Abstract
Introduction:
A significant treatment gap has been observed in patients with osteoporosis. Our previous audit found a 31.5% rate of anti-osteoporosis medication initiation after fragility fractures at one year. We piloted the use of telecarers to monitor osteoporosis treatment and compliance.
Methods:
From January 2017 to January 2018, all hip fracture patients at Changi General Hospital, Singapore, were automatically enrolled into the Health Management Unit valued care hip fracture programme. Telecarer calls were scheduled at discharge, 3, 6 and 12 months. We assessed the acceptability, completion and treatment rates of patients enrolled in this programme.
Results:
A total of 537 patients with a hip fracture were enrolled in the telecarer programme over one year. Their average age was 79.8 ± 8.23 years, and 63.1% of them were female. A total of 341 patients completed 12 months of follow-up, of which 251 (73.6%) patients were on treatment at 12 months. The most common cause of lack of initiation of secondary osteoporosis treatment was patient or family rejection (34.4%), followed by physician failure to prescribe (24.4%) and renal impairment (24.4%). 16.7% of patients were deemed to have advanced dementia with a life-limiting illness and were, thus, deemed unsuitable for treatment.
Conclusion:
Telecarers may be a useful adjunct in the monitoring of osteoporosis treatment after hip fractures in an elderly population. The main limitations are patient or family rejection and physician inertia. Further studies should focus on a combination of interventions for both patients and physicians to increase awareness of secondary fracture prevention.
Keywords: Hip fractures, osteoporosis, telemedicine
INTRODUCTION
There remains a significant treatment gap in patients with osteoporosis, with reported declining rates of anti-osteoporosis medication prescription.[1] Despite advances in diagnosis and interventions that reduce the risk of fracture, a minority of men and women at high fracture risk receive treatment.[2,3] Our previous institutional audit showed a low rate of antiresorptive initiation at 31.5% in patients older than 65 years presenting with fragility fractures.[4] Compliance rates for antiresorptive medications are also known to be low. Furthermore, recent national data shows that although the Singapore population is expected to have one of the world's longest life expectancies at 85 years, studies have found that 20% of older patients spend that last 10 years in disability due to musculoskeletal reasons.[5] As such, addressing the treatment of osteoporosis is an important element of improving the quality of life and reducing morbidity in this aged population. Various strategies have been employed to address the treatment gap in osteoporosis, and inpatient osteoporosis liaison services have been set up to increase detection, initiate investigation and treatment of osteoporosis. However, with increasing resource limitation and in light of the recent COVID-19 pandemic, where physical patient-doctor consultations may be limited, telemedicine and telecarers may be a potential avenue in aiding the treatment of chronic diseases such as osteoporosis. Telemedicine has been around for the last 20 years and its use in chronic disease management in the older population has been well demonstrated.[6,7] Its effectiveness has been shown in the management of congestive heart failure, stroke, chronic obstructive pulmonary disease and diabetes mellitus.[8,9] In particular, it has demonstrated effectiveness in reducing hospital readmissions and promoting medication compliance.[10] Increasing interest has been observed in the use of telemedicine for osteoporosis management; previous studies have looked into telemedicine and telementoring of physicians in rural areas for the integration of osteoporosis care.[11,12,13] However, similar studies are lacking in Southeast Asia, where telemedicine has yet to be widely adopted. We hypothesise that the use of telecarers in the management of our local population of patients with osteoporosis after hip fracture will aid in increasing the anti-osteoporosis treatment rates and facilitate compliance. We piloted the use of a telecarer over one year to assess the acceptance of this programme in patients and families and to assess the changes in osteoporosis treatment rates.
METHODS
Patients discharged from Changi General Hospital, Singapore who had been admitted with a hip fracture between January 2017 and January 2018 were recruited into this pilot study. Changi General Hospital is the sole regional hospital that provides care to the eastern part of the Singapore population. The hospital is part of the SingHealth healthcare network, which allows sharing of clinical documentation and electronic medical records across SingHealth institutions and primary care clinics in the region. Eligibility included the patient's or family's willingness to be followed up via telephone calls and non-nursing home resident status. The Health Management Unit in Changi General Hospital consists of 14 telecarers who are nurses. They provide a telephone service to monitor patients with chronic disease. Before this study, the nurses were trained in basic osteoporosis management and were provided with a specific osteoporosis telecarer script and questionnaires on initiation of anti-osteoporosis medication, calcium and vitamin D supplementation, compliance and presence of adverse effects. Telecarers spend an average of 15 minutes per phone call, as directed by the patient's or caregiver's needs and requirements. Patients who required anabolic treatments were reviewed separately in the specialist bone clinic and were excluded from this follow-up cohort. Telecarers also obtained information on recovery from surgery, falls risk and readmission. At the first call, the service was explained to the patient or caregiver, and verbal consent to participate in ongoing follow-up was obtained. Each patient was assigned an individual telecarer and scheduled calls were made at 3–4 days, three months, six months and one year after discharge. Osteoporosis education brochures were mailed out to patients by the telecarers after their first call to increase awareness and encourage patients to initiate and start treatment for osteoporosis. Telecarers also screened the patient's electronic medical records and prescribing database to confirm the accuracy of information regarding anti-osteoporosis prescription and follow-up appointments with their regular physicians. Osteoporosis treatments were recorded to verify the treatment initiated and compliance to treatment. Pharmacologic treatments analysed for this study were alendronate 70 mg oral weekly, risedronate 35 mg oral weekly, and s/c denosumab 60 mg six monthly. Calcium and vitamin D supplementation were also recorded. Reasons for not initiating treatments were documented from the electronic health records and Health Management Unit consultation notes. These were verified independently by study members LG and FT. Chi-square test was used to analyse the paired statistical difference in treatment rates for the group of patients followed through 12 months of telecarer calls.
RESULTS
From December 2016 to January 2018, 537 patients [Supplementary Figure 1 (618.9KB, tif) , Appendix] were admitted with a hip fracture and identified as being suitable for follow-up with the telecarer programme. The average age of the patients was 79.8 ± 8.23 years, and 63.1% of them were female [Table 1]. Of these, 341 (63.5%) successfully completed 12 months of follow-up through the telecarer programme. The highest rejection rate was during the first call at 17.5%, which reduced with time to 13.5% at three months, 8.9% at six months and 2.3% at 12 months [Figure 1]. The most common reason for failure to complete telecarer follow-up over the 12-month follow-up period was nursing home residential status (n = 61, 31.1%), followed by death (n = 59, 30.1%); 47 patients (24.0%) were uncontactable and 14.8% (n = 29) rejected further follow-up phone calls as they themselves or their family members were uninterested [Figure 2]. Male patients were more likely to not complete the 12-monthly follow-ups compared with female patients (P < 0.05), and there was no statistical difference in the age of those who completed and did not complete the 12-month follow-up. An increase in the percentage of patients undergoing anti-osteoporosis treatment was observed, with 73.4% of patients undergoing treatment at 12 months compared with 31.4% undergoing treatment at the first call [Figure 3], whereas 79.8% of patients were on calcium and vitamin D supplements at 12 months, up from 62.3% at the first call. However, an 80.8% drop from the six-month anti-osteoporosis treatment was observed. Accounting for patients who were uncontactable by the telecarers at the time of analysis at 12 months following their six-month call (n = 8), 23 patients stopped their treatments despite being on this telecarer programme. A separate analysis was conducted to analyse reasons for not continuing treatment at different time points of 3, 6 and 12 months, and the proportion of causes for treatment cessation was similar. These reasons are summarised in Figure 4. The most common reason for not continuing treatment for osteoporosis was patient and family rejection at 34.4%; physician lack of initiation contributed to 24.4% of the reasons for not commencing treatment; 24.4% of patients had renal impairment during follow-up; and another 16.7% of patients developed advanced dementia and life-limiting illness and were deemed unsuitable for anti-osteoporosis treatments. The Appendix contains a flowchart summary of the patients enrolled in the telecarer programme for the monitoring of secondary osteoporosis prevention.
Table 1.
Basic demographics of hip fracture patients enrolled in the telecarer programme.
| Characteristic | n (%) |
|---|---|
| Age* (yr) | 79.8±8.23 |
|
| |
| Gender | |
|
| |
| Female | 339 (63.1) |
|
| |
| Male | 198 (36.9) |
|
| |
| Ethnicity | |
|
| |
| Chinese | 411 (76.5) |
|
| |
| Malay | 78 (14.5) |
|
| |
| Indian | 22 (4.1) |
|
| |
| Others | 26 (4.8) |
*Data presented as mean±standard deviation.
Figure 1.
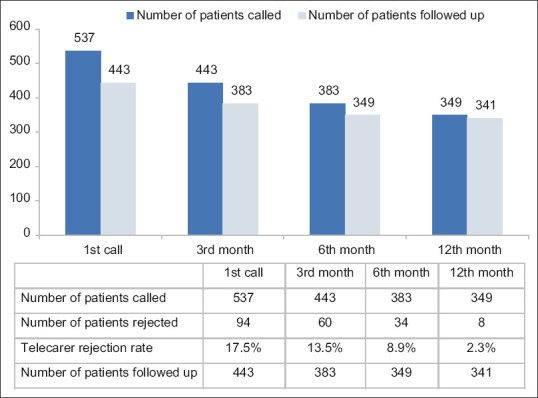
Bar chart and table show telecarer call acceptance over 12 months.
Figure 2.
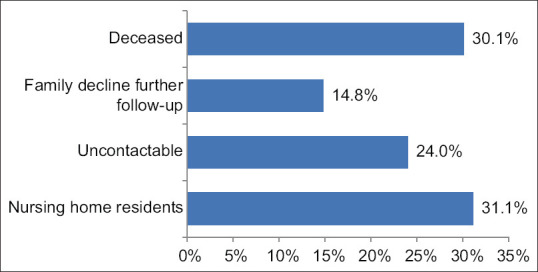
Bar chart shows telecarer dropout reasons over 12 months.
Figure 3.
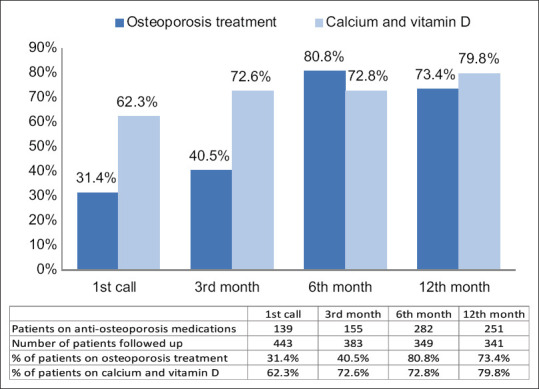
Bar chart and table show the percentage of patients on osteoporosis treatment and calcium and vitamin D supplementation over 12 months.
Figure 4.
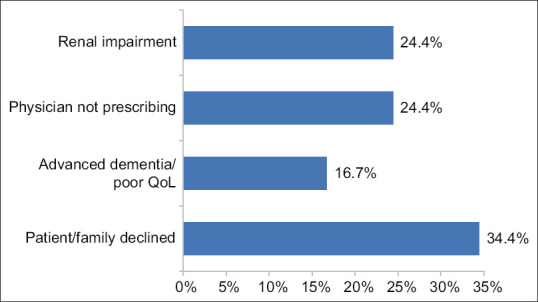
Bar chart shows reasons for osteoporosis treatment rejection. QoL: quality of life
DISCUSSION
This is a pilot study evaluating the utility of telecarers in individualised monitoring of patients after discharge following a hip fracture, to increase initiation and maintain compliance with anti-osteoporosis medication. To our knowledge, this is the first study in the Southeast Asian population assessing the use of telecarers in the management of osteoporosis.
Telemedicine may have an increasing role in the management of chronic diseases and with resource limitations and the potential need to limit physical medical consultations in light of the recent COVID-19 pandemic. We have demonstrated the feasibility and challenges of using telecarers in following up older patients with a hip fracture after discharge for the management of their osteoporosis. Telecarer follow-up of patients after discharge was acceptable to most patients and caregivers, with only 14.8% of patients and families dropping out of the programme owing to lack of interest. However, only 63.5% of all patients with a hip fracture were able to successfully complete the 12-month telecarer programme. This was mostly because of a significant proportion of patients who were admitted to nursing homes after discharge and, thus, were unable to continue enrolment into this programme; in addition, a significant proportion of patients died during the 12 months. Those who persisted and completed the telecarer programme showed high rates of commencement of anti-osteoporosis medications. 73.4% of patients completed the telecarer programme, which was a significant improvement from our previous institution data, which showed a treatment rate of 31.5% in patients above 65 years old with a fragility hip fracture at one year.[4] In this regard, our pilot programme was successful in increasing anti-osteoporosis treatment rates one year after hip fracture compared with our previous institutional data. Among those who failed to commence any treatments at 12 months, the most common cause of treatment rejection was patient or family preference at 34.5%, followed by clinician failure to prescribe at 24.4%. A significant mortality and morbidity rate was observed one year following a hip fracture, with 24.4% of patients developing renal impairment, and 16.7% having advanced dementia and life-limiting illness.
This data also demonstrates the multiple challenges that lie in the utility of telemedicine in the secondary prevention of osteoporosis in our population with fragility hip fracture. First is the high mortality and morbidity that develop after a hip fracture, with up to 20% of the total patients with initial hip fracture dying within one year or having to enter nursing homes; these patients account for most of those who failed to complete the telecarer follow-up in our study. Furthermore, 41.1% of patients who completed follow-up did not commence any osteoporosis treatment because they developed renal impairment, advanced dementia or life-limiting illness.
Patient or family preference remains the main reason for rejection of treatment for osteoporosis; in our study, this was the reason in 34.4% of those who did not commence anti-osteoporosis treatment. Despite the telecarer's advice and education, these short intermittent contacts do not seem to be adequate in reinforcing the importance of secondary fracture prevention in all our patients with a fragility hip fracture. Future strategies should include further research into a patient's understanding of myths or misconceptions regarding osteoporosis and its treatment, and addressing these barriers in the initiation of therapy. Increasing public awareness of this disease and treatment should also be proposed as a way to tackle the lack of knowledge in the community.
Unfortunately, a proportion of patients did not have any treatment commenced for their fragility fracture and osteoporosis despite seeing their regular physician. Although we were unable to find out individual physician reasons for not commencing these osteoporosis medications, our clinical records review suggested that despite regular review and documentation by their regular physician, no mention of osteoporosis and treatment was recorded. This may potentially point to physician treatment inertia that could be caused by factors such as inadequate knowledge, lack of confidence or experience in treatment initiation, or lack of time during consultation to address these issues. Further research effort should also be made to better understand these barriers and address them with targeted education programmes for primary care physicians and specialists looking after osteoporosis patients on identifying and treating these patients. Furthermore, as our study demonstrated, as there is a large burden of mortality and morbidity in the hip fracture population, future interventions should also focus on primary prevention of hip fractures as a strategy to reduce the morbidity and mortality. In our study, we also found a substantial proportion (31.1%) of hip fracture patients enter into nursing home residential care. There is still a paucity of evidence regarding the efficacy of osteoporosis treatment in this population, with few nursing home patients included in the trials of these medications.[14] A small study has shown evidence of bone mineral density gains in osteoporosis treatment among women in long-term care facilities who are still ambulatory.[15] We propose that strategies should be implemented to identify nursing home patients who are still ambulatory and who may benefit from osteoporosis treatment. These may include liaising with the nursing home physician and educating the patients on the evidence and benefits of these treatments. Future research should also be focused on assessing the benefits of osteoporosis treatment in nursing home patients where preserving mobility and independence may not be a gain, as there is now increasing evidence of potential extraskeletal benefits of nitrogen-containing bisphosphonates in reducing mortality from pneumonia and myocardial infarction in patients with hip fractures.[16,17] Given that most hip fractures are preceded by previous sentinel osteoporotic fractures, further studies should look into the earlier intervention of osteoporosis treatment in these preceding fractures to prevent future hip fractures.[18] Subsequent telecarer programmes in the care of osteoporosis should ideally incorporate simultaneously targeted strategies into addressing treatment barriers and potential myths or misconceptions in the management of osteoporosis in patients and their caregivers. Earlier intervention targeting not just hip fracture patients but those who present with other osteoporotic fractures such as vertebral and wrist fractures may be of more benefit, as these are typically younger populations that may benefit from earlier prevention of subsequent major hip fractures. Lastly, physician education and telementoring should be considered with the use of this technology to address physician inertia.
This study has some limitations. As the study duration was only for 24 months for recruitment followed by one year of follow-up, the sustainability of the telecarer service and longer-term compliance of patients on anti-osteoporosis medications are yet to be determined. All patients included in this follow-up had hip fracture, and whether the same intervention will be effective in patients with other types of fragility fractures warrants further studies. We did not have a concurrent control group that was not on follow-up with telecarers for comparison of treatment initiation and adherence rates. However, we used our historical data of treatment rates for evaluating the effectiveness of commencement of anti-osteoporosis treatment in our patient population. We also utilised electronic health records of the SingHealth institutions to check for medication prescription and clinic follow-up; a small proportion of patients may have chosen to have an ongoing follow-up in other institutions, which may not have been captured in this study. The reasons for treatment rejection were also collected from electronic records and may not fully represent individual reasons for treatment rejections. Individual physician reasons for not prescribing osteoporosis treatments were also not fully attainable in this study.
In conclusion, telecarers may play a role in increasing treatment rates in older patients with a hip fracture. However, patient or family rejection and physician inertia remain the main limitations of treatment. Further studies should look into a combination of interventions for both patients and physicians to address barriers, misconceptions and offer telementoring of physicians. Because of the significant proportion of patients with hip fracture entering a nursing home, strategies to identify patients in this population that may continue to benefit from osteoporosis treatment are needed. Given the significant mortality and morbidity of post-hip fractures, future efforts should be aimed at primary prevention of hip fractures by introducing this programme in younger patients who present with other fractures such as vertebral and wrist fractures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Supplement Materials
Flowchart of hip fracture patients enrolled into telecarer programme
Acknowledgement
We thank the Health Management Unit in Changi General Hospital, Singapore for its help in providing patient data.
REFERENCES
- 1.Solomon DH, Johnston SS, Boytsov NN, McMorrow D, Lane JM, Krohn KD. Osteoporosis medication use after hip fracture in U.S. patients between 2002 and 2011. J Bone Miner Res. 2014;29:1929–37. doi: 10.1002/jbmr.2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Díez-Pérez A, Hooven FH, Adachi JD, Adami S, Anderson FA, Boonen S, et al. Regional differences in treatment for osteoporosis. The Global Longitudinal Study of Osteoporosis in Women (GLOW) Bone. 2011;49:493–8. doi: 10.1016/j.bone.2011.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guggina P, Flahive J, Hooven FH, Watts NB, Siris ES, Silverman S, et al. Characteristics associated with anti-osteoporosis medication use: Data from the Global Longitudinal Study of Osteoporosis in Women (GLOW) USA cohort. Bone. 2012;51:975–80. doi: 10.1016/j.bone.2012.08.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gani L, Reddy SK, Alsuwaigh R, Khoo J, King TFJ. High prevalence of missed opportunities for secondary fracture prevention in a regional general hospital setting in Singapore. Arch Osteoporos. 2017;12:60. doi: 10.1007/s11657-017-0356-x. [DOI] [PubMed] [Google Scholar]
- 5.Times S. The Burden of Disease in Singapore 1990-2017. Straits Times Graphics. 2019. [Last accessed on 03 Jun 2022]. Available from: https://static1.straitstimes.com.sg/s3fs-public/attachments/2019/06/20/st_20190620_vndis_4920886.pdf.
- 6.Darkins A, Ryan P, Kobb R, Foster L, Edmonson E, Wakefield B, et al. Care Coordination/Home Telehealth: The systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemed J E Health. 2008;14:1118–26. doi: 10.1089/tmj.2008.0021. [DOI] [PubMed] [Google Scholar]
- 7.Celler BG, Lovell NH, Basilakis J, Magrabi F, Mathie M. Home telecare for chronic disease management.2001 Conference Proceedings of the 23rd Annual International Conference of the IEEE Engineering in Medicine and Biology Society. Istanbul, Turkey. 2001:3586–9. [Google Scholar]
- 8.Hu Y, Wen X, Wang F, Yang D, Liu S, Li P, et al. Effect of telemedicine intervention on hypoglycaemia in diabetes patients: A systematic review and meta-analysis of randomised controlled trials. J Telemed Telecare. 2019;25:402–13. doi: 10.1177/1357633X18776823. [DOI] [PubMed] [Google Scholar]
- 9.Bashshur RL, Shannon GW, Smith BR, Alverson DC, Antoniotti N, Barsan WG, et al. The empirical foundations of telemedicine interventions for chronic disease management. Telemed J E Health. 2014;20:769–800. doi: 10.1089/tmj.2014.9981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Lusignan S, Wells S, Johnson P, Meredith K, Leatham E. Compliance and effectiveness of 1 year's home telemonitoring. The report of a pilot study of patients with chronic heart failure. Eur J Heart Fail. 2001;3:723–30. doi: 10.1016/s1388-9842(01)00190-8. [DOI] [PubMed] [Google Scholar]
- 11.Lewiecki EM, Bouchonville MF, 2nd, Chafey DH, Bankhurst A, Arora S. Bone Health ECHO: Telementoring to improve osteoporosis care. Womens Health (Lond) 2016;12:79–81. doi: 10.2217/whe.15.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dickson L, Cameron C, Hawker G, Ratansi A, Radziunas I, Bansod V, et al. Development of a multidisciplinary osteoporosis telehealth program. Telemed J E Health. 2008;14:473–8. doi: 10.1089/tmj.2007.0079. [DOI] [PubMed] [Google Scholar]
- 13.Palcu P, Munce S, Jaglal SB, Allin S, Chishtie JA, Silverstein A, et al. Understanding patient experiences and challenges to osteoporosis care delivered virtually by telemedicine: A mixed methods study. Osteoporosis Int. 2020;31:351–61. doi: 10.1007/s00198-019-05182-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parikh S, Mogun H, Avorn J, Solomon DH. Osteoporosis medication use in nursing home patients with fractures in 1 US state. Arch Intern Med. 2008;168:1111–5. doi: 10.1001/archinte.168.10.1111. [DOI] [PubMed] [Google Scholar]
- 15.Greenspan SL, Schneider DL, McClung MR, Miller PD, Schnitzer TJ, Bonin R, et al. Alendronate improves bone mineral density in elderly women with osteoporosis residing in long-term care facilities. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2002;136:742–6. doi: 10.7326/0003-4819-136-10-200205210-00009. [DOI] [PubMed] [Google Scholar]
- 16.Sing CW, Kiel DP, Hubbard RB, Lau WC, Li GH, Kung AW, et al. Nitrogen-containing bisphosphonates are associated with reduced risk of pneumonia in patients with hip fracture. J Bone Miner Res. 2020;35:1676–84. doi: 10.1002/jbmr.4030. [DOI] [PubMed] [Google Scholar]
- 17.Sing CW, Wong AY, Kiel DP, Cheung EY, Lam JK, Cheung TT, et al. Association of alendronate and risk of cardiovascular events in patients with hip fracture. J Bone Miner Res. 2018;33:1422–34. doi: 10.1002/jbmr.3448. [DOI] [PubMed] [Google Scholar]
- 18.Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: A summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–39. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Flowchart of hip fracture patients enrolled into telecarer programme


