Abstract
The COVID-19 pandemic has impacted the mental health of the youngest, worsening their emotional well-being. The demand for care in psychiatric emergencies may indirectly reflect the mental health state of children and adolescents and the emotional consequences of the pandemic. Moreover, suicidality can be considered a marker of severity in this population group.
Therefore, we have aimed to longitudinally describe the number of children and adolescents attended in the psychiatry emergency department due to suicidal ideation or attempts and, to explore differences in suicidality according to gender and age. A retrospective study was carried out in the University Hospital of San Juan, Alicante, Spain, from January 01, 2018 to December 31, 2021. A total of 138 participants under 18 years requesting psychiatric care due to suicidal ideation or attempts were included. The sample was composed by 35% of males and the mean age was 14.8 years old (SD = 2.2).
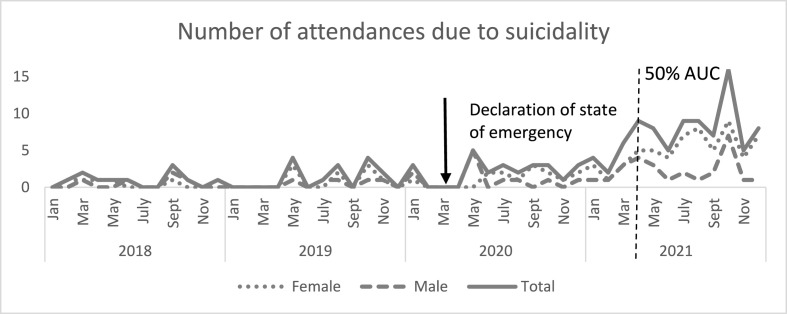
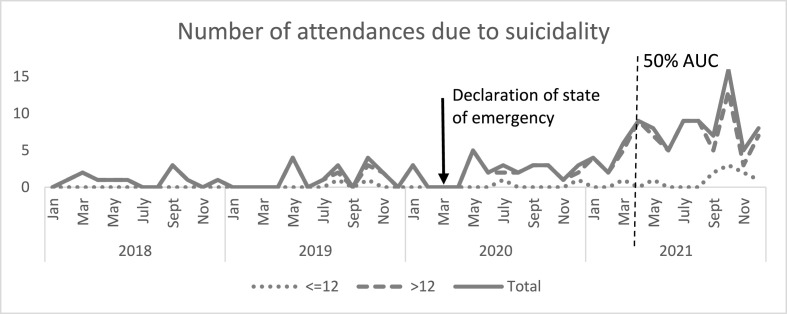
The number of cases per year range from 10 in 2018 to 88 in 2021. Attendances were significantly higher between 2021 and the three previous years. Besides, the number of attentions registered in the last 9 months of 2021 equals those that occurred in the entire previous period. Most of the cases were girls and middle adolescents.
Suicide ideation or attempts have skyrocketed in children and adolescents. This alarming increase presents a one-year lag peak from the COVID-19 outbreak and continues until the end of 2021. Girls and those over 12 years have been identified as risk groups to present suicidal ideation or attempts.
Keywords: Children, Adolescents, Suicide ideation, Suicide attempts, Emergency department, COVID-19
1. Introduction
For the time being, the Coronavirus Disease 2019 (COVID-19) has supposed the biggest health crisis experienced in the 21st century, and a persistent threat to health and to the economic and social system worldwide (Joffe, 2021).
At the beginning of the outbreak, the increase in the number of cases and deaths and, therefore, the need to adopt urgent measures to stop the spread of the virus, led to the paralysis of all activities considered non-essential, including the closure of schools (BOE, 2020; Viner et al., 2020). Forced quarantine, social distancing, self-isolation, confinement, move restrictions, and the limitation of leisure and sports have characterized the interpersonal, occupational, and social relationships since the beginning of the pandemic, also for children and adolescents (López-Bueno et al., 2021; Viner et al., 2020).
Age has been found to be a relevant factor moderating the relationship between stress due to COVID-19 pandemic and emotional wellbeing (Barber and Kim, 2021). Research suggests that older adults have been more capable to handle the stress caused by the pandemic (García-Fernández et al., 2020) while children and adolescents have been especially prone to the development of emotional distress during the COVID-19 outbreak (Marques de Miranda et al., 2020; Ravens-Sieberer et al., 2021). In fact, compared to adults, the youngest have shown a higher risk of developing mental health problems and even long-term adverse consequences (Shen et al., 2020; Singh et al., 2020) whose quality and magnitude is moderated by factors like fear of infection, quarantine or lockdown, developmental age, educational status, previous mental health disorders and, economic and social precariousness (Singh et al., 2020).
Of particular concern has been the alarming increase in mental disorders in children and adolescents reported by scientific societies, who noticed a significant rise in symptoms of stress, depression, and anxiety, as well as a significant decrease in life satisfaction during the COVID-19 outbreak (Magson et al., 2021). This increase, which has been particularly pronounced among girls (Tamarit et al., 2020; Magson et al., 2021), has led to a saturation of emergencies services due to psychosocial morbidity in paediatric hospitals.
Research focused on attentions to the psychiatric emergency department in children and adolescents have experienced an initial increase in mental health presentations despite the immediate fall that followed the lockdown (Davico et al., 202; Ferrando et al., 2021) and the decrease in overall paediatric emergencies for any reason at the beginning of the outbreak (Chadi et al., 2021; Carison et al., 2022). This increase has been especially prominent for suicidal ideation or attempts throughout the following school year, especially among girls in Spain (Gracia et al., 2021).
Regarding to suicide, which continues to be the second leading cause of death among 15–29 year-olds worldwide (Yuodelis-Flores and Ries 2015), research conducted during the pandemic yields discrepant results depending on the duration of the observation period and its relationship with the COVID-19 first wave (Brasso et al., 2022). Studies conducted at the beginning of confinement with short follow-up periods do not find significant changes in the suicide rate compared to previous periods (Isumi et al., 2020), or even some point to a decrease in attentions to the psychiatric emergency department due to suicidal ideation or attempts (Davico et al., 2021; Mourouvaye et al., 2021; Zhu et al., 2021). On the other hand, studies with longer observation periods coincide in detecting an increase in young people requesting urgent psychiatric care due to suicidal thoughts or gestures (Carison et al., 2022; Chadi et al., 2021; Cousien et al., 2021; Gracia et al., 2021; Leff et al., 2021; Sokoloff et al., 2021; Yard et al., 2021). However, the follow-up period of the studies evaluating suicidality in the psychiatric emergency department do not exceed March 2021, nor they analyse differences based on age.
Therefore, in this report we have aimed to fill this gap by describing the pattern of change in the frequency of attentions to the psychiatry emergency department of children and adolescents requesting care for suicidal ideation or attempts with three main objectives: 1) to carry out a two year long-term follow-up study from the COVID-19 outbreak; 2) to examine whether there are differences in the frequency of suicidality according to gender and; 3) to examine whether there are differences in the frequency of suicidality according to age.
2. Methods
A longitudinal retrospective review was carried out to evaluate the children and adolescent's request for psychiatric emergency attention in the University Hospital of San Juan in Alicante, Spain, from January 01, 2018 to December 31, 2021. The psychiatry emergency department of this hospital assumes an area with a population of 550,000 inhabitants, including children and adolescents as well as adults, from both rural and urban areas. The dates selected included the initial period of the pandemic in which the whole Spanish population was confined from March to June 2020 and the schools were closed until September 2020, as well as the entire year 2021 when children and adolescents began to return to normality. The two years prior to the outbreak of the pandemic were also collected for basal comparison. The study was approved by the local clinical research ethics committee (20/018).
All assistances to the psychiatry emergency department for any reason were collected from the hospital's electronic health information system, both in adults and, children and adolescents. Participants were included if they 1) themselves or their families had requested urgent psychiatric care, 2) were aged under 18 years and, 2) the reason for attention was suicidal ideation or attempts. Participants were excluded if 1) they presented with any demand or diagnosis different from suicidality, 2) the information regarding the reason for attention or referral to discharge was missing and 3) they were treated twice or more for suicidal ideation or attempts, when only the first attention was recorded.
Data on age and gender of each patient were obtained from the hospital's electronic health information system. The diagnosis was based on constructed interviews performed by experienced psychiatrists, according to the International Classification of Diseases 10, the hospital's diagnostic coding system. The number of total attentions throughout the four-year period were also registered.
2.1. Statistical analysis
Mean and standard deviation was used to describe quantitative variables, and proportions for qualitative ones. To test differences in the proportion of attendances at psychiatric emergency services due to suicidal ideation or attempts over the years, binomial tests (using the Bonferroni correction to control the Type I error rate) were carried out. Additionally, using the number of cases separated by month and year, half of the area under the curve (AUC) was calculated. This time point can be considered an indication of the moment at which the number of suicidal behaves start to escalate. Also, binomial tests were used to study the effect of gender and age (≤12 vs. >12 years old) on suicidality.
3. Results
A total of 138 cases (age range from 8 to 17) who attended to the psychiatric emergency department between January 2018 and December 2021 due to suicidal ideation or attempts were studied. The sample was composed by 35% of males, the mean age was 14.8 years old (SD = 2.2). The number of cases range from 10 attentions during 2018, 14 attentions during 2019, 26 attentions during 2020 and up to 88 attentions during 2021 (See Table 1 ).
Table 1.
Number and percentage of attentions due to suicidal ideation or attempts in children and adolescents in relation to the total number of patients and to the paediatric population attended for any reason in the psychiatric emergency department during the study period.
| Psychiatric emergency department attentions | 2018 | 2019 | 2020 | 2021 |
|---|---|---|---|---|
| Total attentions for any reason in adults, children and adolescents, n | 2006 | 2023 | 2065 | 2538 |
| Suicidal ideation or attempts attentions in children and adolescents, n (%) | 10 (0.5%) | 14 (0.7%) | 26 (1.3%) | 88 (3.5%) |
| Total attentions for any reason in children and adolescents, n | 62 | 84 | 109 | 283 |
| Suicidal ideation or attempts attentions in children and adolescents, n (%) | 10 (16.1%) | 14 (16.6%) | 26 (23.8%) | 88 (31.1%) |
Binomial test showed that differences in the number of attendances due to suicidal ideation or attempts were statistically significant between 2021 and the three previous years (See Table 2 ).
Table 2.
Results of the binomial test comparing the total number of cases per year using the Bonferroni adjustment for p-values.
| Comparing years | Binomial test | Adjusted p-value |
|---|---|---|
| 2018 vs. 2019 | Z = −0.59 | p = 0.999 |
| 2018 vs. 2020 | Z = −2.46 | p = 0.084 |
| 2018 vs. 2021 | Z = −6.84 | p < 0.001 |
| 2019 vs. 2020 | Z = −1.97 | p = 0.288 |
| 2019 vs. 2021 | Z = −6.70 | p < 0.001 |
| 2020 vs. 2021 | Z = −4.92 | p < 0.001 |
Regarding gender differences, binomial tests showed that an increase in the number of girls occurred in 2021, meanwhile no differences in the proportion of males and females were detected in previous years. On the other hand, in the case of age, the proportion of attentions is significantly larger in the >12 age group throughout the study (see Table 3 ).
Table 3.
Results of the binomial test comparing the proportion of gender using the Bonferroni adjustment for p-values.
| Year | Male vs. Female | Adjusted p -value | ≤12 years vs. >12 years | Adjusted p -value |
|---|---|---|---|---|
| 2018 | Z = 0.30 | p = 0.999 | Z = −2.71 | p = 0.028 |
| 2019 | Z = 1.07 | p = 0.999 | Z = −2.67 | p = 0.032 |
| 2020 | Z = 0.60 | p = 0.999 | Z = −4.20 | p < 0.001 |
| 2021 | Z = 3.62 | p = 0.004 | Z = −7.25 | p < 0.001 |
Additionally, half of the area under the curve (AUC) was calculated to illustrate the time-point at which considerably increase in the number of suicidal behaviours occurred. As can be seen in Fig. 1 , the AUC in the last 9 months of 2021 equate to the previous three years and three months in terms of attendances to the psychiatric emergency department due to suicidality in children and adolescents. As can also be observed in Fig. 1, Fig. 2 , most of the cases are girls and above 12 years old. Specifically, from the 62 cases who received care before April 2021, 58.1% of them were girls, and 91.9% of them older than 12 years. From the remaining 76 cases that occurred on or after April 2021, 71.1% of them were girls and 88.2% of them older than 12 years.
Fig. 1.
Representation of attendances due to suicidal ideation or attempts in children and adolescents during the 2018–2021 period. The total number of cases is also presented separated by gender.
Fig. 2.
Representation of attendances due to suicidal ideation or attempts in children and adolescents during the 2018–2021 period. The total number of cases is also presented separated by age (≤12 vs. >12 years old).
4. Discussion
The main objective of this study was to analyse the evolution of the psychiatric emergencies due to suicidal ideation or attempts in children and adolescents in a 4-year follow-up period, from January 2018 to December 2021, based on the review of electronic health records. Such period includes the psychiatric morbidity of the youngest during the COVID-19 pandemic and also along the two years previous to the COVID-19 outbreak in order to visualize the trend of suicidality in this population group.
Regarding to the objectives of this study, the first interesting finding is the significant increase peaking in 2021 in the demand for emergency psychiatric care due to suicidal ideation or attempts, which may reflect an unprecedented disturbance of the well-being of children and adolescents, markedly larger than that of the grown-ups (Singh et al., 2020; Meherali et al., 2021), and significantly higher when compared to 2018, 2019 and 2020 separately, in addition to a one-year lag between the initial peak of the pandemic and the peak of suicidality.
Suicidal behaviour among children and adolescents, one of the most robust mental health outcomes, was not significantly affected during the first wave of the pandemic (Isumi et al., 2020), with studies that even describe an immediate decrease in suicidality assessed in the emergency department in the initial phases of the outbreak compared to the previous few weeks or months (Davico et al., 2021; Ferrando et al., 2021; Mourouvaye et al., 2021). This could be due in part, at least in Spain, to the initial lockdown period, which lasted from March 14th to June 21st and entailed a restriction of all non-essential activities, which undoubtedly might have limited the access to emergency services. However, suicidal ideation or attempts have worryingly increased in adolescents during the last period of the COVID-19 pandemic (Mayne et al., 2021; Hertz and Barrios, 2021) especially in girls (Gracia et al., 2021; Tanaka et al., 2021) and, as our results point out, this dramatic increase appears exactly one year after the outbreak of the pandemic, in the spring of 2021 and is maintained until December 2021, when the observation period ends.
The reasons for suicide are complex and diverse, but the social stress experienced during the pandemic may partially explain the increased demand for urgent care due to suicidality. In the initial phase of the outbreak, a period of cessation of all activity and closure of schools with no academic pressure, followed by a summer period characterized by the end of confinement and the control of the first wave, could explain the absence of differences in the rate of suicidality between 2020 and, 2019 and 2018. Otherwise, coinciding with the start of the school year in September 2020, a progressive increase in suicidal ideation or attempts is observed with its maximum peak at the beginning of the next school year, in September 2021, that remains high until the end of the year. Stress from returning to school (Tanaka et al., 2021), disruptions with children and adolescent's usual lifestyle (Ghosh et al., 2020), together with the lack of normalized social interactions with peers may have led to difficulties to self-regulate emotions and acting out behaviours (Gracia et al., 2021). Without forgetting, furthermore, that adolescence itself is characterized by emotional lability, a tendency to magnify problems and a lack of impulse control that may also promote suicidal behaviours in adverse circumstances such as the pandemic.
The second important finding has to do with gender. Our results identify girls as especially vulnerable to developing suicidal ideation or attempts since the outbreak of the COVID-19 pandemic, more specifically during 2021, supporting the limited research evaluating gender differences in suicidality during a longer time span after COVID-19 (Gracia et al., 2021; Tanaka and Okamoto, 2021; Yard et al., 2021). We can assume that these data reflect the gender differences already observed in adulthood, with women showing more suicide attempts and men more completed suicides (Hamdi et al., 1991), the so-called gender paradox in suicidal behaviour (O'Loughlin and Sherwood, 2005), which could respond to the greater predisposition of women to suffer from anxiety or depression.
Our data also indicate that middle adolescents are more vulnerable to the deleterious psychological effects of the pandemic compared to younger children, at least in Spain, where the study was developed (Gracia et al., 2021). Adolescents are therefore a target population for which effective strategies to reduce suicide should be implemented.
We acknowledge some limitations. First, no differentiation was made between suicidal ideation and attempts, which were evaluated as a single category; second, no structured interview was carried out being a retrospective study based on electronic files and finally, our data may not apply to other cultural, or social context. Besides, strengths should also be mentioned. As far as we know, this study fills a gap providing a large longitudinal information from both the pre-COVID-19 period and the COVID-19 period, extending the observation period for almost two years of COVID-19 pandemic, the longest follow-up period published to date. Moreover, special emphasis on gender and age differences has been made, which could be a useful risk marker to be incorporated into suicide prevention programs.
Our data highlight the alarming increase in suicidality in children and adolescents and, support the negative emotional impact of the COVID-19 pandemic among the youngest widely reported (Nearchou et al., 2020; Singh et al., 2020; Binagwaho and Senga, 2021; de Figueiredo et al., 2021). Furthermore, they draw a progressive worsening in suicidal ideation and attempts from the initial phases as the pandemic progresses, emphasizing the special vulnerability of girls and those over 12 years old.
Youth mental health is of great concern since the children of today will be the adults of the future. Thus, this study aims to highlight the urgent need to mitigate the long-term deleterious consequences of the pandemic on children's and adolescents' mental health and to provide guidance for the development of skills to face the challenges of adulthood.
Authors contributions
Lorena García-Fernández and Roberto Rodriguez-Jimenez: Conceptualization, Methodology, Investigation, Project administration, Resources. Verónica Romero-Ferreiro: Methodology, Data curation, Formal Analysis. Lorena García-Fernández: Writing- Original draft preparation. Roberto Rodriguez-Jimenez: Supervision. Verónica Romero-Ferreiro, Marta Izquierdo, Victoria Rodríguez, Guillermo Lahera, Miguel A. Alvarez-Mon and José Luis Santos: Writing- Reviewing and Editing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
Dr. R. Rodriguez-Jimenez has been a consultant for, spoken in activities of, or received grants from: Instituto de Salud Carlos III, Fondo de Investigación Sanitaria (FIS), Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM), Madrid Regional Government (S2010/BMD-2422 AGES; S2017/BMD-3740), JanssenCilag, Lundbeck, Otsuka, Pfizer, Ferrer, Juste, Takeda, Exeltis, Casen-Recordati, Angelini. Dr. G. Lahera has been a consultant to or has received honoraria or grants from Janssen-Cilag, Otsuka-Lundbeck, Lilly, Astra-Zeneca, CIBERSAM and Instituto de Salud Carlos III. All other authors declare that they have no conflict of interest.
Acknowledgments
We thank the Hospital de San Juan's Documentation Department for their kindly contribution to this study.
References
- Barber S.J., Kim H. COVID-19 worries and behavior changes in older and younger men and women. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021;76(2):e17–e23. doi: 10.1093/geronb/gbaa068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binagwaho A., Senga J. Children and adolescent mental health in a time of COVID-19: a forgotten priority. Annals of global health. 2021;87(1):57. doi: 10.5334/aogh.3330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BOE Real Decreto 463/2020, de 14 de marzo, por el que se declara el estado de alarma para la gestión de la situación de crisis sanitaria ocasionada por el COVID-19. Boletín Oficial del Estado. 2020;67:25390–25400. [Google Scholar]
- Brasso C., Bellino S., Blua C., Bozzatello P., Rocca P. The impact of SARS-CoV-2 infection on youth mental health: a narrative review. Biomedicines. 2022;10(4):772. doi: 10.3390/biomedicines10040772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carison A., Babl F.E., O'Donnell S.M. Increased paediatric emergency mental health and suicidality presentations during COVID-19 stay at home restrictions. Emerg. Med. Australasia (EMA): Emerg. Med. Australasia (EMA) 2022;34(1):85–91. doi: 10.1111/1742-6723.13901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chadi N., Spinoso-Di Piano C., Osmanlliu E., Gravel J., Drouin O. vol. 69. 2021. Mental health-related emergency department visits in adolescents before and during the COVID-19 pandemic: a multicentric retrospective study; pp. 847–850. (The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine). 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cousien A., Acquaviva E., Kernéis S., Yazdanpanah Y., Delorme R. Temporal trends in suicide attempts among children in the decade before and during the COVID-19 pandemic in paris, France. JAMA Netw. Open. 2021;4(10) doi: 10.1001/jamanetworkopen.2021.28611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davico C., Marcotulli D., Lux C., Calderoni D., Cammisa L., Bondone C., Rosa-Brusin M., Secci I., Porro M., Campanile R., Bosia C., Di Santo F., Terrinoni A., Ricci F., Amianto F., Urbino A., Ferrara M., Vitiello B. Impact of the COVID-19 pandemic on child and adolescent psychiatric emergencies. J. Clin. Psychiatr. 2021;82(3) doi: 10.4088/JCP.20m13467. 20m13467. [DOI] [PubMed] [Google Scholar]
- Ferrando S.J., Klepacz L., Lynch S., Shahar S., Dornbush R., Smiley A., Miller I., Tavakkoli M., Regan J., Bartell A. Psychiatric emergencies during the height of the COVID-19 pandemic in the suburban New York City area. J. Psychiatr. Res. 2021;136:552–559. doi: 10.1016/j.jpsychires.2020.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Figueiredo C.S., Sandre P.C., Portugal L., Mázala-de-Oliveira T., da Silva Chagas L., Raony Í., Ferreira E.S., Giestal-de-Araujo E., Dos Santos A.A., Bomfim P.O. COVID-19 pandemic impact on children and adolescents' mental health: biological, environmental, and social factors. Progress in neuro-psychophar & biologi psychi. 2021;106 doi: 10.1016/j.pnpbp.2020.110171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Fernández L., Romero-Ferreiro V., López-Roldán P.D., Padilla S., Rodriguez-Jimenez R. Mental health in elderly Spanish people in times of COVID-19 outbreak. Am. J. Geriatr. Psychiatr.: offici. j. Am Asso. Geriatric Psychi. 2020;28(10):1040–1045. doi: 10.1016/j.jagp.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh R., Dubey M.J., Chatterjee S., Dubey S. Impact of COVID -19 on children: special focus on the psychosocial aspect. Minerva Pediatr. 2020;72(3):226–235. doi: 10.23736/S0026-4946.20.05887-9. [DOI] [PubMed] [Google Scholar]
- Gracia R., Pamias M., Mortier P., Alonso J., Pérez V., Palao D. Is the COVID-19 pandemic a risk factor for suicide attempts in adolescent girls? J. Affect. Disord. 2021;292:139–141. doi: 10.1016/j.jad.2021.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamdi E., Amin Y., Mattar T. Clinical correlates of intent in attempted suicide. Acta Psychiatr. Scand. 1991;83:406–411. doi: 10.1111/j.1600-0447.1991.tb05565.x. [DOI] [PubMed] [Google Scholar]
- Hertz M.F., Barrios L.C. Adolescent mental health, COVID-19, and the value of school-community partnerships. Injury prevention. j. Intern.Soc. Child.Adolescent Injury Preven. 2021;27(1):85–86. doi: 10.1136/injuryprev-2020-044050. [DOI] [PubMed] [Google Scholar]
- Isumi A., Doi S., Yamaoka Y., Takahashi K., Fujiwara T. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse Negl. 2020;110(Pt 2) doi: 10.1016/j.chiabu.2020.104680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joffe A.R. COVID-19: rethinking the lockdown groupthink. Frontiers in public healt. 2021;9 doi: 10.3389/fpubh.2021.625778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leff R.A., Setzer E., Cicero M.X., Auerbach M. Changes in pediatric emergency department visits for mental health during the COVID-19 pandemic: a cross-sectional study. Clin. Child Psychol. Psychiatr. 2021;26(1):33–38. doi: 10.1177/1359104520972453. [DOI] [PubMed] [Google Scholar]
- López-Bueno R., López-Sánchez G.F., Casajús J.A., Calatayud J., Tully M.A., Smith L. Potential health-related behaviors for pre-school and school-aged children during COVID-19 lockdown: a narrative review. Prev. Med. 2021;143 doi: 10.1016/j.ypmed.2020.106349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magson N.R., Freeman J., Rapee R.M., Richardson C.E., Oar E.L., Fardouly J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J. Youth Adolesc. 2021;50(1):44–57. doi: 10.1007/s10964-020-01332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques de Miranda D., da Silva Athanasio B., Sena Oliveira A.C., Simoes-E-Silva A.C. How is COVID-19 pandemic impacting mental health of children and adolescents? Int. J. Disaster Risk Reduc.: IJDRR. 2020;51 doi: 10.1016/j.ijdrr.2020.101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mourouvaye M., Bottemanne H., Bonny G., Fourcade L., Angoulvant F., Cohen J.F., Ouss L. Association between suicide behaviours in children and adolescents and the COVID-19 lockdown in Paris, France: a retrospective observational study. Arch. Dis. Child. 2021;106(9):918–919. doi: 10.1136/archdischild-2020-320628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayne S.L., Hannan C., Davis M., Young J.F., Kelly M.K., Powell M., Dalembert G., McPeak K.E., Jenssen B.P., Fiks A.G. COVID-19 and adolescent depression and suicide risk screening outcomes. Pediatrics. 2021;148(3) doi: 10.1542/peds.2021-051507. [DOI] [PubMed] [Google Scholar]
- Meherali S., Punjani N., Louie-Poon S., Abdul Rahim K., Das J.K., Salam R.A., Lassi Z.S. Mental health of children and adolescents amidst COVID-19 and past pandemics: a rapid systematic review. Int. J. Environ. Res. Publ. Health. 2021;18(7):3432. doi: 10.3390/ijerph18073432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nearchou F., Flinn C., Niland R., Subramaniam S.S., Hennessy E. Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: a systematic review. Int. J. Environ. Res. Publ. Health. 2020;17(22):8479. doi: 10.3390/ijerph17228479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Loughlin S., Sherwood J. A 20-year review of trends in deliberate self-harm in a British town, 1981-2000. Soc. Psychiatr. Psychiatr. Epidemiol. 2005:446–453. doi: 10.1007/s00127-005-0912-3. [DOI] [PubMed] [Google Scholar]
- Ravens-Sieberer U., Kaman A., Erhart M., Devine J., Schlack R., Otto C. European Child & Adolescent Psychiatry, 1–11. Advance Online Publication. 2021. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen K., Yang Y., Wang T., Zhao D., Jiang Y., Jin R., Zheng Y., Xu B., Xie Z., Lin L., Shang Y., Lu X., Shu S., Bai Y., Deng J., Lu M., Ye L., Wang X., Wang Y., gao L. Children: Experts' Consensus Statement. World Journal of Pediatrics : WJP. Global Pediatric Pulmonology Alliance. 2020. Diagnosis, treatment, and prevention of 2019 novel coronavirus infection; pp. 1–9. (PubMed) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S., Roy D., Sinha K., Parveen S., Sharma G., Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatr. Res. 2020;293 doi: 10.1016/j.psychres.2020.113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokoloff W.C., Krief W.I., Giusto K.A., Mohaimin T., Murphy-Hockett C., Rocker J., Williamson K.A. Pediatric emergency department utilization during the COVID-19 pandemic in New York City. Am. J. Emerg. Med. 2021;45:100–104. doi: 10.1016/j.ajem.2021.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamarit A., de la Barrera U., Mónaco E., Schoeps K., Montoya-Castilla I. Psychological impact of COVID-19 pandemic in Spanish adolescents: risk and protective factors of emotional symptoms. Revista de Psicologia Clínica Con Niños y Adolescentes. 2020;7(3):73–80. doi: 10.21134/rpcna.2020.mon.2037. [DOI] [Google Scholar]
- Tanaka T., Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Human Behav. 2021;5(2):229–238. doi: 10.1038/s41562-020-01042-z. [DOI] [PubMed] [Google Scholar]
- Viner R.M., Russell S.J., Croker H., Packer J., Ward J., Stansfield C., Mytton O., Bonell C., Booy R. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. The Lancet. Child & adolescent health. 2020;4(5):397–404. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yard E., Radhakrishnan L., Ballesteros M.F., Sheppard M., Gates A., Stein Z., Hartnett K., Kite-Powell A., Rodgers L., Adjemian J., Ehlman D.C., Holland K., Idaikkadar N., Ivey-Stephenson A., Martinez P., Law R., Stone D.M. Emergency department visits for suspected suicide attempts among persons aged 12-25 Years before and during the COVID-19 pandemic - United States, january 2019-may 2021. MMWR. Morbidity and mortality weekly report. 2021;70(24):888–894. doi: 10.15585/mmwr.mm7024e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuodelis-Flores C., Ries R.K. Addiction and suicide: a review. Am. J. Addict. 2015;24(2):98–104. doi: 10.1111/ajad.12185. [DOI] [PubMed] [Google Scholar]
- Zhu S., Zhuang Y., Lee P., Wong P. The changes of suicidal ideation status among young people in Hong Kong during COVID-19: a longitudinal survey. J. Affect. Disord. 2021;294:151–158. doi: 10.1016/j.jad.2021.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]