INTRODUCTION
Since the first case of COVID-19 that was reported in Wuhan, China, in December 2019, the novel coronavirus has rapidly spread worldwide.[1] On 30 January 2020, the World Health Organization declared the situation a public health emergency of international concern; on 12 March 2020, it was declared a pandemic.[2]
Rapid measures have been implemented by governments worldwide in an attempt to curb the pandemic and minimise its impact on health services. In Singapore, with the first confirmed COVID-19 case on 23 January 2020, the Ministry of Health implemented wide-ranging multi-agency public health measures and raised national emergency alert levels based on a Disease Outbreak Response System Condition (DORSCON) system.[3] Scale-down measures included safe social distancing, segregation of working teams, working from home, stay home notices for returning residents, school closures, virtual learning and a ‘circuit breaker’ that only allowed essential services to function, similar to a progressive lockdown [Figures 1 and 2, Table 1].[4]
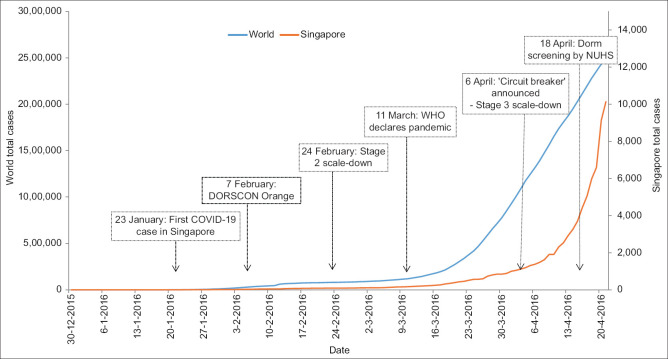
Figure 1.
Graph shows the total number of COVID-19 cases in Singapore and the world as of April 2020. DORSCON: Disease Outbreak Response System Condition, NUHS: National University Health System, WHO: World Health Organization
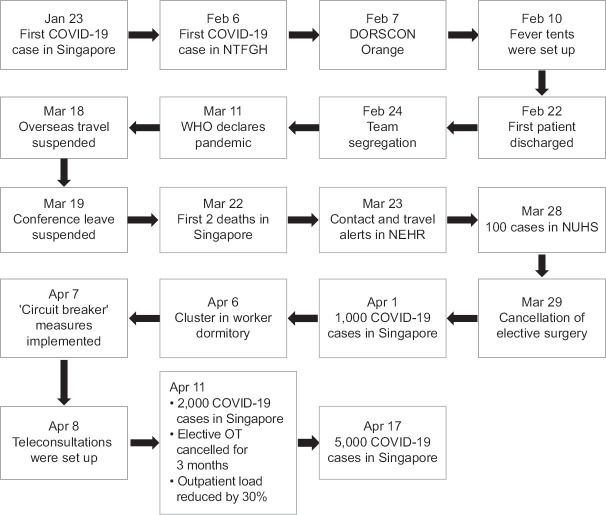
Figure 2.
Flow diagram shows the timeline of the COVID-19 outbreak in Singapore as of April 2020. NEHR: National Electronic Health Record, NTFGH: Ng Teng Fong General Hospital, OT: operating theatre
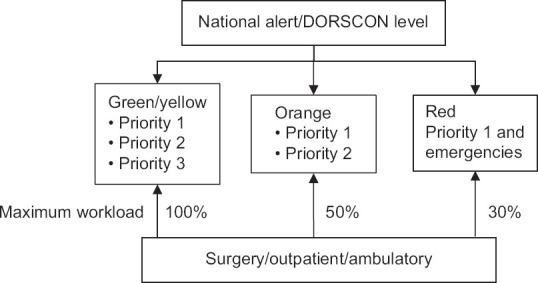
Table 1.
Scale-down in hospitals based on level of emergency.
| Location | Stage 1 | Stage 2 scale-down | Stage 3 scale-down |
|---|---|---|---|
| Hospital | No Change | • SOC reduced by 50% | • SOC reduced by >70% |
| • OT listed reduced by 25% | • OT listed reduced by >90% | ||
|
| |||
| Department | No Change | • Team segregation implemented/phone consultations started | • Only Priority 1 emergency operations performed |
| • Operations for Priority 1/2 and emergencies | • Selected ambulatory procedures performed | ||
OT operating theatre, SOC: specialist outpatient clinics
At our institution, Ng Teng Fong General Hospital, protocols for inpatient surgery and outpatient care were implemented swiftly according to the DORSCON status. A COVID-19 action team was activated to optimise patient care. Department-level changes were implemented for inpatient and outpatient urology care, including reallocation of staff, team segregation, prioritisation of surgery, ambulatory procedures and outpatient clinic visits in a streamlined manner.
We herein provide a simple urology action plan that we developed for urology patient management during the pandemic. It has two categories: protocols for inpatient surgery and outpatient care, consisting of clinic visits and ambulatory procedures.
METHODS
In order to formulate a comprehensive urology action plan, a literature review was performed, taking into consideration all the major guidelines (National Institute for Health and Care Excellence, British Association of Urological Surgeons and European Association of Urology [EAU] guidelines) and the recently released rapid response guidelines from the EAU.[5,6,7,8] We incorporated suggestions from institutes such as the Cleveland Clinic, Royal College of Surgeons and Singapore's earliest responders to COVID-19, Tan Tock Seng Hospital.[9,10,11] Additional focused literature review was done on the COVID-19 response in surgery and urology subspecialties, urologic oncology and endourology.[12,13,14,15] This laid the foundation for our urology action plan.
To cater to our local and Southeast Asian population, we revised institutional protocols for inpatient surgery and outpatient care that were available on the National University Health System intranet. These were implemented swiftly to be aligned with evolving recommendations by the Ministry of Health [Figure 2].[3]
PROTOCOLS FOR INPATIENT SURGERY
The COVID-19 pandemic has crippled healthcare systems even in developed countries in Europe and the United States.[16,17] Governments have had to redistribute their resources to support healthcare needs and prevent healthcare systems from being overwhelmed. Singapore, being one of the first ASEAN countries outside China to be affected by COVID-19, responded quickly with timely measures based on a DORSCON system. Having learnt from its experience with severe acute respiratory syndrome (SARS) in the past, decisive measures were taken to contain the spread of the virus.[18]
In a pandemic, the aim of scaling down is to free up inpatient beds, healthcare personnel (surgeons, anaesthetist, nurses, ancillary staff), personal protective equipment (PPE) and operating rooms. Moreover, a reduction in elective surgery lowers the need for intensive care unit (ICU) stays postoperatively, allowing unstable COVID-19 patients to receive ventilator support. The degree to which scaling-down occurs directly correlates to the emergency status of the healthcare systems and needs of the respective urological departments. If implemented systematically, this reduces the burden on the healthcare systems, optimises preparedness and mitigates any chaotic response to the pandemic.
Our inpatient surgical protocol was developed based on rapid response EAU guidelines and was aligned with government policies based on DORSCON status,[8] and considered both patient and disease factors and system factors in the institution or department [Figure 3].
Figure 3.
Summary of our urinary action plan during the COVID-19 pandemic. DORSCON: Disease Outbreak Response System Condition
Patient and disease factors
Patient-related factors included the need for blood transfusion, presence of comorbidities, possible need for a postoperative high-dependency bed, nature of the disease and urgency of treatment.
System factors
System factors consisted of the availability of: (a) resources (e.g. ICU beds, ventilators, blood bank, PPE); (b) manpower (e.g. anaesthetists, manpower in ICU/operating theatre/wards); and (c) non-COVID-19-designated wards.
We classified urological procedures based on the nature of the disease and urgency of intervention needed, as follows [Table 2]:
Table 2.
Surgical workflow based on DORSCON status.
| Type | DORSCON status | Disease/procedure |
|---|---|---|
| Emergencies | Green/Yellow, Orange, Red | • Urosepsis with obstruction (not amenable to PCN) |
| • Abscess/Fournier’s gangrene | ||
| • Testicular torsion | ||
| • Priapism that failed initial treatment, requiring shunt procedures | ||
| • Penile fracture/genitourinary trauma | ||
| • Cystodiathermy (intractable haematuria from BPE, bladder cancer, radiation cystitis) | ||
|
| ||
| Priority 1 | Green/Yellow, Orange, Red | • Radical cystectomy |
| • TURBT | ||
| • Nephrouretectomy | ||
| • Radical nephrectomy (> T2 renal tumours) | ||
| • Radical inguinal orchidectomy (testicular tumours) | ||
|
| ||
| Priority 2 | Green/Yellow, Orange | • Radical prostatectomy |
| • Obstructed kidney | ||
| • Stented patients with obstructing ureteric stones | ||
| • Nephron-sparing surgery for T1 renal tumours | ||
|
| ||
| Priority 3 | Green/Yellow | • Varicocelectomy/hydrocoelectomy |
| • Elective andrology procedures | ||
| • Nephrectomy (benign cause) | ||
| • PCNL | ||
| • BPE surgery | ||
| • Reconstructive/functional urology surgery | ||
DORSCON Yellow/Green: Priority 1, 2 and 3; DORSCON Orange: only Priority 1 and 2; DORSCON Red: only Priority 1 and emergencies. All procedures to follow institution-specific protocols for personal protective equipment. BPE: benign prostatic enlargement, DORSCON: Disease Outbreak Response System Condition, PCN: percutaneous nephrostomy, PCNL: percutaneous nephrolithotripsy, TURBT: transurethral resection of bladder tumour
-
(a)
Priority 1 (high priority): cannot be delayed/urgent, includes patients with cancers that have high risk of progression, are likely to affect overall survival, and may lead to loss of renal function without early intervention.
-
(b)
Priority 2 (moderate priority): can proceed with precautions, second to be cancelled. This category involves less aggressive cancers such as prostate cancer and T1 renal tumours for which intervention is less time-sensitive and unlikely to affect oncological and survival outcomes. It also includes benign stone conditions such as obstructing ureteric calculi, for which there are alternate options for decompression of the kidney (e.g. image-guided percutaneous drainage of the kidney) while awaiting definitive stone surgery.
-
(c)
Priority 3 (low priority): non-urgent and should be deferred, first to be cancelled. This category includes all benign urological conditions for which the intervention is not time bound and does not affect survival.
-
(d)
Urological emergencies: to be done irrespective of DORSCON status. This category consists of urological conditions that are life- or organ-threatening and require immediate intervention.
OUTPATIENT CARE
The ability to deliver optimal outpatient care to urological patients is challenging during a pandemic. To minimise the risk of exposure (for patient and healthcare providers) to COVID-19 in the outpatient setting, we recognised that some factors play an important role. They are the ability to conduct virtual clinics via telecommunication/video conferencing and to prescribe/deliver medications, and the urgency of the patient's condition. Most outpatient referrals in the urology department are non-urgent and can be managed virtually or delayed for review after relevant investigations or imaging, while most ambulatory procedures are non-urgent and easily postponed.
Clinics
Based on the rapid-response EAU guidelines, we devised the following guidelines to suit our local population [Table 3].
Table 3.
Outpatient workflow in clinics based on DORSCON status.
| Type | DORSCON status | Disease/procedure |
|---|---|---|
| Priority 1 | Green/Yellow, Orange, Red | New referrals: |
| • Repeat visits to emergency room for ureteric colic | ||
| • Acute urinary retention/obstructive uropathy | ||
| • Gross haematuria (high risk of cancer) Follow-up: | ||
| • Metastatic prostate cancer requiring androgen deprivation therapy • Obstructing ureteric calculi on CT | ||
| • Post-ureterorenoscopy strictures seen on intravenous urography/computed tomography urogram (CTU) | ||
|
| ||
| Priority 2 | Green/Yellow, Orange | New referrals: |
| • Ureteric colic | ||
| • LUTS with moderate symptoms | ||
| • Gross hematuria (low risk for cancer) | ||
| • LUTS with abnormal prostate-specific antigen/digital rectal examination Follow-up: | ||
| • Significantly bothersome LUTS not responding to medical therapy | ||
| • Small renal mass on active surveillance | ||
| • Postoperative surveillance for renal cell carcinoma and upper tract urothelial carcinoma | ||
| • Prostate cancer on active surveillance | ||
|
| ||
| Priority 3 | Green/Yellow | New referrals: |
| • Asymptomatic microscopic haematuria Andrology (erectile dysfunction, premature ejaculation) | ||
| • Mild LUTS | ||
| • Chronic pelvic pain syndrome Circumcision/vasectomy Repeat visits on follow-up: | ||
| • Benign prostatic enlargement on medication | ||
| • Overactive bladder on medication | ||
| • Erectile dysfunction on medication | ||
| • Angiomyolipoma, Bosniak 2/2F cysts on surveillance | ||
| • Chronic pelvic pain syndrome | ||
DORSCON Yellow/Green: Priority 1, 2 and 3; DORSCON Orange: only Priority 1 and 2; DORSCON Red: only Priority 1 and emergencies. CT: computed tomography, LUTS: lower urinary tract symptoms
-
(a)
Priority 1 (high priority): urgent or see early. This includes patients with symptoms that need early diagnosis and treatment, which may affect survival or renal function.
-
(b)
Priority 2 (moderate priority): semi-urgent. Appropriate investigations should be arranged, if required, to enable planning of further treatment, with virtual clinics when possible. This category includes patients with symptoms and conditions that need treatment, who are amenable to teleconsultation.
-
(c)
Priority 3 (low priority): non-urgent, can be delayed by more than six months or until after the pandemic. This includes patients with conditions that are considered non-urgent and where delays in diagnosis or treatment are unlikely to affect survival outcomes.
Outpatient ambulatory procedures
Based on the rapid-response EAU guidelines, we devised the following guidelines for outpatient ambulatory procedures [Table 4].
Table 4.
Outpatient workflow for ambulatory procedures based on DORSCON status.
| Type | DORSCON status | Disease/procedure |
|---|---|---|
| Priority 1 | Green/Yellow, Orange, Red | • Scope for high-grade UC surveillance |
| • Prostate biopsy (high-risk category) | ||
| • Intravesical instillation therapy for high-risk UC | ||
|
| ||
| Priority 2 | Green/Yellow, Orange | • Scope for low-grade UC surveillance |
| • Prostate biopsy (low-risk category) cancers | ||
| • Shock wave lithotripsy for non-obstructive ureteric and symptomatic renal calculi | ||
| • Intravesical instillation therapy for low/intermediate-risk UC | ||
|
| ||
| Priority 3 | Green/Yellow | • Scope for asymptomatic microscopic haematuria |
| • Scope for LUTS | ||
| • Shock wave lithotripsy for asymptomatic renal calculi | ||
DORSCON Yellow/Green: Priority 1, 2 and 3; DORSCON Orange: only Priority 1 and 2; DORSCON Red: only Priority 1 and emergencies. LUTS: lower urinary tract symptoms, UC: urothelial cancer
-
(a)
Priority 1 (high priority): do not postpone. This includes patients on follow-up, treatment and surveillance of high-risk/-grade urothelial cancers. Recurrences detected during these procedures may need early intervention, affecting overall survival. This also includes patients with prostate cancer that is potentially high-risk and needs early histopathological diagnosis, staging and treatment.
-
(b)
Priority 2 (moderate priority): second to be cancelled, can be delayed by up to six months. This includes patients on follow-up, treatment and surveillance of low-grade urothelial cancers. It also includes patients with low-risk prostate cancer who need histopathological diagnosis. These are patients who are suitable for active surveillance and for whom treatment delays do not affect overall survival. Patients with non-obstructive, symptomatic renal and ureteric stones planned for shock wave lithotripsy are also included in this category.
-
(c)
Priority 3 (low priority): non-urgent, first to be cancelled (to be done after pandemic resolves). This includes patients with benign conditions or asymptomatic renal calculi, for whom treatment delays are unlikely to affect or alter the nature of the disease or condition.
CONCLUSION
Every disease outbreak has taught us lessons in preparedness, but a pandemic is a calamity of global scale that can overwhelm healthcare systems. Having an action plan will allow institutions to cope better and if followed in a similar manner across countries, a unified swift response can be established. We believe this first-of-its-kind proposed urology action plan from the ASEAN region can be an one-stop solution for urology units to effectively mitigate the pandemonium in crisis situations such as pandemics.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–33. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus disease (COVID-19) pandemic. [Last accessed on 24 Mar 2020]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 3.Ministry of Health, Singapore. Updates on COVID-19 (coronavirus disease 2019) local situation. [Last accessed on 24 Mar 2020]. Available from: https://www.moh.gov.sg/covid-19.
- 4.Hasell J, Mathieu E, Beltekian D, Macdonald B, Giattino C, Ortiz-Ospina E, et al. A cross-country database of COVID-19 testing. Sci Data. 2020;7:345. doi: 10.1038/s41597-020-00688-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Institute for Health and Care Excellence, UK. COVID-19. [Last accessed on 25 Mar 2020]. Available from: https://www.nice.org.uk/guidance/conditionsand-diseases/infections/covid19.
- 6.The British Association of Urological Surgeons. About coronavirus & COVID-19. [Last accessed on 25 Mar 2020]. Available from: https://www.baus.org.uk/about/coronavirus_covid-19.aspx.
- 7.(EAU). EAoU. EAU guidelines 2020 edition. [Last accessed on 28 Mar 2020]. Available from: https://uroweb.org/guideline/urological-infections/-3.
- 8.Ribal MJ, Cornford P, Briganti A, Knoll T, Gravas S, Babjuk M, et al. EAU Section Offices, EAU Guidelines Panels. EAU Guidelines Office Rapid Reaction Group: An organisation-wide collaborative effort to adapt the EAU guidelines recommendations to the COVID-19 era. Eur Urol. 2020;78:21–8. doi: 10.1016/j.eururo.2020.04.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldman HB, Haber GP. Recommendations for tiered stratification of urological surgery urgency in the COVID-19 era. J Urol. 2020;204:11–3. doi: 10.1097/JU.0000000000001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Royal College of Surgeons of England, UK. Updated intercollegiate general surgery guidance on COVID-19. [Last accessedon 28 Mar 2020]. Available from: https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2/
- 11.Chan MC, Yeo SEK, Chong YL, Lee YM. Stepping forward: Urologists’ efforts during the COVID-19 outbreak in Singapore. Eur Urol. 2020;78:e38–9. doi: 10.1016/j.eururo.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al-Shamsi HO, Alhazzani W, Alhuraiji A, Coomes EA, Chemaly RF, Almuhanna M, et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: An international collaborative group. Oncologist. 2020;25:e936–45. doi: 10.1634/theoncologist.2020-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wallis CJD, Novara G, Marandino L, Bex A, Kamat AM, Karnes RJ, et al. Risks from deferring treatment for genitourinary cancers: A collaborative review to aid triage and management during the COVID-19 pandemic. Eur Urol. 2020;78:29–42. doi: 10.1016/j.eururo.2020.04.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Proietti S, Gaboardi F, Giusti G. Endourological stone management in the era of COVID-19. Eur Urol. 2020;78:131–3. doi: 10.1016/j.eururo.2020.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.A. P. SAGES Recommendations Regarding Surgical Response to COVID-19 Crisis-SAGES Society of American Gastrointestinal and Endoscopic Surgeons. 2020. [Last accessed on 28 Mar 2020]. Available from: https://www.sages.org/recommendations-surgical-response-covid-19.
- 16.Cohen J, Kupferschmidt K. Countries test tactics in ‘war’ against COVID-19. Science. 2020;367:1287–8. doi: 10.1126/science.367.6484.1287. [DOI] [PubMed] [Google Scholar]
- 17.James JJ. Public health and COVID-19: From response to recovery. Disaster Med Public Health Prep. 2020;14:161–2. doi: 10.1017/dmp.2020.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tan CC. SARS in Singapore--key lessons from an epidemic. Ann Acad Med Singap. 2006;35:345–9. [PubMed] [Google Scholar]