Abstract
Despite the active posttraumatic stress disorder (PTSD) screening program in Department of Veterans Affairs (VA) primary care clinics and the availability of empirically-supported treatments for PTSD at VA, many veterans for whom screening suggests treatment may be indicated do not gain access to VA-based mental healthcare. To determine where we may be losing veterans to follow-up, we need to begin by identifying the initial action taken in response to a positive PTSD screen in primary care. Using VA administrative data and chart review, we identified the spectrum of initial actions taken after veterans screened positive for PTSD in VA primary care clinics nationwide between October 2017 and September 2018 (N=41,570). We collapsed actions into those that could lead to VA-based mental healthcare (e.g., consult placed to a VA mental health clinic) versus not (e.g., veteran declined care), and then examined the association between these categories of actions and contextual- and individual-level variables. More than 61% of veterans with positive PTSD screens had evidence that an initial action toward VA-based mental healthcare was taken. Urban-dwelling and female veterans were significantly more likely to have evidence of these initial actions, whereas White and Vietnam-era veterans were significantly less likely to have this evidence. Our findings suggest that most veterans screening positive for PTSD in VA primary care clinics have evidence of initial actions taken toward VA-based mental healthcare; however, a substantial minority do not, making them unlikely to receive follow-up care. Findings highlight the potential benefit of targeted primary care-based access interventions.
Keywords: PTSD, veterans, access to care, primary care
Posttraumatic stress disorder (PTSD), one of the most common mental disorders impacting U.S. military veterans, is associated with numerous adverse outcomes, including mental and physical health comorbidities and impaired functioning and quality of life (see Yehuda et al., 2015, for a review). Further, the economic cost of PTSD is immense; health care costs for veterans with PTSD are 3.5 times higher than for those without (Congressional Budget Office, 2012).
To address the need for PTSD treatment, VA medical facilities are required to offer a full spectrum of evidence-based options for veterans with PTSD (Management of Posttraumatic Stress Disorder Workgroup, 2017; Veterans Health Administration, 2002). Research consistently demonstrates that veterans who receive these treatments exhibit clinically significant decreases in PTSD symptoms and increased quality of life (Chard et al., 2012; Eftekhari et al., 2013). Screening to identify veterans with PTSD is an important first step to connect them to mental health services.
Primary care is the most common point of entry for veterans with PTSD. Because of this, core VA ambulatory clinics are required to screen for PTSD (Bohnert, Sripada, Mach, & McCarthy, 2016; Lecruibier, 2004; Veterans Health Administration, 2002). VA primary care staff are prompted to complete this screen by a clinical reminder in VA’s electronic health record (Department of Veterans Affairs, 2021; Seal et al., 2008).
Despite the active VA PTSD screening program and the availability of empirically-supported treatments for PTSD within VA, many veterans for whom screening suggests treatment may be indicated do not obtain VA-based mental healthcare (Bohnert et al., 2016). It is important to recognize that a positive PTSD screen is not equivalent to a PTSD diagnosis, nor is it a guarantee that treatment is clinically indicated, which may explain why not all veterans who screen positive receive treatment. The VA currently uses the Primary Care PTSD Screen for DSM-5 (PC-PTSD-5; Prins et al., 2015) to screen for PTSD (Veterans Health Administration, 2017). In a recent study of the PC-PTSD-5, Bovin et al. (2021) found that although the instrument demonstrated excellent psychometric properties, a minority of veterans who screened positive did not meet criteria for a PTSD diagnosis according to the diagnostic reference standard (i.e., false positives). However, veterans who are true positives (i.e., screen positive on the PC-PTSD-5 and meet diagnostic criteria for PTSD according to the reference standard) cannot be reliably separated from veterans who are false positives without a diagnostic interview. Because busy primary care providers may not have the opportunity to administer structured diagnostic interviews, and clinical judgment is not always consistent with standardized assessment (e.g., Holowka et al., 2014), it is unclear what percentage of veterans who screen positive do not receive treatment due to lack of clinical need versus other reasons. Thus, investigation into why veterans who screen positive may not receive follow-up care is warranted.
Efforts to study this nationwide have been stymied by a lack of consistency in the coding of mental health referrals (Institute of Medicine, 2012). Most studies examining the association between screening and access have therefore only looked at small geographic areas, which has made generalizability to the entire VA system difficult (Lindley et al., 2010; Lu et al., 2011; Lu et al., 2012). To date, only one study has examined this on a national scale, using a random sample of new VA primary care patients in fiscal year (FY) 2009. Bohnert et al. (2016) investigated whether the location of the services received on the day a veteran screened positive for PTSD predicted the veteran’s initial receipt of VA-based mental healthcare. Results indicated that nearly 45% of veterans did not receive any follow-up VA mental healthcare within one year of screening positive for PTSD. Of note, this study was conducted more than a decade ago, and may therefore not reflect the current context.
Several different pathways to VA-based care are possible after a positive screen. We have adopted the term “access pathways” to refer to the series of options offered to, and choices made by, veterans after screening positive for PTSD in a VA primary care-based clinic that may eventually lead to the receipt of VA-based mental healthcare. Our conceptualization of access as a process, rather than as a destination, highlights both the complex interplay between the provider and veteran in determining movement along the access pathways, as well as the importance of examining each step in each possible access pathway to understand who ultimately receives care. Each access pathway likely has many steps, e.g., if the pathway leads to a veteran ultimately receiving care in a VA-based mental health clinic, a consult must first be placed, then an intake must be scheduled, and then the intake must be attended; the absence of an action toward care at any step of a pathway – whether it is the result of the provider not offering care options, the veteran declining care, or a combination of the two – could lead to the veteran not receiving care. Therefore, to accurately trace the access pathways and determine who is being lost in the pathway, where they are being lost, and why they are being lost, we need to begin by identifying the initial action taken in response to a positive PTSD screen in primary care.
The current study represents the first step in comprehensively mapping the access pathways veterans may follow after screening positive for PTSD by identifying the spectrum of initial actions taken directly after this screen. We used a combination of VA administrative data and chart review to identify the initial actions following a positive PTSD screen for veterans presenting for treatment in primary care. Our primary goal was to classify these responses into those that could lead to VA-based mental healthcare versus not, to understand where veterans with PTSD may be initially lost. To begin to understand which veterans may be at risk for being lost, we also examined the association between these action categories and contextual- and individual-level factors.
Methods
Sample and Data
Our sample included all veterans with a positive PTSD screen recorded in a VA primary care clinic between October 2017 and September 2018 (specifically, a score of ≥ 3 on the Primary Care Screen for PTSD for DSM-IV [PC-PTSD] or ≥ 4 on the PC-PTSD-5, both of which demonstrate excellent psychometric properties [Bovin et al., 2021; Prins et al., 2003]); who did not have a recorded PTSD diagnosis or evidence of either a VA or non-VA mental health visit 12 months prior to screening (i.e., “new” screens); were not excluded from the VA screening program (e.g., those with a life expectancy of less than 6 months); and were at least 18 years old at the time of screening, for a total of 41,570 veterans. All data were accessed from the VA Corporate Data Warehouse (CDW; Department of Veterans Affairs, 2018). The VA Boston Healthcare System Institutional Review Board approved this study.
Measures
Primary Outcome
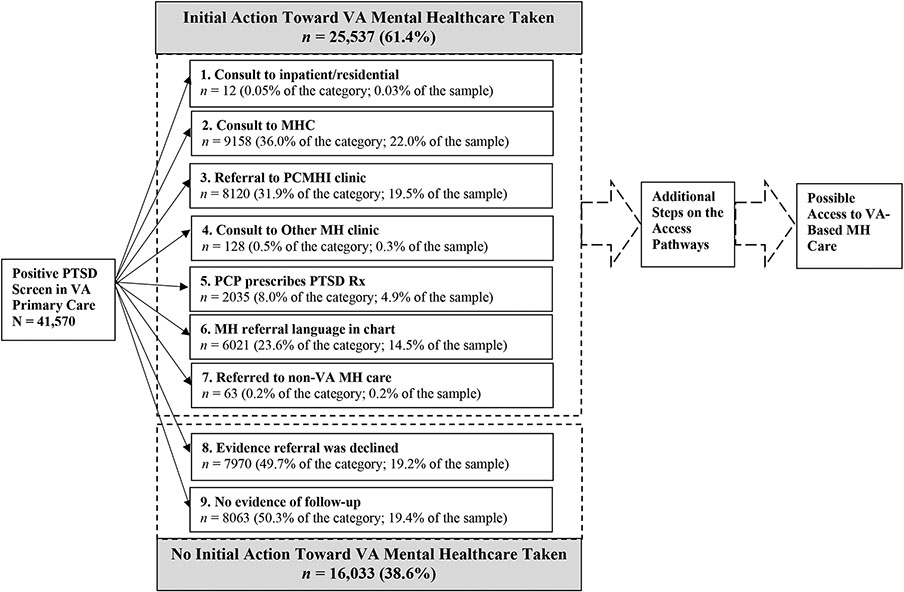
The primary outcome of interest was the initial action taken after a veteran screened positive for PTSD (particularly, whether an initial action toward VA mental healthcare was taken after a new positive PTSD screen). Initial actions toward VA care, which were limited to actions that (1) occurred following a new positive PTSD screen in a VA primary care clinic and (2) could plausibly lead to accessing VA-based mental health care, included evidence of a referral to a VA inpatient or residential clinic, VA mental health clinic (MHC), Primary Care Mental Health Integration (PCMHI) clinic, VA non-treatment related mental health clinic (e.g., Health Care for Homeless Veterans/Homeless Chronically Mentally Ill clinic), and/or referral to a community care provider, and/or evidence of a prescription written for a psychotropic medication consistent with PTSD treatment. Because we were interested in actions that followed directly after the positive screen, we operationalized evidence of a referral to include a mental health consult placed within seven days of the positive screen; and/or evidence of intent to refer based on a search of chart notes from the visit associated with the positive screen (accessed by using the Text Integration Utility domain of the CDW, and querying for key terms including – but not limited to – stock language indicating follow-up actions from the electronic screening reminder). This was necessary in large measure for PCMHI consults which are frequently same-day warm handoffs (and as such not necessarily recorded as formal consults in the CDW). Because of this, we also included evidence of a PCMHI visit within 60 days of the screen, in addition to consults placed to PCMHI, as evidence of this initial action. New and refilled prescriptions were limited to those associated with the screening visit. To comprehensively identify prescriptions that would represent an initial VA action we considered medications recommended or suggested by the VA/DoD Clinical Practice Guideline for the treatment of PTSD (Management of Posttraumatic Stress Disorder Workgroup, 2017) and, in consultation with an expert in evidence-based psychopharmacology, medications that might be used for PTSD treatment but were not listed in the Guidelines (D. Osser, personal communication, 10/2/2019). Based on these considerations, we classified prescriptions placed for the following medications as evidence of an initial action toward VA care: sertraline, paroxetine, fluoxetine, venlafaxine, nefazodone, imipramine, phenelzine, prazosin, trazodone, and mirtazapine. Veterans with evidence of more than one type of action were classified hierarchically (see Figure 1), consistent with our framework relating to intensity of care and consistency with the VA/DoD Clinical Practice Guideline.
Figure 1. Classification of Veterans by Whether an Initial Action towards VA-Based Mental Healthcare was Taken.
Note. Actions are listed in the order in which participants were classified.
Moderating Factors
We examined two contextual variables (site of care, site rurality) and four individual factors (gender, race, ethnicity, and service era) that we hypothesized might moderate classification. All variables were accessed via the VA CDW. The CDW dichotomizes site of care into VA medical center (VAMC) and community-based outpatient clinic (CBOC). Site rurality was classified by the CDW into three categories: urban, rural, and highly rural. Gender was coded in the CDW as either female or male. From the CDW, participants were classified into one of seven categories of race: American Indian or Alaska Native; Asian; Black or African American; Declined to Answer; Native Hawaiian or Other Pacific Islander; Unknown by Patient; and White. Ethnicity in the CDW is divided into four categories: Declined to Answer; Hispanic or Latino/a; Not Hispanic or Latino/a and Unknown by Patient. The CDW identified nine service era categories: Gulf War (veterans who served since August 20, 1990, including those who served during the wars in Iraq and Afghanistan); Korean War; None; Other; Post-Korean; Post-Vietnam; Pre-Korean; Vietnam Era; and World War II.
Analyses
First, using CDW data, we classified veterans based on evidence of one of nine actions, which represented the spectrum of initial responses taken after a veteran screened newly positive for PTSD. We calculated frequencies for each of these actions. Second, we collapsed the identified actions into a single dichotomous variable: evidence that an initial action toward VA-based mental healthcare was taken versus not. Our classification method demonstrated a high level of accuracy: when our CDW classification was checked for 200 randomly selected participants using chart review, PPV = .92; NPV = .81; κ = .73. Frequency counts and percentages of moderating variables within the two action categories were then calculated. Third, we collapsed our moderating variables into smaller categories, which both increased power and preserved data (see Table 1). Fourth, we divided the Gulf War service era category into two sub-categories: 1) the first Gulf War era, which included veterans who served in the Gulf War era prior to 9/11/2001, and 2) Operation Enduring Freedom, Operation Iraqi Freedom, and Operation New Dawn (OEF/OIF/OND), which included veterans who served during the Second Gulf War era starting on or after 9/11/2001. Fifth, we conducted univariate chi-square and bivariate logistic regression analyses to determine the association between moderating variables and the initial action taken. Due to the large sample size, we adopted a dual criterion for significance, as we have done with other large-scale VA administrative database studies (Miller et al., 2014; Miller et al., 2015). Specifically, we considered a χ2 to be significant if p < .001 and the associated odds ratio (OR) corresponded to an effect size of d > 0.20 (Cohen, 1988). According to Chinn (2000), this effect size is equivalent to an OR that is less than 0.70 or greater than 1.40.
Table 1.
Sample Characteristics
| Characteristic | M/n | SD/% |
|---|---|---|
| Age (M, SD) | 50.7 | 16.1 |
| Gender (n, %) | ||
| Female | 4747 | 11.4 |
| Male | 36823 | 88.6 |
| Race (n, %) | ||
| Black | 10201 | 24.5 |
| White | 26286 | 63.2 |
| Othera | 2161 | 5.1 |
| Asian | 715 | 1.7 |
| Native American/Alaska Native | 734 | 1.8 |
| Pacific Islander/Hawaiian | 677 | 1.6 |
| Missingb | 2957 | 7.1 |
| Declined to Answer | 1148 | 2.8 |
| Unknown to Patient | 239 | 0.6 |
| Missing in Chart | 1570 | 3.8 |
| Ethnicity (n, %) | ||
| Hispanic or Latino/a | 3810 | 9.2 |
| Not Hispanic or Latino/a | 36240 | 87.2 |
| Missingb | 1520 | 3.7 |
| Declined to Answer | 147 | 0.4 |
| Unknown by Patient | 386 | 0.9 |
| Missing in Chart | 987 | 2.4 |
| Service Era (n, %) | ||
| World War II/Koreac | 511 | 1.2 |
| WWII | 26 | 0.1 |
| Pre-Korea | 3 | 0.0 |
| Korea | 321 | 0.8 |
| Post-Korea | 161 | 0.4 |
| Vietnam | 11168 | 26.9 |
| Post-Vietnam | 3126 | 7.5 |
| First Gulf Ward | 12413 | 29.9 |
| OEF/OIF/ONDe | 14239 | 34.3 |
| Otherf | 113 | 0.3 |
| Other | 9 | 0.0 |
| None | 83 | 0.2 |
| Missing in Chart | 21 | 0.1 |
| Site of Screening (n, %)g | ||
| CBOC | 25369 | 61.0 |
| VAMC | 15977 | 38.4 |
| Site Rurality (n, %)h | ||
| Rurali | 14290 | 34.4 |
| Highly Rural | 524 | 1.3 |
| Rural | 13766 | 33.1 |
| Urban | 27067 | 65.1 |
Note. N = 41, 570.
CBOC = Community-Based Outpatient Center; VAMC = Veterans Affairs Medical Center.
Other = category used for analyses that subsumes veterans who identified as Asian, Native American/Alaska Native or Pacific Islander/Hawaiian
Missing = category used for analyses that subsumes Declined to Answer, Unknown by Patient, and Missing in Chart
World War II/Korea = category used for analyses that subsumes veterans who served during World War II, the pre-Korean War era, the Korean War, and the post-Korean War era
First Gulf War = category used for analyses that includes veterans who served during the Gulf War era prior to 9/11/2001
OEF/OIF/OND = category used for analyses that includes veterans who served during the Second Gulf War era starting on or after 9/11/2001 in service of Operation Enduring Freedom, Operation Iraqi Freedom, and/or Operation New Dawn
Other = category used for analyses that subsumes veterans whose reported service era was Other Non-Veteran or Other or None, or who had missing data
Missing data for this variable was less than 0.05% of the sample (n = 224) and was dropped from subsequent analyses
Missing data for this variable was less than 0.05% of the sample (n = 213) and was dropped from subsequent analyses
Rural = category used for analyses that subsumes veterans who were seen in either Highly Rural or Rural Settings.
Results
Our final sample included 41,570 veterans. Participants were mostly White, Non-Hispanic, urban-dwelling male veterans, who ranged in age from 19-97 years (M = 50.7 years, SD = 16.1 years). Nearly two thirds of the sample were Gulf War era veterans, and the majority were screened for PTSD in CBOCs (see Table 1).
Our categorization analyses revealed that nearly two-thirds of participants had evidence that an initial action toward VA care had been taken (61.4%), made up of seven exclusive sub-categories of actions (Figure 1). These sub-categories included evidence that (1) a consult was placed to VA inpatient or residential care; (2) a consult was placed to a VA MHC; (3) a referral had been made to a VA PCMHI clinic; (4) a consult was placed to a non-treatment related mental health clinic (e.g., Health Care for Homeless Veterans/Homeless Chronically Mentally Ill); (5) a prescription was placed by the VA provider for a PTSD medication; (6) a referral was discussed and/or would be placed; and (7) a consult was placed to a community care practitioner. The largest percentage of veterans categorized as having had an initial VA action taken had evidence that a consult was placed to either a MHC or a PCMHI clinic; the smallest had evidence of being referred to an inpatient or residential clinic (Figure 1).
Of the patients without evidence that an initial VA action was taken (38.6% of the sample), we identified two sub-categories of veterans: those who had evidence in their charts of being offered, but declining, follow-up care; and those without any evidence of any follow-up care (VA or non-VA) after a positive PTSD screen (Figure 1).
Although χ2 tests were significant for all moderating variables in predicting the initial action taken, only seven individual comparisons represented at least a small effect and were therefore considered significant. Veterans living in urban locations (in comparison to rural locations), female veterans (in comparison to male veterans), Black veterans (in comparison to White veterans), and veterans who served in in the post-Vietnam era, the First Gulf War era, the Second Gulf War era, and those classified as Other (in comparison to those who served in the Vietnam era) were all significantly more likely to have evidence that an initial action toward VA mental healthcare was taken (see Table 2).
Table 2.
Univariate Comparisons of Veterans with Evidence that an Initial Action Towards VA Mental Healthcare was Taken by Contextual and Individual Factors
| Factor | Initial Action Taken (n) |
Initial Action Taken (%) |
χ2 | OR | Lower 95% CI | Upper 95% CI |
|---|---|---|---|---|---|---|
| Site of Screening | 51.1* | 1.16 | 1.11 | 1.21 | ||
| VAMC | 10150 | 63.5 | ||||
| CBOCa | 15225 | 60.0 | ||||
| Site Rurality | 281.5* | 1.42* | 1.37 | 1.48 | ||
| Urban | 17447 | 64.5 | ||||
| Rurala | 8005 | 56.0 | ||||
| Gender | 255.8* | 1.72* | 1.60 | 1.83 | ||
| Female | 3421 | 72.1 | ||||
| Malea | 22116 | 60.1 | ||||
| Race | 235.5* | |||||
| Black | 6878 | 67.4 | 1.45* | 1.38 | 1.52 | |
| Other | 1342 | 63.1 | 1.20 | 1.09 | 1.31 | |
| Missing | 1857 | 62.8 | 1.18 | 1.09 | 1.28 | |
| Whitea | 15460 | 58.8 | ||||
| Ethnicity | 79.3* | |||||
| Hispanic | 2595 | 68.1 | 1.38 | 1.28 | 1.48 | |
| Missing | 913 | 60.1 | 0.97 | 0.87 | 1.08 | |
| Non-Hispanica | 22029 | 60.8 | ||||
| Service Era | 1944.2* | |||||
| WWII/Korea | 215 | 42.1 | 0.86 | 0.72 | 1.03 | |
| Post-Vietnam | 1889 | 60.4 | 1.81* | 1.67 | 1.96 | |
| First Gulf War | 8029 | 64.7 | 2.17* | 2.06 | 2.29 | |
| OEF/OIF/OND | 10215 | 71.7 | 3.01* | 2.86 | 3.17 | |
| Other | 82 | 72.6 | 3.14* | 2.07 | 4.75 | |
| Vietnama | 5107 | 45.7 |
Reference group
Because the two sub-groups of veterans without an initial action toward VA mental healthcare taken – those with evidence that a referral was offered but declined and those without evidence of any follow-up – may differ importantly from one another, we compared these two groups to one another across the six moderating variables. Only one variable – service era – represented at least a small effect and was therefore considered a significant difference (χ2 = 204.8; p < .05). Specifically, whereas Vietnam veterans were half as likely as World War II and Korean veterans to have no evidence of follow-up (versus evidence that they had declined care; OR = 0.57; 95% CI: 0.44-0.73), they were approximately 1.5 times more likely to have no evidence of follow-up (versus evidence of that they declined care) than veterans who served in the post-Vietnam era (OR = 1.45; 95% CI: 1.28-1.64), the First Gulf War era (OR = 1.52; 95% CI: 1.40-1.65), and the OEF/OIF/OND era (OR = 1.53; 95% CI: 1.41-1.65). Despite this difference, when the original analyses were repeated comparing veterans with an initial action toward VA mental healthcare to those with evidence that care was declined and with those without evidence of follow-up respectively, the two new sets of analyses both demonstrated an identical pattern to the one presented in Table 2.
Discussion
Our analyses identified seven initial actions which, if taken, would put veterans on a VA mental health access pathway. Results indicated that more than 61% of veterans who screened positive for PTSD had evidence that at least one of these actions was taken. This suggests that the VA screening program is generally successful; nearly two-thirds of veterans who screen positive are placed on a pathway toward VA mental healthcare. Despite this, nearly 39% of veterans with a new positive PTSD screen in primary care nationwide did not have evidence of an initial VA screening action. Thus, more than one in three veterans who screened positive for PTSD in a VA primary care clinic – over 16,000 veterans in a single year – had no evidence within the VA medical record of an accepted referral to mental health care. A portion of these veterans may not have evidence of this initial action because follow-up care was not clinically indicated. However, our finding that evidence of an initial action varied as a product of contextual- and individual-level factors suggests that other factors beyond clinical need may be relevant to access (e.g., there is no reason to think that individuals for whom care is not clinically indicated are more likely to live in rural, rather than urban, areas).
Our findings suggest that both contextual- and individual-level factors may importantly influence whether an initial VA action is taken after a veteran screens positive for PTSD. Veterans were more likely to enter a VA access pathway to care if they were women (vs. men), Black (vs. White), or urban (vs. rural), and less likely if they served during the Vietnam era (vs. all other eras except the WWII/Korean War). The reasons for these differences are not clear. Interestingly, our finding that Black veterans are more likely to have evidence of an initial action than White veterans stands in contrast to research demonstrating that Black veterans may be less likely than White veterans to receive psychotherapy in VA primary care settings (e.g., Spoont, Sayer, Kehle-Forbes, Meis, & Nelson, 2017). Because available evidence suggests the presence of possible racial-ethnic disparities in VA psychotherapy services (e.g., Hunt & Rosenheck, 2011; Spoont et al., 2017), research is needed to explore whether different factors may be influencing Black veterans, in comparison to White veterans, which may negatively impact their ability to access care. This would pave the way for tailored access interventions. In the case of the urban/rural difference, which is consistent with other research suggesting that rural residence is associated with lower VA mental health service use (e.g., Boscarino et al., 2020), the finding may be the result of a confluence of factors associated with rurality, including a shortage of providers, fewer options for specialized treatment both within and outside the VA, and geographic barriers (Gale & Heady, 2013). Regardless of the reason(s), this finding suggests that additional intervention may still be needed, as methods currently in effect (e.g., telehealth) do not appear to completely solve the problem of access for rural veterans who may benefit from care.
By determining that more than one-third of veterans who screened positive for PTSD nationwide do not have evidence that an initial action toward VA care was taken, our work revealed a key place in the access pathways where veterans who may benefit from care may be being lost to follow-up. However, access problems may also manifest later in the pathways. If the trends estimated by Bohnert et al. (2016) remain consistent, our findings would conservatively estimate that thousands of additional veterans every year who screen positive for PTSD and have evidence of an initial action towards VA care will not ultimately receive VA-based mental health care. To best inform implementation strategies that can maximize the number of veterans receiving appropriate VA-based mental health treatment, it is imperative to map the remainder of the access pathways veterans follow after a positive PTSD screen.
Research is also needed to identify the range of contextual- and individual-level factors that influence progress along the VA access pathways. The interaction of these factors is particularly relevant, as each action taken is a product of the context and the individual. For example, for a consult to a VA MHC to be placed, the clinic must be available to take new patients, the provider must offer the option of treatment in the clinic to the veteran, the veteran must agree to have the consult placed, and the provider must then enter the consult.
Our classification system categorized the small number of veterans referred to non-VA care (i.e., to community providers) as those with evidence of an initial VA action. This decision is consistent with mechanisms like the Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act (VA Mission Act of 2018), which allow VA providers to place referrals to appropriate community care providers as an extension of VA care. Despite the increased ability for patients to be referred in this manner, it is noteworthy that our sample included such a small number of veterans who were offered and accepted this type of consult (n = 63; 0.2% of the sample). One reason for the limited number of community care consults may be a lack of coordination between systems. Consistent with this, qualitative analyses have suggested that care coordination between VA and non-VA providers is often limited (Miller, Gurewich et al., 2021; Miller, Shin, Pugatch, & Kim, 2021), minimizing referrals by VA clinicians to community providers who are able to deliver guideline-recommended care. Additional work is needed to explore how to facilite additional referrals, therefore providing additional options for veterans in need of care.
Our primary analyses classified veterans with evidence that a referral was offered but declined into the category of veterans without evidence of an initial VA action. This is not meant to imply that patient refusal of VA follow-up care necessarily represents a system failure on the part of VA. Veterans may have good reasons for declining VA follow-up care despite screening positive for PTSD. Further, our results suggest that there may be important differences between veterans who decline care and those without evidence of follow-up; although our analyses only identified one variable upon which these two groups differ (i.e., service era), other differences that may lead veterans to appropriately decline care may exist. However, because it remains unclear what percentage of these veterans did not receive care even though clinically indicated, additional work is needed to better understand the factors that may have led to veterans declining care.
More broadly, for the veterans who would benefit from care but did not have evidence of an initial VA action, the lack of action taken may have been the result of a choice by the veteran and/or provider (e.g., a veteran who declines care because they lack knowledge about the benefits of trauma-focused therapy; a provider who does not offer services to a veteran due to lack knowledge of/access to available services) which could benefit from intervention. Without studying this group as a whole, we will be unable to identify those for whom care is warranted, and where we must intervene to provide access to that care. Our work therefore represents the first step in improving access to care for these veterans.
Our findings are limited by the use of data that were entered into the VA CDW (both administrative data and electronic clinical data via chart review). Therefore, we captured only what the provider billed for and/or included in the note, including errors. However, the high level of reliability observed for our methodology helps mitigate this concern. Also, despite the strong psychometric properties of the PC-PTSD and PC-PTSD-5, a proportion of veterans who screened positive – and were therefore included in our analyses – will not meet diagnostic criteria for PTSD according to a structured interview. Although some of these veterans may meet criteria for subthreshold PTSD and still benefit from PTSD treatment, others may not, which may in part explain why not all veterans who screened positive for PTSD were referred to VA care. However, even if a veteran’s positive screen was a false positive, this does not necessarily mean that follow-up care for the veteran is not indicated. Research suggests that a substantial portion of patients who are false positives on a mental health screen will meet diagnostic criteria for at least one other psychiatric diagnosis (Leon et al., 1997). Consistent with this, Bovin et al. (2021) found that more than 92% of veterans who were false positives on the PC-PTSD-5 screened positive for another VA screen, suggesting that many of these veterans could potentially benefit from additional clinical attention. The potential need for clinical attention of a large percentage of false positives, combined with the likelihood that true and false positives cannot be reliably separated in primary care, suggest that veterans without an initial VA action could benefit from further study. Finally, because the medications we considered as indicating an initial VA action may have been prescribed for conditions other than the treatment of PTSD (e.g., antidepressants have demonstrated effectiveness in treating fibromyalgia; see Moret & Briley, 2006 for a review), we may have misclassified a percentage of these veterans as having an initial VA action when none was present. Future work is needed to determine whether veterans who received these prescriptions did so as a direct result of the screen and not due to comorbid conditions.
Despite these limitations, the current study advances the comprehensive mapping of access pathways to VA-based mental healthcare for veterans with PTSD. By conceptualizing access as a process rather than a destination, we uncovered an important potential barrier to access: nearly 39% of veterans who screened positive for PTSD did not enter a VA access pathway, and some veteran subgroups were less likely than others to enter a trajectory toward care. Our results suggest that additional work is needed to understand the process of access, so that targeted interventions can be put in place at each step of the access pathways in order to maximize the number of veterans who get the care they need.
Impact Statement:
This study examined the initial actions taken after veterans screened positive for PTSD in VA primary care clinics nationwide between October 2017 and September 2018 (N=41,570). More than 61% of these veterans had evidence that the screen resulted in an action taken toward VA-based mental healthcare, suggesting that the VA screening program is generally successful. Despite this, nearly 39% of these veterans did not have evidence of an initial VA screening action, highlighting the importance of further research to refine and deploy primary care-based access interventions.
Acknowledgments
This research was supported by award I21 HX002613-01A1 from the US Veterans Health Administration Health Services Research & Development Service, awarded to Dr. Bovin (PI). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the U.S. Department of Veterans Affairs or the U.S. government. The authors have no conflicts of interest to disclose. Portions of this project were presented as a poster presentation to the Academy Health Annual Research Meeting (Virtual), June 14-17, 2021.
References
- Bohnert KM, Sripada RK, Mach J, & McCarthy JF (2016). Same-day integrated mental health care and PTSD diagnosis and treatment among VHA primary care patients with positive PTSD screens. Psychiatric Services, 67(1), 94–100. 10.1176/appi.ps.201500035 [DOI] [PubMed] [Google Scholar]
- Boscarino JJ, Figley CR, Adams RE, Urosevich TG, Kirchner HL, & Boscarino JA (2020). Mental health status in veterans residing in rural versus non-rural areas: results from the veterans' health study. Military Medical Research, 7(1), 44. 10.1186/s40779-020-00272-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovin MJ, Kimerling R, Weathers FW, Prins A, Marx BP, Post EP, & Schnurr PP (2021). Diagnostic accuracy and acceptability of the primary care posttraumatic stress disorder screen for the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) among US veterans. JAMA Network Open, 4(2), e2036733. 10.1001/jamanetworkopen.2020.36733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chard KM, Ricksecker EG, Healy ET, Karlin BE, & Resick PA (2012). Dissemination and experience with cognitive processing therapy. Journal of Rehabilitation Research and Development, 49(5), 667–678. 10.1682/jrrd.2011.10.0198 [DOI] [PubMed] [Google Scholar]
- Chinn S (2000). A simple method for converting an odds ratio to effect size for use in meta-analysis. Statistics in Medicine, 19(22), 3127–3131. [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Associates. [Google Scholar]
- Congressional Budget Office. (2012). The Veterans Health Administration’s treatment of PTSD and traumatic brain injury among recent combat veterans. Congress of the United States. www.cbo.gov/sites/default/files/112th-congress-2011-2012/reports/02-09-PTSD_0.pdf [Google Scholar]
- Department of Veterans Affairs. (2018). 172VA10P2: VHA Corporate Data Warehouse - VA. 79 FR 4377. Accessed July 27, 2020.
- Department of Veterans Affairs. (2021). VistA Monograph. Department of Veterans Affairs. https://www.va.gov/vdl/documents/Monograph/Monograph/Vista_Monograph_0421_REDACTED.pdf [Google Scholar]
- Eftekhari A, Ruzek JI, Crowley JJ, Rosen CS, Greenbaum MA, & Karlin BE (2013). Effectiveness of national implementation of prolonged exposure therapy in Veterans Affairs care. JAMA Psychiatry, 70(9), 949–955. 10.1001/jamapsychiatry.2013.36 [DOI] [PubMed] [Google Scholar]
- Gale JA, & Heady HR (2013). Rural vets: their barriers, problems, needs. Health Progress, 94(3), 48–51. [PubMed] [Google Scholar]
- Holowka DW, Marx BP, Gates MA, Litman HJ, Ranganathan G, Rosen RC, & Keane TM (2014). PTSD diagnostic validity in veterans affairs electronic records of Iraq and Afghanistan veterans. Journal of Consulting and Clinical Psychology, 82, 569–579. 10.1037/a0036347 [DOI] [PubMed] [Google Scholar]
- Hunt MG, & Rosenheck RA (2011). Psychotherapy in mental health clinics of the Department of Veterans Affairs. Journal of Clinical Psychology, 67(6), 561–573. 10.1002/jclp.20788 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2012). Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations: Initial Assessment. National Academies Press (US). [PubMed] [Google Scholar]
- Lecrubier Y (2004). Posttraumatic stress disorder in primary care: a hidden diagnosis. Journal of Clinical Psychiatry, 65, 49–54. [PubMed] [Google Scholar]
- Leon AC, Portera L, Olfson M, Weissman MM, Kathol RG, Farber L, … & Pleil AM (1997). False positive results: A challenge for psychiatric screening in primary care. American Journal of Psychiatry, 154, 1462–1464. 10.1176/ajp.154.10.1462 [DOI] [PubMed] [Google Scholar]
- Lindley S, Cacciapaglia H, Noronha D, Carlson E, & Schatzberg A (2010). Monitoring mental health treatment acceptance and initial treatment adherence in veterans: Veterans of Operations Enduring Freedom and Iraqi Freedom versus other veterans of other eras. Annals of the New York Academy of Sciences, 1208, 104–113. 10.1111/j.1749-6632.2010.05692.x [DOI] [PubMed] [Google Scholar]
- Lu MW, Duckart JP, O'Malley JP, & Dobscha SK (2011). Correlates of utilization of PTSD specialty treatment among recently diagnosed veterans at the VA. Psychiatric Services, 62(8), 943–949. 10.1176/ps.62.8.pss6208_0943 [DOI] [PubMed] [Google Scholar]
- Lu MW, Carlson KF, Duckart JP, & Dobscha SK (2012). The effects of age on initiation of mental health treatment after positive PTSD screens among Veterans Affairs primary care patients. General Hospital Psychiatry, 34(6), 654–659. 10.1016/j.genhosppsych.2012.07.002 [DOI] [PubMed] [Google Scholar]
- Management of Posttraumatic Stress Disorder Workgroup. (2017). VA/DoD clinical practice guidelines for the management ofposttraumatic stress disorder and acute stress disorder. Department of Veterans Affairs, Department of Defense. https://www.healthquality.va.gov/guidelines/MH/ptsd/VADoDPTSDCPGFinal012418.pdf [Google Scholar]
- Miller CJ, Gurewich D, Garvin L, Pugatch M, Koppelman E, Pendergast J, Harrington K, & Clark JA (2021). Veterans Affairs and rural community providers’ perspectives on interorganizational care coordination: A qualitative analysis. Journal of Rural Health, 37(2), 417–425. 10.nn/jrh.12453. [DOI] [PubMed] [Google Scholar]
- Miller CJ, Li M, Penfold RB, Lee AF, Smith EG, Nordberg SS, Osser DN, Bajor L, Zhang F, & Bauer MS (2015). The ascendancy of second-generation antipsychotics as frontline antimanic agents. Journal of Clinical Psychopharmacology, 35(6), 645–653. 10.1097/JCP.0000000000000405 [DOI] [PubMed] [Google Scholar]
- Miller CJ, Li M, Penfold RB, Lee AF, Smith EG, Osser DN, Bajor L, & Bauer MS (2014). Patterns of initiation of second generation antipsychotics for bipolar disorder: A month-by-month analysis of provider behavior. BMC Psychiatry, 14, 339. 10.1186/s12888-014-0339-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller CJ, Shin M, Pugatch M, & Kim B (2021). Veteran perspectives on care coordination between Veterans Affairs and community providers: A qualitative analysis. Journal of Rural Health, 37(2), 437–446. 10.1111/jrh.12526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moret C, & Briley M (2006). Antidepressants in the treatment of fibromyalgia. Neuropsychiatric Disease and Treatment, 2(4), 537–548. 10.2147/nedt.2006.2.4.537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Bovin MJ, Kimerling R, Kaloupek DG, Marx BP, Pless Kaiser A, & Schnurr PP (2015). The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5). [Measurement instrument; ]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, Thrailkill A, Gusman FD, & Sheikh JI (2003). The Primary Care PTSD Screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry, 9(1), 9–14. [Google Scholar]
- Seal KH, Bertenthal D, Maguen S, Gima K, Chu A, & Marmar CR (2008). Getting beyond "Don't ask; don't tell": An evaluation of US Veterans Administration postdeployment mental health screening of veterans returning from Iraq and Afghanistan. American Journal of Public Health, 98(4), 714–720. 10.2105/AJPH.2007.115519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoont MR, Sayer NA, Kehle-Forbes SM, Meis LA, & Nelson DB (2017). A prospective study of racial and ethnic variation in VA psychotherapy services for PTSD. Psychiatric Services, 68(3), 231–237. 10.1176/appi.ps.201600086 [DOI] [PubMed] [Google Scholar]
- VA MISSION Act of 2018, Pub. L. No. 115-182, 132 Stat. 1393 (2018).https://uscode.house.gov/statutes/pl/115/182.pdf
- Veterans Health Administration. (2002). Post-traumatic stress disorder: Implications for primary care. Washington, DC: Department of Veterans Affairs. https://www.mirecc.va.gov/cih-visn2/Documents/Provider_Education_Handouts/PTSD_Implications_for_Primary_Care.pdf [Google Scholar]
- Veterans Health Administration. (2008). VHA Handbook 1160.01: Uniform mental health services in VA medical centers and clinics. Washington, DC: Department of Veterans Affairs. https://www.mentalhealth.va.gov/providers/sud/docs/UniformServicesHandbook1160-01.pdf [Google Scholar]
- Veterans Health Administration. (2017). VHA Directive 1160.03: Programs for veterans with posttraumatic stress disorder (PTSD). Washington, DC: Department of Veterans Affairs. Amended April 24, 2019. Retrieved from https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=5506 [Google Scholar]
- Yehuda R, Hoge CW, McFarlane AC, Vermetten E, Lanius RA, Nievergelt CM, Hobfoll SE, Koenen KC, Neylan TC, & Hyman SE (2015). Post-traumatic stress disorder. Nature Reviews Disease Primers, 1, 15057. 10.1038/nrdp.2015.57 [DOI] [PubMed] [Google Scholar]