Abstract
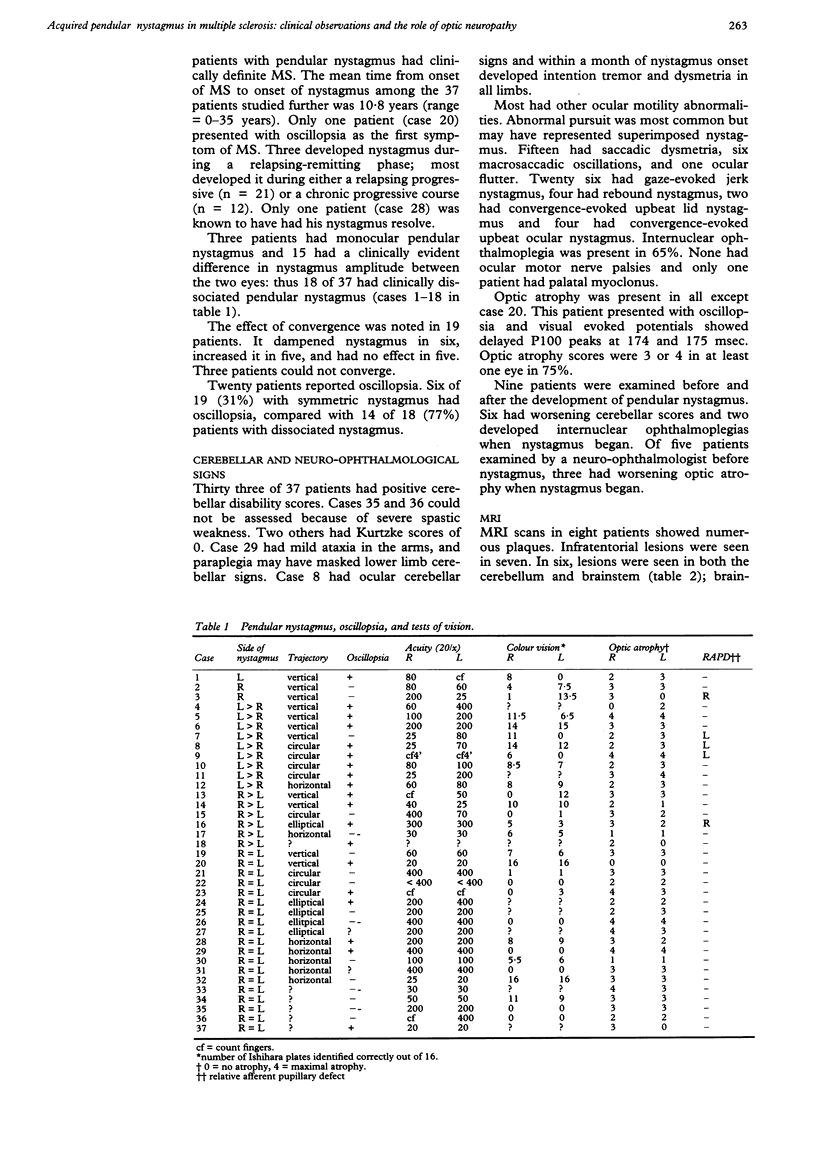
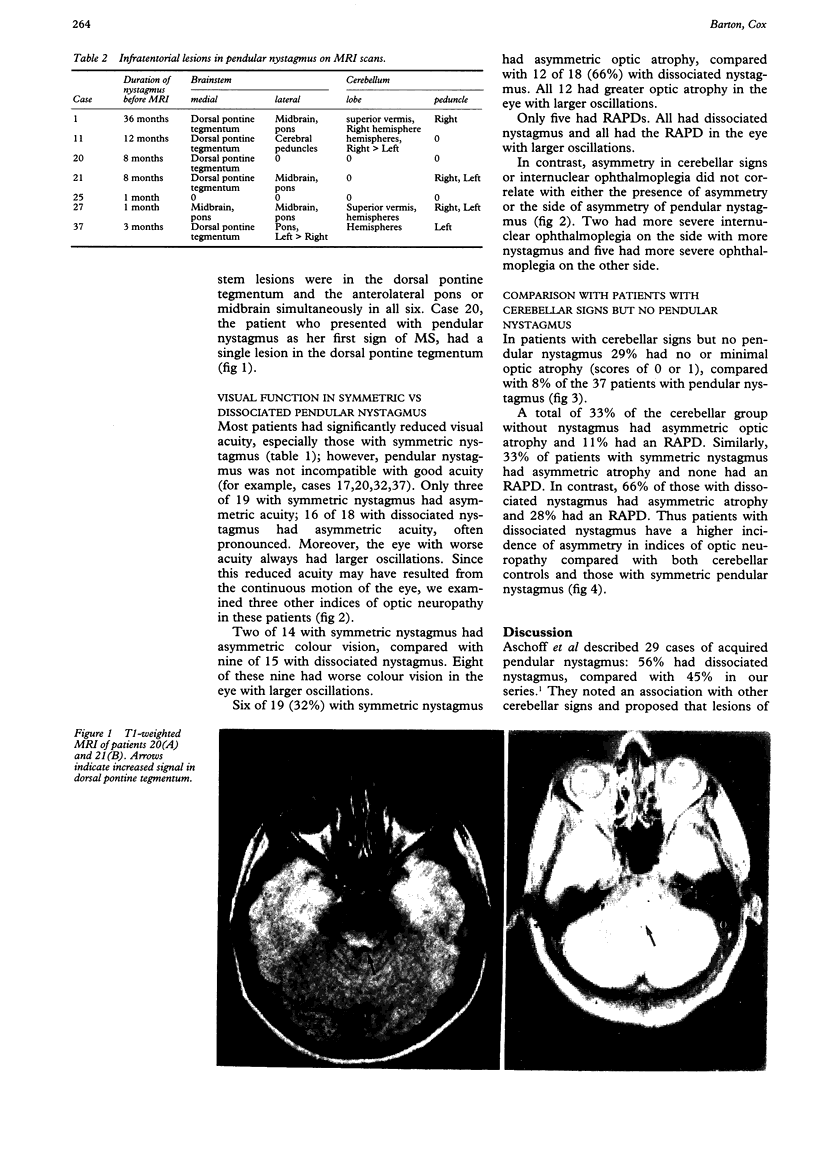
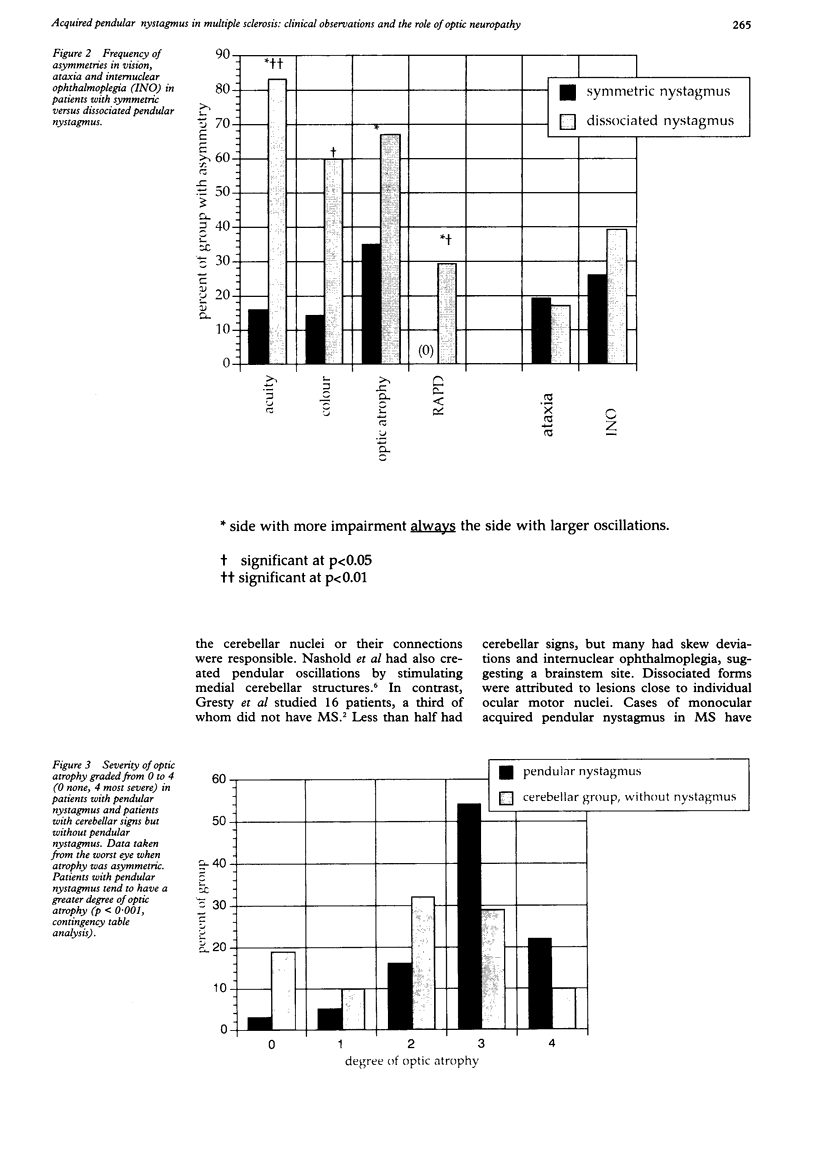
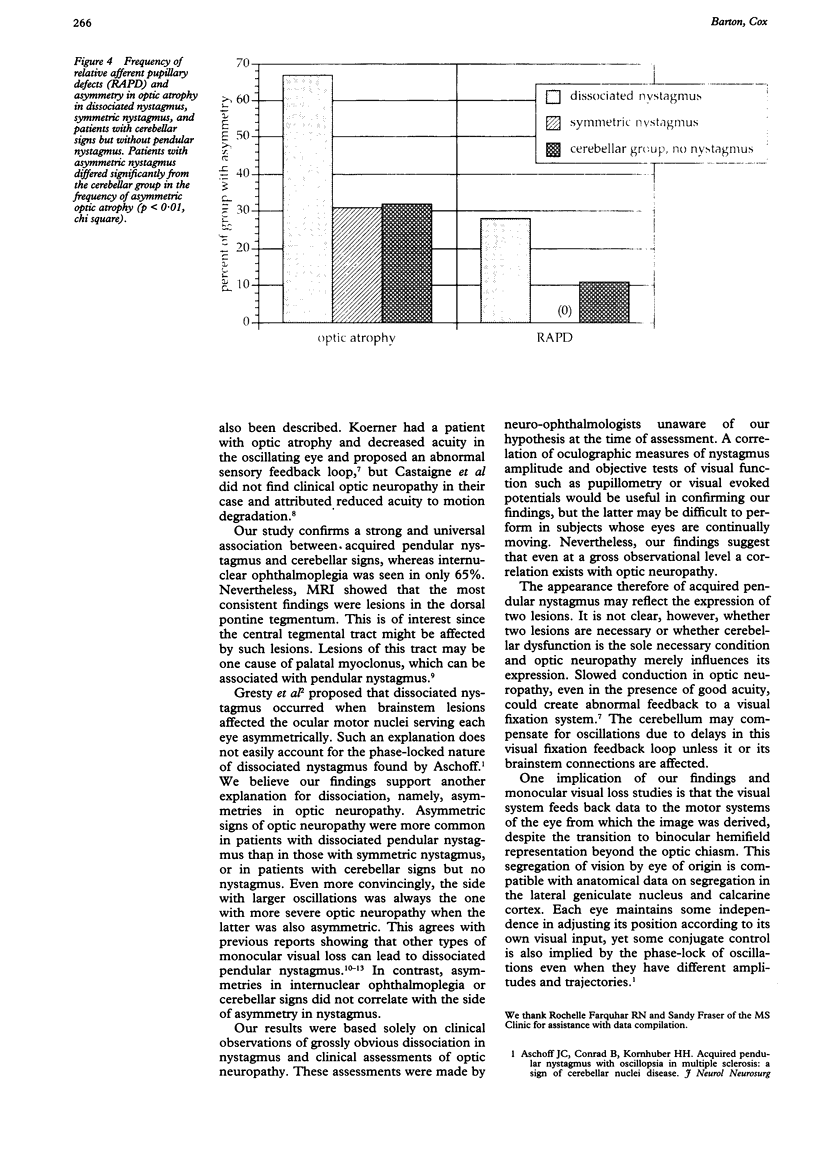
Thirty seven patients with pendular nystagmus due to multiple sclerosis were reviewed. Most developed nystagmus later in a progressive phase of the disease. All had cerebellar signs on examination and evidence of optic neuropathy. MRI in eight patients showed cerebellar or brainstem lesions in seven; the most consistent finding was a lesion in the dorsal pontine tegmentum. Dissociated nystagmus was seen in 18 patients: in these the signs of optic neuropathy were often asymmetric and the severity correlated closely with the side with larger oscillations. This suggests that dissociations in acquired pendular nystagmus may be due to asymmetries in optic neuropathy rather than asymmetries in cerebellar or brainstem disease.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Castaigne P., Chain F., Pierrot-Deseilligny C., Larmande P. Le nystagmus de circumduction monoculaire. Etude clinique, oculographique et électro-myographique d'un cas, dans la sclérose en plaques. Rev Neurol (Paris) 1979 Jan;135(1):51–57. [PubMed] [Google Scholar]
- Cox T. A. Relative afferent pupillary defects in multiple sclerosis. Can J Ophthalmol. 1989 Aug;24(5):207–210. [PubMed] [Google Scholar]
- Gresty M. A., Ell J. J., Findley L. J. Acquired pendular nystagmus: its characteristics, localising value and pathophysiology. J Neurol Neurosurg Psychiatry. 1982 May;45(5):431–439. doi: 10.1136/jnnp.45.5.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh R. J., Thurston S. E., Tomsak R. L., Grossman G. E., Lanska D. J. Effect of monocular visual loss upon stability of gaze. Invest Ophthalmol Vis Sci. 1989 Feb;30(2):288–292. [PubMed] [Google Scholar]
- Nakada T., Kwee I. L. Oculopalatal myoclonus. Brain. 1986 Jun;109(Pt 3):431–441. doi: 10.1093/brain/109.3.431. [DOI] [PubMed] [Google Scholar]
- Nashold B. S., Jr, Slaughter D. G., Gills J. P. Ocular reactions in man from deep cerebellar stimulation and lesions. Arch Ophthalmol. 1969 Apr;81(4):538–543. doi: 10.1001/archopht.1969.00990010540013. [DOI] [PubMed] [Google Scholar]
- Sharpe J. A., Hoyt W. F., Rosenberg M. A. Convergence-evoked nystagmus. Congenital and acquired forms. Arch Neurol. 1975 Mar;32(3):191–194. doi: 10.1001/archneur.1975.00490450071010. [DOI] [PubMed] [Google Scholar]
- Smith J. L., Flynn J. T., Spiro H. J. Monocular vertical oscillations of amblyopia. The Heimann-Bielschowsky phenomenon. J Clin Neuroophthalmol. 1982 Jun;2(2):85–91. [PubMed] [Google Scholar]
- Stangler-Zuschrott E. Störungen der Okulomotorik während Punktfixation des führenden Auges bei einseitiger Deprivationsamblyopie, Schielamblyopie und einseitigem Organschaden. Klin Monbl Augenheilkd. 1987 Nov;191(5):403–408. doi: 10.1055/s-2008-1050542. [DOI] [PubMed] [Google Scholar]
- Yee R. D., Jelks G. W., Baloh R. W., Honrubia V. Uniocular nystagmus in monocular visual loss. Ophthalmology. 1979 Apr;86(4):511–522. doi: 10.1016/s0161-6420(79)35489-6. [DOI] [PubMed] [Google Scholar]