Abstract
Bilharzia or schistosomiasis is a parasitic disease due to infestation by a hematophagous trematode of the genus Schistosoma. It is the second most frequent parasitic endemic in the world after malaria. The most frequent tissue infections are intestinal and genitourinary. Testicular localizations of schistosoma are very rare. When lesions become chronic, they present as non-specific masses, bilharziomas, posing enormous problems of differential diagnosis with other benign and malignant pathologies, which impacts management. We report a case of epididymal schistosomiasis in a 37 years old patient simulating a malignant tumor. This case allowed us to review the diagnostic difficulties of this rare localization and the challenges of management.
Keywords: Schistosomiasis, Testis, Pseudotumor, Pathological anatomy
Introduction
Schistosomiasis or bilharzia is one of the neglected tropical diseases. It is caused by a hematophagous trematode of the genus Schistosoma, first described by Theodor Bilharz in 1851. The evolutionary cycle of the parasite was established in 1915 by Leiper who specified that the intermediate host was a freshwater snail [1], [2], [3]. The definitive host, i.e. the human, is infested transcutaneously by swimming or wading in contaminated fresh water. The parasites are mainly located in the vessels of the digestive tract or the genitourinary system [4], [5], [6], [7], [8], [9]. Schistosoma has a known carcinogenic effect in the bladder and has been implicated in other types of cancer such as cervical cancer. In addition, Schistosoma infection increases the risk of contracting other types of urogenital tract infections such as HIV and human papillomavirus [1], [2], [3]. Testicular involvement by Schistosoma is very rare and is caused by Schistosoma mansoni and Schistosoma haematobium [6]. Immunopathological reactions against schistosome eggs trapped in tissues lead to inflammatory and fibrosis phenomena resulting in pseudotumor masses called bilharzias [10], [11], [12], [13], [14], [15]. Bilharzias are often the site of numerous malignant-like changes, thus posing problems of differential diagnosis [15]. We report here a case of epididymal schistosomiasis simulating a testicular tumor in a 37-year-old man. Through this case, we will review the specificities of this rare localization with emphasis on the challenges of management.
Case report
This was a 37-year-old patient with a history of chronic and intermittent testicular pain. He was seen for an exacerbation of testicular pain that had become permanent over the last few days. Clinical examination showed a firm indurated testicular swelling massing on the epididymal cuff. The biological assessment showed a slight hyperleukocytosis at 11000/mm3 with a slight hypereosinophilia at 1100/mm3. Ultrasound revealed an irregularly contoured epididymal mass measuring 63×47 mm. The mass was hyperechoic in the periphery and hypoechoic in the center making a malignant tumor suspicious. The patient underwent a total orchidectomy. The postoperative course was simple without complications. The surgical specimen was received for anatomopathological examination. Macroscopically it was a deformed testis of 8 × 6.5×5 cm. On section, a cystic lesion of 5.5 cm was observed in the epididymis. The cystic lesion was bounded on the periphery by a thick indurated fibrous shell with areas of calcification. The cystic lumen was occupied by blackish gelatinous pasty debris. The adjacent testicular parenchyma was macroscopically normal without lesion (Fig. 1).
Fig. 1.
macroscopic section of the testis showing an epididymal cystic lesion of 5.5 cm in its largest axis with brownish pasty content surrounded by a fibrous shell. The adjacent testicular parenchyma is macroscopically normal without lesion.
Microscopically, the cystic wall was fibrous, and was the site of a granulomatous inflammatory reaction with a few eosinophilic polynuclei around a calcified terminal spur of bilharzia eggs. The epididymal ducts opposite were of normal histostructure (Fig. 2, Fig. 3).
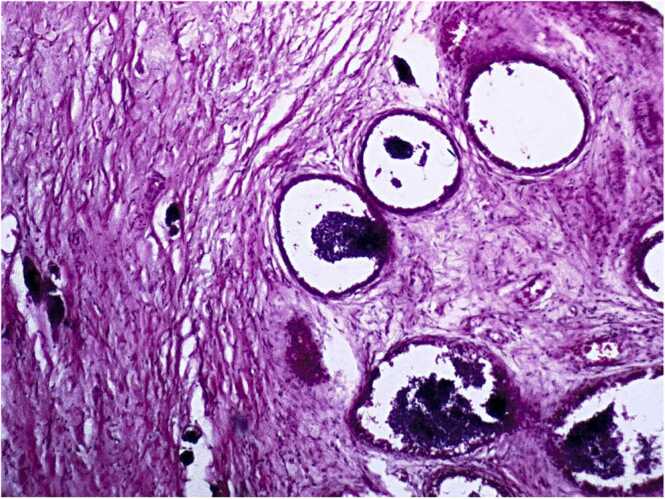
Fig. 2.
microscopy HE staining G100 showing on the left calcified bilharzia eggs in a fibrous tissue. On the right, epididymal ducts are seen opposite calcified bilharzia eggs.
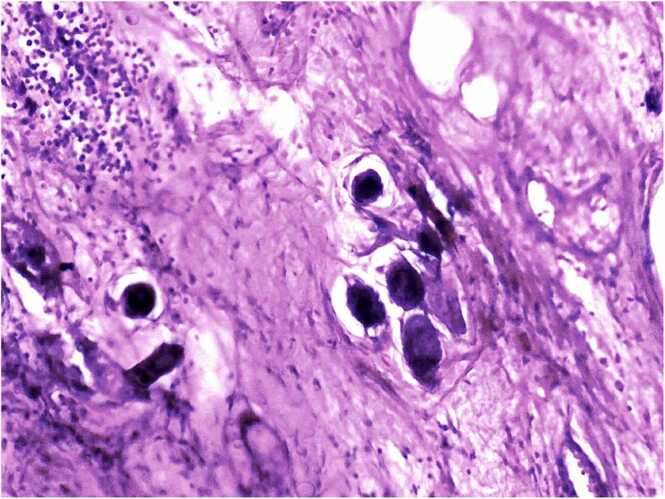
Fig. 3.
microscopy HE staining G200 showing a fibrous cystic wall, seat of a granulomatous inflammatory reaction around calcified bilharzia eggs terminal spur.
Discussion
Bilharzia is the second most common parasitic endemic after malaria. It mainly affects poor populations living in endemic areas with hygiene and sanitation problems. The organs usually most affected by schistosomiasis are the bladder and the colon [1], [2], [3], [4], [5], [6]. Rarer locations have been described in the literature, including the appendix, prostate, ovaries, fallopian tubes and cervix [6], [9], [10], [11]. Localizations in the testicles and testicular adnexa are very rare or even exceptional. The pathogenesis of testicular localizations is thought to be related to anastomoses between the gonadal veins and the mesenteric veins in the case of Schistosoma mansoni and between the gonadal veins and the vesical plexus in the case of Schistosoma haematobium.
The contact of bilharzia eggs with tissues causes a granulomatous inflammatory reaction which evolves towards a pseudo-tumoral reactional fibrosis resulting in Bilharziomas with time. Clinically, these pseudo-tumoral lesions do not present any specificity allowing to evoke the diagnosis of tissue bilharziasis. They are indurated masses with often irregular contours, painful or not, which may suggest tuberculous orchitis or testicular neoplasia [9], [10], [11], [12], [13], [14], [15].
On ultrasound, testicular bilharzia typically presents a nodular hypoechoic lesion in the center surrounded by hyperechoic tissue in the periphery [16]. The sonographic characteristics of these lesions are very similar to those of testicular malignancies. Indeed, on ultrasound, any hypoechoic nodule should be considered malignant, until proven otherwise, as this is the most common sign of testicular cancer [6]. Magnetic resonance imaging (MRI) is more sensitive than ultrasound. It allows the suspicion of a granulomatous process without being able to specify the etiology. However, MRI does not allow a formal differential diagnosis between a benign lesion and a malignant tumor in certain cases. New radiological protocols are being evaluated for a better characterization of testicular lesions in order to better distinguish benign lesions from malignant tumors [15], [16].
Biology allows serology to look for serum antibodies to schistosoma. Serology allows to prove that the patient has already been in contact with schistosoma. It does not allow to specify the species involved and especially does not allow to judge the evolutionary, chronic or resolved character of the disease. Recently, the diagnosis of active infection by Schistosoma haematobium has been improved by the detection of specific DNA fragments in filtered urine samples [17], [18]. In our case, biology would not have been of much use in characterizing the testicular lesions of our patient.
In our case, pathological anatomy was used to make the diagnosis with standard histology by demonstrating the bilharzian granuloma on an excessive orchidectomy specimen. Some authors think that the extemporaneous examination is the best indicated examination. It allows in the same operation time, on the one hand to specify the benign or malignant character of the lesions, and on the other hand to be able to apply the adapted operation protocol for each case on the basis of formal scientific evidence [10]. In the case of a benign lesion, conservative treatment can be proposed. In our case a total or partial epididymectomy could have been proposed. This operation would certainly not have made it possible to preserve the natural reproductive function of the testicle but would at least have made it possible to preserve the endocrine function. Our patient, in addition to the surgical treatment, benefited from a medical treatment based on praziquantel.
Conclusion
Schistosomiasis is a very common parasitosis in many parts of the world. However, testicular localization of schistosomiasis is very rare. The clinical, biological or radiological signs are not very specific. This poses enormous problems of differential diagnosis with other benign and malignant pathologies complicating the therapeutic management. It is therefore necessary to discuss the management of a testicular mass in a parasitic endemic area during multidisciplinary meetings. This will allow a personalized management for each case while avoiding standardized management which often leads to an unnecessary orchiectomy.
Author agreement
The authors agree to the eventual publication of the article if it is accepted.
Author statement
The authors declare that they have read the reviewers' remarks and have taken them into account.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Santos L.L., Santos J., Gouveia M.J., Bernardo C., Lopes C., Rinaldi G., et al. Urogenital Schistosomiasis-history, pathogenesis, and bladder cancer. J Clin Med. 2021;10(2):205. doi: 10.3390/jcm10020205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bustinduy A.L., Randriansolo B., Sturt A.S., Kayuni S.A., Leustcher P.D.C., Webster B.L., et al. An update on female and male genital schistosomiasis and a call to integrate efforts to escalate diagnosis, treatment and awareness in endemic and non-endemic settings: The time is now. Adv Parasitol. 2022;115:1–44. doi: 10.1016/bs.apar.2021.12.003. [DOI] [PubMed] [Google Scholar]
- 3.Kayuni S.A., Alharbi M.H., Makaula P., Lampiao F., Juziwelo L., LaCourse E.J., et al. Male genital Schistosomiasis along the Shoreline of Lake Malawi: baseline prevalence and associated knowledge, attitudes and practices among local fishermen in Mangochi District, Malawi. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.590695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Colley D.G., Bustinduy A.L., Secor W.E., King C.H. Human schistosomiasis. Lancet. 2014;383(9936):2253–2264. doi: 10.1016/S0140-6736(13)61949-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lo N.C., Bezerra F.S.M., Colley D.G., et al. Review of 2022 WHO guidelines on the control and elimination of schistosomiasis. Lancet Infect Dis. 2022;22(11):e327–e335. doi: 10.1016/S1473-3099(22)00221-3. [DOI] [PubMed] [Google Scholar]
- 6.Collège des universitaires de maladies infectieuses et tropicales, Pulcini C, Rapp C. E. Pilly 2016. Maladies infectieuses et tropicales. Paris: Alinéa Plus; 2016.
- 7.Organisation mondiale de la santé. Schistosomiase (bilharziose). Aide-mémoire N°115 [En ligne]. Geneva: WHO; 2016. 〈http://www.who.int/mediacentre/factsheets/fs115/fr/〉.
- 8.Centers for Disease Control and Prevention. Parasites. Schistosomiasis [En ligne]. Atlanta: CDC; 2012. 〈https://www.cdc.gov/parasites/schistosomiasis/〉.
- 9.Boissier J., Grech-Angelini S., Webster B.L., Allienne J.F., Huyse T., Mas-Coma S., et al. Outbreak of urogenital schistosomiasis in Corsica (France): an epidemiological case study. Lancet Infect Dis. 2016;16(8):971–979. doi: 10.1016/S1473-3099(16)00175-4. [DOI] [PubMed] [Google Scholar]
- 10.Ekenze S.O., Modekwe V.O., Nzegwu M.A., Ekpemo S.C., Ezomike U.O. Testicular Schistosomiasis mimicking malignancy in a child: a case report. J Trop Pedia. 2015;61(4):304–309. doi: 10.1093/tropej/fmv041. [DOI] [PubMed] [Google Scholar]
- 11.Periyasamy P., Subramaniam S.R., Rajalingham S. An increasingly notorious mimicker of testicular tumours; crossing borders. BMJ Case Rep. 2011;2011:bcr0920114816. Published 2011 Oct 11. doi: 10.1136/bcr.09.2011.4816. [DOI] [PMC free article] [PubMed]
- 12.Sinha V., Shankar M., Sardana N., Aggarwal R. A rare case of epididymal cyst due to Schistosomiasis. Cureus. 2019;11(9) doi: 10.7759/cureus.5755. Published 2019 Sep 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ze Ondo C., Sarr A., Sow Y., et al. Bilharziome testiculaire à Schistosomia haematobium: à propos de deux observations [Testicular bilharzioma by Schistosomia haematobium: about two cases] Prog Urol. 2014;24(1):67–69. doi: 10.1016/j.purol.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 14.Alves L.S., Assis B.P., Rezende M.M. Schistosomal epididymitis. Int Braz J Urol. 2004;30(5):413–415. doi: 10.1590/s1677-55382004000500012. [DOI] [PubMed] [Google Scholar]
- 15.Ferreira T.N., Higa H.C., Rondina R.G., Miranda M.M., Kaddoun M.L., Santos M.C., et al. Testicular schistosomiasis as differential diagnosis for testicular nodules: a case report. Rev da Soc Bras De Med Trop. 2015;48(4):501–503. doi: 10.1590/0037-8682-0229-2014. [DOI] [PubMed] [Google Scholar]
- 16.Salah M.A., Böszörményi-Nagy G., Al Absi M., Nagi M.A., Alsaaidi A.A. Ultrasonographic urinary tract abnormalities in Schistosoma haematobium infection. Int Urol Nephrol. 1999;31(2):163–172. doi: 10.1023/a:1007168507070. [DOI] [PubMed] [Google Scholar]
- 17.Haute Autorité de Santé. Actualisation des actes de biologie médicale relatifs au diagnostic de la bilharziose (schistosomoses). Feuille de route. Saint-Denis La Plaine: HAS; 2016.
- 18.Société française de microbiologie, Société française de mycologie médicale, Société française de parasitologie. Rémic 5.2. Référentiel en microbiologie médicale. Paris: SFM; 2015.