Abstract
BACKGROUND:
Sociolegal barriers to cancer care are defined as health-related social needs like affordable healthy housing, stable utility service, and food security that may be remedied by public policy, law, regulation, or programming. Legal support has not been studied in cancer care.
METHODS:
The authors conducted a randomized controlled trial of patients who had newly diagnosed cancer at a safety-net medical center in Boston from 2014 through 2017, comparing standard patient navigation versus enhanced navigation partnered with legal advocates to identify and address sociolegal barriers. English-speaking, Spanish-speaking, or Haitian Creole-speaking patients with breast and lung cancer were eligible within 30 days of diagnosis. The primary outcome was timely treatment within 90 days of diagnosis. Secondary outcomes included patient-reported outcomes (distress, cancer-related needs, and satisfaction with navigation) at baseline and at 6 months.
RESULTS:
In total, 201 patients with breast cancer and 19 with lung cancer enrolled (response rate, 78%). The mean patient age was 55 years, 51% of patients were Black and 22% were Hispanic, 20% spoke Spanish and 8% spoke Haitian Creole, 73% had public health insurance, 77% reported 1 or more perceived sociolegal barrier, and the most common were barriers to housing and employment. Ninety-six percent of participants with breast cancer and 73% of those with lung cancer initiated treatment within 90 days. No significant effect of enhanced navigation was observed on the receipt of timely treatment among participants with breast cancer (odds ratio, 0.88; 95% CI, 0.17-4.52) or among those with lung cancer (odds ratio, 4.00; 95% CI, 0.35-45.4). No differences in patient-reported outcomes were observed between treatment groups.
CONCLUSIONS:
Navigation enhanced by access to legal consultation and support had no impact on timely treatment, patient distress, or patient needs. Although most patients reported sociolegal barriers, few required intensive legal services that could not be addressed by navigators.
Keywords: breast cancer, cancer disparities, comparative effectiveness, health equity, lung cancer, patient navigation
LAY SUMMARY:
In patients with cancer, the experience of sociolegal barriers to care, such as unstable housing, utility services, or food insecurity, is discussed. Addressing these barriers through legal information and assistance may improve care.
This study compares standard patient navigation versus enhanced navigation partnered with legal advocates for patients with breast and lung cancers. Almost all patients in both navigation groups received timely care and also reported the same levels of distress, needs, and satisfaction with navigation.
Although 75% of patients in the study had at least 1 sociolegal barrier identified, few required legal advocacy beyond what a navigator who received legal information and coaching could provide.
BACKGROUND
Cancer health disparities are growing despite overall declines in cancer mortality.1 Death rates among people with lower socioeconomic status, as defined by education, occupation, or residence, have shown little or no decrease and even have increased for some.2–4 Any decrease in cancer death rates among people from racial and ethnic minority groups has occurred later and has been slower compared with the rates among people in the majority. It is increasingly recognized that racial differences in health outcomes are intricately related to social environments that are rooted in structural racism.5 Race as a social construct acknowledges the complex interplay of socioeconomic status, culture, and social classification and is the relevant focus for research and remediation. Social determinants of health, the conditions in which people are born, grow, live, work, and age,6 are shaped by the distribution of money, power, and resources and are directly linked to population-level health inequities. Individual-level social needs are the downstream manifestations of the impact of the Social determinants of health on communities.7
Research has clearly documented that health-related social needs8 like unhealthy housing conditions, energy insecurity, food insecurity, and interpersonal violence can operate as barriers to accessing cancer care and can impact outcomes, regardless of race/ethnicity.3,4,9,10 Sociolegal barriers are defined as social problems related to meeting life’s most basic needs that could be addressed by existing public policy, law, regulation, and programming and thus are potentially remedied through legal advocacy/action.11–13 These barriers have a legal dimension to the extent that a remedy exists at law, a patient has sought resources or assistance from an agency/authority and has been denied that support, or the patient is neither aware that they have legal rights nor how to exercise them effectively.14 This range of poorly understood barriers to accessing and engaging with cancer services creates documented delays in care and is increasingly scrutinized as a source of poor survival for many vulnerable populations.15–24
Patient navigation in the cancer care setting refers to individualized assistance offered to patients, families, and caregivers to help overcome health care barriers and facilitate timely access to quality care through all phases of the cancer experience.25–30 There is a body of scientific evidence that patient navigation may improve delays in cancer care across the continuum of care, from screening to diagnosis, treatment, and survivorship, with a recognized paucity of data during breast cancer treatment.31–33 Data from the National Patient Navigation Research Program indicated that patients who had sociolegal barriers were less likely to have timely resolution of diagnostic care compared with those who had other barriers, even when accounting for the presence of multiple barriers.34 This was a stronger predictor of delay in treatment than insurance status or race/ethnicity. These findings are supported by other studies reporting that outcomes are limited by housing, insurance, and financial needs.35–38 Yet no navigation studies to date have systematically targeted sociolegal needs. To address patient-reported sociolegal barriers, we designed Project SUPPORT39 (Sociolegal Services for Underserved Populations Through Patient Navigation to Optimize Resources During Treatment; ClinicalTrials.gov identifier NCT02232074), a comparative-effectiveness study.
METHODS
We used community-engaged research methods to conduct a comparative-effectiveness, randomized controlled trial of racially/ethnically diverse, low-income patients with cancer at the largest safety-net medical center in New England from February 2013 through August 2017. Project SUPPORT compared standard-of-care navigation versus an enhanced navigation intervention supported by legal advocacy on clinical and patient-reported outcomes (PROs). The Boston University Medical Center Institutional Review Board approved this study.
Study Setting and Patients
Patients with cancer who were seeking care at Boston Medical Center were eligible if they had a newly diagnosed breast cancer or nonsmall cell lung cancer during the study period and spoke English, Spanish, or Haitian Creole. Exclusion criteria included: 1) >30 days elapsed since the cancer diagnosis, 2) a history of cancer in the past 5 years, or 3) cognitive impairment, such as dementia or delirium. On the basis of feedback from both our Patient Advisory Group and our Scientific Advisory Board, the presence of a sociolegal concern was intentionally not included as an eligibility criteria for 2 main reasons: 1) eliminating pre-enrollment screening would reduce burden on patients with cancer who chose not to participate in the study, and 2) including all patients would allow us to include those who might develop a sociolegal concern during the course of their treatment, regardless of baseline status.
Recruitment and Randomization
We identified eligible patients from: 1) weekly tumor board meetings, 2) pathology reports, and 3) oncology schedules. Eligible patients were invited to participate at an office visit by a research assistant fluent in English, Spanish, and Haitian Creole. Those who declined were offered standard-of-care navigation services outside of the study. Enrolled participants were randomly assigned to a study group at the time of informed consent, when the respective navigator met with the patient to initiate navigation services. Navigators were randomly assigned to serve as standard or enhanced navigators for the duration of the study and underwent project-specific training, including procedures for randomization and assignment to navigation as well as duration and documentation of navigation services. We targeted a total enrollment sample of 260 patients with breast and lung cancer to address our objectives. With 130 patients randomized to each of the 2 study groups, we had >80% power to detect an advantage to navigation enhanced by a medical-legal partnership if the enhanced intervention raised the percentage receiving timely initiation of care from 70% to 86% (testing at the 2-tailed .05 level).
Comparators: Standard Navigation Versus Enhanced Navigation
Standard-of-care navigation
Standard-of-care patient navigation is defined by several key activities that the literature suggests are necessary for effective navigation26,40: 1) case identification, 2) barrier identification, 3) care plans to address identified barriers, and 4) long-term tracking. This protocol was informed by prior participation in clinical navigation trials40,41 and was established for >10 years at the study site. Nonclinical or lay navigators perform these activities after a cancer diagnosis with oversight from a supervisor (who provides support around the patients’ recommended treatment plans) and an oncology social worker (who provides onsite clinical counseling support). Through locally designed protocols, navigators complete online navigation certification42 along with a 3-month, onsite, mentored training program before they act independently as part of the cancer care team. Navigators work directly with oncology providers to identify newly diagnosed patients who are most at risk for delays in care, identify their individual barriers to care, and use local resources to address them throughout their cancer treatment. At a minimum, they are expected to have at least 2 encounters with the patient during their cancer treatment.
Enhanced navigation with legal advocacy
Standard-of-care navigation was enhanced through partnership with Medical-Legal Partnership | Boston (MLPB) legal advocates. Enhanced navigation services were administered by a navigator who completed additional MLPB training focused on problem-solving in 3 sociolegal domains (housing instability, employment insecurity, and disability benefits). Didactic trainings included an overview of legal-rights fundamentals, which were reinforced in ongoing booster trainings and through one-on-one educational consultation with the lawyer during standing meetings and as needed by email, telephone, and in person. Legal support services for enhanced participants included 3 activities:
1. Comprehensive sociolegal needs assessment
An assessment tool designed by the MLPB team aided the navigator in capturing detailed patient information regarding perceived legal barriers across 3 domains (housing and utilities, employment, and disability benefits). Through participant interviews, these assessments were administered in person or on the phone and took approximately 30 minutes. These assessments were performed upon enrollment and at 3 months and 6 months after the start of treatment.
2. Longitudinal interdisciplinary care planning by the navigator in consultation with a lawyer
The navigator and legal advocate met regularly to review sociolegal needs assessments to determine whether each patient’s perceived barriers had legal aspects that were amenable to MLPB support. Together, they systematically determined the participant’s level of legal need (LLN),39 ranging from no legal barrier to simple, intermediate, or complex legal needs. The LLN determination guided navigation care plans, which were co-created with the lawyer at weekly standing team meetings and as needed to address time-sensitive developments.
3. Referral to direct legal support
A small subset of cases required direct legal assistance because of the acuity and/or complexity of the patients’ needs. In those cases, the lawyer facilitated safe hand-offs to free legal assistance curated by MLPB.
Data Collection and Sources
Clinical outcomes
The Clinical Data Warehouse is a comprehensive database that consolidates data from multiple hospital systems, allowing for the automatic capture of sociodemographic and clinical variables. Data elements for complex cancer treatment variables not suited for automated reporting were manually abstracted from the electronic medical record. A clinical adjudication team reviewed and confirmed key clinical data elements. Clinical outcomes included the following:
Timely initiation of cancer treatment (yes/no) was defined based on whether treatment was initiated within 90 days of diagnosis (96%).41 Timely care was calculated as the number of days from diagnosis (time 0) to treatment initiation (time 1). The date chosen for the time 1 variable depended on the recommended care plan for each patient (ie, initiation of surgery, chemotherapy, radiation, or hormonal therapy) as derived from the chart abstraction and based on patient presentation, including but not limited to stage at diagnosis and comorbid medical conditions.
Quality of cancer care was assessed using 3 measures of quality cancer treatment for participants with breast cancer, as defined by the National Quality Forum (NQF)43: 1) (NQF-endorsed measure 219) radiation therapy is administered within 1 year of diagnosis for women younger than 70 years who are undergoing breast-conserving surgery for breast cancer, 2) (NQF-endorsed measure 0559) combination chemotherapy is recommended or administered within 4 months of diagnosis for women younger than 70 years with either American Joint Committee on Cancer T1cN0M0 or stage IB through stage III hormone receptor-negative breast cancer, and 3) (NQF-endorsed measure 0220) tamoxifen or a third-generation aromatase inhibitor is recommended or administered within 1 year (365 days) of diagnosis for women with either American Joint Committee on Cancer T1cN0M0 or stage IB through stage III hormone receptor-positive breast cancer.
PROs were captured using research assistant-administered survey instruments collected at the time of enrollment (baseline) and at 3 and 6 months in the language preferred by the participant. Participants had the option of completing surveys in person or over the phone. PROs included the following:
The Distress Thermometer44 is a validated measure of global distress. This single-item instrument uses a value for individuals to rate distress levels during the past week, ranging from 0 (none) to 10 (extreme distress).
A modified version of the Cancer Needs Distress Inventory (CaNDI)45 survey captures perceived barriers in the past 2 weeks with 38 items across 7 domains (anxiety, depression, emotional, social, health care, practical, and physical) on a scale from 1 (not a problem) to 5 (very severe problem).45
A 25-item sociolegal survey11 identified participant perceived barriers across 5 I-HELP categories (income support, housing/utilities, education/employment, legal status/immigration, and personal/family safety).46 Navigators were blinded to these survey results at each time point. (Note that, for enhanced navigation participants only, we also captured the LLN,39 ranging from no legal barrier to simple, intermediate or complex legal needs. As part of the enhanced navigation, the LLN form included detailed information on the level and type of legal needs as determined by the legal advocate in collaboration with the navigator.)
The Patient Satisfaction With Interpersonal Relationship With Navigator Survey is a 9-item measure that produces a composite score to assess satisfaction with aspects of navigation care.47 By using a 5-point Likert scale to assess satisfaction, this survey instrument was administered only at the 6-month follow-up interview.
Statistical Analyses
The analytic cohort included only those participants who reported perceived sociolegal barriers on their baseline survey (72% of those enrolled, n = 220; 113 enhanced navigation participants and 107 standard navigation participants). Because of the limited sample size of participants with lung cancer (n = 19), the breast and lung cohorts were analyzed separately. Demographic variables were summarized for the total study cohort and by treatment group using univariate statistics.
Our clinical analysis used simple and multiple logistic regression models to compare the proportion of patients who received timely initiation of treatment and quality treatment across study groups. The simple logistic regression models focused only on the association between treatment group and the dichotomous outcome, and the multivariable models were further adjusted for age, race/ethnicity, insurance status, health literacy, and stage of disease. For the 3 quality-of-care metrics, we first identified the subset of participants eligible for each respective quality standard and then conducted simple logistic regression models to compare the proportion of patients who received quality care across the study groups.
For PROs, simple linear regression models and multivariable linear regression models tested whether there was an association between the navigation groups with each PRO at the primary end point (6 months). Simple linear regression models were adjusted by baseline PRO values, and multivariate models also included patient’s age, race, insurance, and health literacy.
RESULTS
Figure 1 displays the details of our recruitment, enrollment, and analytic sample numbers. In total, 894 patients with cancer were assessed for study eligibility and, ultimately, 393 patients were deemed eligible. The most common reasons for ineligibility included: history of cancer within the past 5 years (n = 148), had received initial cancer treatment (n = 136), and date of diagnosis >30 days (n = 119). Among these 393 eligible patients, in total, 306 volunteered to participate in Project SUPPORT, were consented, and were randomly allocated to 1 of the 2 treatment groups, resulting in an overall response rate of 78%. Figure 1 also shows that, in follow-up, 16 participants withdrew consent during the course of the study, so their data were not included in the final analytic cohort, which included only those who reported perceived sociolegal barriers on their baseline survey (72% of those enrolled: n = 220 for clinical outcomes, including 113 in the enhanced navigation group and 107 in the standard navigation group; and n = 216 for PROs, including 112 in the enhanced navigation group and 104 in the standard navigation group).
Figure 1.
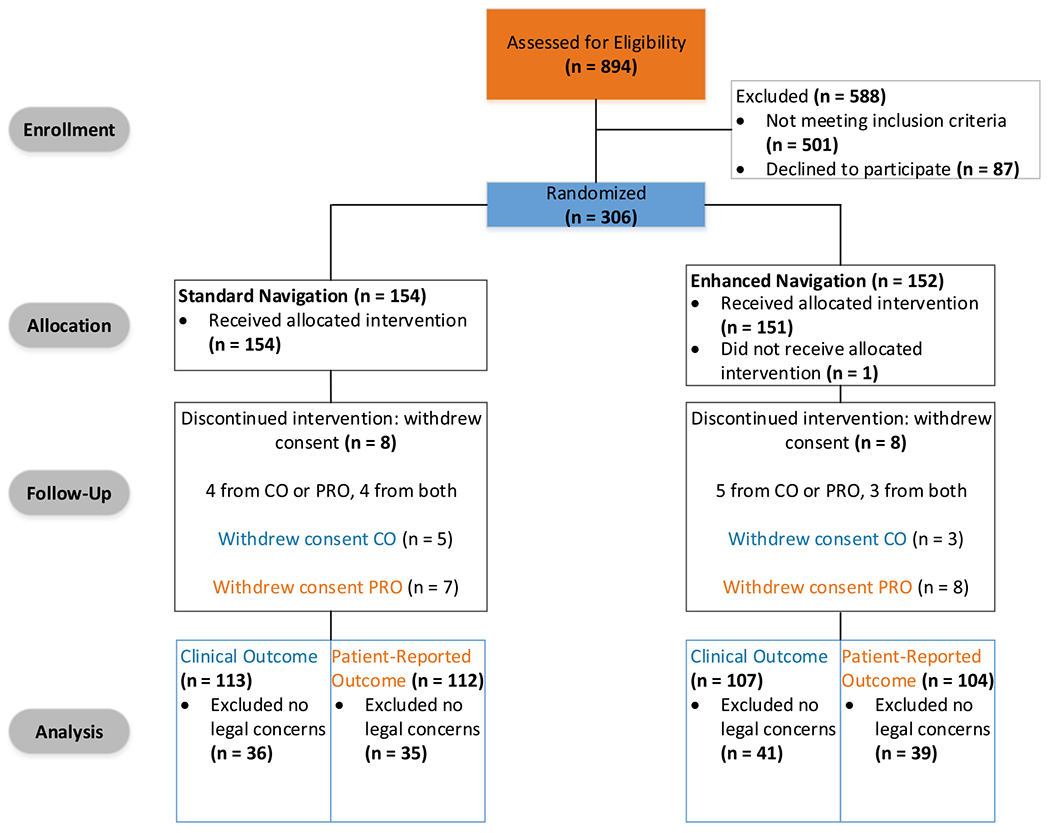
This is a Consolidated Standards of Reporting Trials (CONSORT) diagram of total sample recruitment and enrollment for the Project SUPPORT comparative-effectiveness study (ClinicalTrials.gov identifier NCT02232074). CO indicates clinical outcome; PRO, patient-reported outcome.
Table 1 shows that the mean age of study participants was 55.1 years, most were female, three-quarters were non-White, one-third identified a language other than English as their preferred spoken language, three-quarters had only a public form of health insurance, and the majority had marginal or inadequate health literacy, as measured by the Brief Health Literacy Screen.48 The median number of perceived sociolegal barriers reported at baseline was 2.0. Eighty percent of participants had either stage 0, I, or II cancer at diagnosis. No differences in any of these participant characteristics were observed between the navigation groups.
TABLE 1.
Baseline Demographics for Project SUPPORT Participants by Randomization Group: Clinical Outcomes Cohort, n = 220
| No. of Participants (%) |
|||
|---|---|---|---|
| Variable | Standard Navigation, n = 107 | Enhanced Navigation, n = 113 | Total, n = 220 |
| Cancer type | |||
| Breast cancer | 96 (89.7) | 105 (92.9) | 201 (91.4) |
| Lung cancer | 11 (10.3) | 8 (7.1) | 19 (8.6) |
| Age, y | |||
| Mean ± SD | 54.7 ± 11.8 | 55.6 ± 11.0 | 55.1 ± 11.4 |
| Sex | |||
| Female | 102 (95.3) | 109 (96.5) | 211 (95.9) |
| Male | 5 (4.7) | 4 (3.5) | 9 (4.1) |
| Race/ethnicity | |||
| White | 27 (25.2) | 26 (23.0) | 53 (24.1) |
| Hispanic | 26 (24.3) | 22 (19.5) | 48 (21.8) |
| Black | 51 (47.7) | 60 (53.1) | 111 (50.5) |
| Other | 3 (2.8) | 5 (4.4) | 8 (3.6) |
| Language | |||
| English | 71 (66.4) | 87 (77.0) | 158 (71.8) |
| Spanish | 27 (25.2) | 17 (15.0) | 44 (20.0) |
| Haitian/Creole | 9 (8.4) | 9 (8.0) | 18 (8.2) |
| Insurance | |||
| Public | 79 (73.8) | 83 (73.5) | 162 (73.6) |
| Private | 28 (26.2) | 30 (26.5) | 58 (26.4) |
| Health literacy | |||
| Inadequate | 31 (29.0) | 28 (25.0) | 59 (26.9) |
| Marginal | 38 (35.5) | 37 (33.0) | 75 (34.2) |
| Adequate | 38 (35.5) | 47 (42.0) | 85 (38.8) |
| Sociolegal concerns | |||
| Mean ± SD | 1.8 ± 0.9 | 1.8 ± 0.8 | 1.8 ± 0.9 |
| Median [IQR] | 2.0 [1.0-2.0] | 2.0 [1.0-2.0] | 2.0 [1.0-2.0] |
| Min-Max | 1.0-4.0 | 1.0-4.0 | 1.0-4.0 |
| AJCC clinical cancer stage | |||
| 0 | 21 (19.6) | 21 (18.6) | 42 (19.1) |
| I | 42 (39.3) | 39 (34.5) | 81 (36.8) |
| II | 24 (22.4) | 25 (22.1) | 49 (22.3) |
| III | 4 (3.7) | 5 (4.4) | 9 (4.1) |
| III | 12 (11.2) | 10 (8.8) | 22 (10.0) |
| Missing | 4 (3.7) | 13 (11.5) | 17 (7.7) |
Abbreviations: AJCC, American Joint Committee on Cancer; IQR, interquartile range; Max, maximum; Min, minimum; Project SUPPORT, Sociolegal Services for Underserved Populations Through Patient Navigation to Optimize Resources During Treatment (ClinicalTrials.gov identifier NCT02232074).
Table 2 displays the distribution of initiation of cancer treatment at 30, 60, and 90 days for both participants with breast cancer and those with lung cancer. Because timely care was defined as the initiation of care within 90 days, 96% of all participants with breast cancer achieved timely care regardless of study group. Among the participants with lung cancer, 14 (74%) achieved timely care, and 88% of enhanced navigation participants achieved timely care compared with 63% of standard navigation participants. In adjusted analyses for participants with breast cancer (Table 3), the odds of receiving timely care were actually lower for enhanced navigation participants compared with standard navigation participants, but this finding was not statistically significant (odds ratio, 0.88; 95% CI, 0.17-4.52). There were too few patients with lung cancer to conduct a multivariate logistic regression model (n = 19). The unadjusted odds ratio for lung patients was 4.0 with a very wide confidence interval (95% CI, 0.35-45.4).
TABLE 2.
Number of Participants Receiving First Treatment at 30, 60, and 90 Days by Type of Cancer and Randomization Group
| No. of Participants (%) |
|||
|---|---|---|---|
| Cancer Type | By 30 Days | By 60 Days | By 90 Daysa |
| Breast cancerb | |||
| Overall, n = 194 | 56 (28.9) | 150 (77.3) | 186 (95.9) |
| Standard navigation group, n = 96 | 24 (25.0) | 73 (76.0) | 92 (95.8) |
| Enhanced navigation group, n = 105 | 32 (32.6) | 77 (78.5) | 94 (95.9) |
| Lung cancer | |||
| Overall, n = 19 | 3 (15.8) | 13 (68.4) | 14 (73.7) |
| Standard navigation group, n = 11 | 1 (9.0) | 6 (54.4) | 7 (63.4) |
| Enhanced navigation group, n = 8 | 2 (25.0) | 7 (87.5) | 7 (87.5) |
The primary outcome was receipt of first treatment for cancer by 90 days.
Note that 7 participants with breast cancer were missing data on the time of their first treatment (5 were transferred, and 2 were lost to follow-up).
TABLE 3.
Timely Treatment–Receipt of First Cancer Treatment Within 90 Days of Diagnosis: Logistic Regression, n = 220a
| Type of Cancer | OR (95% CI) |
|---|---|
| Breast cancer, n = 194 | |
| Navigation group | 1.02 (0.25-4.21) |
| Navigation group, adjustedb | 0.88 (0.17-4.52) |
| Lung cancer, n = 19 | |
| Navigation group | 4.00 (0.35-45.4) |
Abbreviations: CI, confidence interval; OR, odds ratio.
The primary outcome was first treatment for cancer occurring within 90 days of diagnosis.
The analysis was adjusted for race, age, insurance status, stage, and health literacy.
Table 4 displays the unadjusted odd ratios of receiving quality treatment by subgroup (radiation, chemotherapy, hormone therapy). No differences were observed between the navigation groups.
TABLE 4.
Receipt of Quality Breast Cancer Care: Unadjusted Odds
| Subgroup | OR (95% CL)a | P |
|---|---|---|
| Radiation therapy within 365 d, N = 123 | 0.85 (0.28-2.79) | .79 |
| Hormone therapy within 365 d, N = 67 | 0.45 (0.13-1.43) | .17 |
| Chemotherapy within 120 d, N = 18 | 0.78 (0.10-6.32) | .81 |
Abbreviations: CL, confidence limits; OR, odd ratio.
The OR was for treatment on the intervention arm versus the control arm.
Table 5 displays univariate results for the PROs. At baseline, the median distress score for all participants was 6.0 (range, 3.00-8.50), it was unchanged at 3 months (6.0; range, 4.00-8.00), and it decreased to 5.00 (range, 2.00-7.00) at 6 months. Overall, participants with breast cancer reported higher distress than participants with lung cancer. Scores went down at 6 months for both groups. Psychosocial needs were measured using the CaNDI survey across each of the 7 domains (anxiety, depression, emotional, social, health care, practical, and physical) on a scale from 1 (not a problem) to 5 (very severe problem), with an overall score consisting of the averaged score. A high overall score represents higher needs. Because the results did not differ across domains, only the total modified CaNDI scores are presented. At baseline, the median total modified CaNDI score for all participants was 1.70 (range, 1.40-2.20) and, at 6 months, it was 1.50 (range, 1.20-2.00). Overall, participants with breast cancer reported slightly higher needs than those with lung cancer at both time points. The median score for satisfaction with navigator at 6 months was 44.0 (range, 36.0-45.0), and no differences were observed between participants who had breast cancer and those who had lung cancer. The multivariable linear regression models (data not shown) did not find any statistically significant associations between treatment group or any of the PROs at 6 months (P values ranged from .14 to .96). These results were consistent for both breast cancer and lung cancer.
TABLE 5.
Univariate Results for Patient-Centered Outcomes at Baseline and Follow-Up at 6 Months by Cancer Type and Randomization Group
| Breast Cancer, n = 197 |
Lung Cancer, n = 19 |
||||
|---|---|---|---|---|---|
| Variable | Standard Navigation, n = 93 | Enhanced Navigation, n = 104 | Standard Navigation, n = 11 | Enhanced Navigation, n = 8 | Overall, n = 216 |
| Distress Thermometer score at baseline | |||||
| No. | 93 | 104 | 11 | 8 | 216 |
| Mean ± SD | 6.10 ± 3.00 | 6.00 ± 3.30 | 4.50 ± 3.30 | 3.50 ± 3.50 | 5.90 ± 3.20 |
| Median (p25, p75) | 6.00 (4.00, 9.00) | 7.00 (3.50, 8.50) | 4.00 (2.00, 8.00) | 3.50 (0.00, 5.50) | 6.00 (3.00, 8.50) |
| Min-Max | 0.00-10.00 | 0.00-10.00 | 0.00-10.00 | 0.00-10.00 | 0.00-10.00 |
| Distress Thermometer score at 6 mo | |||||
| No. | 85 | 91 | 7 | 6 | 189 |
| Mean ± SD | 5.20 ± 3.00 | 4.50 ± 3.30 | 4.00 ± 2.60 | 1.50 ± 1.90 | 4.70 ± 3.10 |
| Median (p25, p75) | 5.00 (3.00, 8.00) | 5.00 (2.00, 7.00) | 3.00 (2.00, 6.00) | 1.00 (0.00, 2.00) | 5.00 (2.00, 7.00) |
| Min-Max | 0.00-10.00 | 0.00-10.00 | 2.00-9.00 | 0.00-5.00 | 0.00-10.00 |
| CaNDI mean total score, sum at baseline | |||||
| No. | 93 | 103 | 11 | 8 | 215 |
| Mean ± SD | 1.90 ± 0.60 | 1.90 ± 0.70 | 1.50 ± 0.40 | 1.80 ± 0.70 | 1.90 ± 0.70 |
| Median (p25, p75) | 1.80 (1.50, 2.10) | 1.70 (1.30, 2.40) | 1.40 (1.30, 1.60) | 1.40 (1.30, 2.20) | 1.70 (1.40, 2.20) |
| Min-Max | 1.10-4.10 | 1.00-4.10 | 1.10-2.50 | 1.20-3.10 | 1.00-4.10 |
| CaNDI mean total score, sum at 6 mo | |||||
| No. | 85 | 91 | 7 | 6 | 189 |
| Mean ± SD | 1.70 ± 0.60 | 1.70 ± 0.70 | 1.50 ± 0.50 | 1.40 ± 0.40 | 1.70 ± 0.60 |
| Median (p25, p75) | 1.60 (1.20, 2.00) | 1.40 (1.20, 2.10) | 1.30 (1.20, 1.90) | 1.30 (1.10, 1.60) | 1.50 (1.20, 2.00) |
| Min-Max | 1.00-3.80 | 1.00-4.10 | 1.10-2.30 | 1.00-2.00 | 1.00-4.10 |
| Patient satisfaction/experience total score at 6 mo | |||||
| No. | 52 | 52 | 3 | 4 | 111 |
| Mean ± SD | 39.7 ± 7.00 | 40.4 ± 7.44 | 39.0 ± 2.65 | 40.3 ± 4.43 | 40.0 ± 7.06 |
| Median (p25, p75) | 43.0 (36.0, 45.0) | 45.0 (36.0, 45.0) | 40.0 (36.0, 41.0) | 40.0 (36.5, 44.0) | 44.0 (36.0, 45.0) |
| Min-Max | 9.0-45.0 | 9.0-45.0 | 36.0-41.0 | 36.0-45.0 | 9.0-45.0 |
Abbreviations: CaNDI, Cancer Needs Distress Inventory, Max, maximum; Min, minimum; p25, 25th percentile; p75, 75th percentile.
Perceived sociolegal barriers reported by treatment group at baseline and at 6 months are displayed in Figure 2. Perceived housing and employment barriers were most common. Compared with participants who had lung cancer, those who had breast cancer reported more perceived barriers across each domain. For each type of concern, there was a decrease in reported perceived barriers at 6 months, with the exception of perceived disability barriers for participants with breast cancer and housing for those with lung cancer. Among enhanced navigation participants, we found that 75% had a confirmed legal need based on the LLN assessment (Table 6). Most legal needs (59.6%) were considered level 1 (eg, imparting a discreet piece of legal information, such as eligibility to apply for a benefit like unemployment insurance and a next step to do so effectively), 27.7% were considered level 2 (eg, developing a verification letter to aid in effectively asserting medical or caregiver leave rights or Americans with Disability Act reasonable accommodation rights), and only 7.4% were considered level 3, requiring legal representation (eg, eviction defense representation in housing court). Five percent of participants had a legal need outside the scope of study’s capacity during the study period (eg, estate planning, criminal legal system involvement, immigration, and family law). The most common legal needs were related to housing, followed by income supports, and then employment.
Figure 2.
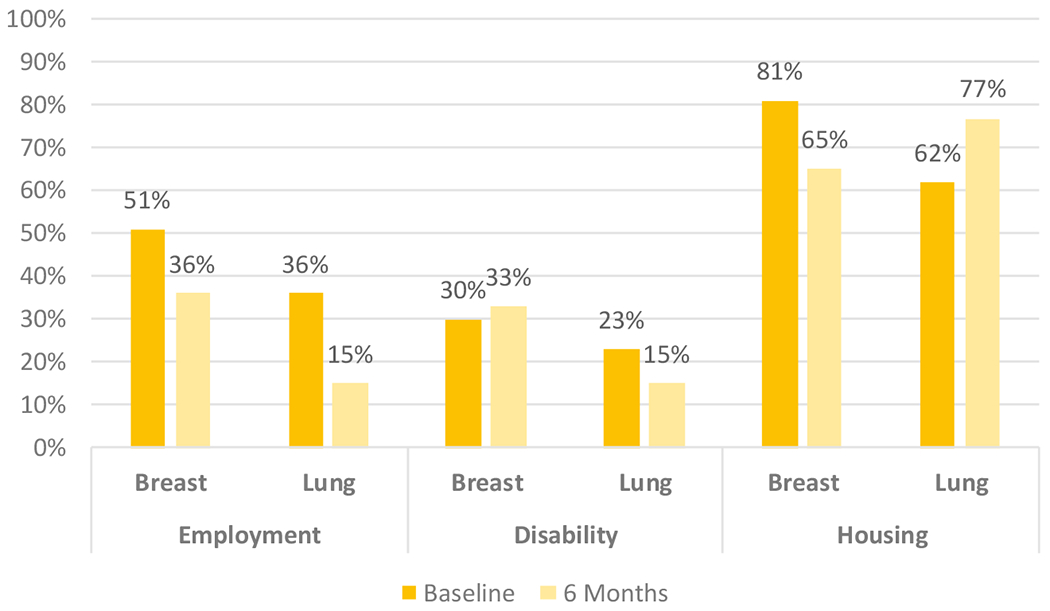
The percentages of patients who had perceived sociolegal barriers at baseline and at 6 months are illustrated by cancer type.
TABLE 6.
| No. of Participants (%) |
|||
|---|---|---|---|
| Baseline Legal Need | Breast Cancer | Lung Cancer | Overall |
| Total no. enrolled | 105 | 8 | 113 |
| Assessment not completed | 8 | 2 | 10 |
| No legal need | 24 (25) | 2 (33.3) | 26 (25) |
| Legal need | 73 (75) | 4 (66.7) | 77 (75) |
| Level 1 need | 44 (60.3) | 1 (25.0) | 45 (59.6) |
| Level 2 need | 19 (26.0) | 2 (50.0) | 21 (27.7) |
| Level 3 need | 7 (9.6) | 0 (0.0) | 7 (7.4) |
| Level 9 need | 3 (4.1) | 1 (25.0) | 4 (5.3) |
Of 113 participants who answered I-HELP (income support, housing/utilities, education/employment, legal status/immigration, and personal/family safety) questions and had concerns at baseline, 10 did not complete the I-HELP survey.
The highest level of legal need noted was for each participant with the exceptions of level 9. If participants had ANY level of need other than 9 (levels 1-3) AND had level 9 need, their highest levels were coded as levels 1 through 3. Level 9 included participants with only level 9 need.
DISCUSSION
This is the first known study to explore the impact of partnering hospital-based patient navigators with legal advocates from a local medical-legal partnership program to target sociolegal barriers among patients with cancer. We found that, compared with standard-of-care navigation, navigation enhanced by legal support did not result in more timely care or improvement in patients’ reported distress, psychosocial needs, or satisfaction with navigation services over a 6-month period. Rather, we found that all participants had high rates of timely care and similar distress, needs, and satisfaction. Overall, we found fewer acute sociolegal needs than anticipated. Although 75% of patients in the enhanced navigation group had at least 1 sociolegal barrier identified, few required legal advocacy beyond what standard navigation could offer.
This comparative-effectiveness study adds needed scientific evidence to support oncology navigation services within our health care delivery system during cancer treatment. In November 2017, the National Cancer Policy Forum of the National Academies of Sciences, Engineering, and Medicine convened a workshop entitled Establishing Effective Navigation Programs in Oncology,49 which highlighted the many models of community-based and hospital-based oncology navigation that exist to address the complexity of care delivery across the continuum of cancer care. A major conclusion from that workshop was a call for more scientific evidence in the cancer treatment phase as well as studies that measure PROs, like Project SUPPORT, to make the case for hospital administrators and policy makers to prioritize resource allocation for these vital oncology services. Our study design did not include a no-navigation arm, so it is impossible to conclude that standard-of-care navigation affected timely care, yet these findings among a population with historic documentation of delays in care is encouraging.50,51
The null findings we observed make sense upon analysis of the data: our a priori study design assumptions—low rates of timely treatment and high rates of acute sociolegal barriers—were not observed in our participants. More specifically, we observed that 96% of all participants with breast cancer achieved timely care (defined as the initiation of treatment within 90 days of cancer diagnosis); this is higher than preliminary data from our prior study, which suggested that roughly 70% of navigated patients received timely initiation of care.52 The navigation literature uses various definitions of timely cancer treatment, ranging from 30, to 60, to 90 days from diagnosis, and reports rates ranging from 55% to 78% in the absence of navigation among similar patients from under-resourced populations.53–57 In terms of the prevalence of sociolegal barriers to care, we observed the expected amount of reported sociolegal concerns (75%) based on our prior study in this population.11 Yet the LLN data demonstrated that the acuity and severity of these needs were lower than expected, reducing the potential impact of the legal advocacy provided in the enhanced navigation arm of the study.
There are several factors that may explain why we observed these outcomes. First is the potential for temporal trends in standard-of-care navigation that have evolved since study inception to contribute to the high rates of timely care observed.58,59 Most notably, under the 2015 Commission on Cancer Standard 3.1: Patient Navigation, cancer program facilities (including Boston Medical Center) are required to demonstrate that they have a navigation process in place that aims to remove barriers to cancer care. In addition, as health care delivery systems in our country have evolved toward greater accountability and value over volume and have focused on care coordination, evidence for better cancer outcomes and quality is starting to accrue.60 Similarly, there is increasing recognition of the importance of identifying health-related social needs as a modifiable barrier to quality care.61 Safety-net health care delivery systems are increasingly focusing resources on identifying and addressing social barriers to care, such that more health care teams are being trained to identify, document, and address social barriers. For example, Change Healthcare (https://www.changehealthcare.com/) was introduced to our study site as a new resource for navigators during the study period. This made direct and in-person assistance with disability benefits advocacy universally available to our study participants through standard navigation.
Second, our study design slightly altered conventional standard-of-care navigation and introduced the potential for contamination of standard navigation participants. The Project SUPPORT study protocol required patients to be randomly allocated as close to their date of diagnosis as possible. Therefore, enrolled participants were approached by the research team much sooner after their diagnosis than usual-care navigation, which relies on referral from an oncology provider and, more often than not, only after an identified delay in care. Consequently, study protocols resulted in both navigation groups being assigned a navigator much earlier than usual care, which likely influenced timely care. In addition, the navigators worked together, often in the same space, attended the same meetings, and had the same supervisor. Although the enhanced navigators had special training and one-on-one support with MLPB’s lawyer, there was no way to completely isolate exposure to the expertise and resources available to the standard-of-care navigators.
Third, our randomized controlled trial study design required voluntary recruitment of eligible patients at the time of their cancer diagnosis. This scientifically sound approach may have compromised our ability to include those patients with cancer who were most at risk for delays in care and thus in need of navigation services. For example, 119 patients (81 with breast cancer and 31 with lung cancer) were deemed ineligible for Project SUPPORT because it had been >30 days since their cancer diagnosis (given that our main outcome was timely care); and, although we had a high response rate, those who declined to participate (n = 87) may well have been at risk for delays in care and most likely to benefit. Compared with patients who enrolled in Project SUPPORT, those who were ineligible and declined to participate were slightly older, >20% identified their race/ethnicity as other, and >20% had a primary spoken language other than English, Spanish, or Haitian Creole. Additional analyses of these hospital data for both the ineligible and declined patients indicated that this group had a timely treatment rate of only 85% (data not published), which was much lower than that observed in the Project SUPPORT participants. These findings strongly suggest the need for multisite, pragmatic study designs to ensure that patients at the highest risk for care delays are included in navigation studies that seek to define best practices in real-life settings.
Our finding that >75% of patients seeking care at an urban safety-net hospital reported 1 or more perceived sociolegal barriers at the time of a new cancer diagnosis is an important message for our health care delivery systems seeking to provide value-based care. Notably, the most pressing perceived barriers are those with the least available resources to address them, namely, housing instability. It is important to note that, despite these high levels of concern, the detailed screening conducted among the enhanced navigation participants to assess LLN found that 25% of those perceived barriers did not constitute a sociolegal barrier to care; and, when present, the majority of sociolegal barriers to care were level 1 (basic legal issue), requiring only a single interaction between legal advocates and navigators, legal information that was then transmitted to the participant with no additional follow-up. This suggests that well trained navigators may be able to support most patients’ needs.
Research demonstrating the effects of integrating legal support into patient care—exemplified by the medical-legal partnership approach—is only beginning to emerge,62–66 but much more needs to be known regarding the size of effects.9,12,67,68 Some of the medical-legal partnership evidence base documents improvements in self-reported health, including feeling more empowered after receiving medical-legal partnership services, having reduced stress,67 and an improvement in one’s general health.9 A retrospective study of patients in palliative care found that 297 referrals made to a medical-legal partnership program from 2004 through 2007 addressed patients’ legal needs, from reinstating Food Stamp benefits to executing last wills and testaments.69 A pilot study of a medical-legal partnership targeting pediatric patients found that the proportion of families who accessed food and income support significantly increased, whereas the proportion of families who avoided medical care because of perceived cost and insurance barriers significantly decreased.9 In a pilot study of 20 patients with cancer who received legal services, 75% said that the legal services reduced stress, 45% reported a positive impact on their financial situation, 30% said that the services helped them maintain their treatment regimen, and 25% said that the legal services helped them keep medical appointments.70 Our study contributes to this knowledge by documenting the types and acuity of legal needs among those who received the enhanced legal advocacy navigation. Although most (75%) had a sociolegal barrier to care, few (7.4%) had a barrier to which a navigator could not respond effectively with some legal-rights training and continuous, consultative access to a public-interest lawyer.
Project SUPPORT had several limitations worth considering. As mentioned above, we acknowledge the high rates of timely treatment among participants, which compromised our power to detect a difference in study groups. The lack of data on patient comorbidity and navigation dose or number of encounters limits our ability to explain our findings. In addition, this was a single-site study in 1 urban safety-net hospital, so the findings may not be generalizable to other settings, particularly given the genesis of the medical-legal partnership approach at the study site and the study site’s leading-edge role in social care nationally. Our methods also precluded us from measuring the effect of the intervention on patient caregivers/family, an area in need of further study. However, lessons learned from this comparative-effectiveness study are relevant to any health system considering patient navigation for their oncology patients. Also as mentioned above, our study design had the potential for introducing contamination into the standard navigation group, although we incorporated several implementation approaches to minimize this risk. Finally, we did not reach our enrollment projections for patients with lung cancer. Therefore, pooled analyses were not possible, and power to detect differences in our categorical clinical outcome was compromised.
Conclusions
In conclusion, with ongoing support from multiple partners, Project SUPPORT enrolled a representative sample of an urban safety-net cancer population into a patient navigation program that systematically documented sociolegal barriers. Although we did not demonstrate an intervention effect, we did document the presence of perceived sociolegal barriers throughout the enhanced navigation group’s cancer care. Whereas the high rates of timely initiation of cancer treatment demonstrated in this vulnerable population are reassuring from a cancer disparities perspective, the continued presence of sociolegal barriers should be a clear message to the United States health care system that we must remain diligent in our pursuit of effective strategies to meet these needs and advance health equity. Although the National Center for Medical-Legal Partnership reports that hundreds of such programs are now established across 46 states, there is much more to explore and learn about how structured approaches to legal support can operate in high-impact ways in the cancer care context.
Acknowledgments
We thank and gratefully acknowledge the support of partnering organizations that share a commitment to reducing disparities and the American Cancer Society for their dedication to patient navigation and the National Navigation Roundtable (NNRT). The National Navigation Roundtable is a collaboration of navigation stakeholders and field experts dedicated to establishing patient navigation as a recognized and valued part of the health care system to assure optimal health outcomes for cancer patients. Thank you to the steering committee of the NNRT for helping lead the direction of this supplement and the hundreds of organizations and patient navigators who provided input and time to help inform this supplement.
FUNDING SUPPORT
This work was supported by the Patient-Centered Outcomes Research Institute (award/project ID: AD-1304-6272) and the American Cancer Society (award/project ID: RSG-13-368-01-CPPB). Christine M. Gunn was supported by a career development award from the National Cancer Institute (K07CA221899).
CONFLICT OF INTEREST DISCLOSURES
Tracy A. Battaglia reports unpaid service as Chair of the National Navigation Roundtable outside the submitted work. JoHanna Flacks and Samantha J. Morton report personal fees from MLPB through a TSNE MissionWorks contract during the conduct of the study. The remaining authors made no disclosures.
Footnotes
We are indebted to the contributions of many partners who contributed to the successful completion of this study, including: our Patient Advisory Group (Carolyn Barnes, Joyce Gandy, Gloria Johnson, Elizabeth Rhodes, Marilyn Simmons, and in memory of Zahra Haghighatatjoo and Roy Davis), our Scientific Advisory Board (Drs. Deb Bowen, Victoria Parker, and Jane Mendez), the patient navigators (Katie Finn, Ina Petreli, Sabrina Morton, Laura Ochoa, and Amy Cann), and our outstanding research team (Emily Bergling, Michelle Carrera, Maria Castano, Kate Festa, Claudia Gumina, Steven Ganem, Serena Haver, Kristine Murray, Vanesa Noel, Jennifer Pamphile, Penny Price-Johnson, Wanda Turner and Sara Waugh).
REFERENCES
- 1.Susan G Komen for the Cure. The Societal and Economic Impact of Cancer Health Disparities. Susan G Komen for the Cure; 2010. [Google Scholar]
- 2.National Program of Cancer Registries. US Cancer Statistics: 2009 Cancer Types Grouped by Race/Ethnicity. Accessed January 20, 2021. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6207a1.htm
- 3.Elmore JG, Nakano CY, Linden HM, Reisch LM, Ayanian JZ, Larson EB. Racial inequities in the timing of breast cancer detection, diagnosis, and initiation of treatment. Med Care. 2005;43:141–148. doi: 10.1097/00005650-200502000-00007 [DOI] [PubMed] [Google Scholar]
- 4.Maly RC, Umezawa Y, Ratliff CT, Leake B. Racial/ethnic group differences in treatment decision-making and treatment received among older breast carcinoma patients. Cancer. 2006;106:957–965. doi: 10.1002/cncr.21680 [DOI] [PubMed] [Google Scholar]
- 5.Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90:1212–1215. doi: 10.2105/AJPH.90.8.1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC). About Social Determinants of Health (SDOH). CDC; 2020. Accessed January 20, 2021. https://www.cdc.gov/socialdeterminants/about.html [Google Scholar]
- 7.Castrucci B, Auerbach J. Health Affairs: Meeting Individual Social Needs Falls Short of Addressing Social Determinants of Health. de Beaumont Foundation; 2019. Accessed January 20, 2021. https://www.debeaumont.org/news/2019/meeting-individual-social-needs-falls-short-of-addressing-social-determinants-of-health/ [Google Scholar]
- 8.Billioux A, Verlander K, Anthony S, Alley D. Standardized Screening for Health-Related Social Needs in Clinical Settings: The Accountable Health Communities Screening Tool. Discussion Paper. National Academy of Medicine; 2017. Accessed January 20, 2021. https://nam.edu/wp-content/uploads/2017/05/Standardized-Screening-for-Health-Related-Social-Needs-in-Clinical-Settings.pdf [Google Scholar]
- 9.Weintraub D, Rodgers MA, Botcheva L, et al. Pilot study of medical-legal partnership to address social and legal needs of patients. J Health Care Poor Underserved. 2010;21(2 suppl):157–168. doi: 10.1353/hpu.0.0311 [DOI] [PubMed] [Google Scholar]
- 10.Whitman S, Ansell D, Orsi J, Francois T. The racial disparity in breast cancer mortality. J Community Health. 2011;36:588–596. doi: 10.1007/s10900-010-9346-2 [DOI] [PubMed] [Google Scholar]
- 11.Ko NY, Battaglia TA, Gupta-Lawrence R, et al. Burden of socio-legal concerns among vulnerable patients seeking cancer care services at an urban safety-net hospital: a cross-sectional survey. BMC Health Ser Res. 2016;16:196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beeson T, McAllister BD, Regenstein M. Making the Case for Medical-Legal Partnerships: A Review of the Evidence. National Center for Medical-Legal Partnership, Department of Health Policy, School of Public Health and Health Services, George Washington University; 2013. [Google Scholar]
- 13.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004 [DOI] [PubMed] [Google Scholar]
- 14.Retkin R, Brandfield J, Bacich C. Impact of Legal Interventions on Cancer Survivors©. LegalHealth; 2007. Accessed January 20, 2021. https://legalhealth.org/wp-content/uploads/2020/03/FinalReportImpactofLegalInterventionsonCancerSurvivors.pdf [Google Scholar]
- 15.Ahuja N, Chang D, Gearhart SL. Disparities in colon cancer presentation and in-hospital mortality in Maryland: a ten-year review. Ann Surg Oncol. 2007;14:411–416. doi: 10.1245/s10434-006-9130-9 [DOI] [PubMed] [Google Scholar]
- 16.Berry DA, Cronin KA, Plevritis SK, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005;353:1784–1792. doi: 10.1056/NEJMoa050518 [DOI] [PubMed] [Google Scholar]
- 17.Bayraktar UD, Chen E, Bayraktar S, et al. Does delay of adjuvant chemotherapy impact survival in patients with resected stage II and III colon adenocarcinoma? Cancer. 2011;117:2364–2370. doi: 10.1002/cncr.25720 [DOI] [PubMed] [Google Scholar]
- 18.Punglia RS, Saito AM, Neville BA, Earle CC, Weeks JC. Impact of interval from breast conserving surgery to radiotherapy on local recurrence in older women with breast cancer: retrospective cohort analysis. BMJ. 2010;340:c845. doi: 10.1136/bmj.c845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gold HT, Thwin SS, Buist DSM, et al. Delayed radiotherapy for breast cancer patients in integrated delivery systems. Am J Manag Care. 2009;15:785–789. [PMC free article] [PubMed] [Google Scholar]
- 20.Fedewa SA, Ward EM, Stewart AK, Edge SB. Delays in adjuvant chemotherapy treatment among patients with breast cancer are more likely in African American and Hispanic populations: a national cohort study 2004-2006. J Clin Oncol. 2010;28:4135–4141. doi: 10.1200/JCO.2009.27.2427 [DOI] [PubMed] [Google Scholar]
- 21.Clark CR, Baril N, Kunicki M, et al. Addressing social determinants of health to improve access to early breast cancer detection: results of the Boston REACH 2010 Breast and Cervical Cancer Coalition Women’s Health Demonstration Project. J Womens Health (Larchmt). 2009;18:677–690. doi: 10.1089/jwh.2008.0972 [DOI] [PubMed] [Google Scholar]
- 22.Siminoff LA, Rogers HL, Thomson MD, Dumenci L, Harris-Haywood S. Doctor, what’s wrong with me? Factors that delay the diagnosis of colorectal cancer. Patient Educ Couns. 2011;84:352–358. doi: 10.1016/j.pec.2011.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McLaughlin JM, Anderson RT, Ferketich AK, Seiber EE, Balkrishnan R, Paskett ED. Effect on survival of longer intervals between confirmed diagnosis and treatment initiation among low-income women with breast cancer. J Clin Oncol. 2012;30:4493–4500. doi: 10.1200/JCO.2012.39.7695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang R, Cheung MC, Byrne MM, et al. Do racial or socioeconomic disparities exist in lung cancer treatment? Cancer. 2010; 116:2437–2447. doi: 10.1002/cncr.24986 [DOI] [PubMed] [Google Scholar]
- 25.ONS, AOSW, and NASW release position statement on patient navigation. Oncol Times. 2010;32:62. doi: 10.1097/01.COT.0000381224.45804.c5 [DOI] [Google Scholar]
- 26.Freeman HP, Rodriguez RL. History and principles of patient navigation. Cancer. 2011;117(15 suppl):3539–3542. doi: 10.1002/cncr.26262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Freeman HP. Patient navigation: a community centered approach to reducing cancer mortality. J Cancer Educ. 2006;21(1 suppl):S11–S14. doi: 10.1207/s15430154jce2101s_4 [DOI] [PubMed] [Google Scholar]
- 28.Fowler T, Steakley C, Garcia AR, Kwok J, Bennett LM. Reducing disparities in the burden of cancer: the role of patient navigators. PLoS Med. 2006;3:e193. doi: 10.1371/journal.pmed.0030193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Calhoun EA, Whitley EM, Esparza A, et al. A national patient navigator training program. Health Promot Pract. 2010;11:205–215. doi: 10.1177/1524839908323521 [DOI] [PubMed] [Google Scholar]
- 30.Battaglia TA, Parker VA, McCoy ME. The Boston Medical Center Patient Navigation Toolkit. 1st ed. Boston Medical Center; 2012. Accessed January 20, 2021. https://ncihub.org/resources/1600/download/BMC_Patient_Navigation_Toolkit_-_Vol_1.pdf [Google Scholar]
- 31.Paskett ED, Harrop JP, Wells KJ. Patient navigation: an update on the state of the science. CA Cancer J Clin. 2011;61:237–249. doi: 10.3322/caac.20111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wells KJ, Battaglia TA, Dudley DJ, et al. Patient navigation: state of the art or is it science? Cancer. 2008;113:1999–2010. doi: 10.1002/cncr.23815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bernardo BM, Zhang X, Hery CMB, Meadows RJ, Paskett ED. The efficacy and cost-effectiveness of patient navigation programs across the cancer continuum: a systematic review. Cancer. 2019;125:2747–2761. doi: 10.1002/cncr.32147 [DOI] [PubMed] [Google Scholar]
- 34.Primeau S, Freund K, Ramachandran A, et al. Social service barriers delay care among women with abnormal cancer screening. J Gen Intern Med. 2013;29:169–175. doi: 10.1007/s11606-013-2615-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ell K, Vourlekis B, Lee PJ, Xie B. Patient navigation and case management following an abnormal mammogram: a randomized clinical trial. Prev Med. 2007;44:26–33. doi: 10.1016/j.ypmed.2006.08.001 [DOI] [PubMed] [Google Scholar]
- 36.Jandorf L, Gutierrez Y, Lopez J, Christie J, Itzkowitz SH. Use of a patient navigator to increase colorectal cancer screening in an urban neighborhood health clinic. J Urban Health. 2005;82:216–224. doi: 10.1093/jurban/jti046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin CJ, Schwaderer KA, Morgenlander KH, et al. Factors associated with patient navigators’ time spent on reducing barriers to cancer treatment. J Natl Med Assoc. 2008;100:1290–1297. doi: 10.1016/s0027-9684(15)31507-8 [DOI] [PubMed] [Google Scholar]
- 38.Ramachandran A, Freund KM, Bak SM, Heeren TC, Chen CA, Battaglia TA. Multiple barriers delay care among women with abnormal cancer screening despite patient navigation. J Womens Health (Larchmnt). 2015;24:30–36. doi: 10.1089/jwh.2014.4869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ko NY, Bak S, Gunn C, et al. An innovation in patient navigation: background, methods, and measures. J Oncol Navig Surviv. 2019;10(6):218–226. [Google Scholar]
- 40.Battaglia TA, Roloff K, Posner MA, Freund KM. Improving follow-up to abnormal breast cancer screening in an urban population. A patient navigation intervention. Cancer. 2007;109(2 suppl):359–367. doi: 10.1002/cncr.22354 [DOI] [PubMed] [Google Scholar]
- 41.Freund KM, Battaglia TA, Calhoun E, et al. National Cancer Institute Patient Navigation Research Program: methods, protocol, and measures. Cancer. 2008;113:3391–3399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.The George Washington University School of Medicine and Health Sciences. Oncology Patient Navigator Training: The Fundamentals. The George Washington University School of Medicine and Health Sciences; 2021. Accessed June 1, 2021. https://cme.smhs.gwu.edu/gw-cancer-center-/content/oncology-patient-navigator-training-fundamentals [Google Scholar]
- 43.National Cancer Database. National Quality Forum Endorsement. American College of Surgeons; 2020. Accessed February 17, 2021. https://www.facs.org/quality-programs/cancer/ncdb/qualitymeasurescocweb/nqf [Google Scholar]
- 44.O’Donnell E. The Distress Thermometer: a rapid and effective tool for the oncology social worker. Int J Health Care Qual Assur. 2013;26:353–359. doi: 10.1108/09526861311319573 [DOI] [PubMed] [Google Scholar]
- 45.Lowery AE, Greenberg MA, Foster SL, et al. Validation of a needs-based biopsychosocial distress instrument for cancer patients. Psychooncology. 2012;21:1099–1106. [DOI] [PubMed] [Google Scholar]
- 46.Sandel M, Hansen M, Kahn R, et al. Medical-legal partnerships: transforming primary care by addressing the legal needs of vulnerable populations. Health Aff (Millwood). 2010;29:1697–1705. doi: 10.1377/hlthaff.2010.0038 [DOI] [PubMed] [Google Scholar]
- 47.Jean-Pierre P, Shao C, Cheng Y, Wells KJ, Paskett E, Fiscella K. Patient Satisfaction with Navigator Interpersonal Relationship (PSN-I): item-level psychometrics using IRT analysis. Support Care Cancer. 2020;28:541–550. doi: 10.1007/s00520-019-04833-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Haun J, Luther S, Dodd V, Donaldson P. Measurement variation across health literacy assessments: implications for assessment selection in research and practice. J Health Commun. 2012;17(suppl 3):141–159. doi: 10.1080/10810730.2012.712615 [DOI] [PubMed] [Google Scholar]
- 49.National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; National Cancer Policy Forum. Establishing Effective Patient Navigation Programs in Oncology: Proceedings of a Workshop. National Academies Press (US); 2018. Accessed October 30, 2020. http://www.ncbi.nlm.nih.gov/books/NBK500558/ [PubMed] [Google Scholar]
- 50.Battaglia TA, Santana MC, Bak S, et al. Predictors of timely follow-up after abnormal cancer screening among women seeking care at urban community health centers. Cancer. 2010;116:913–921. doi: 10.1002/cncr.24851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Raj A, Battaglia TA, Chabner BA, Moy B. Patient navigation for underserved patients diagnosed with breast cancer. Oncologist. 2012;17:1027–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Freund KM, Battaglia TA, Calhoun E, et al. Impact of patient navigation on timely cancer care: the Patient Navigation Research Program. J Natl Cancer Inst. 2014;106:dju115. doi: 10.1093/jnci/dju115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dudley DJ, Drake J, Quinlan J, et al. Beneficial effects of a combined navigator/promotora approach for Hispanic women diagnosed with breast abnormalities. Cancer Epidemiol Biomarkers Prev. 2012;21:1639–1644. doi: 10.1158/1055-9965.EPI-12-0538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ramirez A, Perez-Stable E, Penedo F, et al. Reducing time-to-treatment in underserved Latinas with breast cancer: the Six Cities Study. Cancer. 2014;120:752–760. doi: 10.1002/cncr.28450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Battaglia TA, Darnell JS, Ko N, et al. The impact of patient navigation on the delivery of diagnostic breast cancer care in the National Patient Navigation Research Program: a prospective meta-analysis. Breast Cancer Res Treat. 2016;158:523–534. doi: 10.1007/s10549-016-3887-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yeoh ZY, Jaganathan M, Rajaram N, et al. Feasibility of patient navigation to improve breast cancer care in Malaysia. J Glob Oncol. 2018;4:1–13. doi: 10.1200/JCO.17.00229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chavarri-Guerra Y, Soto-Perez-de-Celis E, Ramos-Lopez W, et al. Patient navigation to enhance access to care for underserved patients with a suspicion or diagnosis of cancer. Oncologist. 2019;24:1195–1200. doi: 10.1634/theoncologist.2018-0133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gunn C, Battaglia TA, Parker VA, et al. What makes patient navigation most effective: defining useful tasks and networks. J Health Care Poor Underserved. 2017;28:663–676. doi: 10.1353/hpu.2017.0066 [DOI] [PubMed] [Google Scholar]
- 59.Baik SH, Gallo LC, Wells KJ. Patient navigation in breast cancer treatment and survivorship: a systematic review. J Clin Oncol. 2016;34:3686–3696. doi: 10.1200/JCO.2016.67.5454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Brooks GA, Hoverman JR, Colla CH. The Affordable Care Act and cancer care delivery. Cancer J. 2017;23:163–167. doi: 10.1097/PPO.0000000000000259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable health communities—addressing social needs through Medicare and Medicaid. N Engl J Med. 2016;374:8–11. doi: 10.1056/NEJMp1512532 [DOI] [PubMed] [Google Scholar]
- 62.University of Wisconsin Population Health Institute School of Medicine and Public Health, Robert Wood Johnson Foundation. Medical-Legal Partnerships. County Health Rankings & Roadmaps; 2018. Accessed January 20, 2021. https://www.countyhealthrankings.org/take-action-to-improve-health/what-works-for-health/strategies/medical-legal-partnerships
- 63.Regenstein M, Trott J, Williamson A, Theiss J. Addressing social determinants of health through medical-legal partnerships. Health Aff (Millwood). 2018;37:378–385. doi: 10.1377/hlthaff.2017.1264 [DOI] [PubMed] [Google Scholar]
- 64.Tsai J, Middleton M, Villegas J, et al. Medical-legal partnerships at Veterans Affairs Medical Centers improved housing and psychosocial outcomes for vets. Health Aff (Millwood). 2017;36:2195–2203. doi: 10.1377/hlthaff.2017.0759 [DOI] [PubMed] [Google Scholar]
- 65.Martin J, Martin A, Schultz C, Sandel M. Embedding civil legal aid services in care for high-utilizing patients using medical-legal partnership. Health Affairs Blog: Innovations in Care Delivery; 2015. Accessed January 20, 2021. 10.1377/hblog20150422.047143/full/ [DOI]
- 66.Tsai J, Jenkins D, Lawton E. Civil legal services and medical-legal partnerships needed by the homeless population: a national survey. Am J Public Health. 2017;107:398–401. doi: 10.2105/AJPH.2016.303596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ryan A. Connecting the Dots: Stress, Health Disparities and Legal Interventions. Paper presented at: 2010 Medical-Legal Partnership Summit; March 25-26, 2010; Arlington, Virginia. [Google Scholar]
- 68.Hernandez D, Hernández D. ‘Extra oomph:’ addressing housing disparities through Medical Legal Partnership interventions. Hous Stud. 2016;31:871–890. doi: 10.1080/02673037.2016.1150431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rodabaugh KJ, Hammond M, Myszka D, Sandel M. A medical-legal partnership as a component of a palliative care model. J Palliat Med. 2010;13:15–18. doi: 10.1089/jpm.2009.0203 [DOI] [PubMed] [Google Scholar]
- 70.Fleishman SB, Retkin R, Brandfield J, Braun V. The attorney as the newest member of the cancer treatment team. J Clin Oncol. 2006;24:2123–2126. [DOI] [PubMed] [Google Scholar]


