Abstract
Objective
To understand the attitudes towards COVID-19 vaccination and trusted sources of vaccination-related information among persons incarcerated in the Federal Bureau of Prisons.
Methods
From June-July 2021, persons incarcerated across 122 facilities operated by the Federal Bureau of Prisons were invited to participate in a survey asking their reasons for receiving or declining COVID-19 vaccination and the information sources they relied upon to make these decisions. Descriptive analyses were conducted.
Results
A total of 130,789 incarcerated persons with known vaccination status were invited to participate in the survey. At the time of survey, 78,496 (62%) were fully vaccinated; 3,128 (3%) were partially vaccinated and scheduled to complete their second dose, and 44,394 (35%) had declined either a first or second dose. 7,474 (9.5%) of the fully vaccinated group and 2,302 (4.4%) of the group declining either a first or second dose chose to participate in the survey; an overall survey return rate of 7.6% (n = 9,905). Among vaccinated respondents, the most common reason given for accepting vaccination was to protect their health (n = 5,689; 76.1%). Individuals who declined vaccination cited concerns about vaccine side effects (n = 1,304; 56.6%), mistrust of the vaccine (n = 1,256; 54.6%), and vaccine safety concerns (n = 1,252; 54.4%). Among those who declined, 21.2% (n = 489) reported that they would choose to be vaccinated if the vaccine was offered again. Those who declined also reported that additional information from outside organizations (n = 1128; 49.0%), receiving information regarding vaccine safety (n = 841; 36.5%), and/or speaking with a trusted medical advisor (n = 565; 24.5%) may influence their decision to be vaccinated in the future.
Conclusion
As the COVID-19 pandemic continues, it is important to increase vaccine confidence in prisons, jails, and detention facilities to reduce transmission and severe health outcomes. These survey findings can inform the design of potential interventions to increase COVID-19 vaccine uptake in these settings.
Keywords: COVID-19 vaccination, Attitudes, Trusted sources, Federal Bureau of Prisons, SARS-CoV-2
1. Introduction
Correctional and detention facilities are high-risk environments for COVID-19 infection and mortality [1], [2]. Space limitations, dense housing arrangements, widespread staff movement, and sanitation concerns in some facilities have made infection prevention and control measures challenging to implement in these settings [3], [4], [5]. In addition, receipt of vaccinations for individuals who are incarcerated in federal correctional facilities are not required. Given the significant risk of COVID-19 transmission among people who are incarcerated, and the high prevalence of underlying medical conditions associated with severe COVID-19 [6], achieving high vaccine coverage remains a vital strategy to reduce COVID-19-related morbidity and mortality [7], [8]. Despite robust evidence showing that COVID-19 vaccines are safe and effective, vaccination rates have continued to lag in some correctional and detention facilities [9], [10], [11].
To understand the barriers to COVID-19 vaccine uptake in correctional settings, various studies have explored the demographic factors and attitudinal barriers associated with vaccine hesitancy and acceptance among incarcerated persons. One of the earliest studies, conducted before the FDA issued an emergency use authorization for COVID-19 vaccines, found that willingness to be vaccinated was lower among incarcerated persons who were younger, identified as Black/African American, or lived in jails (as opposed to prisons) [12]. Similar findings have been reported across state correctional facilities and federal prisons, with significant differences in COVID-19 vaccine acceptance along various demographic characteristics including age, gender/sex, and race/ethnicity [13], [14]. Additionally, having fewer underlying medical conditions or a lower perceived risk of severe COVID-19 were associated with lower vaccination acceptance in correctional settings [12], [14], findings similar to attitudes of unvaccinated adults in the general population [15].
Reasons for COVID-19 vaccine refusals in correctional facilities are multifaceted, including distrust of prison staff, including health care providers [16], and vaccine safety and efficacy concerns [17], [18], [19]. Some studies have found that tailored communication using trusted messengers and providing extensive education that is culturally relevant and appropriate for various health literacy levels have the potential to increase vaccine acceptance among both correctional residents and staff [20]; these strategies have been effective in other high-risk congregate settings as well [21]. Other reports have underscored that the impact of intervention efforts to increase vaccine coverage may be limited if they do not involve efforts to improve trust [18], limit misinformation [19], and offer incentives for vaccination [22].
The Federal Bureau of Prisons (BOP) is uniquely positioned to examine questions surrounding vaccine intentions due to its wide geographic representation, large sample size, and the variety of institution types (e.g., security levels, level of care). BOP’s COVID-19 vaccine guidance also provided uniform direction to its facilities on eligibility for, and administration of, COVID-19 vaccines [23]. We invited all persons incarcerated in BOP facilities whose vaccination status was known (130,789 persons across 122 institutions) to participate in a survey asking their reasons for receiving or declining COVID-19 vaccination and their trusted sources of vaccine-related information. Survey responses were examined based on vaccination status, selected demographic factors, and geographical region.
2. Methods
The BOP includes 122 total institutions, including 3,870 privately managed facilities. At the time of the survey, these 122 institutions housed 139,533 people. To assess attitudes related to COVID-19 vaccination, between June 7, 2021 through June 11, 2021, BOP staff (e.g., unit counselors, unit managers, case managers) invited 130,789 persons who are incarcerated in a BOP-managed institution to participate in a survey asking their reasons for receiving or declining vaccination and the sources of vaccine-related information they trust. Depending on vaccination status, respondents received a survey link to complete a survey for respondents fully vaccinated or for respondents who declined either a first or a second dose. The link was shared on the homepage of the email system utilized by incarcerated individuals. Paper surveys were provided for those, who for security reasons, did not have computer access. Participants that received vaccination signed a consent form which included the most common side effects listed by the manufacture and also were provided the patient/caregiver EUA. Surveys were available in both English and Spanish.
Fully vaccinated respondents were asked the following two questions (for response options see Table 2 ): 1. Select all the reasons why you chose to receive the vaccine, and 2. Select all the sources of information that you relied on in making your decision. Respondents who declined a vaccine were asked the following four questions (for response options see Table 3 ): 1. Select the reasons you chose not to receive the vaccine; 2. Select all of the sources of information that you relied on in making your decision; 3. What additional factor(s) may change your mind to take the vaccine? and; 4. If you were offered the vaccine now, would you take it? Respondents who completed either of the surveys were included in the final analysis.
Table 2.
Trusted Sources of Vaccine-related Information and Reasons for Choosing to Receive the COVID-19 Vaccine among Fully Vaccinated Incarcerated Persons, Federal Bureau of Prisons, June 2021–July 2021.a
|
Fullyvaccinatedrespondents (n = 7,473) n (%) |
|
|---|---|
| Please select all of the sources of information that you relied on in making your decision to receive a COVID-19 vaccine | |
| (Participants could select all that apply) | |
| Family members/Friends | 4056 (54.3%) |
| TV (such as news) | 3754 (50.2%) |
| Health services staff | 2333 (31.2%) |
| Other inmates | 1235 (16.5%) |
| Executive staff | 735 (9.8%) |
| Other staff | 701 (9.4%) |
| Religious services staff (Chaplains) | 190 (2.5%) |
| Otherb | 2223 (29.7%) |
| Please select the reasons you chose to receive the vaccine: | |
| (Participants could select all that apply) | |
| I wanted to protect myself from getting COVID-19 | 5689 (76.1%) |
| Seemed like a good thing to do | 3381 (45.2%) |
| My family advised me to take it | 1627 (21.8%) |
| I believe it will increase my chances of early release/home confinement | 1577 (21.1%) |
| Others have taken it and are OK | 1529 (20.5%) |
| I am either going home or to a Residential Re-entry Center soon and wanted to protect my family | 1436 (19.2%) |
| I believe it will increase my chances of being transferred to another place | 1231 (16.5%) |
| I took it after my healthcare provider answered all my questions | 599 (8.0%) |
| My cell mates advised me to take it | 315 (4.2%) |
| Other | 1678 (22.5%) |
Percentages may not add up to 100 due to rounding, and because of missingness if participants opted to skip a question.
Survey does not specify ‘Other’.
Table 3.
Trusted Sources of Vaccine-related Information and Reasons for Choosing to Decline the COVID-19 Vaccine among Incarcerated Persons who Declined Vaccination, Federal Bureau of Prisons, June 2021–July 2021.a
|
Respondents who declined a first or second vaccine dose (n = 2,302) n (%) |
|
|---|---|
| Please select all of the sources of information that you relied on in making your decision not to receive a COVID-19 vaccine | |
| (Participants could select all that apply) | |
| Family members/Friends | 1150 (50.0%) |
| TV (such as news) | 1094 (47.5%) |
| Otherb | 1075 (46.7%) |
| Health services staff | 719 (31.2%) |
| Other inmates | 375 (16.3%) |
| Executive staffb | 369 (16.0%) |
| Other staffc | 362 (15.7%) |
| Religious services staff (Chaplains) | 124 (5.4%) |
| Please select the reasons you chose not to receive the vaccine: | |
| (Participants could select all that apply) | |
| I am worried about vaccine side effects | 1304 (56.6%) |
| I do not trust the vaccine | 1256 (54.6%) |
| I have vaccine safety concerns | 1252 (54.4%) |
| Not know enough info on the vaccine | 1019 (44.3%) |
| I had COVID-19 and do not need vaccine | 534 (23.2%) |
| I do not see a benefit to taking the vaccine | 501 (21.8%) |
| I am healthy and do not need to be vaccinated | 390 (16.9%) |
| I do not believe COVID-19 is a problem | 221 (9.6%) |
| Decrease chances of early release/home confinement | 143 (6.2%) |
| I want a different COVID-19 vaccine | 110 (4.8%) |
| Do not want to affect chances of being transferred | 77 (3.3%) |
| Vaccine was not offered to me | 30 (1.3%) |
| Other | 580 (25.2%) |
| What additional factor(s) may change your mind to take the vaccine? | |
| (Participants could select all that apply) | |
| More information from outside organizationsd | 1128 (49.0%) |
| More information on vaccine safety | 841 (36.5%) |
| Additional info for those previously infected | 588 (25.5%) |
| Speaking with a trusted medical advisor | 565 (24.5%) |
| Speaking with my family or friends | 453 (19.7%) |
| Knowing that vaccine is still available | 185 (8.0%) |
| Other | 832 (36.1%) |
| Vaccine is still available- if you were offered the vaccine now, would you take it? | |
| No | 1801 (78.2%) |
| Yes | 489 (21.2%) |
Percentages may not add up to 100 due to rounding, and because of missingness if participants opted to skip a question.
Survey does not specify ‘Other’.
Other staff (e.g., Teachers, Correctional Officers, Counselors, Unit Managers, Detail Supervisors).
Outside sources include United States government agencies (e.g., Centers for Disease Control and Prevention, Food and Drug Administration), religious organizations, or community groups.
3. Analysis
BOP collaborated with staff from the Centers for Disease Control and Prevention (CDC) to analyze the survey data. CDC staff conducted descriptive analyses, stratified by vaccination status and demographic factors, including age, sex, race, and region. Excluded from the analysis were respondents who had not yet been offered vaccination or whose vaccination status was unknown, and those who have a second dose scheduled. Analyses were conducted using SAS® software, Version [9.4] [24] and data verified using R software version 4.0.3 [25].
4. Results
4.1. Proportion of surveys completed
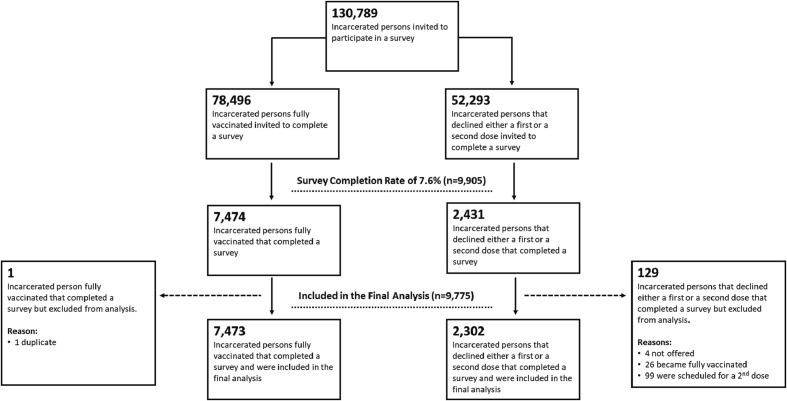
A total of 130,789 persons were invited to participate. At the time of survey, 78,496 persons (60.0%) were fully vaccinated, 52,293 (33.9%) had declined either a first or second dose, and 3,231 (2.5%) were partially vaccinated and scheduled to complete their second dose. 7,473 (9.5%) of the fully vaccinated group and 2,302 (4.4%) of the group declining vaccination chose to participate in the survey, an overall survey return rate of 7.5% (n = 9,775) (Fig. 1 ). The proportion of survey responses were highest among institutions in the South Central region (SCR) (n = 2,029; 20.8%) and lowest in the Western region (WXR) (n = 1,121; 11.5%) (a list of states by region are available in Table 1). One (0.0001%) fully vaccinated respondent and 129 (0.05%) who had refused a first or second dose were excluded from the final analyses. Of these, 26 received the incorrect version of the survey, 4 had not yet been offered the vaccine, 99 were scheduled to receive their second dose, and 1 submitted the same survey twice. A total of 9,775 respondents were included in final analyses (Fig. 1).
Fig. 1.
COVID-10 Vaccination Survey Completions among Incarcerated Persons and inclusion in final analyses, in the Federal Bureau of Prisons, June 7, 2021–July 2021.
Table 1.
Demographic Characteristics of Incarcerated Persons Completing a Federal Bureau of Prisons COVID-19 Vaccination Survey, June 2021–July 2021.
| Overall n (%) | Fully Vaccinated n (%) | Declined a First or Second Dose n (%) | |
|---|---|---|---|
| Total | 9775 (100%) | 7473 (76.5%) | 2302 (23.5%) |
| Sex | |||
| Male | 8519 (87.2%) | 6584 (77.3%) | 1935 (22.7%) |
| Female | 1254 (12.8%) | 888 (70.8%) | 366 (29.2%) |
| Age group | |||
| <40 | 3686 (37.7%) | 2554 (69.1%) | 1132 (30.9%) |
| 40 to 49 | 3312 (33.9%) | 2559 (77.1%) | 753 (22.9%) |
| 50 to 59 | 1939 (19.8%) | 1629 (83.8%) | 310 (16.2%) |
| 60 to 74 | 807 (8.3%) | 702 (86.9%) | 1065 (13.1%) |
| >=75 | 29 (0.3%) | 28 (96.6%) | 1 (3.4%) |
| Race | |||
| White | 6891 (70.5%) | 5591 (81.1%) | 1300 (18.9%) |
| Black | 2498 (25.6%) | 1578 (63.2%) | 920 (36.8%) |
| Native American | 258 (2.6%) | 201 (77.9%) | 57 (22.1%) |
| Asian | 126 (1.3%) | 102 (81.0%) | 24 (19.0%) |
| Ethnicity | |||
| Hispanic | 1484 (15.2%) | 1185 (79.9%) | 299 (20.1%) |
| Non-Hispanic | 8288 (84.8%) | 6286 (75.8%) | 2002 (24.2%) |
| Regiona | |||
| Mid-Atlantic | 1905 (19.5%) | 1456 (76.4%) | 449 (23.6%) |
| North Central | 1515 (15.5%) | 1132 (74.7%) | 383 (25.3%) |
| Northeast | 1545 (15.8%) | 1236 (80.0%) | 309 (20.0%) |
| South Central | 2029 (20.8%) | 1566 (77.2%) | 463 (22.8%) |
| Southeast | 1646 (16.8%) | 1231 (74.8%) | 415 (25.2%) |
| Western | 1121 (11.5%) | 841 (75.0%) | 280 (25.0%) |
bSurvey participants did not answer all demographic questions. Due to non-responses some totals may not add up.
List of states by region: North Central: Colorado, Illinois, Kansas, Michigan, Minnesota, Missouri, New York, South Dakota, Wisconsin; Northeast: Connecticut, Florida, Massachusetts, Mississippi, New Hampshire, New Jersey, New York, Ohio, Pennsylvania; South Central: Arkansas, Louisiana, Oklahoma, Texas; Southeast: Alabama, Florida, Georgia, Mississippi, Puerto Rico, South Carolina; West: Arizona, California, Hawaii, Oregon, Washington.
Across all respondents, the majority were male (n = 8,519; 87.2%), under the age of 40 (n = 3,686; 37.7%), and non-Hispanic (n = 8,288; 84.8%) White (n = 6,891; 70.5%) (Table 1).
4.2. Vaccine uptake among survey respondents
76.5% of survey respondents were fully vaccinated, and 23.5% had refused a first or second dose. The groups with the highest percentage of vaccination were individuals aged 75 years and older (n = 28; 96.6%), male (n = 6,584; 77.3%), Hispanic (n = 1,185; 79.9%), White (n = 5,591; 81.1%) or Asian (n = 102; 81.0%), or held in facilities in the Northeast region (n = 1,236; 80.0%) (Table 1). The groups with the highest percentage of declining a first or second vaccine dose were individuals aged 40 years and younger (n = 1,132; 30.9%), Black (n = 920; 36.8%), female (n = 366; 29.3%), or held in institutions in the North Central (NCR) or Southeast (SER) Regions (NCR n = 383, 25.3%; SER n = 415, 25.2%) (Table 1).
4.3. Reasons for vaccination decisions and trusted sources of information
Among vaccinated survey respondents, the most common reasons for accepting vaccination were to protect their health (n = 5,689; 76.1%) and “because it was a good thing to do” (n = 3,381; 45.2%) (Table 2). The least common reasons for accepting vaccination included the options: “I took it after my healthcare provider answered all my questions” (n = 599; 8.0%) and “my cell mates advised me to take it” (n = 315; 4.2%)” (Table 3).
Individuals who declined vaccination cited concerns about vaccine side effects (n = 1,304; 56.6%), mistrust of the vaccine (n = 1,256; 54.6%), vaccine safety concerns (n = 1,252; 54.4%), and “not know[ing] enough information on the vaccine” (n = 1,019; 44.3%). Among those who declined vaccination, 21.2% (n = 489) reported that they would choose to be vaccinated if the vaccine was offered again. A subset of those who declined also reported that additional information from outside organizations (n = 1128; 49.0%), particularly regarding vaccine safety (n = 841; 36.5%) and “additional information for those previously infected” (n = 588; 25.5%), may influence their decision to be vaccinated in the future. Furthermore, respondents indicated that speaking with a trusted medical provider (n = 565; 24.5%) or with family/friends (n = 453; 19.7%) may help change their mind to accept the vaccine (Table 3).
Across all respondents, sources delivering vaccine-related information that were reported as most influential included family members/friends (n = 4,056, 54.3% of those vaccinated; n = 1,150, 50.5% of those who declined) and news such as television (n = 3,754, 50.2% of vaccinated; n = 1,094, 47.5% of those who declined). Of all staff categories listed, health services staff were most frequently reported as a trusted source of vaccine-related information (n = 2,333, 31.2% of those vaccinated; n = 719, 31.2% of those who declined). Religious services staff were least often reported as an information source respondents relied upon for vaccine-related information (n = 190, 2.5% of vaccinated; n = 124, 5.4% of those who declined).
5. Human subjects determination
This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy. CDC determined that its involvement in this analytic project did not constitute engagement in research involving human subjects; CDC Internal Review Board (IRB) review was not required. This project employs secondary analysis of preexisting data collected by BOP for routine clinical and operational purposes; BOP Bureau Research Review Board (BRRB) review was not required.
6. Discussion
In this large-scale study examining attitudes towards COVID-19 vaccination among incarcerated persons in the BOP, the most common reason respondents cited for accepting vaccination was to protect their health, whereas those who declined vaccination cited concerns around vaccine side effects, mistrust of the vaccine, and vaccine safety. Among those who initially declined receiving a vaccine, approximately half (49.0%) reported that additional information from outside organizations, such as government agencies, religious organizations, or community groups could influence their decision to accept a COVID-19 vaccine in the future. Just over one-fifth of those who initially declined a vaccine reported they would choose to be vaccinated if it was offered again.
Among all survey respondents, vaccination acceptance was lowest among individuals who were aged 40 years and under, female, Black, or held in correctional facilities in the North Central or Southeast Regions. Our study results are consistent with general population studies that have found demographic differences, including race/ethnicity, age, and gender, in COVID-19 vaccination coverage among adult populations in the United States [25], [26], [27], [28], [29], [30]. Regional differences found in this study also align with lower vaccination coverage across the Midwest and Southern states overall [31]. Similar demographic differences in COVID-19 vaccine acceptance have been reported in other high-risk settings, including among persons experiencing homelessness [32]. Although our study results are consistent with the growing literature on demographic differences in vaccine uptake, this data should be carefully interpreted as this survey was conducted during the early phase of vaccine rollout and may not fully represent the vaccine intentions of BOP’s incarcerated population.
Regardless of their vaccination decisions, survey respondents from this study identified family/friends, television, and health services staff as their most trusted sources for COVID-19 vaccination information. Our results are consistent with previously reported findings of family/friends and television serving as trusted sources of COVID-19 information in carceral settings [16], [17], [18]. In the case of health services staff, the literature has been largely mixed. The U.S. Constitution prohibits deliberate indifference to the medical conditions of incarcerated people [34]; however, it is widely known that incarcerated persons often face many challenges receiving the level of clinical care that meets their healthcare needs [35]. For example, the Correctional Association of New York found only 8.8% of all incarcerated survey respondents trusted doctors or healthcare providers in a prison to make medically correct judgments; whereas 48.4% of respondents said that they trusted healthcare providers in the community to make medically correct judgments [33]. However, our study found that 31.2% of survey respondents in both groups relied on information from BOP health services staff, higher than any other staff category, in order to make a decision to either receive or refuse a COVID-19 vaccine. Reasons for why respondents may have declined a first or second vaccine dose even after receiving information from BOP health services staff may have to do with confidence surrounding vaccine safety, its effectiveness, and its side effects. Interestingly, a high prevalence of COVID-19 vaccine hesitancy among healthcare workers has also been reported and thought to influence patient behavior [49]. Moreover, this study did not find religious services staff to be considered a top trusted source of information about COVID-19 vaccines, despite the role religious counseling and other faith-based programming have in other correctional programming [36], and the success that faith-based messaging has shown to have promoting vaccine confidence in some communities outside carceral settings [37]. It is possible that survey respondents had less contact with religious services staff during the study period since many facilities restricted movement and access to in-person programming during COVID-19 outbreaks to reduce transmission.
Importantly, some respondents who declined reported that they may be willing to accept the vaccine in the future. Roughly half (49.0%) of those who declined responded that they may “change their mind” and accept a vaccine if they received more information from outside organizations, including government, religious organizations, and/or community groups, and 21% reported that they would accept vaccination if it was offered again. While this survey question did not ask specifically which outside organization(s) could be most influential in promoting vaccine acceptance, our findings build on a growing number of studies demonstrating the importance of employing trusted sources to boost COVID-19 vaccination among targeted populations [39], [40], [41]. For example, jails in Massachusetts worked with medical students in the community to provide “Ask Me Anything” sessions to persons detained in local jails about COVID-19 vaccination. The authors of this study conclude that having an outside source of information can increase trust in COVID-19 vaccines and assure people living in jails that they are receiving comparable care to what is offered in the community [42]. Our findings reaffirm that reoffering vaccination is a critical component of strengthening vaccine coverage in correctional facilities [13], because attitudes about vaccination can change over time, particularly if incarcerated people feel vaccination may help lift strict COVID-19 restrictions [16].
This study builds on a growing area of literature demonstrating the role of attitudes and trusted information sources in influencing COVID-19 vaccination uptake in correctional facilities; however, key gaps remain in our understanding of how socio-behavioral drivers of vaccine acceptance impacts incarcerated persons. Future studies may consider investigating the role of incentives to help increase vaccine uptake (and other public health interventions), and better understand whether they have the same impact on behavior change among both incarcerated individuals as they do in the general population [38], [22], [39]. Historically, incentives have not been applied as broadly in correctional settings because of ethical implications, such as the potential perception of coercion to participate in research [40], [41]. While outside the scope of this study, strengthening COVID-19 vaccination among correctional staff is considered a vital strategy for reducing mortality and morbidity from this infection [23], as studies have shown that staff member movements to and from surrounding communities [43] might be an important source of virus introduction into facilities [44]. Lastly, there is an urgent need to understand the impact of health misinformation [45], which may be precipitated by low health and informational literacy [46], as well as ways to prevent misinformation or counter it when it occurs [47].
The findings from this study are subject to several key limitations. First, these findings may not be representative of the entire BOP incarcerated population. Second, there may be facility-level factors that could have resulted in different levels of vaccine uptake in different institutions, such as the amount of education provided about vaccines by local staff, and the level of support for vaccination among institutions’ staff and leadership. Facilities that have a strong vaccine advocate may have had better vaccine coverage and greater proportion of survey responses than those at institutions without correctional staff serving as “trusted sources” among incarcerated persons. Third, incarcerated persons had access to the survey either electronically or paper-based; however, a limitation was that the survey was not provided verbally. This may have served as a barrier to complete the survey for some individuals experiencing accessibility issues (e.g., persons with disabilities), some that are unfamiliar with the use of technology, or those with literacy challenges. Fourth, the purpose of the BOP vaccine survey was to explore attitudes underlying vaccine intentions during the early phase of vaccine roll-out across BOP facilities; thus, the overall vaccine data presented in this study should be carefully interpreted and readers may refer to other relevant BOP papers [14]. Lastly, our study findings may not be generalizable to other correctional and detention facilities, due to diversity in operations, security or custody levels, availability of services/programs, staffing levels, resources, correctional philosophy, and administrative leadership across different facilities [48].
Our study findings add to a growing body of literature illustrating the importance of understanding underlying attitudes towards vaccine acceptance and the critical role of trusted sources to promote trust, equity, and transparency both for COVID-19 vaccinations and correctional health in general. We demonstrated that sources of vaccine-related information not only play a key role in influencing one’s decision to accept or decline vaccination; but also is key to influencing decisions regarding vaccinations in the future. As correctional facilities continue to be impacted by COVID-19 transmission and mortality, our survey findings may be used to inform the design of potential interventions to increase COVID-19 vaccine uptake in these settings.
7. Authors’ Contributions
R.F. contributed to methodology, literature search, data analysis and synthesis, and initial manuscript draft; Z.K. contributed to data analysis and synthesis, and initial manuscript draft. T.R. contributed to data synthesis, administrative support, and manuscript review; L.H. contributed to data analysis and synthesis, administrative support and manuscript review; K.A. contributed to data analysis and synthesis, and manuscript review; C.D. contributed to data analysis and manuscript review; M.C. contributed to data synthesis and manuscript review; and M.L. contributed to administrative and technical support, and manuscript review.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
We acknowledge the incarcerated and detained persons that participated in this study, and correctional staff supporting the implementation of the study at the Federal Bureau of Prisons, Dr. Emily Mosites, and the CDC COVID-19 Response for supporting this study.
Funding Information
The authors received no financial support for the re-search, authorship, and/or publication of this article. This work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclaimer
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Federal Bureau of Prisons or the Department of Justice, U.S. Department of Health and Human Services, the Commissioned Corps of the US Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions.
Data availability
The authors do not have permission to share data.
References
- 1.Akiyama M.J., Spaulding A.C., Rich J.D. Flattening the curve for incarcerated populations — Covid-19 in jails and prisons. N Engl J Med. 2020;382:2075–2077. doi: 10.1056/NEJMp2005687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saloner B., Parish K., Ward J.A., DiLaura G., Dolovich S. COVID-19 Cases and Deaths in Federal and State Prisons. JAMA. 2020;324(6):602–603. doi: 10.1001/jama.2020.12528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rubin R. The Challenge of Preventing COVID-19 Spread in Correctional Facilities. JAMA. 2020;323(18):1760–1761. doi: 10.1001/jama.2020.5427. [DOI] [PubMed] [Google Scholar]
- 4.Leibowitz A.I., Siedner M.J., Tsai A.C., Mohareb A.M. Association Between Prison Crowding and COVID-19 Incidence Rates in Massachusetts Prisons, April 2020-January 2021. JAMA Intern Med. 2021;181(10):1315–1321. doi: 10.1001/jamainternmed.2021.4392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beaudry G., Zhong S., Whiting D., Javid B., Frater J., Fazel S. Managing outbreaks of highly contagious diseases in prisons: a systematic review. BMJ Glob Health. 2020 Nov 1;5(11):e003201. doi: 10.1136/bmjgh-2020-003201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maruschak L.M., Berzofsky M., Unangst J. U.S. Department of Justice, Bureau of Justice Statistics; Washington, DC: 2015. Medical Problems of State and Federal Prisoners and Jail Inmates, 2011–12. [Google Scholar]
- 7.Chin ET, Leidner D, Zhang Y, Long E, Prince L, Schrag SJ, et al. Effectiveness of COVID-19 Vaccines among Incarcerated People in California State Prisons: A Retrospective Cohort Study. medRxiv: the preprint server for health sciences, 2021.08.16.21262149. doi: 10.1101/2021.08.16.21262149. [DOI]
- 8.Clemenzi-Allen A.A., Pratt L.A. Avoiding COVID-19 Outbreaks in Carceral Settings. JAMA Intern Med. 2021;181(10):1322–1323. doi: 10.1001/jamainternmed.2021.4389. [DOI] [PubMed] [Google Scholar]
- 9.A.C. Spaulding Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia, USA C. Zawitz Department of Internal Medicine, Division of Infectious Diseases, Rush Medical College , Chicago, Illinois , USA Cermak Health Services , Cook County Jail, Chicago, Illinois , USA Vaccination in Prisons and Jails: Corrections Needed in Future Plans Clinical Infectious Diseases. 75 1 2022 2022 e846 e8. [DOI] [PubMed]
- 10.Klein AH, Turcotte M. Vaccinations are lagging at many U.S. prisons, where major virus outbreaks have been common. New York Times. May 22, 2021. Retrieved from: https://www.nytimes.com/2021/05/22/us/covid-prison-vaccine.html
- 11.Herring T, Widra E, Just over half of incarcerated people are vaccinated, despite being locked in COVID-19 epicenters. Prison Policy Initiative. May 18, 2021. Retrieved from: https://www.prisonpolicy.org/blog/2021/05/18/vaccinationrates/.
- 12.Stern M.F., Piasecki A.M., Strick L.B., Rajeshwar P., Tyagi E., Dolovich S., et al. Willingness to receive a COVID-19 vaccination among incarcerated or detained persons in correctional and detention facilities — four states, September–December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(13):473–477. doi: 10.15585/mmwr.mm7013a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chin E.T., Leidner D., Ryckman T., Liu Y.E., Prince L., Alarid-Escudero F., et al. Covid-19 vaccine acceptance in california state prisons. N Engl J Med. 2021 Jul 22;385(4):374–376. doi: 10.1056/NEJMc2105282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hagan L.M., Dusseau C., Crockett M., Rodriguez T., Long M.J. COVID-19 vaccination in the Federal Bureau of Prisons, December 2020—April 2021. Vaccine. 2021;39(40):5883–5890. doi: 10.1016/j.vaccine.2021.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sparks G, Kirzinger A, Brodie M. KFF COVID-19 Vaccine Monitor: Profile Of The Unvaccinated. June 11, 2011. Retrieved from: https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-profile-of-the-unvaccinated/.
- 16.Ortiz-Paredes D., Varsaneux O., Worthington J., Park H., MacDonald S.E., Basta N.E., et al. Reasons for COVID-19 vaccine refusal among people incarcerated in Canadian federal prisons. PLoS One. 2022;17(3):e0264145. doi: 10.1371/journal.pone.0264145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khorasani S.B., Koutoujian P.J., Zubiago J., Guardado R., Siddiqi K., Wurcel A.G. COVID-19 Vaccine Interest among Corrections Officers and People Who Are Incarcerated at Middlesex County Jail. Massachusetts J Urban Health. 2021 Aug;98(4):459–463. doi: 10.1007/s11524-021-00545-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu Y.E., Oto J., Will J., LeBoa C., Doyle A., Rens N., et al. Factors associated with COVID-19 vaccine acceptance and hesitancy among residents of Northern California jails. Prev Med Rep. 2022;27:101771. doi: 10.1016/j.pmedr.2022.101771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lessard D., Ortiz-Paredes D., Park H., Varsaneux O., Worthington J., Basta N.E., et al. Barriers and facilitators to COVID-19 vaccine acceptability among people incarcerated in Canadian federal prisons: A qualitative study. Vaccine. 2022 Apr;10 doi: 10.1016/j.jvacx.2022.100150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berk J., Murphy M., Chan P., Kane K., Rich J., Brinkley-Rubinstein L. Initial SARS-CoV-2 Vaccination Uptake in a Correctional Setting: Cross-sectional Study. JMIRx Med. 2021;2(3):e30176. doi: 10.2196/30176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meehan A.A., Yeh M., Gardner A., DeFoe T.L., Garcia A., Vander Kelen P., et al. COVID-19 vaccine acceptability among clients and staff of homeless shelters in Detroit, Michigan, February 2021. Health Promot Pract. 2022;23(1):35–41. doi: 10.1177/15248399211049202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Volpp K.G., Cannuscio C.C. Incentives for immunity—strategies for increasing Covid-19 vaccine uptake. N Engl J Med. 2021 Jul 1;385(1):e1. doi: 10.1056/NEJMp2107719. [DOI] [PubMed] [Google Scholar]
- 23.Federal Bureau of Prisons. COVID-19 Vaccine Guidance Federal Bureau of Prisons Clinical Guidance. October 13, 2021. Retrieved from: https://www.bop.gov/resources/pdfs/covid_19_vaccine_guidance_v14_0_2021.pdf.
- 24.SAS Institute Inc . SAS Institute Inc.; Cary, NC: 2013. SAS® 9.4 Statements: Reference. [Google Scholar]
- 25.R. Core Team. R: A Language and Environment for Statistical Computing [Internet] 2021 R Foundation for Statistical Computing Vienna 454 Austria Available from: https://www.R-project.org/.
- 26.Malik A.A., McFadden S.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinical Medicine. 2020 Sep;1(26) doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nguyen L.H., Joshi A.D., Drew D.A., Merino J., Ma W., Lo C.H., et al. Racial and ethnic differences in COVID-19 vaccine hesitancy and uptake. MedRxiv. 2021 Jan 1 doi: 10.1101/2021.02.25.2125240. [DOI] [Google Scholar]
- 28.Razai M.S., Osama T., McKechnie D.G., Majeed A. Covid-19 vaccine hesitancy among ethnic minority groups. BMJ. 2021 Feb;26:372. doi: 10.1136/bmj.n513. [DOI] [PubMed] [Google Scholar]
- 29.Hildreth J.E., Alcendor D.J. Targeting COVID-19 vaccine hesitancy in minority populations in the US: implications for herd immunity. Vaccines. 2021 May;9(5):489. doi: 10.3390/vaccines9050489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shih S.F., Wagner A.L., Masters N.B., Prosser L.A., Lu Y., Zikmund-Fisher B.J. Vaccine hesitancy and rejection of a vaccine for the novel coronavirus in the United States. Front Immunol. 2021 Jun;14(12):2275. doi: 10.3389/fimmu.2021.558270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beleche T, Ruhter J, Kolbe A, Marus, J, Bush L, Sommers B. COVID-19 Vaccine Hesitancy: Demographic Factors, Geographic Patterns, and Changes over Time. 2021. Retrieved from: https://aspe.hhs.gov/sites/default/files/private/pdf/265341/aspe-ib-vaccine-hesitancy.pdf.
- 32.Rogers J.H., Cox S.N., Hughes J.P., Link A.C., Chow E.J., Fosse I., et al. Trends in COVID-19 vaccination intent and factors associated with deliberation and reluctance among adult homeless shelter residents and staff, 1 November 2020 to 28 February 2021–King County. Washington Vaccine. 2022;40(1):122–132. doi: 10.1016/j.vaccine.2021.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Correctional Association of New York. “My Greatest Fear is to be a lab rat for the state: COVID-19 and vaccine hesitancy in New York state prisons (CANY’s Annual Report July 2020-June 2021)”. Retrieved from: https://static1.squarespace.com/static/5b2c07e2a9e02851fb387477/t/61d7dba2bcbd117213e7994a/1641536423998/CANY_2021AnnualReport_010622.pdf.
- 34.Marshall T. Supreme Court of The United States. U.S. Reports: Estelle v. Gamble, 429 U.S. 97. 1976. Periodical. Retrieved from the Library of Congress: http://www.loc.gov/item/usrep429097/.
- 35.Binswanger A., Krueger P.M., Steiner J. Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. J Epidemiol Community Health Care Women. 2009;63:912–919. doi: 10.1136/jech.2009.090662. [DOI] [PubMed] [Google Scholar]
- 36.PEW Research Center: “Religion in Prisons: A 50-State survey of prison chaplains.” 2012. Retrieved from: https://www.pewresearch.org/wp-content/uploads/sites/7/2012/03/Religion-in-Prisons.pdf.
- 37.IFYC-PRRI. “Faith-based approaches can positively impact COVID-19 vaccination efforts: Religious identifies and the race against the virus: Findings from the 1021 PRRI-IFYC Diversity and Vaccine Survey.” 2021. Retrieved from: https://ifyc.org/sites/default/files/PRRI-IFYC-Apr-2021-Vaccine.pdf.
- 38.Campos-Mercade P., Meier A.N., Schneider F.H., Meier S., Pope D., Wengström E. Monetary incentives increase COVID-19 vaccinations. Science. 2021 Nov 12;374(6569):879–882. doi: 10.1126/science.abm0475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Higgins S.T., Klemperer E.M., Coleman S.R. Looking to the empirical literature on the potential for financial incentives to enhance adherence with COVID-19 vaccination. Prev Med. 2021 Apr;1(145) doi: 10.1016/j.ypmed.2021.106421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Persad G., Emanuel E.J. Ethical considerations of offering benefits to COVID-19 vaccine recipients. JAMA. 2021 Jul 20;326(3):221–222. doi: 10.1001/jama.2021.11045. [DOI] [PubMed] [Google Scholar]
- 41.Singer E., Bossarte R.M. Incentives for survey participation: when are they “coercive”? Am J Prev Med. 2006 Nov 1;31(5):411–418. doi: 10.1016/j.amepre.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 42.Erfani P., Sandoval R.S., Rich K.M., Ojo A., Walker L., White-Hammond G., et al. Ask Me Anything”: Lessons learned in implementing a COVID-19 vaccine information initiative in Massachusetts jails. Vaccine. 2022 Apr 8 doi: 10.1016/j.vaccine.2021.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hagan L.M., Williams S.P., Spaulding A.C., Toblin R.L., Figlenski J., Ocampo J., et al. Mass Testing for SARS-CoV-2 in 16 Prisons and Jails - Six Jurisdictions, United States, April-May 2020. MMWR Morb Mortal Wkly Rep. 2020 Aug 21;69(33):1139–1143. doi: 10.15585/mmwr.mm6933a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wallace M., Hagan L., Curran K.G., Williams S.P., Handanagic S., Bjork A., et al. COVID-19 in Correctional and Detention Facilities — United States, February–April 2020. MMWR Morb Mortal Wkly Rep. 2020;69(19):587–590. doi: 10.15585/mmwr.mm6919e1. [DOI] [PubMed] [Google Scholar]
- 45.Office of the Surgeon General. “Confronting Health Misinformation: The U.S Surgeon General’s Advisory on Building a Healthy Information Environment.” 2021. Retrieved from: https://www.hhs.gov/surgeongeneral/priorities/health-misinformation/index.html. [PubMed]
- 46.Bin Naeem S., Kamel Boulos M.N. COVID-19 misinformation online and health literacy: A brief overview. Int J Environ Res Public Health. 2021 Jan;18(15):8091. doi: 10.3390/ijerph18158091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vraga E.K., Bode L. Using expert sources to correct health misinformation in social media. Sci Commun. 2017 Oct;39(5):621–645. doi: 10.1177/1075547017731776. [DOI] [Google Scholar]
- 48.National Academies of Sciences Engineering and Medicine The Growth of Incarceration in the United States: Exploring Causes and Consequences 2014 The National Academies Press Washington DC 10.17226/18613.
- 49.Biswas N., Mustapha T., Khubchandani J., Price J.H. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J Community Health. 2021 Dec;46:1244–1251. doi: 10.1007/s10900-021-00984-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors do not have permission to share data.