Highlights
-
•
Migrants account for over two-fifths of new HIV diagnoses in Europe.
-
•
More than half of all women in Europe are diagnosed late with HIV.
-
•
Structural, sociocultural, and individual factors are the main barriers to HIV testing.
-
•
Focused interventions are needed to address the inequalities in healthcare.
Keywords: HIV, Late diagnosis, Migrant women, Barriers, Inequalities
Abstract
Objectives
HIV transmission persists in Europe, with migrants accounting for over two-fifths of new diagnoses. Over half of all women in Europe are diagnosed late — particularly migrant women. Therefore, an updated understanding of migrant women's needs is crucial to inform inclusive and relevant HIV research, services, and policies.
Methods
A systematic review relating to factors influencing late HIV diagnoses among migrant women living in Europe in 2011–2021 was conducted, based on data from 12 papers relating to 13 European Union (EU) countries and three non-EU countries.
Results
The studies revealed a range of individual, sociocultural, and structural barriers to HIV diagnosis. Individual barriers included low perceived risk of HIV, lack of knowledge about HIV symptoms and HIV services, lack of trust in healthcare systems, and fear of societal implications of an HIV diagnosis. Sociocultural barriers included language and communication challenges, stigma, and lack of community testing opportunities. Structural factors included poverty, poor living conditions, unclear legal rights, administrative barriers to healthcare access, and lack of testing opportunities.
Conclusions
Barriers varied according to resident country, healthcare system, and country/region of origin. The studies highlighted the importance of inclusive research and service design and development, to address the needs of migrant women and reduce inequalities, especially given the current climate in Europe and the everchanging patterns of migration.
Introduction
Over the past decade there has been a 19% increase in new HIV diagnoses in Europe, of which heterosexual women account for 24%. In 2019, 44% of those newly diagnosed with HIV were migrants, from sub-Saharan Africa (18%), Latin America/Caribbean (9%), Central/Eastern Europe (8%), and Western Europe (3%) (ECDC, 2020a).
Over half (53%) of women with HIV are diagnosed late in Europe (CD4 < 350 cells/ml or AIDS-defining illness). Late presentation is more common among migrant women, especially those from sub-Saharan Africa (57%), and South/Southeast Asia (54%) [1]. Nevertheless, evidence suggests that migrants face barriers to accessing prevention and testing services, and that they are not routinely prioritised in national guidance and recommendations.
The ECDC states that action to remove those barriers faced by undocumented migrants it is a priority (ECDC, 2020a). Emerging evidence indicates that a significant proportion of migrants, even those originating from HIV-endemic areas, acquire HIV after arrival in the European Union (EU)/European Economic Area (EEA), suggesting the need for targeted HIV prevention and testing programs on and beyond arrival, including regular HIV testing [2], [3], [4].
More accessible testing and combined prevention/care services are needed for the diverse group of migrants at risk of, or living with, HIV [3]. Identifying and removing structural barriers, such as limited eligibility for healthcare due to uncertain residency status, and facilitating a non-discriminatory healthcare environment can increase the effectiveness of these interventions [1]. Unlike with other key populations (men who have sex with men (MSM) and people who inject drugs (PWID)), there is no clear guidance on the key components of prevention that should be available for migrants, or specifically for migrant women, although community-based testing is recommended by the World Health Organization (WHO) [5]. The European Centre for Disease Prevention and Control (ECDC) 2021 progress report [6] outlines HIV testing recommendations as reported within country-specific guidelines. The progress report states that 90% of the countries that have published national HIV testing guidance have included content specific to the needs of key populations. While PWID and sex worker populations were included in 82% and 74% of guidance documents, respectively, the lowest rates were among migrants and transgender people, with particularly low rates in Eastern Europe. Similarly, among those countries with published recommendations on frequency of testing for key populations, migrants and transgender people were the least likely population groups to be mentioned.
Migrant women have an increased risk of HIV acquisition. Therefore, any failure to address their rights, needs, and access to healthcare threatens broader HIV prevention efforts in Europe.
Aim
Our study involved a systematic review of the available evidence, to provide an updated understanding of the reasons for late HIV diagnoses among migrant women living in Europe. The specific research question was: Which factors influence late HIV diagnosis among migrant women residing in Europe?
Our review used the United Nations International Organization for Migration (IOM) definition of migrants — any person crossing an international border or within a state away from his/her habitual place of residence, regardless of: (1) legal status; (2) voluntary or involuntary movement; (3) causes for the movement; or (4) length of the stay.
Methods
Search strategy and selection criteria
Our review included studies published in English, with data gathered in the EU, the EEA, Switzerland, or the UK between January 1 and September 1, 2021.
Studies were eligible for inclusion if: their population included migrant women (cis and trans) and included information specifically based on migration status/country/region of origin or in which at least 80% of the study populations were from countries with generalized HIV epidemics. The studies were also included if they reported any of the following:
-
•
reasons for late HIV presentation
-
•
barriers to HIV testing among women diagnosed with HIV
-
•
facilitators or motivators supporting HIV testing
Due to the anticipated paucity of relevant data, all study and report types were screened. These included reports, all types of research, systematic reviews, scoping reviews, and grey literature.
Three electronic databases (PubMed, EMBASE, and PsychINFO) were searched between August 19 and September 1, 2021. A detailed search strategy was used, combining synonyms for “HIV”, “migrant”, “Europe”, “barrier”, and “facilitator”, with demonyms for all countries with a generalised HIV epidemic [7].
Eligibility and quality assessment
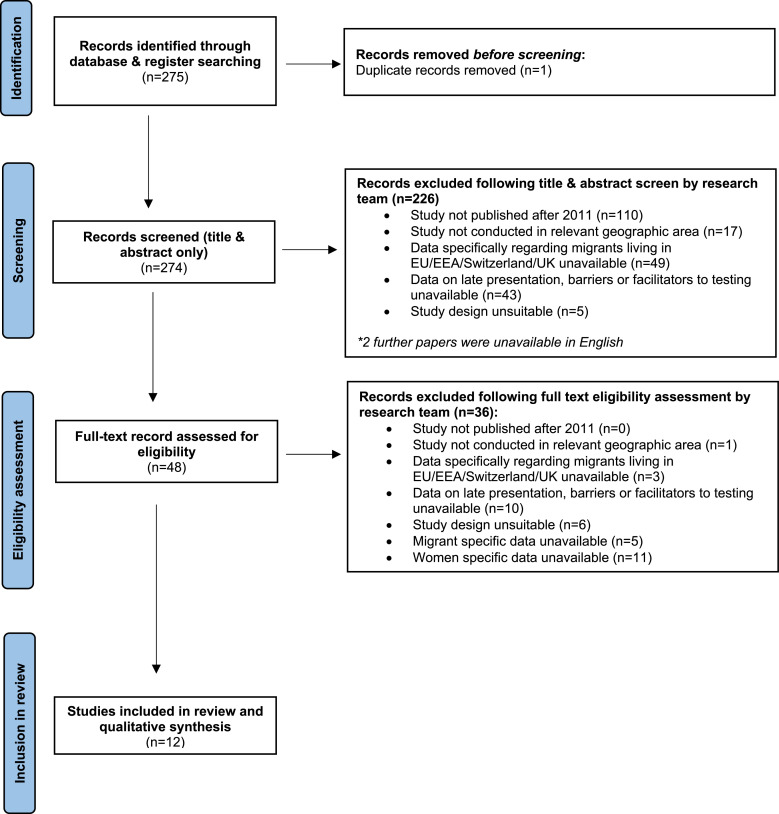
Screening was performed by a team of reviewers using the successive application of the criteria shown in Figure 1. Decisions were double-checked by a third reviewer to resolve possible discrepancies.
Figure 1.
Identification of studies via PubMed, Embase, and PsycINFO.
Data quality appraisal
To ensure quality in extraction, the authors initially extracted data simultaneously from four randomly selected studies, using the Critical Appraisal Skills Programme, to assess the findings for congruence.
Studies received an overall quality score, incorporating several factors such as:
-
i.
Research question — exploring the extent to which the paper was based on a clearly defined research question, which was clearly discussed and referenced throughout the paper.
-
ii.
Internal validity — exploring the extent to which the study design was appropriate for the research question and stated study objectives. The reviewers noted how selection bias and confounding factors were identified and minimized/controlled, and the extent to which the explanatory variables chosen were based on sound scientific principles. The reviewers also discussed the completeness and reliability of outcome measures.
-
iii.
Clarity of results — considering how far the results were well described and clear, the appropriateness of analytical methods, and whether the precision of association given (or that was calculable) was meaningful.
-
iv.
External validity — the reviewers considered whether the source population was well described, the eligible population represented the source population, and whether the selected participants represented the eligible population. The results were reviewed in the context of other studies to explore consistency and generalizability to the source population.
-
v.
Strength of association and statistical significance — the reviewers considered (when applicable) whether the study was sufficiently powered, and whether precise outcomes could be/had been measured. Where reported, the suitability of the stated confidence intervals and/or p-values was considered. Studies were considered in the context of their type, and were given an overall quality score of ‘low’, ‘medium’, or ‘high’. Studies based on surveillance or cross-sectional data received overall quality scores of ‘medium’ or ‘high’.
Data extraction, synthesis, and analysis
The studies were grouped according to the outcomes of interest (reasons for late presentation, barriers, and facilitators) and three reviewers were involved in identification and synthesis of the evidence. Given the inclusivity of study designs, the focus on barriers and facilitators regarding HIV testing, and the variation in study designs, statistical meta-analysis was not deemed appropriate for this review.
Results
Twelve papers were found to have an overall quality score of ‘medium’ or ‘high’ and were included in the final review. The papers related to 13 EU countries Austria [1], Belgium [3], Denmark (ECDC 2020b), France [4], Germany [3], Greece [4], Italy [3], Malta [1], The Netherlands [8], Poland [1], Portugal [2], Spain [8], Sweden [5] and three non-EU countries (The Republic of Ireland [5], Switzerland [5], and the UK [9]. Five studies reported data relating to migrants from multiple countries, including pan-European cohort studies and surveillance databases [8], [9], [10]; Migrants Working Group on behalf of COHERE in EuroCoord; [11]. Figure 1 summarises the study selection process and outcomes at each stage, and Table 1 provides a summary of papers included in the review, with notes concerning the study type, country/ies, population, methods, sample size, results/outcomes, quality scores, biases, and limitations. Observations were discussed and were compiled by two reviewers who read the full texts of all sources included in the review.
Table 1.
Summary of 12 papers included in the review — characteristics of studies.
| Study reference | Study type | Country/ies | Population | Methods | Sample size | Results/outcomes | Quality scores | Bias and limitations |
|---|---|---|---|---|---|---|---|---|
| 14 | Cross-sectional and descriptive quantitative study | Sweden | Migrants from sub-Saharan Africa (SSA), Eastern Europe and Asia, including women, aged 18+ diagnosed with HIV-1 within last 6 months | Questionnaire (English; Swedish) interpreters available Recruitment in 11 HIV clinics |
285 in total 111 female (39%) 190 born outside of Sweden (122 SSA; 36 Eastern Europe, 32 other) |
|
++ | Majority of population studied were men The only gender-based data were the odds of having personal/structural/social/confidentiality barriers between men and women – no difference was observed |
| 22 | Cross-sectional study | Belgium, Germany, Greece, Italy, Netherlands, Portugal, Spain, Switzerland, UK | Migrants living with HIV, aged 18+, diagnosed with HIV within 5 years of arrival. | Questionnaires in 15 languages distributed via 57 HV clinics | 2093 respondents (31% women), from 152 different countries: 35.1% Africa; 31.6% Latin America and Caribbean, and 23.0% Europe | 32.2% of women had experienced difficulties with health services since migration, of whom 1/3 cited long waiting times in clinics, 22% did not trust GP/confidentiality, 19.9% unclear of legal rights to access care
|
+++ | Convenience sample 24 transgender people excluded |
| 28 | Surveillance data from The National Study of HIV in Pregnancy and Childhood (NSHPC) database | UK | Pregnancy data where live or stillbirth is recorded | Statistical analysis of Surveillance data | 4289 births among migrant women | Being of African origin was associated with late booking of antenatal care, including among those newly diagnosed with HIV Cultural/socioeconomic factors resulted in delays in accessing antenatal care and HIV testing in antenatal settings; later diagnosis outside of London |
++ | Women cannot book antenatal care until arrival in the UK Missing data for 9% Respondents may report different dates from national data sets Methods section made it difficult to ascertain where the data sets came from, i.e. the survey vs clinical data collection |
| 37 | Cross-sectional survey | Netherlands | Migrant women | Survey and clinical data (aMASE) | 20 | Diagnosis in hospital for non-MSM due to other health problems Difficulties accessing services due to migrant status — unsure of rights to access healthcare/language barriers Lack of knowledge of PEP in migrant population |
+++ | Small sample of migrant women No non-migrant women were included due to low numbers Only corrected for age; no other multivariate analyses performed, so difficult to separate the effects of migrant status and socioeconomic status |
| 39 | Clinical data collection | Spain (Madrid, southeast and Canary Islands) | Migrant women | Clinical data collection in mobile HIV testing unit | 5920 | Perception of low risk due to feeling healthy/perceived low risk behaviour Fear of rejection if testing positive; fear of legal issues; affordability of testing in migrant community Concerns arising from the loss of anonymity was the second most reported reason for not testing (19%) |
++ | Not representative samples |
| 57 | Qualitative/observational | Amsterdam, Netherlands, and non-EU (Belarus, Moldova, Russia, Ukraine) | Female sex workers | 3 phases: semi-structured interviews with stakeholders, narrative interviews with FSWs, narrative interviews with stakeholders | Number of interviews: 19 stakeholders, five FSW, 12 stakeholders | Six key barriers to testing: 1. migration and sex-work policies; 2. stigma; 3. lack of trust in healthcare providers; 4. low levels of Dutch/English language; 5. negative experiences in accessing healthcare; 6. low perceived risk | ++ | Small number of FSW (5) |
| 60 | Retrospective analysis of data from four cohorts | Belgium, Denmark, Germany, Italy, Netherlands, Poland, Sweden, UK, Ireland, Spain | Migrant women who delivered a child between 2002 and 2012 | Data from four cohorts from 10 European countries Three markers of suboptimal PMTCT interventions compared between migrants and natives |
9421 migrant women | Wider access to HIV testing and care would give migrant women an opportunity to know their HIV-status before conceiving Particular attention should be given to facilitate access to services for migrant women with children Also reports that other studies have highlighted time or financial constraints, language and cultural barriers, and living and working conditions |
+++ | Definition of migrant based on the country of birth No distinction between ethnicity, legal status, time of arrival Women whose country of birth was unknown were excluded (n = 445) Data from four different cohorts |
| 65 | Cross-sectional survey | Belgium, France, Germany, Greece, Italy, Netherlands, Portugal, Spain, UK | People 18+ living outside of their country of birth, irrespective of HIV status, 2014–2015 | Online survey in 14 languages | 559 migrant women | Reasons for not testing: 83.3% low perceived risk; among those who had never tested for HIV — fear of positive test, lack of knowledge about HIV/AIDS; information about access to primary care — varied between different countries of origin; missing appointments/delaying medication for financial reasons | +++ | Convenience sample, focusing on those at a higher risk of HIV (sub-Saharan Africans, Latin Americans, gay or bisexual men, and people who inject drugs) Unknown participation rate as the survey was freely accessible online |
| 110 | Observational cohort study | EU; COHERE participants, where ethnic and geographical origin data available HIV-positive, antiretroviral-naive people accessing care in western Europe from COHERE |
Crude and adjusted mortality rate ratios were calculated by use of Poisson regression, stratified by sex, comparing each group with the native population | 45 877 migrant women | Results focused on mortality rates; no barriers presented in the results section Within discussion section, there were indications of potential barriers, including gender, socioeconomic status, and poor living conditions |
+++ | Difficulties in defining geographical origin; loss to follow up; not all cohorts were able to cross-match their data with the corresponding national death registries; could not adjust to socioeconomic status | |
| 125 | Qualitative observational | UK | African migrant community | Focus groups (conducted in French and Portuguese) | 18 women of the following language (and origin): French (Cameroon), Portuguese (Guinea Bissau), Bemba (Zambia), and Shona and Ndebele (Zimbabwe) |
|
+++ | Purposive sampling; only able to access participants that were members of the community organisation Literature review identified few studies in the regional area under study |
| 140 | Qualitative observational | London, UK | Healthcare leads | Semi-structured interview | 20 | Existing screening models are not perceived to be widely accessible to the new migrant community The main barriers that discourage use are the disease-related stigma present in their own communities, and services being perceived as non migrant friendly New migrants may be disproportionately affected and delays to screening may impact on health status |
++ | Views expressed by participants based on their own experiences and may not reflect wider community No other limitations stated No tabulated data specific to women Focused on healthcare leads within organisations Did not include any data from service users |
| 152 | Qualitative observational | Nottingham, UK | Migrant women from the African community | Focus groups conducted in local community venues (e.g. mosques, churches) | 29 women | Lack of knowledge:
|
+++ | No tabulated data specific to women The decision to adopt a broad-based approach to recruitment rather than sampling on the basis of previous HIV testing experience may have prevented more nuanced insights around testing from emerging Time and language constraints Use of HBM has its own limitations |
Discussion
This narrative synthesis summarised the studies included in this review and highlighted the barriers to HIV testing reported as affecting migrant women living with HIV in Europe. The review did not identify specific reasons for late HIV diagnosis among migrant women, or the facilitators of HIV testing specific to this population.
The main barriers to HIV testing among migrant women related to structural, sociocultural, and individual factors, which often intertwined, as described below.
Structural barriers
Several structural factors were reported to prevent HIV testing among migrant women, relating to the socioeconomic and legal contexts of seeking HIV testing as a migrant. In a cross-sectional survey in Sweden, 42% of respondents experienced structural barriers to HIV testing [12].
Poverty and/or poor living conditions were reported as preventing women from seeking HIV testing [13]. A study from the Netherlands reported lower incomes among migrant women than among migrant heterosexual men, with the former statistically less likely to be in work [14].
In some countries, legal issues, such as unclear/limited legal rights and/or administrative barriers to accessing healthcare due to immigration status, make HIV testing challenging or impossible [8,14]. Half of migrant women in the Netherlands were unsure of their rights to access healthcare [14]. Furthermore, women who had been trafficked or involved in sex work faced heightened barriers to healthcare, related to living conditions and national sexual health policies [11].
World region of birth and immigration status have been found to influence access to care [9]. Studies have reported screening to be inaccessible to migrants, with no screening offered on arrival, delays in providing screening, and further testing opportunities and referral to genito-urinary clinics restricted to those were symptomatic [15]. A study from the UK found that existing screening models were not perceived as widely accessible to the new migrant community [4]. A pan-European cross-sectional survey, including approximately 1000 migrant women, found that structural obstacles strongly affected access to HIV testing among this population [8].
Women miss out on testing opportunities when offered tests exclusively within antenatal services. There are other reports of missed opportunities: only 11.4% of women who visited a GP before HIV diagnosis recalled being offered an HIV test, and only 66% recalled being offered an HIV test at a sexual health clinic [8]. In the same study, migrant women were mostly diagnosed in a hospital setting (40.1%), followed by a general practitioner (GP) setting (17.5%), and a sexual health or HIV testing clinic (12.5%); 14.7% of diagnoses among migrant women were made in ‘other’ settings [8]. These data suggest the need for HIV testing to be offered consistently in a wide range of accessible settings.
The role of primary care in HIV testing is highlighted in some studies: in a multinational study, 73.3% of migrants had access to primary care, with the majority having used services within the previous year [9]. Access to primary care among migrant women ranged from 96.8% in northern Europe to 56.4% in southern Europe [9]. However, only 14.2% had been offered an HIV test by their GP, to which 13.3% agreed. These data suggest that expanding HIV testing within general practice is integral to increasing testing numbers among migrant women. Another study exploring clinical and survey data from the Netherlands suggested that improved access to HIV testing, through provider-initiated testing, may particularly benefit migrant women [14].
Although not statistically significant, one survey found that migrant women who had spent a longer period in Sweden reported more barriers to testing compared with more recent migrants [12]. This suggests a need to explore windows of optimal opportunity for HIV testing alongside routine arrival and antenatal screening options. This was also shown in a recent study by Borchmann et al. (published after our analysis and thus not included in our review), which found that migrants diagnosed with HIV after migration had higher rates of late presentation (up to 68% for specific subgroups) and had been in the host country 3.7 years by the time of diagnosis [16].
Sociocultural barriers
Migrant women in Europe arrive from a variety of countries and socioeconomic backgrounds, and thus have differing cultural approaches to seeking healthcare. Cultural barriers were cited in two studies as preventing HIV testing [13,17]. Cultural, religious, and language norms may delay HIV diagnosis.
African communities tended to seek medical care only when someone was very unwell. This relates to a knowledge gap regarding the importance of HIV testing even when asymptomatic [17]. However, one cross-sectional survey showed no statistically significant differences between migrants from Africa and those from other regions in terms of access to primary care (except for Latin America and Caribbean populations) [9]. This indicates that wider structural issues affecting migrants may play a larger role than sociodemographic characteristics, cultural practices, or individual health status [9].
One quarter of the review studies reported language as a barrier to HIV testing [11,14,17]. Two qualitative studies from the UK and the Netherlands reported language as an important mediator, which may either support or impede women's navigation through the local health system, and may help build trust between service users and healthcare professionals [11,17]. A qualitative study recommended the integration of interpretation services within HIV services to help African communities [18]. Moreover, developing appropriate sociocultural frameworks within HIV services could address challenges and facilitate testing.
Fear was a reported barrier to testing. This was related to HIV as a serious infection, but also to the possible social consequences of living with HIV, because of the enduring social and self-applied stigmatization [12,17,19]. Both social and self-applied stigmatization were reported as barriers to HIV testing in two of the papers in the review [16,11]. Half of the studies reported the fear of social consequences as a major barrier to HIV testing. The fear of discrimination and rejection from their communities, and concerns over a lack of community support, were powerful in preventing women from seeking HIV testing [9,17,19]. Among migrants from Latin America, fear over losing social status was also reported [19].
One qualitative study reported that fear of discrimination may be a barrier to accessing services for black African community members, and that women may feel too uncomfortable discussing intimate problems with male practitioners [18]. Other reviewed studies indicated that poor access to services and strained relationships with healthcare providers, due to cultural and language differences, led many Africans in the UK to present late for HIV care, and that this was supported by previous studies [20,21].
The role of community projects incorporating HIV testing was suggested in one study from the Netherlands, with 70% of migrant women in the studied population attending a religious service at least annually [14]. Several studies highlighted the benefits of including communities in their research, and the potential benefits of doing so in policy making (migrant women, sex workers) and education of healthcare workers (particularly GPs/junior physicians, who are often the first contact) [14,17].
Individual barriers
Several studies reported that low risk perception was a key barrier to HIV testing among migrant women [9,11,16,17,19].
A qualitative study of female sex workers found that low perceived risk presented a barrier to HIV testing, and was linked with low educational levels [11]. Pregnancy and childbirth have been found to increase a woman's self-perceived risk, resulting in improved healthcare-seeking behaviour and thus increased opportunities for HIV testing [11]. This was consistent with findings from previous studies [9,[22], [23], [24], [25], [26], [27]. A UK-based qualitative study reported that HIV risk perception was largely formed by previous personal experiences, which for many had been in Africa. HIV risks were associated with life in Africa rather than the new host country [17]. There was a perception that people within the community were protected from HIV — for example, because their religious beliefs may prevent risky behaviours [13]. In a study conducted in the Netherlands, female sex workers (FSWs) working online were less likely to perceive themselves as ‘sex workers’ [9].
Lack of knowledge was reported to prevent migrant women from seeking HIV testing. This pertained to a lack of clarity regarding migrant women's legal rights to access care in the host country, and a lack of knowledge about HIV/AIDS symptoms and about the importance of asymptomatic testing [8,9,14,[17], [18], [19]. The knowledge gap regarding the perceived risk of infection and the need for asymptomatic testing was significant in migrant women aged below 20 and over 60 years [25]. In one study, one in ten women lacked basic HIV knowledge, with 48.8% not knowing where to access free condoms [9]. Many studies reported lack of awareness of available services and access information as other barriers to HIV testing [9,18]. This was consistent with other studies, and highlighted a continued need to raise awareness about HIV prevention, testing, post-exposure prophylaxis (PEP), and pre-exposure prophylaxis (PrEP) among migrant women [14].
Other studies reported a lack of trust in the consulting physician [11,17]. In one study, 22% of women reported that they did not trust their GP [8]. Another described non-welcoming or unfriendly services as a barrier to seeking HIV testing [16]. A UK-based study reported concerns about being stereotyped and not being treated as an individual, thus highlighting trust and communication barriers [11,17].
Fear of not only societal implcations, but also medical consequences of HIV diagnosis was a major and commonly reported barrier to HIV testing among migrant women. Fear was related to the physical consequences of HIV, illness and morbidity, and impact on sexual life, which may also indirectly point to a lack of knowledge about U=U (undetectable = untransmittable) [12].
Strengths and limitations of this review
This review brought together existing evidence regarding factors relating to late HIV diagnosis among migrant women in EU/EEA/Switzerland/UK, and identified the barriers and possible facilitators regarding HIV testing among this population. The paucity of published literature (12 papers covering information from 16 countries, five of which were pan-European studies) made it difficult to gain a nuanced understanding of the factors that affected women specifically across all studies. Some studies provided evidence indicating the need for HIV testing facilitators, but this was not always documented explicitly in relation to migrant women. The heterogeneity of the data made it challenging to recommend definitive actions for addressing structural, social, and individual barriers to HIV testing among this population.
Limitations of our review methodology may have led to a failure to obtain more relevant information. No papers were retrieved that exclusively discussed reasons for late HIV diagnosis or facilitators of HIV testing among migrant women. Few papers were retrieved based on data from Central and Eastern Europe, where especially non-EU countries have significantly different structures, economic characteristics, rules, and regulations. Moreover, the barriers to HIV testing in those countries and for migrants of different origins (including those not only from African or Latin American countries, but also from the Middle East, with completely different cultural and social characteristics) may be significantly different from those in the EU/EEA or Western European countries. Thus, the results of this study may not be generalized for all of Europe. It is noteworthy that our review did not include data concerning populations affected by the current migration from Eastern European war zones. It is also possible that publication bias and imprecision within the review affected the outcomes reported.
Suggestions for further research
High rates of late HIV diagnosis and, among cases, poor reported experiences with HIV care systems and physicians, highlight migrant women as being a key population in need of better access to HIV testing, treatment, and care. More extended and focused studies and interventions are urgently needed to explore and address the issues faced by these populations in Europe, especially in light of the continually changing migration situation.
This review highlights the need for more research, more culturally appropriate policies and programmes, and more culturally competent practices, in order to address the following:
-
•
Structural and policy changes affecting access to HIV testing, treatment, and care services.
-
•
Testing opportunities for women outside of sexual health and antenatal/pregnancy settings.
-
•
Different approaches towards different subpopulations, including regions of origin and residence, as well as family and work status.
-
•
Attitudes of healthcare professionals towards HIV testing in community settings, stressing the importance of broader testing opportunities.
-
•
Recruitment and training needs (e.g. cultural competence, increased diversity, language skills) for healthcare professionals.
-
•
Sociocultural changes and community education over time, which impact social stigma and fears.
-
•
Access to translation and interpreter services.
-
•
Easier and more accessible repeated testing opportunities post migration.
-
•
Improved access to information about HIV, STIs, and sexual health.
-
•
Information about available healthcare services in the host country, in terms of eligibility and accessibility, including any financial support available.
Conclusion
Both HIV transmission and the migration situation in Europe are fluid and unpredictable. Migrant women are a key population for HIV acquisition. However, few data have been reported over the past decade, specifically relating to the barriers and facilitators of HIV testing among this group in Europe. Further research to review factors that delay or facilitate HIV diagnosis among these populations is needed.
Many studies have reported on individual behavioural choices that have led to delayed HIV testing. This model places the emphasis on the individual's responsibility for their own health rather than examining the sociocultural and structural factors impacting migrant health-seeking and community experiences, and subsequent outcomes related to late HIV diagnosis. Our review included studies reporting on the structural barriers presented by national healthcare policies and migrant population access to care being as significant as barriers to HIV testing and care. Therefore, interventions that address structural barriers, and support early and frequent HIV testing, may be more effective.
This review has highlighted the distinct lack of available data on a susceptible, diverse, and growing population in Europe. Focused interventions and extended research are needed to address the inequalities in healthcare experienced by migrant women. The removal of barriers to accessing HIV testing, minimizing individual and social stigma, and a focus on early testing and diagnosis are urgently needed. This will require support from non-governmental organisations and immigration authorities, in addition to ongoing education and upskilling of healthcare workers who provide care for socially marginalised groups, including migrant women. Changes to wider health policies and practice are likely to influence structural barriers to HIV testing — for example, rights to healthcare for documented versus undocumented migrants [3]. Importantly, taking an inclusive approach to research and service design and development may ensure that the experiences, perceptions, and needs of migrant women are embedded from the outset.
Competing interests
MD, DK, and PL declare no competing interests. NW has been a clinical investigator for Abbvie and MSD, with honoraria paid to her department.
Acknowledgments
Funding
One of the authors, MWO, was paid for data collection and analysis by EACS as part of a self-funded project, Women Against Viruses (WAVE) in Europe. The WAVE project is supported by unrestricted educational grants from Gilead Europe, ViiV Healthcare, and MSD. These pharma companies have no influence on the content or organization of projects. The educational grants received from the pharma companies can only be used for the funded activities.
Ethical approval statement
Development of this manuscript did not involve direct research on human subjects and therefore approval by an institutional review board was not required.
Acknowledgements
The authors would like to thank the EACS Secretariat for its administrative support.
Footnotes
PROSPERO registration number: CRD42021275713
References
- 1.European Centre for Disease Prevention and Control World Health Organization Regional Office for Europe. HIV/AIDS surveillance in Europe. 2020 www.ecdc.europa.eu/sites/default/files/documents/hiv-surveillance-report-2020.pdf Technical report. (Accessed March 8, 2023) [Google Scholar]
- 2.Álvarez-Del Arco D, Monge S, Rivero-Montesdeoca Y, Burns F, Noori T, Del Amo J. Implementing and expanding HIV testing in immigrant populations in Europe: comparing guideline's recommendations and expert's opinions. Enferm Infecc Microbiol Clin. 2017;35(1):47–51. doi: 10.1016/j.eimc.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 3.European Centre for Disease Prevention and Control 2011 Migrant health: HIV testing and counselling in migrant populations and ethnic minorities in EU/EEA/EFTA Member States. Stockholm: ECDC. 2011 https://www.ecdc.europa.eu/sites/default/files/media/en/publications/Publications/1108_TER_HIV_in_migrants.pdf Technical report. (Accessed March 8, 2023) [Google Scholar]
- 4.Seedat F, Hargreaves S, Friedland JS. Engaging new migrants in infectious disease screening: a qualitative semi-structured interview study of UK migrant community health-care leads. PLoS One. 2014;9(10) doi: 10.1371/journal.pone.0108261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.European Centre for Disease Prevention and Control . 2018. Technical report. [Google Scholar]
- 6.European Centre for Disease Prevention and Control . 2022. Technical report. [Google Scholar]
- 7.Woode Owusu M, Weis N, Krankowska D, Lourida P. Late HIV diagnosis among migrant women in Europe. PROSPERO. 2021 doi: 10.1016/j.ijregi.2023.03.006. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021275713 CRD42021275713. (Accessed March 8, 2023) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fakoya I, Álvarez-Del Arco D, Monge S, Copas AJ, Gennotte AF, Volny-Anne A, et al. aMASE Study Team. HIV testing history and access to treatment among migrants living with HIV in Europe. J Int AIDS Soc. 2018;4 doi: 10.1002/jia2.25123. e25123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fakoya I, Álvarez-Del Arco D, Copas AJ, Teixeira B, Block K, Gennotte AF, et al. Factors associated with access to HIV testing and primary care among migrants living in Europe: cross-sectional survey. JMIR Public Health Surveill. 2017;3(4) doi: 10.2196/publichealth.7741. e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Favarato G, Bailey H, Burns F, Prieto L, Soriano-Arandes A, Thorne C. Migrant women living with HIV in Europe: are they facing inequalities in the prevention of mother-to-child-transmission of HIV? The European Pregnancy and Paediatric HIV Cohort Collaboration (EPPICC) study group in EuroCoord. Eur J Public Health. 2018;28(1):55–60. doi: 10.1093/eurpub/ckx048. [DOI] [PubMed] [Google Scholar]
- 11.Tokar A, Osborne J, Hengeveld R, Lazarus JV, Broerse JEW. ‘I don't want anyone to know’: experiences of obtaining access to HIV testing by Eastern European, non-European Union sex workers in Amsterdam, the Netherlands. PLoS One. 2020;15(7) doi: 10.1371/journal.pone.0234551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.George-Svahn L, Eriksson LE, Wiklander M, Björling G, Svedhem V, Brännström J. Barriers to HIV testing as reported by individuals newly diagnosed with HIV infection in Sweden. AIDS Care. 2021;33(10):1286–1295. doi: 10.1080/09540121.2020.1844862. [DOI] [PubMed] [Google Scholar]
- 13.Migrants Working Group on behalf of COHERE in EuroCoord Mortality in migrants living with HIV in western Europe (1997–2013): a collaborative cohort study. Lancet HIV. 2015;2(12):e540–e549. doi: 10.1016/S2352-3018(15)00203-9. [DOI] [PubMed] [Google Scholar]
- 14.Bil JP, Zuure FR, Alvarez-Del Arco D, Prins JM, Brinkman K, Leyten E, et al. Disparities in access to and use of HIV-related health services in the Netherlands by migrant status and sexual orientation: a cross-sectional study among people recently diagnosed with HIV infection. BMC Infect Dis. 2019;19(1):906. doi: 10.1186/s12879-019-4477-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.French CE, Thorne C, Byrne L, Cortina-Borja M, Tookey PA. Presentation for care and antenatal management of HIV in the UK, 2009–2014. HIV Med. 2017;18(3):161–170. doi: 10.1111/hiv.12410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Borchmann O, Omland LH, Gerstoft J, Larsen CS, Johansen IS, Lunding S, et al. Length of stay in Denmark before HIV diagnosis and linkage to care: a population-based study of migrants living with HIV, Denmark, 1995 to 2020. Euro Surveill. 2022;27(30) doi: 10.2807/1560-7917.ES.2022.27.30.2100809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Evans C, Turner K, Suggs LS, Occa A, Juma A, Blake H. Developing a mHealth intervention to promote uptake of HIV testing among African communities in the UK: a qualitative study. BMC Public Health. 2016;16:656. doi: 10.1186/s12889-016-3278-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shangase P, Egbe CO. Barriers to accessing HIV services for Black African communities in Cambridgeshire, the United Kingdom. J Community Health. 2015;40(1):20–26. doi: 10.1007/s10900-014-9889-8. [DOI] [PubMed] [Google Scholar]
- 19.Hoyos J, Fernández-Balbuena S, de la Fuente L, et al. Madrid Rapid HIV Testing Group. Never tested for HIV in Latin-American migrants and Spaniards: prevalence and perceived barriers. J Int AIDS Soc. 2013;16(1):18560. doi: 10.7448/IAS.16.1.18560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Erwin J, Morgan M, Britten N, Gray K, Peters B. Pathways to HIV testing and care by black African and white patients in London. Sex Transm Infect. 2002;78(1):37–39. doi: 10.1136/sti.78.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National AIDS Trust. HIV and Black African Communities in the UK. A Policy Report. 2014 https://www.nat.org.uk/sites/default/files/publications/NAT-African-Communities-Report-June-2014-FINAL.pdf. (Accessed October 28, 2022)
- 22.Anderson J. Coming and going: some aspects of care for migrants with HIV in the UK. J Infect. 2008;57(1):11–15. doi: 10.1016/j.jinf.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 23.Burns FM, Imrie JY, Nazroo J, Johnson AM, Fenton KA. Why the(y) wait? Key informant understandings of factors contributing to late presentation and poor utilization of HIV health and social care services by African migrants in Britain. AIDS Care. 2007;19(1):102–108. doi: 10.1080/09540120600908440. [DOI] [PubMed] [Google Scholar]
- 24.Burns F, Fenton KA, Morison L, Mercer C, Erens B, Field J, et al. Factors associated with HIV testing among black Africans in Britain. Sex Transm Infect. 2005;81(6):494–500. doi: 10.1136/sti.2004.013755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chappuis M, Pauti MD, Tomasino A, Fahet G, Cayla F, Corty JF. Knowledge of HIV and hepatitis B and C status among people living in extreme poverty in France, in 2012. Med Mal Infect. 2015;45(3):72–77. doi: 10.1016/j.medmal.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 26.Manirankunda L, Loos J, Alou TA, Colebunders R, Nöstlinger C. ‘It's better not to know’: perceived barriers to HIV voluntary counseling and testing among sub-Saharan African migrants in Belgium. AIDS Educ Prev. 2009;21(6):582–593. doi: 10.1521/aeap.2009.21.6.582. [DOI] [PubMed] [Google Scholar]
- 27.O'Brien O, Khan S. In: Crossing borders: Migration, Ethnicity and AIDS. Hanour-Knipe M, Rector S, editors. Taylor and Francis; London: 1996. Stigma and racism as they affect minority ethnic communities; pp. 102–117. editors. [Google Scholar]