Abstract
Background
Although total hip and knee arthroplasty have largely moved to the outpatient setting, total elbow arthroplasty (TEA) remains a predominantly inpatient procedure. Currently, evidence on the safety and potential cost savings of outpatient TEA is limited. Therefore, we aimed to compare the costs and complications associated with performing TEA in the inpatient versus outpatient setting.
Methods
We identified patients who received elective TEA using the Truven Health MarketScan database. Outcomes of interest were 90-day complication rate, readmission rate, and procedure costs in the inpatient and outpatient settings. We used propensity score matching and logistic regression analysis to assess how patient comorbidities and surgical setting influenced complications and readmission rates. The median cost per patient was compared using the Mann-Whitney U test.
Results
We identified 307 outpatient and 414 inpatient TEA procedures over a 9-year period. Elixhauser comorbidity scores were higher for the inpatient cohort. The incidence of surgical complications was significantly higher in the inpatient than the outpatient cohort (27% vs 9%). The odds of 90-day readmissions were similar in the 2 groups (37% vs 25%). In terms of cost, the median inpatient TEA was more expensive than outpatient TEA ($26 817 vs $18 412). However, the median cost for occupational therapy within 90 days of surgery was higher for outpatient TEA patients ($687 vs $571).
Conclusions
The results of this study demonstrate that surgeons can consider a transition toward outpatient TEA for patients without significant comorbidities, as this will substantially reduce health care costs.
Keywords: arthroplasty, arthritis, diagnosis, elbow, health policy, research and health outcomes, surgery, epidemiology
Introduction
Total elbow arthroplasty (TEA) is a surgical option for patients with a range of conditions including advanced rheumatoid arthritis, osteoarthritis, acute distal humerus fractures, and sequelae of elbow trauma.1,2 Utilization of TEA has increased substantially in recent years with a reported 250% rise in procedure volume and a $900 increase in the cost of a TEA procedure per year between 1993 and 2007. 3 Although recent advances in pain control and efforts to reduce health care costs led to a 30% increase in the utilization of outpatient TEA between 2010 and 2017, TEA remains a predominantly inpatient procedure. Meanwhile, hip, knee, and shoulder arthroplasty procedures have largely transitioned to the outpatient setting to reduce costs and enhance patient satisfaction.4-7
The potential benefits of outpatient TEA are significant with respect to cost and patient satisfaction.8-11 A nationwide analysis of academic medical centers revealed that each inpatient procedure cost $16 300 and the average inpatient length of stay was 4.2 days. 3 However, evidence on the safety and cost of outpatient TEA is scarce. Although a single-center study reported good 90-day outcomes among a cohort of 28 patients who had outpatient TEA, we do not know whether these results translate on a larger scale. 12 Therefore, we performed a retrospective, nationwide study to examine the influence of surgical setting on elective TEA costs, readmission rates, and 90-day postoperative complications.
Materials and Methods
Data Source
A retrospective review of the Truven Health Analytics MarketScan Commercial Claims and Encounters (MarketScan) database was performed. This database contains inpatient and outpatient claims, clinical records, and health care expenditures on more than 250 million patients that can be tracked over time. The data are contributed by large employers, managed care organizations, hospitals, electronic medical record providers, Medicare, and Medicaid.
Study Population
We queried the database for all patients who underwent TEA in the inpatient or outpatient setting between 2009 and Q3 of 2017 using the Current Procedural Terminology code 24363. Patients who had nonelective TEA or a revision procedure were excluded if the primary diagnosis indicated an associated upper arm injury or implant complication (Table S1). Patients with both outpatient and inpatient TEA recorded in the database were excluded because we could not determine whether complications were associated with a specific surgical setting. Furthermore, those who lacked enrollment data in the 90 days after the procedure were excluded because we could not confirm that their postoperative complications were captured in the database.
We created 2 matched samples to compare inpatient and outpatient outcomes based on sex, age, household income, geographic region, and comorbidities. We identified comorbidities using International Classification of Diseases, Ninth Revision (ICD-9) codes for years 2009 through 2014. We used ICD, Tenth Revision (ICD-10) codes for the years 2015 to 2017, when providers transitioned to the new system (Table S2).
Outcomes
We identified complications in the 90-day postoperative window using ICD diagnosis and procedure codes. Surgical complications included wound dehiscence, wound infection, postoperative shock, and blood transfusion. Medical complications included respiratory failure, pneumonia, pulmonary embolism, renal insufficiency, acute renal failure, urinary tract infection, stroke, cardiac arrest, myocardial infarction, deep venous thrombosis, and sepsis (Tables S3 and S4). In addition, the 90-day postoperative readmission rates for both acute pain and other causes were examined. The cost of surgical intervention and the cost of occupational therapy (OT) for the 90-day postoperative period were queried from the database. Cost of surgical intervention was defined as the total gross payment to all providers associated with the encounter and represented the sum of the following database variables: coordination of benefits and other savings, coinsurance, deductible, and net payments.
Analyses
The adjusted odds ratios (ORs) and associated 95% confidence intervals (CIs) were calculated for the association between surgical setting and the outcomes of interest. The calculations were derived from the logistic regression model and inverse probability of treatment weighting using the propensity score. The propensity scores were estimated with generalized boosted regression models and accounted for the following variables: age, sex, Elixhauser comorbidity score, income, region, obesity, tobacco use, diabetes, coronary artery disease, chronic kidney disease, and chronic anemia. A statistical significance was considered for a 2-sided value of P < .05 for all tests.
We also assessed the difference in complication rates, readmissions, and costs of the inpatient and outpatient matched cohorts. We applied χ2 tests to compare categorical variables and Student’s t tests to compare continuous variables. To calculate the median cost per patient, we used the Mann-Whitney U test. Again, values of P < .05 were considered significant.
Results
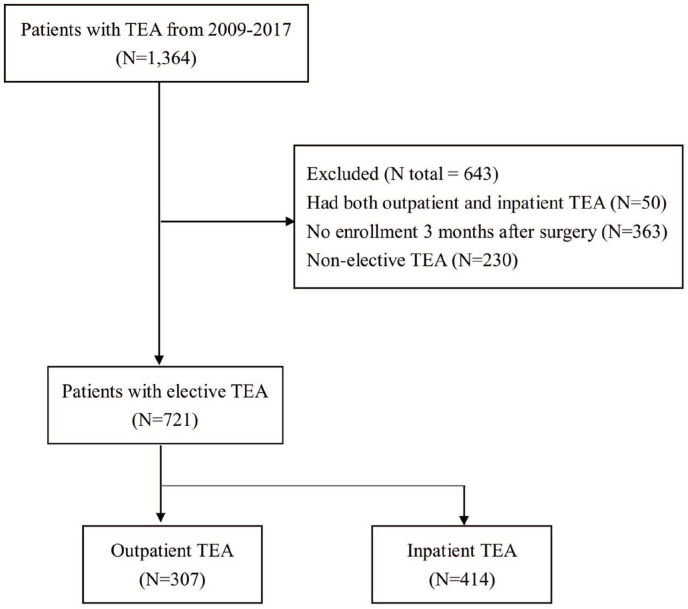
The patient selection process is displayed in Figure 1. We identified a total of 1364 patients who underwent TEA between 2009 and quarter one of 2017. Of these patients, 643 were excluded: 50 had both outpatient and inpatient TEA records, 363 were not enrolled in the 90-day postoperative period, and 230 had nonelective TEA. Of the remaining 721 patients, 307 and 414 had outpatient and inpatient TEA, respectively (Figure 2, Table S5).
Figure 1.
Patient selection process.
Note. TEA = total elbow arthroplasty.
Figure 2.
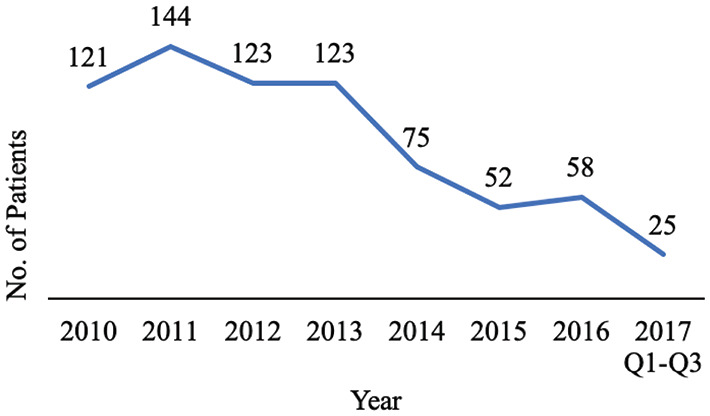
Trends in procedure volume over time.
The demographic data of the 721 patients are shown in Table 1. Age was not significantly different between the 2 groups. Inpatient TEA patients were on average 61.9 ± 14.9 years old and outpatient TEA patients were 59.6 ± 13.9 years old. There was a statistically significant difference in sex between the 2 groups with more men in the inpatient group (347, 84%) compared with the outpatient group (231, 75%). Inpatients had significantly higher Elixhauser comorbidity scores (P = .01), particularly at the higher end of the scoring system (>8). We did not identify a significant difference in the rate of any particular comorbidities between the 2 groups.
Table 1.
Demographic Characteristics and Comorbidities.
| Characteristic | Inpatient TEA (N = 414) | Outpatient TEA (N = 307) | P value | ||
|---|---|---|---|---|---|
| N | (%) | N | (%) | ||
| Male | 347 | (83.8) | 231 | (75.2) | <.01 |
| Age, y, mean (SD) | 65.1 | ±14.2 | 63.7 | ±14.2 | .20 |
| Elixhauser comorbidity score | .01 | ||||
| 0 | 113 | (27.3) | 104 | (33.9) | |
| 1-3 | 47 | (11.4) | 54 | (17.6) | |
| 4-7 | 101 | (24.4) | 60 | (19.5) | |
| ≥8 | 153 | (37.0) | 89 | (29.0) | |
| Median household income | <.01 | ||||
| ≤40 000 | 10 | (2.4) | 12 | (3.9) | |
| 40 001-50 000 | 95 | (22.9) | 101 | (32.9) | |
| 50 001-60 000 | 137 | (33.1) | 106 | (34.5) | |
| 60 001-70 000 | 51 | (12.3) | 16 | (5.2) | |
| >70 000 | 25 | (6.0) | 3 | (1.0) | |
| Unspecified | 96 | (23.2) | 69 | (22.5) | |
| Geographic region | .01 | ||||
| Northeast | 74 | (17.9) | 27 | (8.8) | |
| North Central | 114 | (27.5) | 92 | (30.0) | |
| South | 151 | (36.5) | 136 | (44.3) | |
| West | 68 | (16.4) | 45 | (14.7) | |
| Missing | 7 | (1.7) | 7 | (2.3) | |
| Comorbidity | |||||
| Obesity | 0 | (0) | 0 | (0) | NA |
| Diabetes mellitus | 1 | (0.2) | 0 | (0) | .39 |
| Smoking | 21 | (5.1) | 20 | (6.5) | .41 |
| Coronary artery disease | 42 | (10.1) | 30 | (9.8) | .87 |
| Chronic kidney disease | 21 | (5.1) | 15 | (4.9) | .91 |
| Anemia | 74 | (17.9) | 52 | (16.9) | .74 |
Note. TEA = total elbow arthroplasty; NA = not applicable.
The frequency and ORs for complications and readmissions are shown in Table 2. The outpatient setting was associated with significantly fewer overall surgical complications (27% vs 9%, OR: 0.39, 95% CI, 0.18-0.85, P = .02) than the inpatient setting. Wound infections in particular were more significantly common among inpatients (4.3% vs 2.0%, OR: 0.37, 95% CI, 0.14-0.95). Although wound dehiscence was also more common among inpatients, the difference was not significant. Medical complications, readmissions for all causes, and readmissions for acute pain were also not significantly different between the 2 groups.
Table 2.
Complication and Readmission Rates.
| Complications | Surgery place, N (%) | AOR and 95% CI* (ref: inpatient) | P value | |||
|---|---|---|---|---|---|---|
| Inpatient | Outpatient | |||||
| Surgical complications | 27 | (6.5) | 9 | (2.9) | 0.39 (0.18-0.85) | .02 |
| Wound dehiscence | 9 | (2.2) | 3 | (1.0) | 0.47 (0.12-1.86) | .28 |
| Wound infection | 18 | (4.3) | 6 | (2.0) | 0.37 (0.14-0.95) | .04 |
| Postoperative shock | 0 | (0) | 0 | (0) | NA | NA |
| Blood transfusion | 0 | (0) | 0 | (0) | NA | NA |
| Medical complications | 26 | (6.3) | 15 | (4.9) | 0.89 (0.44-1.82) | .75 |
| Stroke | 0 | (0) | 0 | (0) | NA | NA |
| UTI/Renal complications | 8 | (1.9) | 5 | (1.6) | 0.77 (0.24-2.49) | .66 |
| DVT/Pulmonary embolism | 4 | (1.0) | 5 | (1.6) | 2.32 (0.47-11.50) | .30 |
| Myocardial infarction | 0 | (0) | 0 | (0) | NA | NA |
| Respiratory failure/Pneumonia | 11 | (2.7) | 5 | (1.6) | 0.73 (0.23-2.33) | .59 |
| Cardiac arrest | 0 | (0) | 0 | (0) | NA | NA |
| Sepsis | 3 | (0.7) | 1 | (0.3) | 0.82 (0.06-11.70) | .89 |
| Readmission for all cause | 37 | (8.9) | 25 | (8.1) | 0.93 (0.53-1.65) | .81 |
| Readmission for acute pain | 3 | (0.7) | 2 | (0.7) | 0.73 (0.12-4.53) | .73 |
Note. AOR = adjusted odds ratios; CI = confidence interval; UTI = urinary tract infection; DVT = deep venous thrombosis.
The potential confounding bias for interested outcomes was controlled by the propensity score weighting (PSW)and calculated the adjusted odds ratios.The confounding factors includedage, sex, Elixhauser comorbidity score, income, region, obesity, tobacco use, diabetes, coronary artery disease, chronic kidney disease, and chronic anemia.
Table 3 demonstrates the cost of TEA by service location. The cost of outpatient TEA was significantly lower than that of inpatient TEA ($18 412 vs $26 817, P < .01). Postoperative OT costs were higher for patients undergoing outpatient TEA compared with those who had inpatient TEA ($687 vs $571), but the difference did not reach statistical significance.
Table 3.
Total Elbow Arthroplasty Costs.
| US dollars | Inpatient TEA | Outpatient TEA | P value |
|---|---|---|---|
| Total cost for TEA, median (IQR) | 26 817 (18 719-45 122) | 18 412 (11 734-35 546) | <.01 |
| OT a within 90 d of TEA, median (IQR) | 571 (271-1075) | 687 (271-1548) | .35 |
Note. TEA = total elbow arthroplasty; IQR = interquartile range; OT = occupational therapy.
The OT costs were calculated only for patients who had OT within 90 days of TEA. P values were derived using the Mann-Whitney U test to measure the statistical difference for median.
Discussion
This retrospective, multi-institution database study demonstrated that outpatient TEA is a safe and cost-effective procedure for patients with few comorbidities. Although readmission rates were similar between patients who had inpatient versus outpatient TEA, surgical complication rates were higher among inpatients. Furthermore, the associated costs were on average $10 000 higher for inpatient procedures. The cost savings encourage the continued transition away from the inpatient setting for many TEA procedures, especially in light of the current emphasis on value-based care in the United States and globally. With the transition to bundled payment in episode of care models, all savings will be beneficial in capturing additional professional revenue. Furthermore, our finding that complication rates are lower or unchanged among outpatients suggests that this surgical setting can be safer and lead to better outcomes. However, although we did not identify a significant difference with respect to the prevalence of smoking or diabetes, specifically, it is possible that some patients’ comorbid conditions put them at a greater risk of experiencing complications such as wound infection.
Our complication analysis differs from prior research. Zhou et al used a national administrative database to identify an overall complication rate of 3.1% and a readmission rate of 4.4% for inpatient TEA. 3 In our study, patients undergoing inpatient TEA had higher medical (6.3%) and surgical (6.5%) complication rates as well as a higher readmission rate (8.9%). In a single-center study, Stone et al reported on complications, reoperations, and readmissions within the 90 days after outpatient TEA. 12 Although their study reported similar complication rates, it was limited by the small sample size of 28 patients and lack of an inpatient comparison group.
More recently, Pasternack et al conducted a retrospective review of both inpatient and outpatient TEA in the American College of Surgeons National Surgical Quality Program database. 13 The authors reported a lower 30-day complication rate among outpatients, although the difference was not significant. We evaluated the same complications and identified a significant difference in complication rates within the 90-day period. It is possible that our study cohorts were distinct with respect to health status, as Pasternack et al did not report on comorbidities. Meanwhile, the inpatients in our study had higher Elixhauser comorbidity scores than the outpatients. There are disadvantages to the Elixhauser system, as the relative influence of specific comorbidities cannot be assessed and there is no one statistic to describe a sample. 14 Nevertheless, inpatient TEA may be justified for patients who have an increased risk of complications, despite the current trend toward performing outpatient arthroplasty to save costs.
Our cost analyses were in line with prior findings. Although research comparing the costs of inpatient and outpatient TEA is limited, cost analyses of shoulder, knee, hip, and ankle arthroplasty also demonstrate major cost savings in the outpatient setting. 7 ,15-17 For example, patients undergoing outpatient shoulder arthroplasty save an estimated $4000 compared with those who have inpatient shoulder arthroplasty. 6 This is in parallel with our findings, which demonstrated nearly $10 000 reduction in costs per case for outpatient TEAs. We did observe higher OT costs in the outpatient group compared with the inpatient group. Although the difference in OT costs was not significantly different, it may be attributable to the fact that inpatients have some OT while in the hospital postoperatively. It is also important to note that Zhou et al estimated that the direct hospital cost for inpatient TEA was $16 300 per case, which is substantially less than the total payment of $26 800 that we calculated. However, these values cannot be compared directly—the total payment includes costs paid by the patient and net payments by the insurer. Given that hospitals aim to make a profit, the sum of these costs should be higher than the hospital costs. Furthermore, accounting variations likely contributed substantially to the variation observed, given that we analyzed a different database than Zhou et al.
The similar readmission rate for inpatient and outpatient TEA is another notable finding from this study. We specifically queried the database for ICD codes indicating readmission for pain and observed no difference between the 2 study groups. Often, upper extremity surgeons cite pain management as a reason why TEA should be an inpatient procedure. However, advances in pain control, including the use of 1-shot regional blocks with longer lasting anesthetic, have made outpatient TEA a practical option. We did not explore the implications that the outpatient setting and different pain control methods have on patient satisfaction. However, the 90% satisfaction rate among outpatient TEA patients in the study by Stone et al suggests that patients are accepting of these factors. High satisfaction rates among patients who undergo other outpatient arthroplasty procedures have also been reported.9,18 The implications of cost savings are not relevant in countries outside the United States with different payment systems. Nevertheless, outpatient surgery may be universally preferable from the patient’s perspectives.
Although we were able to assess TEA procedures across all payer types and multiple institutions, we were limited by the lack of surgery- and patient-specific data in the MarketScan database. For example, we could not determine the precise reasons why patients underwent TEA, which may justify use of the inpatient setting. Although we relied on the literature to identify the most common complications associated with TEA, we also may have neglected to identify rarer complications that were not included in Table 2. In addition, we could not determine whether specific complications resulted in a longer length of stay for inpatients, which would drive up costs. However, the literature indicates that perioperative complications are associated with a longer stay. The type of anesthesia and pain medications administered to each patient also could not be assessed. Furthermore, we excluded a large number of patients who either had no enrollment data 90 days postoperatively or had both inpatient and outpatient records. Nevertheless, this enabled a more focused analysis of the influence of surgical setting on long-term complications and associated costs.
It is important to evaluate complications and costs in the 90-day window to inform the development of new payment models for TEA. For example, bundled payment methodology combines reimbursements for all aspects of care, from the start of a procedure through 90 days postoperatively, into a single payment amount. Although bundled payments have not been introduced for TEA, they already exist for other procedures and will likely become more common, given the growing emphasis on value-based care. 19 Further investigation into the variation in OT costs based on surgical setting will be necessary to ensure that therapy remains accessible under new payment systems, as well.
The lower cost of outpatient TEA highlights a major area for cost reduction moving forward. Although patients with significant comorbidities will continue to require hospitalization for TEA, this study demonstrates that the procedure can be performed in the outpatient setting to reduce costs. However, it is important to consider whether patients with significant comorbidities are at increased risk of postoperative complications, warranting the need for inpatient surgery.
Supplemental Material
Supplemental material, sj-pdf-1-han-10.1177_15589447211030693 for Utilization, Complications, and Costs of Inpatient versus Outpatient Total Elbow Arthroplasty by Natalie B. Baxter, Elissa S. Davis, Jung-Sheng Chen, Jeffrey N. Lawton and Kevin C. Chung in HAND
Supplemental material, sj-pdf-2-han-10.1177_15589447211030693 for Utilization, Complications, and Costs of Inpatient versus Outpatient Total Elbow Arthroplasty by Natalie B. Baxter, Elissa S. Davis, Jung-Sheng Chen, Jeffrey N. Lawton and Kevin C. Chung in HAND
Supplemental material, sj-pdf-3-han-10.1177_15589447211030693 for Utilization, Complications, and Costs of Inpatient versus Outpatient Total Elbow Arthroplasty by Natalie B. Baxter, Elissa S. Davis, Jung-Sheng Chen, Jeffrey N. Lawton and Kevin C. Chung in HAND
Supplemental material, sj-pdf-4-han-10.1177_15589447211030693 for Utilization, Complications, and Costs of Inpatient versus Outpatient Total Elbow Arthroplasty by Natalie B. Baxter, Elissa S. Davis, Jung-Sheng Chen, Jeffrey N. Lawton and Kevin C. Chung in HAND
Supplemental material, sj-pdf-5-han-10.1177_15589447211030693 for Utilization, Complications, and Costs of Inpatient versus Outpatient Total Elbow Arthroplasty by Natalie B. Baxter, Elissa S. Davis, Jung-Sheng Chen, Jeffrey N. Lawton and Kevin C. Chung in HAND
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was deemed exempt and not regulated by our institutional review board.
Statement of Human and Animal Rights: The project was deemed exempt by the institutional review board at the home institution. No identifying information was obtained for the analysis during this study, nor was it included in the article.
Statement of Informed Consent: Informed consent was not required for this study because data were obtained from a database with deidentified patient information.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: K.C.C. receives book royalties from Wolters Kluwer and Elsevier. He has received financial support from Axogen. J.N.L. receives royalties from Innomed, AO North America, and Wolters Kluwer. These organizations had no role in the design and conduct of this study. The authors have no other financial remuneration to report.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was supported by the Maintenance Project of the Center for Artificial Intelligence in Medicine (Grant CLRPG3H0012) at Chang Gung Memorial Hospital for the data analysis and interpretation. This research was funded by a joint Chang Gung Memorial Hospital-University of Michigan Medical Center grant (CORPG3H0071, CORPG3J0191, and CORPG3J0201) to K.C.C.
ORCID iD: Kevin C. Chung  https://orcid.org/0000-0002-2822-3164
https://orcid.org/0000-0002-2822-3164
References
- 1.Zhang D, Chen N.Total elbow arthroplasty. J Hand Surg Am. 2019;44(6):487-495. [DOI] [PubMed] [Google Scholar]
- 2.Triplet JJ, Kurowicki J, Momoh E, et al. Trends in total elbow arthroplasty in the Medicare population: a nationwide study of records from 2005 to 2012. J Shoulder Elbow Surg. 2016;25(11):1848-1853. [DOI] [PubMed] [Google Scholar]
- 3.Zhou H, Orvets ND, Merlin G, et al. Total elbow arthroplasty in the United States: evaluation of cost, patient demographics, and complication rates. Orthop Rev (Pavia). 2016;8(1):6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carey K, Morgan JR, Lin MY, et al. Patient outcomes following total joint replacement surgery: a comparison of hospitals and ambulatory surgery centers. J Arthroplasty. 2020;35(1):7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dorr LD, Thomas DJ, Zhu J, et al. Outpatient total hip arthroplasty. J Arthroplasty. 2010;25(4):501-506. [DOI] [PubMed] [Google Scholar]
- 6.Cancienne JM, Brockmeier SF, Gulotta LV, et al. Ambulatory total shoulder arthroplasty: a comprehensive analysis of current trends, complications, readmissions, and costs. J Bone Joint Surg Am. 2017;99(8):629-637. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez T, Fisk E, Chiodo C, et al. Economic analysis and patient satisfaction associated with outpatient total ankle arthroplasty. Foot Ankle Int. 2017;38(5):507-513. [DOI] [PubMed] [Google Scholar]
- 8.Aynardi M, Post Z, Ong A, et al. Outpatient surgery as a means of cost reduction in total hip arthroplasty: a case-control study. HSS J. 2014;10(3):252-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelly MP, Calkins TE, Culvern C, et al. Inpatient versus outpatient hip and knee arthroplasty: which has higher patient satisfaction. J Arthroplasty. 2018;33(11):3402-3406. [DOI] [PubMed] [Google Scholar]
- 10.Kingery MT, Cuff GE, Hutzler LH, et al. Total joint arthroplasty in ambulatory surgery centers: analysis of disqualifying conditions and the frequency at which they occur. J Arthroplasty. 2018;33(1):6-9. [DOI] [PubMed] [Google Scholar]
- 11.Huang A, Ryu JJ, Dervin G.Cost savings of outpatient versus standard inpatient total knee arthroplasty. Can J Surg. 2017;60(1):57-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stone MA, Singh P, Rosario SL, et al. Outpatient total elbow arthroplasty: 90-day outcomes. J Shoulder Elbow Surg. 2018;27(7):1311-1316. [DOI] [PubMed] [Google Scholar]
- 13.Pasternack JB, Mahmood B, Martins AS.The transition of total elbow arthroplasty into the outpatient theater. JSES Int. 2020;4:44-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Walraven C, Austin PC, Jennings A, et al. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626-633. [DOI] [PubMed] [Google Scholar]
- 15.Gromov K, Jørgensen CC, Petersen PB, et al. Complications and readmissions following outpatient total hip and knee arthroplasty: a prospective 2-center study with matched controls. Acta Orthop. 2019;90(3):281-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Charles MD, Cvetanovich G, Sumner-Parilla S, et al. Outpatient shoulder arthroplasty: outcomes, complications, and readmissions in 2 outpatient settings. J Shoulder Elbow Surg. 2019;28(6S):S118-S123. [DOI] [PubMed] [Google Scholar]
- 17.Brolin TJ, Mulligan RP, Azar FM, et al. Neer Award 2016: outpatient total shoulder arthroplasty in an ambulatory surgery center is a safe alternative to inpatient total shoulder arthroplasty in a hospital: a matched cohort study. J Shoulder Elbow Surg. 2017;26(2):204-208. [DOI] [PubMed] [Google Scholar]
- 18.Leroux TS, Zuke WA, Saltzman BM, et al. Safety and patient satisfaction of outpatient shoulder arthroplasty. JSES Open Access. 2018;2(1):13-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Siddiqi A, White PB, Mistry JB, et al. Effect of bundled payments and health care reform as alternative payment models in total joint arthroplasty: a clinical review. J Arthroplasty. 2017;32(8):2590-2597. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-han-10.1177_15589447211030693 for Utilization, Complications, and Costs of Inpatient versus Outpatient Total Elbow Arthroplasty by Natalie B. Baxter, Elissa S. Davis, Jung-Sheng Chen, Jeffrey N. Lawton and Kevin C. Chung in HAND
Supplemental material, sj-pdf-2-han-10.1177_15589447211030693 for Utilization, Complications, and Costs of Inpatient versus Outpatient Total Elbow Arthroplasty by Natalie B. Baxter, Elissa S. Davis, Jung-Sheng Chen, Jeffrey N. Lawton and Kevin C. Chung in HAND
Supplemental material, sj-pdf-3-han-10.1177_15589447211030693 for Utilization, Complications, and Costs of Inpatient versus Outpatient Total Elbow Arthroplasty by Natalie B. Baxter, Elissa S. Davis, Jung-Sheng Chen, Jeffrey N. Lawton and Kevin C. Chung in HAND
Supplemental material, sj-pdf-4-han-10.1177_15589447211030693 for Utilization, Complications, and Costs of Inpatient versus Outpatient Total Elbow Arthroplasty by Natalie B. Baxter, Elissa S. Davis, Jung-Sheng Chen, Jeffrey N. Lawton and Kevin C. Chung in HAND
Supplemental material, sj-pdf-5-han-10.1177_15589447211030693 for Utilization, Complications, and Costs of Inpatient versus Outpatient Total Elbow Arthroplasty by Natalie B. Baxter, Elissa S. Davis, Jung-Sheng Chen, Jeffrey N. Lawton and Kevin C. Chung in HAND