Abstract
Introduction
Displaced distal radius fractures often require manipulation under anaesthesia. Many anaesthetic techniques are described, with the two most commonly used being Bier’s block (BB) and haematoma block (HB). Despite national guidance preferring a BB, an HB is often performed instead. This study aims to compare the analgesic properties of a BB with those of an HB when manipulating distal radius fractures.
Methods
This is an observational cohort study comparing the management of displaced distal radius fractures requiring reduction across two National Health Service trusts. Patients aged over 18 with isolated, displaced distal radius fractures were recruited. Patient demographics, AO fracture classification and grade of clinician performing the procedure were recorded. A numeric rating scale (NRS) pain score was obtained for each patient after manipulation. The quality of reduction was judged against standardised anatomical parameters.
Results
Some 200 patients were recruited (100 HB, 100 BB). There were no differences in age (BB: median 66.5 years, interquartile range [IQR] 55–74; HB: median 67 years, IQR 55–74; p = 0.79) or fracture characteristics (p = 0.29) between cohorts. Patients undergoing BB had significantly lower pain scores with a lower IQR than those undergoing HB (p < 0.005). Patients undergoing BB manipulation were more likely to have the fracture reduced and normal anatomy restored (p < 0.005). BBs were performed mainly by Foundation Year 2 junior doctors, whereas HB manipulations were performed by a range of clinicians from emergency nurse practitioners to consultants.
Conclusions
BB provides better analgesia than an HB. This can be performed successfully and reliably by Senior House Officer-level junior doctors.
Keywords: Radius fractures, Trauma, Closed fracture reduction, Nerve block, Local anaesthetics
Introduction
Fractures of the distal radius are a common injury, both in young patients following high-energy trauma and in the elderly following simple falls.1 Typically following a fall onto an outstretched hand, the fracture is often displaced and requires reduction to prevent neurovascular complications, provide pain relief and potentially restore almost anatomical reduction to allow conservative treatment.2 The process of reducing the fracture is painful, and a form of anaesthesia is required both for the comfort of the patient and to allow enough muscle relaxation to obtain a satisfactory outcome.
There are many different methods of providing anaesthesia, from conscious sedation to manipulation under local anaesthetic. Two common methods performed in United Kingdom (UK) practice are either a haematoma block (HB) or intravenous regional anaesthesia (Bier’s block [BB]);3 both are well-established techniques. The BB was first described by Arnold Bier in 19084 and is performed by inflating a proximally located tourniquet on the affected limb with intravenous anaesthetic injected distally to achieve regional anaesthesia. By contrast, an HB provides local anaesthesia by inserting a needle into the fracture site, aspirating blood to confirm its position and injecting anaesthetic directly into the fracture haematoma.
There is a limited evidence base comparing HB with BB. A Cochrane review found only five studies and concluded that although there is some evidence for BB providing better pain relief and easier manipulation compared with HB, it was not enough to confirm its clinical superiority.5 Subsequent guidance from the British Society for Surgery of the Hand and the National Institute for Health and Care Excellence (NICE) advocates the use of BB.2,6 However, a survey of British hospitals found that the majority still use HB. It is suggested that the practicalities of performing the procedure in terms of time, cost, relevant training of clinicians and procedural concerns prevented the widespread use of BB.3
This study aims to compare the analgesic properties of a BB with those of an HB when manipulating distal radius fractures. A secondary outcome measure of interest was the quality of fracture reduction.
Methods
This is an observational cohort study comparing the management of distal radius fractures across two National Health Service (NHS) trusts. King’s Mill Hospital (Sherwood Forest Hospitals NHS Foundation Trust), is a large district general hospital that routinely uses HBs to reduce distal radius fractures. Queen’s Medical Centre (Nottingham University Hospitals NHS Trust) uses BBs to reduce distal radius fractures. Patients presenting to either site were consecutively recruited to create two cohorts for study. A sample size of 200 patients was chosen to exceed that of previously reported studies demonstrating statistically significant results.7-9 This study was registered with the research and audit departments of Nottingham University Hospitals NHS Trust and Sherwood Forest Hospitals NHS Foundation Trust, and was considered exempt from ethical approval.
Inclusion and exclusion criteria
Patients aged over 18 with a single, isolated displaced distal radius fracture, for which the clinical team deemed manipulation was necessary, were included. Patients with open or multiple injuries, dementia or other cognitive impairment were excluded.
Variables
Patient demographic and radiographic data were collected. After having a manipulation, patients were asked to complete a short questionnaire by plaster room staff. This included a numeric rating scale (NRS; ordered 0–10) to assess the severity of pain experienced during manipulation. A subsequent review of radiographs and medical notes allowed the quality of the reduction to be assessed. This was judged against the anatomical parameters of an uninjured distal radius (radial height of 22mm, volar tilt of 11° and radial inclination of 22°). Pre-reduction X-rays were graded by the AO classification for distal radius fractures. The grade of doctor performing the manipulation was also recorded.
Haematoma block
Patients presenting to King’s Mill Hospital underwent an HB performed by an emergency department (ED) clinician at the time of presentation. The choice of local anaesthetic, dose and volume was chosen at the discretion of the treating clinician to best reflect normal practice and not artificially alter their outcomes. This was typically done with between 5 and 10ml of 1% lidocaine. The dose of anaesthetic was recorded where available. Reduction was performed without an image intensifier, using manual traction and the fracture was immobilised with a dorsal slab. The patient was immediately sent for a check X-ray following reduction, which was reviewed prior to discharge from the ED. Once discharged from the ED, the patient was followed up routinely in the fracture clinic by the orthopaedic team.
Bier’s block
Patients presenting to Queen’s Medical Centre were initially seen and assessed by an ED clinician. If the patient presented during working hours they were referred to the orthopaedic team for manipulation under BB. If the patient presented out of hours they were brought back the following day for routine manipulation and subsequent follow-up in the fracture clinic.
The BB was performed in the plaster room under the care of an orthopaedic clinician and a registered nurse. The procedure was performed according to a departmental protocol. A limb tourniquet was attached to the upper arm and inflated to 100mmHg above the systolic blood pressure. Then 40mg of prilocaine diluted to 50ml with 0.9% saline was injected intravenously. The hand was hung from finger traps and immobilised with a split plaster. An image intensifier was not used. Patients were taken to the adjacent X-ray department with the tourniquet inflated for a check X-ray, which was reviewed immediately in the X-ray department by the clinician who performed the manipulation.
Statistical analysis
Data were analysed using SPSS statistics program version 23. Categorical variables are presented as proportions. Ordinal variables are presented as mean or median with interquartile range (IQR) as appropriate. Groups were compared using chi-squared, Student’s t test or Mann–Whitney U test as appropriate. A p value of <0.05 was considered significant.
Binary logistic regression analysis was conducted to investigate the association between block type and visual analogue pain scores (VAS), adjusted for age, sex and AO fracture classification. In order to use binary logistic regression, VAS scores were dichotomised into ≤4 (no-to-mild pain) and ≥5 (moderate to severe pain) on the basis of previous literature.10 Further logistic regression models were constructed to identify associations between the different measures of fracture reduction (radial height, radial inclination and volar tilt) and type of block used, adjusting for age, sex and AO fracture classification. A further model was constructed using the same covariates but with the outcome variable being complete reduction in which all three radiographic parameters were restored.
The primary outcome measure was any difference in pain scores between the two groups of patients. The secondary outcome measure of interest was the quality of reduction.
Results
Some 239 patients were recruited across both sites: 39 patients were subsequently excluded because they did not meet the inclusion criteria and 200 patients were included for analysis, of whom 100 had undergone HB and 100 BB. The median patient age was 67 years (IQR 55–74), and the vast majority of patients (85.5%) were female. The majority of fractures were extra-articular (57%, AO classification A2/A3). Patient and fracture characteristics are summarised in Table 1. There were no significant differences in patient age, sex or fracture pattern between the two groups. The grade of clinician did vary significantly; in the BB group the manipulations were performed almost exclusively by Senior House Officer-level (SHO)-level junior doctors. By comparison, the HBs were performed either by emergency nurse practitioners or more senior doctors such as a specialty registrars or consultants.
Table 1 .
Patient and fracture characteristics
| Bier’s block | Haematoma block | p value | |
|---|---|---|---|
| Age, years (median, IQR) | 66.5 (55–74) | 67 (55–74) | 0.79 (Mann–Whitney U test) |
| Sex | 0.32 (chi-squared test) | ||
| Male | 17 | 12 | |
| Female | 83 | 88 | |
| AO fracture classification | 0.29 (chi-squared test) | ||
| A1 | 0 | 0 | |
| A2 | 16 | 26 | |
| A3 | 36 | 35 | |
| B1 | 0 | 0 | |
| B2 | 2 | 0 | |
| B3 | 7 | 2 | |
| C1 | 17 | 17 | |
| C2 | 17 | 16 | |
| C3 | 5 | 4 | |
| Clinician grade | < 0.05 (chi-squared test) | ||
| FY2 | 99 | 2 | |
| SPR | 1 | 23 | |
| CONS | 0 | 6 | |
| ENP | 0 | 47 | |
| Not documented | 0 | 22 |
CONS = consultant; ENP = emergency nurse practitioner; FY2 = Foundation Year 2 junior doctor; IQR = interquartile range; SPR = specialty registrar
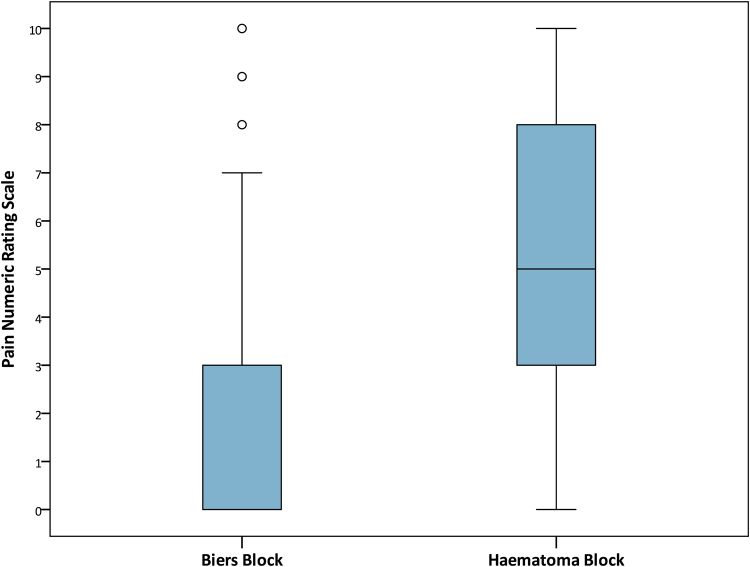
Patients receiving an HB reported significantly higher levels of pain than those receiving a BB (p < 0.005 Mann–Whitney U test). There was a greater spread of pain scores in those receiving an HB with a larger IQR in comparison with those who received a BB (Figure 1). A binary logistic regression model was constructed with no-to-mild pain (NRS ≤ 4) as the outcome variable and block type, age, sex and AO fracture classification as covariates. Regression analysis found that, even after adjusting for age, gender and AO fracture classification, patients receiving an HB were significantly less likely to report no-to-mild pain (NRS ≤ 4) compared with those receiving a BB (Table 2).
Figure 1 .
Box and whisker plot of reported pain for biers block and haematoma block
Table 2 .
Binary logistic regression model with a no-to-mild pain score (NRS ≤ 4) as the outcome using all patients (n = 200). Adjusted ORs, relative to a reference category for each variable and adjusted for all other included variables, are presented.
| Variable | NRS pain score of ≤4 |
|
|---|---|---|
| Adjusted OR (95% CI) | p value | |
| Block type | ||
| Bier’s | 1 | – |
| Haematoma | 0.12 (0.06–0.23) | <0.001 |
| Age | 0.98 (0.96–1.00) | 0.039 |
| Sex | ||
| Female | 1 | – |
| Male | 0.71 (0.27–1.92) | 0.502 |
| AO classification | ||
| A2 | 1 | – |
| A3 | 1.35 (0.56–3.27) | 0.509 |
| B2 | 1 | – |
| B3 | 0.77 (0.14–4.30) | 0.765 |
| C1 | 1.54 (0.54–4.40) | 0.416 |
| C2 | 1.21 (0.42–3.47) | 0.729 |
| C3 | 3.03 (0.47–19.47) | 0.242 |
| Constant | 17.20 (2.86–103.31) | 0.002 |
CI = confidence interval; NRS = numeric rating scale; OR = odds ratio
In total, 99% of BB procedures were performed by an SHO-level doctor. Consequently, it was not appropriate to include the clinician grade variable in any of the regression analysis owing to collinearity between block type and clinician grade, rendering the models unstable (the two variables themselves are almost perfectly related and hence cannot act as independent predictors). Regression analysis found patients receiving an HB are significantly less likely to achieve radial height, radial inclination, volar tilt and by extension, overall complete reduction, than patients receiving a BB, even after adjusting for age, sex and AO fracture classification (Table 3).
Table 3 .
Binary logistic regression model with restoration of radial height, radial inclination, volar tilt or complete reduction as the outcome using all patients (n = 200). Adjusted ORs, relative to a reference category for each variable and adjusted for all other included variables, are presented for each category.
| Variable | Restoration of radial height | Restoration of radial inclination | Restoration of volar tilt | Complete reduction | ||||
|---|---|---|---|---|---|---|---|---|
| Adjusted OR (95% CI) | p value | Adjusted OR (95% CI) | p value | Adjusted OR (95% CI) | p value | Adjusted OR (95% CI) | p value | |
| Block type | ||||||||
| Bier’s | 1 | – | 1 | – | 1 | – | 1 | – |
| Haematoma | 0.20 (0.09 to 0.48) | < 0.001 | 0.22 (0.10 to 0.51) | < 0.001 | 0.03 (0.01 to 0.64) | < 0.001 | 0.02 (0.00–0.18) | < 0 . 001 |
| Age | 0.98 (0.95 to 1.01) | 0.130 | 0.98 (0.96 to 1.01) | 0.223 | 1.00 (0.97 to 1.03) | 0.954 | 0.98 (0.95–1.02) | 0.298 |
| Sex | ||||||||
| Female | 1 | – | 1 | – | 1 | – | 1 | – |
| Male | 1.04 (0.33 to 3.29) | 0.947 | 0.81 (0.25 to 2.55) | 0.715 | 0.83 (0.25 to 2.72) | 0.756 | 1.00 (0.22–4.45) | 1 |
| AO classification | ||||||||
| A2 | 1 | – | 1 | – | 1 | – | 1 | – |
| A3 | 1.37 (0.50 to 3.76) | 0.536 | 1.10 (0.40 to 3.00) | 0.859 | 0.48 (0.17 to 1.39) | 0.177 | 1.98 (0.62–6.31) | 0.250 |
| B2 | 1 | – | 1 | – | 1 | – | 1 | – |
| B3 | 0.39 (0.06 to 2.61) | 0.332 | 0.97 (0.09 to 10.09) | 0.982 | 0.14 (0.02 to 0.97) | 0.047 | 0.43 (0.03–6.79) | 0.549 |
| C1 | 0.68 (0.22 to 2.05) | 0.491 | 0.72 (0.23 to 2.26) | 0.578 | 0.29 (0.08 to 1.08) | 0.064 | 0.92 (−3.570.25 to 3.31) | 0.893 |
| C2 | 0.75 (0.24 to 2.35) | 0.625 | 1.02 (0.31 to 3.41) | 0.973 | 0.12 (0.03 to 0.46) | 0.002 | 1.51 (−1.040.37 to 6.12) | 0.561 |
| C3 | 0.13 (0.02 to 0.69) | 0.016 | 0.35 (0.06 to 1.89) | 0.222 | 0.17 (0.02 to 1.33) | 0.092 | 0.49 (0.06–3.89) | 0.502 |
| Constant | 41.00 (4.60 to 365.37) | 0.001 | 33.72 (3.82 to 297.91) | 0.002 | 17.96 (2.20 to 146.80) | 0.007 | 285.72 (10.57–7,723.31) | 0.001 |
CI = confidence interval; OR = odds ratio
Where available, the final treatment outcome was recorded following review of the medical notes. This was available for 83 patients in the HB cohort and all patients in the BB cohort. One patient required re-manipulation in each cohort and there were no significant differences in the final treatment outcome in either cohort (chi-squared, p = 0.33). In total, 53 patients (64%) were managed conservatively and 29 (35%) underwent fixation following an HB. By comparison, 74 patients (74%) were managed conservatively and 25 (25%) underwent fixation following a BB.
Discussion
BB provided better analgesia to patients undergoing reduction of a displaced distal radius fracture. Patients having a BB were also more likely to have their fracture reduced successfully. The superiority of BB seen in this study is in keeping with existing evidence and supports the current national guidance.2,6 The relatively low use of BB in the UK despite existing evidence and recommendations suggests that either logistical or safety concerns have led to clinicians favouring HBs.
This may be due in part to staffing. NICE costings allocate two specialty registrars when performing an HB; given the frequency of distal radius fractures, staffing this would be a burden for any department. In this study, the manipulations in the BB cohort were performed almost exclusively by SHO-level doctors who had undergone training during induction and following an agreed departmental protocol. Training and allowing junior doctors to perform this procedure would alleviate this staffing burden.
Despite BB being performed by comparatively junior clinicians, the BB cohort provided consistently better analgesia in comparison with the HB cohort, in which there was a significant variation in pain scores. A successful HB is reliant on anaesthetic being infiltrated into the fracture site, and to do so accurately and consistently requires experience. Junior clinicians have previously been shown to have poorer outcomes in comparison with more senior colleagues when manipulating fractures using an HB.11 By contrast, the BB technique requires intravenous cannulation, which is performed routinely by most clinicians and may explain the consistent analgesia demonstrated in the BB cohort. Providing a standardised procedure for clinicians to follow is also likely to have been an influential factor. Standardisation of medical care has been associated with improved outcomes across many areas of medical practice, from perioperative care to resuscitation of trauma patients.12,13
The BBs were performed in a dedicated manipulation area created within the plaster room under the care of the on-call orthopaedic junior doctor with support from plaster room staff. The plaster room in QMC is adjacent to both the emergency and X-ray departments, and the location allows patients to have a check X-ray immediately post manipulation with the tourniquet still inflated. Should the X-ray be unsatisfactory it is possible for the clinician to have a second attempt at manipulation, which is not possible with an HB. Although not essential, performing the manipulation in the plaster room provided a controlled environment and helps offload a busy ED. If required, a BB can be performed just as easily in the ED, as is done regularly when urgently manipulating a fracture out of hours. Some clinicians may presume that the process of performing a BB was more time-consuming. However, Kendall et al demonstrated that when manipulating a fracture in the ED, performing a BB did not delay the patient’s transit through the department.7
There have been safety concerns surrounding BBs, particularly of anaesthetic toxicity inducing seizures and cardiac arrythmias. However, several large studies have reported no such complications.14-16 Even inadvertently deflating the tourniquet early has not been shown to have any significant side effects.17 Equally, although an HB is generally considered a safe procedure it has been associated with seizures.18,19 There is also a theoretical risk of introducing infection into the fracture site and, although rare, there have been case reports of osteomyelitis following an HB.20
Study limitations
This is an observational cohort study across two sites, which has its limitations. Recruitment was not randomised, being determined by the site to which the patient presented. Within the HB cohort, the volume of local anaesthetic that was infiltrated was left to the discretion of the clinician. Although previous studies have not demonstrated a significant difference when varying the dose of anaesthetic, it is a confounder that may contribute to the high range of pain scores reported in this cohort.21 HB requires accurate infiltration of anaesthetic into the fracture site to be effective and was performed without X-ray control. It is possible that some high pain scores in this cohort were due to anaesthetic not being infiltrated directly into the fracture site and thus are not representative of its true efficacy. However, allowing this variation of anaesthetic dosage and technique does provide a reflection of normal practice when manipulating fractures using an HB.
Other aspects of treatment were not standardised across the two sites, such as reduction technique and plaster technique, both of which may be confounding factors. Although the simplicity of finger trap traction may be a contributing factor to the outcomes seen in the BB cohort, previous studies have not shown a difference in comparison with manual traction.22 The patients in the BB cohort had a split plaster applied instead of a backslab. This is unlikely to have had any effect on the X-ray immediately post manipulation. A randomised study found no differences in reported pain and concluded that the method of immobilisation did not significantly alter patient outcome.23 Although limited by potential differences in decision-making between clinicians, patient factors and a high loss to follow-up, no significant differences in fixation or re-manipulation rates were demonstrated between cohorts in this study.
Finally, assessing subjective outcomes such as pain has its limitations. Although the NRS is a validated method of assessing pain, it is a single assessment and many other factors can influence patient reports of pain.24 A similar challenge is encountered when assessing the outcome of a manipulation; in this study a radiographic outcome was chosen as a marker of success. Although the aim of any manipulation is to anatomically reduce the fracture, there is evidence that anatomical reduction of the fracture may not correlate with the clinical outcome.25,26
Conclusion
Reducing displaced distal radius fractures under BB provides better analgesia than under an HB. With training and the use of a departmental protocol, BB can be performed both successfully and reliably by FY2 junior doctors.
Author Contributions
All authors made significant contributions to the paper. BO designed the study, undertook data collection and analysis, and prepared the manuscript. CB collected data and reviewed the manuscript. SK undertook data collection and statistical analysis, and reviewed the manuscript. SJA collected data and reviewed the manuscript. SSK designed the study, collected data and reviewed the manuscript. BJO designed the study, performed statistical analysis and reviewed the manuscript.
References
- 1.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury 2006; 37: 691–697. [DOI] [PubMed] [Google Scholar]
- 2.Blue Book Committee BSSH. Best practice for management of DistCOal Radial Fractures: British Orthopaedic Association and British Society for Surgery of the Hand; 2018. https://www.bssh.ac.uk/ (cited April 2023).
- 3.Sprot H, Metcalfe A, Odutola Aet al. . Management of distal radius fractures in emergency departments in England and Wales. Emerg Med J 2013; 30: 211–213. [DOI] [PubMed] [Google Scholar]
- 4.Brill S, Middleton W, Brill G, Fisher A. Bier's block; 100 years old and still going strong! Acta Anaesthesiol Scand 2004; 48: 117–122. [DOI] [PubMed] [Google Scholar]
- 5.Handoll HHG, Madhok R, Dodds C. Anaesthesia for treating distal radial fracture in adults. Cochrane Database Syst Rev 2002; 3: CD003320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Institute for Health and Care Excellence. Fractures (non-complex): Assessment and Management (NICE Guideline 38); 2016. https://www.nice.org.uk/guidance/ng38 (cited April 2023). [PubMed]
- 7.Kendall JM, Allen P, Younge Pet al. . Haematoma block or Bier's block for Colles’ fracture reduction in the accident and emergency department–which is best? J Accid Emerg Med 1997; 14: 352–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cobb AG, Houghton GR. Local anaesthetic infiltration versus Bier's block for Colles’ fractures. Br Med J (Clin Res Ed) 1985; 291: 1683–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abbaszadegan H, Jonsson U. Regional anesthesia preferable for Colles’ fracture. controlled comparison with local anesthesia. Acta Orthop Scand 1990; 61: 348–349. [DOI] [PubMed] [Google Scholar]
- 10.Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain 2003; 4: 407–414. [DOI] [PubMed] [Google Scholar]
- 11.Kakarlapudi TK, Santini A, Shahane SA, Douglas D. The cost of treatment of distal radial fractures. Injury 2000; 31: 229–232. [DOI] [PubMed] [Google Scholar]
- 12.Van Olden GD, Meeuwis JD, Bolhuis HWet al. . Clinical impact of advanced trauma life support. Am J Emerg Med 2004; 22: 522–525. [DOI] [PubMed] [Google Scholar]
- 13.Haynes AB, Weiser TG, Berry WRet al. . A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009; 360: 491–499. [DOI] [PubMed] [Google Scholar]
- 14.Thamizavel RC, Shankar S. BRIEF REPORT: How safe is Biers block in the accident and emergency department? Eur J Emerg Med 1996; 3: 56–58. [DOI] [PubMed] [Google Scholar]
- 15.Jakeman N, Kaye P, Hayward Jet al. . Is lidocaine Bier's block safe? Emerg Med J 2013; 30: 214–217. [DOI] [PubMed] [Google Scholar]
- 16.Bou-Merhi JS, Gagnon AR, Laurent J-YSet al. . Intravenous regional anesthesia administered by the operating plastic surgeon: Is it safe and efficient? experience of a medical center. Plast Reconstr Surg 2007; 120: 1591–1597. [DOI] [PubMed] [Google Scholar]
- 17.Bartholomew K, Sloan JP. Prilocaine for Bier's block: how safe is safe? Arch Emerg Med 1990; 7: 189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dorf E, Kuntz AF, Kelsey J, Holstege CP. Lidocaine-induced altered mental status and seizure after hematoma block. J Emerg Med 2006; 31: 251–253. [DOI] [PubMed] [Google Scholar]
- 19.Dezfuli B, Edwards CJ, DeSilva GL. Distal radius fracture hematoma block with combined lidocaine and bupivacaine can induce seizures while within therapeutic window: A case report. J Orthop Case Rep 2012; 2: 10–13. [PMC free article] [PubMed] [Google Scholar]
- 20.Basu A, Bhalaik V, Stanislas M, Harvey IA. Osteomyelitis following a haematoma block. Injury 2003; 34: 79–82. [DOI] [PubMed] [Google Scholar]
- 21.Orbach H, Rozen N, Rinat B, Rubin G. Hematoma block for distal radius fractures - prospective, randomized comparison of two different volumes of lidocaine. J Int Med Res 2018; 46: 4535–4538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Earnshaw SA, Aladin A, Surendran S, Moran CG. Closed reduction of Colles’ fractures: comparison of manual manipulation and finger-trap traction: a prospective, randomized study. J Bone Joint Surg Am 2002; 84: 354–358. [DOI] [PubMed] [Google Scholar]
- 23.Wik TS, Aurstad ÅT, Finsen V. Colles’ fracture: dorsal splint or complete cast during the first 10 days? Injury 2009; 40: 400–404. [DOI] [PubMed] [Google Scholar]
- 24.Thong ISK, Jensen MP, Miró J, Tan G. The validity of pain intensity measures: what do the NRS, VAS, VRS, and FPS-R measure? Scand J Pain 2018; 18: 99–107. [DOI] [PubMed] [Google Scholar]
- 25.Forward DP, Davis TR, Sithole JS. Do young patients with malunited fractures of the distal radius inevitably develop symptomatic post-traumatic osteoarthritis? J Bone Joint Surg Br 2008; 90: 629–637. [DOI] [PubMed] [Google Scholar]
- 26.Johnson N, Leighton P, Pailthorpe C, Dias J. Defining displacement thresholds for surgical intervention for distal radius fractures - A Delphi study. PLoS One 2019; 14: e0210462. [DOI] [PMC free article] [PubMed] [Google Scholar]