Abstract
This is a case report of a 69-year-old Japanese man who has been undergoing treatment for primary Sjögren’s syndrome (pSS) since he was 62 years. A renal biopsy, which revealed diffuse and severe mononuclear cell infiltration in the tubulointerstitium, was performed because of progressive renal dysfunction. Immunostaining demonstrated most of the infiltrating cells to be IgA, kappa, CD38, and CD138 positive. Immunofixation blood test revealed IgA kappa-type M protein; however, bone marrow abnormalities or lymph node enlargements on examination or imaging, respectively, were not observed. Tubulointerstitial nephritis caused by monotypic plasmacytic infiltration in pSS, accompanied with a monoclonal gammopathy of undetermined significance (MGUS), was diagnosed. A treatment of prednisolone 40 mg/day was initiated, promptly improving the patient’s serum creatinine levels from 3.0 to 1.5 mg/dl. The infiltrating cells in pSS-associated tubulointerstitial nephritis are generally polytypic plasmacytes and lymphocytes, but in the present case, monotypic plasmacytes were predominant. This case is remarkable and rare and can be considered a complication of pSS or MGUS. Since it may become a new disease entity, it is important to accumulate similar cases.
Keywords: Tubulointerstitial nephritis, Monoclonal gammopathy of undetermined significance, IgA paraproteinemia, Primary Sjögren’s syndrome
Introduction
Sjögren’s syndrome is an autoimmune disease characterized by lymphocytic infiltration in the exocrine glands, such as the salivary and lacrimal glands. Organs other than the exocrine glands are often affected, but renal impairment is rare, occurring in 5% of cases [1]. The most common form of renal impairment is tubulointerstitial nephritis, which is characterized by polytypic plasmacytes and lymphocytes infiltrating the interstitium [2].
Herein, we report a case of acute kidney injury resulting from tubulointerstitial nephritis caused by an IgA kappa-type monoclonal gammopathy of undetermined significance (MGUS) with IgA kappa-positive monotypic plasmacytic infiltration during Sjögren’s syndrome.
Case report
A 69-year-old man was diagnosed with primary Sjögren’s syndrome 7 years ago because he experienced mouth dryness, decreased salivary secretion, positivity for anti-SS-A and anti-SS-B antibodies, which met the 2002 American–European Consensus Group Criteria for this disease [3]. He was referred because of the progression of his renal function impairment, indicated by the serum creatinine (Cr) levels of 1.0 mg/dl 1 year prior, 2.1 mg/dl 3 months prior, and 2.4 mg/dl 1 month prior to his admission. At admission, his height was 172.5 cm, weight 54.5 kg, body temperature 36.3 °C, and blood pressure 105/66 mmHg. No abnormal physical findings were observed other than mouth dryness.
Urinalysis showed normal urine protein levels (0.1 g/day), with no occult blood or urinary glucose. However, urinary beta 2-microglobulin and N-acetyl-beta-glucosaminidase levels were abnormally high at 4360 μg/L and 12.2 U/L, respectively. The laboratory findings were as follows: hemoglobin, 10.9 g/dl, white blood cells, 6390/μl, platelets, 230,000/μl, serum Cr, 2.39 mg/dl (normal range: 0.40–0.80), estimated glomerular filtration rate, 22.0 ml/min/1.732, and blood urea nitrogen, 37.0 mg/dl (8.0–22.0). Serum electrolyte and liver function tests were normal. The other laboratory findings included serum C-reactive protein, 0.17 mg/dl, serum total protein, 9.5 mg/dl, albumin, 3.5 g/dl, IgG, 2117 mg/dl (870–1700), IgA, 2653 mg/dl (110–410), IgM, 51 mg/dl (57–288), serum CH50 68 U/ml (32–58), free kappa light chain, 419 mg/l (2.42–18.92), lambda, 78.4 mg/l (4.44–26.18), and kappa/lambda ratio, 8.9 (0.244–1.804). Blood gas analysis revealed no metabolic acidosis (pH 7.32 and HCO3: 24.1 mmol/l). Serum immunoelectrophoresis showed the presence of IgA kappa-type M protein. On examination, no increase in plasmacytes (0.4%) was found in normocellular bone marrow. Whole-body computed tomography scans did not reveal enlarged lymph nodes, lytic bone lesions, or tumors.
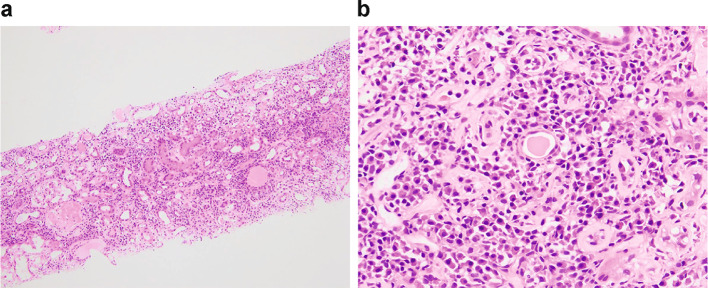
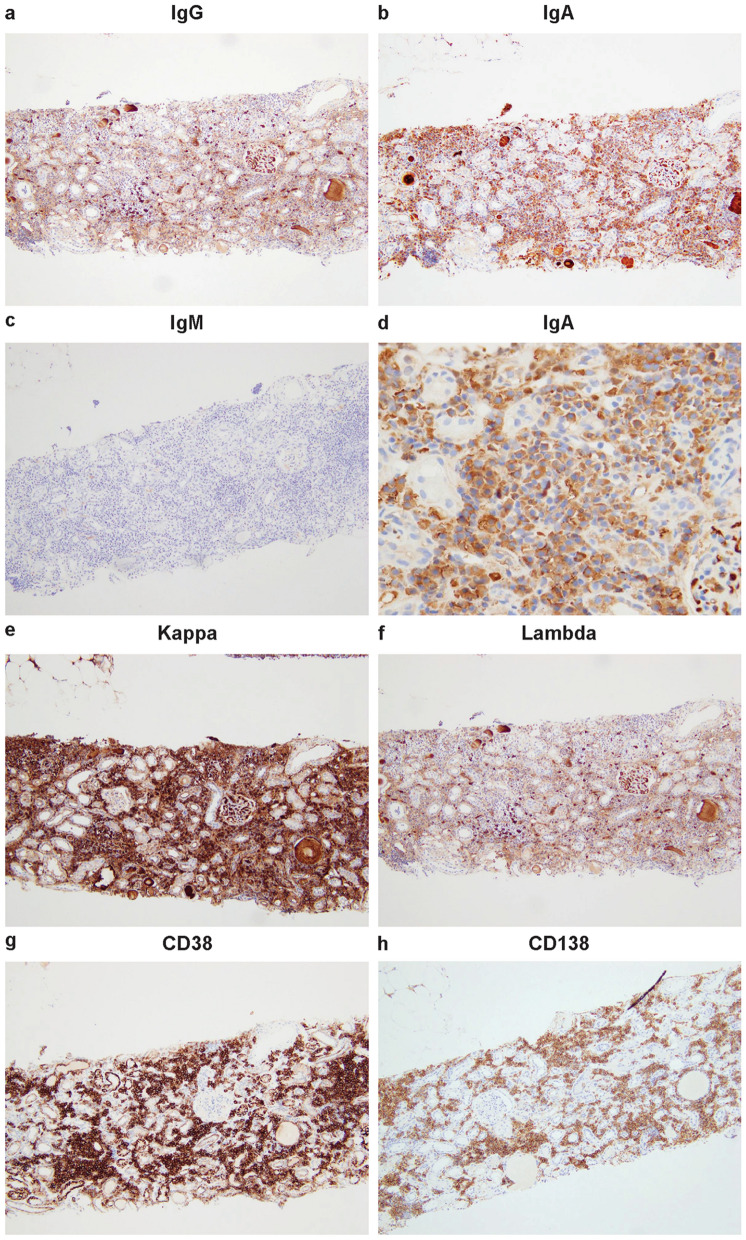
Severe and diffuse mononuclear cell infiltration was found in the interstitium on renal biopsy (Fig. 1a, b). A total of 14 out of 30 glomeruli had global sclerosis, with the remaining glomeruli showing minimal changes. On immunostaining, most of the infiltrating cells were observed to be IgA and kappa positive. The number of IgG-positive plasmacytes was small (Fig. 2a–f). The cells were negative for IgG4. Most of the infiltrating cells were positive for CD38 and CD138 (Fig. 2g, h). Immunofluorescence revealed that immunoglobulins, complements, and light chains were not deposited in the glomeruli and tubules. Electron microscopy did not find higher electron density or crystal deposits in the glomeruli or tubules. Based on these findings, the patient was diagnosed with interstitial nephritis caused by IgA kappa-positive plasmacytic infiltration.
Fig. 1.
Light microscopy image of the patient’s kidney biopsy specimen. (hematoxylin and eosin; a × 100, b × 400)
Fig. 2.
Immunohistochemical staining for IgG (a), IgA (b, d), IgM (c), kappa (e), lambda (f), CD138 (g), and CD38 (h) of renal biopsies (a, b, c, e, f, g × 200, d × 400)
Treatment was started with prednisolone 40 mg/day. The serum Cr levels improved rapidly from 3.0 mg/dl at the start of the treatment to 1.5 mg/dl within 2 days. Six months after treatment initiation, the maintenance prednisolone dose was 5 mg/day, and the serum Cr levels remained at 1.5 mg/dl.
Discussion
A patient with a 7-year history of Sjögren’s syndrome demonstrated a gradual deterioration of renal function and underwent a detailed investigation of the cause. As a result, interstitial nephritis caused by IgA kappa-type MGUS and IgA kappa-positive plasmacytic infiltration was diagnosed. The most common form of renal impairment in Sjögren’s syndrome is interstitial nephritis, and the infiltrating cells have been identified as polytypic plasmacytes and lymphocytes [2]. Interstitial nephritis associated with Sjögren’s syndrome clinically presents with mildly elevated serum Cr levels, which may be associated with tubular functional abnormalities, such as Fanconi syndrome, distal tubular acidosis, and nephrogenic diabetes insipidus. No electrolyte abnormalities were observed in this case, and the blood gas analysis displayed normal results.
The close relationship between primary Sjögren’s syndrome (pSS) and monoclonal gammopathies has been elucidated in recent studies. Although 20% of pSS cases are accompanied with MGUS, the IgA type, as in this case, is very rare, accounting for only 10% of cases [4]. At the 2017 International Kidney and Monoclonal Gammopathy Research Group meeting, the definition of monoclonal gammopathy of renal significance (MGRS) was updated to include any plasmacytic and B cell lymphoproliferative disorders with at least one M-protein-associated renal lesion that neither produces a tumor nor meets hematological treatment criteria [5]. Most MGRS are caused by monoclonal immunoglobulin deposition. In the glomeruli, organized deposits are found in light-chain amyloidosis and cryoglobulin nephropathy, whereas non-organized deposits are found in monoclonal immunoglobulin deposition disease (MIDD). Light-chain proximal tubulopathy (LCPT) and MIDD are tubular disorders in MGRS, with basement membrane deposits in LCPT and intracytoplasmic deposits in MIDD. Although no evidence of immunoglobulin deposition in the glomeruli or tubules was found, this case meets the definition of MGRS. In the future, it may be considered as an MGRS disease.
Tubulointerstitial nephritis is occasionally accompanied with monoclonal gammopathy; however, in most cases, its etiology is monoclonal light chains, and the infiltrating cells are not monotypic [6]. Attias et al. [7] reported a rare case of a patient who experienced monotypic plasma cell interstitial nephritis caused by IgG kappa-type MGUS. However, unlike our case, the infiltrating cells were CD138 positive and atypical, with apparently multinucleated malignant cells.
There have been four reports of interstitial nephritis caused by monotypic plasmacytic infiltration in Sjögren’s syndrome accompanied with MGUS (Table 1). In 2006, Kobayashi et al. [8] reported a 49-year-old woman hospitalized with hypokalemia and impaired renal function diagnosed with interstitial nephritis accompanied with Fanconi syndrome and type 1 distal tubular acidosis. The interstitium infiltrating cells were IgA kappa-positive. Her renal function improved rapidly (serum Cr levels changed from 1.29 to 0.91 mg/dl) with steroid monotherapy (prednisolone 30 mg daily). In 2017, Saglam et al. [9] reported two cases. One of the patients was a 68-year-old man whose serum monoclonal paraprotein was IgA lambda. The serum Cr level was 2.2 mg/dl, and renal biopsy revealed interstitial nephritis caused by IgA lambda-positive plasmacytic infiltration. The other patient was a 69-year-old woman whose serum monoclonal paraprotein was IgA kappa. The serum Cr level was 2.3 mg/dl, and renal biopsy revealed interstitial nephritis caused by IgA kappa-positive plasmacytes. They received chemotherapy (melphalan–prednisolone for the former and bortezomib–dexamethasone for the latter). Their renal function improved to a Cr level of 1.8 mg/dl for the former and 1.1 mg/dl for the latter. In 2019, Saeki et al. [10] reported the case of a 74-year-old woman whose renal biopsy revealed IgA kappa-positive plasmacytic infiltration in the tubular interstitium. Immunostaining of the infiltrating cell was positive for CD38, CD138, CD19, and CD45 in normal plasma cells. However, it was negative for CD19 and CD45 (although it remained positive for CD38 and CD138) in myeloma cells (i.e., when plasma cells became cancerous). Saeki et al. reported that their case was unique because such findings (i.e., infiltrating cells positive for CD38, CD138, CD19, and CD45) are consistent with those of infiltrating cells, rather than myeloma cells, in patients with lymphoplasmacytic lymphoma/primary macroglobulinemia [10]. This patient was also treated with steroid monotherapy (prednisolone 40 mg daily) and her renal function quickly recovered from a serum Cr level of 1.2–0.9 mg/dl. The five cases, including our case, had three common characteristics: (1) mild decline in renal function, (2) good response to treatment and (3) IgA paraprotein. In patients with Sjögren’s syndrome, chronic stimulation of B cells causes infiltration of plasma cells and lymphocytes into the tubular and interstitium, resulting in the onset of interstitial nephritis. A unique interstitial nephritis may develop when Sjögren's syndrome is accompanied by IgA paraprotein-MGUS.
Table 1.
Summary of our case and other cases
| References | Sex/age (years) | History of SS | Clinical presentation | s-Cr (mg/dL) | Paraprotein | Treatment | s-Cr (after the treatment) (mg/dL) | Renal biopsy | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Saglam et al. [9] | F/68 | N.A | AKI | 2.2 | IgA-λ | Melphalan prednisolone | 1.8 | Diffuse TIN |
| 2 | Saglam et al. [9] | M/69 | 15 years | AKI | 2.3 | IgA-κ | Bortezomib dexamethasone | 1.1 | Diffuse TIN |
| 3 | Kobayashi et al. [8] | F/49 | 7 years |
AKI FS RTA |
1.29 | IgA-κ | Prednisolone | 0.91 | Diffuse TIN |
| 4 | Saeki et al. [10] | F/74 | 16 years | AKI | 1.2 | IgA-κ | Prednisolone | 0.95 | Diffuse TIN |
| 5 | Our case | M/69 | 7 years | AKI | 3.02 | IgA-κ | Prednisolone | 1.5 | Diffuse TIN |
F female, M male, N.A not available, SS Sjögren syndrome, s-Cr serum creatinine, AKI acute kidney injury, FS Fanconi’s syndrome, RTA renal tubular acidosis, TIN tubulointerstitial nephritis
In summary, we presented a case of tubulointerstitial nephritis caused by IgA-type MGUS and IgA kappa-positive monotypic plasmacytic infiltration during pSS. This case is very rare and remarkable and can be considered either a complication of Sjögren’s syndrome or MGUS. Since it may be considered a new disease entity, accumulating similar cases is essential.
Declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study to publish the information that appears in this case report.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Aiyegbusi O, McGregor L, McGeoch L, Kipgen D, Geddes CC, Stevens KI. Renal disease in primary Sjögren’s syndrome. Rheumatol Ther. 2021;8:63–80. doi: 10.1007/s40744-020-00264-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.François H, Mariette X. Renal involvement in primary Sjögren syndrome. Nat Rev Nephrol. 2016;12:82–93. doi: 10.1038/nrneph.2015.174. [DOI] [PubMed] [Google Scholar]
- 3.Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, Daniels TE, Fox PC, Fox RI, Kassan SS, Pillemer SR, Talal N, Weisman MH. European study group on classification criteria for Sjögren’s syndrome. Ann Rheum Dis. 2002;61(6):554–558. doi: 10.1136/ard.61.6.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brito-Zerón P, Ramos-Casals M, Nardi N, Cervera R, Yague J, Ingelmo M, Font J. Circulating monoclonal immunoglobulins in Sjögren syndrome: prevalence and clinical significance in 237 patients. Med (Baltim) 2005;84:90–97. doi: 10.1097/01.md.0000157398.37679.47. [DOI] [PubMed] [Google Scholar]
- 5.Leung N, Bridoux F, Batuman V, Chaidos A, Cockwell P, D’Agati VD, Dispenzieri A, Fervenza FC, Fermand JP, Gibbs S, Gillmore JD. The evaluation of monoclonal gammopathy of renal significance: a consensus report of the international kidney and monoclonal gammopathy research group. Nat Rev Nephrol. 2019;15:45–59. doi: 10.1038/s41581-018-0077-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Herrera GA, Picken MM. Renal disease associated with plasma cell dyscrasias, amyloidosis, and Waldenstrom macroglobulinemia. In: Jannette JC, Olson JL, Silva FG, D’agati VD, editors. Heptinstall’s pathology of the kidney. 7. Philadelphia: Wolters Kluwer; 2015. pp. 951–1014. [Google Scholar]
- 7.Attias P, Moktefi A, Matignon M, Dupuis J, Debiais-Delpech C, Grimbert P, Lang P, Audard V. Monotypic plasma cell interstitial nephritis as the only clinical manifestation in a patient with previously undiagnosed indolent multiple myeloma: a case report. Med (Baltim) 2016;95:e4391. doi: 10.1097/MD.0000000000004391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kobayashi T, Muto S, Nemoto J, Miyata Y, Ishiharajima S, Hironaka M, Asano Y, Kusano E. Fanconi’s syndrome and distal (type 1) renal tubular acidosis in a patient with primary Sjögren’s syndrome with monoclonal gammopathy of undetermined significance. Clin Nephrol. 2006;65:427–432. doi: 10.5414/CNP65427. [DOI] [PubMed] [Google Scholar]
- 9.Saglam A, Balaban S, Yıldırım T, Erdem Y, Uner A, Büyükaşık Y. Monoclonal gammopathy of renal significance presenting as monotypic plasma cell interstitial nephritis in two patients with Sjögren’s syndrome. Virchows Arch. 2018;472:865–869. doi: 10.1007/s00428-017-2270-4. [DOI] [PubMed] [Google Scholar]
- 10.Saeki T, Kuroha T, Sato Y, Tamura M, Iguchi A, Ito T, Yamazaki H, Ito Y, Yoshita K, Imai N, Narita I, Usuda H. Tubulointerstitial nephritis with monotypic lympho-plasmacytic infiltrates in a patient with primary Sjogren's syndrome accompanied by IgA-type monoclonal gammopathy. BMC Nephrol. 2019;20:464. doi: 10.1186/s12882-019-1646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]