Abstract
Objective:
This study aimed to conduct a systematic review and meta-analysis of randomized controlled trials (RCTs) on the comparative effects of different types or parameters of lumbar traction in low back pain (LBP).
Methods:
CENTRAL, CINAHL, ISI Web of Science, PEDro, PubMed, and Scopus databases were searched from their inception to March 31, 2021. We considered all RCTs comparing different types or parameters of lumbar traction on adults who complained of LBP with or without lumbar radiculopathy (LR). Any restriction regarding publication time or language was applied. Two reviewers independently selected the studies, performed the quality assessment, and extracted the results. Meta-analysis employed a random-effects model.
Results:
Sixteen studies met the inclusion criteria for qualitative analysis, and five were pooled. Meta-analyses of results from five studies on LBP with LR showed no significant difference between diverse tractions modalities at short-term follow-up. Very low to low-quality evidence supports these results. High-force and low-force traction demonstrated clinically significant improvements in pain.
Conclusion:
The literature suggests the short-term effectiveness of traction on pain in LBP with LR, regardless of the type or the dosage employed. Different effects of traction other the mechanical ones can be hypothesized. This systematic review may be relevant for clinical practice due to the similar effects of different traction types or dosages.
Level of Evidence:
Level I, Therapeutic Study
Keywords: Traction, Sciatica, Radiating pain, Low back pain, Randomized controlled trials
HIGHLIGHTS
Traction is commonly used in patients who complained of low back pain, despite conflicting opinions on its effectiveness. This study aimed to investigate the comparative effectiveness of different types of traction or the same traction delivered with different parameters (patient position or force delivered).
The results showed that no significant difference in clinical effectiveness appears between diverse tractions modalities, at short-term follow-up. High-force and low-force traction both demonstrate clinically significant improvements in pain.
The literature suggests the short-term effectiveness of traction on pain in low back pain with or without lumbar radiculopathy, regardless of the type or dosage employed. These results highlight that the so-called “sham” traction is actually a clinically effective traction.
Introduction
Several past systematic reviews suggested the ineffectiveness of traction as a single treatment for low back pain (LBP) with or without lumbar radiculopathy (LR) when compared with other conservative treatments or physiotherapy.1-5 More recently, other systematic reviews drew opposite conclusions, showing positive effects of traction for lumbar disk herniation and LR.6-9
Systematic reviews may make competing interpretations of the data due to many factors, including differences in the inclusion criteria for each of the pooled studies as well as the treatment parameters for each traction method used in the interventions of pooled studies. Moreover, some reviews included studies comparing subjects with control groups which received sham interventions based on a presumably ineffective traction force (e.g., less than 25% body weight), treatments without traction, or even no treatment at all. Furthermore, the variability in many of the forms in which traction may be implemented further frustrates drawing clear conclusions about the value of traction. This treatment may be also “patient-tailored”: it can be exerted using the clinician’s force (manual traction), motorized tools (mechanical traction), the patient’s own ability to provide the traction force (auto-traction), the body weight (inverted or gravitational traction), and underwater suspension with the addition of weights (underwater traction).10 It can be delivered in continuous or intermittent ways; different forces and patient positioning can be adopted11; it may be accompanied by vibration, and also a combination of low-tension traction and shock wave therapy has been proposed to reshape the environment for disc regeneration and repair.12 Finally, the generally poor methodological quality of included studies must also be taken into account.5
The debate on the effectiveness of traction is not trivial as traction is frequently used as a non-pharmacologic conservative intervention for LBP and LR, justified clinically on its purported ability to reduce pain and disability, improve lumbar range of motion, and modulate neural mechanical sensitivity.10 We hypothesized that the discrepancy between several evidence and clinical practice may persist because only traction performed with certain forces or in certain positions was considered an effective intervention in most systematic reviews.
The persistent debate on this treatment and the uncertainty about its clinical effects, particularly when compared to the so-called “sham” traction, prompted us to do a systematic review with meta-analysis to investigate the comparative effectiveness of different types of traction or the same traction delivered with different parameters (patient position or force delivered). Moreover, we investigated if the changes induced by different types/parameters of traction resulted in clinically significant effects on pain in adults who complained of LBP with or without LR.
Materials and Methods
We followed the Cochrane Handbook for Systematic Reviews of Intervention as our methodological guidance.13 The Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement for the reporting was used.14 This systematic review protocol was registered in the PROSPERO database (code CRD42020180507).
Data sources and searches
Search strings were developed for the following databases: CENTRAL, CINAHL, ISI Web of Science, PEDro, PubMed, and Scopus. The following search terms were used in various combinations and adapted for the search in all databases: “back”/“lumbar”; “sciatica”/“radiculopathy”/“radicular syndrome”/“nerve root pain”/“leg pain”/ low back pain”; “traction”/“physical therapy modalities.” The search strings adopted for each database are reported in Appendix 1.
Databases were searched from inception until March 31, 2021. Moreover, reference lists of included articles, systematic reviews, and guidelines were manually searched together with other gray literature sources. If necessary, authors were contacted for missing information.
Two independent blinded authors (KS, CV) conducted the study selection. All results were first imported on EndNote V.X9 (Clarivate Analytics, Philadelphia, USA) to search for and delete duplicates, and then titles, abstracts, and full texts were screened one by one using Rayyan QRCI. Systematically, the 2 authors compared their results; in case of disagreement, a third author (PP) was consulted.
Studies selection
Types of studies
We included randomized controlled trials (RCTs) without any restriction on publication date, status, or language. Studies reporting means and standard deviations of outcome measures at baseline and any follow-up were included; for studies in which standard deviations were not reported, P-value or mean of standard deviations of similar studies were used following the instructions of Cochrane Handbook for Systematic Reviews of Interventions version 6.0.15
Types of participants
We included studies on adults, aged ≥18 years, who complained of LBP with or without LR. We excluded trials involving patients with myelopathy, infection, fracture, dystonia, cancer, inflammation disease, osteoporosis, and fibromyalgia, or subjects with current pregnancy or early postpartum period.
Types of interventions and comparator(s)/control
We included RCTs in which different types of traction or the same type of traction delivered with different parameters were compared. Only trials with complete data regarding traction (patient position, traction type, force, frequency, etc.) were selected for inclusion in this study.
Types of outcome measures
We included RCTs that used at least one of the following primary outcomes: pain intensity, measured with a Visual Analog Scale or a Numerical Rating Scale (NRS), and physical functioning, measured with the Roland & Morris Disability Questionnaire or the Oswestry Disability Index. Secondary outcomes were quality of life (e.g., measured with SF-36); lumbar and leg mobility (e.g., measured with metric or angular devices); changes in neurological function (e.g., measured with neurodynamics tests); and psychological parameters (e.g., measured with Questionnaires on Fear-Avoidance Beliefs, Anxiety or Depression). Adverse effects were also collected, when reported.
Outcome measures must have been collected both at baseline and at another time point, e.g., short- (up to 3 months after baseline), mid- (between 3 and 6 months), or long-term (more than 6 months) follow-ups.
Data Extraction and quality assessment
Selection and coding
Two reviewers (KS, CV) independently conducted data extraction and collection using an Excel spreadsheet. To obtain missing data, we contacted the study authors.
Risk of bias assessment
Two authors (KS, LT) independently conducted the risk of bias assessment using the Cochrane Collaboration’s Risk of Bias (RoB 2.0) tool.13,16
Quality of evidence assessment
Two authors (AP, LT) independently conducted the overall quality of evidence assessment using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach.17
We rated the evidence across studies for specific clinical outcomes, by considering the 5 GRADE domains: i) study limitations from RoB assessment; ii) indirectness; iii) inconsistency; iv) imprecision, and v) publication bias. The quality of the evidence was adjusted by a level based on the performance of the studies against the 5 domains.18
Data synthesis and analysis
Strategy for synthesis
We provided a descriptive synthesis of the findings from the included studies commenting on the difference between treatments and summarizing intervention effects for each study using mean difference. To calculate the effects of interventions, different analyses were made according to traction type, patient position, and force delivered. When possible, meta-analyses of aggregate data were conducted using statistical analysis to generate a summary (pooled) estimate using effect estimates of individual studies. The data were synthesized using a meta-analytic method based on a random-effects model to calculate Hedge’s g in order to give a more conservative estimate of effect. Hedges g is an inferential measure that assesses the magnitude of differences between 2 groups incorporating a small sample bias correction.19
Analysis
For statistical analysis, the software ProMeta v.2.0 (Internovi by Scarpellini Daniele s.a.s., Cesena (FC), Italy; now owned by Idostatistics) was used. Standardized mean differences (SMDs) with 95% CIs were calculated for continuous data. To interpret the effect size calculated with SMD, we used Cohen’s interpretations of d 20 as a guide to identify small (0.20), medium (0.50), or large (0.80) effects. The calculation of effect size was based on the best possible data (e.g., final means/standard deviations/sample sizes of intervention and control groups). The studies for which these or other essential data were not reported or obtainable by contacting authors were excluded.
To evaluate heterogeneity, we addressed 2 questions: Is there significant heterogeneity across studies? And how large is this heterogeneity? To answer these, the Q2 and I2 statistics were used. The first question was addressed by means of the Q statistic, with a significant Q value indicating significant heterogeneity of results among studies. The second question was addressed by computing the I2 index.21 The I2 estimates the proportion of observed variance that reflects real differences in effect sizes, with values of 25%, 50%, and 75% that might be considered as low, moderate, and high, respectively.22 The potential publication bias was assessed using the Egger t-test.
These methods were applied both to between-groups and within-groups analyses. The first one aimed to calculate the different effects of diverse traction types/parameters, whereas the second one aimed to calculate the cumulative differences between pre- and post-treatment for each traction group. This second analysis attempted to explore if the minimum clinically important difference (MCID) was reached for the outcome pain. We adopted a within-group change of 25 on a 0-100 NRS as a threshold for MCID on pain.7
Results
We identified 1326 records through database searching, and 36 further studies were obtained through other sources. After duplicate removal, 701 articles were screened; after reading titles and abstracts, 30 were assessed for reading full texts. By screening these studies, 14 full texts were excluded; 16 studies were selected for qualitative analysis, and 5 were selected for quantitative synthesis and meta-analysis (Figure 1). The complete list of excluded articles with reasons is presented in Appendix 2.
Figure 1.

Flow chart of included studies.
Studies were sub-grouped according to population (LBP without LR, LBP with/without LR, LBP with LR) and comparison (traction force, traction type, patient position) (Table 1). When possible, the study population was classified into acute (less than 6 weeks), sub-acute (6-12 weeks), and persistent (more than 12 weeks) categories.
Table 1.
Characteristics of studies included in qualitative analysis
| Author | Inclusion criteria | Exclusion criteria | Diagnostic criteria | Groups | Treatments | Outcome measures | Results (as reported by the authors) |
|---|---|---|---|---|---|---|---|
| LBP without radicular pain—comparison: different traction types | |||||||
| Tanabe et al, 2020, Japan | - Age >20 to <64 - Nonspecific LBP - More than 3 months duration - More than 70° at SLR test - Negative femoral nerve stretching test - No superficial sensory deficits - No muscle weakness |
- Radicular pain or neurological deficits - Tumor, infection, or fracture - Previous back surgery - Severe osteoporosis - Psychiatric disorders - Liver and renal dysfunction - Pregnancy - Medication for cardiac failure - History of cerebrovascular accident and/or myocardial infarction within 6 months |
Symptoms+physical exam | 95 patients randomly assigned into 2 groups which received the same 2 treatments but in reverse order (ITV to ITO first n = 49; ITO to ITV first n = 46) | Patients were treated for a period of 2 weeks, 3 days a week, switching treatment mode after 1 week. They received 10’ traction with 30″ hold 5″ rest, with 40% bw traction force |
6 check-points were conducted during the 2 weeks of observation, assessing each time | Both treatments significantly improved the JLEQ score compared to pre-treatment |
| LBP with or without radicular pain—comparison: different traction forces | |||||||
| van der Heijden et al, 1991, The Netherlands | - 25 to 65 years - Chronic LBP (more than 3 months), with or without radiation |
- Previous lumbar traction treatment - Ongoing psychiatric or psychological treatment - Inguinal hernia - Pregnancy - Malignancy - Scheuerman, Bechterew, or Ehier–Danlos syndrome - Osteoporosis - Previous thoracic, lumbar, or pelvic fracture, surgery or dislocation - Hemiplegia - Local acute inflammation - Lower limb dysmetria (more than 5 cm) - Cardiac or bronchial disorders - Previous lumbar disc herniation - Spondylosis, spondylolostesis - Hemilumbarization, hemisacralization - Congenital hip dysplasia |
Not specified | 25 patients, randomized into 2 groups: - High dose (30% to 50% bw) group (n = 13) - Low dose/sham (max 25% bw) group (n = 12) |
During a 4-week period, at most 3 times/week (10 to 12 sessions), patients underwent a 20-minute continuous mechanic lumbar traction treatment in supine position. Every patient also received an LBP-management pamphlet for at-home self-treatment |
At baseline, at the end of treatment, and 1 month after: - Pain (VAS) - ADL impact (VAS) - Disability (Roland and Morris Disability Questionnaire (RMDQ)) |
- Better VAS score compared to placebo, no statistically significant difference - ADL impact has better score at end of treatment in placebo groups; both groups have the same improvement at FU assessment, with no statistically significant difference compared to baseline - Both groups have little improvement with no significant difference inter and intra-group at RMDQ score |
| Schimmel et al, 2009, The Netherlands | - LBP for more than 3 months - Bulging disc - Lumbar degenerative disc disease |
- Previous surgical treatment with dynamic stabilization, fusion or disc replacement - Radicular leg pain - Malignancy - Pregnancy - Osteoporosis |
Symptoms+physical exam | 60 patients randomized into 2 groups: - Intervertebral Differential Dynamics Therapy with 50% bw+4.45 kg traction weight (n = 31) - Sham Therapy with 4.45 kg traction weight (n = 29) |
20 traction sessions during 6 weeks, combining - 25’-30’ intermittent traction with the patient in supine position - Massage, heat, blue relaxing light, and music during the treatment session The traction treatment was held 5 times/ week for the first 2 weeks, thrice/week the second 2 weeks, twice/week for the last 2 weeks - 2 weeks after the start of the traction sessions, a standard graded activity program was added (1 h training 2 days/week for 12 weeks, always on different days compared to the traction sessions) |
At baseline, at the end of treatment, and 8 weeks after: - Back pain (VAS) - Leg pain (VAS) - Disability (Oswestry Disability Index) - Health Status (Short Form 36) - Kinesiophobia (Tampa Scale) |
- LBP VAS score significantly decreased in both groups at the FU measurement, with no differences among them. No time × group interaction detected - ODI, SF-36, and leg pain VAS score significantly improved at the end of treatment in both groups, with no significant differences among them. - Tampa Scale score showed no improvement at the end of treatment and no differences among the groups |
| Beurskens et al, 1995, The Netherlands | - Nonspecific LBP for at least 6 weeks - 18 years old or more |
- Previous lumbar traction treatment - Underlying diseases or anatomic abnormalities (malignancy, osteoporosis, etc.) - Significant improvement during the previous 2 weeks |
Not specified | 151 patients randomized into 2 groups: - High dose (35% to 50% bw traction force) group (n = 77) - Low dose/sham (20% bw traction force) group (n = 74) |
5 weeks duration, 12 treatment sessions Patient on a traction table in semi-Fowler position, receiving 20’ continuous motorized lumbar traction Patients were allowed to continue taking pain medication they had used before entry into the study |
At baseline and at the end of treatment - Main complaint (VAS) - Second main complaint (VAS) - Pain at the moment (VAS) - Pain during last week (VAS) - Functional Status (Roland and Morris Disability Questionnaire) - Severity of LBP (11 point scale) - Spine ROM (inclinometer) |
- Both groups significantly improved in all of the items except for the back ROM, but no significant differences among them |
| Beurskens et al, 1997, The Netherlands | - Nonspecific LBP for at least 6 weeks - 18 years old or more |
- Previous lumbar traction treatment - Underlying diseases or anatomic abnormalities (malignancy, osteoporosis, etc.) - Significant improvement during the previous 2 weeks |
Not specified | 151 patients randomized into 2 groups: - High dose (35% to 50% bw traction force) group (n = 77) - Low dose/sham (20% bw traction force) group (n = 74) |
5 weeks duration, 12 treatment sessions Patient on a traction table in semi-Fowler position, receiving 20’ continuous motorized lumbar traction Patients were allowed to continue taking pain medication they had used before entry into the study |
At baseline, at 12 weeks, and 6 months - Main complaint (VAS) - Second main complaint (VAS) - Pain at the moment (VAS) - Pain during last week (VAS) - Functional Status (Roland and Morris Disability Questionnaire) - Severity of LBP (11-point scale) - Spine ROM (inclinometer) |
- Both groups significantly improved in all of the items except for the back ROM, but no significant differences among them |
| LBP with or without radicular pain—comparison: different traction positions | |||||||
| Beyki et al, 2007, Iran | - Chronic LBP (more than 3 months) - Discogenic origin of the pain cleared by clinical examination - Symptoms, signs, and clinical exam correlate with MRI |
- Osseous stenosis - Unstable spine - Previous spinal surgery - Spinal pain due to tumors, infection, inflammatory diseases - Pregnancy - Formal therapeutic or medical intervention within the last 3 months - Cardiac or respiratory conditions, neurological disorders or organ disease - Long-term oral steroid intake - History of major psychiatric illness |
Symptoms+physical exam | 124 patients, randomized into 2 groups: - Prone group (n = 62) - Supine group (n = 62) |
1-month duration, 6 sessions every other day and 4 sessions every 3 days - 15 minutes of TENS with Hot Pack - 15 minutes of prone or supine intermittent mechanic traction Traction force: 35% to 50% body weight |
At baseline and after treatment - Pain (VAS) - Disability (ODI) |
- VAS score significantly improved in both groups, with meaningful differences prominent in prone group - ODI score significantly improved in both groups, meaningful differences prominent in prone group |
| Kim et al, 2013, South Korea | - LBP in everyday life - Diagnosed after x-ray, CT, and MRI scans - Duration of the symptoms at least 12 weeks |
- Past or present neurological, hypertension, cardiopulmonary diseases, etc. - Chronic diseases, surgery for LBP. - Abnormal ophthalmic artery pressure during inversion |
Symptoms+physical exam | 47 patients, randomized in 3 groups: - Supine group (n = 15) - Inversion -30° group (n = 18) - Inversion -60° group (n = 14) |
8 weeks duration, 4 times per week - 20 minutes of intermittent inversion traction in supine position, lying on a motorized gravitational machine Traction force: not specified |
At baseline and after treatment: - Pain (VAS) - Night pain (VAS) - Flexibility of lumbo-sacral joint (seat and reach test, back extension from prone position (cm)) - Isokinetic strength of trunk muscles at 60°/s (flexor and extensor peak torque (Nm)) |
- VAS score, Lumbar flexibility, Isokinetic torques at 60°/s significantly improved in both groups |
| LBP with or without radicular pain—comparison: different hold and rest time combinations | |||||||
| Santhumayor et al, 2016, India | - Age 18-45 - Lumbar IVDP stage of degeneration/protrusion confirmed by radiography - Acute and subacute IVDP (<12 weeks) - VAS score more than 3 on a 10-point scale |
- Previous spinal surgery - Last stage of IVDP (sequestration) - Therapeutic or medical intervention within the last 3 months - Conditions as ankylosing, spondylitis, spondylolisthesis, RA, spinal stenosis, spinal fracture or tumor, osteoporosis - Any systemic condition - Long-term oral steroid intake - Pregnancy - Hip pathologies |
Symptoms+physical exam | 40 patients randomly assigned into 4 different groups | All patients received intermittent traction delivered through similar traction apparatus, once a day for 1 week, for 15-20 minutes per session | Before and 1 week after the intervention | Groups with longer hold and rest time (60/10, 80/20) showed greater improvement in lumbar mobility and SLR score, reduction in disability, and VAS score. |
| LBP with radicular pain—comparison: different traction forces | |||||||
| Isner-Horobeti et al, 2016, France | - Lumbar sciatica of less than 6 weeks duration secondary to disc herniation - Pain radiating down the leg, along the distribution of the sciatic nerve - SLR + |
- Duration of symptoms more than 6 weeks - Signs of clinical neurologic deficit - Lumbar sciatica not caused by disc herniation - Presence of abnormalities on lumbar tomodensitometry - Pregnancy - Patients aged less than 18 years - Patients on medical leave for more than 3 weeks at inclusion - History of lumbar surgery or previous lumbar traction therapy |
Symptoms+physical exam | 17 patients randomly divided into 2 groups: - High-level (50% of BW, LT50) group (n = 8) - Low-level (10% of BW, LT10) group (n = 9) |
Patients received 10 lumbar traction sessions (5 per week for 2 weeks) - They rested in Fowler position receiving a traction force that was progressively applied for 5’, and subsequently maintained at the target level continuously for 20’. At the end of the session, relaxation was done progressively for 5’ - Patients could take their usual medications |
At baseline, at the end of treatment, and after 2 weeks: - Radicular pain (VAS) - Mobility of the lumbo-pelvic-hip complex (Finger-To-Toe test (FTT)) - Lumbar spine mobility (Schöber–Macrae test) - Signs of nerve root compression (SLR) - Functional impairment (validated French version of the Roland and Morris Disability Questionnaire) |
- In both groups, a statistically significant improvement was found for all the outcome but the Schöber test. No statistically meaningful difference was found when considering the inter-group analysis - No interaction effect was noted for VAS, FTT, SLR or Roland and Morris score - No differences were observed within or between groups for Schöber–Macrae test. |
| Murat et al, 2018, Turkey | - Lumbar disc herniation diagnosed after clinical evaluation and MRI - Pain in the back of the leg - Duration of the symptoms between 2 weeks and 3 months |
- Pregnancy - Previous lumbar spine surgery or traction therapy - Progressive neurological loss - Umbilical, hiatal, and inguinal hernia - Malignancy - Infectious disease - Inflammatory pathologies - Severe lung and cardiovascular disease |
Symptoms+physical exam | 61 patients randomized into 2 groups: - Traction group (n = 30) - Placebo traction group (n = 31) |
2-week duration 10 daily sessions (5/week) combining: - 20’ of intermittent lumbar traction of 35% to 50% bw or 10% to 20% bw - 20’ of 250 watt infrared 50 cm from the area - PT program, exercises to strengthen abdominal and back muscles Patients were allowed to use up to 4000 mg of paracetamol tablets |
At baseline, at the end of treatment, and 40 days after: - Pain at rest and during activities (VAS) - Disability (Oswestry Disability Index - ODI and Roland and Morris Disability Questionnaire (RMDQ)) - Quality of life (Short Form 36 (SF-36)) |
- VAS values at rest and exercise and RMDQ scores significantly improved between pretreatment and first control in both groups. - ODI scores significantly improved for the study group. - SF-36 scores showed statistically significant improvement in both groups. - No statistically significant difference between groups |
| Reust et al, 1988, Switzerland | - Lumbosciatalgia with or without neurological deficit | - Previous lumbar traction treatment - Rapid progressive neurological loss - Behavioral problems - Referred allergies to diclofenac, diazepam, or heparin - Previous gastroduodenal problems - Specific bone diseases at the origin of the symptoms (spondylolysis, osteoporosis with settlements) |
Not specified | 60 patients randomized into 3 groups: - Placebo (5 kg) traction group (n = 20) - Light (15 kg) traction group (n = 22) - Normal (up to 50 kg) traction group (n = 18) |
12 days duration, with consecutive daily treatment combining - 10’ continuous mechanic traction, lying supine on a traction table - Lit Strict, diclofenac 3 × 50 mg/day, diazepam 5-5-10 mg/day, Heparin 3 × 5000 U sc/day - 20’ Lumbar parafango - 20’ Muscle relaxing massage therapy |
At baseline and at the end of treatment: - Pain (VAS) - Back mobility (Finger-Floor distance) - Neural tension (Lasègue) |
- Pain and Lasègue scores showed a statistically significant improvement in all 3 groups, no significant differences between them - Finger-To-Floor score significantly improved in placebo and light traction group (no significant difference between groups), but not in normal traction group |
| Weber H. 1973, Germany | - Radiating pain and neurological signs corresponding to a lesion in the L5 and/or S1 root - Positive radiculogram |
- Bladder paresis - Strong persistent pain - Acutely occurring paresis - Considerable constraint of the spinal column |
Symptoms+physical exam | 72 patients randomly assigned into 2 groups: - Actual traction group (n = 37), traction force corresponding to 1/3 bw - Sham traction group (n = 35), traction force of 7 kg |
Patients had to lie supine on a Tru-Trac traction table. Intermittent traction was administered 20’ a day, daily, for 5 to 7 days |
At baseline and at the end of treatment: - Lumbar spine mobility in sagittal and frontal plane - Lasègue test - Achille’s reflex - Motility (isometric strength in plantar and dorsal flexion of the foot, extension of the big toe, eversion of the foot, flexion of the knee, abduction and extension of the hip) - Sensory function (pin pricking) - Need for analgesic - Back and leg pain (NRS) |
- No effect on lumbar spine mobility, sensory function and need for analgesic - No definite differences between groups for Lasègue test and Achille’s reflex - General increase in strength in both groups, no systematic trend comparing the groups; no beneficial effect on the paresis - A certain reduction of pain was detected, with no differences among groups. |
|
LBP with radicular pain—comparison: different traction positions
| |||||||
| Bilgilisoy-Filiz et al, 2018, Turkey | - Age 18-65 years, - Chronic LBP with accompanying radiculopathy of L4-L5, L5-S1, or L4-S1 for more than 3 months - Moderate symptoms severity (pain threshold of 4/10 VAS) |
- LBP due to neoplastic, inflammatory or infectious causes - Indication of urgent surgery (cauda equina syndrome, progressive motor deficit) - Previous spinal surgery - Pregnancy or early post-partum period (6 months) - Co-existing medical conditions (severe central or foraminal spinal stenosis with narrowing of the normal canal cross-sectional area by more than 2/3; osteoporosis, gross structural abnormalities such as spondylolisthesis or scoliosis, ankylosing spondylitis, spinal fracture, spinal tumor) |
Symptoms+physical exam | 125 patients randomized into 3 groups: - Supine traction group (n = 42) - Prone traction group (n = 41) - No traction group (n = 42) |
Patients in traction groups received 15 sessions of treatment, 5/week for 3 weeks total, combining: -15’ intermittent mechanical lumbar traction, lying on a traction table in Fowler position or prone position. Traction force of 25% to 50% bw. - Standard PT program, with 20’ low-back HP, 10’ continuous ultrasounds, 20’ of low back TENS All patients asked to perform home exercises (strengthening of paraspinal and abdominal muscles, and stretching for back extensors, hamstrings, and calf muscles) |
At baseline and at the end of treatment - Pain (VAS) - Back mobility (Schöber test) - Disability (Oswestry Disability Index) |
- There were statistically significant improvements in all groups for all outcomes. - The between-groups analysis showed a greater improvement in all outcomes in the prone group compared to the other 2, statistically significant for ODI and VAS scores. |
|
LBP with radicular pain—comparison: different traction types
| |||||||
| Choi et al, 2015, South Korea | - Radiating pain caused by LBP (more than 3 months) | - Previous lumbar surgery - Malignancy - Intervertebral disc infection - Inflammatory diseases (e.g., rheumatism) - Fractures or other contraindications for manual therapy |
Symptoms+physical exam | 30 patients randomized into 2 groups: - Spinal decompression therapy group (n = 15), receiving intermittent traction from level 5 up to the maximum tolerated - General traction therapy group (n = 15), receiving the most traction tolerated, from 1/3 up to 50% bw (not specified whether continuous or intermittent traction) |
During a 4-week period, patients underwent 3/week the following treatments: - Conservative physical therapy with 20’ HP, 15’ Interferential current therapy and 5’ ultrasounds - 20’ traction (through a spinal decompression or a traction device), both in supine position |
At baseline and at the end of treatment - Pain (VAS) - Neural tension (SLR test) - Disability (Oswestry Disability Index) |
- Both groups showed statistically significant improvement in VAS, ODI, and SLR scores. - The comparison between the 2 groups found no statistically meaningful differences |
| Güevenol et al, 2000, Turkey | - Complaint of LBP and lower extremity pain of not less than 1 month - Lumbar disc herniation diagnosed by CT |
- Previous spinal surgery - History of cerebrovascular accident, thyroid disorders, hypertension, cardiac disorders - Previous hiatus hernia - Previous glaucoma, detachment of retina - Chronic obstructive and restrictive lung disorders - Osteoporosis and excessive joint laxity - Malignant, inflammatory, infectious, metabolic, congenital, and developmental disorders of the spine |
Symptoms+physical exam | 31 patients randomized into 2 groups: - Inverted traction group (n = 16) - Conventional traction group (n = 15) |
Both groups received the treatments daily for 10 days, combining: - 20’ continuous traction (30 to 45 kg traction force) in supine position for the conventional traction group, or 5 to 10’ inverted gravitational traction in the inversion traction group - 15’ infrared radiation to heat superficial tissues - Abdominal and gluteal muscle exercises Patients were not allowed to take non-steroid anti-inflammatory drugs throughout the study. Analgesics were given as needed. Bed rest was required for all patients |
At baseline, at the end of treatment, and 3 months after - Pain cluster 1: morning pain, pain throughout the day, night pain, pain with Valsalva maneuver, radicular pain (VAS) - Pain cluster 2: flexion, extension, lateral flexion, rotation - Lumbar spine mobility (Finger-To-Floor distance) - Neural tension (SLR) |
- A significant increment in SLR from pre- to post-treatment was obtained in both groups - Pain clusters 1 and 2 showed a meaningful decrement from pre- to post-treatment in both groups - There were similar changes from pre-treatment to follow up - No statistically significant difference between the post-treatment and the FU values was found in both groups - No statistically meaningful difference between any of the parameters tested comparing the groups was found |
| Kocak et al, 2018, Turkey | - Diagnosis of lumbar disc herniation - Protruding disc herniation according to the MRI - Longer than 3 months duration LBP |
- Extruded and/or sequestrated LDH, spinal compression fracture, spondylolisthesis, vertebral infection - Lumbar spinal injection or lumbar surgery history, spinal fusion - Physical therapy and rehabilitation session during the past 6 months - Cognitive dysfunction - Neurological deficits, severe peripheral neuropathy - Pregnancy - Malignancy - Aortic aneurysms - Rheumatic diseases - Moderate-to-severe depression, as assessed by a Beck Depression Inventory (BDI) score of ≥19. |
Symptoms+physical exam | 48 patients randomized into 2 groups - Conventional motorized traction group (n = 24), with traction force of 25% up to a maximum of 50% bw - Non-surgical spinal decompression group (n = 24), with traction force of 50% bw—10 pounds up to 50% bw+10 pounds |
20 sessions over 6 weeks (5 days/week during first 2 weeks, 3 days/week during the following 2 weeks, and 2 days/week during the last 2 weeks), combining: - 20’ HP and 20’ TENS - 30’ intermittent mechanical traction, applied to the patient in supine position - At the second week, patients were instructed on exercises to strengthen low back and abdominal muscles Patients could take paracetamol during treatment period |
At baseline and at the end of treatment: - Pain (VAS) - Functional status (Oswestry Disability Index - ODI) - Quality of life (Short Form-36) - State of depression mood (Beck Depression Inventory - BDI) |
- A statistically significant decline was found in the VAS, ODI, and BDI scores after treatment in both groups - Except for 2 subgroups (physical role restriction in the NSD group and pain in the CMT group), no significant changes were observed in the SF-36 Form. - No significant difference was observed in the evaluation outcomes after treatment between groups. |
ADL, Activities of Daily Living; BDI, Beck Depression Inventory; BW, Body Weight; CMT, Conventional Motorized Traction; CT, Computed Tomography; FTT, Finger to Toe Test; FU, Follow Up; HP, Hot Packs; ITO, Intermittent Traction Only; ITV, Intermittent Traction with Vibration; IVDP, Acute Inter-Vertebral Disc Prolapse; JLEQ, Japan Low back pain Evaluation Questionnaire; LBP, Low Back pain; LDH, Lumbar Disc Herniation; MRI, Magnetic Resonance Imaging; Nm, Newton meter; NRS, Numerical Rating Scale; NSD, Non-surgical Spinal Decompression; ODI, Oswestry Disability Index; PT, Physical Therapy; RA, Rheumatoid Arthritis; RMDQ, Roland & Morris Disability Questionnaire; ROM, Range Of Motion; SF-36, Short-Form 36; SLR, Straight Leg Raising; TENS, Transcutaneous Electrical Nerve Stimulation; VAS, Visual Analogue Scale. ADL, Activities of Daily Living; BDI, Beck Depression Inventory; BW, Body Weight; CMT, Conventional Motorized Traction; CT, Computed Tomography; FTT, Finger to Toe Test; FU, Follow Up; HP, Hot Packs; ITO, Intermittent Traction Only; ITV, Intermittent Traction with Vibration; IVDP, Acute Inter-Vertebral Disc Prolapse; JLEQ, Japan Low back pain Evaluation Questionnaire; LBP, Low Back pain; LDH, Lumbar Disc Herniation; MRI, Magnetic Resonance Imaging; Nm, Newton meter; NRS, Numerical Rating Scale; NSD, Non-surgical Spinal Decompression; ODI, Oswestry Disability Index; PT, Physical Therapy; RA, Rheumatoid Arthritis; RMDQ, Roland & Morris Disability Questionnaire; ROM, Range Of Motion; SF-36, Short-Form 36; SLR, Straight Leg Raising; TENS, Transcutaneous Electrical Nerve Stimulation; VAS, Visual Analogue Scale.
Results at follow-ups were classified as short-, mid-, and long- (longer than 6 months) term. In this review, we analyzed results on pain and disability at short-term follow-ups (up to 3 months post-intervention), because long-term follow-up was reported in only 1 study.23
Of the 16 RCTs selected for qualitative analysis, 1 included patients who complained of LBP without LR and compared mechanical traction combined with additional vibration vs. mechanical traction alone;24 7 included patients who complained of LBP with or without LR; of those, 4 compared the same traction delivered with different force amounts 23,25-27; 2 compared traction delivered in different positions,28,29 and 1 compared intermittent traction delivered with different hold and rest time combinations.30 Eight RCTs included patients who complained of LBP with LR; 4 compared different traction forces,31-34 1 same traction delivered in different positions,35 and 3 different traction types.36-38 The information collected through the qualitative analysis is summarized in Table 1.
We pooled together studies on the same population subgroup, comparing different traction delivered in treatment and control groups, and analyzing the same outcomes through similar measures, at the same follow-up time. Of the 16 RCTs selected, 5 met the criteria for quantitative synthesis, the others being only considered for the qualitative analysis. The studies included in our meta-analysis were conducted in France,31 Switzerland,33 Turkey,32,38 and South Korea36 and were published between 1988 and 2018.
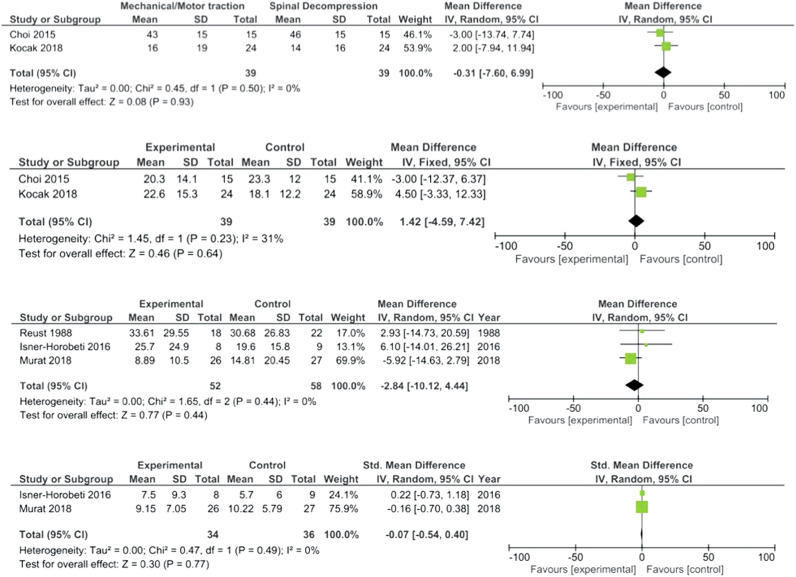
Of these articles, 2 compared different types of tractions, and the meta-analysis considered the effects on pain and disability.36,38 The other 3 compared tractions with different force amounts;31-33 for all these 3 studies, we meta-analyzed data on pain, whereas for 2 out of 3 also on disability.31,32 Short-term results were considered for all included studies. Effect sizes and associated 95% CIs were calculated and reported for each outcome. Meta-analyses are also presented in forest plots depicting the effect size calculated for each study by the outcome as well as the overall effect size obtained for the outcome across studies at each time interval. They also indicate whether the effects obtained across studies favor the control or the intervention group (Figure 2).
Figure 2.
Results of meta-analyses (between-groups comparisons).
Comparison between different tractions types/parameters
Mechanical traction delivered in different positions
Two RCTs compared traction delivered in prone vs. supine position (Beyki et al, 2007;28 Bilgilisoy-Filiz et al, 201835), while 1 RCT compared different inversion angle: 0° vs. −30° vs. −60° (Kim et al, 201329). Due to the heterogeneity of studies for population (Beyki et al28 included LBP with or without LR, whereas Bilgilisoy-Filiz et al35 only patients with LR) or intervention, no meta-analysis was performed.
Mechanical traction delivered with different hold and rest time combinations
One RCT (Santhumayor et al, 201630) compared intermittent traction delivered with 20 seconds hold and 1 second rest vs. 40 seconds hold and 5 seconds rest vs. 60 seconds hold and 10 seconds rest vs. 80 seconds hold and 20 seconds rest.
Mechanical traction combined with additional vibration versus mechanical traction alone
One trial (Tanabe et al, 2021324) compared intermittent traction (repeated cycles for 30 seconds hold and 5 seconds rest, for a total of 10 minutes) added to 10 minutes of vibration vs. intermittent traction alone.
Mechanical traction versus spinal decompression
Three RCTs compared mechanical traction (delivered by motorized devices performing general traction), to other traction modalities: spinal decompression, inducing segmental traction (Choi et al, 2015;36 Koçak et al, 201838), and inversion spinal traction (Güvenol et al, 200037). Given the similarity between mechanical traction and spinal decompression, we pooled together 2 studies (Choi et al, 2015;36 Koçak et al, 201838), including 78 participants with a mean age of 43 years, who complained of persistent LBP with LR.
Patients were treated in supine position, during a period of 4 to 6 weeks for 12 to 20 sessions lasting 20 to 30 minutes. Short-term follow-up was made at the end of treatments for both studies. No participant was lost to follow-up.
Outcome: pain. The mean difference was −0.31, CI ranging from −7.60 to 6.99. The overall effect (Z) was 0.08, with non-significant P-value = .93.
Outcome: disability. The mean difference was 1.42, CI ranging from −4.59 to 7.42. The overall effect (Z) was 0.46, with non-significant P-value = .64.
High-force versus low-force traction
Eight RCTs made a comparison between the same traction delivered with different traction forces. Six studies compared the effects of traction force equal to 30% to 50% of bw for the experimental groups and 10% to 25% bw for the control group (Beurskens et al, 1995;27 Beurskens et al, 1997;23 Isner-Horobeti et al, 2016;31 Murat et al, 2018;32 Reust et al, 198833; van der Heijden et al, 199125); 1 RCT compared 50% bw + 4.45 kg to 4.45 kg traction force (Schimmel et al, 200926), and 1 article compared 1/3 bw to 7 kg traction force (Weber, 197334).
Three RCTs (Isner-Horobeti et al, 2016;31 Murat et al, 2018;32 Reust et al, 198833) were pooled together on 118 participants with a mean age of 41 years who complained of LBP with LR. Participants received traction in supine position, with intermittent32 or continuous31-33 modality. Treatment lasted 10 to 20 minutes for 10 to 12 sessions within 2 weeks. The outcomes were measured only at post-treatment. Participants were divided into 2 groups (effective and sham traction), the first one receiving mechanical traction with force >30% bw, and the other one receiving the same traction with force <20% bw. The 25% bw was taken as a threshold value. Eight participants were lost to follow-up; all of them took part in Murat et al’s32 study.
Outcome: pain. The mean difference was −2.84, CI ranging from −10.12 to 4.44. The overall effect (Z) was 0.77, with non-significant P-value = .44.
Outcome: disability. The mean difference was −0.07, CI ranging from −0.54 to 0.40. Test overall effect (Z) was 0.30, with non-significant P-value = .77.
No meta-analysis reached statistical significance: no difference emerged in the considered outcomes between different traction delivering. More specifically, no difference was observed between mechanical traction and decompression, or high-force vs. low-force traction.
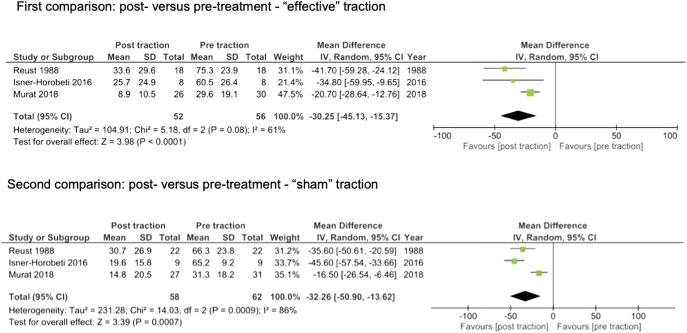
Clinical significance of effects
The within-groups analyses, aiming to explore the clinical significance of traction for pain, were performed on the studies which compared different traction forces. Both effective (−30.25) and sham (−32.26) traction groups reached the MCID at post-treatment compared to pre-treatment for pain (see Figure 3).
Figure 3.
Results of meta-analyses (within-groups comparisons).
Adverse events
Side effects related to traction among the meta-analyzed studies were only found in 1 study (Murat et al, 201832), reporting that 3 participants out of 61 had severe pain at the end of treatment and 1 showed neurological deficiency at follow-up; all these 4 patients took part in the experimental group (high-force traction).
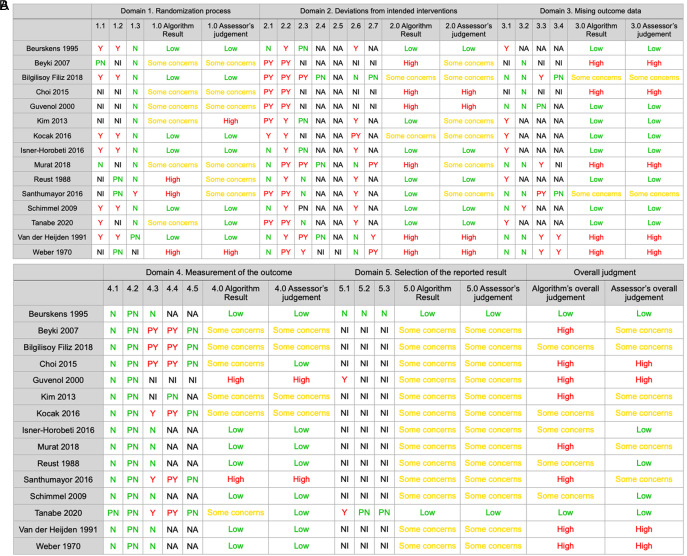
Risk of bias and quality assessment
The Cochrane Collaboration’s Risk of Bias (RoB 2.0) tool was applied to all studies included in the qualitative analysis. The follow-up study published by Beurskens et al23 was considered together with the original study of the same author.27 The risk of bias analysis showed that only 5 studies have a low risk of bias, whereas 6 have some concerns and 4 have a high risk of bias (see Figure 4).
Figure 4.
Risk of bias assessment. Y. Yes, N: No, PN: Probably No, PY: Probably Yes, NA: Not applicable, NI: No information.
The results on quality assessment according to GRADE criteria were applied to the 5 meta-analyzed studies and showed that low quality of evidence supports the results concerning the comparison between different traction forces and very low quality of evidence supports the results concerning the comparison between different traction types. A complete description of quality of evidence for each comparison and each outcome is shown in Table 2.
Table 2.
Results of GRADE assessment
| Traction vs. traction | |||||||
|---|---|---|---|---|---|---|---|
| Quality | Summary of findings | ||||||
| Outcome (no. of studies) | RoB | Inconsistency | Indirectness | Imprecision | No. of participants | Effect size (SMD) with CI | GRADE |
| Effective traction vs. “sham” traction | |||||||
| Pain31,32,33 | Serious | Not serious | Not serious | Serious | (60 + 17 + 61) = 138 | −2.84 (−10.12, 4.44) | Low |
| Disability31,32 | Serious | Not serious | Not serious | Serious | (17 + 61) = 78 | −0.07 (−0.54, 0.40) | Low |
| Mechanical traction vs. spinal decompression | |||||||
| Pain36,38 | Serious | Serious | Not serious | Serious | 39 | 1.42 (−4.59, 7.42) | Very low |
| Disability36,38 | Serious | Serious | Not serious | Serious | 39 | −0.31 (−7.60, 6.99) | Very low |
SMD, standardized mean difference.
Discussion
This review aimed to investigate the comparative effectiveness of different traction modalities on pain and disability, in adults who complained of LBP with or without LR. This systematic review sub-grouped RCTs according to Population, Intervention, Comparator/control, and Outcome model. Although several different types of traction are investigated in the literature, only few studies compared different traction devices or modalities with each other. Out of the 16 included RCTs, due to the lack of homogeneity in participants’ selection and traction parameters, only 5 studies on the population who complained of LBP with LR could be pooled together.31-33,35-37 Our meta-analysis considered only the short-term effects on pain and disability in patients with LBP and LR, comparing different traction devices or the same traction delivered with different parameters.
No significant difference appeared by comparing the same type of traction delivered with different forces. Regarding the hypothesized superiority and selectivity of spinal decompression compared to common mechanical traction, our meta-analysis did not show higher results using this modality vs. mechanical traction, on pain and disability.
Only single studies showed some differences between different traction positions (better results in prone vs. supine position28,35 and better results with −60° inversion traction angle29), between different hold and rest time (better results with 60-80 seconds hold and 10-20 seconds rest30), or between intermittent traction with vibration vs. intermittent traction only (better results with the addition of vibration24).
Several mechanisms have been proposed to explain the effects of traction (e.g., elongation of soft tissues around the facet joints, correction of displaced intervertebral discs and facet joints, separation of facet joints, expansion of intervertebral foramina, reduction of intervertebral discs pressure, reduction of disc protrusions, elongation of anterior and posterior longitudinal ligaments, relaxation of muscle spasm, improvement of blood circulation, and psychological effects).10
According to the biomechanical model, separation of vertebral bodies, distraction of lumbar joints, and widening of intervertebral foramina have been shown as a result of lumbar traction.5 Also a reduction of intradiscal pressure and an increased level of oxygen, nutrients and water content, with higher intervertebral disc height, particularly in the posterior regions of lower lumbar discs, have been demonstrated.12,39
Concerning the amount of traction force, according to Judovich et al.41,42 a force of at least 26% of the patient’s bw should be used to obtain a separation between vertebrae and traction of less than 25% of patient’s bw should be considered as a “sham” traction. However, our between-groups meta-analyses yielded similar results regardless of the different traction forces. The equivalence of results between high-force and low-force traction may confirm the hypothesis that the effects of traction may not be only mechanical but also neurophysiological.
A reduction of muscle spasm, together with inhibition of nociceptive impulses and increasing mobility, have been hypothesized. However, no significant differences emerged after traction in studies on spinal muscles tone,42 and short-term effects of traction on morphology and mechanical properties of lumbar muscles (thickness and stiffness) appear conflicting.43,44
According to the same mechanisms hypothesized for manual therapies,45 other effects may be suggested. Stimulation of mechanoreceptors, provoking a decrease of sensitivity within the muscle spindles and the increase or the pressure pain threshold, as well as pain modulation and inhibition of ectopic impulse generators, may be taken into consideration as possible traction-induced effects.46 This hypothesis could be confirmed by the better results obtained by combining distraction force with additional vibration, probably due to a stronger stimulation of the somatosensory system.47 These effects seemed not in direct relation to the force exerted, being also low-threshold stimuli clinically effective.48
Given the equivalence in results between different tractions, it could be concluded that lumbar traction is ineffective, in line with some systematic reviews.1-5 However, taking into consideration pre- and post-treatment within-groups analysis, this assumption may be disputed. In fact, our review showed clinically significant effects on pain, regardless of different traction forces. The lack of a control group which did not receive traction must be considered as a limitation; however, from a clinical point of view, these results are in line with the more recent reviews on lumbar traction.6-9
Adverse events were reported in only 1 study32 and were related to high-force traction. The results of this systematic review provide physical therapists with some suggestions for avoiding such episodes, by delivering low-force traction, well tolerated by patients and not related to worsening symptoms in any study.
The major strengths of our study are the extensive search, reducing the publication bias, and the selection, risk of bias, and qualitative assessment independently done by 2 authors.
Limitations
The small number of studies included in quantitative synthesis is the most important limitation of this review. Including only RCTs may have influenced the potential publication bias and we do not exclude that negative studies were not published. Because of the relatively scarce studies retrieved within the different subgroups, it was not possible to conduct a sensitivity analysis.
No study included in quantitative synthesis declared a registered protocol, including the statistical analysis intention, and thus, it was difficult assessing reporting bias. Very often, no information was reported about dropouts, and even if they are reported, the data related to the participants who have not completed the study were not specified. Several studies were excluded due to incomplete data on the outcomes, mostly when only percentages of improvement or worsening were reported, instead of pre- and post-treatment means and standard deviations. All the authors of these studies were contacted to obtain complete data, but only in 2 cases, an exhaustive answer was obtained. In other cases, we were not able to retrieve full texts or complete data, forcing the exclusion of some studies.
Concerning internal validity, several articles did not report the randomization method, preventing the authors from evaluating whether this was appropriate or not. The lack of double blind was a common finding in the RCTs analyzed: the physical therapist delivering the treatment was always informed about the patient’s allocation, or there was no clear statement about the clinician’s blindness. In 7 out of 16 articles, the patient was blind to the assignment; in the other cases, information about the blinding was not reported or impossible, due to the study design, when different devices or positions were used. Only 5 studies have a low risk of bias, and this may have reduced the strength of our results.
Concerning GRADE assessment, only very low- to low-quality evidence supports our results.
Further research is highly likely to have an important impact on the estimate of effect. We suggest improving the quality of future RCTs in this field to reduce biases in future systematic reviews, especially by more rigorous selection and definition of participants and treatments. As recently suggested, better patient stratification49 and parameter setting in a repeatable way, according to therapeutic goals,50 may be the future of studies on lumbar traction.
Conclusion
This systematic review with meta-analysis did not find any significant difference in results on pain and disability using different types of traction (lumbar decompression vs. mechanical traction) or the same traction delivered with different forces (using high-force vs. low-force traction).
Clinically significant effects of traction on pain in adults who complained of LBP and LR emerged, regardless of traction force delivered. Traction may be considered a therapeutic tool for the short-term reduction of pain and disability in patients with LBP and LR. A clinician can use it regardless of the availability of devices able to carry out traction on specific levels or deliver high-force amount since it can be administered with different parameters without losing its effectiveness.
Footnotes
Author Contributions: Concept – C.V., P.P.; Design – C.V., P.P.; Supervision – A.G., C.V., P.P.; Materials – A.P., K.S., L.T.; Data Collection and/or Processing – A.P., C.V., K.S., L.T.; Analysis and/or Interpretation – A.P., C.V., K.S., L.T.; Literature Review – C.V., K.S.; Writing – A.G., A.P., C.V., K.S., L.T., P.P.; Critical Review – A.G., P.P.
Acknowledgments: We thank Silvia Giagio for performing statistical analysis.
Declaration of Interests: The authors have no conflicts of interest to declare.
Funding: The authors declared that this study has received no financial support.
Appendix 1. Details of search strings adopted for each database.
PUBMED
("traction"[MeSH Terms] OR traction*[All Fields] OR distraction*[All Fields]) AND ("low back pain"[MeSH Terms] OR "back pain"[MeSH Terms] OR "spinal pain"[All Fields] OR lumbar* OR "lower extremity"[MeSH Terms] OR "leg pain"[All Fields]) AND ("intervertebral disc degeneration"[MeSH Terms] OR "intervertebral disc displacement"[MeSH Terms] OR "discopathy" OR "radiculopathy"[MeSH Terms] OR "sciatica"[MeSH Terms] OR "radicular syndrome"[All Fields] OR "nerve root pain"[All Fields] OR “radicular pain”[All Fields])
CINAHL
traction OR distraction
AND "low back pain" OR "lumbar pain" OR "lumbar spine pain" OR "leg pain" OR "lower extremity"
AND "disc displacement" OR "disc degeneration" OR radiculopathy OR sciatica OR radicular OR "nerve root"
PEDRO
traction*
COCHRANE
#1 MeSH descriptor: [Traction] explode all trees
#2 (traction);ti,ab,kw
#3 (distraction);ti,ab,kw
#4 MeSH descriptor: [Low Back Pain] explode all trees
#5 ("spinal pain");ti,ab,kw
#6 (lumbar);ti,ab,kw
#7 ("lower extremity");ti,ab,kw
#8 ("leg pain") ti, ab, kw
#9 MeSH descriptor: [Radiculopathy] explode all trees
#10 MeSH descriptor: [Sciatica] explode all trees
#11 ("nerve root");ti, ab, kw
#12 (radicular);ti, ab, kw
#13 ("disc degeneration");ti, ab, kw
#14 ("disc displacement");ti, ab, kw
#15 (discopathy) ti, ab, kw
#16 (#1 OR #2 OR #3) AND (#4 OR #5 OR #6 OR #7 OR #8) AND (#9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15)
WEB OF SCIENCE
TOPIC (traction* OR distraction*) AND
TOPIC ("low back pain" OR "spinal pain" OR "leg pain" OR "lower extremity" OR lumbar*) AND
TOPIC ("disc displacement" OR "disc degeneration" OR discopathy OR sciatica OR radicul* OR "nerve root")
SCOPUS
(traction OR distraction) AND ("low back pain" OR "spinal pain" OR "lower extremity" OR "leg pain") AND ("disc displacement" OR "disc degeneration" OR discopathy OR radiculopathy OR sciatica OR "nerve root" OR radicular)
Appendix 2. Details of the studies excluded from this review, with reasons.
| Author | Title |
|---|---|
| Population (4) | |
| Mathews W. (1988) | Manipulation and traction for lumbago and sciatica: physiotherapeutic techniques used in two controlled trials |
| Pal B. (1986) | A controlled trial of continuous lumbar traction in the treatment of back pain and sciatica |
| Shealy C. (1997) | Decompression, reduction and stabilization of the lumbar spine: a cost-effective treatment for lumbosacral pain |
| Kiliç C (2021) | Clinical and functional effects of traction for lumbar disk hernia patients |
| Intervention (2) | |
| Oh H. (2018) | The impact of manual spinal traction therapy on the pain and Oswestry Disability Index of patients with chronic back pain |
| Tesio L. (1993) | Autotraction versus passive traction: an open controlled study in lumbar disc herniation |
| Comparison (1) | |
| Konrad K. (1992) | Controlled trial of balneotherapy in treatment of low back pain |
| Outcome (2) | |
| Cevik R. (2007) | Effect of new traction technique of prone position on distraction of lumbar vertebrae and its relation with different application of heating therapy in low back pain |
| Tadano S. (2019) | Lumbar mechanical traction: a biomechanical assessment of change at the lumbar spine |
| Study design (5) | |
| Bonaiuti D. (2004) | Manual autotraction: preliminary study of the effectiveness of a new device for back pain treatment |
| Letchuman (1993) | Comparison of sacrospinalis myoelectric activity and pain levels in patients undergoing static and intermittent lumbar traction |
| Ljunggren A.E. (1984) | Autotraction versus manual traction in patients with prolapsed lumbar intervertebral disc |
| Meszaros T.F. (2000) | Effect of 10%, 30%, and 60% body weight traction on the straight leg raise test of symptomatic patients with low back pain |
| Zhang Y. (2011) | A comparison between multi-directional mechanical traction and longitudinal traction for treatment of lumbar disc herniation: a randomized clinical trial with parallel-group design |
References
- 1. Luijsterburg PA, Verhagen AP, Ostelo RW, van Os TA, Peul WC, Koes BW. Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review. Eur Spine J. 2007;16(7):881 899. ( 10.1007/s00586-007-0367-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hahne AJ, Ford JJ, McMeeken JM. Conservative management of lumbar disc herniation with associated radiculopathy: a systematic review. Spine (Phila Pa 1976). 2010;35(11):E488 E504. ( 10.1097/BRS.0b013e3181cc3f56) [DOI] [PubMed] [Google Scholar]
- 3. Lewis RA, Williams NH, Sutton AJ.et al. Comparative clinical effectiveness of management strategies for sciatica: systematic review and network meta-analyses. Spine J. 2015;15(6):1461 1477. ( 10.1016/j.spinee.2013.08.049) [DOI] [PubMed] [Google Scholar]
- 4. Vroomen PC, de Krom MC, Slofstra PD, Knottnerus JA. Conservative treatment of sciatica: a systematic review. J Spinal Disord. 2000;13(6):463 469. ( 10.1097/00002517-200012000-00001) [DOI] [PubMed] [Google Scholar]
- 5. Wegner I, Widyahening IS, van Tulder MW.et al. Traction for low-back pain with or without sciatica. Cochrane Database Syst Rev. 2013;2013(8):CD003010. ( 10.1002/14651858.CD003010.pub5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang X, Zhang Z, Wen J, Lu J, Sun Y, Sang D. The effectiveness of therapeutic strategies for patients with radiculopathy: a network meta-analysis. Mol Pain. 2018;14:1744806918768972. ( 10.1177/1744806918768972) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cheng YH, Hsu CY, Lin YN. The effect of mechanical traction on low back pain in patients with herniated intervertebral disks: a systemic review and meta-analysis. Clin Rehabil. 2020;34(1):13 22. ( 10.1177/0269215519872528) [DOI] [PubMed] [Google Scholar]
- 8. Vanti C, Panizzolo A, Turone L.et al. Effectiveness of mechanical traction for lumbar radiculopathy: a systematic review and meta-analysis. Phys Ther. 2021;101(3):pzaa231. ( 10.1093/ptj/pzaa231) [DOI] [PubMed] [Google Scholar]
- 9. Vanti C, Turone L, Panizzolo A, Guccione AA, Bertozzi L, Pillastrini P. Vertical traction for lumbar radiculopathy: a systematic review. Arch Physiother. 2021;11(1):7. ( 10.1186/s40945-021-00102-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Madson TJ, Hollman JH. Lumbar traction for managing low back pain: a survey of physical therapists in the United States. J Orthop Sports Phys Ther. 2015;45(8):586 595. ( 10.2519/jospt.2015.6036) [DOI] [PubMed] [Google Scholar]
- 11. Alrwaily M, Almutiri M, Schneider M. Assessment of variability in traction interventions for patients with low back pain: a systematic review. Chiropr Man Therapap. 2018;26:35. ( 10.1186/s12998-018-0205-z) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Che YJ, Hou JJ, Guo JB.et al. Low energy extracorporeal shock wave therapy combined with low tension traction can better reshape the microenvironment in degenerated intervertebral disc regeneration and repair. Spine J. 2021;21(1):160 177. ( 10.1016/j.spinee.2020.08.004) [DOI] [PubMed] [Google Scholar]
- 13. Furlan AD, Malmivaara A, Chou R.et al. 2015 Updated method guideline for systematic reviews in the Cochrane Back and Neck Group. Spine (Phila Pa 1976). 2015;40(21):1660 1673. ( 10.1097/BRS.0000000000001061) [DOI] [PubMed] [Google Scholar]
- 14. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 2009;6(7):e1000097. ( 10.1371/journal.pmed.1000097) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Higgins JPT, Thomas J, Chandler J. et al. eds. Cochrane Handbook for Systematic Reviews of Interventions version 6.0. 2019. Available at: www.training.cochrane.org/handbook [Google Scholar]
- 16. Higgins JP, Altman DG, Gøtzsche PC.et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. ( 10.1136/bmj.d5928) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Atkins D, Best D, Briss PA.et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490. ( 10.1136/bmj.328.7454.1490) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schünemann H, Brożek J, Guyatt G.et al., eds. The GRADE working group. GRADE handbook for grading quality of evidence and strength of recommendations. 2013. Available at: gdt.guidelinedevelopment.org/app/handbook/handbook.html [Google Scholar]
- 19. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177 188. ( 10.1016/0197-2456(86)90046-2) [DOI] [PubMed] [Google Scholar]
- 20. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 21. Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q Statistic or I2 index? Psychol Methods. 2006;11(2):193 206. ( 10.1037/1082-989X.11.2.193) [DOI] [PubMed] [Google Scholar]
- 22. Gavaghan DJ, Moore AR, McQuay HJ. An evaluation of homogeneity tests in meta-analyses in pain using simulations of individual patient data. Pain. 2000;85(3):415 424. ( 10.1016/S0304-3959(99)00302-4) [DOI] [PubMed] [Google Scholar]
- 23. Beurskens AJ, de Vet HC, Köke AJ, Regtop W.et al. Efficacy of traction for nonspecific low back pain. 12-week and 6-month results of a randomized clinical trial. Spine (Phila Pa 1976). 1997;22(23):2756 2762. ( 10.1097/00007632-199712010-00011) [DOI] [PubMed] [Google Scholar]
- 24. Tanabe H, Akai M, Doi T.et al. Immediate effect of mechanical lumbar traction in patients with chronic low back pain: a crossover, repeated measures, randomized controlled trial. J Orthop Sci. 2021;26(6):953 961. ( 10.1016/j.jos.2020.09.018):() [DOI] [PubMed] [Google Scholar]
- 25. Van der Heijden GJMG, Bouter LM, Terpstra-Linderman E.et al. De effectiviteit van tractie bij lage rugklachten, De resultaten van een gerandomiseerde en geblindeerde pilot study. Ned T Fysiotherapie. 1991;101(2):37 41. [Google Scholar]
- 26. Schimmel JJ, de Kleuver M, Horsting PP, Spruit M, Jacobs WC, van Limbeek J. No effect of traction in patients with low back pain: a single centre, single blind, randomized controlled trial of intervertebral Differential Dynamics Therapy. Eur Spine J. 2009;18(12):1843 1850. ( 10.1007/s00586-009-1044-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Beurskens AJ, de Vet HC, Köke AJ.et al. Efficacy of traction for non-specific low back pain: a randomised clinical trial. Lancet. 1995;346(8990):1596 1600. ( 10.1016/s0140-6736(95)91930-9) [DOI] [PubMed] [Google Scholar]
- 28. Beyki M, Abedi M, Soleimani F, Mousavi ME, Roghani RS. Efficacy of prone lumbar traction on chronic discogenic low back pain and disability. Iran Rehabil J. 2007;5:20 23. [Google Scholar]
- 29. Kim JD, Oh HW, Lee JH, Cha JY, Ko I, Jee YS. The effect of inversion traction on pain sensation, lumbar flexibility and trunk muscles strength in patients with chronic low back pain. Isokinet Exer Sci. 2013;21(3):237 246. ( 10.3233/IES-130506) [DOI] [Google Scholar]
- 30. Santhumayor RE, Dhanesh Kumar KU, Ajith S. Effects of four different hold and rest time combinations of intermittent lumbar traction in the treatment of lumbar intervertebral disc prolapse: a comparative study. IJHSR. 2016;6(1):214. [Google Scholar]
- 31. Isner-Horobeti ME, Dufour SP, Schaeffer M.et al. High-force versus low-force lumbar traction in acute lumbar sciatica due to disc herniation: a preliminary randomized trial. J Manipulative Physiol Ther. 2016;39(9):645 654. ( 10.1016/j.jmpt.2016.09.006) [DOI] [PubMed] [Google Scholar]
- 32. Murat S, Uzunca K, Erden N. The effect of traction with two different load on clinic and functional status of patients with subacute lumbar disc herniation. Medeniyet Med J. 2018;2:82 88. ( 10.5222/MMJ.2018.34711) [DOI] [Google Scholar]
- 33. Reust P, Chantraine A, Vischer TL. Traitement par tractions mécaniques des lombosciatalgies avec ou sans déficit neurologique. Une étude en “double aveugle”. Schweiz Med Wschr. 1988;118:8. [PubMed] [Google Scholar]
- 34. Weber H. Traction. J Oslo City Hosp. 1973;23(10):167 176. [PubMed] [Google Scholar]
- 35. Bilgilisoy Filiz M, Kiliç Z, Uçkun A, Çakir T, Koldaş Doğan Ş, Toraman NF. Mechanical traction for lumbar radicular pain: supine or prone? A randomized controlled trial. Am J Phys Med Rehabil. 2018;97(6):433 439. ( 10.1097/PHM.0000000000000892) [DOI] [PubMed] [Google Scholar]
- 36. Choi J, Lee S, Hwangbo G. Influences of spinal decompression therapy and general traction therapy on the pain, disability, and straight leg raising of patients with intervertebral disc herniation. J Phys Ther Sci. 2015;27(2):481 483. ( 10.1589/jpts.27.481) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Güvenol K, Tüzün Ç, Peker Ö, Göktay Y. A comparison of inverted spinal traction and conventional traction in the treatment of lumbar disc herniations. Physiother Theor Pract. 2000;16(3):151 160. ( 10.1080/095939800750036079) [DOI] [Google Scholar]
- 38. Koçak FA, Tunç H, Tomruk Sütbeyaz S, Akkuş S, Köseoğlu BF, Yılmaz E. Comparison of the short-term effects of the conventional motorized traction with non-surgical spinal decompression performed with a DRX9000 device on pain, functionality, depression, and quality of life in patients with low back pain associated with lumbar disc herniation: a single-blind randomized-controlled trial. Turk J Phys Med Rehabil. 2018;64(1):17 27. ( 10.5606/tftrd.2017.154) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Liu ZZ, Wen HQ, Zhu YQ.et al. Short-term effect of lumbar traction on intervertebral discs in patients with low back pain: correlation between the T2 value and ODI/VAS score. Cartilage. 2021;13(1_suppl):414S 423S. ( 10.1177/1947603521996793) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Judovich BD. Lumbar traction therapy; elimination of physical factors that prevent lumbar stretch. J Am Med Assoc. 1955;159(6):549 550. ( 10.1001/jama.1955.02960230013005) [DOI] [PubMed] [Google Scholar]
- 41. Judovich BD, Nobel GR. Traction therapy, a study of resistance forces: preliminary report on a new method of lumbar traction. Am J Surg. 1957;93(1):108 114. ( 10.1016/0002-9610(57)90748-1) [DOI] [PubMed] [Google Scholar]
- 42. Cholewicki J, Lee AS, Reeves NP, Calle EA. Trunk muscle response to various protocols of lumbar traction. Man Ther. 2009;14(5):562 566. ( 10.1016/j.math.2008.08.005) [DOI] [PubMed] [Google Scholar]
- 43. Sari H, Akarirmak U, Karacan I, Akman H. Computed tomographic evaluation of lumbar spinal structures during traction. Physiother Theor Pract. 2005;21(1):3 11. ( 10.1080/09593980590911507) [DOI] [PubMed] [Google Scholar]
- 44. Lo WLA, Lei D, Leng Y.et al. Impact of nonsurgical spinal decompression on paraspinal muscle morphology and mechanical properties in young adults with low back pain. J Int Med Res. 2020;48(7):300060520919232. ( 10.1177/0300060520919232) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531 538. ( 10.1016/j.math.2008.09.001) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Krause M, Refshauge KM, Dessen M, Boland R. Lumbar spine traction: evaluation of effects and recommended application for treatment. Man Ther. 2000;5(2):72 81. ( 10.1054/math.2000.0235) [DOI] [PubMed] [Google Scholar]
- 47. Millan M, Leboeuf-Yde C, Budgell B, Amorim MA. The effect of spinal manipulative therapy on experimentally induced pain: a systematic literature review. Chiropr Man Therapap. 2012;20(1):26. ( 10.1186/2045-709X-20-26) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bialosky JE, Beneciuk JM, Bishop MD.et al. Unraveling the mechanisms of manual therapy: modeling an approach. J Orthop Sports Phys Ther. 2018;48(1):8 18. ( 10.2519/jospt.2018.7476) [DOI] [PubMed] [Google Scholar]
- 49. Kuligowski T, Dębiec-Bak A, Skrzek A. Effectiveness of traction in young patients representing different stages of degenerative disc disease. Ortop Traumatol Rehabil. 2019;21(3):187 195. ( 10.5604/01.3001.0013.2925) [DOI] [PubMed] [Google Scholar]
- 50. Dylewski MI, Dylewska M, Kasprzak A.et al. Proposition of patient stratification and parameter setting for mechanical traction in patients with LBP. J Educ Health Sport. 2020;10(2):85 96. ( 10.12775/JEHS.2020.10.02.012) [DOI] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a