Abstract
Background
Patients received care over telemedicine during the COVID-19 pandemic, and their perspective is useful for hand surgeons.
Methods
Online surveys were sent October-November 2020 to 497 patients who received telemedicine care. Questions were free-response and multi-item Likert scales asking about telehealth in general, limitations, benefits, comparisons to in-person visits, and opinions on future use.
Results
The response rate was 26% (n = 130). Prior to the pandemic, 55% had not used telemedicine for hand surgery consultation. Patients liked their telemedicine visit and felt their provider spent enough time with them (means = 9/10). In all, 48% would have preferred in-person visits despite the pandemic, and 69% would prefer in-person visits once the pandemic concludes. While 43% had no concerns with telemedicine, 36% had difficulties explaining their symptoms. Telemedicine was easy to access and navigate (M = 9/10). However, 23% saw telemedicine of limited value due to the need for an in-person visit soon afterward. Of these patients, 46% needed an in-person visit due to inadequate physical examination. Factors that make telemedicine more favorable to patients included convenience, lack of travel, scheduling ease, and time saved. Factors making telemedicine less favorable included need for in-person examination or procedure, pain assessment, and poor connectivity. There was no specific appointment time the cohort preferred. Patient recommendations to improve telemedicine included decreasing wait times and showing patient queue, wait time, or physician status online.
Conclusions
Telemedicine was strongly liked by patients during the COVID-19 pandemic. However, nearly 70% of patients still preferred in-person visits for the future.
Keywords: COVID-19, telemedicine, telehealth, hand surgery, virtual visits, patient survey
Introduction
Telemedicine provides patients with an alternative means of receiving their healthcare. Previously, hand and upper extremity surgery patients especially benefited from telemedicine if they were from rural areas or had travel limitations. 1 However, the COVID-19 pandemic has altered the traditional delivery of healthcare, and made telemedicine a more attractive option for more patients amidst quarantines and social distancing.
The rationale for this study was to capture patient’s perceptions on, and plans to use, telemedicine during the COVID-19 pandemic and in the future. We hypothesized that telemedicine would be viewed positively by patients due to its convenience, and when compared to traditional visits patients would have difficulty with the physical examination. As far as future applications, we postulated that patients would be interested in using telemedicine more frequently and recommend it to friends and family.
Materials and Methods
This study was designed to capture patient opinions on telemedicine during the COVID-19 pandemic. A survey was constructed online using SurveyMonkey and consisted of 19 questions in a free-response or Likert scale (ranging from 0 to 10) format. A complete survey can be found in the Supplemental Appendix.
Eligible patients were those who received care over the Chiron telemedicine platform (Medici, Austin, Texas) during the COVID-19 pandemic at our high-volume academic institution. This included both new patients and follow up visits including postoperative visits.
Using the electronic scheduling software from our practice, all patients who were seen for telemedicine encounters between the dates of May 16 and September 25 were contacted over email to complete the survey. These dates of service were chosen because they were after the initial spike of the pandemic, which allowed our healthcare system, government, and patients to adjust to the new environment. The survey was first delivered to patients via email in October, and 2 reminder emails were sent 1 and 2 weeks afterward. The authors believed that a survey a few months into the pandemic would provide the best responses, as patients, governments, and institutions were better acclimated.
Extraction of all survey responses resulted in the primary dataset. Data analysis for Likert scale questions involved calculations of means. Free response questions were compiled and analyzed manually by the authors to highlight common themes.
Results
Surveys were emailed to 497 patients, consisting of a random mix of new patients, follow-up visits, and postoperative visits. We received 130 responses for a response rate of 26%.
Prior to the pandemic, 55% of patients had not previously used telemedicine for a hand surgery visit. Generally, patients strongly liked their telemedicine visit (M = 9/10) and felt that their provider spend enough time with them (M = 9/10). However, 48% of patients would have preferred to have had their visit in-person, even despite the risks incurred by the pandemic. If there was a normal healthcare environment (ie, no pandemic) 69% of patients preferred in-person visits.
Table 1 summarizes what patients reported via free response as the best aspects of the telemedicine visit. Convenience and travel was the most common (n = 41, 37%), followed by the ability to see and interact with a physician (n = 36, 33%).
Table 1.
The Best Attribute of Telemedicine Visit.
| Reported attribute | Number | Percentage of respondents |
|---|---|---|
| Convenience or travel | 41 | 37 |
| Seeing and interacting with their physician | 36 | 33 |
| Lack of wait time or scheduling ease | 14 | 13 |
| Comfort or safety | 12 | 11 |
| General ease of use | 7 | 6 |
Table 2 summarizes what patients reported via free response as the most difficult aspects of telemedicine. Most patients had no concerns (n = 52, 43%). However, some had concerns with explaining their symptoms and the physical examination (n = 36, 36%).
Table 2.
The Most Difficult Part of Telemedicine Visit.
| Reported difficulty | Number | Percentage of respondents |
|---|---|---|
| Nothing, no concerns | 52 | 43 |
| Explaining symptoms or the physical exam | 36 | 30 |
| Connectivity | 13 | 11 |
| Waiting time | 11 | 9 |
| Ease of use or learning curve | 8 | 7 |
Overall, patients found it easy to access and use telemedicine (M = 9/10). Patients rated the difficulty of explaining symptoms over telemedicine as mildly difficult (M = 3/10). Patients did not find it difficult to understand the explanation of their condition or instruction for medical care (M = 2/10). Most patients believed that their physician was able to understand, diagnose, and treat just as well over telemedicine as they would in-person (n = 101, 78%). However, a cohort of patients did find telemedicine of limited value due to the need for an in-person visit soon afterward (n = 30, 23%). Table 3 summarizes patient reasons via free response within that cohort for needing an in-person visit after an initial telemedicine consultation. The most common reason reported was inadequate physical examination (n = 12, 46%). Other reasons reported were as follows: surgery or perioperative care (n = 5, 19%), an in-office procedure (n = 4, 15%), issues with patient or physician connectivity (n = 3, 12%), and need to obtain imaging (n = 2, 8%).
Table 3.
Patient-Reported Reasons for Needing an In-Person Visit After Telemedicine.
| Reported reason for subsequent in-person visit | Number | Percentage of respondents |
|---|---|---|
| Inadequate physical exam | 12 | 46 |
| Surgery | 5 | 19 |
| In-office procedure (eg, casting, injection) | 4 | 15 |
| Issues with patient or physician telemedicine connectivity | 3 | 12 |
| Need to obtain imaging | 2 | 8 |
For future visits during the pandemic, without knowledge of any vaccine, 49% of patients preferred telemedicine rather than in-person visits. In the absence of the pandemic, 29% of patients prefer future visits over telemedicine. Table 4 summarizes factors that patients stated via free response that would make telemedicine favorable in the future in the absence of the pandemic. Factors making telemedicine more favorable include general convenience (n = 24, 22%), lack of travel (n = 20, 18%), and scheduling ease or time saved (n = 11, 10%). Factors making telemedicine less favorable include: in-person exam or procedure (n = 46, 42%), adequate pain assessment (n = 6, 5%), and poor connectivity (n = 3, 3%).
Table 4.
Factors Making Telemedicine More or Less Favorable to Patients.
| Reported factor | Number | Percentage of respondents |
|---|---|---|
| More favorable | ||
| General convenience | 24 | 22 |
| Lack of travel | 20 | 18 |
| Scheduling ease or time saved | 11 | 10 |
| Less favorable | ||
| In-person physical exam, procedure, or imaging | 46 | 42 |
| Pain assessment | 6 | 5 |
| Poor connectivity | 3 | 3 |
Regarding telemedicine appointment times, there was no overwhelming preference in the following choices: before work (n = 39, 30%), lunch break (n = 52, 40%), and after work (n = 39, 30%). Overall, 85% of patients were likely to recommend telemedicine to friends or family.
Figure 1 depicts respondents’ single greatest recommendation via free response to improve telemedicine. The most common recommendation was to decrease wait times or show patients a queue or physician status.
Figure 1.
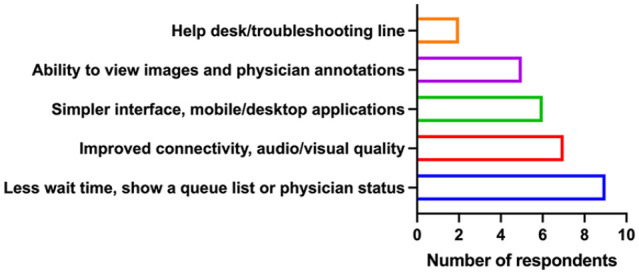
Patient recommendations to improve telemedicine.
Discussion
The rationale for this survey was to capture patients’ attitudes on telemedicine during the COVID-19 pandemic, opinions on its use in the future, as well as identify strengths and weaknesses from the patient’s perspective.
We found that despite the reported ease of telemedicine, patients still prefer in-person visits. Even during the pandemic, patients were split on their preference for telemedicine, as nearly half would prefer to have in-person visits. Moreover, most patients stated they would prefer in-person visits in a normal healthcare environment. This implies that there are some underlying patient-perceived limitations to telemedicine. However, we found 29% of patients would prefer telemedicine visits in the future, which we view as a substantial number. It is critical moving forward that we continue to identify the patients or clinical scenarios that are most amenable to both effective care and high patient satisfaction with telemedicine.
Conversely, since nearly a quarter of our patients saw telemedicine of limited value due to needing an in-person visit soon afterward, we see a potential concern if telemedicine is presented as a system to provide time-savings and cost containment. Almost half of the patients needing subsequent in-person visits were reportedly for in-person examinations. There are naturally going to be circumstances where a diagnosis and treatment plan cannot be adequately rendered over a telemedicine physical exam, which occurred in 12 out of 110 patients in this study. We view this 11% rate as subjectively acceptable; however, we as a specialty should continue to identify areas that may require more of a hands-on exam (ie, ulnar-sided wrist pain) and perhaps toward favoring in-person assessments in those circumstances.
The need for “surgery” in 19% of this cohort and 5% of the total study population. We believe that this correlates with the rates of an in-person visit. We acknowledge that we had potentially preventable repeat visits in the cases where 15% of this cohort and 4% of the total cohort needed to come in for an office procedure, and 8% of the cohort and 2% of the total cohort needed to come in for further imaging. While further patient screening in scheduling can optimize these scenarios, we find these rates to be acceptable. For example, first-time evaluations of acute trauma concerning for fracture or ligamentous injury will likely be low-yield without accompanying radiographs. However, such patients will have often already received an initial evaluation in an urgent care or emergency department setting, and with appropriate coordination can forward those images for review during a telemedicine appointment. This process has potential to streamline care for these patients, as their treatment is often time-sensitive and they can have difficulties with transportation to-and-from office appointments given their acute upper extremity injury. Likewise, a scheduling filter can be applied to new patients with symptoms consistent with digital stenosing tenosynovitis or other conditions typically treated with corticosteroid injections at the initial visit.
When examining the best aspects of telemedicine, time-saving and general convenience, not surprisingly, were the hallmark benefits of telemedicine to patients. However, we found it more surprising that seeing and interacting with their physician was the second-highest favorable factor. Face-to-face contact is typically also a part of an in-person visit, so it is unclear why this was such a strength of telemedicine. This may imply that the lack of human touch over telemedicine may not undermine patient confidence. Regardless, it appears that telemedicine with a video connection was still considered by patients to be a valid forum where they can still establish a good personal connection with their provider, which we view as a strongly positive finding. Further studies on how telemedicine encounters affect the physician–patient relationship is warranted.
When examining the most difficult aspects of telemedicine, it was encouraging to see that 43% of patients had no concerns. Aside from the challenges with physical exam cited above, we also were encouraged that only 18% of patients had issues with connectivity or using the telemedicine platform. One would expect this will only improve as platforms mature and patients and providers become more familiar with the process.
Consistent with our hypothesis, multiple parts of our survey showed that the physical exam was difficult for patients. The hand and upper extremity physical examination is notorious for its nuance, especially over videoconference. 2 Many patients therefore listed the physical examination as a major limitation on telemedicine. However, this did not necessarily translate into patient dissatisfaction, as 78% of patients thought the physician was able to understand, diagnose, and treat over telemedicine just as well as in-person. This follows reports, such as by Buvik et al, 3 whose prospective randomized clinical trial on general outpatient orthopedic care over telemedicine showed equivalent results as in-person visits. In that study, surgeons also rated their ability to examine the patient as “good” or “very good” for 98% of visits.
Interestingly, 6 of our patients reported that pain assessment is not as good over telemedicine as in-person visits. The subjective and objective evaluation of pain is known to be difficult even in-person. Potential drawbacks of pain evaluation over telemedicine include: diminished patient-physician interaction quality, challenges in psychological and social history evaluation, and patient engagement issues (eg, presence of distractors, lack of privacy, poor connectivity)—along with the aforementioned concerns. 4 This should be investigated further in the hand surgery literature. As surgeons, it is imperative that we offer a service that can adequately allow us to communicate and address our patients’ pain and discomfort.
Despite these challenges, telemedicine remained a positive form of clinical encounters for patients, as 85% of patients were likely to recommend its use to family and friends. This echoes results from a prospective hand surgery telemedicine program by Grandizio et al, 5 which found that telemedicine had high levels of patient satisfaction levels. Another orthopedic randomized controlled trial demonstrated that 63% of patients in the in-person clinic group and 86% of patients in the telemedicine group preferred telemedicine for future encounters. 6 This implies that positive prior experience with telemedicine may make patients more likely to prefer its use, which supports the notion that telemedicine will eventually become more mainstream if not already secondary to the pandemic. Overall, we can deduce that in certain instances, patients are able to consistently accomplish basic clinical care goals such as articulating their problems and history, receiving education, and obtaining treatment plans over telemedicine.
Specific benefits of telemedicine that patients mentioned included general convenience, time saving, and cost reduction secondary to lack of travel and parking expenses. Telemedicine has anecdotally reduced the number of postoperative visits and simple urgent consultations, as well as proven in studies to reduce lags in follow-up, minimize travel time, and decrease the carbon footprint. 7 For example, after implementing a rural telemedicine program for hand surgery in Arkansas, Tripod et al 8 found a significant decrease in the number of transfers and transportation costs. Our survey results are congruent with these studies and provide insight into patient-specific factors of interest.
Furthermore, our survey asked patients to provide their recommendations to improve telemedicine, and most of the responses centered around technical aspects of the process rather than general aspects of communicating with the physician or scheduling inefficiencies. The most common recommendation was to decrease wait times, show a queue list, or identify physician status. Some telemedicine platforms already have these features, which may alleviate patient frustration. For example, improved connectivity, audiovisual quality, and the option for both mobile and desktop applications may be useful to some patients. The ability to view radiographs and images is important to patients, and surgeons, as well. Since many new patients obtain radiographs at an emergency department or urgent care center, having patients upload images via disk or email can provide earlier initiation of telemedicine visits. Other suggestions included creating a helpdesk or displaying a troubleshooting button, which is useful to know for any practice interested in initiating telemedicine services to ensure a smooth transition and maintain patient comfort.
In our experience, there are certain scenarios that are more amenable to telemedicine than others, which patients seemed to allude to in our survey. Postoperative visits with external suture closures or emergency department follow-ups for lacerations would not be amenable, neither would patients with symptoms consistent with DeQuervain’s tenosynovitis since that is treated via corticosteroid injections at the initial visit. However, telemedicine seems to be useful for general follow-ups, either after surgery or injection, as well as to communicate any imaging or study results to patients. We performed a study on the surgeon’s perspective, which is still under review—but preliminarily we also saw that surgeons were more likely to use telehealth for general follow-ups but not fracture care follow-ups. We found that visit selection is key for the practical use of telemedicine. Filtering out the aforementioned visits could improve patients and physician satisfaction with telemedicine.
Lastly, it is useful to know that our cohort of patients did not have a strong preference for a specific telemedicine appointment time. Before work, lunch breaks, and after work hours were all equally preferred by our cohort. Thus, practitioners may best facilitate these encounters for their patients by scattering telemedicine appointment slots at various times throughout a clinic day rather than placing them all within a narrow time window.
This study has limitations. The response rate was 26%, which is a relatively high nonresponse rate. A follow-up email was sent to participants in an effort to mitigate nonresponse bias. Due to the conditions of the pandemic, we nevertheless believe that it is a good representation of the patient perspective, and all respondents received care over telehealth during the pandemic. The retrospective nature of this study is subject to recall biases, as well as the inherent flaws of surveys. Since we included a mixture of free response and multi-item Likert scale questions, this approach allowed for personal input but less standardization and therefore less generalizability of our results. A more comprehensive survey can increase generalizability, but would not have been feasible, as we had wanted to capture patient opinions of their visit during the pandemic and at this specific time. Nevertheless, we believe our study accomplishes the primary aim.
All encounters in this cohort were performed using the Chiron platform (Medici, Austin, Texas), which is integrated into our electronic health record and is Health Insurance Portability and Accountability Act-compliant. It certainly may be that platform-related likes or dislikes may not pertain to other systems. The issue of “connectivity” can be multifactorial, as it can relate to the quality of the internet connection of the provider or the patient, or related to the ability to log on to the platform itself. Nevertheless, connectivity and platform problems were relatively uncommon.
This study during the COVID-19 pandemic shows that telemedicine has high patient satisfaction and may be preferred for use by some patients in the future. Future research should focus on limitations of, best-practices for, and implementations of telemedicine in hand surgery practices. 9 As surgeons, we should meet the needs of our patients in an ethical and secure manner amid the fast-changing technological landscape.
Supplemental Material
Supplemental material, sj-pdf-1-han-10.1177_15589447211030692 for Patient Perspectives on Telemedicine During the COVID-19 Pandemic by Farhan Ahmad, Robert W. Wysocki, John J. Fernandez, Mark S. Cohen and Xavier C. Simcock in HAND
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board (IRB).
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: This study was reviewed by the Rush University Medical Center institutional review board (IRB) and was approved for a waiver of informed consent.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Farhan Ahmad  https://orcid.org/0000-0001-7974-8641
https://orcid.org/0000-0001-7974-8641
References
- 1.Grandizio LC, Foster BK, Klena JC.Telemedicine in hand and upper-extremity surgery. J Hand Surg Am. 2020;45(3):239-242. doi: 10.1016/j.jhsa.2019.09.007. [DOI] [PubMed] [Google Scholar]
- 2.Van Nest DS, Ilyas AM, Rivlin M.Telemedicine evaluation and techniques in hand surgery. J Hand Surg Glob Online. 2020;2(4):240-245. doi: 10.1016/j.jhsg.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buvik A, Bugge E, Knutsen G, et al. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res. 2016;16:483. doi: 10.1186/s12913-016-1717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Emerick T, Alter B, Jarquin S, et al. Telemedicine for chronic pain in the COVID-19 era and beyond. Pain Med. 2020;21(9):1743-1748. doi: 10.1093/pm/pnaa220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grandizio LC, Mettler AW, Caselli ME, et al. Telemedicine after upper extremity surgery: a prospective study of program implementation. J Hand Surg Am. 2020;45(9):795-801. doi: 10.1016/j.jhsa.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buvik A, Bugge E, Knutsen G, et al. Patient reported outcomes with remote orthopaedic consultations by telemedicine: a randomised controlled trial. J Telemed Telecare. 2019;25(8):451-459. doi: 10.1177/1357633X18783921. [DOI] [PubMed] [Google Scholar]
- 7.Bravo D, Gaston RG, Melamed E.Environmentally responsible hand surgery: past, present, and future. J Hand Surg Am. 2020;45(5):444-448. doi: 10.1016/j.jhsa.2019.10.031. [DOI] [PubMed] [Google Scholar]
- 8.Tripod M, Tait M, Bracey J, et al. The use of telemedicine decreases unnecessary hand trauma transfers. Hand (N Y). 2020;15(3):422-427. doi: 10.1177/1558944718810877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blake JH, Schwemmer MK, Sade RM.The patient-surgeon relationship in the cyber era: communication and information. Thorac Surg Clin. 2012;22(4):531-538. doi: 10.1016/j.thorsurg.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-han-10.1177_15589447211030692 for Patient Perspectives on Telemedicine During the COVID-19 Pandemic by Farhan Ahmad, Robert W. Wysocki, John J. Fernandez, Mark S. Cohen and Xavier C. Simcock in HAND


