In The Oxford Handbook of Stress, Health, and Coping, ed. Folkman S, pp. 334–68. New York: Oxford Univ. Press [Google Scholar]
- Aspinwall LG, Taylor SE. 1997. A stitch in time: self-regulation and proactive coping.Psychol.Bull.121(3):417–36 [DOI] [PubMed] [Google Scholar]
- Backe EM, Seidler A, Latza U, Rossnagel K, Schumann B. 2012. The role of psychosocial stress at work for the development of cardiovascular diseases: a systematic review. Int. Arch. Occup. Environ. Health 85:67–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bancks MP, Kershaw K, Carson AP, Gordon-Larsen P, Schreiner PJ, Carnethon MR. 2017. Association of modifiable risk factors in young adulthood with racial disparity in incident type 2 diabetes during middle adulthood. J. Am. Med. Assoc. 318:2457–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes CM, Wagner DT, Ghumman S. 2012. Borrowing from sleep to pay work and family: expanding time-based conflict to the broader nonwork domain. Pers. Psychol. 65:789–819 [Google Scholar]
- Barnes DM, Bates LM. 2017. Do racial patterns in psychological distress shed light on the Black-White depression paradox? A systematic review. Soc. Psychiatry Psychiatr. Epidemiol. 52:913–28 [DOI] [PubMed] [Google Scholar]
- Bateson P 2007. Developmental plasticity and evolutionary biology. J. Nutr. 137:1060–62 [DOI] [PubMed] [Google Scholar]
- Bateson P, Gluckman P, Hanson M. 2014. The biology of developmental plasticity and the Predictive Adaptive Response hypothesis. J. Physiol. 592:2357–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckles GL, Bullard KM, Saydah S, Imperatore G, Loustalot F, Correa A. 2019. Life course socioeconomic position, allostatic load, and incidence of type 2 diabetes among African American adults: the Jackson Heart Study, 2000–04 to 2012. Ethn. Dis. 29:39–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone-Heinonen J, Gordon-Larsen P. 2011. Life stage and sex specificity in relationships between the built and socioeconomic environments and physical activity. J. Epidemiol. Community Health 65:847–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. 2010. Socioeconomic disparities in health in the United States: what the patterns tell us. Am. J. Public Health 100:S186–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Chen Y, Kogan SM. 2010. A cascade model connecting life stress to risk behavior among rural African American emerging adults. Dev. Psychopathol. 22:667–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Yu T, Chen E, Miller GE, Kogan SM, Beach SRH. 2013. Is resilience only skin deep? Rural African Americans’ preadolescent socioeconomic status-related risk and competence and age 19 psychological adjustment and allostatic load. Psychol. Sci. 24:1285–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Yu T, Miller GE, Chen E. 2016. Resilience in adolescence, health, and psychosocial outcomes. Pediatrics 138:e20161042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browman AS, Destin M. 2016. The effects of a warm or chilly climate toward socioeconomic diversity on academic motivation and self-concept. Pers. Soc. Psychol. Bull. 42:172–87 [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Cacioppo S. 2014. Social relationships and health: the toxic effects of perceived social isolation. Soc. Pers. Psychol. Compass 8:58–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC. 2003. Social isolation and health, with an emphasis on underlying mechanisms. Perspect. Biol. Med. 46:S39–52 [PubMed] [Google Scholar]
- Castagne R, Delpierre C, Kelly-Irving M, Campanella G, Guida F, et al. 2016. A life course approach to explore the biological embedding of socioeconomic position and social mobility through circulating inflammatory markers. Sci. Rep. 6:25170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Debrosse R, Ham PJ, Hoffer LC, Leigh AKK, Destin M. 2021. Effects of social support in an academic context on low-grade inflammation in high school students. J. Behav. Med. In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Langer DA, Raphaelson YE, Matthews KA. 2004. Socioeconomic status and health in adolescents: the role of stress interpretations. Child Dev. 75(4):1039–52 [DOI] [PubMed] [Google Scholar]
- Chen E, Miller GE. 2012. “Shift-and-persist” strategies: why being low in socioeconomic status isn’t always bad for health. Perspect. Psychol. Sci. 7:135–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Miller GE, Brody GH, Lei M. 2015. Neighborhood poverty, college attendance, and diverging profiles of substance use and allostatic load in rural African American youth. Clin. Psychol. Sci. 3(5):675–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Miller GE, Walker HA, Arevalo JM, Sung CY, Cole SW. 2009. Genome-wide transcriptional profiling linked to social class in asthma. Thorax 64(1):38–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Shalowitz MU, Story RE, Hayen R, Leigh AKK, Hoffer LC, et al. 2019. The costs of high self-control in Black and Latino youth with asthma: divergence of mental health and inflammatory profiles. Brain Behav. Immun. 80:120–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Strunk RC, Trethewey A, Schreier HM, Maharaj N, Miller GE. 2011. Resilience in low-socioeconomic-status children with asthma: adaptations to stress. J. Allergy Clin. Immunol. 128(5):970–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Yu T, Siliezar R, Drage JN, Dezil J, Miller GE, Brody GH. 2020. Evidence for skin-deep resilience using a co-twin control design: Effects on low-grade inflammation in a longitudinal study of youth.Brain Behav. Immun. 88:661–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinn DJ, White M, Harland J, Drinkwater C, Raybould S. 1999. Barriers to physical activity and socioeconomic position: implications for health promotion. J. Epidemiol. Community Health 53:191–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke PJ, O’Malley PM, Johnston LD, Schulenberg JE, Lantz P. 2009. Differential trends in weight-related health behaviors among American young adults by gender, race/ethnicity, and socioeconomic status: 1984–2006. Am. J. Public Health 99:1893–901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole ER, Omari SR. 2003. Race, class and the dilemmas of upward mobility for African Americans. J. Soc. Issues 59:785–802 [Google Scholar]
- Coombes E, Jones AP, Hillsdon M. 2010. The relationship of physical activity and overweight to objectively measured green space accessibility and use. Soc. Sci. Med. 70:816–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtin E, Nafilyan V, Avendano M, Meneton P, Berkman LF, Goldberg M, et al. 2019. Longer schooling but not better off? A quasi-experimental study of the effect of compulsory schooling on biomarkers in France. Soc. Sci. Med. 220:379–86 [DOI] [PubMed] [Google Scholar]
- Cruz-Pereira JS, Rea K, Nolan YM, O’Leary OF, Dinan TG, Cryan JF. 2020. Depression’s unholy trinity: dysregulated stress, immunity, and the microbiome. Annu. Rev. Psychol. 71:49–78 [DOI] [PubMed] [Google Scholar]
- Danese A,McEwen BS. 2012. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol. Behav. 106(1):29–39 [DOI] [PubMed] [Google Scholar]
- Delva J, O’Malley PM, Johnston LD. 2006. Racial/ethnic and socioeconomic status differences in overweight and health-related behaviors among American students: national trends 1986–2003. J. Adolesc. Health 39:536–45 [DOI] [PubMed] [Google Scholar]
- Destin M, Debrosse R. 2017. Upward social mobility and identity. Curr. Opin. Psychol. 18:99–104 [DOI] [PubMed] [Google Scholar]
- Destin M, Rheinschmidt-Same M, Richeson JA. 2017. Status-based identity: a conceptual approach integrating the social psychological study of socioeconomic status and identity. Perspect. Psychol. Sci. 12:270–89 [DOI] [PubMed] [Google Scholar]
- Diez Roux AV, Mair C. 2010. Neighborhoods and health. Ann. N. Y. Acad. Sci. 1186:125–45 [DOI] [PubMed] [Google Scholar]
- Duckworth A 2016. Grit: The Power of Passion and Perseverance. New York: Scribner [Google Scholar]
- Duggan KA, Jennings JR, Matthews KA. 2019. Prospective associations of adolescent conscientiousness with psychological resources and metabolic syndrome in Black and White men. Psychosom. Med. 81:341–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan GJ, Murnane RJ. 2011. Whither Opportunity? Rising Inequality, Schools, and Children’s Life Chances. New York: Russell Sage Found. [Google Scholar]
- Elhakeem A, Hardy R, Bann D, Caleyachetty R, Cosco TD, et al. 2017. Intergenerational social mobility and leisure-time physical activity in adulthood: a systematic review. J. Epidemiol. Community Health 71:673–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis BJ, Bianchi J, Griskevicius V, Frankenhuis WE. 2017. Beyond risk and protective factors: an adaptationbased approach to resilience. Perspect. Psychol. Sci. 12:561–87 [DOI] [PubMed] [Google Scholar]
- Everson-Rose SA, Lewis TT. 2005. Psychosocial factors and cardiovascular diseases. Annu. Rev. Public Health 26:469–500 [DOI] [PubMed] [Google Scholar]
- Everson-Rose SA, Lutsey PL, Roetker NS, Lewis TT, Kershaw KN, et al. 2015. Perceived discrimination and incident cardiovascular events. Am. J. Epidemiol. 182:225–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farah MJ. 2017. The neuroscience of socioeconomic status: correlates, causes, and consequences. Neuron 96:56–71 [DOI] [PubMed] [Google Scholar]
- Finkelstein DM, Kubzansky LD, Capitman J, Goodman E. 2007. Socioeconomic differences in adolescent stress: the role of psychological resources. J. Adolesc. Health 40(2):127–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frankenhuis WE, de Weerth C. 2013. Does early-life exposure to stress shape or impair cognition? Curr. Dir. Psychol. Sci. 22:407–12 [Google Scholar]
- Frankenhuis WE, Nettle D. 2020. The strengths of people in poverty. Curr. Dir. Psychol. Sci. 29(1):16–21 [Google Scholar]
- Frestad D, Prescott E. 2017. Vital exhaustion and coronary heart disease risk: a systematic review and meta-analysis. Psychosom. Med. 79:260–72 [DOI] [PubMed] [Google Scholar]
- Fuligni AJ, Pedersen S. 2002. Family obligation and the transition to young adulthood. Dev. Psychol. 38(5):856–68 [DOI] [PubMed] [Google Scholar]
- Fuligni AJ, Telzer EH, Bower J, Irwin MR, Kiang L, Cole SW. 2009. Daily family assistance and inflammation among adolescents from Latin American and European backgrounds. Brain Behav. Immun. 23(6):803–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallicchio L, Kalesan B. 2009. Sleep duration and mortality: a systematic review and meta-analysis. J. Sleep Res. 18:148–58 [DOI] [PubMed] [Google Scholar]
- Gallo LC, Matthews KA. 2003. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychol. Bull. 129(1):10–51 [DOI] [PubMed] [Google Scholar]
- Gaydosh L, Schorpp K, Chen E, Miller G, Harris KM. 2018. College completion predicts lower depression but higher metabolic syndrome among disadvantaged minorities in young adulthood.PNAS 115:109–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert JA, Blaser MJ, Caporaso JG, Jansson JK, Lynch SV, Knight R. 2018. Current understanding of the human microbiome. Nat. Med. 24:392–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert-Ouimet M, Trudel X, Brisson C, Milot A, Vezina M. 2014. Adverse effects of psychosocial work factors on blood pressure: systematic review of studies on demand-control-support and effort-reward imbalance models. Scand. J. Work Environ. Health 40:109–32 [DOI] [PubMed] [Google Scholar]
- Glaser R, Kiecolt-Glaser JK. 2005. Stress-induced immune dysfunction: implications for health. Nat. Rev. Immunol. 5:243–51 [DOI] [PubMed] [Google Scholar]
- Glover LM, Cain-Shields LR, Spruill TM, O’Brien EC, Barber S, et al. 2020a. Goal-striving stress and incident cardiovascular disease in Blacks: the Jackson Heart Study. J. Am. Heart Assoc. 9:e015707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glover LM, Cain-Shields LR, Wyatt SB, Gebreab SY, Diez Roux AV, Sims M. 2020b. Life course socioeconomic status and hypertension in African American adults: The Jackson Heart Study. Am. J. Hypertens. 33:84–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon-Larsen P, Adair LS, Popkin BM. 2003. The relationship of ethnicity, socioeconomic factors, and overweight in US adolescents. Obes. Res. 11(1):121–29 [DOI] [PubMed] [Google Scholar]
- Grandner MA, Williams NJ, Knutson KL, Roberts D, Jean-Louis G. 2016. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. 18:7–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajat A, Hsia C, O’Neill MS. 2015. Socioeconomic disparities and air pollution exposure: a global review. Curr. Environ. Health Rep. 2:440–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale CJ, Hannum JW, Espelage DL. 2005. Social support and physical health: the importance of belonging. J. Am. Coll. Health 53:276–84 [DOI] [PubMed] [Google Scholar]
- Hanson MD, Chen E. 2007a. Socioeconomic status and health behaviors in adolescence: a review of the literature. J. Behav. Med. 30(3):263–85 [DOI] [PubMed] [Google Scholar]
- Hanson MD, Chen E. 2007b. Socioeconomic status, race, and body mass index: the mediating role of physical activity and sedentary behaviors during adolescence. J. Pediatr. Psychol. 32(3):250–59 [DOI] [PubMed] [Google Scholar]
- Harackiewicz JM, Priniski SJ. 2018. Improving student outcomes in higher education: the science of targeted intervention. Annu. Rev. Psychol. 69:409–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hariri AR, Tessitore A, Mattay VS, Fera F, Weinberger DR. 2002. The amygdala response to emotional stimuli: a comparison of faces and scenes. NeuroImage 17:317–23 [DOI] [PubMed] [Google Scholar]
- Harris KF, Matthews KA.2004.Interactions between autonomic nervous system activity and endothelial function: a model for the development of cardiovascular diseas. Psychosom. Med. 66:153–64 [DOI] [PubMed] [Google Scholar]
- Hatch SL, Dohrenwend BP. 2007. Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: a review of the research. Am. J. Community Psychol. 40(3–4):313–32 [DOI] [PubMed] [Google Scholar]
- He Y, Wu W, Wu S, Zheng HM, Li P, et al. 2018. Linking gut microbiota, metabolic syndrome and economic status based on a population-level analysis. Microbiome 6:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heidt T, Sager HB, Courties G, Dutta P, Iwamoto Y, et al. 2014. Chronic variable stress activates hematopoietic stem cells. Nat. Med. 20:754–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heraclides A, Brunner E. 2010. Social mobility and social accumulation across the life course in relation to adult overweight and obesity: the Whitehall II study. J. Epidemiol. Community Health 64:714–19 [DOI] [PubMed] [Google Scholar]
- Hill DC, Moss RH, Sykes-Muskett B, Conner M, O’Connor DB. 2018. Stress and eating behaviors in children and adolescents: systematic review and meta-analysis. Appetite 123:14–22 [DOI] [PubMed] [Google Scholar]
- Hogberg L, Cnattingius S, Lundholm C, Sparen P, Iliadou AN. 2012. Intergenerational social mobility and the risk of hypertension. J. Epidemiol. Community Health 66:e9. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. 2015. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect. Psychol. Sci. 10:227–37 [DOI] [PubMed] [Google Scholar]
- Huynh VW, Fuligni AJ. 2010. Discrimination hurts: the academic, psychological, and physical well-being of adolescents. J. Res. Adolesc. 20:916–41 [Google Scholar]
- Irwin MR, Cole SW. 2011. Reciprocal regulation of the neural and innate immune systems. Nat. Rev. Immunol. 11:625–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Itani O, Jike M, Watanabe N, Kaneita Y. 2017. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. 32:246–56 [DOI] [PubMed] [Google Scholar]
- Jackson CL, Redline S, Emmons KM. 2015. Sleep as a potential fundamental contributor to disparities in cardiovascular health. Annu. Rev. Public Health 36:417–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson CL, Redline S, Kawachi I, Williams MA, Hu FB. 2013. Racial disparities in short sleep duration by occupation and industry. Am. J. Epidemiol. 178(9):1442–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Knight KM, Rafferty JA. 2010. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am. J. Public Health 100(5):933–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James SA, Fowler-Brown A, Raghunathan TE, Van Hoewyk J. 2006. Life-course socioeconomic position and obesity in African American women: the Pitt County Study. Am. J. Public Health 96:554–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James SA, Keenan NL, Strogatz DS, Browning SR, Garrett JM. 1992. Socioeconomic status, John Henryism, and blood pressure in black adults: the Pitt County Study. Am. J. Epidemiol. 135(1):59–67 [DOI] [PubMed] [Google Scholar]
- James SA, Strogatz DS, Wing SB, Ramsey DL. 1987. Socioeconomic status,John Henryism, and hypertension in blacks and whites. Am. J. Epidemiol. 126(4):664–73 [DOI] [PubMed] [Google Scholar]
- Johnson DA, Billings ME, Hale L.2018.Environmental determinants of insufficient sleep and sleep disorders: implications for population health. Environ. Epidemiol. 5:61–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SE, Richeson JA, Finkel EJ. 2011. Middle class and marginal? Socioeconomic status, stigma, and self-regulation at an elite university. J. Pers. Soc. Psychol. 100:838–52 [DOI] [PubMed] [Google Scholar]
- Joseph RP, Ainsworth BE, Keller C, Dodgson JE. 2015. Barriers to physical activity among African American women: an integrative review of the literature. Women Health 55:679–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kallem S, Carroll-Scott A, Rosenthal L, Chen E, Peters SM, et al. 2013. Shift-and-persist: a protective factor for elevated BMI among low socioeconomic status children. Obesity 21:1759–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw KN, Lewis TT, Diez Roux AV, Jenny NS, Liu K, et al. 2016. Self-reported experiences of discrimination and inflammation among men and women: the Multi-Ethnic Study of Atherosclerosis. Health Psychol. 35:343–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kittleson MM, Meoni LA, Wang NY, Chu AY, Ford DE, Klag MJ. 2006. Association of childhood socioeconomic status with subsequent coronary heart disease in physicians. Arch. Intern. Med. 166(21):2356–61 [DOI] [PubMed] [Google Scholar]
- Kraus MW, Piff PK, Mendoza-Denton R, Rheinschmidt ML, Keltner D. 2012. Social class, solipsism, and contextualism: how the rich are different from the poor. Psychol. Rev. 119:546–72 [DOI] [PubMed] [Google Scholar]
- Krishnan S, Cozier YC, Rosenberg L, Palmer JR. 2010. Socioeconomic status and incidence of type 2 diabetes: results from the Black Women’s Health Study. Am. J. Epidemiol. 171:564–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuh D, Ben Shlomo Y. 2004. A Life Course Approach to Chronic Diseases Epidemiology. New York: Oxford Univ. Press [Google Scholar]
- Langhout RD, Rosselli F, Feinstein J. 2007. Assessing classism in academic settings. Rev. High. Educ.30:145–84 [Google Scholar]
- Levine CS, Atkins AH, Waldfogel HB, Chen E. 2016. Views of a good life and allostatic load: physiological correlates of theories of a good life depend on the socioeconomic context. Self Identity 15:536–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine CS, Hoffer LC, Chen E. 2017. Moderators of the relationship between frequent family demands and inflammation among adolescents. Health Psychol. 36:493–501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine CS, Markus HR, Austin MA, Chen E, Miller GE. 2019. Students of color show health advantages when they attend schools that emphasize the value of diversity. PNAS 116:6013–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Everson-Rose SA, Powell LH, Matthews KA, Brown C, et al. 2006. Chronic exposure to everyday discrimination and coronary artery calcification in African American women: the SWAN Heart Study. Psychosom. Med. 68:362–68 [DOI] [PubMed] [Google Scholar]
- Lidfeldt J, Li TY, Hu FB, Manson JE, Kawachi I. 2007. A prospective study of childhood and adult socioeconomic status and incidence of type 2 diabetes in women. Am. J. Epidemiol. 165:882–89 [DOI] [PubMed] [Google Scholar]
- Loef M, Walach H. 2012. The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev. Med. 55:163–70 [DOI] [PubMed] [Google Scholar]
- Loucks EB, Pilote L, Lynch JW, Richard H, Almeida ND, et al. 2010. Life course socioeconomic position is associated with inflammatory markers: the Framingham Offspring Study. Soc. Sci. Med. 71:187–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manczak EM, DeLongis A, Chen E. 2016. Does empathy have a cost? Diverging psychological and physiological effects within families. Health Psychol. 35:211–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markus HR, Ryff CD, Curhan KB, Palmersheim K. 2004. In their own words: well-being at midlife among high school and college educated adults. In How Healthy Are We? A National Study of Well-Being at Midlife, ed. Brim OG, Ryff CD, Kessler RC, pp. 273–319. Chicago: Univ. Chicago Press [Google Scholar]
- Martire LM, Stephens MAP. 2003. Juggling parent care and employment responsibilities: the dilemmas of adult daughter caregivers in the workforce. Sex Roles 48(3–4):167–73 [Google Scholar]
- Matthews KA, Gallo LC. 2011. Psychological perspectives on pathways linking socioeconomic status and physical health. Annu. Rev. Psychol. 62:501–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Gallo LC, Taylor SE. 2010. Are psychosocial factors mediators of socioeconomic status and health connections? A progress report and blueprint for the future. Ann. N. Y. Acad. Sci. 1186:146–73 [DOI] [PubMed] [Google Scholar]
- Mays VM, Cochran SD, Barnes NW. 2007. Race, race-based discrimination, and health outcomes among African Americans. Annu. Rev. Psychol. 58:201–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS, Seeman T. 1999. Protective and damaging effects of mediators of stress: elaborating and testing the concepts of allostasis and allostatic load. Ann. N. Y. Acad. Sci. 896:30–47 [DOI] [PubMed] [Google Scholar]
- Melamed S, Shirom A, Toker S, Berliner S, Shapira I. 2006. Burnout and risk of cardiovascular disease: evidence, possible causal paths, and promising research directions. Psychol. Bull. 132:327–53 [DOI] [PubMed] [Google Scholar]
- Melchior M, Berkman LF, Kawachi I, Krieger N, Zins M, et al. 2006. Lifelong socioeconomic trajectory and premature mortality (35–65 years) in France: findings from the GAZEL Cohort Study. J. Epidemiol. Community Health 60:937–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezuk B, Rafferty JA, Kershaw KN, Hudson D, Abdou CM, et al. 2010. Reconsidering the role of social disadvantage in physical and mental health: stressful life events, health behaviors, race, and depression. Am. J. Epidemiol. 172(11):1238–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, Cole SW. 2009. Health psychology: developing biologically plausible models linking the social world and physical health. Annu. Rev. Psychol. 60:501–24 [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Sze J, Marin T, Arevalo JM, et al. 2008. A functional genomic fingerprint of chronic stress in humans: blunted glucocorticoid and increased NF-κB signaling. Biol. Psychiatry 64(4):266–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, Yu T, Brody GH. 2020. Youth who achieve upward socioeconomic mobility display lower psychological distress but higher metabolic syndrome rates as adults: prospective evidence from Add Health and MIDUS. J. Am. Heart Assoc. 9:e015698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Cohen S, Janicki-Deverts D, Brody GH, Chen E.2016a. Viral challenge reveals further evidence of skin-deep resilience in African Americans from disadvantaged backgrounds. Health Psychol. 35:1225–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Engen PA, Gillevet PM, Shaikh M, Sikaroodi M, et al. 2016b. Lower neighborhood socioeconomic status associated with reduced diversity of the colonic microbiota in healthy adults. PLOS ONE 11:e0148952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Yu T, Chen E, Brody GH. 2015. Self-control forecasts better psychosocial outcomes but faster epigenetic aging in low-SES youth. PNAS 112(33):10325–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittal C, Griskevicius V, Simpson JA, Sung S, Young ES. 2015. Cognitive adaptations to stressful environments: when childhood adversity enhances adult executive function. J. Pers. Soc. Psychol. 109:604–21 [DOI] [PubMed] [Google Scholar]
- Moody DLB, Chang YF, Pantesco EJ, Darden TM, Lewis TT, et al. 2019. Everyday discrimination prospectively predicts blood pressure across 10 years in racially/ethnically diverse midlife women: Study of Women’s Health Across the Nation. Ann. Behav. Med. 53:608–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers HF. 2009. Ethnicity- and socio-economic status-related stresses in context: an integrative review and conceptual model. J. Behav. Med. 32:9–19 [DOI] [PubMed] [Google Scholar]
- Na-Ek N, Demakakos P. 2017. Social mobility and inflammatory and metabolic markers at older ages: the English Longitudinal Study of Ageing. J. Epidemiol. Community Health 71:253–60 [DOI] [PubMed] [Google Scholar]
- Nomaguchi KM, Bianchi SM. 2004. Exercise time: gender differences in the effects of marriage, parenthood, and employment. J. Marriage Fam. 66:413–30 [Google Scholar]
- Ostrove J, Long SM. 2007. Social class and belonging: implications for college adjustment. Rev. High. Educ. 30:363–89 [Google Scholar]
- Pascarella ET, Pierson CT, Wolniak GC, Terenzini PT. 2004. First-generation college students: additional evidence on college experiences and outcomes. J. High. Educ. 75:249–84 [Google Scholar]
- Pearson Q 2008. Role overload, job satisfaction, leisure satisfaction, and psychological health among employed women. J. Couns. Dev. 86:57–63 [Google Scholar]
- Pena PA, Perez-Diaz I, Pulido-Ayala AK, Osorio-Landa HK, Lopez-Navarro JM, et al. 2019. Association of grit scores with treatment adherence and biomarkers in patients with type 2 diabetes. JAMA Netw. Open 2:e1911476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penley JA, Tomaka J, Wiebe JS.2002.The association of coping to physical and psychological health outcomes: a meta-analytic review. J. Behav. Med 25(6):551–603 [DOI] [PubMed] [Google Scholar]
- Phillips LT, Stephens NM, Townsend SSM, Goudeau S. 2020. Access is not enough: Cultural mismatch persists to limit first-generation students’ opportunities for achievement throughout college. J. Pers. Soc. Psychol. 119:1112–31 [DOI] [PubMed] [Google Scholar]
- Pollak SD, Kistler DJ. 2002. Early experience is associated with the development of categorical representations for facial expressions of emotion. PNAS 99:9072–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollitt RA, Rose KM, Kaufman JS. 2005. Evaluating the evidence for models of life course socioeconomic factors and cardiovascular outcomes: a systematic review. BMC Public Health 5:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell ND, Sloan EK, Bailey MT, Arevalo JMG, Miller GE, et al. 2013. Social stress up-regulates inflammatory gene expression in the leukocyte transcriptome via beta-adrenergic induction of myelopoiesis. PNAS 110:16574–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prag P, Richards L. 2019. Intergenerational social mobility and allostatic load in Great Britain. J. Epidemiol. Community Health 73:100–5 [DOI] [PubMed] [Google Scholar]
- Pudrovska T, Anikputa B. 2013. Early-life socioeconomic status and mortality in later life: an integration of four life-course mechanisms. J. Gerontol. Ser. B 69:451–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravelli ACJ, van der Meulen JHP, Michels RPJ, Osmond C, Barker DJP, et al. 1998. Glucose tolerance in adults after prenatal exposure to famine. Lancet 9097:173–77 [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. 2019. Neighborhoods and violent crime. In Community Health Equity, ed. De Maio F, Shah RC, Mazzeo J, Ansell DA, pp. 282–303. Chicago: Univ. Chicago Press [Google Scholar]
- Savelieva K, Pulkki-Raback L, Jokela M, Kubzansky LD, Elovainio M, et al. 2017. Intergenerational transmission of socioeconomic position and ideal cardiovascular health: 32-year follow-up study. Health Psychol. 36:270–79 [DOI] [PubMed] [Google Scholar]
- Schreier HM, Chen E. 2013. Socioeconomic status and the health of youth: a multilevel, multidomain approach to conceptualizing pathways. Psychol. Bull. 139(3):606–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellers SL, Neighbors HW, Zhang R, Jackson JJ. 2012. The impact of goal-striving stress on physical health of White Americans, African Americans, and Caribbean Blacks. Ethn. Dis. 22:21–28 [PubMed] [Google Scholar]
- Shultz KS, Wang M, Olson DA. 2010. Role overload and underload in relation to occupational stress and health. Stress Health 26:99–111 [Google Scholar]
- Siegrist J 2010. Effort-reward imbalance at work and cardiovascular diseases.Int. J. Occup. Med. Environ. Health 23:279–85 [DOI] [PubMed] [Google Scholar]
- Siegrist J, Li J. 2016. Associations of extrinsic and intrinsic components of work stress with health: a systematic review of evidence on the effort-reward imbalance model. Int. J. Environ. Res. Public Health 13(4):432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sjostrand M, Eriksson JW. 2009. Neuroendocrine mechanisms in insulin resistance. Mol. Cell. Endocrinol. 297:104–11 [DOI] [PubMed] [Google Scholar]
- Slopen N, Lewis TT, Williams DR. 2016. Discrimination and sleep: a systemic review. Sleep Med. 18:88–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: Natl. Acad. Press; [PubMed] [Google Scholar]
- Smith BT, Lynch JW, Fox CS, Harper S, Abrahamowicz M, et al. 2011. Life-course socioeconomic position and type 2 diabetes mellitus: the Framingham Offspring Study. Am. J. Epidemiol. 173:438–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith TW, Ruiz JM, Uchino BN. 2000. Vigilance, active coping, and cardiovascular reactivity during social interaction in young men. Health Psychol. 19(4):382–92 [DOI] [PubMed] [Google Scholar]
- Smith WA, Hung M, Franklin JD. 2011. Racial battle fatigue and the miseducation of Black men: racial microaggressions, societal problems, and environmental stress. J. Negro Educ. 80:63–82 [Google Scholar]
- Sominsky L, Spencer SJ. 2014. Eating behavior and stress: a pathway to obesity. Front. Psychol. 5:434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens MAP, Townsend AL, Martire LM, Druley JA. 2001. Balancing parent care with other roles: interrole conflict of adult daughter caregivers. J. Gerontol. Ser. B 56(1):24–34 [DOI] [PubMed] [Google Scholar]
- Stephens NM, Hamedani MG, Destin M. 2014. Closing the social-class achievement gap: a difference-education intervention improves first-generation students’ academic performance and all students’ college transition. Psychol. Sci. 25:943–53 [DOI] [PubMed] [Google Scholar]
- Stephens NM, Markus HR, Phillips LT. 2014. Social class culture cycles: how three gateway contexts shape selves and fuel inequality. Annu. Rev. Psychol. 65:611–34 [DOI] [PubMed] [Google Scholar]
- Stephens NM, Townsend SSM, Dittmann AG. 2019. Social-class disparities in higher education and professional workplaces: the role of cultural mismatch. Curr. Dir. Psychol. Sci. 28:67–73 [Google Scholar]
- Stephens NM, Townsend SSM, Markus HR, Phillips LT. 2012. A cultural mismatch: Independent cultural norms produce greater increases in cortisol and more negative emotions among first-generation college students. J. Exp. Soc. Psychol. 48:1389–93 [Google Scholar]
- Stetler C, Chen E, Miller GE. 2006.Written disclosure of experiences with racial discrimination and antibody response to an influenza vaccine. Int. J. Behav. Med. 13:60–68 [DOI] [PubMed] [Google Scholar]
- Stringhini S, Batty GD, Bovet P, Shipley MJ,Marmot MG, et al. 2013. Association of lifecourse socioeconomic status with chronic inflammation and type 2 diabetes risk: the Whitehall II prospective cohort study. PLOS Med. 10:e1001479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringhini S, Zaninotto P, Kumari M, Kivimaki M, Lassale C, Batty GD. 2018. Socio-economic trajectories and cardiovascular disease mortality in older people: the English Longitudinal Study of Ageing. Int. J. Epidemiol. 47:36–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suglia SF, Koenen KC, Boynton-Jarrett R, Chan PS, Clark CJ, et al. 2018. Childhood and adolescent adversity and cardiometabolic outcomes: a scientific statement from the American Heart Association. Circulation 137:e15–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tesser A 1988. Toward a self-evaluation maintenance model of social behavior. Adv. Exp. Soc. Psychol. 21:181–227 [Google Scholar]
- Tiikkaja S, Hemstrom O. 2008. Does intergenerational social mobility among men affect cardiovascular mortality? A population-based register study from Sweden. Scand. J. Public Health 36:619–28 [DOI] [PubMed] [Google Scholar]
- Tiikkaja S, Hemstrom O, Vagero D. 2009. Intergenerational class mobility and cardiovascular mortality among Swedish women: a population-based register study. Soc. Sci. Med. 68:733–39 [DOI] [PubMed] [Google Scholar]
- Torres SJ, Nowson CA. 2007. Relationship between stress, eating behavior, and obesity. Nutrition 23:887–94 [DOI] [PubMed] [Google Scholar]
- Tryon MS, Carter CS, DeCant R, Laugero KD. 2013. Chronic stress exposure may affect the brain’s response to high calorie food cues and predispose to obesogenic eating habits. Physiol. Behav. 120:233–42 [DOI] [PubMed] [Google Scholar]
- Tucker JM, Welk GJ, Beyler NK. 2011. Physical activity in U.S. adults: compliance with the physical activity guidelines for Americans. Am. J. Prev. Med. 40:454–61 [DOI] [PubMed] [Google Scholar]
- Van Dyke ME, Vaccarino V, Dunbar SB, Pemu P, Gibbons GH, et al. 2017. Socioeconomic status discrimination and C-reactive protein in African American and White adults. Psychoneuroendocrinology 82:9–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Laar C, Bleeker D, Ellemers N, Meijer E. 2014. Ingroup and outgroup support for upward mobility: divergent responses to ingroup identification in low status groups. Eur. J. Soc. Psychol. 44:563–77 [Google Scholar]
- Walker RE, Keane CR, Burke JG. 2010. Disparities and access to healthy food in the United States: a review of food deserts literature. Health Place 16:876–84 [DOI] [PubMed] [Google Scholar]
- Warburton DER, Nicol CW, Bredin SSD. 2006. Health benefits of physical activity: the evidence. Can. Med. Assoc. J. 174:801–09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitaker KM, Everson-Rose SA, Pankow JS, Rodriguez CJ, Lewis TT, et al. 2017. Experiences of discrimination and incident type 2 diabetes mellitus. Am. J. Epidemiol. 186:445–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. 2009. Discrimination and racial disparities in health: evidence and needed research. J. Behav. Med. 32:20–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA, Leavell J, Collins C. 2010. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann. N. Y. Acad. Sci. 1186:69–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Priest N, Anderson NB. 2016. Understanding associations among race, socioeconomic status, and health: patterns and prospects. Health Psychol. 35(4):407–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson AE, Shuey KM. 2016. Life course pathways of economic hardship and mobility and midlife trajectories of health. J. Health Soc. Behav. 57:407–22 [DOI] [PubMed] [Google Scholar]
- Wright RJ, Steinbach SF. 2001. Violence: an unrecognized environmental exposure that may contribute to greater asthma morbidity in high risk inner-city populations. Environ. Health Perspect. 109:1085–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young ES, Griskevicius V, Simpson JA, Waters TEA, Mittal C. 2018. Can an unpredictable childhood environment enhance working memory? Testing the sensitized-specialization hypothesis. J. Pers. Soc. Psychol. 114:891–908 [DOI] [PubMed] [Google Scholar]


