Abstract
Suicide is the tenth leading cause of death in the United States. Caring Contacts (CC) is a suicide prevention intervention involving care teams sending brief messages expressing unconditional care to patients at risk of suicide. Despite solid evidence for its effectiveness, CC has not been broadly adopted by healthcare organizations. Technology has the potential to facilitate CC if barriers to adoption were better understood. This qualitative study assessed the needs of organizational stakeholders for a CC informatics tool through interviews that investigated barriers to adoption, workflow challenges, and participant-suggested design opportunities. We identified contextual barriers related to environment, intervention parameters, and technology use. Workflow challenges included time-consuming simple tasks, risk assessment and management, the cognitive demands of authoring follow-up messages, accessing and aggregating information across systems, and team communication. To address these needs, we propose design considerations that focus on automation, cognitive support, and data and workflow integration. Future work will incorporate these findings to design informatics tools supporting broader adoption of Caring Contacts.
Introduction
Suicide rates have increased by 28% over the past two decades, and suicide is now the tenth leading cause of death in the United States, with some populations, e.g., military veterans and youth, disproportionately affected1. At the same time, our lives increasingly unfold online, making new data sources available that enable the development of new supportive technologies. A range of suicide-related risk prediction models have been developed by the informatics and computer science communities2,3, but little is known about how to integrate such models to support clinical practice at the point of care. This study endeavors to take these technologies a step closer toward translational impact by identifying opportunities for informatics support within an evidence-based suicide prevention intervention.
Recommended by clinical practice guidelines4, Caring Contacts (CC) is a suicide prevention intervention currently used by several healthcare organizations across the United States. In this intervention, care team members or supportive staff (e.g., behavioral health providers, social workers, clerical staff) periodically send brief messages expressing unconditional care and concern to patients who are or previously were at risk of suicide. CC messages have been sent via letters, postcards, emails, and text messages. CC has been shown to be effective in reducing suicidal ideation and suicide attempts across diverse settings, including in clinical trials5–7. However, organizations wishing to implement CC face challenges in deciding how to make judicious use of available resources, address patient safety, and reach recipients in a meaningful way. The CC intervention is labor-intensive, as it requires time commitments from clinicians and support staff as well as physical and technological resources. Messages must be sent on a specified schedule, and some implementation sites customize messages for each recipient. Organizations must carefully weigh the advantages and disadvantages of different modalities (e.g., mail, email, text message) for staff and resource requirements. For example, emails and texts are presumed to be cheaper and faster than sending CC messages via post. It is also easier to program a sending schedule and keep track of message history with emails and texts. On the other hand, interventions based on postal mail technology are not impacted by internet availability and technology literacy. Most CC messages sent via mail never receive a response requiring clinical action, but some text messages yield responses indicating that the recipient is experiencing distress or an acute crisis. Programs must have an appropriate response and safety plan for such cases.
As a result of these kinds of challenges, CC has not been widely adopted despite its demonstrated effectiveness. Informatics approaches hold promise for addressing these challenges. A challenge of particular interest is how to leverage suicide risk prediction models to triage responses to CC messages. However, as recommended by published frameworks that guide the operationalization of predictive models for clinical decision support (CDS), a thorough understanding of the context of use and user needs must be established before model development begins8,9. Carefully designing informatics tools with the opinions and experiences of organizational stakeholders in mind is critical to successful adoption10. Therefore, there is a need to engage stakeholders to understand how an informatics tool can help address barriers to the adoption and delivery of CC among healthcare organizations.
To address this research gap, we drew on principles of human-centered design (HCD)10 to describe specific barriers to CC adoption faced by healthcare organizations, delineate workflow challenges faced by intervention staff, and formulate design considerations that can guide the development of informatics tools supporting the CC intervention. The objective of this study was to characterize specific barriers to adoption, workflow challenges, and implementation bottlenecks among organizational stakeholders, including program coordinators, leadership, social workers, and intervention staff, affecting the CC suicide prevention intervention. Findings inform design considerations for the development of CC informatics tools that help address these barriers.
Methods
We conducted a needs assessment using qualitative interviews to inform CC design considerations that meet user needs by directly engaging organizational stakeholders. The methods used for this study follow the principles of HCD as outlined by Maguire et al.10 to establish the context of use and user needs. The Institutional Review Board of the University of Washington approved study procedures.
To understand how an informatics tool can help address the barriers to the adoption and delivery of CC, we engaged organizational stakeholders with experience in planning, implementing, and delivering CC. We purposively sampled interview participants with diverse perspectives as professionals in various roles, including program coordinators (e.g., principal investigators, care directors) and CC authors (social workers, psychologists, clerical staff). We recruited participants from programs using different CC message modalities (i.e., mail, email, text message) and in different intervention settings, including research (i.e., intervention research such as clinical trials) and clinical settings (i.e., routine primary care, specialty care, and public health programs). We recruited through the authors’ existing professional networks of suicide prevention researchers and practitioners. We recruited professionals conducting suicide prevention programs serving marginalized groups, including Native American, rural, veteran, and active duty military communities. These recruitment efforts yielded mostly program coordinators, so we employed snowball sampling to reach additional participants in social work and clerical staff roles.
Data was collected via semi-structured interviews. The interview guide was developed based upon CC implementation challenges in prior research (Table 1). Across three large randomized trials Comtois et al.5,11,12 refined CC via text message and, based on expert consensus, collected an initial list of challenges and bottlenecks that a digital solution might help address. Topic areas for inquiry were based on this expert input and organized around the structure of the CC workflow (i.e., eligibility determination and enrollment; scheduling and sending caring contacts; monitoring for incoming patient responses; determining urgency and how to follow up; authoring follow-up messages; creating any external documentation). Interviews were structured to flow from general CC intervention considerations to technology-specific challenges and design opportunities to identify where informatics tools might facilitate adoption and cost-effective, time-efficient delivery of the intervention. The interview guide was pilot tested with AK, who served as domain expert and interviewee, due to her experience as both a social worker serving as a CC author and as a researcher acting as a champion.
Table 1.
Interview guide topics and example prompts
| Topics | Example prompts | |
|---|---|---|
| A. Overall intervention structure, goals, and high-level challenges | Goals and expectations | What does your program seek to accomplish? How do you align patient expectations with the intervention goals? What related risks are there? How are they addressed? |
| Barriers to intervention adoption | From your perspective, what’s the biggest reason why CC is not more broadly adopted? How is the intervention funded? What resource limitations impact the intervention? |
|
| Team makeup and dynamics | What roles have to be fulfilled to support CC? Who do you work with to support CC? How do you communicate with team members? |
|
| B. Task-specific challenges and corresponding design opportunities | Workflow challenges by task | Which tasks take the most time? Which tasks are most difficult? How do you solve the problems involved with these tasks? What do you need to complete the individual tasks (people, information)? |
| Design opportunities by task | How could an informatics platform assist with these challenges? What are the most important things you require from a CC information system? Which tasks could be automated, and which tasks should not be automated? |
|
Interviews lasted 45-60 minutes and were conducted via video conference by HAB, a Ph.D. student. The video conference software recorded and transcribed interviews for qualitative analysis. No bias due to a power differential was expected due to the relative seniority of participants and the absence of a professional relationship between interviewer and interviewee. We conducted interviews until reaching saturation, i.e., until no new themes emerged13.
In accordance with guidance from Ancker et al.14, we followed a four-stage process to conduct a deductive qualitative data analysis. First, we developed a codebook based on the topics for inquiry identified from expert input (KAC). First, to enhance the reliability of coding, two authors (HAB, ML) independently coded one-third of transcripts. Codes applied by HAB and ML were compared in consensus meetings. The definitions for the codes in the codebook were iteratively refined based on feedback from the consensus process until there was agreement in coding between coders. Second, codes were applied to all interview transcripts by one author (HAB)15,16. Third, to discover themes within our topics of inquiry, coded excerpts were grouped by similarity into emerging themes16. Fourth, we utilized member checking to verify the face validity of the themes.
Results
Sixteen individuals completed interviews (P1-P16), representing 12 unique CC programs (Table 2). The organizations included large health systems, community-based health advocacy groups, and a managed care organization. The populations served by the programs included both rural and urban communities, veterans, active duty military, and indigenous communities. Several programs sent caring messages via multiple modalities, depending on patient preference. Of the 14 participants (88%) who completed the demographic survey , nine (64%) were female, four were male (29%), and one was non-binary (7%). Ten identified as white (71%), four as Asian (29%), and one as Hispanic or Latino (7%). Six (43%) were mid-career professionals aged 40 to 49; six (43%) were 39 or younger, and two (14%) were older. Two (14%) worked primarily with indigenous communities and one (7%) was a suicide prevention professional with lived experience of suicidal thoughts and behaviors.
Table 2.
Participant characteristics
| Participants (N=16), n (%) | Programs (N=12), n (%) | ||
|---|---|---|---|
| Role | Coordinator | 6 (38%) | |
| Author | 5 (31%) | ||
| Both coordinator and author | 5 (31%) | ||
| Setting | Research | 11 (69%) | 7 (64%) |
| Clinical | 5 (31%) | 4 (36%) | |
| Modality | 6 (38%) | 4 (36%) | |
| Text | 11 (69%) | 4 (36%) | |
| 5 (31%) | 7 (64%) | ||
| Phone | 1 (6%) | 1 (9%) |
We report findings from interviews across the two topic areas in our interview guide: (A) barriers and facilitators in the overall work system surrounding the intervention structure, goals, and high-level challenges involved with adoption, implementation, and overall success of current CC programs, and (B) challenges and their potential solutions surrounding the day-to-day tasks of the CC workflow.
A. Overall work system barriers and facilitators
Three themes reflect workflow barriers expressed by participants: Context and environment, Intervention parameters, and Technology.
Context and environment. This theme describes issues stemming from CC intervention settings, ranging from incentive structures, policies, and public health trends to business considerations at the healthcare organization level. Several participants mentioned difficulties in obtaining organizational buy-in. For example, P15, a program coordinator with lived experience of suicidal thoughts and behaviors, was concerned that compared with conventional approaches to mental health treatment, CC could fuel skepticism:
“Initially, there was a lot of resistance … I was working on trying to find sustainability funding, and then it was like no we don’t want to do this … I think part of that is the uhm, not really truly believing in the fact that peer support can make a difference, the way other support cannot. And so I think there’s some of the older school thinking behind that decision making.” (P15)
Resource scarcity was a consistent theme limiting implementation efforts, ranging from a lack of funding for programs to insufficient staff, staff time, or necessary expertise. For example, P7, a CC author on a research program, shared staffing and funding constraints:
“I think it would be great to offer [CC] as another support system, but we also know that takes someone to do them, right. I mean it’s going to be part of someone’s workload, or maybe them being hired in for just that purpose, so it would really depend on whether or not they have the funding.” (P8)
Other barriers at the organizational level include the lack of focus on prevention and mental health in current incentive structures, resulting in difficulties aligning unreimbursed prevention efforts with organizational priorities. For instance, P10, a CC author working in clinical care, shared challenges with insurance reimbursement:
“How do we stop people from falling through the cracks in the medical field? They come in for something that’s medical, and unfortunately society says that medical and mental health are two separate things and they’re not. They are one big element that we should be treating the same, but instead insurance says, you can go to the hospital for your heart, but if you’re having mental health issues we’re not paying for therapy.” (P10)
P9, a researcher, emphasized that the litigious nature of the current healthcare landscape requires carefully defining the scope of practice for liability reasons:
“Someone asked me a question like, I think it was a psychiatrist who asked me, … I’m providing my care, but once they’re discharged my relationship with that person it’s over like that legal clinical relationship is over. Are you asking me to like maintain this kind of legal you know clinic relationship past that, and I was like I kind of like - well, well yeah, so, not to, maybe. You know it’s a valid question, and it does raise some issues of like liability too right. … Valid questions.” (P9)
In addition to barriers to implementing CC, participants also described several contextual and environmental facilitators. For example, organizational culture, such as an organizational mission to reduce suicides and attempts in the served population, resulted in healthcare organizations prioritizing suicide prevention. P10 shared:
“Our organization believes in it so much that they fund my position fully… we want to implement [Zero Suicide] fully, they have completely backed me … whatever I feel like I need to do for our patients to help them.” (P10)
The expectation that suicide prevention will save money in the long run facilitated investments in CC for organizations with payment structures that incentivize cost-effective care, as P13, a community health clinic director, shared:
“When you look at return on investment, we can also say that the savings do accrue to the health plan. Again this isn’t why we did [CC], but if you are a hospital, for instance, you could say, well, yes, this is good because it reduces suicidality, you know completed suicide, suicide attempts. But the savings don’t actually accrue to the hospital, or to an outpatient provider. Ethically, morally, clinically it’s the correct thing to do, but, in our case – again, this wasn’t the driver – but we should see a financial benefit from reduced hospitalizations and ED visits” (P13)
Finally, P11, a coordinator and message author in a clinical care program, added regulatory requirements as another incentive for CC:
“I think a big piece of what helped our system get to where it is, is the Joint Commission requirements as far as addressing Suicide Prevention and assessment” (P11)
Intervention parameters. Participants also described barriers and facilitators regarding intervention parameters, i.e. the intervention design and implementation specifics. This includes program goals and operating procedures, such as how people will be referred to the program, eligibility criteria, the number and timing of messages, the content of the intial CC messages, whether to include disclaimers, and whether the program entails one-way or two-way communication. Considering the wide variety of CC program designs reported, each organization must carefully consider its individual approach, which takes time and effort. Establishing policies and communicating expectations that attenuate potential risks of the intervention causing harm was a primary objective some participants described. For example, P3, a program coordinator and message author in a research study, described the challenges of developing efficient referral procedures:
“Another barrier …, in terms of kind of the complexity of moving information from the health system to the hotline, is just figuring out what that process looks like. So we have over 900 referring providers that are helping get patients referred to [the study], so training all of the providers that this resource exists and that it’s available.” (P3)
P5, a message author in a research study, added:
“I think having good protocols in order to respond well over text is probably the most time-consuming thing.” (P5)
Establishing expectations with patients was mentioned as an essential component of avoiding patient harm. P7 shared the need to clarify with patients what types of support the program is or is not designed to deliver:
“We tell participants we’re not a crisis service. And so we tell them we’re not available 24 hours” (P7)
Further, adapting the intervention to the needs of specific populations and individual patients was time-consuming. CC message authors must tailor the text, message schedules, and delivery modes for recipients of different age groups and cultural groups (e.g., indigenous communities, veterans, and healthcare workers). For example, P16, a program coordinator working with indigenous communities in a public health setting, shared:
“Our biggest lift is creating the messages [our population identifies with]” (P16)
P7 explained that messages should be caring and undemanding:
“Caring contacts is based upon the idea that if you feel connected to people in your community and you don’t feel like a burden, you feel like you like belong, that your risk of suicide goes down… It’s never asking someone to do something or telling them to do something, it should just be like generally positive, encouraging good vibes.” (P7)
P8 added that CC messages should not be too generic or repetitive:
“We don’t like to repeat the same old thing, because it makes them feel like it’s not personal for one thing, that like it’s just computer-generated. And technically, it was software, but technically it was a human behind it.” (P8)
The simplicity of CC was seen as a barrier when the complexity of its logistics was overlooked. P4 shared:
“It’s a combination of that it gets sold as a simple suicide prevention intervention. The concept is simple, right? It’s mail. Yeah. The logistics of sending and managing a year’s worth of mail is not simple.” (P4)
Technology use. Technology was generally perceived as a facilitator, but was described as a barrier when it was difficult to use, introduced inefficient workflows, obscured needed information, or did not function correctly. For example, P5 reported that some software was not usable because it required specialized skills to operate:
“One of the reasons that we had a lot of issues with our Access Database is that it requires like special SQL code and stuff for it, that me and my coworkers are not specialized to program” (P5)
P12, a coordinator of a community-based program, described how software bugs necessitated labor-intensive workarounds:
“The capability to notify staff when a patient texts back … is really important. Because in the beginning, that email notification wasn’t working. We ran into issues where I was seeing … no one responding back to this patient and it’s been, you know, a day already. And I would reach out to the clinical care pointers and they’re like Oh, we never got an email. … That actually happened, like, a few times. So that’s why, like every day, I would monitor and also have another clinical care coordinator, instead of relying on notification coming through … they would be in the portal, and they would check in the morning, midday, and then in the evening… those are kind of the type of bottlenecks that we did not anticipate” (P12)
Further, there were technology-related barriers arising from the characteristics and perceptions of the served population. Internet access and technology literacy were barriers to patient adoption of digital health tools, especially for elderly patients and those belonging to rural and native communities. For instance, P4 shared:
“There’s a lot of disconnect … especially with age. Like I have folks… like, I have to walk them through the steps of how to use their phone. … I have one who doesn’t… know how to send a text message, and he doesn’t want to know how to send a text message either.” (P4)
In contrast, technology was a facilitator when it eased data and workflow integration between different systems (e.g., transferring patient information between electronic health record (EHR) systems and text message platforms), provided mechanisms to plan and execute tasks (e.g., automatic message scheduling and sending), or captured data automatically (e.g., text message conversation history, call durations). For example, P3 shared how workflow integration with referring providers and data sharing across intervention staff facilitates the CC intervention:
“We have a best practice advisory alert the fires in Epic which informs providers that you have a patient that may be eligible… We also built out through EpicCare Link the ability to share portions of patient charts with the hotline directly, so they can see directly the safety plan that was developed… there’s a lot of technology that is facilitating this work for us.” (P3)
B. Task-specific workflow challenges and participant-suggested design opportunities
Five themes reflect workflow challenges and design opportunities reported by participants: Time-consuming simple tasks, Managing risk, Authoring helpful follow-up messages, Accessing data across sources/systems, and Team communication and collaboration.
Time-consuming simple tasks. The workload imposed by suicide prevention efforts was a recurring theme, and is particularly concerning in the context of the resource constraints we identified as system-wide barriers. The burden due to inefficient workflows emerged as a significant bottleneck in both clinical and clerical tasks completed by CC authors. Program coordinators are affected by this as well, because productivity levels will determine staffing requirements. Participants described considerable time spent on repetitive manual tasks, such as eligibility determination, scheduling and sending templated messages, and documenting communications. For example, P1 explained:
“Every person I enroll, I want them to get 11 texts on this schedule, you know, one day, one week, one month, two months. You couldn’t just tell it that; you had to literally go in there and every single message, pick the date and time.” (P1)
On the other hand, P14, a CC message author in a research study, shared that automation of such tasks is a big help:
“The fact that it just sends out texts for us automatically on a schedule and we don’t have to manually type or send a text is obviously very helpful.” (P14)
P10 described the manual nature of documenting contacts and their hopes for future technological assistance:
“In our EHR, I write that a caring contact did go out and what date it went out. … I type it out because I’m the only one. I’m sure that, as the system hires more zero suicide coordinators, because that’s the hope, that they may put something in that you can just hit a button for. But for now, I just type it out.” (P10)
Managing risk. Participants reiterated that first and foremost, patient harm must be avoided. This requires vigilance regarding the content of outgoing CC messages, monitoring and assessing risk in patient responses, and composing follow-up communications. Managing risk is a shared responsibility between all stakeholders, and therefore, both CC authors and program leadership/coordinators are affected. One key component is timeliness. Participants perceived intense pressure to provide high-quality support promptly, especially in urgent crisis situations. P3 shared the need to keep close track of patients:
“Just having a better way to track and make sure nobody falls through the cracks. I think all of us have a lot of anxiety about potentially causing harm by introducing this relationship and then someone drops accidentally when they really need help, I mean that’s like the worst thing that could happen… it’s a big concern.” (P3)
P6 shared frustration about manually collecting relevant information when time is of the essence:
“Being on call, you know… if I get a text message at, you know, one o’clock in the morning, and it’s something distressful, and I don’t even know who this person is because it wasn’t one of my [patients], now I’ve got to, you know, … gather my wits about me, trying to get on it, get some insight and some direction, and to be able to respond as quickly as possible and as accordingly as possible to ensure that person gets connected and is safe.” (P6)
Reviewing historical interactions can also reveal sensitive issues. P1 shared that bringing up something that is difficult for the patient to think or talk about should be avoided:
“If you mentioned their access to clinical care, and like the last few times they wrote back … with you know some degree of distress you might not want to [mention their access to care] again.” (P1)
P12 shared an approach to automatic flagging of potentially high-risk messages, which could help address risk management concerns:
“Say if a patient texts back and uses any of the words like, you know, hurt, kill, like any of those words, the system flags it … then sends an automated response text back to the member letting them know resources if they need help, and then also we get notified too … [we were] able to review that list and anytime we want to add new words to that list we can do that” (P12)
Authoring helpful follow-up messages. Apart from the scheduled, pre-written (or templated) CC messages, the ongoing execution of the program may require being responsive to patients who reach out for further support. While most responses from patients are straightforward expressions of gratitude, there are rare patient responses that express distress and require careful consideration to determine follow-up actions based on each patient’s individual situation. In these cases, participants emphasized that writing follow-up messages is a complex cognitive task. P1 shared:
“Authoring responses is a lot of work.” (P1)
If the intervention team determines that a CC recipient is experiencing adversity, the team must extrapolate the patient’s needs (e.g., crisis support vs. encouraging words) and compose an appropriate follow-up message. CC authors may review the patient’s history and known coping mechanisms. P14 shared:
“We look in their medical record and see if there is a safety plan … their supports and coping mechanisms and things like that.” (P14)
Assessing patients and their communications accurately is another concern. P1 shared the potential need to incorporate patient-specific factors, such as a patient’s baseline risk level, to avoid missing warning signs:
“There was one person that we classified as urgent where it kind of took a little nuance to get it, you know, for him it was urgent.” (P1)
Finally, P16 added that a CC author might customize message resources based on the patient’s individual needs:
“If somebody responds back and is like, oh sorry, I got a really bad grade on my math test, so that’s why I told you I was feeling down. And then we’ll respond back and be like, oh that’s such a bummer, did you know that, you know, if you ever want some more resources about math tutoring or anything like that to try out … From where you’re located, here are some resources for that area, specifically.” (P16)
Accessing data across sources/systems. Participants reported referring to information from several systems throughout the intervention workflow. For example, when evaluating a patient response or composing follow-up messages, staff might review prior message exchanges within the messaging system, but they might also refer to external information such as the patient’s demographics, details of their clinical history (e.g., suicidality questionnaire responses, previously documented safety plans), their current healthcare providers, and past or upcoming appointments. These data may be in one or more EHR systems, intervention-specific records (e.g., patient notes kept by intervention staff), or other data sources (e.g., text-messaging platform). CC authors are affected by these challenges in terms of productivity and ease of use. Program coordinators have to take these challenges into account when making intervention design and implementation decisions, balancing feasibility and affordability with ease of use and intervention reach. For example, P11 shared that EHR data can be informative:
“Risk factors are broad that could be someone having particular diagnoses …. [or] they’re missing a bunch of appointments” (P11)
P6 shared that integrating patient data in a single access point is desirable:
“If there was some way to provide all of that in a centralized location, where maybe ... you could write notes or keep a log of all the service members versus having to go to an excel spreadsheet and open up, and like kind of toggle back and forth, if you could have that kind of functionality … with one application” (P6)
P11 shared that access to and integration of different systems is a benefit:
“The benefit of us having a work system is that a lot of who we’re working with is kind of integrated into our current system, so I can typically see the documentation of the therapist or the treatment team, or whoever it may be. And also communicate with them in the electronic health record. Our behavioral health system uses one and our like medical side, like the hospital and stuff they use a separate one, but we can access them both.” (P11)
Team communication and collaboration. CC team members have different responsibilities, expertise, and roles, ranging from behavioral health providers and social workers to program administrators and clerical support staff. Participants describe collaboration across team members as critical to completing intervention tasks requiring diverse expertise. This affects all CC authors. For example, P16 described routing messages to follow-up specialists based on content:
“If it’s a concerning thing, he will route it to our concerning message team, within our protocol for what to do whenever we receive a concerning message/post/email. And depending on why it’s concerning, it goes to certain people.” (P16)
Sharing information across the team is essential for efficient handoff. P10 shared that different staff collect patient information at different points in a patient’s journey, requiring the transfer of notes:
“Our behavioral health evaluators are the ones that will meet them in the hospital and do all of the treatment and engagement with them in the hospital. … they will print off a face sheet and send that to me, and sometimes they will write notes like, dealing with this, please send them extra cards, or call and send the card” (P10)
Similarly, sharing intervention notes and updates with referring providers can benefit patient care continuity. P14 shared challenges to data sharing between providers due to poor data integration and system access:
“The notes that we write are kept in the research database … and their providers don’t have access to that. If they create a safety plan with their provider or with a social worker … then that is included in their chart and is visible to [both us and] their provider, but if we create the safety plan, their provider doesn’t have access to that.” (P14)
Finally, sharing the workload between intervention staff is necessary, especially when staff cover for each other (e.g., after hours). Thus, team communication is essential and represents a barrier when inefficient or when misunderstandings occur. P11 shared the need to communicate how the workload is balanced across team members:
“Just some sort of way to know that someone else did it even if it’s not fully documented yet…. That’s something that we run into as a team, that we try to support each other, but if we don’t get the opportunity to communicate something like that, it just, it doesn’t go as smoothly.” (P11)
Discussion
Through this needs assessment, we established the context of use, identified barriers to adopting the CC suicide prevention intervention among organization stakeholders, and identified opportunities for informatics tools to help address these barriers. Our findings broadly fall into two categories: overall work system barriers and facilitators and task-specific workflow challenges.
Any informatics tool must be designed with the context of use in mind. The work system themes that establish this context included high-level contextual and environmental obstacles, intervention design and implementation issues, and system-level technology concerns. While it may not be possible to address all barriers and challenges directly with an informatics tool, they must be accounted for, as they place constraints on tool design and deployment. For example, a significant limitation is that the incentive structures currently in place in the U.S. healthcare system are not favorable to preventive care. To make CC broadly feasible within this constraint, we must prioritize the judicious use of human resources to control costs.
Task-level workflow challenges represent pain points in current workflows and therefore reflect opportunities for informatics tools to help. Five themes emerged from these workflow challenges. We now present design considerations for addressing these challenges within the work system constraints, including context of use/environment, intervention design, and technology use, along with examples illustrating how informatics support could be implemented in future work.
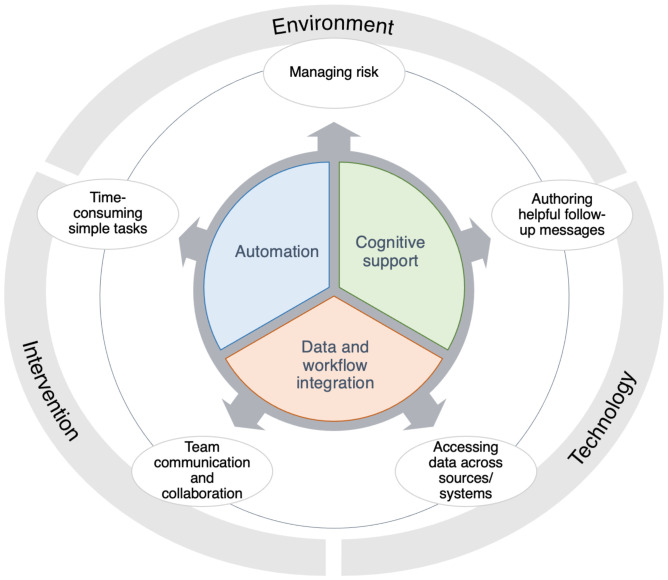
Our findings point to three cross-cutting design considerations that are key to addressing these workflow challenges: Automation, Cognitive support, and Data and workflow integration (Figure 1).
Figure 1.
Summary of findings mapped to design considerations for informatics-supported suicide prevention Work system constraints are shown on the outer circle. Workflow challenges are shown in bubbles. Design considerations for addressing challenges are shown in the inner circle.
Automation. Resource scarcity emerged as a recurring theme. The workload imposed by CC can present an insurmountable barrier to implementation. Informatics tools can help alleviate this burden, as many repetitive tasks could be partially or fully automated. These tasks include checking patient suitability or eligibility for CC, scheduling initial CC messages, and sending automated responses to texts or emails. There are also opportunities to integrate predictive modeling tools. For example, several promising approaches to personalized risk modeling using Natural Language Processing (NLP) and machine learning have been reported 2,3; such methods could be used to trigger automatic responses with a crisis line phone number to a patient who expresses immediate intent for self-harm and to flag and prioritize messages for follow-up. Messages could also be automatically routed to staff with appropriate expertise based on message content.
Information retrieval and synthesis for cognitive support. Authoring follow-up messages can be a demanding cognitive task. For this purpose, intervention staff must not only collect various pieces of relevant information, but also synthesize and harmonize that information in order to make clinical judgments and formulate follow-up actions. Participants described using different kinds of data and insights, including a recipient’s health history (e.g., demographics, diagnoses, appointments), risk and protective factors (e.g., social determinants of health), and interaction history (e.g., to determine what kinds of messages were previously well received). Informatics tools could provide cognitive support by aggregating and synthesizing information from different data sources in an easily digestible format (e.g., a timeline of challenging life events and corresponding trends in suicide risk) to reveal insights for CDS. A system could also draw links between available resources and patients’ resource needs and present suggestions to authors accordingly. Opportunities for advanced cognitive support tools include mining message exchange histories for patterns in patient communication and automatic extraction of clinically relevant insights and therapeutic opportunities (e.g., symptoms, risk factors emerging from patient communications, warning signs).
Data and workflow integration. The intervention workflows that informatics tools for CC should support require communication between systems and people with different roles and responsibilities. For example, programs may aim to provide some level of support around the clock, which means that follow-up specialists may not know individual patients well (e.g., when covering for someone else); CC tools may draw on previously described technology-facilitated handoff approaches17 to support these workflows. Additionally, it is essential to avoid miscommunications, e.g. to prevent harm due to a patient in need of support not receiving a response due to a lack of clarity regarding patient assignments. CC tools should therefore provide planning tools such as task and priority lists. Information exchange with other health information technology platforms is also critical. Automatically incorporating external patient information, e.g. safety plans from the referring providers’ EHRs, can benefit intervention staff as they evaluate and follow up with patients, without requiring duplicated data entry efforts. Similarly, sharing intervention notes and updates back to the referring provider’s EHR could support ongoing care or insurance reimbursement. Data integration can also facilitate reporting on outcome metrics to help CC program coordinators monitor and improve the CC program. Additionally, workflow integration is an essential component of reducing the workload imposed by working in multiple information systems. While data and workflow integration between health information technology platforms are well established requirements, they have been prohibitively difficult to enable for many reasons, including privacy and governance concerns, technical infrastructure, and diverging data formats. Fortunately, health data standards and exchange protocols are maturing, and today we have well-adopted, freely available standards such as FHIR and workflow integration tools such as Smart on FHIR and CDS Hooks18 which make it possible to overcome some of these barriers. For example, Smart on FHIR could enable users to launch CC workflows directly from within the EHR, automatically pulling in relevant patient record information. Additionally, FHIR includes API endpoints for common data exchange tasks; for example, with appropriate permissions in place, an external system can use a FHIR endpoint to automatically file a clinical note to any EHR implementing FHIR.
Recently, there has been a proliferation of suicide-related risk prediction models2 using diverse data sources, e.g. patient-generated natural language data3 from Facebook19, Twitter20, and Reddit21 posts, query terms used for internet searches22, and EHR data such as diagnoses23. These approaches demonstrate promise, but it is unclear how to operationalize such models to make a clinical impact, which motivates the current work. CDS tools have been intensely investigated in the field of biomedical informatics, and guidelines for designing effective decision support have been published24. Based on these guidelines, critical questions for CDS tools for CC include: Who has the ability to act upon risk predictions in a way that impacts outcomes? When and how can they benefit from predictions? At that point, what data is available for inference? What else is needed for a clinician to act upon the new knowledge within their established workflows? These questions illustrate the complexity of creating decision support tools with the potential to improve clinical care and impact patient outcomes, which is further underscored by the scarcity of examples of success described in the literature. To guide such work, Shah et al.8 developed a framework for making predictive models useful in practice. Here, we aimed to complete the indispensable first step described in this framework: establishing the use case for a suicide risk assessment model. Our work identified several use cases for artificial intelligence tools, and helps answer the questions listed above. It also revealed a broad set of challenges and opportunities related to end-to-end workflow support, suggesting the need to adopt a broader perspective. In order to realize the translational impact of new and existing predictive technologies, we must therefore design a CDS system that supports the workflow comprehensively. Our design considerations provide holistic guidance for both the workflow and artificial intelligence components that CC informatics support tools may include. In future work, we will use these findings to design and develop an informatics tool suitable for a pilot deployment.
This work must be considered in light of its limitations. Our participants were sampled from our existing professional network and subscribers of a suicide prevention mailing list who responded to a volunteer request, which may have biased our sample towards those who already perceive more benefits than barriers to CC implementation. While we tried to capture broad perspectives on barriers, our focus on technology may have biased participants’ responses. Finally, this work investigated the perspectives of the potential users of CC information technology who administer the intervention, rather than the perspectives of patient users who are the targets of the intervention. Prior work has investigated the acceptability of the intervention to patients5,25; however, if the use of novel informatics tools were to change the patient experience of the intervention, it would be necessary to re-engage patients to ensure acceptability.
Conclusion
This work identified barriers to adoption, workflow challenges, and design opportunities for informatics tools supporting the CC suicide prevention intervention among organizational stakeholders. With newfound clarity regarding the opportunities for technology support, including CDS tools such as risk prediction models, this work contributes to realizing the translational potential of informatics interventions to benefit clinical care.
Acknowledgments
This work was supported by Innovation Grant “Informatics-Supported Authorship for Caring Contacts (ISACC)” from the Garvey Institute for Brain Health Solutions.
Figures & Table
References
- 1.Stone DM, Simon TR, Fowler KA, Kegler SR, Yuan K, Holland KM, et al. Trends in state suicide rates 1999-2016. Morb Mortal Wkly Rep. 2018;67:617–24. doi: 10.15585/mmwr.mm6722a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bernert RA, Hilberg AM, Melia R, Kim JP, Shah NH, Abnousi F. Artificial intelligence and suicide prevention: A systematic review of machine learning investigations. Int J Environ Res Public Health. 2020;17:1–25. doi: 10.3390/ijerph17165929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Resnik P, Foreman A, Kuchuk M, Musacchio Schafer K, Pinkham B. Naturally occurring language as a source of evidence in suicide prevention. Suicide Life-Threatening Behav. 2020. pp. 1–9. [DOI] [PubMed]
- 4.U.S Department of Veteran Affairs. VA/DoD Clinical Practice Guideline for the Assessment and Management of Patients at Risk of Suicide. 2019;35 Available from: https://www.healthquality.va.gov/guidelines/MH/srb/ [Google Scholar]
- 5.Comtois KA, Kerbrat AH, DeCou CR, Atkins DC, Majeres JJ, Baker JC, et al. Effect of Augmenting Standard Care for Military Personnel With Brief Caring Text Messages for Suicide Prevention. JAMA Psychiatry. 2019;76:474. doi: 10.1001/jamapsychiatry.2018.4530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reger MA, Luxton DD, Tucker RP, Comtois KA, Keen AD, Landes SJ, et al. Implementation methods for the caring contacts suicide prevention intervention. Prof Psychol Res Pract. 2017;48:369–77. [Google Scholar]
- 7.Luxton DD, June JD, Comtois KA. Can postdischarge follow-up contacts prevent suicide and suicidal behavior? A Review of the Evidence. Crisis. 2013;34:32–41. doi: 10.1027/0227-5910/a000158. [DOI] [PubMed] [Google Scholar]
- 8.Jung K, Kashyap S, Avati A, Harman S, Shaw H, Li R, et al. A framework for making predictive models useful in practice. J Am Med Informatics Assoc. 2020;00:1–10. doi: 10.1093/jamia/ocaa318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seneviratne MG, Shah NH, Chu L. BMJ Innovations. Vol. 6. BMJ Publishing Group; 2020. Bridging the implementation gap of machine learning in healthcare; pp. 45–7. [Google Scholar]
- 10.Maguire M. Methods to support human-centred design. Int J Hum Comput Stud. 2001;55:587–634. [Google Scholar]
- 11.Nelson L, Comtois K. Caring Contacts: A Strength-based, Suicide Prevention Trial in 4 Native Communities (CARE) clinicaltrials.gov. 2016. Available from: https://clinicaltrials.gov/ct2/show/NCT02825771.
- 12.Comparing two ways for healthcare providers to intervene to prevent suicide among adults and adolescents. 2019.
- 13.Guest G, Bunce A, Johnson L. How Many Interviews Are Enough?: An Experiment with Data Saturation and Variability. Field methods. 2006;18:59–82. [Google Scholar]
- 14.Ancker JS, Benda NC, Reddy M, Unertl KM, Veinot T. Guidance for publishing qualitative research in informatics. J Am Med Informatics Assoc. 2021;00:1–6. doi: 10.1093/jamia/ocab195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 16.Saldaña J. The Coding Manual for Qualitative Researchers. 4th ed. Sage Publications, Inc.; 2021. [Google Scholar]
- 17.Abraham J, Kannampallil T, Patel VL. A systematic review of the literature on the evaluation of handoff tools: Implications for research and practice. J Am Med Informatics Assoc. 2014;21:154–62. doi: 10.1136/amiajnl-2012-001351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Strasberg HR, Rhodes B, Del Fiol G, Jenders RA, Haug PJ, Kawamoto K. Contemporary clinical decision support standards using Health Level Seven International Fast Healthcare Interoperability Resources. J Am Med Informatics Assoc. 2021;00:1–11. doi: 10.1093/jamia/ocab070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gomes de Andrade NN, Pawson D, Muriello D, Donahue L, Guadagno J. Ethics and Artificial Intelligence: Suicide Prevention on Facebook. Philos Technol . 2018;31:669–84. [Google Scholar]
- 20.Coppersmith G. Quantifying Suicidal Ideation via Language Usage on Social Media. Acta Anaesthesiol Scand. 2015;49:1387–90. [Google Scholar]
- 21.Low DM, Rumker L, Talkar T, Torous J, Cecchi G, Ghosh SS. Natural language processing reveals vulnerable mental health support groups and heightened health anxiety on reddit during COVID-19: Observational study. J Med Internet Res. 2020;22:1–16. doi: 10.2196/22635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Areán PA, Pratap A, Hsin H, Huppert TK, Hendricks KE, Heagerty PJ, et al. Perceived Utility and Characterization of Personal Google Search Histories to Detect Data Patterns Proximal to a Suicide Attempt in Individuals Who Previously Attempted Suicide: Pilot Cohort Study. J Med Internet Res. 2021;23:e27918. doi: 10.2196/27918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simon GE, Johnson E, Lawrence JM, Rossom RC, Ahmedani B, et al. Predicting suicide attempts and suicide deaths following outpatient visits using electronic health records. Am J Psychiatry. 2018;175:951–60. doi: 10.1176/appi.ajp.2018.17101167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bates DW, Kuperman GJ, Wang S, Gandhi T, Kittler A, Volk L, et al. Electronic Health Records: Challenges in Design and Implementation. Apple Academic Press; 2013. Ten commandments for effective clinical decision support: Making the practice of evidence-based medicine a reality; pp. 135–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Landes SJ, Jegley SM, Kirchner JE, Areno JP, Pitcock JA, Abraham TH, et al. Adapting Caring Contacts for Veterans in a Department of Veterans Affairs Emergency Department: Results From a Type 2 Hybrid Effectiveness-Implementation Pilot Study. Front Psychiatry. 2021;12:1–11. doi: 10.3389/fpsyt.2021.746805. [DOI] [PMC free article] [PubMed] [Google Scholar]