Abstract
Suboptimal outcomes from behavioral weight loss (BWL) treatments are partially attributable to accumulated instances of non-adherence to dietary prescriptions (i.e., dietary lapses). Results identifying negative internal triggers for dietary lapses are inconsistent, potentially due to individual differences that impact how individuals respond to cues. Impulsivity is one factor that likely influences reactivity to internal states. We examined three dimensions of impulsivity (delay discounting, inhibitory control, and negative urgency) as moderators of the relation between affective and physical states and subsequent dietary lapses at the beginning of BWL. Overweight/obese adults (n = 189) completed behavioral and self-reported measures of impulsivity at baseline of BWL and an ecological momentary assessment (EMA) protocol across the first two weeks of treatment to report on affective/physical states and instances of dietary lapses. Results indicated that baseline negative urgency, but not delay discounting or inhibitory control, was positively associated with overall lapse risk. Moderation analyses indicated that poorer inhibitory control strengthened the relation between momentary increases in stress and subsequent dietary lapse, and higher negative urgency strengthened the relation between increases in loneliness and dietary lapse. Negative urgency also moderated the impact of momentary hunger on subsequent dietary lapse risk in an unexpected direction, such that higher negative urgency weakened the relation between hunger and subsequent lapse. Results lend partial and tentative support for the moderating role of impulsivity on the relation between internal states and lapse likelihood. With replication, the development and testing of personalized treatment components based on baseline impulsivity level may be warranted.
Keywords: Impulsivity, Dietary lapses, Ecological momentary assessment
1. Introduction
Two out of every three American adults are overweight or obese (Yang & Colditz, 2015), and being overweight or obese is associated with a variety of negative health consequences (Caleyachetty et al., 2017; Danaei et al., 2009). Almost half of overweight and obese Americans are actively trying to lose weight (Yaemsiri, Slining, & Agarwal, 2011), but unfortunately, gold standard behavioral weight loss (BWL) programs produce suboptimal weight loss results. Participants in even the most effective BWL treatments lose less weight than: (a) individuals in controlled environments following the same prescription (Weinsier et al., 2000); (b) what is desired by participants themselves (Foster, Wadden, Vogt, & Brewer, 1997); and (c) what is recommended by physicians to lower risk of weight-related health consequences, including hypertension and cardiovascular disease (P. W. Wilson, D'agostino, Sullivan, Parise, & Kannel, 2002). Furthermore, even among participants who achieve clinically significant weight loss through these programs (i.e., 5–10%), nearly all regain a substantial portion of their lost weight within a few years (Wadden, Butryn, & Wilson, 2007; G. T.; Wilson, 1994).
Inability to consistently adhere to a planned diet—which includes calorie restriction, limited intake of certain foods, or eating within certain time frames—appears to be partially responsible for suboptimal outcomes. Frequency of individual instances of dietary non-adherence (i.e., dietary lapses) is negatively associated with weight loss in the context of BWL treatment (Forman et al., 2017), likely due to an accumulation of calories that interferes with achieving a negative calorie balance. In addition, evidence suggests that dietary lapses are associated with negative affective states, such as hopelessness, which may serve to further deteriorate motivation to achieve weight loss goals (Carels, Douglass, Cacciapaglia, & O'brien, 2004; Carels et al., 2001).
Thus, understanding the internal, momentary factors (e.g., affective or physical states) that contribute to dietary lapses is critical to designing treatment components that aim to reduce the frequency of such lapses. Research using ecological momentary assessment (EMA; a method of collecting data in people's everyday lives) indicates that internal states such as hunger, stress, and feelings of deprivation are associated with dietary temptations and lapses (Carels et al., 2001; Forman et al., 2017). However, EMA examinations aimed at identifying momentary internal states that trigger lapses have yielded inconsistent results. In particular, some studies have found certain internal states (e.g., hunger) to be predictors of dietary lapses (Carels et al., 2001; Forman et al., 2017), whereas other studies have found no relation between these same triggers and lapses (Carels et al., 2004). Mixed results could be attributable to high levels of inter-individual variability in responses to triggers that could yield a confusing pattern of overall effects. Specifically, individual differences in certain traits or abilities may influence how individuals respond to internal states, such that some individuals may be at much greater risk of lapsing in response to specific triggers while other individuals may experience no change in lapse risk or in fact be at lesser risk. Failure to account for the influence of these traits or abilities on the relationship between internal states and dietary lapse risk may help to explain inconsistent findings across studies, as these abilities may differ across samples. Additionally, if some individuals are at greater risk of lapsing in response to certain states given particular traits or abilities and other individuals are at lower risk of lapsing, the main effect of these states on lapse risk in a particular study may be found to be nonsignificant, despite meaningful relationships between internal states and dietary lapse occurrence being present for certain individuals.
One individual difference that may influence the relationship between internal states and dietary lapse occurrence is impulsivity, or the tendency to act rashly without forethought or regard for future consequences (Baumeister, Vohs, & Tice, 2007). One prominent model divides impulsivity into two sub-domains: “impulsive decision-making” (i.e., deliberate choice of a short term over a larger, long-term reward) and “impulsive inhibition” (i.e., late-stage inhibition of a prepotent response; Reynolds, Ortengren, Richards, & de Wit, 2006). Impulsivity also refers to trait, personality-based impulsivity, which can manifest in several forms (e.g., sensation-seeking, negative urgency; Whiteside & Lynam, 2001). A large body of research has identified impulsivity as a maintenance factor for deleterious eating behaviors (Davis, Levitan, Muglia, Bewell, & Kennedy, 2004; Manasse et al., 2017; Schag, Schönleber, Teufel, Zipfel, & Giel, 2013; Thamotharan, Lange, Zale, Huffhines, & Fields, 2013). Specifically, delay discounting (i.e., the tendency to choose more immediate, shorter-term rewards over longer-term rewards), inhibitory control (i.e., the ability to withhold an automatic response to a stimulus), and negative urgency (i.e., the tendency to act rashly in the context of negative emotions) are three facets of impulsivity that may contribute to the maintenance of poor eating decisions in the presence of negative internal states (Ames et al., 2014; Anestis, Smith, Fink, & Joiner, 2009; Dassen, Houben, & Jansen, 2015; Fields, Sabet, & Reynolds, 2013; Houben, 2011; Jasinska et al., 2012). Individuals with higher delay discounting tend to place more value on the short-term benefit of eating highly palatable food and less value on prioritizing the longer-term reward of weight loss (Rasmussen, Lawyer, & Reilly, 2010). Individuals with poor inhibitory control may have a difficult time inhibiting an already-initiated desire to eat palatable but unhealthy food (Houben, Nederkoorn, & Jansen, 2014; Mobbs, Van der Linden, d'Acremont, & Perroud, 2008). Those with higher negative urgency are likely to overeat in an immediate attempt to alleviate negative affect (Anestis et al., 2009; Fischer, Peterson, & McCarthy, 2013). As such, these three domains of impulsivity appear to be highly relevant traits to examine in the context of dietary lapses.
Although the literature robustly supports impulsivity's relation to unhealthy eating behaviors among non-treatment-seeking overweight and obese samples, no studies have examined impulsivity's relation to dietary lapses within BWL treatment, or whether impulsivity moderates dietary lapse likelihood. Higher levels of impulsivity may increase an individual's reactivity to negative internal states, and thus increase that individual's likelihood of lapsing. For example, an individual who has more difficulty prioritizing long-term over short-term reward may be more prone to eat when doing so provides immediate comfort (e.g., when feeling sad, bored, or lonely). Similarly, an individual who cannot easily inhibit a craving or desire for food may be more likely to eat when stressed. Likewise, an individual who often engages in rash action when experiencing negative emotions may be more inclined to eat in order to alleviate those emotions. The established links between impulsivity and unhealthy eating behaviors suggest that impulsivity may impact (specifically, strengthen) the relation between momentary elevations in internal states and subsequent dietary lapses. Given past research suggesting that certain facets of impulsivity may be more strongly related to both obesity (Lawyer, Boomhower, & Rasmussen, 2015) and other health behaviors (e.g., alcohol misuse; (Courtney et al., 2012), it is also important to assess the relationship between various aspects of impulsivity and dietary lapses occurrence.
The present study aimed to examine whether (1) three facets of impulsivity (delay discounting, inhibitory control, and negative urgency), as measured at baseline, predicted dietary lapse risk, as measured by EMA, within the first two weeks of a BWL intervention; and (2) whether these facets of impulsivity moderated the impact of momentary levels of internal (i.e., affective and physical) states (measured by EMA) on dietary lapse occurrence. Of note, although stress is a distinct experience that does not fall neatly into the category of an affective or physical state (Lazarus, 2006), for the purposes of simplicity, we have classified it as under the umbrella of affective and physical states. We hypothesized that baseline impulsivity would be positively associated with lapse risk and that the relation between elevations in negative internal states and subsequent dietary lapses would be strongest for those at the highest levels of baseline impulsivity. Specifically, we expected that individuals with higher delay discounting, poorer inhibitory control, and higher negative urgency would be more likely to lapse in response to momentary elevations in negative affective and physical states.
2. Methods
2.1. Participants
The sample consisted of 189 overweight/obese (BMI 27–50 kg/m2) adults (82.0% female; 70.9% Caucasian; Mage = 51.81 ± 9.76 years; MBMI = 36.93 ± 5.83 kg/m2) participating in a BWL treatment study (see Forman et al., 2016 for details). Participants were recruited from the community in the greater Philadelphia metropolitan areas through various methods including radio advertisements, flyers, and primary care clinics.
2.2. Procedure
The current study represents a secondary data analysis of a study by Forman et al. (2017). In the larger treatment study, participants received 25 group sessions of BWL treatment delivered over 12 months, which included all features of standard BWL. Of note, although the larger treatment study compared the efficacy of two BWL treatment approaches, data were collapsed across conditions for the present analyses, as conditions were nearly identical for the first two weeks of treatment when EMA occurred. Procedures were approved by the Institutional Review Board of Drexel University and complied with all ethical standards for research.
2.3. Ecological momentary assessment (EMA)
Participants were given an Android player (Samsung Galaxy Player 4.0) pre-loaded with a custom-designed EMA smartphone application (DrexelEMA). The EMA protocol occurred for 14 days in the beginning of treatment. Participants were given written and verbal instructions on how to use DrexelEMA and how to identify a dietary lapse. Participants received six prompts daily at semi-random intervals and were also instructed to initiate a survey whenever they experienced a dietary lapse.
At each prompt, participants were asked to indicate whether they had experienced a dietary lapse since last completing a survey, with lapsing defined as “eating or drinking likely to cause weight gain, and/or put weight loss/maintenance at risk.” During the period at which EMA was administered (the first two weeks of BWL), participants were prescribed a daily calorie goal and were trained to recognize that going over this goal was likely to prevent weight loss. Based on an adapted version of the PANAS (Watson, Clark, & Tellegen, 1988), negative affect (sadness, irritation, loneliness, and boredom) and a stress item (created for the current study based on the PANAS), and physical states (hunger, deprivation, and fatigue) were measured on a 5-point Likert scale. Although additional negative affective states (e.g., guilt) have been shown to be associated with binge eating behavior (Berg et al., 2015) and could also foreseeably predict dietary lapses, we limited the number of affective states assessed to reduce participant burden and chose to assess several dimensions of negative affect that have been associated with dietary temptations and/or lapses in previous literature (Carels et al., 2001). Additionally, given evidence that specific affective states are associated with dysregulated eating behavior (Berg et al., 2014; Carels et al., 2001), we decided to use individual PANAS items rather than composite scores. For greater detail on the EMA protocol, see (Forman et al., 2017).
2.4. Measures
All measures of impulsivity were administered at a baseline assessment, prior to randomization.
2.4.1. Inhibitory control
A modified version of a computerized Stop Signal Task (SST) was used to measure inhibitory control in response to both neutral and food-specific stimuli (see Manasse et al., 2016 for more details). In this task, participants categorize various stimuli on a screen with a keyboard press. The task included two blocks: neutral (e.g., staplers) and food (e.g., pizza) stimuli. In a subset of categorization trials, a stop signal is displayed after the stimulus presentation but before the participant response, which indicates to participants that they are to refrain from responding. As in previous studies, the outcome measure used for the current study was the stop signal reaction time (SSRT), which was calculated by subtracting the average reaction time on normal trials from the average stop signal delay (Verbruggen & Logan, 2008). The SSRT was calculated for each subject. A smaller SSRT is indicative of better inhibitory control whereas a larger SSRT reflects poorer inhibitory control. Because of a programming error in the task, the data from approximately half the sample (the first two waves of recruitment) was not usable. Individuals with missing SSTs (n = 97) were excluded from analyses that included the SST.
2.4.2. Delay discounting
Delay discounting was assessed using the Delay Discounting Task (DDT; Robles & Vargas, 2007), a commonly used computerized monetary discounting task. Discounting is the extent to which the subjective value of an immediate reward is deemed greater than the subjective value of a future (“delayed”) reward, despite the future reward's higher objective value. Participants were asked over several trials to choose between a hypothetical, variable monetary amount that could be received immediately and a larger amount to be received after varying time intervals. Area-under-the-curve (AUC) was calculated from the points at which the subjective value of the delayed reward was equal to the amount of the immediate reward (Myerson, Green, & Warusawitharana, 2001). We chose to use AUC as the outcome variable of delay discounting given its prevalent use in obesity literature (Appelhans et al., 2012; Rasmussen et al., 2010) and to avoid imposing a specific distribution on the data. Other outcome measures from delayed discounting tasks (e.g., k), assume a quadratic function of the data and maybe a better fit for confirming hypotheses that certain subsets of individuals (e.g., those who are overweight) fit a hyperbolic decision-making curve. AUC may be a better fit for examining an individual's tendency to discount and how it relates to outcome (e.g., dietary lapses). Greater AUC values indicate less discounting of delayed rewards.
2.4.3. Negative urgency
The UPPS (Whiteside & Lynam, 2001) is a self-report measure that assesses negative urgency, or the tendency towards rash action in the context of negative affect. We utilized the negative urgency subscale (UPPS-NU), in which higher scores indicate greater affect-driven impulsivity. The UPPS has good internal consistency (Whiteside & Lynam, 2001). Cronbach's alpha for the UPPS-NU subscale in our sample was 0.81.
2.5. Statistical analyses
Separate generalized estimating equation (GEE) models based on a negative binomial distribution with a log link function and a first-order autoregressive matrix structure were used to examine the main effect of each measure of impulsivity on risk of lapse, as well as whether each trigger's impact on lapse risk at the following survey was moderated by impulsivity variables. The interaction between within-subjects triggers (i.e., one's level of a trigger at a given EMA survey, relative to one's average level across all EMA surveys) and impulsivity variables was of particular interest. All models controlled for between-subject effects (i.e., participants' average level of each internal state across all EMA surveys), as well as whether a lapse was reported at the previous survey. Each impulsivity variable was included as a predictor in each model and interactions between the impulsivity variable and both between- and within-subjects predictors were included in the model. All between-subjects variables were grand mean centered. Within-subjects effects were centered within person.
3. Results
3.1. Compliance
Mean compliance with prompted EMA surveys was 82.4% (SD = 13.3%). Consistent with previous investigations, participants with less than 40% compliance (n = 3) with prompted surveys were excluded from analyses (Forman et al., 2017). Fourteen participants reported no lapses during the assessment period (n = 14); thus, the final number of participants contributing data for analyses predicting lapses was 172.
3.2. EMA data characteristics and triggers
A total of 13,402 baseline EMA recordings were provided by 172 participants representing 2470 participant days. Main effects of affective and physical states on subsequent dietary lapses are described in detail in Forman et al. (2017). In that study, elevated momentary levels of physical states (e.g., hunger, fatigue and deprivation) were associated with higher likelihood of subsequent dietary lapse, but affective/emotional (e.g., stress, boredom, sadness, irritation, and loneliness) states were not. In general, between-subjects’ levels of the individual affective/emotional states were moderately-to-highly associated with each other (rs = 0.35-0.81, all ps < .01) as were the individual physical states, to a lesser degree (rs = 0.25-0.66, all ps < .01). Within-subjects affective/emotional states were associated with each other to a small to moderate degree (rs = 0.04-0.49, ps = .00-.66), as were physical states (rs = 0.09-0.39, all ps < .01).
3.3. Main effect of impulsivity
Neither delay discounting nor inhibitory control at baseline was significantly associated with risk of lapsing at a given survey. However, baseline negative urgency was associated with lapse risk (b = 0.37, SE = 0.17, p = .03).
3.4. Interactions between internal states and impulsivity
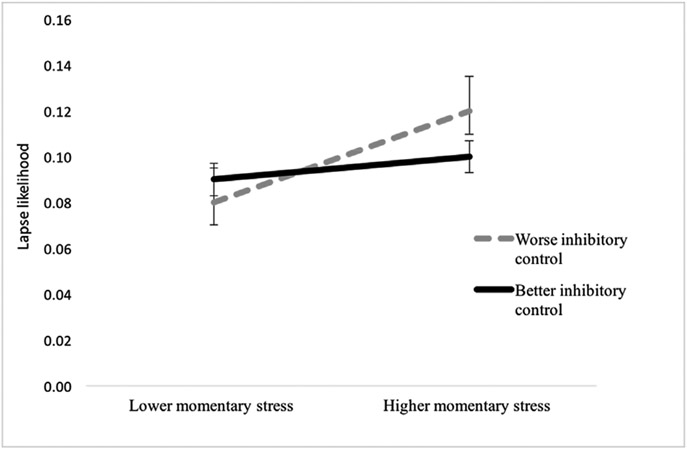
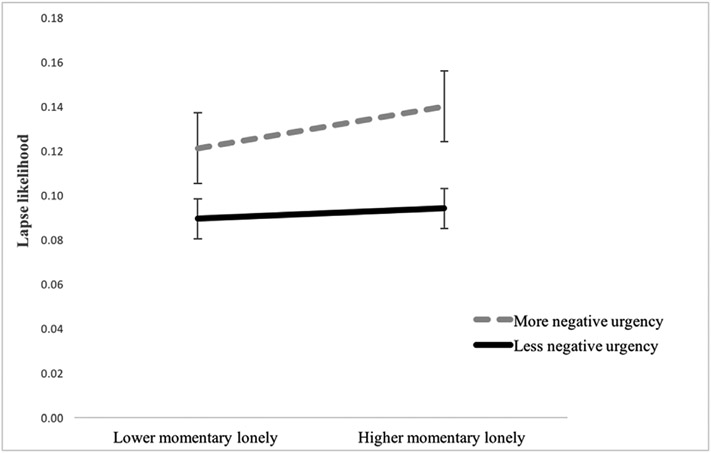
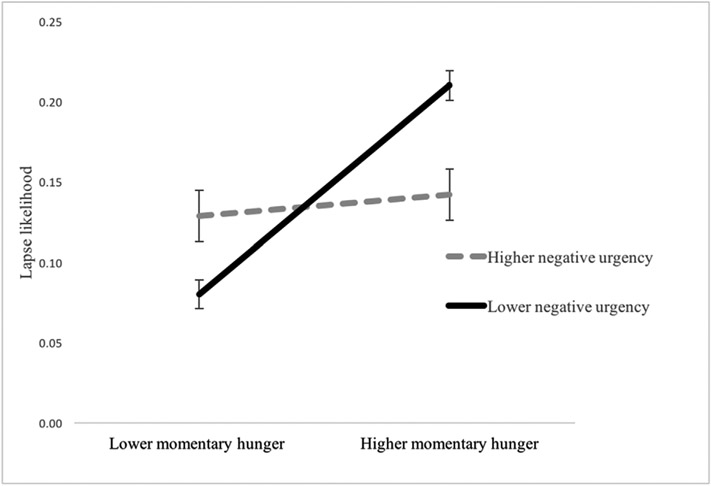
See Table 1 for within-subjects predictors x impulsivity variable interaction effect statistics. The level of delay discounting did not significantly moderate the relation between momentary elevations in any internal states and subsequent dietary lapse, except for fatigue (at trend level), such that the relation between increases in fatigue and likelihood of lapse was stronger for those who were greater discounters (i.e., prioritized short-term over long-term rewards). Inhibitory control moderated the relation between momentary elevations in stress and subsequent dietary lapse occurrence (i.e., at the following survey), such that increased stress more strongly predicted dietary lapse (at the following survey) for those with lower inhibitory control (see Fig. 1). Inhibitory control did not moderate the relation between any other affective/physical predictors and dietary lapse at the following survey. Additionally, as hypothesized, negative urgency significantly moderated the relation between elevations in loneliness and subsequent dietary lapse, such that loneliness more strongly predicted dietary lapse at the following survey among those with higher levels of negative urgency (i.e., more tendency to act rashly in response to negative affect; see Fig. 2). The same moderation effect of negative urgency was detected for irritation at the trend level. Unexpectedly, hunger more strongly predicted lapses in those with lower levels of negative urgency (see Fig. 3).
Table 1.
Interactions between impulsivity and momentary (within-subjects) internal states on likelihood of dietary lapse.
| B | SE | 95% CI | Wald χ2 | P | OR | |
|---|---|---|---|---|---|---|
| Delay discounting x internal states interaction effects | ||||||
| Sadness | .30 | 1.08 | [−1.08, 2.43] | .08 | .78 | 1.35 |
| Loneliness | .190 | .387 | [−.569, .949] | .240 | .62 | 1.21 |
| Boredom | −.203 | .371 | [−.929, .524] | .298 | .59 | 0.81 |
| Irritation | −.027 | .254 | [−.525, .471] | .011 | .92 | 0.97 |
| Stress | .269 | .261 | [−.243, .781] | 1.063 | .30 | 1.31 |
| Hunger | −.246 | .187 | [−.613, .121] | 1.727 | .19 | 0.78 |
| Deprivation | −.252 | .256 | [−.754, .250] | .969 | .33 | 0.77 |
| Fatigue | −.416 | .225 | [−.857, .025] | 3.417 | .07 | 0.65 |
| Inhibitory control x internal states interaction effects | ||||||
| Sadness | −.004 | .003 | [−.009, .001] | 2.531 | .11 | 0.99 |
| Loneliness | .000 | .001 | [−.002, .003] | .041 | .84 | 1.00 |
| Boredom | .000 | .001 | [−.002, .003] | .058 | .81 | 1.00 |
| Irritation | .000 | .001 | [−.001, .001] | .187 | .66 | 1.00 |
| Stress | .002 | .001 | [.00, .003] | 6.233 | .01 | 1.00 |
| Hunger | .000 | .000 | [−.001, .001] | .068 | .79 | 1.00 |
| Deprivation | −.001 | .001 | [−.002, .00] | 2.146 | .94 | 0.99 |
| Fatigue | .000 | .001 | [−.001, .001] | .001 | .99 | 1.00 |
| Negative urgency x internal states interaction effects | ||||||
| Sadness | −.303 | .540 | [−1.362, .755] | .316 | .57 | 0.74 |
| Loneliness | .549 | .244 | [.071, .1.028] | 5.063 | .02 | 1.73 |
| Boredom | .220 | .249 | [−.267, .708] | .786 | .38 | 1.24 |
| Irritation | .289 | .168 | [−.040, .617] | 2.969 | .09 | 1.34 |
| Stress | .204 | .150 | [−.090, .498] | 1.844 | .17 | 1.23 |
| Hunger | −.236 | .110 | [−.451, −.021] | 4.630 | .03 | 0.79 |
| Deprivation | −.053 | .135 | [−.317, .212] | .152 | .70 | 0.95 |
| Fatigue | .048 | .094 | [−.136, .231] | .258 | .61 | 1.05 |
OR = odds ratio.
Fig. 1.
The moderating role of inhibitory control on the relation between momentary (within-subjects) stress and subsequent likelihood of dietary lapse.
Note: Analyses were run with continuous variables, but were dichotomized (median split) for graphical purposes. Error bars reflect standard error of estimated marginal means obtained from models using dichotomized variables.
Fig. 2.
The moderating role of negative urgency on the relation between momentary (within-subjects) levels of loneliness and subsequent likelihood of dietary lapse.
Note: Analyses were run with continuous variables, but were dichotomized for graphical purposes. Error bars reflect standard error of estimated marginal means obtained from models using dichotomized variables.
Fig. 3.
The moderating role of negative urgency on the relation between momentary levels of hunger and subsequent likelihood of dietary lapse.
Note: Analyses were run with continuous variables, but were dichotomized for graphical purposes. Error bars reflect standard error of estimated marginal means obtained from models using dichotomized variables.
4. Discussion
This is the first study to examine impulsivity as (1) a predictor of dietary lapse likelihood and (2) a moderator of the relation between momentary levels of internal (i.e., physical and affective) states and lapses. Results meaningfully extend prior research implicating impulsivity in unhealthy eating behaviors, and dietary lapses in suboptimal weight loss, by examining how impulsivity and internal states may interact in real-time to trigger dietary lapses, which have been shown to accumulate to result in poorer weight loss (Forman et al., 2017). Overall, our results provided tentative and partial support for our expectations that (1) baseline levels of impulsivity were related to dietary lapse likelihood in the first two weeks of BWL treatment; and (2) impulsivity moderated the relation between momentary levels of internal states and subsequent risk of dietary lapse. However, we emphasize that support for our hypotheses should be understood to be tentative given the number of statistical tests that were performed. As such, strong conclusions should wait until replication, as discussed below.
As expected, baseline negative urgency was positively associated with risk of lapsing during the first two weeks of BWL treatment, suggesting that individuals with higher levels of negative urgency may struggle to adhere to dietary goals in the early phases of treatment. However, baseline levels of delay discounting and inhibitory control at baseline were not significantly associated with dietary lapse risk. It is possible that baseline levels of delay discounting and inhibitory control are more related to longer-term weight outcomes from BWL (Manasse et al., 2017), while behavioral reactivity to negative emotions (i.e., negative urgency) is more predictive of difficulty with adherence early in treatment. For example, in the early stages of treatment, high levels of motivation may temporarily supersede tendencies to value short-term reward or problems inhibiting automatic responses.
Interestingly, inhibitory control appeared to moderate only the impact of feeling stressed on risk for subsequent dietary lapses; it did not appear to moderate the effect of other internal states. Specifically, poor inhibitory control strengthened the relationship between increases in stress and risk for lapsing at the following survey. One explanation for this result may be that feeling stressed may result from events or other demands that require time and/or attention. It may be that greater inhibitory control is necessary to resist giving into temptation when an individual is busy, does not have time to plan, or is feeling overwhelmed by daily stressors. While there are no studies that compare the demands/tasks associated with stress versus other emotions, research does suggest that stress demands attentional resources and can lead to cognitive interference (Klein & Boals, 2001; Sliwinski, Smyth, Hofer, & Stawski, 2006). As such, when individuals are experiencing stress, adherence to dietary goals may become more difficult. These effects of stress may be especially problematic among individuals with lower baseline inhibitory control and place them at greater risk of dietary lapses compared to individuals with greater inhibitory control abilities.
Negative urgency was also found to moderate the relationship between loneliness and dietary lapse in the expected direction, such that individuals higher in negative urgency appeared to be more susceptible to lapsing when experiencing higher levels of loneliness than were individuals lower in negative urgency. For every unit increase in negative urgency, a one-unit increase in loneliness increased the odds of lapsing at the next survey by 1.7 It is possible that loneliness is an especially distressing feeling, and those with higher negative urgency show increased susceptibility to overeating in an attempt to alleviate this feeling (Rotenberg & Flood, 1999). By comparison, however, the effect of other types of negative affect, such as sadness and stress, on subsequent dietary lapses was not moderated by negative urgency. It is possible that emotions like sadness and stress may lead to an increase or decrease in appetite (Finch & Tomiyama, 2015; Hou et al., 2013; Wallis & Hetherington, 2004), and individuals with greater negative urgency may therefore not be at elevated risk of responding through eating to these emotions.
Contrary to our initial expectations, results suggested that negative urgency moderated the relation between momentary increases in hunger and subsequent dietary lapses, such that lower levels of baseline negative urgency increased likelihood of lapsing in response to hunger. For every one-unit increase in negative urgency, an increase in momentary hunger decreased the odds of lapsing by 1.2. In retrospect, however, it follows that overweight/obese individuals who are less likely to respond rashly to negative affect may be more reactive to other internal states, such as hunger. In other words, overweight people with low negative urgency may have distinct maintenance factors for dysregulated eating—such as overeating in response to hunger cues—from those with high negative urgency (who may have greater difficulties controlling their food intake due to emotionally-driven eating). Although individuals with greater levels of negative urgency appear to be at overall greater risk for lapsing early in weight loss treatment, those with lower levels of negative urgency may be especially sensitive to hunger during this period.
Delay discounting did not appear to moderate the relation between elevations in internal states and subsequent dietary lapse. While increased discounting of future rewards is strongly linked with overeating and obesity cross-sectionally (Emery & Levine, 2017; Lavagnino, Arnone, Cao, Soares, & Selvaraj, 2016; Schiff et al., 2016; Stojek & MacKillop, 2017) and has been found to be more strongly associated with obesity status compared to other measures of impulsivity (Lawyer et al., 2015), it is possible that it does not modulate the momentary relation between internal states and dietary lapses early in treatment. Instead, it may be that delay discounting has a greater impact on lapsing later in treatment. Early in treatment, many individuals experience considerable weight loss from week to week (Feig & Lowe, 2017), which provides strong, relatively short-term reinforcement for the effort required to adhere to dietary recommendations, even when experiencing distressing emotions or other internal states that may prompt eating. As treatment progresses, however, weight loss typically slows, and the strong reinforcement of seeing results on the scale is diminished. At this time, the salience of the short-term reward of overeating may strengthen and increase reactivity to internal states, particularly among those with higher delay discounting. Future research is warranted to examine this possibility.
The above findings, while tentative, could have several potential clinical implications with replication. Given findings that early response to weight loss treatment is predictive of later weight loss (Carels, Cacciapaglia, Douglass, Rydin, & O'Brien, 2003; Gow et al., 2016; Unick et al., 2015; Waring et al., 2014), it may be important to develop and test intervention components to be provided to those high in negative urgency early in treatment in order to promote better adherence to dietary prescriptions and foster early self-efficacy for success. In addition, individuals with poorer inhibitory control may benefit from the provision of stress management strategies early in treatment to reduce the likelihood of lapsing. Further, those with higher levels of negative urgency appeared to be particularly sensitive to loneliness and irritation, and thus even more specifically, it may be beneficial to teach participants with higher levels of negative urgency skills for tolerating these types of negative affect. Additionally, while at lower risk for lapsing overall, individuals with lower levels of negative urgency may benefit from strategies for better minimizing (e.g., via more frequent eating episodes or greater consumption of reduced energy dense foods) or better tolerating hunger. Future research aimed at testing potentially adjunctive interventions that can reduce negative urgency and improve inhibitory control (e.g., inhibitory control trainings) is also warranted. Additionally, is essential that the current study's findings are replicated. The current study required a relatively large number of statistical tests to be conducted given our need to parse out relationships among specific facets of internal states and impulsivity, and the importance employing multi-modal measurement. As a result, the chance of spurious findings is higher than is ideal. Future research should aim to narrow the scope of measurement.
Strengths of the current study include the use of behavioral measurement for two of the impulsivity measures, use of EMA to examine prospective momentary relationships between internal states and subsequent dietary lapses, and a relatively large sample. In addition, this is one of the few studies to use EMA within the context of a BWL treatment, allowing us to examine important and potentially modifiable processes that may impact treatment success. However, despite these strengths, findings must be interpreted within the context of several limitations. First, a technical error rendered half of the inhibitory control task data unusable, and thus we suffered from reduced power for analyses examining inhibitory control. Second, while EMA confers many benefits, it is still ultimately a self-report tool and thus is prone to many limitations of self-report measurement, such as an individual's interpretation of what constitutes a dietary lapse, or, in the case of EMA, that participants consistently reported all their dietary lapses. We also were limited in the number of items we could include in the EMA protocol (in order to minimize burden), meaning that we potentially missed assessing important variables. Third, our sample was predominately white and female, constraining our abilities to generalize our findings, and we only examined the relations between impulsivity and internal states at the start of treatment. Fourth, because two of the facets of impulsivity we examined were measured via behavioral tasks (i.e., inhibitory control, delay discounting) and the other via self-report (i.e., negative urgency), shared method-related variance among self-report measures (i.e., negative urgency and EMA) may have accounted for some of our findings. Additionally, given some evidence that individuals with obesity exhibit decreased interoceptive sensitivity (Herbert & Pollatos, 2014; Simmons & DeVille, 2017) and elevated alexithymia (Giel et al., 2016; Pinna et al., 2011), our sample's ability to accurately report on their internal physical and emotional states may have been impaired. Lastly, given the strong links between negative affect and dysregulated eating, we limited the investigation to examining the moderating role of impulsivity on the relation between only a subset of negative affective states and dietary lapses. However, future investigations should be conducted to examine the potential moderating role of impulsivity on positive affect, additional negative affective states (e.g., guilt, anxiety), and/or exposure to palatable food, all of which have strong links with dysregulated eating.
Overall, results tentatively support the role of impulsivity in impacting the relation between internal states and dietary lapses. Targeted research and interventions for impulsivity may have a significant impact on the highly prevalent epidemic of obesity in our society, especially for those whose level of impulsivity is known to make BWL treatment outcomes less successful over time.
Acknowledgements
This study was funded by grants from the National Institute for Diabetes and Digestive and Kidney Diseases (R01 DK095069) to Dr. Forman and the National Institute of Mental Health (F31 MH108279) to Dr. Manasse.
Footnotes
Declarations of interest
None.
References
- Ames SL, Kisbu-Sakarya Y, Reynolds KD, Boyle S, Cappelli C, Cox MG, … Stacy AW (2014). Inhibitory control effects In adolescent binge eating and consumption of sugar-sweetened beverages and snacks. Appetite, 81, 180–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anestls MD, Smith AR, Fink EL, & Joiner TE (2009). Dysregulated eating and distress: Examining the specific role of negative urgency in a clinical sample. Cognitive Therapy and Research, 33(4), 390–397. [Google Scholar]
- Appelhans BM, Waring ME, Schneider KL, Pagoto SL, DeBiasse MA, Whited MC, et al. (2012). Delay discounting and intake of ready-to-eat and away-from-home foods in overweight and obese women. Appetite, 59(2), 576–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister RF, Vohs KD, & Tice DM (2007). The strength model of self-control. Current Directions in Psychological Science, 16(6), 351–355. [Google Scholar]
- Berg KC, Crosby RD, Cao L, Crow SJ, Engel SG, Wonderlich SA, et al. (2015). Negative affect prior to and following overeating-only, loss of control eating-only, and binge eating episodes in obese adults. International Journal of Eating Disorders, 48(6), 641–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg KC, Peterson CB, Crosby RD, Cao L, Crow SJ, Engel SG, et al. (2014). Relationship between dally affect and overeating-only, loss of control eating-only, and binge eating episodes in obese adults. Psychiatry Research, 215(1), 185–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caleyachetty R, Thomas GN, Toulis KA, Mohammed N, Gokhale KM, Balachandran K, et al. (2017). Metabolically healthy obese and incident cardiovascular disease events among 3.5 million men and women. Journal of the American College of Cardiology, 70(12), 1429–1437. [DOI] [PubMed] [Google Scholar]
- Carels RA, Cacciapaglia HM, Douglass OM, Rydin S, & O'Brien WH (2003). The early identification of poor treatment outcome in a women's weight loss program. Eating Behaviors, 4(3), 265–282. [DOI] [PubMed] [Google Scholar]
- Carels RA, Douglass OM, Cacciapaglia HM, & O'brien WH (2004). An ecological momentary assessment of relapse crises in dieting. Journal of Consulting and Clinical Psychology, 72(2), 341. [DOI] [PubMed] [Google Scholar]
- Carels RA, Hoffman J, Collins A, Raber AC, Cacciapaglia H, & O'Brien WH (2001). Ecological momentary assessment of temptation and lapse in dieting. Eating Behaviors, 2(4), 307–321. [DOI] [PubMed] [Google Scholar]
- Courtney KE, Arellano R, Barkley-Levenson E, Gálvan A, Poldrack RA, MacKillop J, … Ray LA (2012). The relationship between measures of impulsivity and alcohol misuse: An integrative structural equation modeling approach. Alcoholism: Clinical and Experimental Research, 36(6), 923–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, et al. (2009). The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Medicine, 6(4), e1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dassen FC, Houben K, & Jansen A (2015). Time orientation and eating behavior: Unhealthy eaters consider immediate consequences, while healthy eaters focus on future health. Appetite, 91, 13–19. [DOI] [PubMed] [Google Scholar]
- Davis C, Levitan RD, Muglia P, Bewell C, & Kennedy JL (2004). Decision-making deficits and overeating: A risk model for obesity. Obesity, 12(6), 929–935. [DOI] [PubMed] [Google Scholar]
- Emery RL, & Levine MD (2017). Questionnaire and Behavioral Task Measures of Impulsivity are Differentially Associated with Body Mass Index: A Comprehensive Meta-Analysis. [DOI] [PubMed] [Google Scholar]
- Feig EH, & Lowe MR (2017). Variability in weight change early in behavioral weight loss Treatment: Theoretical and clinical implications. Obesity, 25(9), 1509–1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fields S, Sabet M, & Reynolds B (2013). Dimensions of impulsive behavior in obese, overweight, and healthy-weight adolescents. Appetite, 70, 60–66. [DOI] [PubMed] [Google Scholar]
- Finch LE, & Tomiyama AJ (2015). Comfort eating, psychological stress, and depressive symptoms in young adult women. Appetite, 95, 239–244. [DOI] [PubMed] [Google Scholar]
- Fischer S, Peterson CM, & McCarthy D (2013). A prospective test of the influence of negative urgency and expectancies on binge eating and purging. Psychology of Addictive Behaviors, 27(1), 294. [DOI] [PubMed] [Google Scholar]
- Forman EM, Butryn ML, Manasse SM, Crosby RD, Goldstein SP, Wyckoff EP, et al. (2016). Acceptance-based versus standard behavioral treatment for obesity: Results from the mind your health randomized controlled trial. Obesity, 24(10), 2050–2056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman EM, Schumacher LM, Crosby R, Manasse SM, Goldstein SP, Butryn ML, … Thomas JG (2017). Ecological momentary assessment of dietary lapses across behavioral weight loss Treatment: Characteristics, predictors, and relationships with weight change. Annals of Behavioral Medicine, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster GD, Wadden TA, Vogt RA, & Brewer G (1997). What is a reasonable weight loss? Patients' expectations and evaluations of obesity treatment outcomes. Journal of Consulting and Clinical Psychology, 65(1), 79. [DOI] [PubMed] [Google Scholar]
- Giel KE, Hartmann A, Zeeck A, Jux A, Vuck A, Gierthmuehlen PCG, … Joos A (2016). Decreased emotional perception in obesity. European Eating Disorders Review, 24(4), 341–346. 10.1002/erv.2444. [DOI] [PubMed] [Google Scholar]
- Gow ML, Baur LA, Ho M, Chisholm K, Noakes M, Cowell CT, et al. (2016). Can early weight loss, eating behaviors and socioeconomic factors predict successful weight loss at 12-and 24-months in adolescents with obesity and insulin resistance participating in a randomised controlled trial? International Journal of Behavioral Nutrition and Physical Activity, 13(1), 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbert BM, & Pollatos O (2014). Attenuated interoceptive sensitivity in overweight and obese individuals. Eating Behaviors, 15(3), 445–448. [DOI] [PubMed] [Google Scholar]
- Houben K (2011). Overcoming the urge to splurge: Influencing eating behavior by manipulating inhibitory control. Journal of Behavior Therapy and Experimental Psychiatry, 42(3), 384–388. [DOI] [PubMed] [Google Scholar]
- Houben K, Nederkoorn C, & Jansen A (2014). Eating on impulse: The relation between overweight and food-specific inhibitory control. Obesity, 22(5). [DOI] [PubMed] [Google Scholar]
- Hou F, Xu S, Zhao Y, Lu Q, Zhang S, Zu P, … Tao F (2013). Effects of emotional symptoms and life stress on eating behaviors among adolescents. Appetite, 68, 63–68. [DOI] [PubMed] [Google Scholar]
- Jasinska AJ, Yasuda M, Burant CF, Gregor N, Khatri S, Sweet M, et al. (2012). Impulsivity and inhibitory control deficits are associated with unhealthy eating in young adults. Appetite, 59(3), 738–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein K, & Boals A (2001). The relationship of life event stress and working memory capacity. Applied Cognitive Psychology, 15(5), 565–579. [Google Scholar]
- Lavagnino L, Arnone D, Cao B, Soares JC, & Selvaraj S (2016). Inhibitory control in obesity and binge eating disorder: A systematic review and meta-analysis of neurocognitive and neuroimaging studies. Neuroscience & Biobehavioral Reviews, 68, 714–726. [DOI] [PubMed] [Google Scholar]
- Lawyer SR, Boomhower SR, & Rasmussen EB (2015). Differential associations between obesity and behavioral measures of impulsivity. Appetite, 95, 375–382. [DOI] [PubMed] [Google Scholar]
- Lazarus RS (2006). Stress and emotion: A new synthesis. Springer publishing company. [Google Scholar]
- Manasse SM, Espel HM, Schumacher LM, Kerrigan SG, Zhang F, Forman EM, et al. (2016). Does impulsivity predict outcome in treatment for binge eating disorder? A multimodal investigation. Appetite, 105, 172–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manasse SM, Flack D, Dochat C, Zhang F, Butryn ML, & Forman EM (2017). Not so fast: The impact of impulsivity on weight loss varies by treatment type. Appetite, 113, 193–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mobbs O, Van der Linden M, d'Acremont M, & Perroud A (2008). Cognitive deficits and biases for food and body in bulimia: Investigation using an affective shifting task. Eating Behaviors, 9(4), 455–461. [DOI] [PubMed] [Google Scholar]
- Myerson J, Green L, & Warusawitharana M (2001). Area under the curve as a measure of discounting. Journal of the Experimental Analysis of Behavior, 76(2), 235–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinna F, Lai L, Pirarba S, Orru W, Velluzzi F, Loviselli A, et al. (2011). Obesity, alexithymia and psychopathology: A case-control study. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 16(3), e164–e170. [DOI] [PubMed] [Google Scholar]
- Rasmussen EB, Lawyer SR, & Reilly W (2010). Percent body fat is related to delay and probability discounting for food in humans. Behavioural Processes, 83(1), 23–30. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Ortengren A, Richards JB, & de Wit H (2006). Dimensions of impulsive behavior: Personality and behavioral measures. Personality and Individual Differences, 40(2), 305–315. [Google Scholar]
- Robles E, & Vargas PA (2007). Functional parameters of delay discounting assessment tasks: Order of presentation. Behavioural Processes, 75(2), 237–241. [DOI] [PubMed] [Google Scholar]
- Rotenberg KJ, & Flood D (1999). Loneliness, dysphoria, dietary restraint, and eating behavior. International Journal of Eating Disorders, 25(1), 55–64. [DOI] [PubMed] [Google Scholar]
- Schag K, Schönleber J, Teufel M, Zipfel S, & Giel K (2013). Food-related impulsivity in obesity and Binge Eating Disorder–a systematic review. Obesity Reviews, 14(6), 477–495. [DOI] [PubMed] [Google Scholar]
- Schifif S, Amodio P, Testa G, Nardi M, Montagnese S, Caregaro L, … Sellitto M (2016). Impulsivity toward food reward is related to BMI: Evidence from intertemporal choice in obese and normal-weight individuals. Brain and Cognition, 110, 112–119. [DOI] [PubMed] [Google Scholar]
- Simmons WK, & DeVille DC (2017). Interoceptive contributions to healthy eating and obesity. Current opinion in psychology, 17, 106–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sliwinski MJ, Smyth JM, Hofer SM, & Stawski RS (2006). Intraindividual coupling of daily stress and cognition. Psychology and Aging, 21(3), 545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stojek MM, & MacKillop J (2017). Relative reinforcing value of food and delayed reward discounting in obesity and disordered eating: A systematic review. Clinical Psychology Review, 55, 1–11. [DOI] [PubMed] [Google Scholar]
- Thamotharan S, Lange K, Zale EL, Huffhines L, & Fields S (2013). The role of impulsivity in pediatric obesity and weight status: A meta-analytic review. Clinical Psychology Review, 33(2), 253–262. [DOI] [PubMed] [Google Scholar]
- Unick JL, Neiberg RH, Hogan PE, Cheskin LJ, Dutton GR, Jeffery R, … Wing RR (2015). Weight change in the first 2 months of a lifestyle intervention predicts weight changes 8 years later. Obesity, 23(7), 1353–1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbruggen F, & Logan GD (2008). Response inhibition in the stop-signal paradigm. Trends in Cognitive Sciences, 22(11), 418–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadden TA, Butryn ML, & Wilson C (2007). Lifestyle modification for the management of obesity. Gastroenterology, 132(6), 2226–2238. [DOI] [PubMed] [Google Scholar]
- Wallis DJ, & Hetherington MM (2004). Stress and eating: The effects of ego-threat and cognitive demand on food intake in restrained and emotional eaters. Appetite, 43(1), 39–46. [DOI] [PubMed] [Google Scholar]
- Waring ME, Schneider KL, Appelhans BM, Busch AM, Whited MC, Rodrigues S, … Pagoto SL (2014). Early-treatment weight loss predicts 6-month weight loss in women with obesity and depression: Implications for stepped care. Journal of Psychosomatic Research, 76(5), 394–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063. [DOI] [PubMed] [Google Scholar]
- Weinsier RL, Nagy TR, Hunter GR, Darnell BE, Hensrud DD, & Weiss HL (2000). Do adaptive changes in metabolic rate favor weight regain in weight-reduced individuals? An examination of the set-point theory. American Journal of Clinical Nutrition, 72(5), 1088–1094. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, & Lynam DR (2001). The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30(4), 669–689. [Google Scholar]
- Wilson GT (1994). Behavioral treatment of obesity: Thirty years and counting. Advances in Behaviour Research and Therapy, 16(1), 31–75. [Google Scholar]
- Wilson PW, D'agostino RB, Sullivan L, Parise H, & Kannel WB (2002). Overweight and obesity as determinants of cardiovascular risk: The Framingham experience. Archives of Internal Medicine, 162(16), 1867–1872. [DOI] [PubMed] [Google Scholar]
- Yaemsiri S, Slining MM, & Agarwal SK (2011). Perceived weight status, overweight diagnosis, and weight control among US adults: The NHANES 2003–2008 study. International Journal of Obesity, 35(8), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Yang L, & Colditz GA (2015). Prevalence of overweight and obesity in the United States, 2007-2012. JAMA Internal Medicine, 175(8), 1412–1413. [DOI] [PMC free article] [PubMed] [Google Scholar]