Key Points
Question
Does intravenous thrombolysis (IVT) prior to unsuccessful thrombectomy improve functional outcomes in patients with acute ischemic stroke compared with thrombectomy alone?
Findings
In this multicenter cohort study of 746 patients with acute ischemic stroke, prior treatment with IVT was associated with improved functional outcomes on the modified Rankin Scale at 90 days compared with thrombectomy alone.
Meaning
These findings suggest a new perspective to the debate on noninferiority of combined stroke treatment; the subgroup of patients with unsuccessful thrombectomy might particularly benefit from prior IVT, presumably driven by improvements of cerebral macrocirculation and microcirculation.
This cohort study investigates the potential treatment benefit of intravenous thrombolysis in patients with acute ischemic stroke due to large-vessel occlusion in whom successful mechanical reperfusion was not achieved.
Abstract
Importance
Clinical evidence of the potential treatment benefit of intravenous thrombolysis preceding unsuccessful mechanical thrombectomy (MT) is scarce.
Objective
To determine whether intravenous thrombolysis (IVT) prior to unsuccessful MT improves functional outcomes in patients with acute ischemic stroke.
Design, Setting, and Participants
Patients were enrolled in this retrospective cohort study from the prospective, observational, multicenter German Stroke Registry–Endovascular Treatment between May 1, 2015, and December 31, 2021. This study compared IVT plus MT vs MT alone in patients with acute ischemic stroke due to anterior circulation large-vessel occlusion in whom mechanical reperfusion was unsuccessful. Unsuccessful mechanical reperfusion was defined as failed (final modified Thrombolysis in Cerebral Infarction grade of 0 or 1) or partial (grade 2a). Patients meeting the inclusion criteria were matched by treatment group using 1:1 propensity score matching.
Interventions
Mechanical thrombectomy with or without IVT.
Main Outcomes and Measures
Primary outcome was functional independence at 90 days, defined as a modified Rankin Scale score of 0 to 2. Safety outcomes were the occurrence of symptomatic intracranial hemorrhage and death.
Results
After matching, 746 patients were compared by treatment arms (median age, 78 [IQR, 68-84] years; 438 women [58.7%]). The proportion of patients who were functionally independent at 90 days was 68 of 373 (18.2%) in the IVT plus MT and 42 of 373 (11.3%) in the MT alone group (adjusted odds ratio [AOR], 2.63 [95% CI, 1.41-5.11]; P = .003). There was a shift toward better functional outcomes on the modified Rankin Scale favoring IVT plus MT (adjusted common OR, 1.98 [95% CI, 1.35-2.92]; P < .001). The treatment benefit of IVT was greater in patients with partial reperfusion compared with failed reperfusion. There was no difference in symptomatic intracranial hemorrhages between treatment groups (AOR, 0.71 [95% CI, 0.29-1.81]; P = .45), while the death rate was lower after IVT plus MT (AOR, 0.54 [95% CI, 0.34-0.86]; P = .01).
Conclusions and Relevance
These findings suggest that prior IVT was safe and improved functional outcomes at 90 days. Partial reperfusion was associated with a greater treatment benefit of IVT, indicating a positive interaction between IVT and MT. These results support current guidelines that all eligible patients with stroke should receive IVT before MT and add a new perspective to the debate on noninferiority of combined stroke treatment.
Introduction
Since 1995, intravenous thrombolysis (IVT) has been the standard of care in patients with ischemic stroke who present within 4.5 hours of symptom onset.1,2,3 In recent years, a paradigm shift occurred with the broad use of endovascular mechanical thrombectomy (MT) for the treatment of acute ischemic stroke due to large-vessel occlusion. Multiple randomized clinical trials have demonstrated the substantial treatment effect of MT for large-vessel occlusions, whereby all eligible patients received prior IVT.4,5,6,7,8,9,10,11
There has been much debate whether MT alone is as effective as combined IVT plus MT with respect to functional outcomes and periprocedural complications. While some studies found that functional outcomes did not differ significantly between patients with acute ischemic stroke who received and did not receive IVT before MT,4,12,13 others reported a clinical benefit of a combined treatment.14 Most recently, DIRECT-SAFE (DIRECT Endovascular Clot Retrieval Versus Standard Bridging Thrombolysis With Endovascular Clot Retrieval)15 and SWIFT DIRECT (Solitaire With the Intention for Thrombectomy Plus Intravenous t-PA Versus DIRECT Solitaire Stent-Retriever Thrombectomy in Acute Anterior Circulation Stroke)16 did not show noninferiority of MT alone compared with IVT plus MT in terms of functional outcomes. These important noninferiority trials had very low failure rates of MT and therefore investigated the treatment effect of IVT primarily in patients with successful mechanical flow restoration. However, international stroke registries and the HERMES (Highly Effective Reperfusion Evaluated in Multiple Endovascular Stroke Trials) meta-analysis4,17,18,19,20,21 reported unsuccessful mechanical reperfusion in up to 30% of patients, with potentially detrimental consequences for functional outcomes.
To date, clinical evidence of the efficacy and safety of IVT prior to unsuccessful MT is scarce. In this retrospective multicenter study, we aimed to investigate the potential treatment benefit of IVT in patients with acute ischemic stroke due to large-vessel occlusion in whom successful mechanical reperfusion was not achieved. We hypothesized that in this subgroup of patients, a combined treatment of IVT plus MT was associated with improved functional outcomes compared with MT alone. We further hypothesized that partial mechanical reperfusion might be associated with a greater treatment benefit of preceding IVT.
Methods
Study Design and Participating Centers
In this retrospective multicenter cohort study, we compared MT alone with IVT plus MT in patients with acute ischemic stroke with unsuccessful endovascular recanalization. Patients were enrolled from the German Stroke Registry–Endovascular Treatment (GSR-ET) study22 and treated between May 1, 2015, and December 31, 2021. The GSR-ET is an ongoing, prospective, open-label, multicenter registry including patients who received MT from 25 comprehensive stroke centers in Germany.23,24 The GSR-ET was approved by the responsible ethics committee of the Ludwig Maximilian University, Munich, Germany. In addition, the local ethics committee of each participating center gave approval to contribute fully anonymized data to the GSR-ET. Informed consent for this study was waived after review of the central ethics committee due to the retrospective design of the study. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.25
Study Cohort
Inclusion criteria were defined as follows: (1) diagnosis of acute ischemic stroke in the anterior circulation due to an isolated occlusion of the intracranial internal carotid artery or of the M1 or M2 segment of the middle cerebral artery; (2) treatment by MT with or without prior IVT; and (3) unsuccessful endovascular reperfusion defined as a final modified Thrombolysis in Cerebral Infarction (mTICI) grade of 0, 1, or 2a. Time from symptom onset to hospital admission and unknown symptom onset were not used as exclusion criteria. eFigure 1 in Supplement 1 provides a detailed flowchart of the inclusion and exclusion criteria. No specific data on race and ethnicity were given since this is outside the scope of the study and the hypothesis. Stroke is an entity that affects all sexes, ethnicities, and races alike, thus we would not expect an uneven distribution between these groups.
Clinical and Radiologic Assessment
Patient characteristics, radiological findings, and treatment outcomes were obtained from the GSR-ET. Baseline imaging, digital subtraction angiograms, and follow-up imaging were reviewed by local investigators at each participating center. The Alberta Stroke Program Early CT Score (ASPECTS) was used to determine the extent of baseline infarct hypoattenuation on results of noncontrast computed tomography of the head in 853 of 903 patients (94.5%) who met inclusion criteria.26 Baseline ASPECTS was assessed in 50 patients (5.5%) on magnetic resonance imaging. Unsuccessful reperfusion after MT was defined as a final mTICI grade of 0, 1, or 2a on angiographic images. In addition, unsuccessful reperfusion was subclassified into failed reperfusion (mTICI grade of 0 or 1) and partial reperfusion (mTICI grade of 2a).20 Clinical assessments were performed at baseline and at 90 days using the National Institutes of Health Stroke Scale (NIHSS) and the modified Rankin Scale (mRS).
Outcomes and Safety Measures
The primary outcome was a score of 0 to 2 on the mRS at 90 days, indicating functional independence. Secondary outcomes included a score of 0 to 3 on the mRS, indicating independent ambulation (at most moderate disability) and an ordinal shift across the mRS toward lower values (better functional outcomes) at 90 days. Safety outcomes were the occurrence of symptomatic intracranial hemorrhage within 24 hours and death within 90 days. Symptomatic intracranial hemorrhage was defined according to the Second European-Australasian Acute Stroke Study (ECASS II) as evidence of any intracranial hemorrhage within 24 hours and a corresponding neurological deterioration (defined as an increase of ≥4 points on the NIHSS).27
Statistical Analysis
Propensity score matching was performed to reduce the possible influence of selection bias and confounders on the treatment outcomes. The propensity scores were estimated using a multivariable logistic regression model in which the treatment status (administration of IVT) was regressed on selected baseline covariates: age, sex, NIHSS score on admission, and baseline ASPECTS. We conducted a 1:1 pair matching using nearest-neighbor matching without replacement (for detailed information see eMethods and eFigure 2 in Supplement 1).
Univariable comparisons were performed between treatment groups (MT alone and IVT plus MT) before and after propensity score matching. Categorical variables were reported as counts and percentages. Continuous variables were reported as median and IQR. Categorical variables were compared between treatment groups using the χ2 test. Continuous variables were compared between treatment groups using the Mann-Whitney test after assessment for normal distribution.
Odds ratios (ORs) and risk differences of binary outcome and safety measures were estimated before and after propensity score matching by means of univariable and multivariable logistic regression (eTables 1-3 in Supplement 1). The adjusted common OR representing the shift in the direction of lower values on the mRS (better functional outcomes) was estimated by multivariable ordinal logistic regression. The proportional odds assumption was met (Brant test omnibus, P = .07). Odds ratios and risk differences were adjusted for age, sex, interval from symptom onset to hospital admission, NIHSS score on admission, extensive baseline infarction defined as ASPECTS of 0 to 5, and final mTICI grade. Odds ratios and risk differences were reported with 95% CI. Complete case analysis was performed for all regression models. Patients with missing values are displayed in eFigure 1 in Supplement 1. We performed subgroup analyses of the primary and secondary outcomes to explore modifications to the value of IVT based on age, sex, interval from symptom onset to hospital admission, NIHSS score on admission, site of arterial occlusion, baseline ASPECTS, etiology of stroke, and final mTICI grade (eFigure 3 in Supplement 1).
A 2-tailed P < .05 was considered significant for all statistical tests. No adjustments for multiple tests were made, and the analyses were considered explorative. All analyses were performed using R statistical software, version 4.1.2 (R Project for Statistical Computing), RStudio statistical software, version 2021.09.1 + 372 (RStudio), and Stata/MP statistical software, version 17.0 (StataCorp LLC).
Results
Patient Characteristics
A total of 13 082 patients from the GSR-ET were assessed for eligibility (eFigure 1 in Supplement 1). After 1:1 propensity score matching, 746 patients were included for further analysis. Of those patients, 373 received MT alone and 373 received IVT plus MT. The median age of all patients was 78 (IQR, 68-84) years; 308 (41.3%) were men and 438 (58.7%) were women. The median NIHSS score on admission was 15 (IQR, 9-18) and the median baseline ASPECTS was 9 (IQR, 7-10). Failed mechanical reperfusion (mTICI grade 0 or 1) was observed in 481 patients (64.5%), while partial reperfusion (mTICI grade 2a) was achieved in 265 (35.5%). Patients who received IVT plus MT showed a lower frequency of atrial fibrillation (126 of 373 [33.8%] vs 179 of 373 [48.0%]; P < .001) and a lower rate of premedication with anticoagulants (23 of 373 [6.2%] vs 71 of 373 [19.0%]; P < .001). All other baseline patient and imaging characteristics, workflow times, and treatment characteristics were balanced between study groups after propensity score matching (Table 1).
Table 1. Baseline, Imaging, and Treatment Characteristics Compared Between Intravenous Thrombolysis Plus Thrombectomy and Thrombectomy Alone Before and After Propensity Score Matching.
| Characteristic | Treatment groupa | |||||||
|---|---|---|---|---|---|---|---|---|
| Before propensity score matching | After propensity score matching | |||||||
| All (n = 903) | MT alone (n = 513) | IVT plus MT (n = 390) | P value | All (n = 746) | MT alone (n = 373) | IVT plus MT (n = 373) | P value | |
| Baseline characteristics | ||||||||
| Age, median (IQR), y | 78 (68-84) | 78 (69-84) | 77 (65-84) | .08b | 78 (68-84) | 78 (68-84) | 77 (67-84) | .90b |
| Sex | ||||||||
| Men | 381/903 (42.2) | 221/513 (43.1) | 160/390 (41.0) | .54c | 308/746 (41.3) | 157/373 (42.1) | 151/373 (40.5) | .66c |
| Women | 522/903 (57.8) | 292/513 (56.9) | 230/390 (59.0) | 438/746 (58.7) | 216/373 (57.9) | 222/373 (59.5) | ||
| Prestroke mRS score 0-2d | 729/885 (82.4) | 411/501 (82.0) | 318/384 (82.8) | .76c | 600/732 (82.0) | 298/364 (81.9) | 302/368 (82.1) | .95c |
| Medical history | ||||||||
| Atrial fibrillation | 380/903 (42.1) | 251/513 (48.9) | 129/390 (33.1) | <.001c | 305/746 (40.9) | 179/373 (48.0) | 126/373 (33.8) | <.001c |
| Arterial hypertension | 716/903 (79.3) | 409/513 (79.7) | 307/390 (78.7) | .92c | 594/746 (79.6) | 297/373 (79.6) | 297/373 (79.6) | .61c |
| Diabetes | 197/903 (21.8) | 128/513 (25.0) | 69/390 (17.7) | .03c | 158/746 (21.2) | 90/373 (24.1) | 68/373 (18.2) | .13c |
| Dyslipidemia | 340/903 (37.7) | 198/513 (38.6) | 142/390 (36.4) | .76c | 285/746 (38.2) | 147/373 (39.4) | 138/373 (37.0) | .73c |
| Anticoagulant treatment | 123/903 (13.6) | 100/513 (19.5) | 23/390 (5.9) | <.001c | 94/746 (12.6) | 71/373 (19.0) | 23/373 (6.2) | <.001c |
| Etiology of stroke | ||||||||
| Large-artery atherosclerosis | 196/903 (21.7) | 102/513 (19.9) | 94/390 (24.1) | .03c | 165/746 (22.1) | 75/373 (20.1) | 90/373 (24.1) | .15c |
| Cardioembolism | 461/903 (51.1) | 283/513 (55.2) | 178/390 (45.6) | 373/746 (50.0) | 201/373 (53.9) | 172/373 (46.1) | ||
| Dissection | 10/903 (1.1) | 4/513 (0.8) | 6/390 (1.5) | 6/746 (0.8) | 2/373 (0.5) | 4/373 (1.1) | ||
| Stroke of other determined etiology | 51/903 (5.6) | 31/513 (6.0) | 20/390 (5.1) | 39/746 (5.2) | 22/373 (5.9) | 17/373 (4.6) | ||
| Stroke of undetermined etiology | 185/903 (20.5) | 93/513 (18.1) | 92/390 (23.6) | 163/746 (21.8) | 73/373 (19.6) | 90/373 (24.1) | ||
| Admission NIHSS score,e median (IQR) | 15 (10-19) | 15 (10-19) | 15 (9-18) | .41b | 15 (9-18) | 15 (9-19) | 15 (9-18) | .95b |
| Imaging characteristics | ||||||||
| Occlusion site | ||||||||
| ICA | 170/903 (18.8) | 89/513 (17.3) | 81/390 (20.8) | .42c | 143/746 (19.2) | 65/373 (17.4) | 78/373 (20.9) | .46c |
| MCA M1 | 451/903 (49.9) | 262/513 (51.1) | 189/390 (48.5) | 358/746 (48.0) | 181/373 (48.5) | 177/373 (47.5) | ||
| MCA M2 | 282/903 (31.2) | 162/513 (31.6) | 120/390 (30.8) | 245/746 (32.8) | 127/373 (34.0) | 118/373 (31.6) | ||
| Baseline ASPECTS,f median (IQR) | 8 (7-10) | 8 (7-10) | 9 (7-10) | <.001b | 9 (7-10) | 9 (7-10) | 9 (7-10) | .55b |
| Workflow times | ||||||||
| Stroke onset to admission, median (IQR), min | 122 (57-210) | 117 (57-240) | 129 (56-197) | .27b | 122 (57-206) | 107 (57-223) | 130 (57-198) | .79b |
| Missing data, No. | 413 | 304 | 109 | NA | 323 | 217 | 106 | NA |
| Stroke onset to groin, median (IQR), min | 210 (148-282) | 210 (145-320) | 210 (150-275) | .75b | 210 (150-282) | 200 (145-314) | 214 (152-276) | .84b |
| Missing data, No. | 430 | 311 | 119 | NA | 337 | 222 | 115 | NA |
| Treatment characteristics | ||||||||
| Administration of IVT | 390/903 (43.2) | 0/513 | 390/390 (100.0) | NA | 373/746 (50.0) | 0/373 | 373/373 (100.0) | NA |
| General anesthesia | 592/903 (65.6) | 349/513 (68.0) | 243/390 (62.3) | .07c | 487/746 (65.3) | 252/373 (67.6) | 235/373 (63.0) | .19c |
| Final mTICI gradeg | ||||||||
| 0 | 471/903 (52.2) | 274/513 (53.4) | 197/390 (50.5) | .61c | 384/746 (51.5) | 194/373 (52.0) | 190/373 (50.9) | .93c |
| 1 | 117/903 (13.0) | 67/513 (13.1) | 50/390 (12.8) | 97/746 (13.0) | 49/373 (13.1) | 48/373 (12.9) | ||
| 2a | 315/903 (34.9) | 172/513 (33.5) | 143/390 (36.7) | 265/746 (35.5) | 130/373 (34.9) | 135/373 (36.2) | ||
Abbreviations: ASPECTS, Alberta Stroke Program Early CT Score; ICA, internal carotid artery; IVT, intravenous thrombolysis; MCA, middle cerebral artery; mRS, modified Rankin Scale; MT, mechanical thrombectomy; mTICI, modified Thrombolysis in Cerebral Infarction; NA, not applicable; NIHSS, National Institutes of Health Stroke Scale.
Unless otherwise indicated, data are expressed as No./total No. (%) of patients. Percentages have been rounded and may not total 100.
Compared between MT and IVT plus MT groups using Mann-Whitney test for continuous variables.
Compared between MT and IVT plus MT groups using χ2 test for categorical variables.
Scores range from 0 to 6, with higher scores indicating greater disability.
Scores range from 0 to 42, with higher scores indicating worse neurologic deficits.
Scores range from 0 to 10, with lower scores indicating larger infarction.
Scores range from 0 to 3, with higher grades indicating increased reperfusion.
Primary and Secondary Outcomes
The percentage of patients who achieved functional independence, defined as an mRS score of 0 to 2 at 90 days, was 68 of 373 (18.2%) in the IVT plus MT group and 42 of 373 (11.3%) in the MT alone group (adjusted OR [AOR], 2.63 [95% CI, 1.41-5.11]; P = .003). The adjusted risk difference in the proportion of patients who were functionally independent was 6.6% in favor of the IVT plus MT group (95% CI, 4.7%-8.4%; P = .003) (Table 2).
Table 2. Functional Outcomes and Safety Measures After Propensity Score Matching.
| Outcome | Treatment group after propensity score matchinga | Adjusted risk difference (95% CI), %b | Unadjusted OR (95% CI) | Adjusted OR (95% CI)b | P value | |||
|---|---|---|---|---|---|---|---|---|
| All (n = 746) | MT alone (n = 373) | IVT plus MT (n = 373) | P value | |||||
| Primary | ||||||||
| 90-d mRS score 0-2c | 110 (14.7) | 42/373 (11.3) | 68/373 (18.2) | .007d | 6.6 (4.7 to 8.4) | 1.76 (1.17 to 2.68) | 2.63 (1.41 to 5.11) | .003 |
| Secondary | ||||||||
| 90-d mRS score 0-3c | 173 (23.2) | 74/373 (19.8) | 99/373 (26.5) | .03d | 6.7 (1.8 to 11.6) | 1.46 (1.04 to 2.06) | 1.76 (1.03 to 3.04) | .04 |
| 90-d mRS score,c median (IQR) | 5 (4 to 6) | 6 (4 to 6) | 5 (3 to 6) | .002e | NA | 1.51 (1.16 to 1.98)f | 1.98 (1.35 to 2.92)f | <.001 |
| Safety measures | ||||||||
| Symptomatic ICH within 24 h | 44/737 (6.0) | 22/370 (5.9) | 22/367 (6.0) | .98d | 0.0 (−3.4 to 3.4) | 1.00 (0.54 to 1.84) | 0.71 (0.29 to 1.81) | .45 |
| Death within 90 d | 366/746 (49.1) | 201/373 (53.9) | 165/373 (44.2) | .008d | −11.2 (−19.2 to −3.2) | 0.68 (0.51 to 0.91) | 0.54 (0.34 to 0.86) | .01 |
Abbreviations: ICH, intracranial hemorrhage; IVT, intravenous thrombolysis; mRS, modified Rankin Scale; MT, mechanical thrombectomy; NA, not applicable; OR, odds ratio.
Unless otherwise indicated, data are expressed as No./total No. (%) of patients.
Results were adjusted for age, sex, interval from symptom onset to hospital admission, National Institutes of Health Stroke Scale, Alberta Stroke Program Early CT Score, and final modified Thrombolysis in Cerebral Infarction grade.
Scores range from 0 to 6, with higher scores indicating greater disability.
Compared between MT and IVT plus MT groups using a χ2 test for categorical variables.
Compared between MT and IVT plus MT groups using Mann-Whitney test for continuous variables.
Common OR was derived from ordinal logistic regression analysis. Values greater than 1 indicate a shift in the distribution of 90-day mRS scores toward lower values (better functional outcomes) favoring IVT plus MT compared with MT alone.
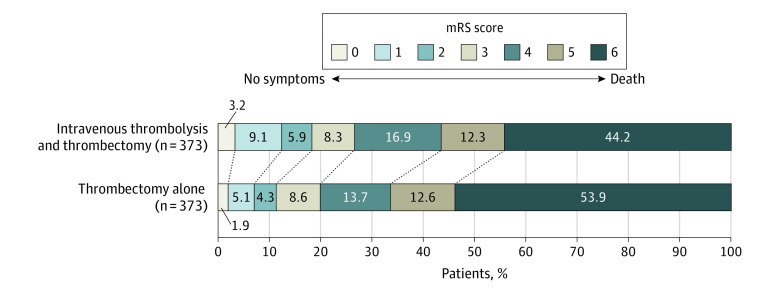
As a secondary outcome, treatment with IVT plus MT was associated with higher odds of achieving independent ambulation, defined as an mRS score of 0 to 3 at 90 days (AOR, 1.76 [95% CI, 1.03-3.04]; P = .04). There was a shift in the distribution of 90-day mRS scores toward lower values (better functional outcomes) in patients with IVT plus MT compared with MT alone (adjusted common OR, 1.98 [95% CI, 1.35-2.92]; P < .001). The direction of the shift was consistent for all levels on the mRS (Figure 1).
Figure 1. Distribution of Modified Rankin Scale (mRS) Scores at 90 Days After Stroke Stratified by Administration of Intravenous Thrombolysis.
The mRS scores range from 0 to 6, with 0 indicating no symptoms; 1, no clinically significant disability; 2, slight disability; 3, moderate disability (patient is able to walk unassisted); 4, moderately severe disability; 5, severe disability; and 6, death. There was a significant difference between the 2 treatment groups in the overall distribution of scores in the multivariable ordinal regression analysis, favoring the intravenous thrombolysis plus thrombectomy group (adjusted common odds ratio, 1.98 [95% CI, 1.35-2.92]; P < .001).
Subgroup Analysis
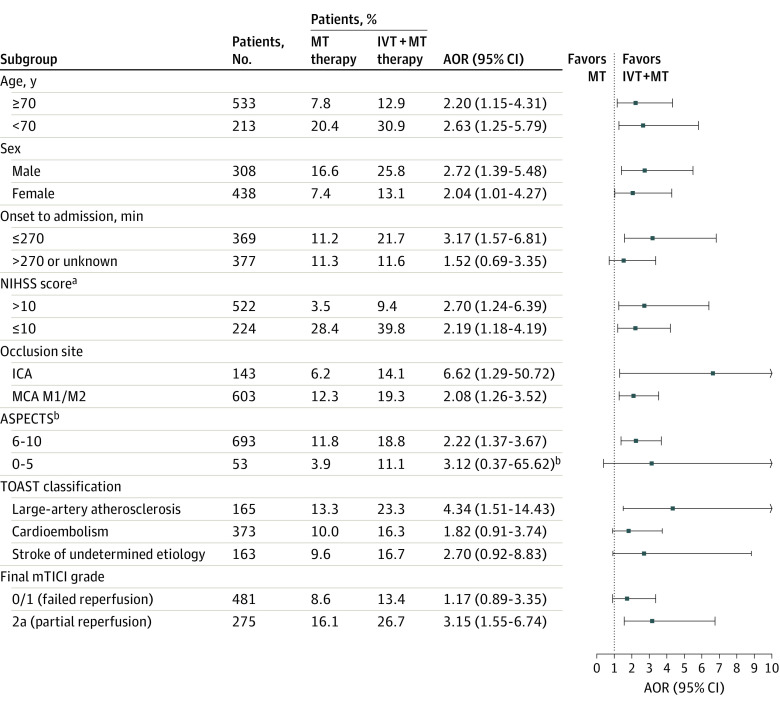
Subgroup analyses for the primary outcome are shown in Figure 2. The odds of achieving functional independence at 90 days were generally in the same direction favoring the treatment with IVT across all predefined subgroups. Prior treatment with IVT remained associated with improved functional outcomes in patients of different sex (women and men), older and younger patients (<70 and ≥70 years), those with higher and lower NIHSS scores on admission (≤10 and >10 points), and those with ASPECTS of 6 to 10, various sites of arterial occlusion (internal carotid artery and middle cerebral artery), and stroke due to large-artery atherosclerosis. A treatment benefit was also observed in patients who were admitted to the hospital within 4.5 hours after onset, but not in those who arrived after 4.5 hours or with unknown onset.
Figure 2. Subgroup Analyses for Functional Independence.
The forest plot demonstrates that the odds of achieving functional independence at 90 days (defined as modified Rankin Scale sores of 0 to 2) favored the intravenous thrombolysis plus mechanical thrombectomy (IVT plus MT) group across all predefined subgroups. Arrows indicate that the limits of the 95% CI are not fully shown. AOR indicates adjusted odds ratio; ASPECTS, Alberta Stroke Program Early CT Score; ICA, internal carotid artery; IVT, intravenous thrombolysis; MCA, middle cerebral artery; MT, mechanical thrombectomy; mTICI, modified Thrombolysis in Cerebral Infarction; NIHSS, National Institutes of Health Stroke Scale; TOAST, Trial of ORG 10172 in Acute Stroke Treatment.44
aScores ranges from 0 to 42, with higher scores indicating worse neurologic deficits.
bScores range from 0 to 10, with lower scores indicating larger infarction.
Treatment with IVT was associated with higher odds of achieving functional independence at 90 days in the subgroup of patients with partial reperfusion (mTICI grade 2a), while no treatment benefit of IVT was found in patients with failed reperfusion (mTICI grade 0 or 1). However, patients with failed reperfusion who received IVT plus MT had a higher likelihood of achieving independent ambulation at 90 days compared with patients who received MT alone (eFigure 3 in Supplement 1).
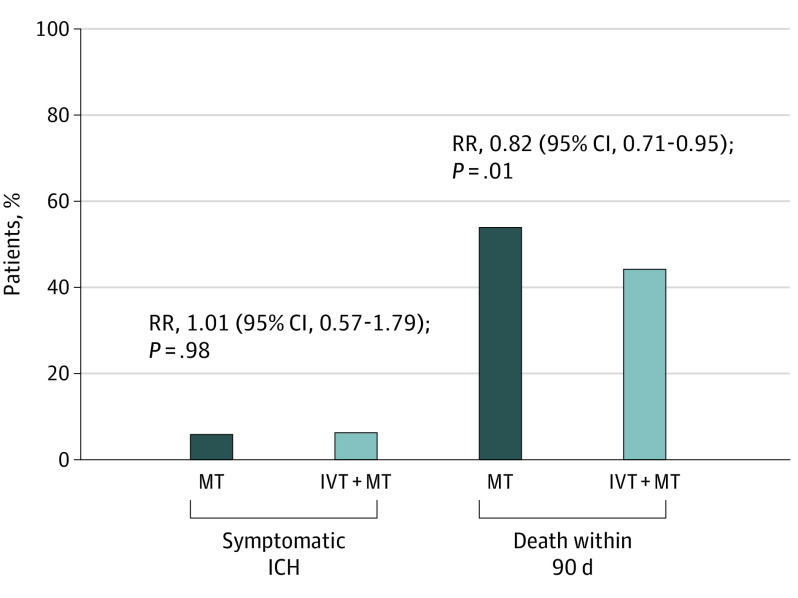
Safety Outcomes
The rate of symptomatic intracranial hemorrhage was 22 of 367 (6.0%) in the IVT plus MT group and 22 of 370 (5.9%) in the MT group (P = .98). There was no difference in symptomatic intracranial hemorrhage between the treatment groups (AOR, 0.71 [95% CI, 0.29-1.81]; P = .45). Death within 90 days was less frequent in patients who received IVT plus MT compared with patients who received MT alone (165 of 373 [44.2%] vs 201 of 373 [53.9%]; P = .008; AOR, 0.54 [95% CI, 0.34-0.86]; P = .01) (Table 2 and Figure 3).
Figure 3. Safety Outcomes Stratified by Administration of Intravenous Thrombolysis (IVT).
There was no difference in symptomatic intracranial hemorrhage (ICH) between IVT plus mechanical thrombectomy (MT) and MT alone (22 of 367 [6.0%] vs 22 of 370 [5.9%]; P = .98). However, death within 90 days decreased in patients who received IVT plus MT compared with MT alone (164 of 373 [44.2%] vs 201 of 373 [53.9%]; P = .008). RR indicates relative risk.
Discussion
This retrospective multicenter cohort study investigated the potential treatment benefit of IVT preceding unsuccessful mechanical reperfusion in patients with acute ischemic stroke due to large-vessel occlusion in the anterior circulation. Our findings suggest that a combined treatment with IVT plus MT was associated with improved functional outcomes at 90 days compared with MT alone in patients with unsuccessful reperfusion. The treatment benefit of IVT was greater in patients in whom partial reperfusion (mTICI grade 2a) was achieved during MT compared with those with failed reperfusion (mTICI grade 0 or 1). The rate of symptomatic intracranial hemorrhage was not higher in patients who received IVT prior to MT, while mortality at 90 days was lower in the IVT plus MT group. This study provides novel insights into patients with acute ischemic stroke when successful endovascular recanalization cannot be achieved and adds a new perspective to the recent debate whether MT alone is equally as effective as IVT plus MT in large-vessel occlusions.
Reliable data on IVT prior to unsuccessful thrombectomy are scarce. In 6 major randomized noninferiority trials, consistently less than 20% of patients had a final mTICI grade of 2b or lower, and even 10% or less in SWIFT DIRECT and DIRECT-SAFE trials.15,16,28,29,30 This very low failure rate might be explained by the conservative and strict selection of patients and the high standard of care of participating centers. However, international stroke registries suggest higher rates of patients with unsuccessful reperfusion during MT.17,21,31 Consequently, patients without mechanical flow restoration might be underrepresented in the latest noninferiority trials compared with clinical data, although this subgroup might particularly benefit from additional IVT.
In this study, treatment with IVT preceding unsuccessful MT was associated with higher rates of functional independence and a shift toward better functional outcomes on the mRS at 90 days. At the macrocirculatory level, the treatment benefit of IVT may be explained by delayed reperfusion after MT has been discontinued with failed or only partial recanalization of the large-vessel occlusion. A recent study32 described the phenomenon of delayed reperfusion in patients with stroke who underwent incomplete mechanical recanalization, largely due to persisting distal occlusions, and its favorable association with both tissue outcome and functional independence. To date, empirical evidence of delayed reperfusion and its clinical benefit in patients with unsuccessful MT is missing. This hypothesis requires further investigation, for example, by studies using multimodal computed tomography as follow-up imaging.
Recently, the CHOICE (Intraarterial Alteplase Versus Placebo After Mechanical Thrombectomy) trial and observational studies suggested a clinical benefit of adjunct intra-arterial thrombolysis after both successful and unsuccessful mechanical reperfusion, hypothetically driven by improved perfusion at the microcirculatory level.33,34,35 Whether this pathophysiological concept can be applied to patients who received IVT prior to successful or even unsuccessful MT remains unclear. Our findings point to potential improvements in functional outcomes by preceding IVT, despite the persistence of a large-vessel occlusion, which might also result from improved capillary perfusion in ischemic brain tissue due to removal of microemboli.36 In this context, better pial arterial collateral flow and cerebral tissue microperfusion could mediate a wider distribution and higher effectiveness of thrombolytic agents in the microcirculation, as proposed by prior studies.36,37,38 Future studies are warranted to investigate the interaction of IVT with the collateral status and elucidate the use of adjunct intra-arterial thrombolysis in patients with unsuccessful reperfusion in more detail.
Our subgroup analyses suggest that prior treatment with IVT was associated with greater odds of achieving functional independence in patients with partial reperfusion (mTICI grade 2a) compared with those with failed reperfusion (mTICI grade 0 or 1). Partial flow restoration might result in a better distribution and higher effectiveness of thrombolytic agents across the affected hemisphere. In addition, partial reperfusion itself was associated with higher odds of achieving functional independence at 90 days. The potential synergy of these effects underlines the importance of achieving the highest possible degree of reperfusion on the mTICI scale, even among patients with technically unsuccessful MT. Notably, our data also point to a potential treatment benefit of IVT in patients with failed reperfusion (mTICI grade 0 or 1) reflected by the higher rates of independent ambulation at 90 days defined as mRS scores of 0 to 3. The subgroup of patients with failed reperfusion might profit from IVT, as the thrombolytic effects could improve cerebral microperfusion, even after MT has been discontinued.36,39
Our findings support the safety of IVT preceding unsuccessful mechanical reperfusion. The rate of symptomatic intracranial hemorrhage did not differ between the 2 treatment groups, which is in line with prior studies on combined treatment.15,16,29,40 The risk of death at 90 days decreased from 53.9% to 44.2% in patients who received IVT plus MT compared with MT alone. Accordingly, a large meta-analysis showed a significant reduction in death for administration of IVT in the framework of best medical treatment.41 In combination with MT, the MR CLEAN-NO IV (Endovascular Treatment for Acute Ischemic Stroke in the Netherlands) trial reported a strong trend toward lower rates of death in the IVT group, but none of the noninferiority trials found a significant treatment effect on mortality.15,16,29,40 The reduction of death rates should be treated with caution until further evidence becomes available.
Limitations
This study has certain limitations. First, the retrospective and nonrandomized study design might introduce selection bias and reduce the generalizability of the main findings. We performed propensity score matching to create balanced distributions of baseline characteristics between the treatment groups. However, unmeasured confounders, such as medical contraindications for IVT, might lead to a higher prestroke morbidity in the MT alone group, which could worsen functional outcomes in this treatment group. A subanalysis of IRIS (Improving Reperfusion Strategies in Ischemic Stroke), a meta-analysis of 6 randomized noninferiority trials,42 could further elucidate the value of IVT prior to MT in the subgroup of patients with unsuccessful reperfusion. Second, no adjustments for multiple tests were made and the analyses should therefore be considered explorative. Third, the subgroup analysis implies that the clinical benefit of IVT is time dependent as shown in prior studies.43 However, the exact starting time of IVT was not collected by the GSR-ET and precluded a more detailed analysis on the temporal dependency. Fourth, imaging information, such as the final mTICI grades, were determined by local investigators at each study center without standardized assessment by an independent core laboratory. Fifth, while the study results are based on a White population, future studies should validate our findings in different ethnic groups.
Conclusion
The findings of this multicenter cohort study suggest that IVT preceding unsuccessful mechanical reperfusion is safe and improves functional outcomes at 90 days. Partial mechanical reperfusion was associated with a greater treatment benefit of IVT, indicating a positive synergy between IVT and MT. Patients with prior IVT and failed mechanical reperfusion still achieved higher rates of independent ambulation compared with those treated by MT alone. Hence, the subgroup of patients with unsuccessful MT might particularly benefit from prior IVT, presumably due to improvements in cerebral macrocirculation and microcirculation. Our study adds a new perspective to the debate on the latest noninferiority trials, in which patients with unsuccessful mechanical reperfusion might be underrepresented compared with clinical data.
eMethods. Propensity Score Matching
eFigure 1. Flowchart of Patient Inclusion and Exclusion Criteria
eFigure 2. Propensity Score Matching
eFigure 3. Subgroup Analyses for Independent Ambulation
eTable 1. Functional Outcomes and Safety Measures Before Propensity Score Matching
eTable 2. Multivariable Logistic Regression Models
eTable 3. Multivariable Ordinal Logistic Regression Model
Nonauthor Collaborators. German Stroke Registry–Endovascular Treatment Investigators
Data Sharing Statement
References
- 1.Ma H, Campbell BCV, Parsons MW, et al. ; EXTEND Investigators . Thrombolysis guided by perfusion imaging up to 9 hours after onset of stroke. N Engl J Med. 2019;380(19):1795-1803. doi: 10.1056/NEJMoa1813046 [DOI] [PubMed] [Google Scholar]
- 2.Lees KR, Emberson J, Blackwell L, et al. ; Stroke Thrombolysis Trialists’ Collaborators Group . Effects of alteplase for acute stroke on the distribution of functional outcomes: a pooled analysis of 9 trials. Stroke. 2016;47(9):2373-2379. doi: 10.1161/STROKEAHA.116.013644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from TPA therapy? an analysis of patient eligibility. Neurology. 2001;56(8):1015-1020. doi: 10.1212/WNL.56.8.1015 [DOI] [PubMed] [Google Scholar]
- 4.Goyal M, Menon BK, van Zwam WH, et al. ; HERMES collaborators . Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723-1731. doi: 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- 5.Goyal M, Demchuk AM, Menon BK, et al. ; ESCAPE Trial Investigators . Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019-1030. doi: 10.1056/NEJMoa1414905 [DOI] [PubMed] [Google Scholar]
- 6.Jovin TG, Nogueira RG, Lansberg MG, et al. Thrombectomy for anterior circulation stroke beyond 6 h from time last known well (AURORA): a systematic review and individual patient data meta-analysis. Lancet. 2022;399(10321):249-258. doi: 10.1016/S0140-6736(21)01341-6 [DOI] [PubMed] [Google Scholar]
- 7.Jovin TG, Chamorro A, Cobo E, et al. ; REVASCAT Trial Investigators . Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296-2306. doi: 10.1056/NEJMoa1503780 [DOI] [PubMed] [Google Scholar]
- 8.Albers GW, Marks MP, Kemp S, et al. ; DEFUSE 3 Investigators . Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(8):708-718. doi: 10.1056/NEJMoa1713973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berkhemer OA, Fransen PS, Beumer D, et al. ; MR CLEAN Investigators . A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11-20. doi: 10.1056/NEJMoa1411587 [DOI] [PubMed] [Google Scholar]
- 10.Nogueira RG, Jadhav AP, Haussen DC, et al. ; DAWN Trial Investigators . Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378(1):11-21. doi: 10.1056/NEJMoa1706442 [DOI] [PubMed] [Google Scholar]
- 11.Campbell BC, Mitchell PJ, Kleinig TJ, et al. ; EXTEND-IA Investigators . Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009-1018. doi: 10.1056/NEJMoa1414792 [DOI] [PubMed] [Google Scholar]
- 12.Broeg-Morvay A, Mordasini P, Bernasconi C, et al. Direct mechanical intervention versus combined intravenous and mechanical intervention in large artery anterior circulation stroke: a matched-pairs analysis. Stroke. 2016;47(4):1037-1044. doi: 10.1161/STROKEAHA.115.011134 [DOI] [PubMed] [Google Scholar]
- 13.Coutinho JM, Liebeskind DS, Slater LA, et al. Combined intravenous thrombolysis and thrombectomy vs thrombectomy alone for acute ischemic stroke: a pooled analysis of the SWIFT and STAR studies. JAMA Neurol. 2017;74(3):268-274. doi: 10.1001/jamaneurol.2016.5374 [DOI] [PubMed] [Google Scholar]
- 14.Mistry EA, Mistry AM, Nakawah MO, et al. Mechanical thrombectomy outcomes with and without intravenous thrombolysis in stroke patients: a meta-analysis. Stroke. 2017;48(9):2450-2456. doi: 10.1161/STROKEAHA.117.017320 [DOI] [PubMed] [Google Scholar]
- 15.Mitchell PJ, Yan B, Churilov L, et al. ; DIRECT-SAFE Investigators . Endovascular thrombectomy versus standard bridging thrombolytic with endovascular thrombectomy within 4.5 h of stroke onset: an open-label, blinded-endpoint, randomised non-inferiority trial. Lancet. 2022;400(10346):116-125. doi: 10.1016/S0140-6736(22)00564-5 [DOI] [PubMed] [Google Scholar]
- 16.Fischer U, Kaesmacher J, Strbian D, et al. ; SWIFT DIRECT Collaborators . Thrombectomy alone versus intravenous alteplase plus thrombectomy in patients with stroke: an open-label, blinded-outcome, randomised non-inferiority trial. Lancet. 2022;400(10346):104-115. doi: 10.1016/S0140-6736(22)00537-2 [DOI] [PubMed] [Google Scholar]
- 17.Flottmann F, Broocks G, Faizy TD, et al. ; GSR investigators . Factors associated with failure of reperfusion in endovascular therapy for acute ischemic stroke: a multicenter analysis. Clin Neuroradiol. 2021;31(1):197-205. doi: 10.1007/s00062-020-00880-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zaidat OO, Castonguay AC, Nogueira RG, et al. TREVO stent-retriever mechanical thrombectomy for acute ischemic stroke secondary to large vessel occlusion registry. J Neurointerv Surg. 2018;10(6):516-524. doi: 10.1136/neurintsurg-2017-013328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Froehler MT, Saver JL, Zaidat OO, et al. ; STRATIS Investigators . Interhospital transfer before thrombectomy is associated with delayed treatment and worse outcome in the STRATIS registry (Systematic Evaluation of Patients Treated With Neurothrombectomy Devices for Acute Ischemic Stroke). Circulation. 2017;136(24):2311-2321. doi: 10.1161/CIRCULATIONAHA.117.028920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaesmacher J, Gralla J, Mosimann PJ, et al. Reasons for reperfusion failures in stent-retriever-based thrombectomy: registry analysis and proposal of a classification system. AJNR Am J Neuroradiol. 2018;39(10):1848-1853. doi: 10.3174/ajnr.A5759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.El Nawar R, Lapergue B, Piotin M, et al. ; ETIS Investigators . Higher annual operator volume is associated with better reperfusion rates in stroke patients treated by mechanical thrombectomy: the ETIS Registry. JACC Cardiovasc Interv. 2019;12(4):385-391. doi: 10.1016/j.jcin.2018.12.007 [DOI] [PubMed] [Google Scholar]
- 22.German Stroke Registry–Endovascular Treatment (GSR-ET). ClinicalTrials.gov identifier: NCT03356392. Accessed June 2015. https://clinicaltrials.gov/ct2/show/NCT03356392
- 23.Alegiani AC, Dorn F, Herzberg M, et al. Systematic evaluation of stroke thrombectomy in clinical practice: the German Stroke Registry Endovascular Treatment. Int J Stroke. 2019;14(4):372-380. doi: 10.1177/1747493018806199 [DOI] [PubMed] [Google Scholar]
- 24.Wollenweber FA, Tiedt S, Alegiani A, et al. Functional outcome following stroke thrombectomy in clinical practice. Stroke. 2019;50(9):2500-2506. doi: 10.1161/STROKEAHA.119.026005 [DOI] [PubMed] [Google Scholar]
- 25.Simera I, Moher D, Hoey J, Schulz KF, Altman DG. A catalogue of reporting guidelines for health research. Eur J Clin Invest. 2010;40(1):35-53. doi: 10.1111/j.1365-2362.2009.02234.x [DOI] [PubMed] [Google Scholar]
- 26.Pexman JH, Barber PA, Hill MD, et al. Use of the Alberta Stroke Program Early CT Score (ASPECTS) for assessing CT scans in patients with acute stroke. AJNR Am J Neuroradiol. 2001;22(8):1534-1542. [PMC free article] [PubMed] [Google Scholar]
- 27.Hacke W, Kaste M, Fieschi C, et al. ; Second European-Australasian Acute Stroke Study Investigators . Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Lancet. 1998;352(9136):1245-1251. doi: 10.1016/S0140-6736(98)08020-9 [DOI] [PubMed] [Google Scholar]
- 28.Yang P, Zhang Y, Zhang L, et al. ; DIRECT-MT Investigators . Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med. 2020;382(21):1981-1993. doi: 10.1056/NEJMoa2001123 [DOI] [PubMed] [Google Scholar]
- 29.LeCouffe NE, Kappelhof M, Treurniet KM, et al. ; MR CLEAN–NO IV Investigators . A randomized trial of intravenous alteplase before endovascular treatment for stroke. N Engl J Med. 2021;385(20):1833-1844. doi: 10.1056/NEJMoa2107727 [DOI] [PubMed] [Google Scholar]
- 30.Zi W, Qiu Z, Li F, et al. ; DEVT Trial Investigators . Effect of endovascular treatment alone vs intravenous alteplase plus endovascular treatment on functional independence in patients with acute ischemic stroke: the DEVT randomized clinical trial. JAMA. 2021;325(3):234-243. doi: 10.1001/jama.2020.23523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Webb M, Essibayi M, Al Kasab S, et al. O-061 Predictors of failed mechanical thrombectomy for large vessel occlusion: insights from the Stroke Thrombectomy and Aneurysm Registry (STAR). J Neurointerv Surg. 2022;14(suppl 1):A39-A40. doi: 10.1136/neurintsurg-2022-SNIS.61 [DOI] [Google Scholar]
- 32.Mujanovic A, Jungi N, Kurmann CC, et al. Importance of delayed reperfusions in patients with incomplete thrombectomy. Stroke. 2022;53(11):3350-3358. doi: 10.1161/STROKEAHA.122.040063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaesmacher J, Abdullayev N, Maamari B, et al. Safety and angiographic efficacy of intra-arterial fibrinolytics as adjunct to mechanical thrombectomy: results from the INFINITY Registry. J Stroke. 2021;23(1):91-102. doi: 10.5853/jos.2020.01788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kaesmacher J, Bellwald S, Dobrocky T, et al. Safety and efficacy of intra-arterial urokinase after failed, unsuccessful, or incomplete mechanical thrombectomy in anterior circulation large-vessel occlusion stroke. JAMA Neurol. 2020;77(3):318-326. doi: 10.1001/jamaneurol.2019.4192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Renú A, Millán M, San Román L, et al. ; CHOICE Investigators . Effect of intra-arterial alteplase vs placebo following successful thrombectomy on functional outcomes in patients with large vessel occlusion acute ischemic stroke: the CHOICE randomized clinical trial. JAMA. 2022;327(9):826-835. doi: 10.1001/jama.2022.1645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Desilles JP, Loyau S, Syvannarath V, et al. Alteplase reduces downstream microvascular thrombosis and improves the benefit of large artery recanalization in stroke. Stroke. 2015;46(11):3241-3248. doi: 10.1161/STROKEAHA.115.010721 [DOI] [PubMed] [Google Scholar]
- 37.Leng X, Lan L, Liu L, Leung TW, Wong KS. Good collateral circulation predicts favorable outcomes in intravenous thrombolysis: a systematic review and meta-analysis. Eur J Neurol. 2016;23(12):1738-1749. doi: 10.1111/ene.13111 [DOI] [PubMed] [Google Scholar]
- 38.Faizy TD, Mlynash M, Marks MP, et al. Intravenous tPA (tissue-type plasminogen activator) correlates with favorable venous outflow profiles in acute ischemic stroke. Stroke. 2022;53(10):3145-3152. doi: 10.1161/STROKEAHA.122.038560 [DOI] [PubMed] [Google Scholar]
- 39.Campbell BCV, Kappelhof M, Fischer U. Role of intravenous thrombolytics prior to endovascular thrombectomy. Stroke. 2022;53(6):2085-2092. doi: 10.1161/STROKEAHA.122.036929 [DOI] [PubMed] [Google Scholar]
- 40.Suzuki K, Matsumaru Y, Takeuchi M, et al. ; SKIP Study Investigators . Effect of mechanical thrombectomy without vs with intravenous thrombolysis on functional outcome among patients with acute ischemic stroke: the SKIP randomized clinical trial. JAMA. 2021;325(3):244-253. doi: 10.1001/jama.2020.23522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wardlaw JM, Murray V, Berge E, del Zoppo GJ. Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev. 2014;2014(7):CD000213. doi: 10.1002/14651858.CD000213.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Abstracts LB. Late breaking abstracts. Eur Stroke J. 2021;6(1)(suppl):514-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hacke W, Kaste M, Bluhmki E, et al. ; ECASS Investigators . Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317-1329. doi: 10.1056/NEJMoa0804656 [DOI] [PubMed] [Google Scholar]
- 44.Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35-41. doi: 10.1161/01.STR.24.1.35 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Propensity Score Matching
eFigure 1. Flowchart of Patient Inclusion and Exclusion Criteria
eFigure 2. Propensity Score Matching
eFigure 3. Subgroup Analyses for Independent Ambulation
eTable 1. Functional Outcomes and Safety Measures Before Propensity Score Matching
eTable 2. Multivariable Logistic Regression Models
eTable 3. Multivariable Ordinal Logistic Regression Model
Nonauthor Collaborators. German Stroke Registry–Endovascular Treatment Investigators
Data Sharing Statement