Abstract
Coronavirus disease 2019 (COVID-19) infection is a recent pandemic. Healthcare workers (HCW) are at high risk of acquiring the infection and transmitting it to others. Seroprevalence for COVID-19 among HCW varies between countries, hospitals in the same country and even among different departments in the same hospital. In this study, we aim to determine the prevalence of severe acute respiratory syndrome coronavirus 2 antibodies and the seroconversion among the HCW in our hospital. A total of 203 HCW were included. The rate of conversion to seropositive was 19.7% in total, with a rate of 13.4% in female versus 25% in male. The seropositivity in the House keeping group was 83%, followed by 45% in the COVID Floor while the seropositivity in the Anesthesia was 4% and the Infection Control 0%. The highest seropositivity rate in the COVID floor, and in the intensive care unit was explained by the long time spent with the patients. While in the inhalation team and the anesthesia, the lower rates of seropositivity was due to the N95 mask wearing the whole time. Seropositivity for COVID-19 in HCW is a major public health concern. Policies should be implemented to better protect HCWs.
Keywords: COVID-19, healthcare workers, seroconversion, seropositivity
1. Introduction
Coronavirus disease 2019 (COVID-19) infection is a recent pandemic, known to cause severe respiratory illness, with more than 600 million people infected all over the world, and around 6.5 million people dead as of October, 2022.[1] It has a wide clinical spectrum. COVID-19 patients can be asymptomatic. When symptoms are present, they range from minimal respiratory symptoms to life threatening respiratory failure.[2] Health care setting transmission and infection remains is a major public health issue.[3] Asymptomatic cases play a role in the silent transmission of COVID-19 and probably contributed to the start and perpetuation of the pandemic.[4] Healthcare workers (HCW) are at high risk of acquiring the infection and transmitting it to others.[3] In the era before vaccine or medications became available, reports of HCW infected with COVID-19 showed a prevalence of around 11% by polymerase chain reaction, and 7% by serology testing.[5] Preexisting antibodies for COVID-19 affect the clinical response during an infection.[2] Antibody titers remain several months after an infection.[6] COVID-19 produces detectable level of antibodies. However, it is not clear whether these levels can produce adequate immunity, to which extent, and for how long.[1] In a study conducted in HCW in Oxford university hospitals, UK, the presence of IgG antibodies was associated with a reduced risk of COVID-19 reinfection in the following 6 months.[1] Seroprevalence for COVID-19 among HCW range from 0% to 45.3%.[6] This percentage is different across the countries and among different centers in the same country. Studies in the USA report the rate for prevalence among HCW to be between 6% and 35.8%.[7–13] Percentages of seroprevalence are variable and depends on many factors. No study was conducted in the Lebanese hospitals on seroprevalence rates among the HCW. In this study, we report the prevalence of COVID-19 antibodies and the seroconversion rate among the HCW in different departments in the hospital in the beginning of the pandemic.
2. Materials and Methods
The study was conducted in the year 2020 before any vaccination or established treatment for COVID-19 was available. The study was approved by the Lebanese American University Institutional Review Board IRB #: LAUMCRH.RH1.16/Apr/2020. This systematic study aimed to determine the prevalence of severe acute respiratory syndrome coronavirus 2 antibodies and the seroconversion among the HCW within our hospital. Participants included in the study were HCW at the Lebanese American University Medical Center, Beirut, Lebanon dealing with COVID-19 patients or working in COVID-19 units. All participants signed a consent form, and data was obtained anonymously. Two blood tests were performed for the participants included, on the beginning of the study and 6 months later. Blood tests consisted of a serum anti severe acute respiratory syndrome coronavirus 2 antibodies levels using the Roche test. Data was collected and analyzed.
3. Results
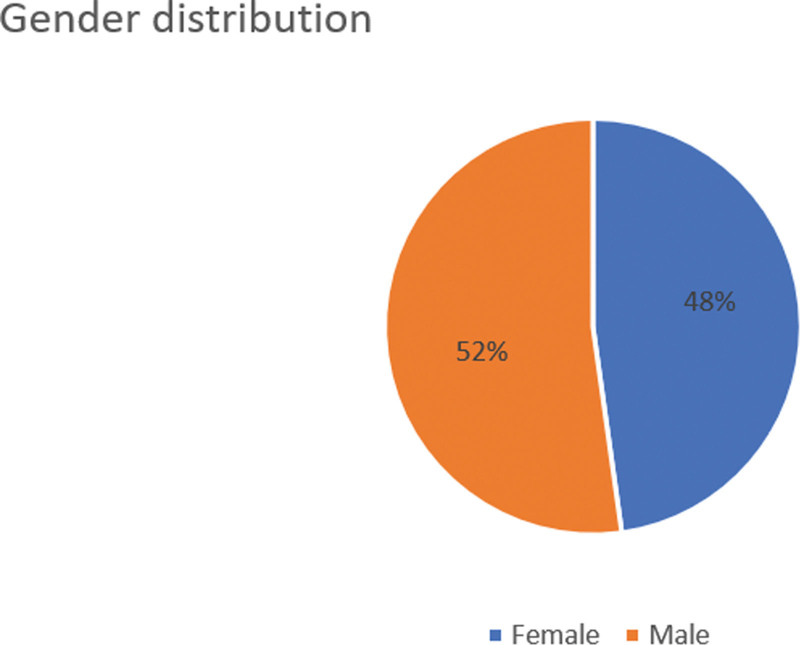
A total of 203 HCW from different specialties were included in the study (Table 1 and Fig. 1). The majority were registered nurses, practical nurses or medical doctors.
Table 1.
Number of healthcare workers in each specialty.
| Registered nurse | 90 |
|---|---|
| Practical nurse | 43 |
| Laboratory technician | 9 |
| Infection control | 1 |
| Medical doctor | 37 |
| Transporter | 13 |
| Secretary | 4 |
| House keeper | 6 |
| Total | 203 |
Figure 1.
Gender Distribution for Healthcare Workers.
Table 2 shows the distribution of the HCW among different areas in the hospital, with the highest numbers being in the Emergency Room or in the Operating Room.
Table 2.
Distribution of the Healthcare Workers among different areas in the hospital.
| COVID floor | 20 |
|---|---|
| Laboratory | 11 |
| Infection control | 1 |
| Emergency | 41 |
| Inhalation | 10 |
| Anesthesia | 26 |
| Intensive care unit | 26 |
| Operation room | 39 |
| Dialysis | 11 |
| COVID floor physicians | 12 |
| House keeper | 6 |
| Total | 203 |
The rate of conversion to seropositive was 19.7% in total, with a rate of 13.4 % in female versus 25% in male (Table 3).
Table 3.
Rate of conversion to seropositive by gender.
| Gender | Number | Converted to seropositive (Number) | Percentage |
|---|---|---|---|
| Female | 97 | 13 | 13.40% |
| Male | 106 | 27 | 25% |
| Total | 203 | 40 | 19.70% |
Seropositive rate is variable from 1 area to another in the hospital. For example, the seropositivity in the House keeping group was 83%, followed by 45 % in the COVID Floor compared to the seropositivity in the Anesthesia and Infection Control (4% and 0%) (Table 4). If we exclude the housekeeping staff, the prevalence rate become 17.7%.
Table 4.
Rate of seropositivity per different areas in the hospital.
| Healthcare workers | Number | Seropositive converted | Percentage |
|---|---|---|---|
| COVID floor | 20 | 9 | 45% |
| Laboratory | 11 | 1 | 9% |
| Infection control | 1 | 0 | 0% |
| Emergency | 41 | 8 | 19% |
| Inhalation | 10 | 1 | 10% |
| Anesthesia | 26 | 1 | 4% |
| Intensive care unit | 26 | 6 | 23% |
| Operation room | 39 | 5 | 13% |
| Dialysis | 11 | 2 | 18% |
| COVID floor physicians | 12 | 2 | 17% |
| House keeper | 6 | 5 | 83% |
| Total | 203 | 40 | 19.70% |
4. Discussion
As we have obtained from our data, 19.7% of our HCW converted to seropositive. These rates varied with gender and job location and position. The highest rates were in the housekeeping division and the COVID Floor staff.
Many studies were conducted worldwide to evaluate the seroconversion rate of the HCW for COVID-19. Table 5 summarizes all studies with the different rates of seropositivity among HCW.[1,3, 6–13, 17–31, 45–66]
Table 5.
Rate of seropositivity among Healthcare workers in different countries worldwide.
| Study | City/Country | Year of data collection | Sample size (N) | Setting | Seropositive rate (%) |
|---|---|---|---|---|---|
| Moscola et al, 2020[12] | New York, USA | 2020 | 40329 | Primary care facilities and hospitals | 13.7 |
| Jeremias et al, 2020[7] | New York/USA | 2020 | 1699 | Hospitals | 9.8 |
| Houlihan et al, 2020[3] | London/UK | 2020 | 181 | Hospitals | 45 |
| Poulikakos et al, 2020[20] | England/UK | 2020 | 281 | Hospitals | 6 |
| Steensels et al, 2020[21] | Genk/Belgium | 2020 | 3056 | Hospitals | 6 |
| Blairon et al, 2020[22] | Brussels/Belgium | 2020 | 1485 | Hospitals | 14.6 |
| Pallett et al, 2020[23] | London/UK | 2020 | 6440 | Hospitals | 18 |
| Korth et al, 2020[24] | Essen/Germany | 2020 | 316 | Hospitals | 1.6 |
| Martin et al, 2020[25] | Brussels/Belgium | 2020 | 326 | Hospitals | 11 |
| Amendola et al, 2020[26] | Milan/Italy | 2020 | 547 | Hospitals | 5 |
| Self et al, 2020[9] | USA | 2020 | 3248 | Hospitals | 6 |
| Grant et al, 2020[17] | London/UK | 2020 | 2004 | Primary care facilities and hospitals | 31 |
| Mughal et al, 2020[8] | New Jersey/USA | 2020 | 121 | Hospitals | 8 |
| Hunter et al, 2020[27] | Indiana/USA | 2020 | 690 | Hospitals | 1.4 |
| Plebani et al, 2020[28] | Veneto Region/ Italy | 2020 | 8285 | Primary care facilities and hospitals | 4.6 |
| Mansour et al, 2020[11] | New York/ USA | 2020 | 285 | Hospitals | 35 |
| Sotgiu et al, 2020[19] | Milan/Italy | 2020 | 202 | Hospitals | 14 |
| Garcia-Basteiro et al, 2020[29] | Barcelona/Spain | 2020 | 578 | Hospitals | 9 |
| Sydney et al, 2020[13] | New York/USA | 2020 | 1700 | Hospitals | 19 |
| Khalil et al, 2020[30] | London/UK | 2020 | 190 | Hospitals | 21 |
| Stubblefield et al, 2021[10] | Tennessee/USA | 2020 | 249 | Hospitals | 7.6 |
| Lackermair et al, 2020 | Bavaria/Germany | 2020 | 151 | Primary care facilities | 2.6 |
| Paderno et al, 2020[32] | Brescia/Italy | 2020 | 58 | Hospitals | 8.6 |
| Kassem et al, 2020[33] | Cairo/Egypt | 2020 | 74 | Hospitals | 12 |
| Olalla et al, 2020[34] | Marbella/Spain | 2020 | 498 | Hospitals | 1.8 |
| Iversen et al, 2020[16] | Denmark | 2020 | 28792 | Hospitals | 4 |
| Hains et al, 2020[35] | Indiana/USA | 2020 | 25 | Hospitals | 44 |
| Solodky et al, 2020[36] | Lyon/France | 2020 | 244 | Hospitals | 5 |
| Behrens et al, 2020[37] | Hannover/Germany | 2020 | 217 | Hospitals | 1.4 |
| Brandstetter et al, 2020[38] | Regensburh/Germany | 2020 | 201 | Hospitals | 10.9 |
| Fusco et al, 2020[39] | Naples/Italy | 2020 | 115 | Hospitals | 0.9 |
| Lahner et al, 2020[40] | Rome/Italy | 2020 | 2115 | Hospitals | 0.4 |
| Schmidt et al, 2020[41] | Hessisch Oldendorf/ Germany | 2020 | 406 | Hospitals | 2.9 |
| Xu et al, 2020[42] | China | 2020 | 4384 | Hospitals | 1.8 |
| Zhao et al, 2020[43] | Beijing/China | 2020 | 276 | Hospitals | 10 |
| Barallat et al, 2020[44] | Barcelona/ Spain | 2020 | 7563 | Primary care facilities and hospitals | 10 |
| Kammon et al, 2020[45] | Alzintan/Libya | 2020 | 77 | Hospitals | 0.6 |
| Xiong et al, 2020[46] | Wuhan. China | 2020 | 797 | Hospitals | 4.4 |
| Galán et al, 2020[47] | Madrid/Spain | 2020 | 2590 | Hospitals | 31.6 |
| Nakamura et al, 2021[48] | Iwate/Japan | 2020 | 1000 | Hospitals | 0.4 |
| Psichogiou et al, 2020[49] | Athens/Greece | 2020 | 1495 | Hospitals | 1 |
| Chibwana et al, 2020[50] | Blantyre/Malawi | 2020 | 500 | Hospitals | 16.8 |
| Tosato et al, 2020[51] | Padova/Italy | 2020 | 133 | Hospitals | 4.5 |
| Paradiso et al, 2021[52] | Bari/Italy | 2020 | 606 | Hospitals | 1.2 |
| Fujita et al, 2020[53] | Kyoto/Japan | 2020 | 92 | Hospitals | 5.4 |
| Sikora et al, 2020[54] | UK | 2020 | 161 | Cancer centers | 7.5 |
| Rudberg et al, 2020[18] | Stockholm/Sweden | 2020 | 410 | Hospitals | 19 |
| Shields et al, 2020[55] | Birmingham/UK | 2020 | 516 | Hospitals | 24 |
| Takita et al, 2020[56] | Tokyo/Japan | 2020 | 55 | Primary care facilities | 9 |
| Eyre et al, 2020[57] | UK | 2020 | 9958 | 10.7 | |
| Lidstrom et al, 2020[58] | Sweden | 2020 | 8679 | 6.6 | |
| Jones et al, 2021[59] | UK | 2020 | 6858 | 9.3 | |
| Calcagno et al, 2021[60] | Italy | 2020 | 5444 | 6.9 | |
| Delmas et al, 2021[61] | France | 2020 | 4600 | 11.5 | |
| De Carlo et al, 2020[4] | Italy | 2020 | 3242 | 1.9 | |
| Brant-Zawadzki et al, 2020[62] | USA | 2020 | 2932 | 1.1 | |
| Racine-Brzostek et al, 2020[63] | USA | 2020 | 2274 | 35.4 | |
| Dimcheff et al, 2020[64] | USA | 2020 | 1476 | 4.9 | |
| Papasavas et al, 2021[6] | Connecticut/USA | 2020 | 6863 | 6.3 | |
| Mostafa et al, 2021[65] | Cairo/Egypt | 2020 | 4040 | University healthcare facilities | 4.4 |
| Nicholson et al, 2021[66] | San Diego/USA | 2020 | 11993 | Hospitals | 0.94 |
| Lumley et al, 2021[1] | UK | 2020 | 12541 | Hospitals | 10 |
A recent meta-analysis of seroprevalence in HCWs collected 127480 HCW from 49 studies.[14] The overall seroprevalence rate was estimated at 8.7%. Many factors were associated with seropositivity as male gender, race, working in a COVID-19 unit, and working in areas with a shortage of personal protective equipment (PPE). Another meta-analysis including 25 studies found an average seroprevalence of 8%.[15] Similarly, studies found a significant higher probability of positive antibody tests in HCW working in a COVID unit.[16–18]
Our study showed an average rate of seroprevalence of 19.7 % which is higher than the rates found in the 2 meta-analysis. This was mainly due to the outbreak in the house keeping department with a rate of 84% in the housekeeping. To note here that the housekeeping team live in the same house, so the outbreak might be community related more than hospital acquired.
If we remove the outbreak in the housekeeping division, the total prevalence in our study will drop to 17.7% and will be the highest in the COVID floor, and in the intensive care unit. This result is similar to other studies like in Denmark, the highest rate of seropositivity was among frontline care workers.[16] In another study, the highest rate was among patient care support.[7] One of the factors that can interfere with the rate of conversion is the time spend with the patient, this is why the rate is higher in departments where there is prolonged duration of contact with the patient, and possible respiratory procedures creating contagious aerosols.
Men are more commonly seropositive than female, 25% versus 13.4%. Other studies found that COVID antibodies are more frequently detectable in male gender.[9,16,19] This could be explained by the difference in behavior, the higher ACE 2 receptors, and hormonal differences as reported in the literature.[9,16,19]
Other factors reported in the literature to be associated with seropositivity were black, Asian and Hispanic, healthcare assistants and shortage of PPEs. A study conducted in Egypt, showed more than 50% of the HCW had occupational safety concern at their workplace, and around 60% of them were not compliant with the PPE use.[67]
With the financial crisis in our country, hospitals in Lebanon suffered huge shortage in the medical supplies and in particular the PPEs. However, our hospital used strict Infection Control policies, PPEs were available to all. Negative pressure rooms were created at the beginning of the COVID pandemic with frequent education sessions and audits. Therefore, it is clear that personal effort of each healthcare worker to comply with the policies will protect him in the setting of a pandemic.
The inhalation team (respiratory therapist) and the anesthesia had the lower rates of seropositivity. This is possibly because these were the only teams provided N95 Masks at all times since the beginning of the pandemic, being the group at the highest risk of exposure.
These infection control measures are of major importance to prevent the infection of HCW, and their possible need of hospitalization and treatment.[68]
The study was conducted in 1 hospital in Lebanon, which makes the data limited. However, the importance of this data remains for infection control purposes among the hospital, and this is of major importance during the COVID-19 pandemic.
Another limitation is the period of time of the study, which is before the era of the vaccination. However, data is still important since we witness actually variants of the virus, that makes the vaccine efficacy questionable.
5. Conclusion
Seropositivity for COVID-19 in HCW is a major public health concern. Policies should be implemented to better protect HCWs. In addition, HCW surveillance is of major importance in a hospital setting to protect both HCW and patients from nosocomial transmission.
Author contributions
Conceptualization: Mariana Helou, Jonathan Mina, Jacques Mokhbat, Rola Husni.
Data curation: Mariana Helou, Sanaa Zoghbi, Nour El Osta, Jonathan Mina, Jacques Mokhbat, Rola Husni.
Formal analysis: Mariana Helou, Jonathan Mina, Jacques Mokhbat, Rola Husni.
Funding acquisition: Mariana Helou.
Investigation: Rola Husni.
Methodology: Mariana Helou, Rola Husni.
Project administration: Mariana Helou, Rola Husni.
Resources: Jonathan Mina, Rola Husni.
Supervision: Rola Husni.
Validation: Mariana Helou, Rola Husni.
Visualization: Rola Husni.
Writing – original draft: Mariana Helou, Nour El Osta, Rola Husni.
Writing – review & editing: Mariana Helou, Rola Husni.
Abbreviations:
- COVID-19
- coronavirus disease 2019
- HCW
- healthcare workers
- PPE
- personal protective equipment
The authors have no funding and conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].How to cite this article: Helou M, Zoghbi S, El Osta N, Mina J, Mokhbat J, Husni R. COVID-19 infection and seroconversion rates in healthcare workers in Lebanon: An observational study. Medicine 2023;102:17(e32992).
Contributor Information
Mariana Helou, Email: mariana.helou@lau.edu.lb.
Sanaa Zoghbi, Email: sanaa.zoghbi@laumcrh.com.
Nour El Osta, Email: nour.osta@lau.edu.
Jonathan Mina, Email: jonathan.mina@lau.edu.
Jacques Mokhbat, Email: Jacques.mokhbat@lau.edu.lb.
References
- [1].Lumley SF, O’Donnell D, Stoesser NE, et al. Antibody status and incidence of SARS-CoV-2 infection in health care workers. N Engl J Med. 2021;384:533–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Jackson-Thompson BM, Goguet E, Laing ED, et al. Prospective assessment of SARS-CoV-2 seroconversion (PASS) study: an observational cohort study of SARS-CoV-2 infection and vaccination in healthcare workers. BMC Infect Dis. 2021;21:544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Houlihan CF, Vora N, Byrne T, et al. Pandemic peak SARS-CoV-2 infection and seroconversion rates in London frontline health-care workers. Lancet. 2020;396:e6–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].De Carlo A, Lo Caputo S, Paolillo C, et al. SARS-COV-2 serological profile in healthcare professionals of a Southern Italy Hospital. Int J Environ Res Public Health. 2020;17:9324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Gómez-Ochoa SA, Franco OH, Rojas LZ, et al. COVID-19 in health-care workers: a living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am J Epidemiol. 2021;190:161–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Papasavas P, Olugbile S, Wu U, et al. Seroprevalence of SARS-CoV-2 antibodies, associated epidemiological factors and antibody kinetics among healthcare workers in Connecticut. J Hosp Infect. 2021;114:117–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Jeremias A, Nguyen J, Levine J, et al. Prevalence of SARS-CoV-2 infection among health care workers in a tertiary community hospital. JAMA Intern Med. 2020;180:1707e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Mughal MS, Kaur IP, Patton CD, et al. The prevalence of severe acute respiratory coronavirus virus 2 (SARS-CoV- 2) IgG antibodies in intensive care unit (ICU) healthcare personnel (HCP) and its implications e a single-center, prospective, pilot study. Infect Control Hosp Epidemiol. 2020;12:1e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Self WH, Tenforde MW, Stubblefield WB, et al. Seroprevalence of SARS-CoV-2 among frontline health care personnel in a multistate hospital network e 13 academic medical centers, April-June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1221e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Stubblefield WB, Talbot HK, Feldstein L, et al. Seroprevalence of SARS-CoV-2 among frontline healthcare personnel during the first month of caring for COVID-19 patients e Nashville, Tennessee. Clin Infect Dis. 2021;72:1645e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Mansour M, Leven E, Muellers K, et al. Prevalence of SARS-CoV-2 antibodies among healthcare workers at a tertiary academic hospital in New York City. J Gen Intern Med. 2020;35:2485e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Moscola J, Sembajwe G, Jarrett M, et al. Prevalence of SARS-CoV-2 antibodies in health care personnel in the New York City area. JAMA. 2020;324:893e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sydney ER, Kishore P, Laniado I, et al. Antibody evidence of SARS-CoV-2 infection in healthcare workers in the Bronx. Infect Control Hosp Epidemiol. 2020;41:1348e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Galanis P, Vraka I, Fragkou D, et al. Seroprevalence of SARS-CoV-2 antibodies and associated factors in healthcare workers: a systematic review and meta-analysis. J Hosp Infect. 2021;108:120–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kayi I, Madran B, Keske S, et al. The seroprevalence of SARS-CoV-2 antibodies among health care workers before the era of vaccination: a systematic review and meta-analysis. Clin Microbiol Infect. 2021;27:1242–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Iversen K, Bundgaard H, Hasselbalch RB, et al. Risk of COVID-19 in health-care workers in Denmark: an observational cohort study. Lancet Infect Dis. 2020;20:1401–8. Epub 2020 Aug 3. Erratum in: Lancet Infect Dis. 2020 Oct;20(10):e250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Grant JJ, Wilmore S, McCann NS, et al. Seroprevalence of SARS-CoV-2 antibodies in healthcare workers at a London NHS trust. Infect Control Hosp Epidemiol. 2020;4:1e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Rudberg AS, Havervall S, Månberg A, et al. SARS-CoV-2 exposure, symptoms and seroprevalence in healthcare workers in Sweden. Nat Commun. 2020;11:5064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Sotgiu G, Barassi A, Miozzo M, et al. SARS-CoV-2 specific serological pattern in healthcare workers of an Italian COVID-19 forefront hospital. BMC Pulm Med. 2020;20:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Poulikakos D, Sinha S, Kalra PA. SARS-CoV-2 antibody screening in healthcare workers in a tertiary centre in North West England. J Clin Virol. 2020;129:104545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Steensels D, Oris E, Coninx L, et al. Hospital-wide SARS-CoV-2 antibody screening in 3056 staff in a tertiary center in Belgium. JAMA. 2020;324:195e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Blairon L, Mokrane S, Wilmet A, et al. Large-scale, molecular and serological SARSCoV- 2 screening of healthcare workers in a 4-site public hospital in Belgium after COVID-19 outbreak. J Infect. 2020;4453:30514–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Pallett S, Rayment M, Patel A, et al. Point-of-care serological assays for delayed SARS-CoV-2 case identification among health-care workers in the UK: a prospective multicentre cohort study. Lancet Respir Med. 2020;8:885e94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Korth J, Wilde B, Dol_ S, et al. SARS-CoV-2-specific antibody detection in healthcare workers in Germany with direct contact to COVID-19 patients. J Clin Virol. 2020;128:104437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Martin C, Montesinos I, Dauby N, et al. Dynamics of SARS-CoV-2 RT-PCR positivity and seroprevalence among high-risk healthcare workers and hospital staff. J Hosp Infect. 2020;106:102e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Amendola A, Tanzi E, Folgori L, et al. Low seroprevalence of SARS-CoV-2 infection among healthcare workers of the largest children hospital in Milan during the pandemic wave. Infect Control Hosp Epidemiol. 2020;41:1468e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Hunter E, Price DA, Murphy E, et al. First experience of COVID-19 screening of health-care workers in England. Lancet. 2020;395:e77e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Plebani M, Padoan A, Fedeli U, et al. SARS-CoV-2 serosurvey in health care workers of the Veneto region. Clin Chem Lab Med. 2020;58:2107e11. [DOI] [PubMed] [Google Scholar]
- [29].Garcia-Basteiro AL, Moncunill G, Tortajada M, et al. Seroprevalence of antibodies against SARS-CoV-2 among health care workers in a large Spanish reference hospital. Nat Commun. 2020;11:3500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Khalil A, Hill R, Wright A, et al. SARS-CoV-2- specific antibody detection in healthcare workers in a UK maternity hospital: correlation with SARS-CoV-2 RT-PCR results. Clin Infect Dis. 2020;8:ciaa893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Lackermair K, William F, Grzanna N, et al. Infection with SARS-CoV-2 in primary care health care workers assessed by antibody testing. Fam Pract. 2020;7:cmaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Paderno A, Fior M, Berretti G, et al. SARS-CoV-2 infection in health care workers: cross-sectional analysis of an otolaryngology unit. Otolaryngol Head Neck Surg. 2020;163:671e2. [DOI] [PubMed] [Google Scholar]
- [33].Kassem AM, Talaat H, Shawky S, et al. SARS-CoV-2 infection among healthcare workers of a gastroenterological service in a tertiary care facility. Arab J Gastroenterol. 2020;21:151e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Olalla J, Correa AM, Marti´n-Escalante MD, et al. Search for asymptomatic carriers of SARS-CoV-2 in healthcare workers during the pandemic: a Spanish experience. QJM. 2020;10:hcaa238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Hains DS, Schwaderer AL, Carroll AE, et al. Asymptomatic seroconversion of immunoglobulins to SARS-CoV-2 in a pediatric dialysis unit. JAMA. 2020;323:2424e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Solodky ML, Galvez C, Russias B, et al. Lower detection rates of SARS-COV2 antibodies in cancer patients versus health care workers after symptomatic COVID-19. Ann Oncol. 2020;31:1087e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Behrens GMN, Cossmann A, Stankov MV, et al. Perceived versus proven SARS-CoV-2-specific immune responses in health-care professionals. Infection. 2020;48:631–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Brandstetter S, Roth S, Harner S, et al. Symptoms and immunoglobulin development in hospital staff exposed to a SARS-CoV-2 outbreak. Pediatr Allergy Immunol. 2020;31:841e7. [DOI] [PubMed] [Google Scholar]
- [39].Fusco FM, Pisaturo M, Iodice V, et al. COVID-19 among healthcare workers in a specialist infectious diseases setting in Naples, Southern Italy: results of a cross-sectional surveillance study. J Hosp Infect. 2020;105:596e600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Lahner E, Dilaghi E, Prestigiacomo C, et al. Prevalence of SARS-CoV-2 infection in health workers (HWs) and diagnostic test performance: the experience of a teaching hospital in central Italy. Int J Environ Res Public Health. 2020;17:4417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Schmidt SB, Gru¨ter L, Boltzmann M, et al. Prevalence of serum IgG antibodies against SARS-CoV-2 among clinic staff. PLoS One. 2020;15:e0235417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Xu X, Sun J, Nie S, et al. Seroprevalence of immunoglobulin M and G antibodies against SARS-CoV-2 in China. Nat Med. 2020;26:1193–5. [DOI] [PubMed] [Google Scholar]
- [43].Zhao R, Li M, Song H, et al. Early detection of SARS-CoV-2 antibodies in COVID-19 patients as a serologic marker of infection. Clin Infect Dis. 2020;71:2066e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Barallat J, Fernández-Rivas G, Quirant-Sánchez B, et al. Seroprevalence of SARS-CoV-2 IgG specific antibodies among healthcare workers in the Northern Metropolitan Area of Barcelona, Spain, after the first pandemic wave. PLoS One. 2020;15:e0244348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Kammon AM, El-Arabi AA, Erhouma EA, et al. Seroprevalence of antibodies against SARS-CoV-2 among public community and health-care workers in Alzintan City of Libya. medRxiv. Preprint. May 26, 2020. [Google Scholar]
- [46].Xiong S, Guo C, Dittmer U, et al. The prevalence of antibodies to SARS-CoV-2 in asymptomatic healthcare workers with intensive exposure to COVID-19. medRxiv. Preprint. June 2, 2020. [Google Scholar]
- [47].Galán I, Velasco M, Casas ML, et al. SARS CoV-2 seroprevalence among all workers in a teaching hospital in Spain: unmasking the risk. medRxiv. Preprint. May 29, 2020. medRxiv. preprint. May 29, 2020. [Google Scholar]
- [48].Nakamura A, Ando S, Endo H, et al. Seroprevalence of antibodies to SARS-CoV-2 in healthcare workers in a nonepidemic region, Japan: a hospital-based study on May, 2020. J Med Virol. 2021;93:4608–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Psichogiou M, Karabinis A, Pavlopoulou I, et al. Antibodies against SARS-CoV-2 among health care workers in a country with low burden of COVID-19. PLoS One. 2020;15:e0243025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Chibwana MG, Jere KC, Kamn'gona R, et al. High SARS-CoV-2 seroprevalence in health care workers but relatively low numbers of deaths in urban Malawi. medRxiv. Preprint. 2020 Aug 5. [Google Scholar]
- [51].Tosato F, Pelloso M, Gallo N, et al. Severe acute respiratory syndrome coronavirus 2 serology in asymptomatic healthcare professionals: preliminary experience of a tertiary Italian academic center. medRxiv. Preprint. May 1, 2020. [Google Scholar]
- [52].Paradiso AV, De Summa S, Silvestris N, et al. Prospective observational COVID-19 screening and monitoring of asymptomatic cancer center health-care workers with a rapid serological test. Diagnostics. 2021;11:975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Fujita K, Kada S, Kanai O, et al. Quantitative SARS-CoV-2 antibody screening of healthcare workers in the southern part of Kyoto city during the COVID-19 peri-pandemic period. Front Public Health. 2020;8:595348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Sikora K, Barwick I, Hamilton C. Serological prevalence of antibodies to SARS CoV-2 amongst cancer centre staff. medRxiv. Preprint. May 20, 2020. [Google Scholar]
- [55].Shields A, Faustini SE, Perez-Toledo M, et al. SARS-CoV-2 seroprevalence and asymptomatic viral carriage in healthcare workers: a cross-sectional study. Thorax. 2020;75:1089–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Takita M, Matsumura T, Yamamoto K, et al. Preliminary results of seroprevalence of SARS CoV- 2 at community clinics in Tokyo. MedRxiv. Preprint. May 5, 2020. [Google Scholar]
- [57].Eyre DW, Lumley SF, O’Donnell D, et al. Differential occupational risks to health care workers from SARS- CoV- 2 observed during a prospective observational study. Elife. 2020;9:e60675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Lidstrom AK, Sund F, Albinsson B, et al. Work at in patient care units is associated with an increased risk of SARS-CoV-2 infection; a cross-sectional study of 8679 health care workers in Sweden. Ups J Med Sci. 2020;125:305–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Jones CR, Hamilton FW, Thompson A, et al. SARS-CoV-2IgG seroprevalence in health care workers and other staff at North Bristol NHS Trust: a socio demographic analysis. J Infect. 2021;82:e24e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Calcagno A, Ghisetti V, Emanuele T, et al. Risk for SARS-CoV-2 infection in healthcare workers, Turin, Italy. Emerg Infect Dis. 2021;27:303–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Delmas C, Plu-Bureau G, Canouï E, et al. Clinical characteristics and persistence of severe acute respiratory coronavirus virus 2 (SARS-CoV-2) IgG antibodies in 4,607 French healthcare workers: comparison with European countries. Infect Control Hosp Epidemiol. 2021;42:1406–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Brant-Zawadzki M, Fridman D, Robinson PA, et al. SARS-CoV-2 antibody prevalence in health care workers: preliminary report of a single center study. PLoS One. 2020;15:e0240006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Racine-Brzostek SE, Yang HS, Chadburn A, et al. COVID-19 viral and serology testing in New York City health care workers. Am J Clin Pathol. 2020;154:592–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Dimcheff DE, Schildhouse RJ, Hausman MS, et al. Seroprevalence of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection among Veterans Affairs healthcare system employees suggests higher risk of infection when exposed to SARS-CoV outside the work environment. Infect Control Hosp Epidemiol. 2020;42:392–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Mostafa A, Kandil S, El-Sayed MH, et al. SARS-CoV-2 seroconversion among 4040 Egyptian healthcare workers in 12 resource-limited healthcare facilities: a prospective cohort study. Int J Infect Dis. 2021;104:534–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Nicholson L, McLawhon RW, Kurian S, et al. Healthcare worker seroconversion for SARS-CoV-2 at two large health systems in San Diego. Am J Infect Control. 2021;49:506–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].El-Raey F, Alboraie M, Youssef N, et al. Predictors for severity of SARS-CoV-2 infection among healthcare workers. J Multidiscip Healthc. 2021;14:2973–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Moustafa EF, Hassany SM, Soliman AMA, et al. Infection and severity of COVID-19 infection among health care workers: a report from Egypt. Infect Disord Drug Targets. 2022. Online ahead of print. [DOI] [PubMed] [Google Scholar]