Abstract
Background
Comorbidities are important risk factors of severe COVID-19 complications. Their impact during the Omicron wave among vaccinated and unvaccinated COVID-19 cases is not well documented.
Purpose
The objective of this study was to estimate the association between the number of comorbidities and the risk of hospitalization, intensive care unit (ICU) admission, and death among vaccinated and unvaccinated confirmed adult COVID-19 cases during the Omicron wave.
Research Design and Study sample
We performed a cohort study of COVID-19 adult cases of primo-infection occurring during the Omicron wave, from December 5, 2021 to January 9, 2022 using surveillance database of the province of Québec, Canada. The database included all laboratory-confirmed cases in the province and the related information on 21 pre-existing comorbidities, hospitalization, ICU admission, death related to COVID-19 and vaccination status.
Analysis
We performed a robust Poisson regression model to estimate the impact of the number of comorbidities on each complication by vaccination status adjusted for age, sex, socioeconomic status, and living environment.
Results
We observed that the risk of complication increased for each additional comorbidity in both vaccinated and unvaccinated individuals and that this risk was systematically higher among unvaccinated individuals. Compared with vaccinated individuals without comorbidities (reference group), the risks of hospitalization, ICU admission, and death were respectively: 9X (95% CI [7.77–12.01]), 13X (95% CI [8.74–18.87]), and 12X (95% CI [7.57–18.91]) higher in vaccinated individuals with ≥3 comorbidities; 22X (95% CI [19.07–25.95]), 45X (95% CI [29.06-69.67]) and 38X (95% CI [23.62-61.14]) higher in unvaccinated individuals with ≥3 comorbidities.
Conclusion
Our results support the importance of promoting vaccination in all individuals, and especially those with pre-existing medical conditions, to reduce severe complications, even during the Omicron wave.
Keywords: Comorbidity, COVID-19, surveillance data, omicron, severe complication
Introduction
Pre-existing comorbidities in COVID-19 cases have been a major risk factor for severe complications, including hospitalization, intensive care unit (ICU) admission, and death, since the beginning of the pandemic. 1 Numerous studies have found that an increase in the number of medical conditions is associated with an increase in the risk of severe complications.1–3 Both vaccination and new variants have had an impact on the severity of the disease among COVID-19 cases.4,5 Vaccination has provided protection against severe complications for many severe acute respiratory coronavirus-2 (SARS-CoV-2) variants, including the Omicron variant. 4
Impact of pre-existing comorbidities during the omicron wave is less well documented than for previous variants. The Omicron variant, first reported in South Africa in November 2021, has spread rapidly worldwide, and cases had been confirmed in more than 57 countries as of December 2, 2021. 6 In Canada's second largest province (Province of Quebec), the majority of cases were from the Omicron variant during the second week of December (between December 5 and 11, 2021). 7 The severity of complications among COVID-19 Omicron variant cases was lower, even among unvaccinated cases. 5 A Danish study using population-based surveillance data reported that an increase in comorbidities remained associated with an increased risk of hospitalization among COVID-19 Omicron variant cases. 8 However, this study did not assess the potential impact of comorbidities on ICU admission and death.
The aim of this study was to estimate the association between the number of comorbidities and the risks of hospitalization, ICU admission, and death in adults during the Omicron wave, accounting for vaccination status.
Methods
Study design and data source
We performed a population-based cohort study using surveillance data including confirmed adult cases of SARS-CoV2 infection during the Omicron wave of the pandemic, from December 5th, 2021 to January 9th, 2022. We started the study when the proportion of the Omicron variant exceeded 50% among COVID-19 cases and stopped when population-based laboratory testing ceased in the province of Quebec. After January 9, systematic testing was restricted to selected groups such as health care workers and nursing homes residents. The surveillance data file (Trajectoire de santé publique [TSP] registry) includes all cases of infection confirmed by laboratory or epidemiologically in the province of Québec and was linked using a unique identifier to the MED-ECHO preliminary transmission file to obtain information on hospitalization and ICU admission related to COVID-19 and to the Quebec Integrated Chronic Disease Surveillance System (QICDSS) to obtain information on pre-existing medical conditions. The QICDSS is a registry that includes information on all physicians’ claims and diagnostic codes for almost all (>99%) of the Quebec population. 9 We excluded cases with no information on pre-existing medical conditions, as well as hospital-associated infections, that is an case detected more than one week after hospital admission. 10 The case date corresponds to the earliest of the following three dates: 1) date of the positive laboratory test, 2) date of symptom onset, 3) date of the beginning of the epidemiological investigation conducted by the public health surveillance team.
COVID-19 complications
A COVID-19 case was considered hospitalized if at least one acute care hospital stay of at least one day with the COVID-19 diagnostic code (International Statistical Classification of Diseases and Health Related Problems, Tenth Revision [ICD-10-CA] diagnosis code: U07.1) was recorded in the preliminary transmissions of the MED-ECHO file. All COVID-19 related hospitalizations were included, regardless of the reason for admission. Any ICU admission was also recorded in MED-ECHO for these hospitalizations. All death directly or indirectly caused by COVID-19 were collected in the surveillance database during the epidemiological investigations of each of the 18 regional Public Health Departments. The relation of each death with COVID-19 is validated by the regional Public Health Departments on the basis of the forms filled in by the doctors at the time of death 11 and the information obtained in real time from Quebec registry of deaths 12 where COVID-19 deaths are entered according to the WHO guidelines. 13 All complications were followed-up from case date until February 13th, 2022 (most up-to-date information at the date of data extraction).
Comorbidities
Using validated algorithms, the number of comorbidities (0, 1, 2, ≥3) was estimated by the cumulation of 21 pre-existing medical conditions identified from ICD codes entered in the QICDSS for all individuals included in the registry on April 1st, 202114,15 (Supplementary files, Table A.1). Those conditions include risk factors (including chronic diseases, their risk factors or symptoms) for complications in individuals with COVID-19 2 such as cardiovascular diseases, respiratory diseases, mental disorders, obesity and Immune system problem (see Table A1 in Supplementary file). Those conditions do not include some low prevalence diseases associated with COVID-19 complications such as Crohn’s disease or Down syndrome as no algorithm is available to extract such conditions in the QICDSS. Based on the 10 years previous to April 1st, 2021, a person was considered to have a medical condition if, at least one diagnostic code was recorded in the hospitalization file or at least two diagnostic codes were recorded in the physicians’ claims database within two years, with at least 30 days between each diagnosis code.14,15 For cancer, depression, alcohol and drug abuse conditions, search of diagnostics codes was limited to the previous 5 years. 16
Vaccination status
Individuals were considered adequately vaccinated if they had received two vaccine doses (or one Janssen vaccine dose) or a combination of these vaccines with a respected minimal interval between the 2 doses. 17 In the rest of the text, “vaccinated group” or “vaccinated individuals” wording refer to adequately vaccinated individuals. In contrast, “unvaccinated group” or “unvaccinated individuals” refer to inadequately vaccinated individuals.
Covariates
Covariates included sex, living environment (private seniors’ residences [RPAs], long-term care facilities [CHSLDs], at home or unknown living environment, others [Including intermediary resources centres]), CDC week (from weeks 2021-49 to 2022-01, January 9th, 2022 was included in the 2022-01 week), age and the material and social deprivation indices. Age was calculated on the episode date. The material and social deprivation indices were assigned from the 2016 census data according to the postal code of the place of residence. 18 Material deprivation included information on income, education and employment status. Social deprivation included information on the proportions of people living alone, single-parent families and people who are separated, divorced or widowed.
Statistical analysis
We estimated frequency distributions for the number of comorbidities, covariates and complications (hospitalization, ICU admission and death) for all cases included in the cohort and by vaccination status. We then estimated the proportion of cases with complication according to the number of comorbidities, stratified by age and vaccination status. For each of these complications, we finally estimated the relative impact of each additional comorbidity on the risk of each complication controlling for vaccination status with a robust Poisson regression model. Each model (one for each outcome) was adjusted for all covariates, and we added an interaction term between the number of comorbidities and vaccination status to allow comparison of the association between the number of comorbidities and the risk of each complication between vaccination groups. Statistical tests were 2-sided with significance at p < 0.05. SAS 9.4 was used for all analyses.
Sensitivity and supplementary analysis
We estimated the proportion of cases with each complication within the last two weeks of available data when the proportion of Omicron variant cases was greater than 90%, to ensure a more homogeneous cohort. We estimated the proportion of cases with each complication when including hospital-associated cases. We finally estimated the proportion of cases with each complication stratified by the number of vaccine doses. For each outcome, we estimated adjusted relative risk stratified by age subgroup using robust Poisson regression models including interaction terms with age.
Ethics
Data linkages and analyses were authorized by the National Director of Public Health (Quebec) under respective provincial public health legislation without requirement for research ethics board review.
Results
We identified 245,956 confirmed adult COVID-19 cases during the first weeks of the Omicron wave that officially began on December 5th, 2021 in the province of Quebec, Canada (Supplementary file, Figure A.1). Respectively 1,7%, 0,3% and 0,5% of cases were hospitalized, admitted to ICU or died due to COVID-19 (Table 1). More than 90% of the cases were adequately vaccinated (79% had received two doses and 12% had received three doses). Cases in the vaccinated group were older (mean age = 43 years; median = 40 years) than the unvaccinated group (mean age = 39 years; median = 36 years) and had fewer complications.
Table 1.
Description of adults with COVID-19 identified during the Omicron wave (Dec 5th 2021-Jan 9th 2022, Quebec, Canada) stratified by vaccination status (n = 245,956).
| Variable | Total | Number of comorbidities | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | ≥3 | |||||||
| n = 245,956 | n = 156,016 | n = 51,367 | n = 18,203 | n = 20,370 | ||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | |
| Mean age ±SD | 42 | ±17 | 37 | ±13 | 45 | ±16 | 52 | ±17 | 66 | ±19 |
| Age group | ||||||||||
| 18–49 | 169,846 | 69.1 | 125,272 | 80.3 | 31,620 | 61.6 | 8,460 | 46.5 | 4,494 | 22.1 |
| 50–64 | 50,699 | 20.6 | 26,204 | 16.8 | 14,233 | 27.7 | 5,592 | 30.7 | 4,670 | 22.9 |
| 65–74 | 12,785 | 5.2 | 3,646 | 2.3 | 3,626 | 7.1 | 2,202 | 12.1 | 3,311 | 16.3 |
| 75+ | 12,626 | 5.1 | 894 | 0.6 | 1,888 | 3.7 | 1,949 | 10.7 | 7,895 | 38.8 |
| Sex | ||||||||||
| Women | 136,175 | 55.4 | 81,059 | 52.0 | 31,801 | 61.9 | 11,608 | 63.8 | 11,707 | 57.5 |
| Men | 109,781 | 44.6 | 74,957 | 48.0 | 19,566 | 38.1 | 6,595 | 36.2 | 8,663 | 42.5 |
| Living environment | ||||||||||
| At home | 239,058 | 97.2 | 155,393 | 99.6 | 50,550 | 98.4 | 17,284 | 95.0 | 15,831 | 77.7 |
| CHSLDs | 2,276 | 0.9 | 94 | 0.1 | 201 | 0.4 | 264 | 1.5 | 1,717 | 8.4 |
| RPAs | 3,144 | 1.3 | 191 | 0.1 | 407 | 0.8 | 454 | 2.5 | 2,092 | 10.3 |
| Others | 1,478 | 0.6 | 338 | 0.2 | 209 | 0.4 | 201 | 1.1 | 730 | 3.6 |
| Number of comorbidities | ||||||||||
| 0 | 156,016 | 63.4 | 156,016 | 100.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| 1 | 51,367 | 20.9 | 0 | 0.0 | 51,367 | 100.0 | 0 | 0.0 | 0 | 0.0 |
| 2 | 18,203 | 7.4 | 0 | 0.0 | 0 | 0.0 | 18,203 | 100.0 | 0 | 0.0 |
| ≥3 | 20,370 | 8.3 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 20,370 | 100.0 |
| Vaccination status a | ||||||||||
| Unvaccinated | 23,370 | 9.5 | 15,485 | 9.9 | 4,664 | 9.1 | 1,574 | 8.6 | 1,647 | 8.1 |
| Vaccinated | 222,586 | 90.5 | 140,531 | 90.1 | 46,703 | 90.9 | 16,629 | 91.4 | 18,723 | 91.9 |
| Number of vaccine doses | ||||||||||
| 0 | 18,789 | 7.6 | 12,526 | 8.0 | 3,731 | 7.3 | 1,275 | 7.0 | 1,257 | 6.2 |
| 1 | 4,338 | 1.8 | 2,832 | 1.8 | 877 | 1.7 | 282 | 1.5 | 347 | 1.7 |
| 2 | 194,025 | 78.9 | 129,181 | 82.8 | 40,364 | 78.6 | 13,220 | 72.6 | 11,260 | 55.3 |
| 3 | 28,707 | 11.7 | 11,446 | 7.3 | 6,375 | 12.4 | 3,417 | 18.8 | 7,469 | 36.7 |
| 4+ | 97 | 0.0 | 31 | 0.0 | 20 | 0.0 | 9 | 0.0 | 37 | 0.2 |
| Epidemiological week | ||||||||||
| 2021–49 | 6,615 | 2.7 | 4,041 | 2.6 | 1,514 | 2.9 | 557 | 3.1 | 503 | 2.5 |
| 2021–50 | 15,277 | 6.2 | 10,054 | 6.4 | 3,186 | 6.2 | 1,130 | 6.2 | 907 | 4.5 |
| 2021–51 | 49,321 | 20.1 | 34,390 | 22.0 | 9,603 | 18.7 | 2,990 | 16.4 | 2,338 | 11.5 |
| 2021–52 | 85,430 | 34.7 | 54,833 | 35.1 | 17,977 | 35.0 | 6,303 | 34.6 | 6,317 | 31.0 |
| 2022–01 | 89,313 | 36.3 | 52,698 | 33.8 | 19,087 | 37.2 | 7,223 | 39.7 | 10,305 | 50.6 |
| Hospitalisation | ||||||||||
| Yes | 4,242 | 1.7 | 775 | 0.5 | 650 | 1.3 | 508 | 2.8 | 2,309 | 11.3 |
| ICU admissions | ||||||||||
| Yes | 650 | 0.3 | 146 | 0.1 | 120 | 0.2 | 94 | 0.5 | 290 | 1.4 |
| Death | ||||||||||
| Yes | 1,108 | 0.5 | 47 | 0.0 | 119 | 0.2 | 123 | 0.7 | 819 | 4.0 |
Abbreviations: CHSLD: Long-term care or nursing facilities; ICU: Intensive care unit; n/a: not available; RPA: private seniors’ residences.
aThe vaccinated group included all individuals adequately vaccinated, i.e., all individuals who received two vaccine doses (or one Janssen vaccine dose) or a combination of these vaccines with a respected minimal interval between the 2 doses. The unvaccinated group included all other individuals.
Hospitalizations
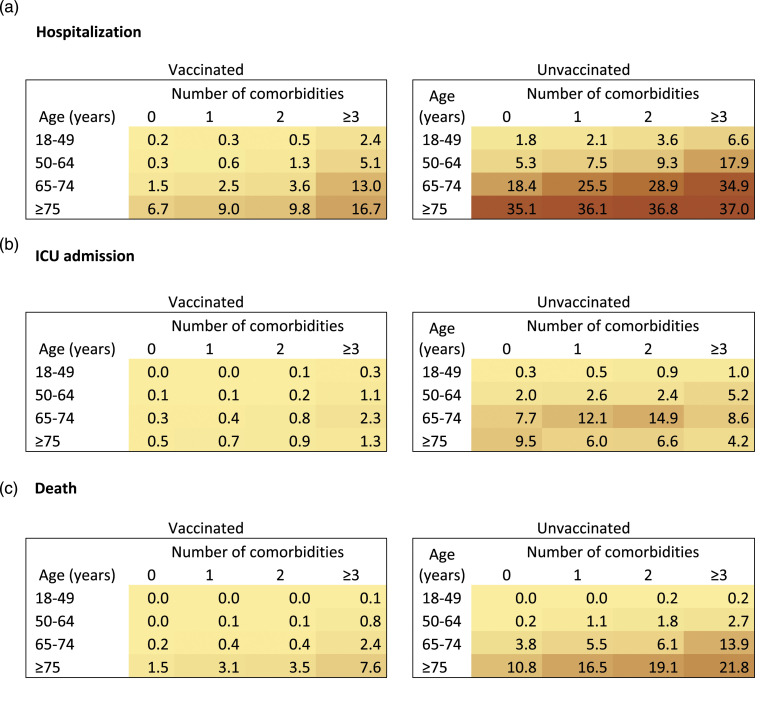
The proportion of cases with hospitalization increased for each additional comorbidity in all age groups, in both vaccinated and unvaccinated confirmed COVID-19 cases (Figure 1). Among the vaccinated cases in the 18-49 age group, the percentage of hospitalization increased from 0.2% in those without comorbidity to 2.4% in those having ≥3 comorbidities (Figure 1). Similar increases were observed in all age groups and the percentage of hospitalization reached 16.7% in the ≥3 comorbidities and ≥75 age groups. Similarly, in unvaccinated cases, the percentage of hospitalization increased when the number of comorbidities increased. The percentage of hospitalization also increased with increasing comorbidities in all age groups. Indeed, the percentage of hospitalization increased from 1.8% to 6.6% and from 35.1% to 37.0% in the 18-49 and ≥75 age groups, respectively, when the number of comorbidities increased from 0 to ≥3. Percentages in unvaccinated cases were higher than in vaccinated cases in all examined age groups.
Figure 1.
Percentage of adults with COVID-19 identified between Dec 5th 2021-Jan 9th 2022 with COVID-19 hospitalisation (a), intensive care unit (ICU) admission (b) or death (c) by 13th February 2022 by number of comorbidities, stratified by age and vaccination status during the Omicron wave Québec, Canada (n = 245,956). Graduated color representation of percentage: yellow (smaller percentage), brown (higher percentage). The vaccinated group included all individuals adequately vaccinated, i.e., all individuals who received two vaccine doses (or one Janssen vaccine dose) or a combination of these vaccines with a respected minimal interval between the 2 doses. The unvaccinated group included all other individuals. Confidence intervals are reported in the supplementary file, Table A.2.
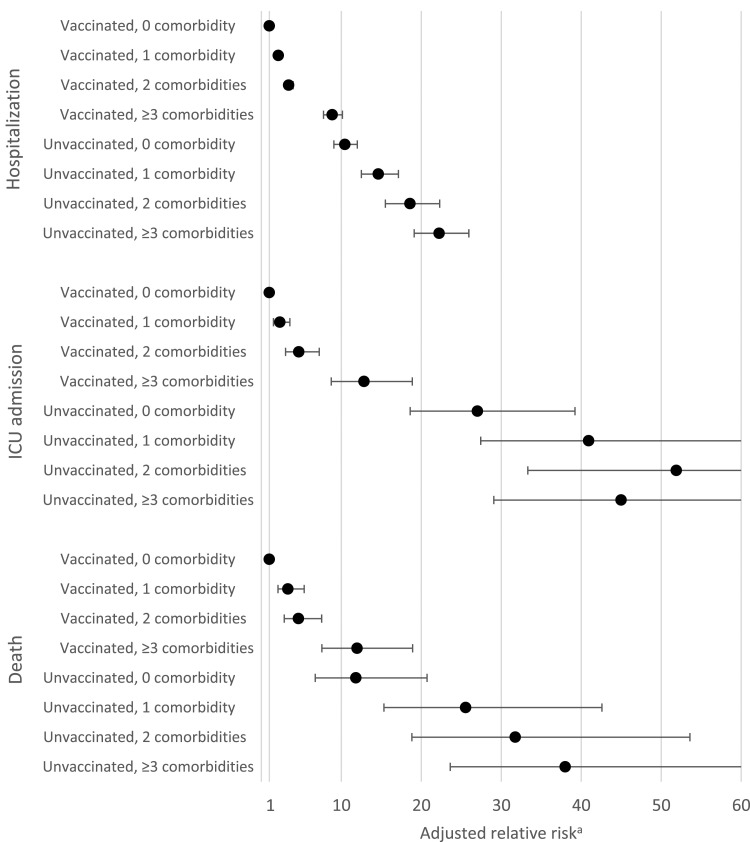
After adjustment for age and all other covariates, the risk of hospitalization (all age groups included) still increased for each additional comorbidity in both vaccinated and unvaccinated groups (Table 2, Figure 2) and the risk was consistently higher among unvaccinated. Compared with vaccinated cases without comorbidities, the risk of hospitalization was almost 9X higher (RRa=8.87; 95%CI[7.77-10.14]) in vaccinated cases with ≥3 comorbidities, but it was 22X higher (RRa=22.24; 95%CI[19.07-25.95]) in unvaccinated cases with ≥3 comorbidities. The adjusted relative risks also indicated that the risks of hospitalisation where similar between the 0 comorbidities/unvaccinated group and ≥3 comorbidities/vaccinated group.
Table 2.
Association between the number of comorbidities and the risks of COVID-19 hospitalisation, intensive care unit admission or death by 13th February 2022 while accounting for vaccination status during the Omicron wave among adults with COVID-19 identified during the Omicron wave (Dec 5th 2021-Jan 9th 2022, Quebec, Canada) (n = 245,956).
| Vaccination status a | Number of comorbidities | Frequency | Adjusted Relative Risk | ||
|---|---|---|---|---|---|
| Event | Non-event | RRa | [IC 95%] | ||
| Hospitalization | |||||
| Vaccinated | 0 | 368 | 140,163 | 1.00 | (reference group) |
| 1 | 416 | 46,287 | 2.13 | [1.85−2.46] | |
| 2 | 358 | 16,271 | 3.42 | [2.94−3.97] | |
| ≥3 | 1,953 | 16,770 | 8.87 | [7.77−10.14] | |
| Unvaccinated | 0 | 407 | 15,078 | 10.44 | [9.07−12.01] |
| 1 | 234 | 4,430 | 14.63 | [12.48−17.14] | |
| 2 | 150 | 1,424 | 18.59 | [15.50−22.29] | |
| ≥3 | 356 | 1,291 | 22.24 | [19.07−25.95] | |
| ICU admission | |||||
| Vaccinated | 0 | 38 | 140,493 | 1.00 | (reference group) |
| 1 | 50 | 46,653 | 2.32 | [1.51−3.56] | |
| 2 | 51 | 16,578 | 4.68 | [3.02−7.23] | |
| ≥3 | 227 | 18,496 | 12.84 | [8.74−18.87] | |
| Unvaccinated | 0 | 108 | 15,377 | 27.02 | [18.61−39.22] |
| 1 | 70 | 4,594 | 40.93 | [27.43−61.06] | |
| 2 | 43 | 1,531 | 51.90 | [33.32−80.83] | |
| ≥3 | 63 | 1,584 | 44.99 | [29.06−69.67] | |
| Death | |||||
| Vaccinated | 0 | 23 | 140,508 | 1.00 | (reference group) |
| 1 | 78 | 46,625 | 3.32 | [2.07−5.35] | |
| 2 | 82 | 16,547 | 4.64 | [2.86−7.54] | |
| ≥3 | 674 | 18,049 | 11.97 | [7.57−18.91] | |
| Unvaccinated | 0 | 24 | 15,461 | 11.82 | [6.74−20.71] |
| 1 | 41 | 4,623 | 25.55 | [15.32−42.59] | |
| 2 | 41 | 1,533 | 31.75 | [18.82−53.59] | |
| ≥3 | 145 | 1,502 | 38.00 | [23.62−61.14] | |
Abbreviation: ICU: Intensive care unit; RRa:Relative risk adjusted for age, sex, week, living environment, material and social deprivation
aThe vaccinated group included all individuals adequately vaccinated, i.e., all individuals who received two vaccine doses (or one Janssen vaccine dose) or a combination of these vaccines with a respected minimal interval between the 2 doses. The unvaccinated group included all other individuals.
Figure 2.
Risks of COVID-19 hospitalisation, intensive care unit admission or death according to the number of comorbidities and the vaccination status by 13th February 2022 during the Omicron wave among adults with COVID-19 identified during the Omicron wave (Dec 5th 2021-Jan 9th 2022, Quebec, Canada) (n = 245,956). Abbreviation: ICU: Intensive care unit. a Adjusted for age, sex, week, living environment, material and social deprivation.
ICU admissions
The proportion of cases with ICU admission increased for each additional comorbidity in all age groups except in the unvaccinated ≥75 age group where it gradually decreased with the number of comorbidities (Figure 1). Proportion of cases with ICU admission in unvaccinated were consistently higher than in vaccinated cases in all subgroups.
In the adjusted analysis (all age groups included), there was an association between each additional comorbidity and the risk of ICU admission in both vaccinated and unvaccinated groups (Table 2, Figure 2). Furthermore, the adjusted relative risk of ICU admission was consistently higher among unvaccinated, and we may observe that the risks were lower in the ≥3 comorbidities/vaccinated group than in the 0 comorbidities/unvaccinated group.
Deaths
The proportion of cases with death increased for each additional comorbidity in all age groups in both vaccinated and unvaccinated cases (Figure 1). Among the vaccinated cases, the percentage of death increased from <0.1% to 0.1% and from 1.5% to 7.6% in the 18-49 and ≥75 age groups, respectively, when the number of comorbidities increased from 0 to ≥3. In unvaccinated individuals, each additional comorbidity was also associated with an increase in the percentage of death in all age groups, and percentages was systematically higher than among vaccinated cases.
After adjustment for age and all other covariates, we observed that the risk of death increased for each additional comorbidity in both vaccinated and unvaccinated groups (Table 2, Figure 2) and that the risk was consistently higher among unvaccinated cases. Compared with vaccinated cases without comorbidities, the risk of death was almost 12X higher (RRa=11.97; 95%CI[7.57-18.91]) in vaccinated cases with ≥3 comorbidities, but it was 38X higher (RRa=38.00; 95%CI[23.62-61.14]) in unvaccinated cases with ≥3 comorbidities. The adjusted relative risks also indicated that the risks of death where similar between the 0 comorbidities/unvaccinated group and ≥3 comorbidities/vaccinated group.
Sensitivity and supplementary analysis
The proportion of cases with hospitalization, ICU admission or death stratified by number of comorbidities were very similar when restricted to the last two weeks of available data when the proportion of Omicron variant cases was greater than 90% when we included hospital-associated cases (except that we observed higher percentage of hospitalization among older adults and those with a higher number of comorbidities) (supplementary file, Tables A.3, A.4, A.7, A.8). The increase with each additional comorbidity in the percentage of hospitalization, ICU admission or death of COVID-19 cases was also observed by number of vaccine doses (supplementary file, Table A.5). In general, risk decreased with the increase of the number of vaccine dose. Estimation of relative risks by age subgroups were possible only for the hospitalisation outcome. Since interaction terms with age were not significant [for ICU admission] or model failed to converge [for death], age subgroups for both outcomes are not reported. The risk of hospitalization for each age subgroup increased for each additional comorbidity in both vaccinated and unvaccinated groups (supplementary file, Table A.9) and the risk was consistently higher among unvaccinated.
Discussion
In this cohort study based on COVID-19 population-based surveillance data, comorbidities remained a significant risk factor of severe complications among COVID-19 cases during the Omicron wave of the pandemic. The proportion of cases with hospitalization, ICU admission, and death increased with the number of comorbidities and the impact of comorbidities appeared to be higher in unvaccinated individuals. Also, the proportion of complications in vaccinated individuals with ≥3 comorbidities were lower than in unvaccinated individuals without comorbidities.
The association we observed in this study between the number of comorbidities and the risk of hospitalization when taking into account the vaccination status is similar to that in a Danish study using surveillance data. 8 In their study, Kahn et al. included 55,269 COVID-19 confirmed cases during the Omicron wave and observed similar associations but a lower risk of hospitalization in both vaccinated and unvaccinated groups. The higher risk of hospitalization observed in our study may be explained by a lower testing capacity in the province of Québec or COVID-19 positives cases hospitalized for non-COVID reasons, possibly more frequent among individuals with comorbidities. To our knowledge, no study has explored the association between the number of comorbidities and the risks of ICU admission or death during the Omicron wave. A pre-print paper using surveillance data of 50 Omicron hospitalized cases in France has shown a higher rate of serious hospital event (that included ICU admission or death) among cases with at least one comorbidity than among those without. 19
In the ≥75 age group, we observed that the proportion of ICU admission was lower than in the 65-74 age group and it was decreasing with increased number of comorbidities. A similar pattern has been observed in all Canadian provinces since the pandemic outbreak. 20 In patients with unfavourable prognosis related to underlying illnesses, a less aggressive therapeutic approach is generally adopted and in Quebec it is determined by a form specifying the predefined levels of care. 21 The lower proportion of ICU admission in the very elderly and those with more comorbidities may be explained by the fact that higher proportion of these groups have predefined levels of care that preclude ICU admission.22,23
This study shows that vulnerability to COVID-19 is higher in unvaccinated individuals, even in the absence of comorbidities. Similar or even lower adjusted risks of hospitalization, ICU admission, and death in vaccinated individuals with ≥3 comorbidities than in unvaccinated individuals without comorbidities indicate a potential efficacy of adequate vaccination in later groups. Furthermore, these results suggest that vaccination may reduce the risk of complications also in individuals not seeing themselves as vulnerable.A key strength of our study is the use of a population-based surveillance database that includes all laboratory confirmed cases in the province of Quebec, Canada. Because the testing capacity was widely available and free of charge, information on a large number of confirmed COVID-19 cases was available. We only excluded cases with no information on their pre-existing medical conditions. As the characteristics of the study population is similar to all cases registered in the surveillance database, our result seemed generalizable to all confirmed COVID-19 cases (supplementary file, Table A.6). Another strength of our surveillance database is the real-time access to the vaccination status, to COVID-19 related hospitalization (including ICU admission) and COVID-19 related death. The low discrepancy between the reported COVID-19 deaths and their estimation based on overall mortality may suggest an adequate report of death information due to COVID-19 in the province of Québec which limits misclassification. 24
A major limitation of our study is that we do not have information on the variant of the virus at the individual-level. The only information available is the weekly proportion of Omicron variant among randomly sampled cases. 7 On the first day of our study (December 5th, 2021), 38% of confirmed cases were Omicron variant and by the end of the week, 73% were Omicron variant. This proportion increase to 86% on December 19th, 2021, and 96% by the end of the study (January 9th, 2022). Tests performed on 627 hospitalized patients (admitted between December 21st and January 10th show that the Delta variant was more present in hospitals (around 20% of tested patients); this suggests that the burden of COVID-19 on the population was still influenced in part by the Delta variant during the Omicron wave. 25 To reduce the potential contamination of our study population by Delta cases, we performed a sensitivity analysis on confirmed cases between December 26th, 2021, and January 9th, 2022, when the proportion of Omicron variant was higher than 90%. The results were quite similar to those of the main analysis. This similarity may be explained by the fact that the majority of cases included in the study (71%) where confirmed in these last two weeks. Another limitation is that the testing capacity was under pressure due to the rapid increase in the number of cases during the Omicron wave. This may have led to an overestimation of proportion of cases with complication, especially among groups of people at lower risk of complications (younger, without pre-existing medical conditions persons), and consequently to an overestimation of the percentage point estimate in those groups and thus to an underestimation of relative risk between groups with and without comorbidities. A shorter lookback search window in administrative data file for cancer, depression and drug and alcohol abuse (5-years), as opposed to 10-years for other diseases, may also have led to an underestimation of relative risk between groups with and without comorbidities, 8 we were unable to distinguish between hospitalization with COVID-19 as the primary cause and incidental cases admitted to hospital for reasons other than COVID-19. Unpublished data using our database show that a majority of hospitalizations during the study period were related to COVID-19 as the primary reason for admission. Patients admitted for reasons other than COVID-19 may have more comorbidities than those admitted for COVID-19. However, because comorbidities are a risk factor for COVID-19 hospitalization, the opposite may also be true. Because we lack information on the distribution of comorbidities among these 2 groups, it is difficult to assess whether our point estimates overestimate or underestimate the true association between comorbidity and hospitalization for COVID-19.
Conclusion
This study using population-based surveillance data shows that comorbidities remain consistently associated with increased risks of hospitalization, ICU admission, and death in Omicron COVID-19 cases, similar to previous SARS-CoV2 variants, and that these risks are highest in unvaccinated individuals. Because the Omicron variant is at the moment of the submission of the manuscript the most prevalent worldwide, our results support the importance to promoting vaccination in persons with pre-existing medical conditions to reduce severe COVID-19 complications. A different study would be needed to study the impact of comorbidities on long COVID-19 in Omicron variant cases.
Supplemental Material
Supplemental Material for Impact of chronic comorbidities on hospitalization, intensive care unit admission and death among adult vaccinated and unvaccinated COVID-19 confirmed cases during the Omicron wave by Marc Simard, Véronique Boiteau, Élise Fortin, Sonia Jean, Louis Rochette, Pierre-Luc Trépanier and Rodica Gilca in Journal of Multimorbidity and Comorbidity
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental material: Supplemental material for this article is available online.
ORCID iD
Marc Simard https://orcid.org/0000-0002-9424-1926
References
- 1.Fang X, Li S, Yu H. Epidemiological, comorbidity factors with severity and prognosis of COVID-19: a systematic review and meta-analysis. Aging 2020; 12: 12493–12503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Williamson EJ, Walker AJ, Bhaskaran K. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020; 584: 430–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simard M, De Montigny C, Jean S, et al. Impact of comorbidities on the risk of death and hospitalization among confirmed cases of COVID-19 during the first months of the pandemic in Québec. 2020. [Google Scholar]
- 4.Ghazy RM, Ashmawy R, Hamdy NA. Efficacy and Effectiveness of SARS-CoV-2 Vaccines: A Systematic Review and Meta-Analysis. Vaccines 2022; 10: 350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mendiola-Pastrana IR, López-Ortiz E, Río de la Loza-Zamora JG. SARS-CoV-2 Variants and Clinical Outcomes: A Systematic Review. Life Basel Switz 2022; 12: 170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organisation . COVID-19 Weekly Epidemiological Update. Edition 69. Geneva, Switzerland: World Health Organization (WHO). [Google Scholar]
- 7.Institut national de santé publique du Québec . Données sur les variants du SRAS-CoV-2 au Québec. Données sur les variants du SRAS-CoV-2 au Québec, https://www.inspq.qc.ca/covid-19/donnees/variants (2022, accessed 28 March 2022). [Google Scholar]
- 8.Kahn F, Bonander C, Moghaddassi M. . Risk of severe COVID-19 from the Delta and Omicron variants in relation to vaccination status, sex, age and comorbidities - surveillance results from southern Sweden, July 2021 to January 2022. Euro Surveill 2022: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blais C, Jean S, Sirois C. Quebec Integrated Chronic Disease Surveillance System (QICDSS), an innovative approach. Chronic Dis Inj Can 2014; 34: 226–235. [PubMed] [Google Scholar]
- 10.Canadian Nosocomial Infection Surveillance Program . Surveillance for viral respiratory infections among inpatients in CNISP hospitals. Public Health Agency of Canada, 2021. [Google Scholar]
- 11.Ministère de la santé et des Services Sociaux . Guide de saisie_Décès_COVID-19.
- 12.Institut de la statistique du Québec . RED deaths database, https://statistique.quebec.ca/en/produit/publication/le-fichier-des-deces-du-registre-des-evenements-demographiques-red (accessed 31 March 2022).
- 13.World Health Organisation . International Guidelines for Certification and Classification(coding) of COVID-19 as Cause of Death. Geneva, Switzerland. [Google Scholar]
- 14.Simard M, Sirois C, Candas B. Validation of the Combined Comorbidity Index of Charlson and Elixhauser to Predict 30-Day Mortality Across ICD-9 and ICD-10. Med Care 2018; 56: 441–447. [DOI] [PubMed] [Google Scholar]
- 15.Simard M, Dubé M, Gaulin M, et al. La prévalence de la multimorbidité au Québec : portrait pour l’année 2016-2017. Institut national de santé publique du Québec, 2019. [Google Scholar]
- 16.Tonelli M, Wiebe N, Fortin M. Methods for identifying 30 chronic conditions: application to administrative data. BMC Med Inform Decis Mak 2015; 15: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Institut national de santé publique du Québec . Données de vaccination contre la COVID-19 au Québec, précisions méthodologiques. Données de vaccination contre la COVID-19 au Québec, précisions méthodologiques, https://www.inspq.qc.ca/covid-19/donnees/vaccination#methodologie (2022, accessed 28 March 2022). [Google Scholar]
- 18.Pampalon R, Raymond G. A deprivation index for health and welfare planning in Quebec. Chronic Can 2000; 21: 104–113. [PubMed] [Google Scholar]
- 19.Auvigne V, Vaux S, Strat YL, et al. Serious hospital events following symptomatic infection with Sars-CoV-2 Omicron and Delta variants: an exposed-unexposed cohort study in December 2021 from the COVID-19 surveillance databases in France. Epub ahead of print 8 February 2022. DOI: 10.1101/2022.02.02.22269952. [DOI] [PMC free article] [PubMed]
- 20.Government of Canada. COVID-19 daily epidemiology update. Government of Canada. [Google Scholar]
- 21.Ministère de la santé et des Services Sociaux . Niveaux de soins et réanimation cardiorespiratoire, http://msssa4.msss.gouv.qc.ca/intra/formres.nsf/961885cb24e4e9fd85256b1e00641a29/d57fc1d9eb98eed385257f50005206c7/$FILE/AH-744_DT9261(2016-01)D.pdf (2016).
- 22.Nguyen Y-L, Angus DC, Boumendil A. The challenge of admitting the very elderly to intensive care. Ann Intensive Care 2011; 1: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amini R, Gilca R, Carazo S. Surveillance des hospitalisations associées à la COVID-19 et autres virus respiratoires, saison grippale 2020-2021. 3171, Québec, Canada: Institut national de la santé publique du Québec. [Google Scholar]
- 24.Wang H, Paulson KR, Pease SA, et al. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. The Lancet; 0. Epub ahead of print 10 March 2022. DOI: 10.1016/S0140-6736(21)02796-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Institut national de santé publique du Québec . Comparaison des durées de séjour hospitalier selon le variant présomptif, https://www.inspq.qc.ca/covid-19/labo/durees-sejour-variants (2022, accessed 6 April 2022). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Impact of chronic comorbidities on hospitalization, intensive care unit admission and death among adult vaccinated and unvaccinated COVID-19 confirmed cases during the Omicron wave by Marc Simard, Véronique Boiteau, Élise Fortin, Sonia Jean, Louis Rochette, Pierre-Luc Trépanier and Rodica Gilca in Journal of Multimorbidity and Comorbidity