Abstract
Present study aimed to develop a questionnaire related to the self-efficacy for the rehabilitation of children using Cochlear Implantation (CI) and to administer the questionnaire on parents of children with cochlear implantation. 100 parents of children with Cochlear Implantation between the years 2010- 2020 were selected randomly to be participants for the present study.A questionnaire on Self- Efficacy was developed. Questionnaire consists of 17 questions related to self-efficacy of therapy and Goal related Strategies, Listening, language and Speech Development and also Parental Involvement in rehabilitation, family and emotional support, device maintenance and follow up, At school engagement. Responses were recorded on three-point rating scale as (2= Yes, 1=sometimes,No=1). In addition, there were 3 open ended questions. This questionnaire was administered on 100 parents of children with CI. Total scores under each domain were calculated. Responses of open-ended question were listed. It was found that majority (more than 90%) of parents were aware of the therapy goals given to their children and also able to join the therapy session. Most (more than 90%)of the parents reported an improvement in the child’s auditory skills post rehabilitation. 80% of parents were able to bring their children for therapy consistently, other parents felt the distance and financial affordability was a main barrier to bring the child consistently for therapy. 27 parents have reported a regression in the child due to the Covid lockdown. Though most of the parents reported to be satisfied with their child’s progress post rehabilitation, other concerns such as inability to spend adequate time and inability for the children to learn via tele-mode were highlighted. These concerns should be carefully considered while providing rehabilitation for the child with CI.
Keywords: Self-efficacy, Strategies, Device maintenance
Introduction
The primary benefit of cochlear implant in children is to promote acquisition of hearing, which promotes the development of spoken language. Parents must be supportive of their children developing spoken language with cochlear implants as they begin to interpret speech. Moeller [1] reported that children of parents actively involved in their child’s early intervention program communicate better with their child with hearing loss. These parents contribute more to their child’s progress than parents who do not participate in such programs.
The support of parents and family members is the main component in the rehabilitation of children with CI.A study by Jardin [2] reported that Family involvement and maternal self-efficacy was found to have had a positive influence on language development of children with hearing impairment. Improvement in other outcomes such as in academic performance and overall communication skills were also reported. Thus, parental self-efficacy assists in influencing the children with hearing impairment to develop their communication skills post CI.
According to DesJardin, Eisenberg and Hodapp [3] as family-centred practice and parental empowerment has become the standard model of intervention.Parental self-efficacy is an important goal in terms of improving the listening and language development of the child with CI. Therefore, the successful habilitation of a child with CI depends on the amount of parental self-efficacy and parental involvement.
The Scale of Parental Involvement and Maternal Self-Efficacy (SPISE) was designed for Parental Self – Efficacy for the rehabilitation of children with hearing loss by Jardin [2] Based on the findings of this questionnaire, it was found that the mothers’ perceived involvement and self-efficacy had a positive impact on in developing their child’s speech and language skills. There were significant positive relationships emerged between the mothers’ perceived competence and involvement in developing their children’s language skills. Robbins and Kirk [4] have developed closed format questionnaires to investigate perceptions of parental outcomes for their child post CI. However, it was found that close set questionnaires can limit the responses obtained from the parents, and hence they may affect the measured outcomes of the study.
The previous study Robbins and Kirk [4] assessed the self-efficacy and parental involvement using questionnaires, however these studies had some limitations. Jardin [2] failed to assess the financial ability for post implant care and maintenance aspects of the devices, the performance of the children in school post CI and managing the technical aspects of maintaining the cochlear implant at home. These studies did not explain about school atmosphere. Robbins and Kirk [4] have used only close-set questionnaires which can limit the responses of the parents. These closed- set questionnaires may influence or affect the measured outcomes in the study. Thus, a questionnaire with open-ended questions should be constructed to receive unrestrained responses from the parents and also receive their insights and improve the outcomes of the study. Most of studies have found that parent of children has financial difficulty with respect to device maintenance, travel for therapy [5–8]. Due to these reasons, the success rate from intervention mainly depends on the economic status of the parent to provide continuous support for rehabilitation and maintenance of the device.
Above listed studies have assessed only some domains of parental perception of children with CI. Studying multiple domains of self-efficacy, parental involvement at home, rehabilitation centre might benefit the CI team in terms of counselling and prediction of outcomes. Thus, this parental study develop questionnaire would study self-efficacy in various domains for the rehabilitation of children with CI. Further, this questionnaire will be administered in parents of children with CI.
Method
Ethical Consideration
The current study was approved by the ethics committee of SriRamachandra Institute of Higher Education and Research (DU), Chennai (reference No CSP/21/MAR/92/307). Parental consent form was taken prior to the study.
Participants
A total of 100 parents ( 88 mothers, 12 father) of children were selected randomly for the study.Parents of 100 Children who were implanted between the year 2010 to 2020 at Sri Ramachandra Hospital were included. All children were implanted with any one of the Food and Drug Administration (FDA) approved CI companies of Advanced Bionics, Cochlear Nucleus and MED-EL. Verbal/Oral consent was obtained from all participants via tele-mode. Table 1 provides details of the participants:
Table 1.
Details of participants in the present study
| Education level | Number of parents |
|---|---|
| College Education | 16 |
| High School | 37 |
| Middle School | 35 |
| Primary School | 3 |
| No Education | 9 |
| Income | Number of parents |
| > Rs. 1,20,000 | 44 |
| = Between Rs. 60,000 – Rs. 1,20,000 | 32 |
| < Rs. 60,000 | 24 |
| Employment status | Number of Parents |
| Farmer/ Labourer | 53 |
| Office | 16 |
| Non- working parents | 31 |
Procedure
The procedure was carried out in two steps. Step 1 included development of questionnaire towards the rehabilitation of children using cochlear implant. Step 2 involved administration of the developed questionnaire to parents of children using CI through telephone interview.
Step 1: Development of Questionnaire
The questionnaire used in the study were composed of sub -domains in Parental Self-Efficacy (i) Therapy and Goal related Strategies (ii) Listening, Language and Speech Development (iii) Management of teaching at home during COVID-19 pandemic.
Questionnaire was developed in English. There were total of 17questions, in which 14 questions were closed-ended questions and 3 questions were open-ended questions. These questions were formed based on the Scale of Parental Involvement and Self- Efficacy (SPISE) developed by DesJardin [9]. However, these questions were modified based on the issues and needs specific for Indian population. Some of the questions were added based on the feedback from rehabilitation professionals,audiologists working in the field of CI and parents of children using Cochlear Implantation. Self-efficacy domain included seven questions focused on therapy goals and strategies and eight questions related to Listening, Language and Speech Development. Questions focused on therapy goals and strategies gathered information regarding the amount of time spent in parents spent with their children for auditory training, awareness and follow up of therapy goals at home, use of appropriate training material for teaching and need for assistance for training the child. Information regarding child’s listening skills in word and sentence level was obtained from Listening, Language and Speech Development domain. Additional questions such as training the child at home during the COVID-19 pandemic were also included in the data collection form.
Responses obtained using data collection form were filled in for close- ended questions. A 3-likert rating scale was used for close ended questions (Yes – 2 points, sometimes – 1 point, No − 0 points). Observed responses on open set questions were listed. Content validation of the data collection form was done by two audiologists and two special educator working with children using CI. Both Audiologist and special educator had an experience in the field of CI for a minimum of 5 to 15 years. The aim of the study and the method of answering to the questions were explained prior to content validation. The suggestions provided by the audiologists were incorporated. Later, in order to check the readability of statements and appropriateness of responses to questions, the data collection form was tested on 6 parents of children using CI. None of the parents reported any remarks with respect to understand ability and content of questionnaire. Thus, the same questions were used for further data collection. However, the pilot study aided the instigator to rephrase a few questions. Table 2 provides questions used to assess self- efficacy.
Table 2.
Questionnaire used to assess self-efficacy
| S.No. | Questions | |||
|---|---|---|---|---|
| I) Therapy Goals and Strategies Related | Yes (2) |
Some times (1) |
No (0) |
|
| 1. | Describe the amount of time spent for auditory training with your child. | |||
| 2. | I am aware of the therapy goals given for my child | |||
| 3. | I am able to follow up the goals given by the therapist at home. | |||
| 4. | I am aware of different strategies to make my child listen better. | |||
| 5. | I am able to use appropriate training material for teaching. | |||
| 6. | I am able to be firm when my child shows temper tantrums or inappropriate behaviour. | |||
| 7. | I motivate my child to express verbally. | |||
| 8. | I require more assistance for training my child. | |||
| 9 | How long is your child’s screen time? What strategies do you use to reduce screen time for your child? | |||
| II) Listening, Language and Speech Development |
Yes (2) |
Sometimes (1) |
No (0) |
|
| 1. | I feel I can help improve my child’s listening development in word level. | |||
| 2. | I feel that I can improve my child’s listening development in sentence level. | |||
| 3. | I feel that I can improve my child’s listening development while reading story books/ reading materials. | |||
| 4. | I feel I can help my child perform language activities at home | |||
| 5. | I feel that I can help my child speak at word level and progressive to sentence level. | |||
| 6 | I feel that I can help my child develop language age appropriately with training. | |||
| 7 | I feel I can improve my child’s language and listening development in day-to-day life. | |||
| 8 | I feel confident to admit my child in a regular school | |||
| 9 | How did you manage your child’s teaching during COVID time? | |||
Step 2: Administration of Questionnaire
Questionnaire was administered through telephone interview. In-person interview could not be done due to the COVID- 19 pandemic during the data collection process. The questionnaire was administered via telephone interview. Telephone interview was scheduled at a mutually convenient time for all the participants in the study. The duration to administer the questionnaire was an average of about 15 to 20 min on an average via phone. The investigator rephrased the questions when the parents were unable to understand it. Parental responses were audio recorded and later the examiner filled the responses in google form for both open and close-set questions. Further, some of these details were crosschecked with hospital records maintained by the clinical coordinator of the paediatric cochlear implant program at Sri Ramachandra Medical Hospital.
Scoring and Analysis
Responses obtained using questionnaire were filled in for both open and close ended questions in google sheet. The close-set responses were rated on a 3-point Likert scale (Yes, Sometimes and No). The responses were coded as, 2 being ‘Yes’ 1 being ‘Sometimes’ and 0 being ‘No’. Open set questions were written verbatim on form based on the response from the parents. These responses for close set data were tabulated on the excel sheet. Total points in each domain of the questionnaire were added. They were converted into percentile score. The results data for all the questions in each domain were represented in the form of tables and graphs.
Results and Discussion
Therapy Goals and Strategies Related
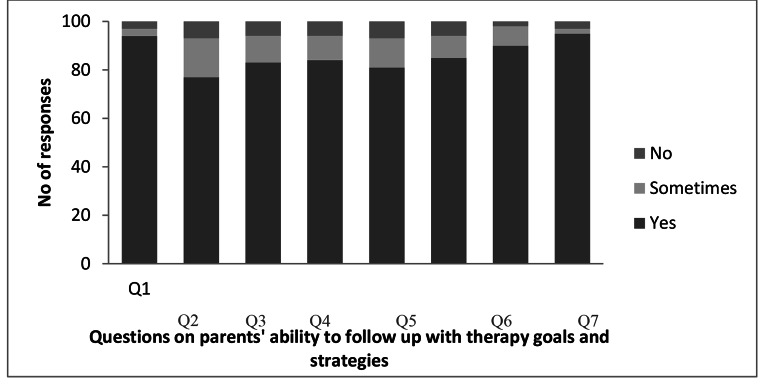
Out of 100 parents, more than 90% parents were aware of the therapy goals given and also were able to follow up the goals given by therapist to improve their speech, language and listening at home (Fig 1). In addition, they were able to use separate training materials for the child (Q1 to Q4), However, only 57% of parents were aware of different strategies to make their child listen better (Q3). Only, 32% of parents reported that they were not able to handle their children’s temper tantrums (Q5).
Fig. 1.
No. of respondents on parents’ ability to follow up with therapy goals and strategies (n = 100)
Similar to the present study, Geers [10] also reported that the parents were unable to handle the child’s temper tantrums and their refusal to cooperate with them. Thus, most of these parents required assistance from the therapist in training their children’s behavioural issues. Need of assistance with respect to therapy goals and strategies by parents were also reported by study by Eyalati and Jafari [11].
Responses were also obtained for open- ended questions regarding the time spend on improving listening and speech and language development for the present study. Only 38% of parents reported that they were able to spend more than 4 h for improving their listening and language development with their children. The remaining 61% of parents reported that they could not spend time with their child due to the following reasons: (1) The inability to balance work and time with the child, (2) The child did not cooperate with the parent during auditory training at home. (3) Regression in speech and language development in the child due to device issues in the CI device. Geers’s [10] also found that parents gradually reduced the duration to weekly for the third-year post- implantation.
Listening, Language and Speech Development
Majority of the parents reported an improvement in the child’s listening, language and speech development post CI rehabilitation on listening, language and speech development domain. Figure 2 provides the listening, language and speech development of children with CI. majority of the parents (> 90%) were confident that they could help improve their child’s listening development in word level (Q1), whereas as only 77% of parents were confident about improving their child’s listening development in sentence level (Q2). 83% of parents felt that with the help of reading materials, they could definitely develop their child’s listening development better at home (Q3). This is in accordance with Kluwin and Stewart’s [12] study reported that, parents found improvement in the child’s language and speech over the time after training at home. In the present study, 84% of parents also felt that they could make their children perform language activities at home. Less than 10% of parents felt that they teach the child based on what the child likes and also felt that their children would cooperate better with a therapist (Q4). 6 parents found it difficult to train their children as they did not have the financial support to buy training materials.
Fig. 2.
No. of respondents on listening, language and speech development of children with CI (n = 100)
A few parents (< 10%) reported to be unmotivated to train their children especially during the COVID-19 pandemic due to emotional trauma at home such as family disputes and losing loved ones due to COVID. Also, the present study found that 85% of parents felt that they could help their children develop language age appropriately (Q6) and 90% of parents felt they could improve their children’s language and listening development in day-to-day life (Q7). Rout and Khanna [13] also have observed that the attitude of the parents influences children with hearing impairment and their performance. Therefore, the authors suggested that parents must have a positive attitude related to coping with the diagnosis and training to improve the progress of the child. Des Jardin, Eisenberg and Laurie [14] also reported that the use of facilitative techniques such as open-ended questions help in improving the literacy development in children with cochlear implants. Therefore, auditory training done by parents at home plays an important role in the development of speech, language and literacy in children with hearing impairment. Thus, the present study also finds that 95% of parents reported that they were confident to admit their children in regular schools as they were confident in developing child’s literacy ability at home (Q8).
Management of Teaching at Home During COVID-19 Pandemic
Table 2 provides the information about the management of teaching during the COVID-19 lockdown. In the present study, 27 parents have reported a regression in the child due to the Covid lockdown. These parents were unable to teach the child as they felt the child benefitted better from a teacher (or) therapist. These parents had a few concerns that the children were restless at home, refused to cooperate with the parents while teaching or the child would go back to sign language. This information would imply that parents’ self-efficacy has to be improved.
From Table 3, parents have reported 4 ways in which they have managed the teaching for the child: Majority of the parents (47 parents) have been helping the child with homework and teaching using school books. 11 parents have reported that their children attend online classes via WhatsApp video call or Google meet, they feel that the online classes keep the children in touch with their schoolwork. Though the parents felt that the online classes are helpful, they also felt that the children found it difficult to learn via online mode. Ayas, Ali Al Amadi, Khaled and Alwaa [15] also reported that 96% of the parents agreed that the home training methods were challenging and 71% of the parents expressed that remote learning lessons were difficult for their children.
Table 3.
Management of child’s teaching during COVID-19 pandemic. (n = 100)
| Help with revision/Homework | 47 |
|---|---|
| Small group Tuition | 6 |
| Online Classes | 11 |
| Self- teaching | 9 |
| Difficult to manage teaching | 27 |
The amounts of screen time of the children per day were also analysed. 32% of children are exposed to more than 2 h of screen time per day other than online classes whereas 68% of children had less than 2 h of screen time. All parents have reported that they were aware that too much screen time is detrimental to the speech and language development of the child.Thus, the results from the current study implements the need of better tele-services in aural rehabilitation for children with cochlear implantation. Parents also need to attend training programs to facilitate better listening and speech development for their children at home.
Conclusion
Majority of parents (> 90%) of parents were aware of the goals given by the therapist and were able to follow them at home. Another concern aspect found in the present study was that 98% parents felt that travelling to the rehabilitation centre was a hindrance. The parents found it stressful to organize the necessary arrangements for the rest of the family, while they had to bring the child to the centre.
The present study noted that 27% parents have reported a regression in the child due to the lockdown. Based on finding of the present study, conducting parent empowerment programs and therapy in tele-mode is a step which should be taken to increase more awareness in parents during COVID-19 pandemic. Developed questionnaire also can be used to study the parental efficacy for the rehabilitation of children using CI.This information would help the professionals in counseling the parents regarding the same while attending therapy.
Acknowledgements
The authors would like to thank Ms. Selvi, the coordinator for cochlear Implantation program of Sri Ramachandra Institute of Higher Education and Research, who helped us to recruit the patient for the study.
Author Contribution
Corresponding authors contributed in terms of conception of the study, design, supervision, analysis, interpretation, critical review.
First Authors contributed in terms of material development, data collection, Literature review writing.
Funding
No funding received for this project.
Declarations
Ethics Approval
The current study was approved by the ethics committee of SriRamachandra Institute of Higher Education and Research (DU), Chennai. (CSP/21/MAR/92/307).
Financial Interest
The authors have no relevant financial or non-financial interest to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Srinidhi Balakrishnan, Email: sribee1996@gmail.com.
Muthuselvi Thangaraj, Email: muthuselvi.t@sriramachandra.edu.in.
References
- 1.Moeller MP. Early intervention and language development in children who are deaf and hard of hearing. Pediatrics. 2000;106:1–9. doi: 10.1542/peds.106.3.e43. [DOI] [PubMed] [Google Scholar]
- 2.Des Jardin JL. Maternal perceptions of self-efficacy and involvement in the auditory development of young children with prelingual deafness. J Early Intervention. 2005;27(3):193–209. doi: 10.1177/105381510502700306. [DOI] [Google Scholar]
- 3.DesJardin JL, Eisenberg LS, Hodapp RM. Sound beginnings: supporting families of young deaf children with cochlear implants. Infants and Young Children. 2006;19(3):179–189. doi: 10.1097/00001163-200607000-00003. [DOI] [Google Scholar]
- 4.Robbins AM, Kirk K. Speech perception assessment and performance in pediatric cochlear implant users. Semin Hear. 1996;17(4):353–369. doi: 10.1055/s-0028-1083065. [DOI] [Google Scholar]
- 5.Vaid N, Deshpande S, Salve K, Nikam R, Vaid S. Fuel for the processor: our experience. J Indian Speech Lang Hear Association. 2015;29(1):1–7. doi: 10.4103/0974-2131.173858. [DOI] [Google Scholar]
- 6.Deepthy J, Muthuselvi T (2018) Profiling of the Average Expense Incurred by Parents of Children with Cochlear Implant [Master’s thesis]. Sri Ramachandra Institute of Higher Education and Research
- 7.Ranjith. RR, Kameswaran R (2014) M. Status Report on Comprehensive Cochlear Implant Scheme - A MERF Study [Poster session]. 12th Annual Conference of Cochlear Implant Group of India - CIGICON 2014, New Delhi
- 8.Shankar S, Prathiba DG (2020) Benefits of Cochlear Implants in children with hearing impairment: parental perspectives from Tertiary Care Hospitals in Tamil Nadu.Indian Journal of Public Health Research & Development, 11(6). [CrossRef]
- 9.DesJardin JL. Assessing parental perceptions of self-efficacy and involvement in families of young children with hearing loss. Volta Rev. 2003;103:391–409. [Google Scholar]
- 10.Geers AE (2002) of Speech, Language, and Literacy in Children with Early Cochlear Implantation. Language, Speech, and Hearing Services in Schools, 33(July), 172–184 [DOI] [PubMed]
- 11.Eyalati N, Jafari Z, Ashayeri H, Salehi M, Kamali M. Effects of parental education level and economic status on the needs of families of hearing-impaired children in the aural rehabilitation program. Iran J Otorhinolaryngol. 2013;25(70):419. [PMC free article] [PubMed] [Google Scholar]
- 12.Kluwin TN, Stewart DA. Cochlear implants for younger children: a preliminary description of the parental decision process and outcomes. Am Ann Deaf. 2000;145(1):26–32. doi: 10.1353/aad.2012.0247. [DOI] [PubMed] [Google Scholar]
- 13.Rout N, Khanna M (2012) Concerns of Indian Mothers with Children Having Severe-to-Profound Hearing Impairment at Diagnosis and after 1–3 Years of Therapy. Rehabilitation Research and Practice, 2012, 1–7. [CrossRef] [DOI] [PMC free article] [PubMed]
- 14.Desjardin J, Eisenberg L (2007) Maternal Contributions: Supporting Language Development in Young Children with Cochlear Implants. Ear and hearing. 28. 456 – 69.[CrossRef] [DOI] [PubMed]
- 15.Ayas M, Amadi AA, Khaled A, D., &, Alwaa AM (2020) Impact of COVID-19 on the access to hearing health care services for children with cochlear implants: a survey of parents. F1000Research:690 [CrossRef] [DOI] [PMC free article] [PubMed]