Abstract
Shoulder arthroscopy is considered a very safe surgical procedure; however, there are possible complications that are prevalent or devastating. This article presents a 52-year-old woman scheduled for elective arthroscopic rotator cuff repair under general anesthesia in the lateral decubitus position. Postoperatively, the patient experienced dyspnea, chest pain, and oxygen desaturation, and a diagnosis of pneumothorax was made. A chest tube was inserted promptly and the patient was discharged in a good condition, experiencing an uneventful follow-up for the next four months. Knowledge of this uncommon complication may enable both surgeons and anesthesiologists to set up preventive and early therapeutic management.
Keywords: anesthesia, risk factors for pneumothorax, pneumothorax (ptx), rotator cuff repair surgery, arthroscopic shoulder surgery
Introduction
Shoulder arthroscopy is a frequently performed and accepted technique for a wide variety of shoulder pathologies [1]. Despite the increasing use of this safe procedure over the past 20 years, common and rare complications still exist [2]. These complications are classified as preoperative (related to surgeon experience, patient selection or positioning, to anesthesia), intraoperative (neurovascular injury, hardware failure, fluid extravasation, fracture), or postoperative (infection, thromboembolic events, hemarthrosis, persistent pain, stiffness, heterotopic ossification) [3]. Moreover, uncommon, respiratory complications such as pneumothorax have been reported in patients undergoing the aforementioned procedure [4]. Although this complication during shoulder arthroscopy is rare [5], its presence might be life-threatening and prompt diagnosis and treatment are mandatory.
Case presentation
A 52-year-old female, reporting a history of pain in her right shoulder associated with limited function and unresponsive to one-year conservative medical treatment, was admitted to our department. The patient’s body mass index was 22.6 kg/m2 (specifically, 167 cm in height and 63 kg in weight). The patient reported a medical past of hypertension and hyperlipidemia, both being under medication. Medical history of pulmonary diseases (such as bronchial asthma, chronic obstructive pulmonary disease, tuberculosis) or allergies, as well as smoking and/or alcohol habits, was not reported. In addition, the patient had no prior invasive procedures on the shoulder. Physical examination and diagnostic imaging were both consistent with a symptomatic full-thickness rotator cuff tear of the supraspinatus tendon. The patient was classified as status I, according to the Anesthesiologist's Physical Status classification system. The preoperative laboratory findings were within normal ranges, and a chest radiograph showed no abnormality.
In the operating room, the patient was connected to a pulse oximeter, a capnograph, an electrocardiograph, and an automated blood pressure cuff for continuous monitoring of her vital signs. The patient underwent general anesthesia, with intubation being accomplished under direct vision and she was placed in a lateral decubitus position (LDP).
The anesthesia was managed with volume-controlled ventilation (VCV), with an intraoperative tidal volume of 7-8 mL/kg of the ideal body weight, while the administered tidal volume (VT) was specifically at 500-525 mL. The respiratory rate (RR) fluctuated between 12 and 14 breaths/min and the end-tidal carbon dioxide (EtCO2) was maintained between 28 and 36 mmHg. Positive end-expiratory pressure (PEEP) values fluctuated between 4 and 5 cm H2O and the FiO2 value was at 0.5 (50%) in oxygen. The maximum airway pressure values, during arthroscopy with the patient in LDP, were between 20 and 27 cm H2O, the P plateau was between 15 and 20 cm H2O while the lowest saturation in the same position was at 95%. General anesthesia was induced by using Propofol, Fentanyl, and Rocuronium. Sugammadex was administered to reverse neuromuscular block. For anesthesia maintenance desflurane was used in a mixture of oxygen/nitrous oxide 50%.
To perform the arthroscopic procedure, three 5 mm stab standard portal incisions, such as anterior, posterior, and lateral, were used. Moreover, an anterolateral portal presents an alternative working and/or diagnostic role. The procedure consisted of subacromial decompression, acromioplasty, bursectomy, and double-row rotator cuff repair using suture anchors (Arthrex, Naples, FL, USA). A 4.5 mm shaver blade, a 5 mm burr as well as an electrocautery suction device were all the instruments used to accomplish acromioplasty. Particularly, the shaver blade and burr were both consecutively positioned through an anterolateral portal incision. In addition, the acromioclavicular joint excision was performed through the anterior portal. There were no difficulties with trocar placement and bleeding was minimal. During the procedure, the pump pressure was maintained at 50 mmHg and it was kept stable throughout the operation. The total surgical time was 100 minutes. During the procedure, the patient's vital signs were stable (oxygen saturation was 99-100%, systolic blood pressure < 90 mmHg, heart rate from 65 to 70 beats/min) and airway pressure remained unchanged.
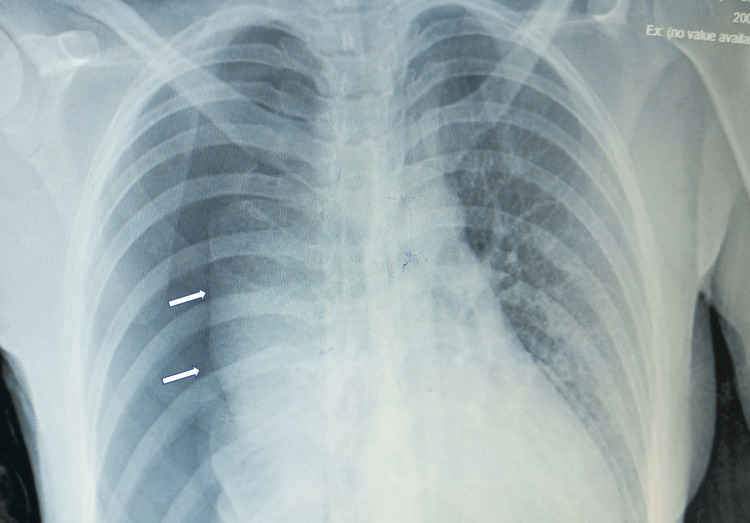
Upon completion of the operation, extubation was achieved with the patient being completely in a status of self-respiration and consciousness. The patient was transferred to the post-anesthesia care unit, where her vital signs were as follows: blood pressure at 120/60 mmHg, heart rate at 70 bpm, RR at 14 breaths/min, body temperature at 36.2oC, and oxygen saturation at 98% with the use of an oxygen mask. Fifteen minutes after recovery, the patient developed dyspnea and chest pain. The oxygen saturation was decreased to 92%, despite the use of a mask for oxygen delivery at a flow rate of five liters per minute, accompanied by a decrease in blood pressure such as 73/47 mmHg along with a simultaneous increase in heart rate at 110 bpm. An urgent portable chest radiograph was performed showing a right-sided pneumothorax (Figure 1).
Figure 1. The chest X-ray shows the right pneumothorax. The two white arrows note the pneumothorax border.
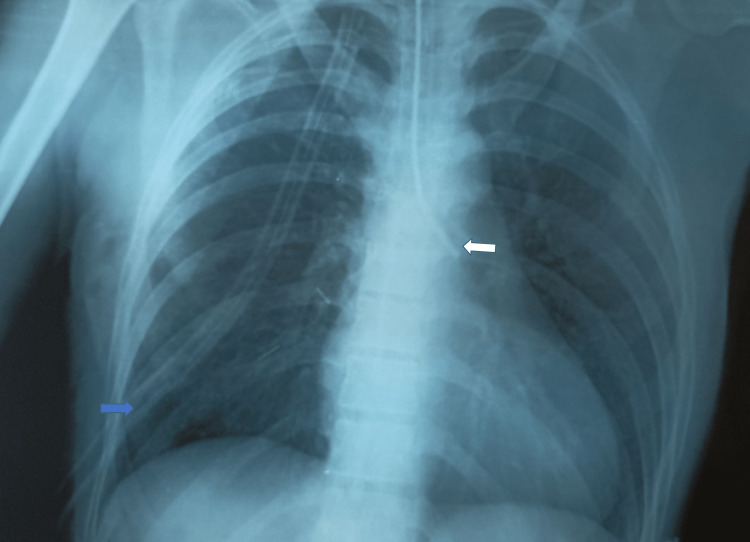
After an immediate thoracic-surgery consultation, a chest tube, with air water seal, was inserted in the theatre. The patient’s vital signs were immediately improved and remained stable (oxygen was completely recovered at a status of 98% saturation, blood pressure at 110/70mmHg, heart rate at 80 bpm, and RR at 12 breaths/min). The repeat chest radiograph revealed successful re-expansion of the right lung (Figure 2).
Figure 2. Chest radiograph showing the successful re-expansion of the right lung after chest tube's insertion (blue arrow). The white arrow represents an endotracheal tube placed in the operating room in order to isolate the left lung thus facilitating the expansion of the pneumothorax.
Three days later, the chest tube was removed and five days after the chest tube's removal, the patient was discharged from the hospital being completely recovered. She was examined one week later, after discharge, in the outpatient clinic department and she did not report any symptoms such as chest pain, dyspnea, and/or shortness of breath. The patient had a follow-up of four months, which was uneventful.
Discussion
To the best of our knowledge, pulmonary complications arising from shoulder arthroscopic invasive procedures are not frequently described in the relevant literature [3,5]. Our patient had an unexpected pneumothorax after a routine procedure of rotator cuff repair, with no obvious or easily identifiable risk factors for the development of this respiratory complication. According to the literature, in most cases, it is difficult to determine the cause of such a complication with certainty [6]. The most prevalent factors include those related to anesthesia (general or regional) [7], technical issues (barotrauma, needle injuries, or pleural puncture), surgical procedures (patient positioning, continuous axial traction in LDP, equipment issues with pumps and suction devices/air entrainment, thermal forces induced by the diathermia) [8] as well as factors related to the patient (smoking habits, underlying lung disease, such as asthma, chronic obstructive pulmonary disease, emphysema, lung bullae, recent thorax trauma, prior history of pneumothorax, obesity, older age, and rare diseases such as alpha-1 antitrypsin deficiency) [9]. In our case, the patient was not obese, with no history of previous pulmonary disease, chest trauma, or smoking habits.
Regarding the correlation with general anesthesia without interscalene nerve blockade, only a few cases of pneumothorax, potentially associated with this type of anesthesia, have been described [10-12]. Numerous possible causes have been hypothesized, such as airway forces, bronchus intubation, and patient risk factors (smoking or lung diseases). The rupture of bullae or bleb seems to be the most common cause of pneumothorax during intubation [13,14]. Moreover, high trans-pulmonary pressure, implying barotrauma, can be attributed to difficult intubation associated with the use of airway exchange catheters or any assisted oxygenation tool with the administered gas being under pressure [11]. In our case, the patient remained stable throughout the procedure, and she was extubated uneventfully. The intubation was performed under direct immediate vision and no bullae were visible on the preoperative chest X-ray.
On the other hand, according to some studies, pulmonary complications occur during shoulder arthroscopy being attributed to the invasive procedure itself [15,16]. The commonest iatrogenic causes are considered to be the high pump pressure [17], changes in pressure in the subacromial space relative to atmospheric pressure, the large volume of irrigation fluids [18], the length of the operative procedure, interscalene nerve blockade technique [19], and the limited surgeon experience [20].
The exact pathogenetic mechanism for the entry of the air, in shoulder arthroscopy, is not clearly known. Nevertheless, it can be considered, that the transitional changes of the pressure emerged in the subacromial space throughout the whole invasive procedure, compared to the atmospheric pressure, facilitate the entry of the air through the lateral portals, causing possible injury to the pleura in association with the invasive handlings, thus leading to pneumothorax occurrence [21-23]. During the arthroscopic technique, the subacromial space is dilated, due to pressure exerted from the injected fluid with the use of an infusion pump, in order to establish a good field of view and most important an appropriate working space. The infusion pump works steadily to maintain a constant pressure. Frequent suction, applied from the instruments used to perform acromioplasty, results in transient falls of the pressure into the subacromial space which becomes negative compared to the atmospheric one. Negation of the pressure into the subacromial space results in air, inserted via lateral portals, trapping in the above space. Also, if the power shaver is turned off, then subacromial pressure becomes positive compared to the atmospheric one, pushing the air from the subacromial space into the surrounding tissue, thus resulting in subcutaneous emphysema [21,24].
Another debatable technical issue related to pulmonary distress is the patients’ positioning (lateral decubitus or beach chair) during arthroscopy. Orthopedic surgeons prefer either the LDP or the beach-chair position (BCP) to perform arthroscopic shoulder procedures with the aim of better visualization and easier access to the surgical field [25]. The LDP has been associated with the potential for peripheral neurapraxia, brachial plexopathy, direct nerve injury, and airway compromise, while the BCP has a higher rate of hypotensive, bradycardia, or cerebrovascular events and cervical neurapraxia [25].
Although the preferred position in most of the studies is the LDP, the authors hypothesized that the use of an arthroscopic pressure pump, combined with power-run shaving devices, was the main factor causing the complication. In our patient’s case, the operating position was also an LDP. However, to date, there is no objective evidence to support that any patient positioning is causally associated with respiratory complications during arthroscopic shoulder procedures [25].
Complications like pneumothorax, appearing in the sequel of invasive diagnostic procedures in the shoulder, such as arthroscopy, might be avoided on the condition that the following will be abided by the orthopedic surgeons: (i) proper placement of the portals, especially the placement of the anteroinferior portal, is considered of great importance; (ii) the outflow and inflow variations should be maintained in balance during the procedure, and the pump lavage fusion must be used as little as possible to avoid major subacromial pressure fluctuations; (iii) the use of sealing dams and arthroscopic cannulas during the procedure seems to prevent air entering through the portals. The preoperative suspicion of potential lung bullae and the prevention of airway trauma during intubation should be the main consideration of anaesthesiologists [25].
Also, the relevant literature reports potential and threatening-life complications arising from shoulder arthroscopy which must be taken into account by anaesthesiologists and surgeons [26]. Moreover, anatomically, the right lung is more developed compared to the left one. Thus, the message of our case is that lesions located in the right hemithorax, when diagnostic techniques are necessitated, can further contribute to the occurrence of complications like pneumothorax, therefore, the whole medical team should be alert when managing such a patient. Table 1 summarizes the cases of respiratory complications following shoulder arthroscopy.
Table 1. A literature review of pneumothorax complications after shoulder arthroscopy procedure.
SLAP: superior labrum anterior posterior
| Author | Age | Mechanism/Diagnosis | Type of Anesthesia | Positioning | Surgical Procedure | Complication(s) | Management | Possible Cause(s) |
| Bamps et al. [5] | 42 | Non mentioned | General | Lateral decubital | Diagnostic shoulder arthroscopy | Pneumothorax | Chest tube | Rupture of parietal pleura, related to the surgical methodology (portal placement and continuous pump infusion with intermittent suction) and subacromial distention used during the procedure |
| Oldman [6] | 41 | SLAP lesion | General | Non mentioned | Arthroscopic subacromial Decompression/SLAP lesion repair | Small pneumothorax | Conservative management without drainage | None |
| Leander-Olsson et al. [7] | 72 | Fracture in fossa glenoidale and partial ruptures in subscapularis and supraspinatus. | Combined interscalene block with ultrasound guidance and general | Beach chair | Arthroscopic rotator cuff and fossa glenoidale fracture repair | Large pneumothorax and extensive subcutaneous emphysema | Chest-drain | Causes related to upper extremity block, general anesthesia, surgical procedure and patient factors |
| Shariyate et al. [11] | 61 | Massive rotator cuff tear | General | Beach chair | Shoulder arthroscopy/Rotator cuff repair | Pneumothorax associated with subcutaneous emphysema which expands to both the neck and the face | Chest tube | Three possible causes: the use of intra-articular shaving/related to general anesthesia/patient factors |
| Lee et al. [13] | 45 | Impingement syndrome | General | Beach chair | Arthroscopic subacromial decompression | Bilateral pneumothorax, extensive subcutaneous emphysema and pneumomediastinum | Chest tubes bilaterally | Transitional changes regarding the subacromial pressure’s values compared to the atmospheric ones, result in air’s insertion in the subacromial space via lateral portal. When the power shaver, connected to a suction device, stops working, the pressure in pump infusion becomes positive dispersing the air in the surrounding tissues, thus creating subcutaneous emphysema. |
| 43 | Impingement syndrome | General | Beach chair | Arthroscopic subacromial decompression | Extensive subcutaneous emphysema and pneumomediastinum | Gradually resolved | ||
| 40 | Impingement syndrome | General | Beach chair | Arthroscopic subacromial decompression | Tension pneumothorax with extensive subcutaneous emphysema and pneumomediastinum. | Chest tube | ||
| Dietzel and Ciullo [14] | 38 | SLAP lesion | General | Lateral decubital | Shoulder arthroscopy/SLAP lesion debridement, and repair | Pneumothorax | Chest tube | Rupture of a bleb or bullae, associated with positive-pressure ventilation and underlying history of heavy smoking, asthma, or underlying lung disease. |
| 22 | Electrocution dislocation/SLAP lesion | General | Lateral decubital | Shoulder arthroscopy/SLAP lesion debridement, and repair | Pneumothorax | Chest tube | ||
| 37 | Motor vehicle accident/labral tear | General | Lateral decubital | Labral tear’s debridement, subacromial decompression with acromioplasty | Pneumothorax | Chest tube | ||
| 34 | Labral tear | General | Lateral decubital | Labral tear repair, subacromial decompression, imbrication of rotator cuff | Pneumothorax | Chest tube | ||
| Li et al. [15] | 56 | Full-thickness supraspinatus tear | Combined interscalene regional and general | Beach chair | Arthroscopic rotator cuff repair | Tension pneumothorax | Chest tube | Accidental damage of the prevertebral fascia, direct eating of the lung parenchyma, during block, leading to bullae ruptures attributed to positive pressure gradients created from ventilation supply when shoulder arthroscopy is performed |
| Kim et al. [17] | 75 | Subscapularis tear | General | Non mentioned | Arthroscopic subscapularis repair | Pneumothorax and subcutaneous emphysema on the chest wall and neck | Chest tube | Extravasation of irrigating fluid |
| Tanoubi et al. [18] | 63 | Rotator cuff injury | Combined ultrasound-guided interscalene nerve block and general | Lateral decubital | Arthroscopic rotator cuff repair | Pneumothorax with subcutaneous emphysema and pneumomediastinum | Gradually resolved | Extravasation of irrigating fluid and air from arthroscopic system |
| Bowden et al. [19] | 30 | Distal clavicle fracture | Combined ultrasound-guided interscalene nerve block and general | Beach chair | Arthroscopic acromioclavicular joint reconstruction and open distal clavicle resection | Large tension pneumothorax | Pigtail catheter | Ultrasound-guided interscalene nerve block anatomical investigation to perform shoulder arthroscopy, causes random perforation of the pleura and/or spontaneous pneumothorax |
| Lau [21] | 62 | Glenoid labral tear | General | Non mentioned | Arthroscopic debridement of the glenoid labral tear | Pneumomediastinum and subcutaneous emphysema | Antibiotic therapy intravenously | Both saline solution and air were extravasated, resulting in subcutaneous emphysema. the subcutaneous air ruptures the prevertebral fascia, allowing air to enter the visceral space of the neck and subsequently the mediastinum |
| Kim et al. [22] | 86 | Rotator cuff injury | General | Beach chair | Arthroscopic rotator cuff repair | Pneumomediastinum associated with subcutaneous and intermuscular emphysema with extension to both the face and neck | Administration of antitussive agent, antibiotics and 5 L/min of oxygen | Mild laceration in the oral cavity/soft tissue structure of the neck loosening by aging process |
| Calvisi et al. [23] | 52 | Subacromial impingement | Scalenic brachial plexus block | Beach chair | Arthroscopic acromioplasty and acromioclavicular osteophytectomy | Pneumomediastinum and subcutaneous emphysema | Spontaneously resolution | Puncture of the prevertebral fascia during scalene block, or high suction shaver, pump and outflow cannula can create a Bernoulli effect |
| Our case | 52 | Rotator cuff injury | General | Lateral decubital | Arthroscopic rotator cuff repair | Pneumothorax | Chest tube | Maybe the positive pressure by the infusion pump during arthroscopy procedure |
Conclusions
Shoulder arthroscopy seems to be a safe and effective technique, based on a review of the literature. Complications like pneumothorax are very rare; however, they could be life-threatening for the patient. The surgical procedure by itself seems to be the most common cause. Portal placement, surgical technique, pump pressure, and continuous irrigation, rarely appear to cause this kind of complication. Traumatic intubation or preexisting pneumo-bullae are also possible causes of pneumothorax emergence. In any case, patients must be informed about the possibility of the later complication. Surgeons and anesthesiologists should be both prepared to deal with this rare event.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Shoulder arthroscopy: the basics. Farmer KW, Wright TW. J Hand Surg Am. 2015;40:817–821. doi: 10.1016/j.jhsa.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Complications associated with arthroscopic shoulder surgery. Weber SC, Abrams JS, Nottage WM. Arthroscopy. 2002;18:88–95. doi: 10.1053/jars.2002.31801. [DOI] [PubMed] [Google Scholar]
- 3.Complications after arthroscopic shoulder surgery: a review of the American Board of Orthopaedic Surgery database. Shin JJ, Popchak AJ, Musahl V, Irrgang JJ, Lin A. J Am Acad Orthop Surg Glob Res Rev. 2018;2:0. doi: 10.5435/JAAOSGlobal-D-18-00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Complications of shoulder arthroscopy. Moen TC, Rudolph GH, Caswell K, Espinoza C, Burkhead WZ Jr, Krishnan SG. J Am Acad Orthop Surg. 2014;22:410–419. doi: 10.5435/JAAOS-22-07-410. [DOI] [PubMed] [Google Scholar]
- 5.Pneumothorax after shoulder arthroscopy: a rare but life-threatening complication. Bamps S, Renson D, Nijs S, Sermon Sermon. J Orthop Case Rep. 2016;6:3–5. doi: 10.13107/jocr.2250-0685.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pneumothorax after shoulder arthroscopy: don't blame it on regional anesthesia. Oldman M, Peng Pi P. Reg Anesth Pain Med. 2004;29:382–383. doi: 10.1016/j.rapm.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 7.Pneumothorax following shoulder arthroscopy under combined regional and general anaesthesia - a case report. Leander-Olsson O, Borglund-Hemph A, Jakobsson JG. Int J Surg Case Rep. 2016;24:73–76. doi: 10.1016/j.ijscr.2016.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pneumothorax following extended latissimus dorsi flap breast reconstruction: rare complication or coincidence? Gandamihardja TA, Chew BK, Weiler-Mithoff EM. J Plast Reconstr Aesthet Surg. 2013;66:1442–1444. doi: 10.1016/j.bjps.2013.04.024. [DOI] [PubMed] [Google Scholar]
- 9.Case report: pneumothorax as a complication of the ultrasound-guided supraclavicular approach for brachial plexus block. Bhatia A, Lai J, Chan VW, Brull R. Anesth Analg. 2010;111:817–819. doi: 10.1213/ANE.0b013e3181e42908. [DOI] [PubMed] [Google Scholar]
- 10.Bilateral tension pneumothorax under anaesthesia. Rastogi PN, Wright JE. Anaesthesia. 1969;24:249–252. doi: 10.1111/j.1365-2044.1969.tb02842.x. [DOI] [PubMed] [Google Scholar]
- 11.Massive emphysema and pneumothorax following shoulder arthroscopy under general anaesthesia: a case report. Shariyate MJ, Kachooei AR, Ebrahimzadeh MH. https://pubmed.ncbi.nlm.nih.gov/29299503/ Arch Bone Jt Surg. 2017;5:459–463. [PMC free article] [PubMed] [Google Scholar]
- 12.Pneumothorax in association with spontaneous ventilation general anaesthesia - an unusual cause of hypoxaemia. Choy MC, Pescod D. Anaesth Intensive Care. 2007;35:270–273. doi: 10.1177/0310057X0703500218. [DOI] [PubMed] [Google Scholar]
- 13.Subcutaneous emphysema, pneumomediastinum, and potentially life-threatening tension pneumothorax. Pulmonary complications from arthroscopic shoulder decompression. Lee HC, Dewan N, Crosby L. Chest. 1992;101:1265–1267. doi: 10.1378/chest.101.5.1265. [DOI] [PubMed] [Google Scholar]
- 14.Spontaneous pneumothorax after shoulder arthroscopy: a report of four cases. Dietzel DP, Ciullo JV. Arthroscopy. 1996;12:99–102. doi: 10.1016/s0749-8063(96)90228-5. [DOI] [PubMed] [Google Scholar]
- 15.Tension pneumothorax after ultrasound-guided interscalene block and shoulder arthroscopy. Li R, Lall A, Lai E, Gruson KI. https://pubmed.ncbi.nlm.nih.gov/26447422/ Am J Orthop (Belle Mead NJ) 2015;44:0–10. [PubMed] [Google Scholar]
- 16.Pathomechanisms and complications related to patient positioning and anesthesia during shoulder arthroscopy. Rains DD, Rooke GA, Wahl CJ. Arthroscopy. 2011;27:532–541. doi: 10.1016/j.arthro.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 17.Chest wall swelling and pneumothorax after shoulder arthroscopy: were the 2 events totally independent? Kim JB, Choi MK, Jeon YK, Lee JM. Medicine (Baltimore) 2017;96:0. doi: 10.1097/MD.0000000000007020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Late subcutaneous emphysema and pneumothorax after shoulder arthroscopy [Article in French] Tanoubi I, Drolet P, Blanchette D. Can J Anaesth. 2010;57:383–384. doi: 10.1007/s12630-009-9258-8. [DOI] [PubMed] [Google Scholar]
- 19.Large asymptomatic pneumothorax following arthroscopic-assisted acromioclavicular joint reconstruction after ultrasound-guided interscalene block: a case report. Bowden BD, Williams WA, Stumpo LA, Stephens SP, DeCoons RM. JSES Int. 2020;4:551–554. doi: 10.1016/j.jseint.2020.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fluid extravasation in shoulder arthroscopic surgery: a systematic review. Memon M, Kay J, Gholami A, Simunovic N, Ayeni OR. Orthop J Sports Med. 2018;6:2325967118771616. doi: 10.1177/2325967118771616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pneumomediastinum caused by subcutaneous emphysema in the shoulder. A rare complication of arthroscopy. Lau KY. Chest. 1993;103:1606–1607. doi: 10.1378/chest.103.5.1606. [DOI] [PubMed] [Google Scholar]
- 22.Pneumomediastinum after arthroscopic shoulder surgery - a case report. Kim HK, Ko ES, Kim JY, Park JM, Kim JY, Woo NS. Korean J Anesthesiol. 2013;64:376–379. doi: 10.4097/kjae.2013.64.4.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Subcutaneous emphysema and pneumomediastinum following shoulder arthroscopy with brachial plexus block: a case report and review of the literature. Calvisi V, Lupparelli S, Rossetti S. Arch Orthop Trauma Surg. 2009;129:349–352. doi: 10.1007/s00402-008-0593-y. [DOI] [PubMed] [Google Scholar]
- 24.Pneumothorax associated with tube exchanger-aided intubation following LMA-Fastrach placement in a patient during anesthesia induction. Chen WY, Lin JA, Chen HL, Wong CS, Ho ST, Lu CC. https://pubmed.ncbi.nlm.nih.gov/15679133/ Acta Anaesthesiol Taiwan. 2004;42:227–231. [PubMed] [Google Scholar]
- 25.Patient positioning in shoulder arthroscopy: which is best? Rojas J, Familiari F, Bitzer A, Srikumaran U, Papalia R, McFarland EG. Joints. 2019;7:46–55. doi: 10.1055/s-0039-1697606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Postoperative management of spontaneous pneumothorax in arthroscopic shoulder superior capsular reconstruction: a case report and review of literature. Lin YJ, Chen GX, Zhang Y. Chin J Traumatol. 2022;25:181–183. doi: 10.1016/j.cjtee.2022.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]