Graphical Abstract
Key Words: cancer, cardio-oncology, cardiovascular disease, disparities, gender medicine, health care, LGBTQI+, sex and gender minority
Cardiovascular disease (CVD) and cancer are leading causes of death worldwide, with a disproportionate burden of illness among minority groups. The complex interactions of social determinants of health, including social, economic, geographic, and cultural factors that influence the underlying biology and health-related behaviors are a significant cause of disparities in cancer and CVD.1
Unfortunately, many investigations reflect the invisibility of the agender, asexual, bisexual, gay, gender diverse, genderqueer, genderfluid, intersex, lesbian, nonbinary, pansexual, queer, and transgender (LGBTQI+) population in the available data analyzed. The LGBTQI+ population faces unique barriers when accessing the health care system when compared with their heterosexual counterparts. There may be differences in interactions with the medical community and differences in societal relationships that have the potential to affect both preventive and essential care, contributing to disparities in CVD and cancer risk and treatment.
At least 7% of U.S. adults self-identify as a sex and gender minority (SGM), and 16% of Generation Z adults, who were born from the mid-1990s to the early 2010s, report that they are SGMs.2 However, in considering these statistics on the LGBTQI+ population, the prevalence of SGMs is likely underreported, given a perceived risk of stigma and discrimination. Furthermore, an additional reporting bias exists in considering the LGBTQI+ population as a single, homogeneous social category. As the LGBTQI+ population is variegated with specific characteristics, we must consider and understand that each member of this community has their own subgroups, which may be assumed to be separate (eg, transgender people are heterosexual, lesbians are cisgender). For any given person, gender identity, sexual attraction, behavior, and identity are distinct. For example, some transgender women are lesbians and some queer men are transgender.
No established biological or physiological differences exist between LGBTQI+ people and their heterosexual counterparts; several indications suggest that health disparities in the LGBTQI+ community may stem from a combination of social/economic factors and behaviors,3 many of which can be traced to the stress of living as an SGM.
LGBTQI+ disparities in cardiovascular health
The traditional cardiovascular risk factors shaping cardiovascular health of SGM populations include tobacco use, physical activity, diet/nutrition, weight management, lipid profile, glycemic status, and blood pressure. There is some evidence that traditional cardiovascular risk factors, such as tobacco use, are increased in SGMs, but there are limited data for blood pressure, lipids, glycemic status, and body mass index. Human immunodeficiency virus infection, vascular health and function, sleep disturbances, and alcohol intake may be unique risk factors to be considered among LGBTQI+ populations; their impact on the cardiovascular health of LGBTQI+ populations specifically remain to be comprehensively examined.4
According to the American Heart Association, LGBTQI+ people compared with their heterosexual counterparts are 36% less likely to have normal cardiovascular health. LGBTQI+ people experience distal (eg, discrimination) and proximal (eg, expectations of rejection, internalized homophobia, and concealment) stressors that may contribute to health disparities. These stressors may result in adverse cardiovascular health behaviors and increase the likelihood of poor cardiovascular health outcomes.
Recent research reported a >2- and 4-fold increased prevalence of myocardial infarction in men who are transgender compared with cisgender men and cisgender women, respectively. Conversely, the prevalence of myocardial infarction in women who are transgender compared with women who are cisgender is increased >2-fold but not in comparison with men who are cisgender.5 The basis for these differences is unknown, but it has been postulated that masculinizing and feminizing hormone therapy could be responsible. For example, venous thromboembolism and ischemic stroke are more frequently observed in transfeminine people on hormone therapy than in cisgender women and men.6
Multiple stressors including discrimination, social stigma, the fear of violence, and hypervigilance are also suspected of worsening the cardiovascular health of LGBTQI+ adults. However, specific data relating to these populations are limited. The precise epidemiology of cardiovascular disease in the LGBTQI+ population remains unknown. To date, the limited collection of data on sexual orientation and gender identity in population-based and clinical datasets hinders the development of research on SGM cardiovascular health.7
As a result, the evidence in LGBTQI+ populations is limited and sometimes conflicting. Most of the available data refer to the transgender population, studies are sporadic and often based on self-assessment questionnaires, and no national health surveys comprehensively and routinely collect sexual orientation and gender identity data.
LGBTQI+ disparities in cancer
The incidence and prevalence of cancer in LGBTQI+ population remain unknown because no national health surveys or cancer registries comprehensively collect sexual orientation and gender identity data.8 Unfortunately, LGBTQI+ people are still rarely included in cancer research so that there are significant limitations to the amount of robust data available on LGBTQI+ population with cancer. The quality of sexual orientation recording in routinely collected health data, if available, is poor, and this raises concerns around completeness and accuracy of analysis when using existing data. Health care barriers and discomfort with screening procedures may influence cancer diagnosis, progression, and outcomes in LGBTQI+ population.
Despite these limitations, we know that at least 7 types of cancer disproportionately affect LGBTQI+ populations, including anal, breast, cervical, colorectal, lung, prostate, and uterine cancer.9 The LGBTQI+ population is more likely to have a cluster of risk factors such as delayed cancer screening, alcohol use, smoking, obesity, human immunodeficiency virus infection, and human papillomavirus infection contributing to increased cancer incidence and late-stage diagnosis.10 Most of these risks affect subgroups of the population identifying as LGBTQI+; however, each sexual orientation and gender identity has its own cancer risks. Awareness of personal risk factors is important, and there is limited guidance on routine cancer screening for LGBTQI+. Lesbian and bisexual women may be at a higher risk for breast cancer, colorectal, skin, cervical, endometrial, and ovarian cancer than heterosexual women. This may be due to higher rates of tobacco and alcohol use and obesity, as well as due to nulliparity. Higher rates of anal, prostate, testicular, and colon cancers are observed in gay and bisexual men. Transgender people have unique cancer risks: they are more likely to forgo cancer screenings and care, putting them at a higher risk of late-stage cancer diagnosis and cancer death.10 Furthermore, a much more sensitive topic exists: transgender individuals may experience gender dysphoria and distress during screening, as it may challenge one’s trans identity11 and may result in a return to a “pretransition ‘existential crisis.’”
As with CVD, an association exists between long-term hormone therapy and cancer risk, but further research is needed to evaluate its impact to understand how masculinizing and femininizing hormones influence cancer risk in sex-specific organs and other organs. Lower risk of prostate cancer is reported among trans women, potentially due to hormone therapy.12
Disparities in cardiovascular and oncologic care and potential solutions
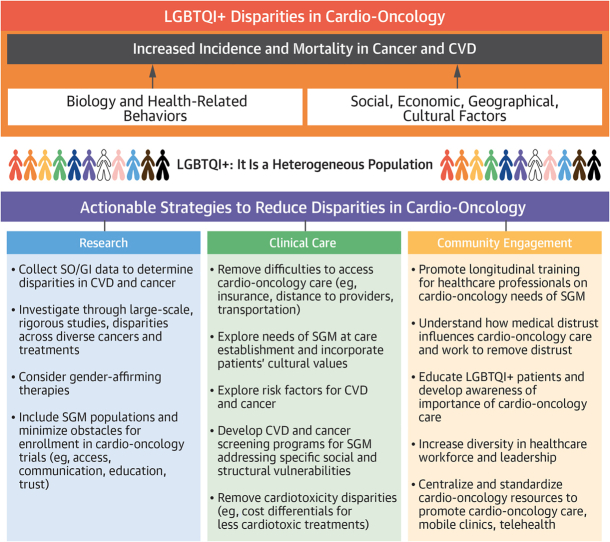
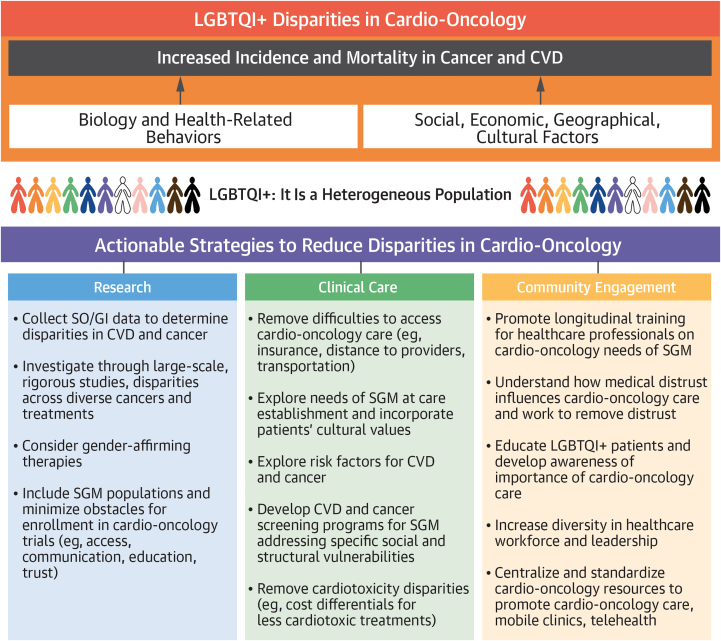
Health outcomes for the LGBTQI+ populations remain worse than for their non-LGBTQI+ peers. In Europe, the European Society for Medical Oncology has underlined the lack of scientific evidence on how to tailor cancer prevention and treatment to the LGBTQI+ community. Leading scientific societies around the world are aware of these issues and have made proposals to the scientific community and health policy makers to bridge this gap. Recently the Sexual and Gender Minority Office of the National Institutes of Health provided a roadmap aimed to develop operational goals to meet the health needs of SGM.13,14 Overcoming all these obstacles requires broad participation of the entire health system, and in particular both health care providers and the “excluded” or discriminated population. Several proposed actions may help overcome discriminations and address the needs of the SGM populations.15 These general recommendations should be implemented in each specific clinical specialty and in cardio-oncology, specifically, where there is a dearth of scientific evidence. To reduce disparities in cardio-oncology, actionable strategies are needed within cardio-oncology research, clinical practice, and community engagement (Figure 1).
Figure 1.
Disparities in Cardio-Oncology for the LGBTQI+ Populations and Actionable Strategies to Reduce Them
Agender, asexual, bisexual, gay, gender diverse, genderqueer, genderfluid, intersex, lesbian, nonbinary, pansexual, queer, and transgender (LGBTQI+) people have a higher incidence of cardiovascular diseases (CVDs) and cancer due to biological, behavioral, social, economic, cultural, and geographical factors. The complex heterogeneity of this population makes it even more difficult to analyze and implement measures to reduce disparities. These strategies must be implemented by involving communities and soliciting the commitment of researchers and clinicians. SGM = sex and gender minority; SO/GI = sexual orientation/gender identity.
In conclusion, despite increased awareness about LGBTQI+ health disparities and known causes of these disparities,16 limited actions are being implemented all over the world. The presence of these inequalities indicates that much still needs to be done to achieve an equitable society. Across the world, there is growing interest for the same goal, but there is still much to be done worldwide. This calls us all to action in cardiovascular and oncologic medicine, 2 leading causes of morbidity and mortality worldwide.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Ohman R.E., Yang E.H., Abel M.L. Inequity in cardio-oncology: identifying disparities in cardiotoxicity and links to cardiac and cancer outcomes. J Am Heart Assoc. 2021;10(24) doi: 10.1161/JAHA.121.023852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones J.M. LGBT identification in U.S. ticks up to 7.1. Gallup News. https://news.gallup.com/poll/389792/lgbt-identification-ticks-up.aspx Accessed October 31, 2022.
- 3.Pöge K., Dennert G., Koppe U., Güldenring A., Matthigack E.B., Rommel A. The health of lesbian, gay, bisexual, transgender and intersex people. J Health Monit. 2020;5(Suppl 1):2–27. doi: 10.25646/6449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Streed C.G., Jr., Beach L.B., Caceres B.A., et al. American Heart Association Council on Peripheral Vascular Disease; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Radiology and Intervention; Council on Hypertension; and Stroke Council. Assessing and addressing cardiovascular health in people who are transgender and gender diverse: a scientific statement from the American Heart Association. Circulation. 2021;144(6):e136–e148. doi: 10.1161/CIR.0000000000001003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alzahrani T., Nguyen T., Ryan A., et al. Cardiovascular disease risk factors and myocardial infarction in the transgender population. Circ Cardiovasc Qual Outcomes. 2019;12(4) doi: 10.1161/CIRCOUTCOMES.119.005597. [DOI] [PubMed] [Google Scholar]
- 6.Getahun D., Nash R., Flanders W.D., et al. Cross-sex hormones and acute cardiovascular events in transgender persons: a cohort study. Ann Intern Med. 2018;169(4):205–213. doi: 10.7326/M17-2785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caceres B.A., Streed C.G., Jr. Cardiovascular health concerns in sexual and gender minority populations. Nat Rev Cardiol. 2021;18(4):227–228. doi: 10.1038/s41569-021-00518-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berrahou I.K., Snow A., Swanson M., Obedin-Maliver J. Representation of sexual and gender minority people in patient nondiscrimination policies of cancer centers in the United States. J Natl Compr Canc Netw. 2022;20(3):253–259. doi: 10.6004/jnccn.2021.7078. [DOI] [PubMed] [Google Scholar]
- 9.Quinn G.P., Sanchez J.A., Sutton S.K., et al. Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA Cancer J Clin. 2015;65(5):384–400. doi: 10.3322/caac.21288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gonzales G., Zinone R. Cancer diagnoses among lesbian, gay, and bisexual adults: results from the 2013-2016 National Health Interview Survey. Cancer Causes Control. 2018;29(9):845–854. doi: 10.1007/s10552-018-1060-x. [DOI] [PubMed] [Google Scholar]
- 11.Connolly D., Hughes X., Berner A. Barriers and facilitators to cervical cancer screening among transgender men and non-binary people with a cervix: a systematic narrative review. Prev Med. 2020;135 doi: 10.1016/j.ypmed.2020.106071. [DOI] [PubMed] [Google Scholar]
- 12.Scheim A.I., Baker K.E., Restar A.J., Sell R.L. Health and health care among transgender adults in the United States. Annu Rev Public Health. 2022;43:503–523. doi: 10.1146/annurev-publhealth-052620-100313. [DOI] [PubMed] [Google Scholar]
- 13.National Institutes of Health Strategic Plan to Advance Research on the Health and Well-being of Sexual & Gender Minorities. Fiscal Years 2021–2025. https://dpcpsi.nih.gov/sites/default/files/SGMStrategicPlan_2021_2025.pdf Accessed October 31, 2022.
- 14.National Institutes of Health NIH FY 2016-2020. Strategic Plan to Advance Research on the Health and Well-being of Sexual and Gender Minorities. https://www.edi.nih.gov/sites/default/files/EDI_Public_files/sgm-strategic-plan.pdf Accessed October 31, 2022.
- 15.Peterson CJ, Sepúlveda M-J, eds. Understanding the Well-Being of LGBTQI+ Populations. Accessed October 31, 2022. https://nap.nationalacademies.org/read/25877/chapter/1
- 16.Sirufo M.M., Magnanimi L.M., Ginaldi L., De Martinis M. Strategies to reduce health care disparities for sexual and gender minorities. Curr Probl Cancer. 2022;47(1) doi: 10.1016/j.currproblcancer.2022.100881. [DOI] [PubMed] [Google Scholar]