Abstract
The objective of this study was to examine the extent to which involvement in high-contact, semicontact, or noncontact sports during the 12th grade is associated with the initiation and developmental course of prescription drug misuse (PDM) between ages 17/18 years and 27/28 years. Data were collected from a national multicohort panel sample of US 12th-graders (cohorts 2006–2017; n = 4,772) from the Monitoring the Future Study who were followed for a decade, through age 27/28 years. Approximately 31% of high school seniors indicated PDM at baseline (age 17/18 years). While past-year PDM remained relatively stable between ages 17/18 years and 27/28 years, participation in both noncontact (adjusted odds ratio = 1.40, 95% confidence interval: 1.02, 1.91) and contact (adjusted odds ratio = 1.57, 95% confidence interval: 1.08, 2.28) sports in the 12th grade increased the odds of initiating prescription stimulant misuse during the 10 years following high school as compared with respondents who did not participate in these types of sports in the 12th grade. To our knowledge, this is the first national study to have assessed how sports participation during high school is associated with the initiation and developmental course of PDM from adolescence to young adulthood. These findings reinforce the need for PDM screening during adolescence, as nearly 1 in 3 high school seniors engage in PDM. Increased prescription stimulant misuse following high school warrants ongoing monitoring during young adulthood, especially among athletes.
Keywords: high school athletes, high school sports, prescription drug misuse, United States, young adulthood
Abbreviations
- AOR
adjusted odds ratio
- CI
confidence interval
- GEE
generalized estimating equations
- MSA
Metropolitan Statistical Area
- MTF
Monitoring the Future
- OR
odds ratio
- PDM
prescription drug misuse
More than 1 in 10 young adults aged 18–25 years report past-year prescription drug misuse (PDM) in the United States (1–5). PDM most commonly involves the misuse of prescription opioids, stimulants, and sedatives/tranquilizers and is most prevalent during the transition to adulthood (4, 5). While some types of PDM have decreased among adolescents and young adults in recent years (5, 6), there is continuing concern that the high prevalence of PDM places many adolescents and young adults at risk for adverse outcomes as they age into adulthood, with misuse of prescription opioids reported by 3.8% of adolescents and 7.8% of young adults (7–10).
Of particular concern are high-school athletes who participate in sports that involve high levels of contact (i.e., football, ice hockey, lacrosse, and wrestling). Several studies have shown that adolescents involved in competitive contact sports during high school have an increased risk of engaging in PDM of both opioids and stimulants (11–13). The greater risk of misusing prescription opioid analgesics may be related to the fact that participants in contact sports typically have the highest rate of severe injury among high school athletes (14) and may be more likely to have been prescribed opioids for injury and surgery. Previous research has demonstrated that the odds of prescription opioid misuse are 1.5 times higher among high school students who have experienced concussion due to sports or physical activity than among those without a history of concussion (15). Moreover, youth who participate in contact sports may be surrounded by peers who are more likely to have leftover prescription opioids, making it easier to receive diverted prescription opioids to ease injuries without having to alert parents and coaches that they need medical attention (1, 3, 16, 17). With respect to misuse of prescription stimulants, high school athletes in some contact sports may be engaging in a form of positive deviance (i.e., performance enhancement) (18). In particular, some sports socialize participants to a set of normative behaviors that facilitate overconformity (e.g., using performance-enhancing drugs to be the best); athletes in highly competitive and masculinized sports will be more accepting of engaging in certain forms of positive deviance like misuse of prescription stimulants and other performance-enhancing drugs, because their identities rely on highly skilled and focused performances in these sports (1, 2, 19, 20). Moreover, peers within these contexts may reinforce norms that it is acceptable to engage in PDM of stimulants and may provide both access to and knowledge on how to use these types of drugs (21).
While many factors may be driving this association between PDM and adolescent athletes involved in contact sports, it must be recognized that high school athletes who participate in these types of sports are at greater risk of engaging in other common types of substance use, and thus the association may simply reflect the fact that these athletes are more prone to engaging in risky behaviors (22, 23). Given this increased risk of substance misuse among adolescents within contact sports, it is necessary to investigate whether exposure to these types of sporting contexts during high school increases the risk of PDM and the initiation of PDM as adolescents transition into young adulthood. Notably, there is a dearth of PDM research assessing how high school participation in certain types of sports shapes the initiation and developmental course of this type of drug misuse. In order to address this knowledge gap, we used US national longitudinal data from the Monitoring the Future Study to examine the extent to which involvement in sports in high school is associated with PDM across the transition to adulthood, accounting for other types of substance-use behaviors and sociodemographic variables. There were 2 purposes of this study: 1) to assess the associations between playing high-contact (football, ice hockey, lacrosse, or wrestling), semicontact (baseball, basketball, field hockey, or soccer), or noncontact (cross-country running, gymnastics, swimming, tennis, track, volleyball, or weight-lifting) sports during the 12th grade and the initiation of PDM in the decade following high school; and 2) to assess how the different types of sports (based on level of contact) were associated with the developmental course of PDM after high school (age 17/18 years through age 27/28 years).
METHODS
Study design
This study used US national panel data from the Monitoring the Future (MTF) Study; detailed information on the project design and sampling methods is provided elsewhere (5, 6). Based on a multistage sampling procedure, MTF surveys nationally representative samples of approximately 17,000 US high school seniors each year using questionnaires administered in classrooms during the school day. The response rates at baseline (12th grade; modal age 17/18 years) ranged from 79% to 85% (6). Approximately 2,450 students from each yearly high school senior sample were randomly selected for biennial follow-up. A random half of the follow-up sample began biennial follow-up the following year (model age 19 years), while the other half began biennial follow-up 2 years after their senior year (modal age 20 years). Mailed questionnaires were used to collect data at 5 follow-up modal ages (hereafter referred to simply as ages): 19/20, 21/22, 23/24, 25/26, and 27/28 years. Drug users were oversampled for follow-up at 3 times the rate of non–drug users, and appropriate weights were then used to best approximate population estimates in the follow-ups. The attrition rate for the different cohorts in the MTF panel study from base year to the first follow-up was approximately 50%, with approximately 3% attrition from the first follow-up to the second follow-up (5). Accordingly, all analyses (excluding the sample characteristics presented in Table 1) incorporated nonresponse adjustments (i.e., attrition weights based on nonresponse at first follow-up) to the panel weights (i.e., unequal probabilities of selection into the panel sample) to explicitly account for MTF covariates that have been shown to be associated with nonresponse at future follow-ups (24–26).
Table 1.
Baseline Characteristics of the Panel Sample (n = 4,772), Monitoring the Future Study, 2006–2017
| Full Sample | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Available Data | Missing Data | Participated in Sports | Did Not Participate in Sports | ||||||
| Baseline (Age 17/18 Years) Variable | % | No. b | % | No. | % | No. b | % | No. b | P Value a |
| Overall sports participation | 12.3 | 586 | |||||||
| Participated in at least 1 sport | 68.1 | 2,851 | N/A | N/A | N/A | N/A | |||
| Did not participate in any sports | 31.9 | 1,335 | N/A | N/A | N/A | N/A | |||
| Type of sports participation | 12.3 | 586 | |||||||
| Contact sports | 20.0 | 836 | N/A | N/A | N/A | N/A | |||
| Semicontact sports | 35.1 | 1,471 | N/A | N/A | N/A | N/A | |||
| Noncontact sports | 35.0 | 1,465 | N/A | N/A | N/A | N/A | |||
| Lifetime nonmedical PDM at baseline | |||||||||
| PDM of opioids | 18.2 | 858 | 1.4 | 65 | 17.3 | 489 | 19.3 | 255 | 0.135 |
| PDM of stimulants | 18.9 | 891 | 1.1 | 52 | 18.0 | 509 | 19.4 | 258 | 0.274 |
| PDM of tranquilizers/sedatives | 19.8 | 937 | 0.9 | 42 | 17.5 | 496 | 22.8 | 303 | 0.001 |
| Any PDM | 30.9 | 1,466 | 0.7 | 33 | 29.2 | 829 | 33.2 | 442 | |
| Sex | 0.6 | 28 | |||||||
| Male | 48.6 | 2,306 | 53.5 | 1,519 | 35.2 | 468 | |||
| Female | 51.4 | 2,438 | 46.5 | 1,321 | 64.8 | 863 | |||
| Race/ethnicity | 0.0 | 0 | |||||||
| White | 60.5 | 2,886 | 64.3 | 1,833 | 57.8 | 772 | |||
| Black | 11.0 | 525 | 9.8 | 280 | 11.1 | 148 | |||
| Hispanic | 15.4 | 736 | 12.9 | 368 | 18.1 | 242 | |||
| Other | 13.1 | 625 | 13.0 | 370 | 13.0 | 173 | |||
| Grade point average | 3.3 | 156 | 0.001 | ||||||
| B− or higher | 82.8 | 3,824 | 86.4 | 2,429 | 78.8 | 1,039 | |||
| C+ or lower | 17.2 | 792 | 13.6 | 382 | 21.2 | 279 | 0.01 | ||
| Parents’ level of education | 4.2 | 199 | 0.001 | ||||||
| Less than a college degree | 48.8 | 2,233 | 43.2 | 119 | 57.8 | 736 | |||
| College degree or higher | 51.2 | 2,340 | 56.8 | 1,574 | 42.2 | 537 | |||
| Urbanicity | 0.0 | 0 | 0.001 | ||||||
| Large MSA (urban) | 29.8 | 1,424 | 29.1 | 831 | 29.6 | 395 | |||
| Other MSA (suburban) | 48.9 | 2,332 | 47.9 | 1,367 | 49.9 | 666 | |||
| Non-MSA (rural) | 21.3 | 1,016 | 22.9 | 653 | 20.5 | 274 | |||
| US region | 0.0 | 0 | |||||||
| Northeast | 18.3 | 872 | 17.5 | 499 | 15.1 | 201 | |||
| Midwest | 23.5 | 1,123 | 25.1 | 717 | 23.8 | 318 | |||
| South | 38.1 | 1,816 | 37.6 | 1,072 | 40.6 | 542 | |||
| West | 20.1 | 961 | 19.7 | 563 | 20.5 | 274 | |||
| Cohort yearc | 0.0 | 0 | 0.01 | ||||||
| 2006–2009 | 34.7 | 1,657 | 35.5 | 1,031 | 31.5 | 420 | |||
| 2010–2013 | 35.0 | 1,668 | 35.8 | 1,021 | 35.4 | 472 | |||
| 2014–2017 | 30.3 | 1,447 | 28.7 | 817 | 33.2 | 443 | |||
Abbreviations: MSA, Metropolitan Statistical Area; N/A, not applicable; PDM, prescription drug misuse.
a Significance tests were based on χ2 tests of independence.
b Sample sizes vary in comparison with the total sample because of missing data across items.
c Year of entering the survey at age 17/18 years.
Sample
Questions regarding participation in specific competitive sports were added to the 12th-grade surveys in 2006 and were included on only 1 of the 6 randomly distributed questionnaire forms (form 5). Accordingly, the current study drew on 4,772 respondents (this included respondents who participated in sports during the 12th grade and those who did not) from 12 recent longitudinal cohorts (2006–2017) who were eligible to complete at least 1 follow-up past their 12th-grade year. Earlier cohorts (i.e., 2006–2007) were able to complete the age 19/20, 21/22, 23/24, 25/26, and 27/28 follow-ups, while more recent cohorts (i.e., 2014–2017) have only been able to complete at least the age 19/20 or 21/22 follow-up. Because of the structure of the data, all fully adjusted models accounted for cohort year. The unweighted demographic characteristics of respondents are shown in Table 1.
Measures
PDM (time-varying outcome).
Past-year PDM was measured at baseline and at each follow-up with identical questions based on separate measures assessing past-year misuse of prescription opioids, stimulants, and sedatives/tranquilizers (i.e., “[Have you] … taken any … on your own—that is, without a doctor telling you to take them?”). Respondents were provided a list of several generic and brand-name examples for each of the prescription drug classes (e.g., hydrocodone, oxycodone, and codeine for prescription opioids). The response scales for the questions ranged from no occasions (1 point) to 40 or more occasions (7 points). Each measure was recoded as a binary variable for the analyses. In order to assess any PDM, respondents who indicated any type of PDM were flagged as engaging in past-year PDM.
Type of competitive sports participation during the 12th grade (time-invariant).
Several variables were used to measure participation in different types of competitive sports based on the level of contact. The MTF survey asks adolescents which competitive sports they have participated in during the past 12 months, either in their school or in the community. Respondents can indicate whether they have participated in specific sports, including baseball, basketball, cross-country running, field hockey, football, gymnastics, ice hockey, lacrosse, swimming, soccer, tennis, track, volleyball, weight-lifting, or wrestling (there was an additional response option indicating “none”). These questions were grouped into 3 unique categories that captured the amount of contact participants experience within certain types of sports; these categorizations have been used in prior studies (22, 23) and align with the classifications outlined by the Council on Sports Medicine and Fitness (27). The first category, high-contact sports, includes sports that involve a great deal of physical contact. Respondents who indicated that they had participated in football, ice hockey, lacrosse, or wrestling during the past year were included within this category. The second category, semicontact sports, includes sports that involve sporadic contact. If adolescents indicated participating in baseball, basketball, field hockey, or soccer, they were included within this category. The final category, noncontact sports, includes sports where no contact can occur between participants. Respondents who indicated participating in cross-country running, gymnastics, swimming, tennis, track, volleyball, or weight-lifting were included within this category.
Note that the variables constructed to capture the level of contact within these 3 groupings of competitive sports are not mutually exclusive—namely, they are treated as 3 separate binary indicators: 1) participates in contact sports versus does not participate in contact sports (reference group); 2) participates in semicontact sports versus does not participate in semicontact sports (reference group); and 3) participates in noncontact sports versus does not participate in noncontact sports (reference group). Adolescents could indicate participating in multiple types of sports (it was possible for respondents to be engaged in both contact sports and noncontact sports). We also note that nonparticipants are included in this conceptualization; however, they do not represent a unique reference group (i.e., “does not participate in sports”). For example, the reference group for the indicator “participates in contact sports” included all respondents who did not indicate participating in this type of activity (i.e., nonparticipants and respondents who participated in other types of sports). The multivariable analytical models included each type of sport (i.e., contact, semicontact, and noncontact) in the analyses (simultaneously) to control for this overlap in participation.
Covariates (time-invariant).
Sociodemographic variables included the following: sex (male, female), race/ethnicity (White, Black, Hispanic, other), US Census geographic region (Northeast, Midwest, South, West), urbanicity based on Metropolitan Statistical Area (MSA) (large MSA (urban), other MSA (suburban), non-MSA (rural)), parental education (neither parent graduated from a 4-year college, at least 1 parent graduated from a 4-year college), average grade in high school (C+ or lower, B− or higher), and cohort year.
Covariates (time-varying).
Additional control variables assessed at baseline and at each follow-up included past-30-day cigarette use, past 2-week binge drinking, past 30-day marijuana use, and whether the participant was currently attending college.
Data analysis
Descriptive statistics, unadjusted odds ratios, and adjusted odds ratios (AORs) were generated in Stata 17.0 (StataCorp LLC, College Station, Texas) to examine the association between different types of competitive sports participation during the 12th grade and the prevalence of past-year PDM between age 17/18 years and age 27/28 years. First, weighted percentages of respondents reporting past-year PDM use at ages 17/18, 19/20, 21/22, 23/24, 25/26, and 27/28 years were estimated and graphed (95% confidence intervals (CIs) were based on standard errors obtained using Taylor linearization). Second, logistic regression models were fitted using the generalized estimating equations (GEE) method (28, 29) with an exchangeable correlation structure to assess whether different types of competitive sports participation were associated with initiation of PDM in young adulthood (i.e., from age 19/20 years to age 27/28 years; time-varying outcome); logistic regression models using GEE were fitted among respondents who indicated no history of PDM at age 17/18 years (baseline). This was assessed for each type of past-year PDM and any type of PDM (e.g., only respondents who indicated no prior history of opioid PDM at age 17/18 years were included in the analyses assessing opioid PDM between ages 19/20 years and 27/28 years; only respondents who indicated no prior history of any PDM at age 17/18 years were included in the analyses assessing any past-year PDM between ages 19/20 and 27/28 years). Both AORs and 95% CIs are reported for the GEE models. Third, additional GEE models were fitted using the full sample (persons with and without a history of PDM at baseline (age 17/18 years)) to assess the association between different types of competitive sports participation and past-year PDM during this 10-year period in early adulthood (ages 17/18–27/28 years) when accounting for the key control variables. Finally, additional analyses also assessed the effects of interaction between cohort and sport type (i.e., cohort × sport type) to determine whether the association between participation in certain types of sports and PDM was moderated by cohort (i.e., 2006–2009, 2010–2013, or 2014–2017).
All descriptive (excluding the sample characteristics presented in Table 1), bivariate, and multivariable analyses were weighted to adjust for differential attrition at the first follow-up (i.e., age 19/20 years) (26); similar approaches for the proposed analyses have been used in prior studies using the MTF panel (30, 31). The University of Michigan Institutional Review Board deemed this study exempt from human subjects review because deidentified data were used.
RESULTS
Overall age-related pattern of past-year PDM prevalence from age 17/18 years to age 29/30 years
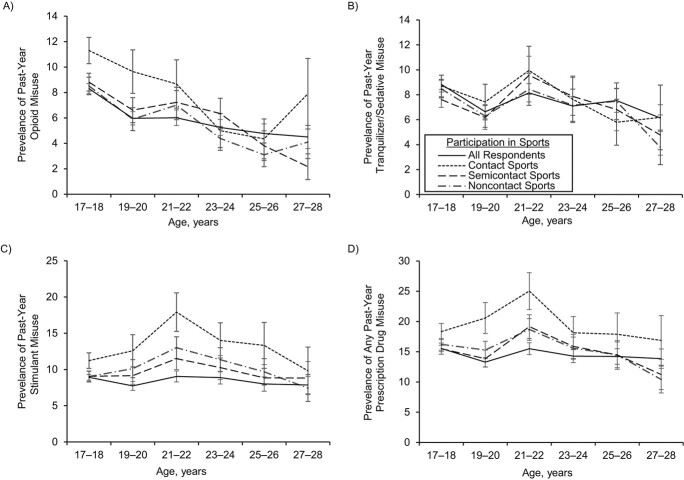
Approximately 31% of respondents in the sample indicated some type of lifetime PDM at baseline (i.e., age 17/18 years). Figure 1 shows the pattern of past-year PDM by age. Overall, past-year PDM (any) was relatively stable from age 17/18 years (15.5%, 95% CI: 14.5, 16.5) through age 27/28 years (13.8%, 95% CI: 11.7, 17.3). Only PDM of opioids was found to decrease between age 17/18 years (8.3%, 95% CI: 7.6, 9.1) and age 27/28 years (4.5%, 95% CI: 3.0, 6.7) among the full sample. Moreover, respondents who participated in contact sports at age 17/18 years had higher past-year prevalence of any PDM at ages 19/20 years (20.6%, 95% CI: 16.0, 26.1) and 21/22 years (25.0%, 95% CI: 19.5, 31.5) when compared with the full sample, but had similar past-year prevalences at age 17/18 years and between ages 23/34 and 27/28 years. No age differences were found between respondents who participated in semicontact and noncontact sports during high school when compared with the full sample. Finally, specific age differences in past-year PDM opioid and stimulant use were found among respondents who participated in contact sports during high school. In particular, PDM of opioids was highest at age 17/18 years (11.3%, 95% CI: 9.4, 13.5), and PDM of stimulants was highest at age 21/22 years (17.9%, 95% CI: 13.3, 23.7) among respondents who participated in contact sports when compared with the full sample.
Figure 1.
Past-year prevalence (%) of prescription drug misuse (PDM) between ages 17/18 and 27/28 years according to participation in different types of high school sports, Monitoring the Future Study, 2006–2017. A) PDM of opioids; B) PDM of tranquilizers/sedatives; C) PDM of stimulants; D) any PDM. Bars, 95% confidence intervals.
Overall association between different types of competitive sports participation and initiation of PDM between ages 19/20 and 27/28 years
Table 2 shows results for the overall association between participation in different types of competitive sports during high school and initiation of PDM during early adulthood (among those who did not engage in PDM by the 12th grade). Accordingly, participation in contact sports increased the odds of initiating PDM of stimulants (AOR = 1.57, 95% CI: 1.08, 2.28) across this 10-year time frame in comparison with respondents who did not participate in contact sports during high school. Moreover, participation in noncontact sports reduced the odds of initiating PDM of opioids (AOR = 0.63, 95% CI: 0.40, 0.99) across this 10-year time frame in comparison with respondents who did not participate in noncontact sports during high school. However, participation in noncontact sports increased the odds of initiating PDM of stimulants (AOR = 1.40, 95% CI: 1.02, 1.91) during the transition to young adulthood. Additional analyses assessing interaction effects between cohort and sport type (with respect to initiation of PDM in young adulthood) found no statistically significant results (results not shown).
Table 2.
Adjusted Odds Ratios (Bivariate and Multivariable Tests) for Initiation of Nonmedical Prescription Drug Use in Early Adulthood According to Type of Sports Participation in High School Among Respondents With No Prior History of Nonmedical Use at Baseline (Age 17/18 Years), Monitoring the Future Study, 2006–2017
| Type of Nonmedical PDM | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Opioids | Stimulants | Tranquilizers/Sedatives | Any PDM | ||||
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Multivariable Associations (No Control Variables) a | ||||||||
| (n = 1,938) | (n = 1,946) | (n = 1,922) | (n = 1,683) | |||||
| Sports participation at age 17/18 years | ||||||||
| Contact sports | ||||||||
| Did not participate | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Participated | 1.75b | 1.02, 3.00 | 2.12c | 1.41, 3.18 | 0.82 | 0.51, 1.31 | 1.88c | 1.28, 2.77 |
| Semicontact sports | ||||||||
| Did not participate | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Participated | 1.02 | 0.65, 1.63 | 1.02 | 0.73, 1.43 | 1.23 | 0.82, 1.86 | 1.11 | 0.81, 1.53 |
| Noncontact sports | ||||||||
| Did not participate | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Participated | 0.63b | 0.40, 0.99 | 1.46b | 1.04, 2.05 | 0.92 | 0.62, 1.35 | 1.12 | 0.82, 1.54 |
| Follow-up period (from age 19/20 years (0) to age 27/28 years (4)) | 0.97 | 0.84, 1.11 | 1.05 | 0.97, 1.15 | 1.08 | 0.99, 1.18 | 1.07 | 0.99, 1.16 |
| Multivariable (Adjusted) Associations d | ||||||||
| (n = 1,837) | (n = 1,852) | (n = 1,825) | (n = 1,593) | |||||
| Sports participation at age 17/18 years | ||||||||
| Contact sports | ||||||||
| Did not participate | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Participated | 1.36 | 0.77, 2.44 | 1.57b | 1.08, 2.28 | 0.65 | 0.37, 1.13 | 1.42 | 0.98, 2.06 |
| Semicontact sports | ||||||||
| Did not participate | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Participated | 1.02 | 0.65, 1.61 | 1.21 | 0.86, 1.71 | 1.19 | 0.78, 1.82 | 1.28 | 0.93, 1.78 |
| Noncontact sports | ||||||||
| Did not participate | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Participated | 0.63b | 0.40, 0.99 | 1.40b | 1.02, 1.91 | 0.89 | 0.59, 1.35 | 1.01 | 0.74, 1.40 |
| Follow-up period (from age 19/20 years (0) to age 27/28 years (4)) | 0.90 | 0.75, 1.06 | 1.19e | 1.04, 1.35 | 1.00 | 0.87, 1.16 | 1.13b | 1.00, 1.28 |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; GPA, grade point average; PDM, prescription drug misuse.
a Models with no control variables still included each type of sports participation and a time-varying measure for age.
b P < 0.05.
c P < 0.001.
d The models controlled for the following: time-invariant variables—sex, race/ethnicity, parents’ level of education, urbanicity, US region, cohort year, and average GPA in the participant’s senior year; and time-varying variables—past-30-day cigarette smoking (ages 17/18–27/28 years), past-2-week binge drinking (ages 17/18–27/28 years), past-30-day marijuana use (ages 17/18–27/28 years), and whether the participant was attending college (ages 19/20–27/28 years).
e P < 0.01.
Overall association between different types of competitive sports participation and past-year PDM between ages 17/18 and 27/28 years
Table 3 shows results for the overall association between participation in different types of competitive sports during high school and past-year PDM during early adulthood. With respect to the fully adjusted models, participation in contact sports increased the odds of any past-year PDM (AOR = 1.30, 95% CI: 1.05, 1.61), PDM of opioids (AOR = 1.31, 95% CI: 1.00, 1.71), and PDM of stimulants (AOR = 1.33, 95% CI: 1.05, 1.68) across this 10-year time frame in comparison with respondents who did not participate in contact sports during high school. Moreover, participation in noncontact sports reduced the odds of past-year PDM of opioids (AOR = 0.79, 95% CI: 0.63, 0.99) across this 10-year time frame in comparison with respondents who did not participate in noncontact sports during high school. Additional analyses assessing interaction effects between cohort and sport type (with respect to the overall association with PDM in young adulthood) found no statistically significant results (results not shown).
Table 3.
Adjusted Odds Ratios (Bivariate and Multivariable Tests) for Nonmedical Prescription Drug Use in Early Adulthood According to Type of Sports Participation in High School, Monitoring the Future Study, 2006–2017
| Type of Nonmedical PDM | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Opioids | Stimulants | Tranquilizers/Sedatives | Any PDM | ||||
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Multivariable Associations (No Control Variables) a | ||||||||
| (n = 4,163) | (n = 4,168) | (n = 4,170) | (n = 4,175) | |||||
| Sports participation at age 17/18 years | ||||||||
| Contact sports | ||||||||
| Did not participate | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Participated | 1.59b | 1.26, 2.00 | 1.61b | 1.31, 1.99 | 1.08 | 0.87, 1.34 | 1.45b | 1.20, 1.74 |
| Semicontact sports | ||||||||
| Did not participate | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Participated | 0.98 | 0.80, 1.21 | 1.01 | 0.84, 1.22 | 0.89 | 0.74, 1.07 | 0.93 | 0.80, 1.09 |
| Noncontact sports | ||||||||
| Did not participate | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Participated | 0.85 | 0.70, 1.04 | 1.11 | 0.93, 1.34 | 0.96 | 0.80, 1.16 | 1.03 | 0.88, 1.20 |
| Follow-up period (from age 17/18 years (0) to age 27/28 years (5)) | 0.85b | 0.81, 0.91 | 1.02 | 0.98, 1.07 | 0.97 | 0.92, 1.01 | 0.99 | 0.97, 1.03 |
| Multivariable (Adjusted) Associations c | ||||||||
| (n = 3,838) | (n = 3,842) | (n = 3,842) | (n = 3,846) | |||||
| Sports participation at age 17/18 years | ||||||||
| Contact sports | ||||||||
| Did not participate | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Participated | 1.31d | 1.00, 1.71 | 1.33d | 1.05, 1.68 | 0.95 | 0.73, 1.24 | 1.30d | 1.05, 1.61 |
| Semicontact sports | ||||||||
| Did not participate | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Participated | 1.02 | 0.82, 1.27 | 1.08 | 0.88, 1.32 | 0.90 | 0.73, 1.11 | 0.99 | 0.84, 1.18 |
| Noncontact sports | ||||||||
| Did not participate | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Participated | 0.79d | 0.63, 0.99 | 1.14 | 0.94, 1.38 | 0.92 | 0.73, 1.15 | 0.99 | 0.84, 1.18 |
| Follow-up period (from age 17/18 years (0) to age 27/28 years (5)) | 0.82b | 0.76, 0.89 | 1.03 | 0.97, 1.10 | 0.97 | 0.91, 1.03 | 0.98 | 0.93, 1.03 |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; GPA, grade point average; PDM, prescription drug misuse.
a Models with no control variables still included each type of sports participation and a time-varying measure for age.
b P < 0.001.
c The models controlled for the following: time-invariant variables—sex, race/ethnicity, parents’ level of education, urbanicity, US region, cohort year, and average GPA in the participant’s senior year; and time-varying variables—past-30-day cigarette smoking (ages 17/18–27/28 years), past-2-week binge drinking (ages 17/18–27/28 years), past-30-day marijuana use (ages 17/18–27/28 years), and whether the participant was attending college (ages 19/20–27/28 years).
d P < 0.05.
DISCUSSION
This was one of the first national US studies to assess how different types of sports participation during high school (based on level of contact) are associated with the initiation and developmental course of PDM during the transition into young adulthood. The analyses found that nearly 1 in every 3 high school students had ever reported some PDM prior to high school graduation. Participation in contact sports during high school (compared with their peers who did not participate in these sports) was modestly associated with greater odds of past-year PDM of opioids, PDM of stimulants, or any PDM during the decade following high school (i.e., between ages 17/18 and 27/28 years). Moreover, the analysis found that participation in contact sports during high school was associated with an approximately 50% increase in the odds of initiating PDM of stimulants among respondents with no prior history of stimulant PDM before the age of 19 years. Taken together, these findings reinforce the importance of screening and monitoring high school athletes during adolescence and young adulthood, especially those who participate in contact sports.
While these results confirm prior findings from cross-sectional studies regarding increased risk of PDM among high school athletes who participate in contact sports (11–13), this study extends prior results by showing how this risk of PDM extends into young adulthood. In particular, the risk of PDM of opioids among contact sport participants was highest during 12th grade (i.e., age 17/18 years); however, this risk diminished as they transitioned into young adulthood (i.e., ages 19/20–27/28 years). This decreased risk of opioid PDM may suggest that a potentially risky context (i.e., contact sports) during high school has only a short-term/immediate impact that may be related to these former athletes’ sustaining fewer injuries (due to retiring from contact sports after high school), having less contact with risky peers (removal from risky peer groups), or simply having reduced access to this type of drug (less opportunity to receive diverted opioid medications) as they transition out of high school and into young adulthood (31–33).
The risk of PDM of stimulants among contact sport participants increased after high school and peaked at age 21/22 years. While these athletes probably gravitated away from actively participating in these risker sports after high school (approximately 7% of high school athletes play in college and professionally) (34), exposure to these types of sports may have a longer-term/extended impact on stimulant PDM. For instance, exposure to these risky sporting contexts during adolescence can directly shape norms that view various types of substance use as acceptable and can have a lasting impact on future behavior (18, 35). Moreover, PDM of stimulants is the most common type of PDM for cognitive enhancement among college-age young adults (5, 6, 9, 36), and stimulants are the most diverted type of prescription drug within this age group (4–6). Given that acceptable normative perceptions of PDM may persist into young adulthood and given the relatively easy access to these drugs (e.g., through one’s own or a friend’s prescription), exposure to these types of sporting contexts during high school may shape later misuse of prescription stimulants during early adulthood when risk for this type of PDM is highest.
Another notable finding was that participation in noncontact sports during high school reduced the risk of PDM of opioids during the transition to young adulthood but increased the risk of PDM of stimulants during the same period. Prior cross-sectional studies have found that participation in noncontact sports reduces the risk of common types of substance use during adolescence (i.e., binge drinking, marijuana use, and cigarette smoking) (22, 23, 37, 38). Noncontact sports may provide a more protective context because these types of sports emphasize an ascetic lifestyle that cultivates a normative orientation that values moderation and self-control in order to sustain long-term health (39). Moreover, adolescents involved in noncontact sports have a lower risk of injury (14). The lowered risk of opioid PDM among participants in noncontact sports could be an extension of both the value placed on a healthy lifestyle and the lower risk of injury embedded within these types of sports.
Although noncontact sports may yield a culture of self-control or an aversion to physical harm, this does not mean that competitiveness or an ethic to be best is undervalued. Indeed, prior studies have found that adolescent athletes in noncontact sports have better academic outcomes and aspirations to attend college (37, 40) and may be more likely to view high school sports as a way of building a well-rounded portfolio to be competitive in the college admissions process. Moreover, PDM of stimulants among adolescents and young adults is not only a way to simply get high but also a way to help them concentrate and study (41–44). In particular, approximately half of high school seniors and the majority of college students who reported using stimulants nonmedically during the past year indicated that they used these medications to help them study (42–44). Given that stimulant PDM is typically done for academic performance, the risk of engaging in this type of drug use may also be increased in the subgroup of students who participated in noncontact sports in high school due to a desire to achieve academically.
Finally, no significant interaction effects were found between cohort (i.e., 2006–2009, 2010–2013, or 2014–2017) and sport type. While this may suggest that the associations found in the present study may be similar across cohorts, it must be acknowledged that the prescription of medication (e.g., rates of prescribing opioids, stimulants, and tranquilizers/sedatives) has declined over the past decade (45–47) and PDM (6) among adolescents has changed substantially during the past decade. In particular, PDM of opioids, PDM of stimulants, and PDM of tranquilizers/sedatives have all declined substantially among adolescents since 2010 (6). Given both the lower rates of prescribing and the lower rates of PDM among adolescents, future studies will need to determine whether newer cohorts of adolescent athletes are at a similar risk of PDM when compared with their peers from older cohorts, who had greater access to these types of drugs.
Accordingly, this study provides one of the first longitudinal assessments of how participation in different types of high school sports is associated with the initiation and developmental course of PDM. Current efforts to target high school athletes to reduce opioid misuse should continue, with an increased focus on athletes engaged in contact sports. For instance, certain types of Web-based interventions (i.e., the Student Athlete Wellness Portal) are being developed to address the potential misuse of prescription opioids among high school athletes (48). Efforts like these should continue and should be initiated prior to the beginning of the season in order to minimize the short-term risk period between opioid misuse and participation in contact sports (e.g., exposure to the intervention prior to injuries). Additionally, there must also be a focus on other types of PDM, particularly PDM of stimulants. Given the wider risk among athletes of engaging in PDM in young adulthood, specific interventions will need to be tailored to address this during high school to help reduce this risk in young adulthood.
Despite the many strengths of this study, several limitations must be highlighted. First, the MTF 12th-grade sampling frame does not include those who drop out of high school, are home-schooled, or are institutionalized, so the findings may not generalize more broadly to the young adult population. Second, sample sizes were relatively small, and it was not possible to study each specific sport assessed. Third, despite the fact that the analyses controlled for substance-use behavior at baseline and during subsequent follow-ups, the association between certain types of sports participation and PDM could have been a reflection of the fact that adolescents who engage in risky substance-use behaviors (e.g., PDM) may also be more likely to participate in sports that are high-risk (e.g., contact sports). While this type of spurious relationship may exist between participation in certain types of sports and substance use, targeting athletes in these types of risker sports for intervention would make the most sense, given that a higher proportion of adolescents who participate in these activities may be at greater risk of engaging in PDM.
Regardless of these limitations, this study advances our understanding of how participation in different types of sports influences PDM in young adulthood and provides necessary information to design focused, preventative programs for adolescent athletes.
ACKNOWLEDGMENTS
Author affiliations: Department of Systems, Population and Leadership, School of Nursing, University of Michigan, Ann Arbor, Michigan, United States (Philip T. Veliz); Department of Psychology, School of Medicine, University of Michigan, Ann Arbor, Michigan, United States (John E. Schulenberg); Department of Human Performance, College of Allied Health and Nursing, Minnesota State University, Mankato, Mankato, Minnesota, United States (Jen Zdroik); School of Medicine, Wayne State University, Detroit, Michigan, United States (Kennedy Star Werner); and Department of Health Behavior and Biological Sciences, School of Nursing, University of Michigan, Ann Arbor, Michigan, United States (Sean Esteban McCabe).
This work was partially supported by a research grant (grant 75F40121C00148) from the Food and Drug Administration. The development of this study was also supported by research grants R01DA001411, R01DA016575, R01DA031160, R01DA036541, R01DA042146, and R01DA043691 from the National Institute on Drug Abuse and the National Institutes of Health.
Restricted panel data files from the Monitoring the Future Study are available from the National Addiction & HIV Data Archive Program (https://www.icpsr.umich.edu/web/NAHDAP/studies/37072).
We thank the principal investigators of the Monitoring the Future Study for collecting the data. We also thank the respondents, school personnel, and research staff for their participation in the study.
The funding agencies (Food and Drug Administration, National Institute on Drug Abuse, and National Institutes of Health) had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; the preparation, review, and approval of the manuscript; or the decision to submit the manuscript for publication. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the Food and Drug Administration, the National Institute on Drug Abuse, or the National Institutes of Health.
Conflict of interest: none declared.
REFERENCES
- 1. Pickover AM, Messina BG, Correia CJ, et al. A behavioral economic analysis of the nonmedical use of prescription drugs among young adults. Exp Clin Psychopharmacol. 2016;24(1):38–47. [DOI] [PubMed] [Google Scholar]
- 2. McCabe SE, Teter CJ, Boyd CJ, et al. Sources of prescription medication misuse among young adults in the United States: the role of educational status. J Clin Psychiatry. 2018;79(2):17m11958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hughes A, Williams MR, Lipari RN, et al. Prescription Drug Use and Misuse in the United States: Results From the 2015 National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR2-2015/NSDUH-FFR2-2015.htm. Accessed February 20, 2022. [Google Scholar]
- 4. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration . Results From the 2019 National Survey on Drug Use and Health: Detailed Tables. Prevalence Estimates, Standard Errors, P Values, and Sample Sizes. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2020. https://www.samhsa.gov/data/sites/default/files/reports/rpt29394/NSDUHDetailedTabs2019/NSDUHDetailedTabs2019.pdf. Accessed December 15, 2021. [Google Scholar]
- 5. Schulenberg JE, Patrick ME, Johnston LD, et al. Monitoring the Future National Survey Results on Drug Use 1975–2020. Volume II. College Students & Adults Ages 19–60. Ann Arbor, MI: Institute for Social Research, University of Michigan; 2021. http://www.monitoringthefuture.org/pubs/monographs/mtf-vol2_2020.pdf. Accessed January 16, 2021. [Google Scholar]
- 6. Miech RA, Johnston LD, O’Malley PM, et al. Monitoring the Future National Survey Results on Drug Use 1975–2020. Volume I. Secondary School Students. Ann Arbor, MI: Institute for Social Research, University of Michigan; 2021. http://www.monitoringthefuture.org/pubs/monographs/mtf-vol1_2020.pdf. Accessed January 16, 2021. [Google Scholar]
- 7. Saha TD, Kerridge BT, Goldstein RB, et al. Nonmedical prescription opioid use and DSM-5 nonmedical prescription opioid use disorder in the United States. J Clin Psychiatry. 2016;77(6):772–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sheridan DC, Laurie A, Hendrickson RG, et al. Association of overall opioid prescriptions on adolescent opioid abuse. J Emerg Med. 2016;51(5):485–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schepis TS, Teter CJ, McCabe SE. Prescription drug use, misuse and related substance use disorder symptoms vary by educational status and attainment in U.S. adolescents and young adults. Drug Alcohol Depend. 2018;189:172–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hudgins JD, Porter JJ, Monuteaux MC, et al. Prescription opioid use and misuse among adolescents and young adults in the United States: a national survey study. PLoS Med. 2019;16(11):e1002922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Veliz PT, Boyd C, McCabe SE. Playing through pain: sports participation and nonmedical use of opioid medications among adolescents. Am J Public Health. 2013;103(5):e28–e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Veliz P, Boyd C, McCabe SE. Adolescent athletic participation and nonmedical Adderall use: an exploratory analysis of a performance-enhancing drug. J Stud Alcohol Drugs. 2013;74(5):714–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Veliz P, McCabe SE. Examining potential substance use disorders among former interscholastic athletes. Subst Abus. 2015;36(4):400–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Comstock RD, Collins CL, Corlette JD, et al. National High School Sports-Related Injury Surveillance Study: 2011–2012 School Year. Columbus, OH: Center for Injury Research and Policy; 2012. https://www.nationwidechildrens.org/-/media/documents/108630. Accessed December 11, 2021. [Google Scholar]
- 15. Tham SW, Palermo TM, Chrisman SPD, et al. Prescription opioid misuse and sports-related concussion among high school students in the United States. J Head Trauma Rehabil. 2021;36(5):338–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Veliz P, Epstein-Ngo QM, Meier E, et al. Painfully obvious: a longitudinal examination of medical use and misuse of opioid medication among adolescent sports participants. J Adolesc Health. 2014;54(3):333–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McCabe SE, Veliz P, Wilens TE, et al. Sources of nonmedical prescription drug misuse among US high school seniors: differences in motives and substance use behaviors. J Am Acad Child Adolesc Psychiatry. 2019;58(7):681–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hughes R, Coakley J. Positive deviance among athletes: the implications of overconformity to the sport ethic. Sociol Sport J. 1991;8:307–325. [Google Scholar]
- 19. Stull T, Morse E, McDuff DR. Substance use and its impact on athlete health and performance. Psychiatr Clin North Am. 2021;44(3):405–417. [DOI] [PubMed] [Google Scholar]
- 20. Messner M. Power at Play: Sports and the Problem of Masculinity. Boston, MA: Beacon Press; 1990. [Google Scholar]
- 21. Schaefer BP, Petkovsek MA. Adolescent use of opioids and stimulants: testing the influence of peers, self-control, and sports participation. Crim Justice Stud. 2017;30(4):365–380. [Google Scholar]
- 22. Veliz PT, Boyd CJ, McCabe SE. Competitive sport involvement and substance use among adolescents: a nationwide study. Subst Use Misuse. 2015;50(2):156–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Veliz P, Schulenberg J, Patrick M, et al. Competitive sports participation in high school and subsequent substance use in young adulthood: assessing differences based on level of contact. Int Rev Sociol Sport. 2017;52(2):240–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Patrick ME, Terry-McElrath YM, Schulenberg JE, et al. Patterns of high-intensity drinking among young adults in the United States: a repeated measures latent class analysis. Addict Behav. 2017;74:134–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Schulenberg JE, Patrick ME, Kloska DD, et al. Substance use disorder in early midlife: a national prospective study on health and well-being correlates and long-term predictors. Subst Abuse. 2015;9(suppl 1):41–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Terry-McElrath YM, O’Malley PM. Trends and timing of cigarette smoking uptake among U.S. young adults: survival analysis using annual national cohorts from 1976–2005. Addiction. 2015;110(7):1171–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rice SG, American Academy of Pediatrics Council on Sports Medicine and Fitness . Medical conditions affecting sports participation. Pediatrics. 2008;121(4):841–848. [DOI] [PubMed] [Google Scholar]
- 28. Hanley JA, Negassa A, Edwardes MD, et al. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157(4):364–375. [DOI] [PubMed] [Google Scholar]
- 29. Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44(4):1049–1060. [PubMed] [Google Scholar]
- 30. Patrick ME, Veliz P, Linden-Carmichael A, et al. Alcohol mixed with energy drink use during young adulthood. Addict Behav. 2018;84:224–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McCabe SE, Veliz P, Schulenberg JE. How collegiate fraternity and sorority involvement relates to substance use during young adulthood and substance use disorders in early midlife: a national longitudinal study. J Adolesc Health. 2018;62(3 suppl):S35–S43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bachman JG, O’Malley PM, Schulenberg JE, et al. The Decline of Substance Use in Young Adulthood: Changes in Social Activities, Roles, and Beliefs. Mahwah, NJ: Lawrence Erlbaum Associates; 2002. [Google Scholar]
- 33. McCabe SE, Schulenberg JE, Johnston LD, et al. Selection and socialization effects of fraternities and sororities on US college student substance use: a multi-cohort national longitudinal study. Addiction. 2005;100(4):512–524. [DOI] [PubMed] [Google Scholar]
- 34. National Collegiate Athletic Association . Estimated probability of competing in college athletics. https://www.ncaa.org/about/resources/research/estimated-probability-competing-college-athletics. Published 2020. Accessed February 1, 2022.
- 35. Grace LA, Knight CJ, Rodgers WM, et al. Exploring the role of sport in the development of substance addiction. Psychol Sport Exerc. 2017;28:46–57. [Google Scholar]
- 36. McCabe SE, West BT. Medical and nonmedical use of prescription stimulants: results from a national multicohort study. J Am Acad Child Adolesc Psychiatry. 2013;52(12):1272–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Women’s Sports Foundation . Teen Sport in America: Why Participation Matters. East Meadow, NY: Women’s Sports Foundation; 2018. https://www.womenssportsfoundation.org/wp-content/uploads/2018/01/teen-sport-in-america-full-report-web.pdf. Accessed November 2, 2021. [Google Scholar]
- 38. Ford JA. Substance use among college athletes: a comparison based on sport/team affiliation. J Am Coll Health. 2007;55(6):367–373. [DOI] [PubMed] [Google Scholar]
- 39. Bourdieu P. Sport and social-class. Soc Sci Inf. 1978;17:819–840. [Google Scholar]
- 40. Women’s Sports Foundation . Teen Sport in America, Part II: Her Participation Matters. East Meadow, NY: Women’s Sports Foundation; 2021. https://www.womenssportsfoundation.org/articles_and_report/teen-sport-report-ii/. Accessed November 2, 2021. [Google Scholar]
- 41. Arria AM, Caldeira KM, O’Grady KE, et al. Nonmedical use of prescription stimulants among college students: associations with attention-deficit-hyperactivity disorder and polydrug use. Pharmacotherapy. 2008;28(2):156–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Johnston LD, O’Malley PM, Bachman JG, et al. Monitoring the Future National Survey Results on Drug Use, 1975–2010. Volume I. Secondary School Students. Ann Arbor, MI: Institute for Social Research, University of Michigan; 2011. http://www.monitoringthefuture.org/pubs/monographs/mtf-vol1_2010.pdf. Accessed December 12, 2021. [Google Scholar]
- 43. Teter CJ, DiRaimo CG, West BT, et al. Nonmedical use of prescription stimulants among US high school students to help study: results from a national survey. J Pharm Pract. 2020;33(1):38–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Teter CJ, McCabe SE, LaGrange K, et al. Illicit use of specific prescription stimulants among college students: prevalence, motives, and routes of administration. Pharmacotherapy. 2006;26(10):1501–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Board AR, Guy G, Jones CM, et al. Trends in stimulant dispensing by age, sex, state of residence, and prescriber specialty—United States, 2014–2019. Drug Alcohol Depend. 2020;217:108297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Gagne JJ, He M, Bateman BT. Trends in opioid prescription in children and adolescents in a commercially insured population in the United States, 2004–2017 [published correction appears in JAMA Pediatr. 2019;173(7):704]. JAMA Pediatr. 2019;173(1):98–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Toce MS, Michelson KA, Hudgins JD, et al. Trends in benzodiazepine prescribing for US adolescents and young adults from 2008 to 2019. JAMA Pediatr. 2022;176(3):312–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Real Prevention, LLC . Student Athlete Wellness Portal for Opioid Abuse. withpower.com https://www.withpower.com/trial/phase-opioid-misuse-3-2020-072c8. Accessed March 1, 2022.