Abstract
What is already known on this topic?
Pneumococcal diseases (PDs) are serious threats to child health. Although vaccination is one of the most effective ways to prevent these diseases, the pneumococcal vaccination coverage rate is still relatively low in China.
What is added by this report?
This study investigated the factors associated with 13-valent pneumococcal conjugate vaccine (PCV13) vaccine hesitancy in parents under an innovative immunization strategy. This study found that 29.7% of the participants hesitated to vaccinate their children against PCV13 and the main reasons for vaccine hesitancy were individual and group influences.
What are the implications for public health practice?
This study can provide scientific evidence for further improving children’s PCV13 vaccination rate and improving the prevention and control strategy for PDs.
Keywords: vaccine hesitancy, 13-valent pneumococcal conjugate vaccine, PCV13, influencing factors
Pneumococcal diseases (PDs) have become a serious public health problem worldwide. According to the latest research data released by the World Health Organization (WHO) in 2018, about 294,000 children under the age of 5 died from Streptococcus pneumonia (Spn) infection globally (1). WHO asserts that pneumococcal vaccination is the most cost-effective way to prevent pneumococcal diseases. The infrequent occurrence of adverse vaccine side effects, lack of understanding, and distribution of misinformation, however, have led to a decline in the public’s trust in vaccines in recent years, an increase in parents’ vaccine hesitancy, and even more vaccine hesitancy in non-national immunization programs (2). In China, the 13-valent pneumococcal conjugate vaccine (PCV13) was officially launched in 2020. Until now, no study has focused on PCV13 vaccine hesitancy in China. In 2021, the Government of Weifang City, Shandong Province, launched the first program in China to vaccinate registered children from 6 months to 2 years old with a free dose of domestic PCV13. Based on this innovative immunization strategy, we analyzed PCV13 vaccine hesitancy and influential factors for parents when making vaccine decisions for their children. The study found that 29.7% of participants were hesitant to vaccinate their children against PCV13. The most important reason for vaccine hesitancy is lack of knowledge about the vaccine.
Based on data from the children’s vaccination information management system in Weifang City, Shandong Province, this study calculated the birth population and the children being vaccinated in each vaccination clinic in 2021. By systematic sampling method, this study selected a total of 57 vaccination clinics from 12 counties as survey sites. All participants were surveyed after their informed consent. The sample size required for this survey was estimated according to the cross-sectional survey formula with an absolute tolerance error of d=3.0%. Considering that participants might reject the survey because their children were too young, the rejection rate was estimated to be 10.0%. Therefore, the final sample size was estimated to be 1,174. The specific calculation formula and the inclusion and exclusion criteria of participants are outlined in a previously published article (3).
After literature screening, research group discussions, and expert consultation, we designed the questionnaire. Pre-investigation was conducted prior to a formal investigation and all investigators were trained uniformly to the same standards. The investigators used the Pad that had been imported into the questionnaire to conduct the investigation. The questionnaire included six main aspects: sociodemographic characteristics of participants, participants’ perceptions of vaccine knowledge, knowledge of pneumonia and pneumococcal vaccine, willingness to receive pneumococcal vaccine, willingness to pay for pneumococcal vaccine, visiting behavior of children with pneumonia. It is important to note that if participants had multiple children, the study was aimed at the youngest child in the family.
SPSS (version 22.0; SPSS Inc., Chicago, IL, USA) was used to complete all data sorting, and classification variables were expressed in frequency (percentage). Chi-square test was used for comparison. Binary logistic regression model was used to analyze the related factors of pneumococcal vaccine hesitation. All statistical methods were adopted by the two-tailed test, and P<0.05 was considered statistically significant. To analyze the reasons for vaccine hesitancy, the WHO vaccine hesitancy determinants matrix was used for judgment (4), which mainly included three categories: contextual, individual and group, and vaccine/vaccination-specific influences.
A total of 1,195 questionnaires were collected in this survey, of which 1,110 were valid, with an effective questionnaire rate of 93.0%. Among the 1,110 participants, more than half were 31 to 40 years old (52.1%), 35.4% were fathers, 61.0% were mothers, and 3.5% were grandparents. Among the participants, 780 (70.2%) were willing to vaccinate their children against PCV13, 121 (10.8%) participants were not willing to vaccinate their children against PCV13, and 209 (18.8%) participants were not sure whether to vaccinate children against PCV13. Therefore, 70.2% of participants were identified as PCV13 vaccine recipients and 29.7% were identified as vaccine hesitators.
A total of 308 parents were unwilling to vaccinate their children against PCV13 due to individual and group influences, which accounted for the largest portion (Figure 1). As presented in Table 1, among the vaccine hesitators, 249 people did not know about the vaccine (A1), 92 people were uncertain about the vaccine’s effects (C2) and 84 people were uncertain about the safety of the vaccine (C3).
Figure 1.
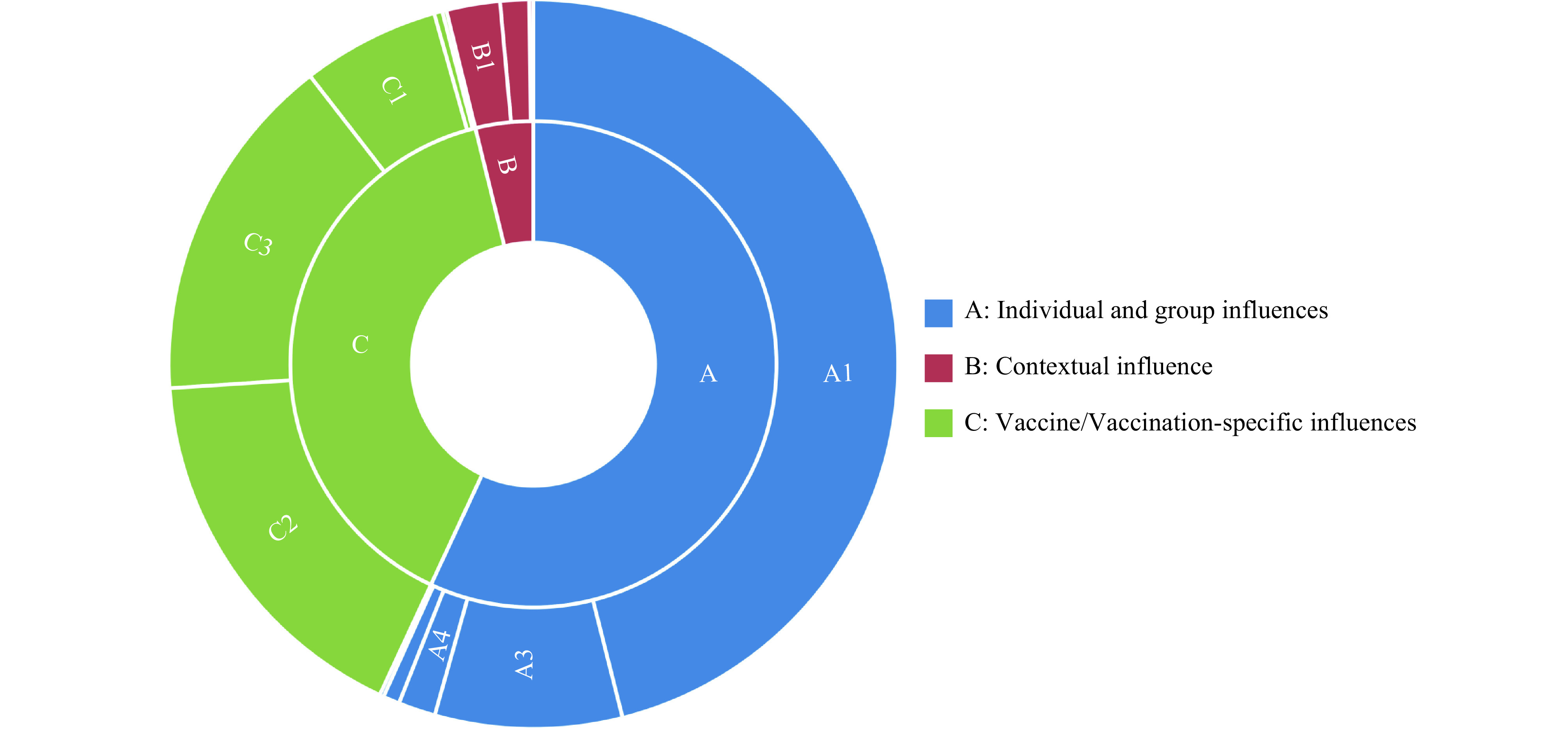
Reasons of hesitancy in 13-valent pneumococcal conjugate vaccines in Weifang, Shandong Province, China.
Table 1. Distribution of reasons for 13-valent pneumococcal conjugate vaccine hesitancy among study participants in Weifang City, Shandong Province, China.
| Reason | No. of participants | Proportion (%) |
| Note: The study used multiple-choice questions to analyze the reasons for vaccine hesitancy, so the sum of these three categories was not 100%. | ||
| A: Individual and group influences | ||
| A1: I don’t know much about 13-valent pneumococcal conjugate vaccine | 249 | 75.5 |
| A2: I don’t know where to get 13-valent pneumococcal conjugate vaccine | 1 | 0.3 |
| A3: The children are healthy and do not need the 13-valent pneumococcal conjugate vaccine | 45 | 13.6 |
| A4: Children with allergies or contraindications cannot receive the 13-valent pneumococcal conjugate vaccine | 9 | 2.7 |
| A5: Children were considered too young to receive the 13-valent pneumococcal conjugate vaccine | 4 | 1.2 |
| B: Contextual influences | ||
| B1: Participants’ work schedule or traveling distance from home to vaccination clinic prevent them from having their children receive the 13-valent pneumococcal conjugate vaccine | 13 | 3.9 |
| B2: Whether children should receive the 13-valent pneumococcal conjugate vaccine should be discussed with family members | 7 | 2.1 |
| B3: Participants are not willing to pay the vaccination fee on their own | 1 | 0.3 |
| C: Vaccine/vaccination-specific influences | ||
| C1: The 13-valent pneumococcal conjugate vaccine is expensive | 33 | 10.0 |
| C2: The efficacy of 13-valent pneumococcal conjugate vaccine is uncertain | 92 | 27.9 |
| C3: The safety of 13-valent pneumococcal conjugate vaccine is uncertain | 84 | 25.5 |
| C4: The 13-valent pneumococcal conjugate vaccine is not included in the immunization program | 2 | 0.6 |
| C5: The 13-valent pneumococcal conjugate vaccine is not mandatory | 1 | 0.3 |
As presented in Table 2, PCV13 vaccine hesitancy among participants who thought vaccination was important was significantly lower than among those who thought vaccination was not important (28.5% vs. 64.1%, P<0.001). PCV13 vaccine hesitancy among participants who were willing to pay for the PCV13 vaccine also was significantly lower than among those who were not willing to pay (19.6% vs. 55.6%, P<0.001). Participants who could clearly distinguish between the PCV13 vaccine and the COVID-19 vaccine were less hesitant toward the PCV13 vaccine (25.2% vs. 39.9%, P<0.001).
Table 2. Characteristics of 1,110 participants in the 13-valent pneumococcal conjugate vaccine hesitancy study in Weifang City, Shandong Province, China.
| Characteristic | N (%) | PCV13 vaccine hesitancy | χ 2 | P | ||||
| Yes | No | |||||||
| N | % | N | % | |||||
| Note: As defined by the World Health Organization, a question will be used in the study to assess participants’ hesitation about pneumococcal vaccine: “Would you be willing to vaccinate pneumococcal vaccine for your child?” The options are Yes, No, and Not Sure. If participants chose either of the latter two options, they were considered to have vaccine hesitancy. Abbreviation: PCV13=13-valent pneumococcal conjugate vaccine; CNY=Chinese Yuan. | ||||||||
| Relationship between participant and child | ||||||||
| Mother | 677 (60.9) | 198 | 29.2 | 479 | 70.8 | 1.499 | 0.473 | |
| Father | 394 (35.4) | 117 | 29.7 | 277 | 70.3 | |||
| Grandparent | 39 (3.5) | 15 | 38.5 | 24 | 61.5 | |||
| Participants’ medical education background | ||||||||
| Yes | 142 (12.7) | 38 | 26.8 | 104 | 73.2 | 0.687 | 0.407 | |
| No | 968 (87.2) | 292 | 30.2 | 676 | 69.8 | |||
| Participants’ age (years) | ||||||||
| ≤30 | 454 (40.9) | 115 | 25.3 | 339 | 74.7 | 7.655 | 0.022 | |
| 31–40 | 579 (52.1) | 187 | 32.3 | 392 | 67.7 | |||
| ≥41 | 77 (6.9) | 28 | 36.4 | 49 | 63.6 | |||
| Participants’ education level | ||||||||
| Elementary school and below | 23 (2.0) | 12 | 52.2 | 11 | 47.8 | 18.619 | 0.001 | |
| Junior high school | 256 (23.0) | 92 | 35.9 | 164 | 64.1 | |||
| High school/technical school/technical secondary school | 271 (24.4) | 88 | 32.5 | 183 | 67.5 | |||
| Junior college/bachelor’s degree | 529 (47.6) | 132 | 25.0 | 397 | 75.0 | |||
| Graduate degree | 31 (2.7) | 6 | 19.4 | 25 | 80.6 | |||
| Children’s gender | ||||||||
| Male | 585 (52.7) | 176 | 30.1 | 409 | 69.9 | 0.075 | 0.793 | |
| Female | 525 (47.2) | 154 | 29.3 | 371 | 70.7 | |||
| Type of family | ||||||||
| Single child family | 472 (42.5) | 121 | 25.6 | 351 | 74.4 | 6.589 | 0.012 | |
| Non-single child family | 638 (57.4) | 209 | 32.8 | 429 | 67.2 | |||
| Average annual family income (CNY) | ||||||||
| <50,000 | 207 (18.6) | 81 | 39.1 | 126 | 60.9 | 14.431 | 0.001 | |
| 50,000–150,000 (not contained) | 669 (60.2) | 196 | 29.3 | 473 | 70.7 | |||
| ≥150,000 | 234 (21.0) | 53 | 22.6 | 181 | 77.4 | |||
| Number of family members | ||||||||
| ≤3 | 232 (20.9) | 56 | 24.1 | 176 | 75.9 | 4.390 | 0.036 | |
| ≥4 | 878 (79.0) | 274 | 31.2 | 604 | 68.8 | |||
| Religious belief | ||||||||
| Conflict | 6 (0.5) | 1 | 16.7 | 5 | 83.3 | 0.493 | 0.676 | |
| No conflict | 1,104 (99.4) | 329 | 29.8 | 775 | 70.2 | |||
| High importance of vaccination | ||||||||
| Yes | 1,071 (96.4) | 305 | 28.5 | 766 | 71.5 | 22.859 | <0.001 | |
| No | 39 (3.5) | 25 | 64.1 | 14 | 35.9 | |||
| High safety of domestic vaccines | ||||||||
| Yes | 1,010 (90.9) | 298 | 29.5 | 712 | 70.5 | 0.271 | 0.647 | |
| No | 100 (9.0) | 32 | 32.0 | 68 | 68.0 | |||
| High safety of imported vaccines | ||||||||
| Yes | 559 (50.3) | 138 | 24.7 | 421 | 75.3 | 13.708 | <0.001 | |
| No | 551 (49.6) | 192 | 34.8 | 359 | 65.2 | |||
| High efficacy of domestic vaccines | ||||||||
| Yes | 1,005 (90.5) | 289 | 28.8 | 716 | 71.2 | 4.820 | 0.028 | |
| No | 105 (9.4) | 41 | 39.0 | 64 | 61.0 | |||
| High efficacy of imported vaccines | ||||||||
| Yes | 660 (59.4) | 163 | 24.7 | 497 | 75.3 | 19.738 | <0.001 | |
| No | 450 (40.5) | 167 | 37.1 | 283 | 62.9 | |||
| Trust in vaccine-related information provided by doctors or nurses | ||||||||
| Yes | 1,048 (94.4) | 301 | 28.7 | 747 | 71.3 | 9.132 | 0.003 | |
| No | 62 (5.5) | 29 | 46.8 | 33 | 53.2 | |||
| Willingness to take children for self-funded vaccinations | ||||||||
| Yes | 940 (84.6) | 234 | 24.9 | 706 | 75.1 | 68.712 | <0.001 | |
| No | 170 (15.3) | 96 | 56.5 | 74 | 43.5 | |||
| Attitudes to the degree of harm to children’s health caused by pneumonia | ||||||||
| Serious | 1,054 (94.9) | 300 | 28.5 | 754 | 71.5 | 19.041 | <0.001 | |
| General | 44 (3.9) | 26 | 59.1 | 18 | 40.9 | |||
| Light | 12 (1.0) | 4 | 33.3 | 8 | 66.7 | |||
| Risk of pneumonia in children | ||||||||
| Serious | 601 (54.1) | 138 | 23.0 | 463 | 77.0 | 33.350 | <0.001 | |
| General | 343 (30.8) | 119 | 34.7 | 224 | 65.3 | |||
| Light | 166(14.9) | 73 | 44.0 | 93 | 56.0 | |||
| Whether the pneumococcal vaccine is COVID-19 vaccine | ||||||||
| Yes or unknown | 343 (30.9) | 137 | 39.9 | 206 | 60.1 | 24.779 | <0.001 | |
| No | 767 (69.0) | 193 | 25.2 | 574 | 74.8 | |||
| Willingness to vaccinate your child with PCV13 if you pay your own expenses |
||||||||
| Yes | 799 (71.9) | 157 | 19.6 | 642 | 80.4 | 138.702 | <0.001 | |
| No | 311 (28.0) | 173 | 55.6 | 138 | 44.4 | |||
| Whether your children had pneumonia before | ||||||||
| Yes | 26 (2.3) | 6 | 23.1 | 20 | 76.9 | 0.560 | 0.454 | |
| No | 1,084 (97.6) | 324 | 29.9 | 760 | 70.1 | |||
The statistically significant variables in Table 2 were incorporated into the logistic multi-factor regression model for further analysis. As presented in Table 3, the participants who were not willing to pay for the PCV13 vaccine for their children [OR=3.85, 95% confidence interval (CI): 2.81–5.25)], who thought vaccination was not important (OR=3.54, 95% CI: 1.66–7.56), and who were not willing to pay for all self-funded vaccines (OR=1.98, 95% CI: 1.35–2.93) were more likely to be vaccine hesitant.
Table 3. Logistic regression analysis of children pneumococcal vaccine hesitancy in Weifang City, Shandong Province, China.
| Independent variables | Category | β |

|
Wald χ2 | P | OR (95% CI) |
| “–” means reference category. Abbreviation: OR=odds ratio; CI=confidence interval. | ||||||
| High importance of vaccination | Yes | − | ||||
| No | 1.265 | 0.387 | 10.692 | 0.001 | 3.542 (1.660–7.558) | |
| High efficacy of imported vaccines | Yes | − | ||||
| No | 0.346 | 0.149 | 5.403 | 0.020 | 1.413 (1.056–1.892) | |
| Willingness to take children for self-funded vaccinations | Yes | − | ||||
| No | 0.685 | 0.198 | 11.934 | 0.001 | 1.984 (1.345–2.927) | |
| Risk of pneumonia in children | Serious | − | ||||
| General | −0.218 | 0.216 | 1.025 | 0.311 | 0.804 (0.527–1.227) | |
| Light | −0.679 | 0.205 | 10.917 | 0.001 | 0.507 (0.339–0.759) | |
| Whether the pneumococcal vaccine is COVID-19 vaccine | Yes or Unknown | − | ||||
| No | −0.809 | 0.154 | 27.732 | <0.001 | 0.445 (0.329–0.602) | |
| Willingness to vaccinate your child with PCV13 if you pay your own expenses | Yes | − | ||||
| No | 1.346 | 0.159 | 71.795 | <0.001 | 3.842 (2.814–5.245) | |
DISCUSSION
This study found that 29.7% of participants hesitated to vaccinate their children against PCV13, which was lower than the vaccine hesitancy rates found in previous studies investigating varicella vaccine (51.2%), enterovirus 71 inactivated vaccine (33.8%), and HPV vaccine (37.2%) (5-7). This finding may be related to effective advertising of the innovative vaccination strategy of Weifang City, Shandong Province. The results showed that the main channels for participants to acquire information about PCV13 were community or hospital advocacy (45.2%), followed by the internet (36.8%), suggesting that participants may have a relatively high understanding of the vaccine due to these advertisements, thus leading to a relatively low degree of vaccine hesitation.
This study shows that the older the participants are, the more likely they are to be hesitant about vaccines, which is contrary to the results of a Swiss study (8). This may be related to China’s national conditions. The results also showed that participants with a lower cultural degree are more prone to be vaccine hesitant, which was consistent with the research results of Rosso (9) but was contrary to the research results of Van (10). This may be explained by China’s overall level of education. Participants with lower levels of education have fewer opportunities to learn about pneumococcal vaccines and related topics, which makes them more likely to become vaccine hesitant.
The survey also showed that participants were relatively hesitant to pay for the full pneumococcal vaccine fee by themselves. This can be explained by the fact that PCV13 is still a non-immunization program vaccine in China. Previous studies have also shown that non-programmed vaccines experience higher rates of hesitancy than programmed vaccines (11). Logistic regression showed that total self-expenditure was the risk factor for participants’ PCV13 vaccine hesitation, reflecting the importance of vaccine price in their decisions to vaccinate.
Globally, 2 to 3 million deaths from infectious diseases can be prevented by vaccination every year. Vaccination is the most cost-effective method for prevention and treatment of infectious diseases. In order to further reduce the burden of pneumococcal diseases in China and similar countries, it is suggested to take the following measures to improve the PCV13 vaccination rate in children:
Carry out multi-channel publicity and vaccine promotion campaigns to improve parental awareness and communicate the importance of PCV13 for children. This study showed that the most important reason for participants’ vaccine hesitancy was lack of knowledge about PCV13. Gilkey stated that medical workers can directly influence the vaccination information of children and parents, which can promote vaccination to some extent (12). Therefore, publicity channels can focus on medical workers, emphasize the standard training of medical workers, and provide information about the safety and effectiveness of PCV13 to vaccination groups. Secondly, internet platforms can be used to promote PCV13 and PCV13-related knowledge. Fundamental working units can also organize health education activities to make parents aware of the importance of vaccination, so as to further improve parents’ awareness of PCV13 and reduce vaccine hesitancy.
Standardize and optimize vaccine management regulations to enhance public confidence regarding the quality and safety of PCV13. In recent years, there have been many incidents of vaccine hesitancy. For example, parents’ trust in vaccines declined significantly after the illegal management of vaccines in Jinan in 2016 (13). Relevant departments should strictly obey the regulations of the Vaccine Administration Law of the People’s Republic of China, strictly supervise the production of vaccines in enterprises, and strengthen the management of all circulation links. It is suggested that government organizations will play an important role in PCV13 vaccination mobilization.
Build the appropriate financial support mechanisms in China to incentivize PCV13 vaccinations effectively and at scale. At present, the price of PCV13 in the Chinese vaccine market is relatively high, which leads to higher vaccine hesitancy (14). Therefore, local governments should provide appropriate financial support to reduce the burden of PCV13 vaccination costs for parents. Secondly, it is possible to include PCV13 vaccination costs in the resident medical insurance system and explore different payment modes to promote non-immunization program vaccines. The government can also get the best price for its citizens through centralized bidding processes. PDs have brought a heavy burden of disease to China. In order to solve this problem to the greatest extent, it is suggested to include PCV13 into the national immunization program as soon as possible.
Earlier in 2022, China CDC Weekly published an article which analyzed the factors associated with PCV13 vaccine willingness in parents (3). Although vaccine willingness and vaccine hesitancy are opposite concepts, they display similar factors. This study further discussed the reasons for participants’ concerns about vaccine safety suggested similar interventions to the previously published study. This study also discussed the appropriate financial support mechanisms for society. These two articles are synergistic and complementary.
This study is subject to some limitations. Firstly, this study is based on a cross-sectional survey, so it may not be representative of all of China. Secondly, this study only selected participants from Weifang City, so it needs to be cautious when extrapolating its conclusions to broader contexts. Given that PCV13 is a newly marketed vaccine in China, more epidemiological studies investigating the surveillance of pneumococcal disease risks among pediatric, adult, and elderly populations are required to evaluate the immunization efficacy of PCV13. In addition, safety monitoring of this vaccine is recommended.
Funding Statement
Supported by Education Foundation of Peking Union Medical College (WH10022021145) and Bill & Melinda Gates Foundation (OPP1216666)
Contributor Information
Jian Zhou, Email: sdwfcdc106@163.com.
Chunping Wang, Email: chpwang@163.com.
Luzhao Feng, Email: fengluzhao@cams.cn.
References
- 1.Wahl B, O’Brien KL, Greenbaum A, Majumder A, Liu L, Chu Y, et al Burden of streptococcus pneumoniae and haemophilus influenzae type b disease in children in the era of conjugate vaccines: global, regional, and national estimates for 2000-15. Lancet Glob Health. 2018;6(7):e744–57. doi: 10.1016/S2214-109X(18)30247-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu S, Fang Y, Chang J, Yu JL, Zhang Y, Ji WJ, et al. Investigation on parents’ confidence and influencing factors of children’s vaccination in Xi’an. In: 2018 Chinese pharmaceutical association pharmaceutical administration professional committee annual meeting and academic symposium proceedings. Ji’nan: Chinese Pharmaceutical Association. 2018; p. 818-27. https://d.wanfangdata.com.cn/conference/ChZDb25mZXJlbmNlTmV3UzIwMjIxMTE3EggxMDIwODQ1MhoINm92ZWlpMXY%3D. (In Chinese).
- 3.Yang Y, Zhang T, Wang Y, Ma LB, Xie SY, Zhou J, et al Willingness of caregivers to have their children vaccinated with pneumococcal vaccines in the context of an innovative immunization strategy — Weifang City, Shandong Province, 2021. China CDC Wkly. 2022;4(20):421–5. doi: 10.46234/ccdcw2022.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MacDonald NE, SAGE Working Group on Vaccine Hesitancy Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 5.Liu HY, Zhao TS, Han BF, Du J, Liu YQ, Liu B, et al A survey of hesitancy of parents to vaccinate children with varicella vaccine in selected areas in 2019. Chin J Vaccines Immun. 2021;27(3):302–6. doi: 10.19914/j.CJVI.2021056. [DOI] [Google Scholar]
- 6.Tang ZM, Yu WZ, Liu YM, Feng ZJ. Parental hesitancy to use inactivated enterovirus 71 vaccine and factors influencing hesitancy. Chin J Vaccines Immun 2018;24(3):334 − 8. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjIxMTE1Eg96Z2pobXkyMDE4MDMwMTYaCHJpZ3E1eGl4. (In Chinese).
- 7.Xu XF, Yin WQ, Liu M, Li QS, Song YN, Yang CX, et al. The status and influencing factors of mother's HPV vaccine hesitation. Mod Prev Med 2020;47(19):3509-12. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjIxMTE1Eg94ZHlmeXgyMDIwMTkwMTUaCGRndm91aWE3. (In Chinese).
- 8.Weiss C, Schröpfer D, Merten S Parental attitudes towards measles vaccination in the canton of Aargau, Switzerland: a latent class analysis. BMC Infect Dis. 2016;16(1):400. doi: 10.1186/s12879-016-1747-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosso A, Massimi A, De Vito C, Adamo G, Baccolini V, Marzuillo C, et al Knowledge and attitudes on pediatric vaccinations and intention to vaccinate in a sample of pregnant women from the City of Rome. Vaccine. 2019;37(14):1954–63. doi: 10.1016/j.vaccine.2019.02.049. [DOI] [PubMed] [Google Scholar]
- 10.Van Lier A, Tostmann A, Harmsen IA, De Melker HE, Hautvast JLA, Ruijs WLM Negative attitude and low intention to vaccinate universally against varicella among public health professionals and parents in the Netherlands: two internet surveys. BMC Infect Dis. 2016;16:127. doi: 10.1186/s12879-016-1442-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yuen WWY, Lee A, Chan PKS, Tran L, Sayko E Uptake of human papillomavirus (HPV) vaccination in Hong Kong: facilitators and barriers among adolescent girls and their parents. PLoS One. 2018;13(3):e0194159. doi: 10.1371/journal.pone.0194159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Učakar V, Fafangel M, Kraigher A Vaccine confidence among mothers of young children, Slovenia, 2016. Vaccine. 2018;36(37):5544–50. doi: 10.1016/j.vaccine.2018.07.062. [DOI] [PubMed] [Google Scholar]
- 13.Qiu J, Hu HJ, Zhou SH, Liu QM Vaccine scandal and crisis in public confidence in China. Lancet. 2016;387(10036):2382. doi: 10.1016/S0140-6736(16)30737-1. [DOI] [PubMed] [Google Scholar]
- 14.Azizi FSM, Kew Y, Moy FM Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine. 2017;35(22):2955–61. doi: 10.1016/j.vaccine.2017.04.010. [DOI] [PubMed] [Google Scholar]


