Abstract
Transdiagnostic frameworks posit a causal link between emotion regulation (ER) ability and psychopathology. However, there is a lack of supporting longitudinal evidence for such frameworks. Among N = 1262 adolescents, we examine the prospective bidirectional relationship between ER and future pathological anxiety, depression, and substance dependence symptoms. In Random-intercept cross-lagged panel models, within-person results do not reveal prospective lag-1 effects of either ER or symptoms. However, between-person analyses showed that dispositional ER ability predicted greater risk for developing clinically significant symptoms during the study. These findings provide some of the first direct evidence of prospective effects of ER on future symptom risk across affect-related disorders, and should strengthen existing claims that ER ability represents a key transdiagnostic risk factor.
Keywords: Emotion Regulation, Depression, Substance Use, Longitudinal, Risk Factor
Individual differences in emotion regulation (ER) can be broadly defined as an individual’s ability to modulate their emotional experiences (Gross & Barrett, 2011). ER has received an enormous amount of empirical attention given its association with mental health outcomes across disorder classifications. For instance, an inability to regulate one’s emotions is typically viewed as an important risk factor for distress disorders like anxiety and depression (Aldao et al., 2010; Campbell-Sills & Barlow, 2007), as well as disorders of substance abuse (Cheetham et al., 2010; Rakesh, Allen, & Whittle, 2020; Sloan et al., 2017). This association between ER and the development of both internalizing and externalizing disorders has contributed to the emergence of transdiagnostic psychiatric frameworks, which suggest that multiple forms of mental illness, including major depression, most anxiety disorders, and substance abuse, are driven by a smaller number of core risk factors such as the inability to regulate or control one’s negative emotions (Aldao, Nolen-Hoeksema, & Schweizer, 2010; Carpenter & Trull, 2013; Kring & Sloan, 2009; Sheppes et al., 2015; Sloan et al., 2017). Theories of this type suggest that a person’s emotion regulation ability should impact their risk for developing both internalizing and externalizing disorders in the future, and, if well-supported, transdiagnostic frameworks could eventually transform the ways that clinical researchers, therapists, and governments approach mental health treatment and prevention.
Problematically, though, despite an expansive body of studies suggesting links between ER and psychiatric disorders, there is surprisingly little direct evidence that ER ability actually precedes and confers risk for the pathology development (for a recent review, see Cludius et al., 2020). Most studies and review articles in this domain rely on evidence that is cross-sectional, or show prospective links between ER and outcomes indirectly related to psychopathology status (Halligan et al., 2013; Schneider et al., 2018; Weissmann et al., 2019). This is a significant problem because although it is clear that increased ER is linked to decreased psychiatric outcomes, there are also salient alternative explanations for such links.
Clinical Symptoms and Future Emotion Regulation
For instance, lower ER ability may be associated with pathology levels across multiple disorders because increased difficulties in controlling one’s emotions could emerge as a consequence of developing affect-related disorders that are characterized by distress. In other words, people who develop pathological depressive or anxiety symptoms may subsequently report an abnormally low ability to regulate their emotions because pervasive sadness, hopelessness, fear, anxiety, etc. are more difficult to manage or downregulate. Relatedly, it is quite plausible that the emergence of intense depressive of anxious symptomology could eventually result in the increased use of maladaptive ER strategies like emotional suppression or rumination. A similar direction of effect is also plausible for disorders of substance abuse, where significant alcohol or drug consumption may decrease future ability to regulate one’s emotions or increase use of maladaptive ER strategies (Weise et al., 2017; Kober, 2014). We propose that there are important reasons to expect a that anxiety, depressive, or substance abuse symptoms could impact the development of future ER ability (Cludius et al., 2020; Kober, 2014; Weiss et al., 2017), and this causes important ambiguity surrounding the strength of the prospective relationship between ER and future mental health problems.
Emotion Regulation and Future Clinical Symptoms
Importantly though, there are specific psychological and social mechanisms that plausibly link individual differences in ER (e.g., lower ER ability) earlier in life to risk for the development of multiple forms of psychopathology. For instance, use of maladaptive ER strategies like suppression and avoidance has mediated relationships between emotional distress and mental health problems in both children and adults (Andrés et al., 2016; Yoon et al., 2013). In social domains, youth who have difficulties regulating their emotions have been less socially competent (Fabes & Eisenberg, 1992), have experienced difficulty forming close relationships (Dollar et al., 2018; Tubman & Lerner, 1994; Yap et al., 2007). Such youth may experience social isolation and excessive negative affect and the associated mental health problems (Bradley, 2003; Yap et al., 2007). In addition, social rejection of this type coupled with a perceived inability to effectively regulation one’s emotions could also confer mental health risk by driving an inner working model where the self is seen as incompetent or worthless, or a perception that one’s problems are hopeless (Bradley, 2003; Tobia, Riva, & Caprin, 2017). In addition, young people who experience excessive negative affect may learn to rely on avoidance, suppression, and other maladaptive coping strategies, further exacerbating or prolonging psychological distress (Yoon et al., 2013).
There is also some longitudinal evidence to support this work. Excessive rumination, a key maladaptive ER strategy, has mediated the link between child maltreatment and generalized psychopathology up to 2 years later (Weissmann et al., 2019). Along these lines, McLaughlin and Nolen-Hoeksema (2011) showed that increased rumination mediated the longitudinal links between baseline depression and future anxiety and also baseline anxiety and future depression. In addition, reduced emotional awareness and abilities to pursue goals when upset (also common behavioral constituents of ER ability; Gratz & Roemer, 2004) have predicted increases in social anxiety over an 18-month time-span (Schneider et al., 2018).
In addition to affective disorders, there are also plausible reasons to expect that lower ER ability could potentially confer risk for future substance abuse symptoms or disorders (SUDs). In the most basic sense, the two constructs show strong covariance—that is, a substantial body of evidence has linked lowered ER ability or use of maladaptive ER strategies to increased substance abuse (for a review, see Kober, 2014). Relatedly, neurological makers associated with decreased ER ability have been consistently associated with concurrent SUDs (for a review, see Wilcox et al., 2016). In longitudinal research, research has shown that emotion regulation interventions have reduced substance abuse behavior (Azizi, et al., 2010). In addition, increased use of ineffective ER strategies during the day has been associated with greater substance consumption later in the day (Weiss et al., 2017). Moreover, children’s performance on delayed gratification tasks, which are thought to index a key emotion regulation dimension (Mischel et al., 2011), have consistently predicted future SUD risk (see Kober, 2014 for a review).
In sum, we see substantial empirical and theoretical reasons to expect that inabilities to successfully regulate emotion early in life could proceed or prospectively predict the development of affective or substance abuse disorders. In addition, though, there are also theoretical and empirical reasons to expect the opposite direction of effect where increased symptomology could prospectively predict lowered emotion regulation ability (for reviews, see Cludius et al., 2020 and Kober et al., 2014; also Weiss et al., 2017). Importantly, these two directions of effect could both explain the extensive existing cross-sectional evidence linking lessor ER ability to multiple forms of psychopathology. We propose that further longitudinal research in this domain is essential to help disentangle and better understand the relative magnitude of both directions of effect, with the overall goal of clarifying the role of ER ability in the development of the most common forms of psychopathology. Evaluating this bidirectional link would require a unique study design—one that is of substantial longitudinal duration that also repeatedly assesses both ER and multiple forms of psychopathology throughout. The existing Pathways to Desistance study (Mulvey et al., 2004) enables such an investigation.
The Present Study
In a series of longitudinal SEMs, we investigate ER ability, both as a stable individual difference and as a developing ability, as a prospective predictor of clinically significant anxiety, depression, and substance dependence. In an identical way, the present models also examine clinical symptoms as predictors of future ER ability. For clinical symptom outcomes, we focus on clinically significant anxiety, depressive, and substance abuse status because, together, these symptom clusters represent both 1) the most common forms of psychopathology and 2) the symptom clusters that are perhaps most associated with ER ability (Wittchen et al., 2011; Kessler et al., 2012).
Drawn from the seven-year Pathways to Desistance study, the present longitudinal dataset includes at-risk adolescents who were involved in the criminal justice system.
The multi-site Pathways to Desistance project began in 2000 and followed 1,354 at-risk youth across seven years from adolescence to young adulthood (Mulvey et al., 2004). Participants completed a battery of dispositional assessments at baseline, and then completed 10 follow-up assessments targeting ER and clinical symptoms as they developed over time.
This sample has several strengths. First, the present assessments generally began in adolescence (M = 16.04), an age that is prior to the typical age of onset for disorders related to anxiety (~ age 17–25; de Lijster et al., 2017) or depressive symptoms (~ age 26; Zisook et al., 2007). Although some studies have reported earlier ages of onset for disorders such as depression in at-risk samples (e.g., age 12–13; Weissman et at., 2019), the present data showed more or less typical onsets for clinically significant depression (17.9 years), anxiety (17.8 years), and substance dependence (18.0 years). Only 35% of the clinically significant pathology assessed in the present analyses was present during or prior to baseline assessment. In this way, the present sample is useful in that it allowed for (typically) the examination of the first incidence of clinically significant psychopathology. Second, the dataset is large, allowing us to study significant numbers of healthy individuals who would go on to develop clinically significant depression (N = 208), anxiety (N = 147), and substance dependence (N = 478).
Hypotheses
Broadly, the present study investigates the ways in which ER ability and clinically significant depressive, anxiety, and substance abuse prospectively interreact throughout the transition from adolescence to adulthood. This question was examined both from a between-person perspective, as well as from a within-person perspective.
Within Person Dynamics.
Across 10 follow-up waves and consistent with existing theory, we expected that person-centered ER levels at each wave would predict person-centered symptom status at the following assessment wave, controlling for concurrent covariance and autoregressive effects. In an exploratory analysis, we also examined an identically structured effect of clinical symptom status as a predictor of subsequent ER ability.
Between Person Dynamics.
Consistent with existing theory and controlling for baseline symptoms, we also expected that dispositional levels of ER measured at baseline would confer greater risk for reporting clinically significant symptoms during the study. In an exploratory analysis, we also examined the opposite direction of effect where individual differences in lifetime history of clinical symptomology were evaluated as predictors of future individual differences in ER ability.
Method
Participants and General Procedures
The multi-site Pathways to Desistance project followed at-risk youth from adolescence to young adulthood (Mulvey et al., 2004; Pathways to Desistance, 2016). The enrolled youth were between the ages of 14 and 18 at the time of enrollment (Final N = 1262, Mage = 16.04, 86.4 % male, 20.2 % White, 41.4 % Black, 33.5% Hispanic, 4.8% Other). Enrollees came from court systems in Maricopa County, Arizona (N = 654) and Philadelphia County, Pennsylvania (N = 700). Youths were recruited based on a review of their court files and were eligible if they had been found guilty of a significant offense (Mulvey et al., 2004). Over a total of 7 years, the study completed a baseline assessment targeting dispositional measures and 10 follow-up waves measuring more proximal experiences (6, 12, 18, 24, 30, 36, 48, 60, 72, 84 months).
Baseline Dispositional Measures
Emotion Regulation Ability.
Dispositional or lifetime experiences of emotion regulation ability were assessed at baseline using 9 items from the Emotion Control component of the How I Feel scale (Walden, Harris, & Catron, 2003; Walden, Lemerise, & Gentile, 1992). The Emotion Control subscale is a broad-bandwidth scale measuring the effectiveness of personal emotion regulation abilities designed specifically for youth. The scale has been reliable as an assessment of ER in youth (Walden et al., 2003), and has shown convergent validity with relevant constructs such as coping with negative events (r = .37), and trait positive (r = .23) or negative affect (r = −.21; Walden et al., 2003). To maximally reduce measurement error in the final data, the Pathways team factor-analyzed the original 12 Emotion Control items to fit the scale to the present at-risk sample. This analysis identified 9 items as a single factor solution that fit the data well (TLI=0.938, CFI=0.958, RMSEA=0.06; Pathways to Desistance Study, n.d.). These 9 items were then carried forward across all waves. Items included “I know things to do to make myself more happy,” and “I can change my feelings by thinking of something else” (Mulvey et al., 2004). Responses were measured using a 4-point Likert scale (1 = “Not at all like me”, 4 = “Really like me”; M = 2.81, SD = .68, alpha = .81).
Lifetime Depression Symptoms.
Binary depressive history was assessed using 6 Brief Symptom Inventory (BSI) items targeting lifetime history of depression-related symptoms (Derogatis & Melisaratos, 1983). Items include “ever” having experienced “feeling no interest in things” or “feeling hopeless about the future” (0 = “not-at-all”, 4 = “extremely). These six items were averaged and T-scored by the Pathways study original authors (Mulvey et al., 2004). These T-scored averages were then binarized using gender-specific cut-offs provided by the BSI authors (Derogatis & Melisaratos, 1983; Pathways to Desistence, n.d.).
A dichotomous outcome was ideal given that our hypotheses concerned the relationship between ER and psychopathology rather than predicting incremental variance above and below clinically significant depression levels. In other words, the authors were specifically concerned with the predictors of clinically significant depression. Past research has found the BSI to have strong internal consistency (Cronbach’s alpha between 0.71 and 0.85) and strong test-retest reliability (r = 0.68 to 0.91; Derogatis & Melisaratos, 1983). The BSI is considered a reliable and appropriate measure of psychopathology capable of identifying and discriminating between depression and anxiety (Skeem et al., 2006).
Lifetime Anxiety Symptoms.
The 6 BSI items measuring individual differences in lifetime history of anxiety symptoms were administered at baseline (BSI, Derogatis & Melisaratos, 1983). The anxiety subscale consists of symptoms associated with anxiety, restlessness, nervousness, etc. (Derogatis & Melisaratos, 1983). Example items include the extent to which the participant had ever experienced “Feeling tensed or keyed up” or “Spells of terror or panic”, rated on a scale of 0–4 (Mulvey et al., 2004). Identically to the depression scores, clinically significant anxiety was classified as a binary score (0 = not clinically significant, 1 = clinical range) using a T-scored average of these six-items that was compared to gender-specific cut-off scores (Derogatis & Melisaratos, 1983).
Lifetime Substance Dependence Symptoms.
Individual differences in substance dependence symptoms were assessed using the dependence scale of the Substance Use/Abuse Inventory, which is a modified version of the measure created by Chassin, Rogosch, and Barrera (1991). The dependence scale is a 10-item questionnaire measuring the extent to which the participants had ever experienced substance dependence symptoms in their lifetime. Items are quite similar to the DSM symptom criteria for clinically significant substance use. Items include: “have you ever given up or cut your usual activities or interests like sports, work, or seeing family or friends in order to drink or use drugs?” (1 = yes, 0 = no) or “…have you ever wanted a drink or drugs so badly that you could not think about anything else?” (Chassin et al., 1991). These binary items were then summed to create a total symptom score for each individual.
Because the present investigation is focused on understanding the etiology and outcomes of clinically significant symptoms, we sought to binarize these symptom totals. To our knowledge, however, well-established clinical significance cut-off scores do not exist for this scale. Thus, a cutoff score of 3 or greater significant dependence symptoms was selected a-priori. This score was selected because it (a) is quite consistent with the DSM-5 procedure for classifying mild/moderate substance use disorder based on the presence of 3 key symptoms (American Psychiatric Association, 2013), (b) represented approximately 1 standard deviation above the current sample mean, and (b) because it yielded an average dependence classification rate of ~ 9.7% for combined drugs and/or alcohol, a rate which approximates the expected prevalence of clinical substance dependence in an adolescent population (e.g., Kessler et al., 1994).
Wave-to-Wave Fluctuations in ER and Symptoms
Emotion Regulation Ability.
At each of 10 follow-up waves, recent experiences of emotion regulation ability were assessed using modified versions of the items included in the baseline trait measure. Follow-up questions were identical but targeted ER experiences occurring “since the last assessment” (either 6 months for waves 1 through 6, or 12 months for waves 7 through 10; Pathways to Desistence Study, n.d.).
Clinically Significant Symptoms.
At each follow-up wave, binary scores were calculated for significant depressive, anxiety, and substance abuse symptoms. Follow-up symptom items were identical to those descried in the baseline protocol, but targeted symptoms experienced since the last assessment.
Statistical Approach
Our research questions involved prospective within and between person processes, including potential bidirectional processes unfolding over time. Questions of this type can be examined simultaneously using a longitudinal SEM variant known as random intercepts cross-lagged panel modeling (RI-CLPM; Hamaker et al. 2015). RI-CLPM is a variant of the more traditional CLPM but deconflicts within-person processes from more stable between-person processes. It does so by calculating latent intercepts which estimate and parse out stable individual differences in the dynamic (i.e., repeated) outcome variables measured repeatedly across waves (see Hamaker et al. (2015) for a detailed review). In RI-CLPMs, between person processes can be assessed using disposition measures entered as time-invariant predictors of future latent intercepts, and within person processes can be assessed via person-centered cross-lagged relationships (see Allemand, & Hill 2019 for a similar approach). In the present RI-CLPMs, we were primarily interested in two effects. First, the cross-lagged associations between symptoms and ER at each wave, while controlling for concurrent covariance, lag 1 autoregressive effects, and individual differences in both outcomes and predictors. Given these controls, these cross-lagged effects can be interpreted as within-person changes in predictors impacting lag 1 changes in outcomes (Hamaker et al. 2015).
Importantly, though, estimating true prospective relationships using lag 1 effects alone is fraught with challenges related to the unique and varied temporal dynamics of the constructs being studied (Dormann & Griffin, 2015). For this reason, lag 1 results can fail to reveal prospective relationships that occur over time-scales other than the somewhat arbitrary lag 1 time period (Dormann & Griffin, 2015). Developmental changes in trait-like ER ability, for instance, may confer risk for future psychopathology over a much longer time scale that six months, or may have a cumulative impact on mental health risk that takes years to manifest. Lower ER ability could also impact future psychopathology as a function of an unmeasured third variable that occurs at different time lags for different people (e.g., a traumatic life event). Moreover, smaller fluctuations in ER ability captured by lag 1 effects may matter less than the impact of more stable individual differences in dispositional ER ability. To address these possibilities, we also tested a simplified prospective relationship between dispositional ER or symptoms (measured at baseline) as predictors of future individual differences in average symptoms or average ER occurring over the course of the entire study. These individual differences were modeled via latent intercepts which summarized 10 follow-up measures of ER or symptom status. Importantly, these longer-term between-person associations also controlled for baseline covariance between ER and pathology, as well as autoregressive effects. Importantly, the present models also controlled for gender. See Figure 1 for an example of one such RI-CLPM.
Figure 1.
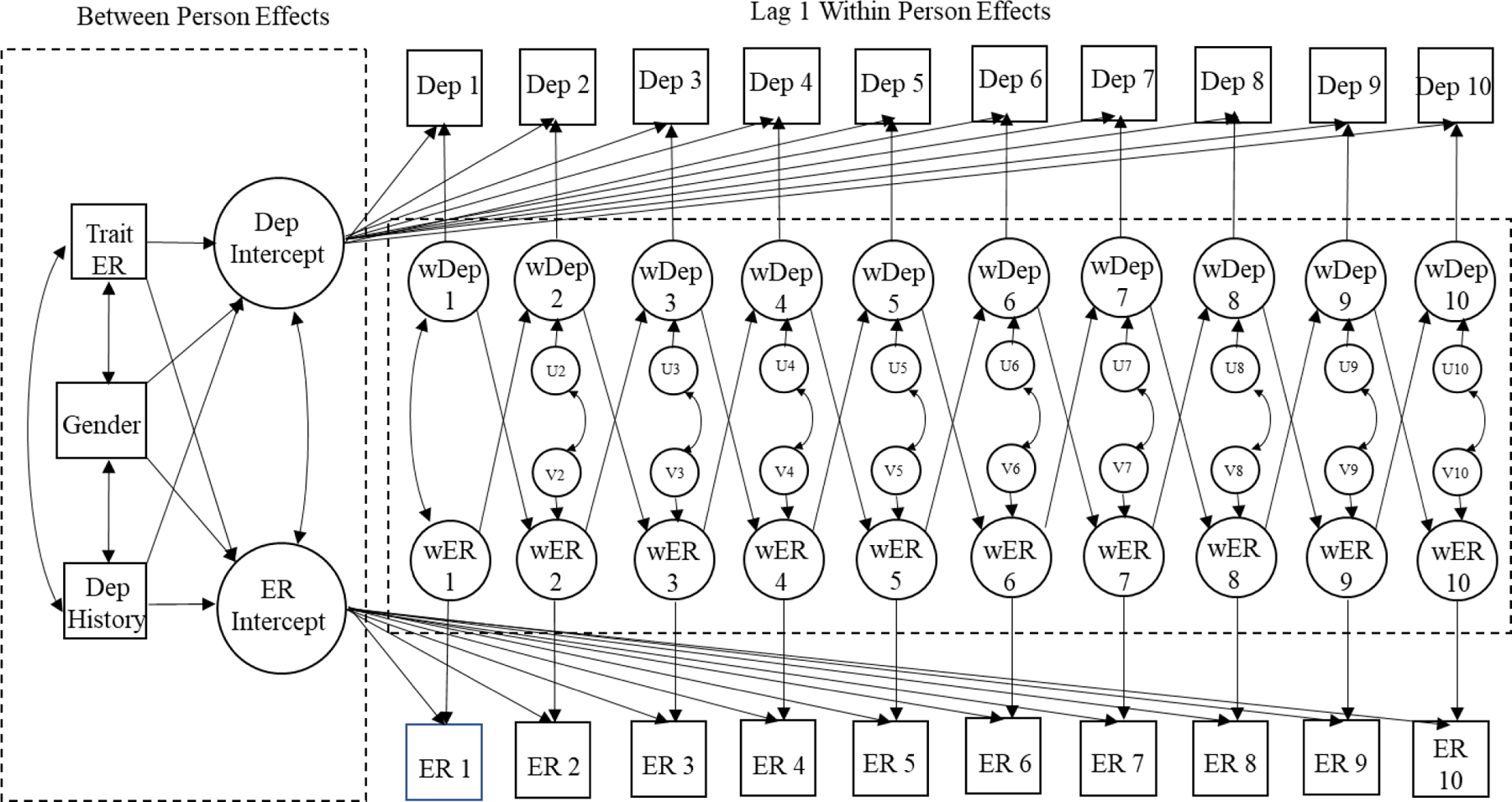
Final RI-CLPM (M3) for ER and Depression
Modeling Strategy
Using the lavaan (Rosseel, 2012) package within R (R Core Team, 2020; RStudio Team 2019), a series of RI-CLPMs were fitted for each of the three clinical outcomes. For each outcome, an initial model (designated M1) examined cross-lagged relationships between ER and wave-to-wave fluctuations in symptoms across the 10 study waves. Following convention, these models included fully unconstrained grand within-wave means, latent intercept means, autoregressive effects, cross-lagged effects, and residual correlations (Hamaker et al., 2015)]. Next, to explicitly quantify the role that individual differences in ER and symptoms had in the present data, a second set of RI-CLPMs (M2) were fitted in which variances in latent intercepts (both for ER and symptoms) were fixed to zero. This model assumes no stable individual differences in ER or clinical symptoms during the study (cf. Hamaker et al., 2015; Usami et al., 2019), and therefore serious misfit would suggest that meaningful (and relatively stable) individual differences exist in ER and symptomology assessed during follow-up waves (e.g., Allemand, & Hill 2019). To address potential misfit in M2s, a third model type (designated M3) was included that returned to unconstrained intercept variance parameters (i.e., M1) but added dispositional ER and lifetime symptomology measured at baseline as prospective predictors of these individual differences in latent ER or symptom intercepts. This inclusion of lifetime/dispositional measures as prospective predictors of individual differences in outcomes enabled us to identify potential longitudinal effects that did not occur solely within the lag 1 timeframe. Importantly, M3 also included gender as time-invariant predictor of future intercepts (see figure 1 for an M3 example).
Missing Data
Of the 1354 participants who completed the Pathways study, our models excluded 92 individuals who did not report manifest variables for lifetime history of pathology symptoms or ER ability. Compared to retained participants, dropped individuals reported slightly higher ER ability during follow-ups (r = .08, p = .004), slightly less clinical substance abuse levels (r = −.07, p = .007), and did not differ in terms of depression or anxiety.
Among those included in the final models, average percentage of missing data was not meaningfully related to average emotion regulation (r = .03), clinically significant depression (r = −.01), or anxiety (r = −.02), and was slightly associated with less substance dependence symptoms (r = −.08, p = .009). See Appendix B for detailed information on missingness rates and correlations with all variables of interest. Missing data were estimated using full information maximum likelihood, a procedure that is thought to be a reliable and valid (Ji et al., 2018). To evaluate model fit, we principally relied on the comparative fit index (CFI; values larger than .90 indicate good fit), and the root mean square error of approximation (RMSEA) where values below .06 indicate good fit and values below .08 represent acceptable fit (Finch & West, 1997; Marsh, Hau, & Wen, 2004).
Finally, to estimate the hypothesized effects on outcome variables that were both continuous (ER follow-ups) and binary (symptom status follow-ups), robust maximum likelihood estimation was used. We chose this approach because previous Monte Carlo simulations have shown that this procedure is capable of estimating unbiased parameters in binary, categorial, and non-normal endogenous distributions (Bandalos, 2014; Kupek, 2005).
Results
Descriptive statistics for our RI-CLPMs can be found in table 1, including bivariate correlations (see Appendix A for complete bivariate correlations). These correlations reveal the expected concurrent and prospective associations between dispositional ER and symptoms.
Table 1.
Descriptive Statistics and Bivariate Correlations
| Covariate | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Trait ER | 1 | −.07* | −.06* | −.05 | −.08* | −.09* | −.12* | .36* |
| 2. History Dep | 1 | .48* | .11* | .26* | .26* | .08* | −.04 | |
| 3. History Anx | 1 | .12* | .21* | .28* | .11* | −.04 | ||
| 4. History Sub | 1 | .06* | .11* | .32* | −.05 | |||
| 5. Follow-up Dep | 1 | .61* | .22* | −.09* | ||||
| 6. Follow-up Anx | 1 | .22* | −.05 | |||||
| 7. Follow-up Sub | 1 | −.16* | ||||||
| 8. Follow-up ER | 1 | |||||||
|
| ||||||||
| MEAN | 2.76 | .08 | .05 | .18 | .04 | .03 | .09 | 2.55 |
| SD | .66 | .27 | .22 | .38 | .11 | .09 | .15 | .47 |
Note.
p < .05
Table 2 shows fit statistics for all models. M1s fit the data well, and M2s showed robust reductions in fit, suggesting that individual differences in ER or pathology reported during the 10 follow-up assessments were an important aspect of the data (cf. Allemand & Hill, 2019). Given these results, we were confident that M3 would provide the most comprehensive understanding of any prospective relationships that existed in the data. All Model 3s fit the data and supported our between-person hypotheses in each symptom cluster.
Table 2.
Model fits for all RI-CLPMs
| Model Type | Adj. χ2 | df | CFI | RMSEA |
|---|---|---|---|---|
| Depression Models | ||||
| M1- unconstrained RI-CLPM | 355.99 | 141 | .958 | .035 |
| M2- M1 without individual differences in RI¥ | 1378.97 | 143 | .760 | .083 |
| M3- M1 with lifetime ER or symptomsƚ | 499.24 | 195 | .946 | .035 |
| Anxiety Models | ||||
| M1- unconstrained RI-CLPM | 400.77 | 141 | .949 | .038 |
| M2- M1 without individual differences | 1430.11 | 143 | .749 | .085 |
| M3- M1 with individual differences added | 546.59 | 195 | .938 | .038 |
| Substance Abuse Models | ||||
| M1- unconstrained RI-CLPM | 343.07 | 141 | .966 | .033 |
| M2- M1 without individual differences | 1672.24 | 143 | .744 | .090 |
| M3- M1 with individual differences added | 506.71 | 195 | .953 | .034 |
Note. Adj. χ2, adjusted chi-square test statistic (MLR estimator); df, degree of freedom; CFI, comparative fit index; RMSEA, root mean square error of approximation.
The variances of the random intercepts and were constrained to zero.
Added dispositional ER and lifetime symptoms as predictors of latent intercepts.
Within-person Fluctuations During the Transition to Adulthood
Final Models (M3) did not reveal consistent relationships between fluctuations in ER ability and prospective lag 1 changes in symptoms, nor did they reveal relationships between changes in symptoms and future changes in ER ability (see Table 3 for all within-person parameter results).
Table 3.
Summary of Person-Centered Effects in M3s: Standardized Estimates of Cross-lagged, Autoregressive, and Concurrent Effects
| Wave(s) | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 to 2 | 2 to 3 | 3 to 4 | 4 to 5 | 5 to 6 | 6 to 7 | 7 to 8 | 8 to 9 | 9 to 10 | |||||||||||||
| Cross-lagged Effects | |||||||||||||||||||||
| ER predicting Depression | −.05 (.02) | .04 (.01) | −.06 (.02) | −.01 (.02) | −.07 (.02) | −.03 (.02) | −.02 (.02) | .04 (.01) | −.11 (.02) * | ||||||||||||
| Depression Predicting ER | .03 (.10) | −.06 (.09) | .00 (.15) | −.06 (.13) | .05 (.13) | −.06 (.13) | −.08 (.12) | −.07 (.11) * | .09 (.12) * | ||||||||||||
| ER predicting Anxiety | −.01 (.01) | .02 (.01) | −.07 (.02) | .04 (.01) | −.01 (.02) | −.02 (.01) | −.05 (.02) | .00 (.02) | −.04 (.01) | ||||||||||||
| Anxiety predicting ER | −.01 (.13) | −.06 (.13) | −.03 (.19) | −.06 (.15) | .06 (.13) | −.08 (.14) | .00 (.15) | −.06 (.13) | .03 (.16) | ||||||||||||
| ER predicting Dependence | −.04 (.01) | −.04 (.02) | −.02 (.02) | .04 (.01) | −.01 (.02) | −.02 (.02) | .00 (.02) | −.05 (.02) | −.02 (.02) | ||||||||||||
| Dependence predicting ER | −.04 (.06) | −.04 (.07) | .02 (.06) | −.08 (.06) * | .04 (.07) | −.02 (.08) | −.02 (.07) | −.02 (.07) | .05 (.06) | ||||||||||||
| Autoregressive Effects | |||||||||||||||||||||
| ER£ | .17 (.03) * | .16 (.04) * | .15 (.04) * | .10 (.05) * | .25 (.04) * | .16 (.04) * | .18 (.04) * | .26 (.04) * | .23 (.04) * | ||||||||||||
| Depression | .22 (.08) * | .12 (.06) | .11 (.10) | .17 (.08) * | .21 (.10) * | .09 (.08) | .19 (.08) * | .16 (.07) * | .08 (.09) | ||||||||||||
| Anxiety | .10 (.09) | .16 (.07) | .34 (.12) * | .20 (.09) * | .18 (.10) | .06 (.10) | .13 (.10) | .05 (.09) | .15 (.09) | ||||||||||||
| Sub Dependence | .09 (.05) | .16 (.06) * | .11 (.06) * | .10 (.05) * | .15 (.06) * | .08 (.05) | .22 (.05) * | .18 (.05) * | .19 (.05) * | ||||||||||||
| Concurrent Covariation | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |||||||||||
| ER and Depression | −.10 (.00) * | −.02 (.00) | .00 (.00) | −.08 (.00) | −.05 (.00) | −.07 (.01) | −.15 (.01) * | −.16 (.00) * | −.20 (.01) * | −.11 (.01) * | |||||||||||
| ER and Anxiety | −.04 (.00) | −.03 (.00) | .04 (.00) | .01 (.00) | −.04 (.00) | .02 (.00) | −.05 (.00) | −.16 (.00) * | −.12 (.00) * | −.09 (.01) | |||||||||||
| ER and Dependence | −.05 (.01) | −.04 (.00) | −.02 (.00) | −.08 (.00) * | .04 (.00) | .02 (.00) | −.04 (.01) | .01 (.00) | −.07 (.00) * | −.05 (.00) | |||||||||||
Note. Standard errors indicated by parentheses.
p < .05
ER coefficients taken from Depression M3 model. Estimates were not meaningfully different in anxiety or substance M3s
Baseline Traits or Lifetime History and Future Outcomes
Final Models (M3) supported the present between person hypotheses, but did not reveal bi-directional effects. Gender was also not a significant predictor of future symptoms or ER. In all three interactions of M3, we find that dispositional ER ability was negatively related to latent symptom intercepts for clinically significant depression, anxiety, and substance dependence symptoms. Thus, we show that individuals reporting lower dispositional ER ability were at increased risk for developing clinically significant symptoms at some point during the 7-year transition to adulthood (see Table 4 for all parameter results). Importantly, these prospective effects are indicated by significant partial regression coefficients that controlled for the predictive effects of lifetime symptom history on future latent symptom intercepts as well as covariance between ER and symptoms at baseline. This effect can be understood as akin to Granger causality (Granger, 1969). In addition, although these reported analyses controlled for binary baseline symptoms, none of the present between-person effect patterns changed when we replaced binary lifetime symptom history with a dimensional form of symptoms peopled tended to experience prior to the study. These dimensional history results increased confidence that we had adequately accounted for autoregressive effects of baseline symptoms as well as covariance between trait ER and life history symptoms.
Table 4.
Between-Person Predictive Effects
| Life History/Dispositional Predictor | Latent Outcome | SE | z | Standardized Estimate & 95% CI |
|---|---|---|---|---|
| Dispositional ER | Follow-up Depressive Status | .04 | −3.52 | −.14** (−.06 to −.22) |
| Dispositional ER | Follow-up Anxiety Status | .04 | −2.54 | −.11* (−.02 to −.19) |
| Dispositional ER | Follow-up Dependence Status | .03 | −3.83 | −.12***(−.06 to −.19) |
| Depression History | Follow-up ER ability | .03 | −1.03 | −.03 (.03 to −.09) |
| Anxiety History | Follow-up ER ability | .03 | −.59 | −.02 (.04 to −.07) |
| Dependence History | Follow-up ER ability | .03 | −1.31 | −.03 (.02 to −.08) |
| Gender (male = 1) | Follow-up ER ability | .03 | −.74 | −.02 (.04 to −.08) |
| Gender | Follow-up Depressive Status | .04 | 1.11 | .05 (.13 to −.04) |
| Gender | Follow-up Anxiety Status | .04 | 1.84 | .08 (.17 to −.01) |
| Gender | Follow-up Dependence Status | .04 | 1.82 | .07 (.14 to −.01) |
Note.
p < .05
p < .01
p < .001
Discussion
Transdiagnostic frameworks have suggested that the ability to manage emotions represents a key modulator of risk for the development of both internalizing and externalizing disorders. Such theories, however, are undermined by a lack of direct evidence of prospective links between ER and future clinical symptoms. In addition, there is reason to expect a bidirectional relationship between ER and symptomology (e.g., Cludius et al., 2020). The present analysis investigated these prospective (potentially reciprocal) associations using both 1) relatively short-term within-person fluctuations in ER or symptoms, as well as 2) between-person analyses of disposition indicators conferring risk for future symptoms or decreased ER ability over a longer time scale. This between-person analysis is critical because a sole emphasis on lag 1 changes in predictors may not capture prospective effects that occur at shorter or longer time-scales (Dormann & Griffin, 2015).
Given that lag 1 effects in RI-CLPMs are typically interpreted as quantifying the impact of changes in predictors on changes in outcomes (e.g., Hamaker et al. 2015), the present results did not show evidence of predictive effects of lag 1 fluctuations in ER on next-wave fluctuations in symptoms. There was also no evidence for lag 1 changes in symptom status predicting future changes in ER. In support of our hypotheses, however, between-person analyses showed that greater baseline ER ability was predictive of less relative risk for developing clinically significant depression, anxiety, and substance dependence over the 7-years follow-up period of the study. Additionally, these prospective between-person analysis showed no evidence of a reciprocal effect where a lifetime history of clinically significant symptoms predicted relative future ER ability levels.
Implications
The most important implication of these longitudinal results is that they represent some of the strongest evidence to date to support transdiagnostic theories (Aldao et al., 2010; Sloan et al., 2017; Aldao, 2012; Carpenter & Trull, 2013; Gratz et al., 2015) which suggest that ER ability plays a causal role in the development of both distress-based and substance abuse disorders. These findings in a large sample assessing clinical pathology across the critical period of adolescence to adulthood should also strengthen the case for transdiagnostic treatments such as the Unified Protocol (Barlow et al., 2017) that emphasize affect regulation skills. Transdiagnostic theories like the UP propose that learning to manage emotions should treat and prevent multiple prevalent disorders simultaneously. These theories are compelling because they could change the way that mental illnesses are conceptualized and treated (Norton & Phillip, 2008).
Relatedly, the present results suggest that ER-focused training could be effective in treating individuals who develop comorbid depression and substance use disorders. From a public policy perspective, these are critical findings which should suggest to caregivers, educators, and policy-makers that an environment conducive to the development of ER ability/skills could have simultaneous prevention and treatment benefits across some of the most prevalent forms of mental illness.
The present prospective link between ER and future substance dependence is also significant given the conflicting theories concerning the temporal relationship between excessive substance use and dysregulated emotion. Although many researchers suggest that use/abuse is commonly caused by an attempt to escape dysregulated negative emotion (Khantzian, 1997; Kober, 2014), much of the relevant evidence is essentially cross-sectional. Studies explicitly attempting to evaluate the temporal relationship between dysregulated negative affect (e.g., depression) and substance use have often been inconclusive (Bromberger et al., 2009; Grant et al, 2009). And, some have found evidence for substance use preceding pathologically dysregulated affect (Rohde et al., 2001). For instance, Rohde et al., (2001) found that individuals with an adolescent alcohol use disorder were more likely to develop future major depressive disorder. Relatedly, some day-to-day investigations have suggested a bidirectional relationship between emotional difficulties and substance use (Weiss et al., 2017). Our data, which clearly looks at the question from a much longer timeframe, does not find statistical evidence for such a bidirectional relationship. In general, the present data supports existing perspectives that suggest that an inability to regulate one’s emotions may be a key risk factor for future substance use (Kober, 2014).
Given the present sociodemographically diverse sample, our findings also provide evidence for the generalizability of theory linking ER to mental health risk to at-risk populations. Increased knowledge of risk factors among low SES populations is crucial given that underprivileged demographics have been at greater risk for developing mental health problems (e.g., Goodman et al., 2003). Such groups could also benefit from the development of transdiagnostic disorder-agnostic treatments that can be delivered more efficiently, with less provider training, and at lower cost (Barlow et al., 2017).
Limitations and Future Directions
Although our results provide evidence of ER modulating future symptoms, these findings should not be interpreted as direct evidence of causality. Our results would be expected, however, if theories suggesting a causal association were valid. In addition, although the present within person (6 month or 1-year lags) and between person regressions do not show evidence of a prospective effect symptoms on ER ability, this pattern should not suggest that there is no such effect. It may be that such an effect is present, but manifests over different time-scales than those assessed here. For instance, an increase in depressive symptoms brough on by some stressor my cause a relatively immediate decrease in ER ability. Future research could capture such an effect if more micro timescales were employed in longitudinal research (Dormann & Griffin, 2015).
The present sample has clear strengths, such as a large and diverse sample, a large number of waves, low attrition rates, and the ability to prospectively predict the development of multiple forms of psychopathology over time. The present time frame is also a key one—we track psychological development through the critical transition period of later adolescence into young adulthood (Ahmed, Bittencourt-Hewitt, & Sebastian, 2015). It should be stated that the present sample focuses on at-risk youth, and so it is possible that the results will not generalize to typical adolescents/young adults. However, rates of depression, anxiety, and substance dependence in the present youth sample were quite similar to youth prevalence estimates of diagnosed anxiety (10%), depression (6%), and substance abuse (15%) based on nationally representative youth samples (Swenson et al., 2012; Center for Disease Control and Prevention, 2020). At-risk and minority groups are also historically underrepresented in scientific samples, and we consider it a strength rather than a weakness to better understand such populations. Future research should replicate the present findings in a normative sample, and potentially focus on shorter lags (e.g., 1 week). Given the present findings in a low SES population, we hope that our research encourages future investigations among underrepresented and disadvantaged groups. Specifically, we hope to stimulate investigations testing digital transdiagnostic interventions that can be delivered remotely at scale with reduced cost and burden to patients.
An additional limitation of this study is that the sample is mostly male (86%), which could limit generalizability. However, we control for participant gender in all models, and gender did not interact with our key findings. In a further potential limitation, mental health status was assessed using self-reported scales rather than in-person interviews. However, an assessment approach that was low-burden and could be reproduced efficiently over 11 waves was required, and the BSI is a widely used scale thought to be a valid tool for identifying clinically significant depression and anxiety (e.g., Skeem et al., 2006). Lastly, the present ER scale does not deconstruct ER ability into specific behavioral elements such as the use of emotional suppression/avoidance. The present analysis, however, controlled for concurrent covariance between ER ability and symptoms, which should help with potential confounds between generalized ER ability and clinical symptoms. In addition, this generalized approach was designed to yield the most valid ER assessments in youth, who may possess less specific emotion-related self-knowledge (Walden et al., 2003).
Conclusions
These findings provide important new evidence suggesting that the ability to regulate one’s emotions may modulate risk for the development of clinically significant depressive, anxiety, and substance dependence symptoms during the critical period of transition to adulthood.
Acknowledgments
This research is supported in part by T32 (T32DA037202–07) and P30 (P30DA029926) grants provided by the National Institute of Drug Abuse (NIDA), along with the Kaminsky Undergraduate Research Award. The present data is drawn from the Pathways to Desistance Study, a project made possible by the Arizona Governor’s Justice Commission, the MacArthur Foundation, NIDA grant # R01 DA 019697 05, NIJ grant # 2008-IJ-CX-0023, OJJDP grant # 2005-JK-FX-K001, the Pennsylvania Commission on Crime & Delinquency, the Robert Wood Johnson Foundation, the William Penn Foundation, and the William T. Grant Foundation.
Appendix A
Zero-order Correlations Between All 44 Manifest Variables, Divided into Three Tables.
Table 3a.
Please note that Row 1 shifts right for all table 3s, and column 1 is identical.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. ER Baseline | 1 | ||||||||||||||
| 2. ER 1 | .42*** | 1 | |||||||||||||
| 3. ER 2 | .41*** | .47*** | 1 | ||||||||||||
| 4. ER 3 | .40*** | .44*** | .53*** | 1 | |||||||||||
| 5. ER 4 | .33*** | .39*** | .50*** | .55*** | 1 | ||||||||||
| 6. ER 5 | .34*** | .39*** | .45*** | .53*** | .51*** | 1 | |||||||||
| 7. ER 6 | .29*** | .37*** | .43*** | .50*** | .51*** | .58*** | 1 | ||||||||
| 8. ER 7 | .30*** | .31*** | .36*** | .41*** | .43*** | .47*** | .52*** | 1 | |||||||
| 9. ER 8 | .27*** | .27*** | .37*** | .41*** | .42*** | .42*** | .46*** | .50*** | 1 | ||||||
| 1. ER 9 | .27*** | .29*** | .34*** | .37*** | .39*** | .41*** | .41*** | .44*** | .51*** | 1 | |||||
| 11. ER SA | .29*** | .26*** | .32*** | .36*** | .36*** | .36*** | .44*** | .42*** | .46*** | .47*** | 1 | ||||
| 12. Depression Baseline | −.07* | −.08** | −.06 | −.06* | −.08** | −.03 | −.05 | −.02 | −.04 | .00 | .01 | 1 | |||
| 13. Depression 1 | −.05 | −.09** | −.02 | .01 | .02 | .02 | .01 | −.02 | −.01 | −.02 | −.01 | .27*** | 1 | ||
| 14. Depression 2 | −.06 | −.10** | −.06 | −.08* | −.09** | −.02 | −.02 | −.06 | .02 | −.04 | −.03 | .19*** | .35*** | 1 | |
| 15. Depression 3 | −.09** | −.08* | −.03 | −.05 | −.06 | .00 | −.06 | −.08* | .03 | .01 | −.05 | .10** | .15*** | .25*** | 1 |
| 16. Depression 4 | −.06 | −.11** | −.07 | −.08* | −.10** | −.07* | −.04 | −.02 | −.01 | −.04 | .04 | .14*** | .06 | .14*** | .22*** |
| 17. Depression 5 | −.05 | −.05 | −.03 | −.05 | −.04 | −.06 | −.02 | −.05 | −.03 | −.05 | −.02 | .14*** | .13*** | .25*** | .16*** |
| 18. Depression 6 | −.08* | −.04 | −.07* | −.10** | −.04 | −.09* | −.08* | −.09** | −.08* | −.04 | −.05 | .13*** | .10** | .10** | .21*** |
| 19. Depression 7 | −.06 | .02 | −.03 | −.01 | −.03 | −.03 | −.05 | −.13*** | −.09* | −.09** | −.10** | .12*** | .23*** | .19*** | .07 |
| 2. Depression 8 | −.07 | .02 | −.04 | −.01 | −.02 | −.07* | −.03 | −.06 | −.14*** | −.10** | −.07 | .14*** | .15*** | .13*** | .15*** |
| 21. Depression 9 | −.07* | −.10** | −.07* | −.10** | −.11** | −.08* | −.07* | −.09** | −.05 | −.20*** | −.04 | .10** | .05 | .20*** | .19*** |
| 22. Depression 10 | −.04 | −.02 | −.05 | −.02 | −.04 | .00 | −.03 | .01 | −.08* | −.12** | −.11** | .06 | .09* | .10* | .08 |
| 23. Anxiety Baseline | −.06 | −.07* | −.02 | −.06* | −.04 | −.05 | −.05 | .00 | .01 | .01 | −.02 | .48*** | .25*** | .18*** | .07* |
| 24. Anxiety 1 | −.04 | −.03 | −.02 | −.03 | .04 | .00 | .02 | −.01 | .03 | −.01 | .01 | .20*** | .40*** | .17*** | .09* |
| 25. Anxiety 2 | −.04 | −.02 | −.03 | −.05 | −.02 | .00 | −.02 | .00 | .06 | −.01 | .03 | .19*** | .14*** | .48*** | .27*** |
| 26. Anxiety 3 | −.03 | −.01 | −.01 | .01 | −.04 | −.03 | −.03 | −.04 | .04 | −.01 | −.06 | .07* | .18*** | .21*** | .47*** |
| 27. Anxiety 4 | −.04 | −.05 | −.05 | −.06 | −.04 | −.07 | −.09** | −.04 | .03 | −.02 | −.04 | .03 | .09* | .15*** | .41*** |
| 28. Anxiety 5 | −.07 | −.01 | −.06 | −.02 | .00 | −.05 | .00 | −.05 | −.04 | −.02 | .03 | .16*** | .14*** | .07 | .15*** |
| 29. Anxiety 6 | −.06 | −.01 | −.06 | −.01 | −.02 | −.03 | −.01 | −.08* | −.05 | −.01 | −.05 | .16*** | .13*** | .05 | .08* |
| 3. Anxiety 7 | −.03 | .01 | −.01 | .03 | −.01 | .00 | −.02 | −.05 | .00 | .02 | −.07 | .09** | .04 | .00 | .07 |
| 31. Anxiety 8 | .00 | .03 | .00 | .01 | −.04 | −.06 | −.02 | −.06 | −.12*** | −.08* | −.07 | .22*** | .20*** | .13*** | .14*** |
| 32. Anxiety 9 | −.08* | −.08* | −.06 | −.07 | −.13*** | −.09* | −.09* | −.09** | −.07 | −.14*** | −.08* | .13*** | .09* | .25*** | .18*** |
| 33. Anxiety SA | −.09* | −.04* | −.08 | −.06 | −.11** | −.10** | −.11** | −.08* | −.08* | −.11** | −.14*** | .07 | .11** | .10* | .08 |
| 34. Dependence Baseline | −.05 | −.07* | −.03 | −.07* | −.06* | −.05 | −.04 | −.03 | −.05 | −.03 | −.05 | .11*** | .02 | .06* | −.02 |
| 35. Dependence 1 | −.06* | −.11*** | −.10*** | −.07* | −.07* | −.06* | −.08** | −.08** | −.03 | −.06* | −.08** | .06* | .06* | .11*** | .17*** |
| 36. Dependence 2 | −.09** | −.12*** | −.11*** | −.11*** | −.10*** | −.12*** | −.10*** | −.06* | −.04 | −.08* | −.06 | .06* | .02 | .11*** | .08* |
| 37. Dependence 3 | −.07* | −.08** | −.10** | −.09** | −.06 | −.08** | −.06* | −.06* | −.06* | −.03 | −.08* | .05 | −.01 | .07* | .1** |
| 38. Dependence 4 | −.09** | −.10*** | −.09** | −.08** | −.13*** | −.14*** | −.14*** | −.08** | −.06* | −.05 | −.02 | .04 | .00 | .10** | .15*** |
| 39. Dependence 5 | −.05 | −.07* | −.06* | −.02 | −.03 | −.05 | −.04 | −.12*** | −.02 | −.04 | −.03 | .06 | −.03 | .10** | .03 |
| 4. Dependence 6 | −.04 | −.08** | −.09** | −.08* | −.09** | −.07* | −.05 | −.08** | −.05 | −.03 | −.04 | .02 | .04 | .07* | .05 |
| 41. Dependence 7 | −.06* | −.08** | −.04 | −.02 | −.01 | −.06* | −.07* | −.09** | −.07* | −.07* | −.09* | .04 | .07 | .04 | .07* |
| 42. Dependence 8 | −.08** | −.08** | −.06* | −.06* | −.04 | −.08** | −.04 | −.08** | −.05 | −.06* | −.09** | .09** | .02 | .10** | .11** |
| 43. Dependence 9 | −.08** | −.09*** | −.09** | −.12*** | −.11*** | −.10*** | −.11*** | −.10*** | −.12*** | −.13*** | −.05 | .04 | .03 | .11*** | .10** |
| 44. Dependence 10 | −.06* | −.07* | −.05 | −.02 | −.05 | −.07* | −.07* | −.02 | −.05 | −.06 | −.08* | .06 | .03 | .11** | .14*** |
Table 3b.
Correlation Matrix Part 2.
| 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | 29 | 30 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. ER Baseline | |||||||||||||||
| 2. ER 1 | |||||||||||||||
| 3. ER 2 | |||||||||||||||
| 4. ER 3 | |||||||||||||||
| 5. ER 4 | |||||||||||||||
| 6. ER 5 | |||||||||||||||
| 7. ER 6 | |||||||||||||||
| 8. ER 7 | |||||||||||||||
| 9. ER 8 | |||||||||||||||
| 1. ER 9 | |||||||||||||||
| 11. ER SA | |||||||||||||||
| 12. Depression Baseline | |||||||||||||||
| 13. Depression 1 | |||||||||||||||
| 14. Depression 2 | |||||||||||||||
| 15. Depression 3 | |||||||||||||||
| 16. Depression 4 | 1 | ||||||||||||||
| 17. Depression 5 | .32*** | 1 | |||||||||||||
| 18. Depression 6 | .28*** | .36*** | 1 | ||||||||||||
| 19. Depression 7 | .03 | .16*** | .24*** | 1 | |||||||||||
| 2. Depression 8 | .21*** | .25*** | .30*** | .32*** | 1 | ||||||||||
| 21. Depression 9 | .21*** | .23*** | .23*** | .17*** | .31*** | 1 | |||||||||
| 22. Depression 10 | .04 | .08 | .13** | .18*** | .21*** | .25*** | 1 | ||||||||
| 23. Anxiety Baseline | .12*** | .20*** | .14*** | .12*** | .09* | .11** | .04 | 1 | |||||||
| 24. Anxiety 1 | .11** | .21*** | .13*** | .07 | .10** | .00 | .01 | .19*** | 1 | ||||||
| 25. Anxiety 2 | .07 | .18*** | .10* | .03 | .04 | .10** | .04 | .22*** | .22*** | 1 | |||||
| 26. Anxiety 3 | .19*** | .31*** | .10* | .01 | .12** | .20*** | .01 | .14*** | .29*** | .29*** | 1 | ||||
| 27. Anxiety 4 | .38*** | .28*** | .22*** | .04 | .16*** | .13** | .01 | .11** | .23*** | .23*** | .50*** | 1 | |||
| 28. Anxiety 5 | .31*** | .55*** | .24*** | .16*** | .27*** | .12** | .07 | .19*** | .23*** | .13*** | .30*** | .34*** | 1 | ||
| 29. Anxiety 6 | .15*** | .34*** | .41*** | .21*** | .25*** | .16*** | .06 | .26*** | .22*** | .09* | .11** | .23*** | .35*** | 1 | |
| 3. Anxiety 7 | .06 | .10* | .09* | .30*** | .09* | .06 | .24*** | .10** | .02 | −.03 | .04 | .07 | .18*** | .19*** | 1 |
| 31. Anxiety 8 | .13** | .17*** | .19*** | .31*** | .38*** | .15*** | .22*** | .25*** | .13*** | .10** | .14*** | .24*** | .24*** | .26*** | .23*** |
| 32. Anxiety 9 | .21*** | .16*** | .13** | .21*** | .27*** | .56*** | .22*** | .15*** | .04 | .12** | .23*** | .12** | .12** | .15*** | .25*** |
| 33. Anxiety SA | .04 | .05 | .12** | .25*** | .20*** | .22*** | .54*** | .07 | .01 | .04 | .02 | .06 | .13** | .05 | .16*** |
| 34. Dependence Baseline | .05 | .07 | .00 | .04 | .03 | .05 | .04 | .12*** | .05 | .04 | .08* | .03 | .08* | .11** | .04 |
| 35. Dependence 1 | .07* | .07* | .04 | .05 | .08* | .09* | −.02 | .07* | .09** | .15*** | .14*** | .12*** | .04 | .05 | .05 |
| 36. Dependence 2 | .13*** | .17*** | .13*** | .03 | .03 | .04 | .02 | .10*** | .15*** | .11*** | .13*** | .14*** | .20*** | .11** | .01 |
| 37. Dependence 3 | .17*** | .10** | .11** | .02 | .01 | .07 | −.02 | .07* | .07* | .07* | .10** | .15*** | .07 | .04 | −.05 |
| 38. Dependence 4 | .15*** | .17*** | .18*** | −.01 | .05 | .10** | .07 | .04 | .05 | .06 | .05 | .14*** | .12*** | .02 | .08* |
| 39. Dependence 5 | .08* | .1*** | .17*** | .13*** | .12*** | .13*** | .00 | .06 | .06 | .07* | .06 | .07* | .12*** | .11** | .12*** |
| 4. Dependence 6 | .08* | .13*** | .22*** | .10** | .07* | .17*** | .02 | .07* | .06 | .06 | .15*** | .08* | .13*** | .14*** | .09* |
| 41. Dependence 7 | .03 | .10** | .09* | .05 | .06 | .11** | .03 | .01 | .06* | .00 | .10** | −.01 | .07* | .06 | .10** |
| 42. Dependence 8 | .08* | .09* | .05 | .10** | .04 | .11** | .01 | .04 | .05 | .05 | .06 | .03 | .10** | .07 | .20*** |
| 43. Dependence 9 | .10** | .09* | .11** | .04 | .08* | .28*** | .06 | .06 | .05 | .08* | .16*** | .07* | .06 | .04 | .07 |
| 44. Dependence 10 | .11 | .02 | .07* | .00 | .09* | .14*** | .11** | .10** | .04 | .11** | .12*** | .11**. | .07 | .03 | .03 |
Table 3c.
Correlation Matrix Part 3.
| 31 | 32 | 33 | 34 | 35 | 36 | 37 | 38 | 39 | 40 | 41 | 42 | 43 | 44 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. ER Baseline | ||||||||||||||
| 2. ER 1 | ||||||||||||||
| 3. ER 2 | ||||||||||||||
| 4. ER 3 | ||||||||||||||
| 5. ER 4 | ||||||||||||||
| 6. ER 5 | ||||||||||||||
| 7. ER 6 | ||||||||||||||
| 8. ER 7 | ||||||||||||||
| 9. ER 8 | ||||||||||||||
| 1. ER 9 | ||||||||||||||
| 11. ER SA | ||||||||||||||
| 12. Depression Baseline | ||||||||||||||
| 13. Depression 1 | ||||||||||||||
| 14. Depression 2 | ||||||||||||||
| 15. Depression 3 | ||||||||||||||
| 16. Depression 4 | ||||||||||||||
| 17. Depression 5 | ||||||||||||||
| 18. Depression 6 | ||||||||||||||
| 19. Depression 7 | ||||||||||||||
| 2. Depression 8 | ||||||||||||||
| 21. Depression 9 | ||||||||||||||
| 22. Depression 10 | ||||||||||||||
| 23. Anxiety Baseline | ||||||||||||||
| 24. Anxiety 1 | ||||||||||||||
| 25. Anxiety 2 | ||||||||||||||
| 26. Anxiety 3 | ||||||||||||||
| 27. Anxiety 4 | ||||||||||||||
| 28. Anxiety 5 | ||||||||||||||
| 29. Anxiety 6 | ||||||||||||||
| 3. Anxiety 7 | ||||||||||||||
| 31. Anxiety 8 | 1 | |||||||||||||
| 32. Anxiety 9 | .22*** | 1 | ||||||||||||
| 33. Anxiety SA | .20*** | .26*** | 1 | |||||||||||
| 34. Dependence Baseline | .05 | .10** | .05 | 1 | ||||||||||
| 35. Dependence 1 | .06 | .09* | .04 | .31*** | 1 | |||||||||
| 36. Dependence 2 | .03 | .05 | .05 | .26*** | .28*** | 1 | ||||||||
| 37. Dependence 3 | .01 | .05 | .04 | .20*** | .20*** | .35*** | 1 | |||||||
| 38. Dependence 4 | .01 | .10** | .04 | .20*** | .17*** | .33*** | .28*** | 1 | ||||||
| 39. Dependence 5 | .05 | .11** | .03 | .14*** | .20*** | .30*** | .31*** | .28*** | 1 | |||||
| 4. Dependence 6 | −.01 | .11** | .07 | .14*** | .12*** | .20*** | .23*** | .22*** | .33*** | 1 | ||||
| 41. Dependence 7 | −.03 | .07 | .06 | .18*** | .16*** | .20*** | .15*** | .14*** | .26*** | .24*** | 1 | |||
| 42. Dependence 8 | .12*** | .11** | .00 | .10*** | .17*** | .17*** | .17*** | .12*** | .21*** | .23*** | .34*** | 1 | ||
| 43. Dependence 9 | .12*** | .18*** | .09* | .11*** | .18*** | .21*** | .11*** | .12*** | .15*** | .21*** | .19*** | .30*** | 1 | |
| 44. Dependence 10 | .08* | .11** | .17*** | .12*** | .15*** | .17*** | .15*** | .12*** | .16*** | .18*** | .18*** | .17*** | .30*** | 1 |
Note:
p<.05.
p<.01.
p<.001
Appendix B
Missingness Means and Correlations for all Variables of Interest
Table B.1.
Correlations with Depression Missingness at Each Wave
| Depression Missing | Covariate | ||||
|---|---|---|---|---|---|
| Missingness (%) | Ave ER Ability | Ave Depression | Ave Anxiety | Ave Dependence | |
| Missing Dep Base | 6.8 | 0.08 | −0.04 | −0.04 | −0.07 |
| Missing Dep 1 | 21.36 | 0.2 | −0.03 | −0.01 | −0.08 |
| Missing Dep 2 | 27.27 | 0.05 | −0.06 | −0.08 | −0.11 |
| Missing Dep 3 | 33.04 | 0.08 | −0.01 | −0.06 | −0.12 |
| Missing Dep 4 | 35.85 | 0.1 | −0.09 | −0.11 | −0.16 |
| Missing Dep 5 | 36.73 | 0.09 | −0.11 | −0.1 | −0.13 |
| Missing Dep 6 | 36.73 | 0.07 | −0.08 | −0.1 | −0.14 |
| Missing Dep 7 | 37.47 | −0.03 | −0.1 | −0.07 | −0.09 |
| Missing Dep 8 | 35.11 | −0.04 | −0.09 | −0.05 | −0.12 |
| Missing Dep 9 | 39.69 | −0.05 | −0.1 | −0.12 | −0.12 |
| Missing Dep 10 | 47.6 | −0.06 | −0.1 | −0.09 | −0.13 |
Note. Depression Missing = binary missingness at each wave (1 = missing, 0 = not missing); Ave Er Ability/Depression/Anxiety/Dependence = within-person average of all scores for which we have data. Clinical scores were binary.
Table B.2.
Correlations with Anxiety Missingness at Each Wave
| Anxiety Missing | Covariate | ||||
|---|---|---|---|---|---|
| Missingness (%) | Ave ER Ability | Ave Depression | Ave Anxiety | Ave Dependence | |
| Missing Anxiety Base | 6.8 | 0.08 | −0.04 | −0.04 | −0.07 |
| Missing Anx 1 | 21.36 | 0.2 | −0.03 | −0.01 | −0.08 |
| Missing Anx 2 | 27.27 | 0.05 | −0.06 | −0.08 | −0.11 |
| Missing Anx 3 | 33.11 | 0.08 | −0.01 | −0.04 | −0.12 |
| Missing Anx 4 | 35.85 | 0.1 | −0.09 | −0.11 | −0.16 |
| Missing Anx 5 | 36.73 | 0.09 | −0.11 | −0.1 | −0.13 |
| Missing Anx 6 | 36.73 | 0.07 | −0.08 | −0.1 | −0.14 |
| Missing Anx 7 | 37.47 | −0.03 | −0.1 | −0.07 | −0.09 |
| Missing Anx 8 | 35.11 | −0.04 | −0.09 | −0.05 | −0.12 |
| Missing Anx 9 | 39.76 | −0.05 | −0.1 | −0.12 | −0.12 |
| Missing Anx 10 | 47.6 | −0.06 | −0.1 | −0.09 | −0.13 |
Table B.3.
Correlations with Substance Dependence Missingness at Each Wave
| Dependence Missing | Covariate | ||||
|---|---|---|---|---|---|
| Missingness (%) | Ave ER Ability | Ave Depression | Ave Anxiety | Ave Dependence | |
| Missing Dependence Base | 0.22 | 0.03 | −0.02 | −0.01 | −0.03 |
| Missing Dep 1 | 6.8 | 0.17 | 0.02 | 0.06 | 0.04 |
| Missing Dep 2 | 6.87 | 0 | 0 | −0.01 | 0.03 |
| Missing Dep 3 | 9.24 | −0.08 | 0.03 | 0 | −0.02 |
| Missing Dep 4 | 9.16 | −0.12 | 0.03 | 0.01 | 0 |
| Missing Dep 5 | 8.87 | −0.14 | 0.01 | 0.02 | −0.01 |
| Missing Dep 6 | 8.94 | −0.18 | 0.02 | 0.03 | 0.01 |
| Missing Dep 7 | 10.27 | −0.15 | 0 | 0 | 0.01 |
| Missing Dep 8 | 11.01 | −0.2 | −0.01 | 0.01 | −0.02 |
| Missing Dep 9 | 12.86 | −0.18 | 0 | −0.02 | −0.02 |
| Missing Dep 10 | 16.41 | −0.16 | 0.01 | −0.01 | −0.02 |
Footnotes
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Ahmed SP, Bittencourt-Hewitt A, & Sebastian CL (2015). Neurocognitive bases of emotion regulation development in adolescence. Developmental Cognitive Neuroscience, 15, 11–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldao A (2012). Emotion Regulation Strategies as Transdiagnostic Processes: A Closer Look at the Invariance of their Form and Function. Revista de Psicopatología y Psicología Clínica, 17(3), 261–277. [Google Scholar]
- Aldao A, Nolen-Hoeksema S, & Schweizer S (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217–237. [DOI] [PubMed] [Google Scholar]
- Allemand M, & Hill PL (2019). Future time perspective and gratitude in daily life: A micro–longitudinal study. European Journal of Personality, 33(3), 385–399. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition). American Psychiatric Association. [Google Scholar]
- Andrés ML, Richaud de Minzi MC, Castañeiras C, Canet-Juric L, & Rodríguez-Carvajal. (2016). Neuroticism and depression in children: The role of cognitive emotion regulation strategies. The Journal of Genetic Psychology, 177(2), 55–71. [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychological Review, 111(1), 33. [DOI] [PubMed] [Google Scholar]
- Bandalos DL (2014). Relative performance of categorical diagonally weighted least squares and robust maximum likelihood estimation. Structural Equation Modeling: a Multidisciplinary Journal, 21(1), 102–116. [Google Scholar]
- Barlow DH, Allen LB, & Choate ML (2004). Toward a unified treatment for emotional disorders. Behavior Therapy, 35(2), 205–230. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S, Bentley KH, Thompson-Hollands J, Conklin LR, Boswell JF, Ametaj A, Carl JR, Boettcher HT, & Cassiello-Robbins C (2017). The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders Compared With Diagnosis-Specific Protocols for Anxiety Disorders: A Randomized Clinical Trial. JAMA Psychiatry, 74(9), 875–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH, Sauer-Zavala S, Carl JR, Bullis JR, & Ellard KK (2014). The Nature, Diagnosis, and Treatment of Neuroticism: Back to the Future. Clinical Psychological Science, 2(3), 344–365. [Google Scholar]
- Berking M, & Wupperman P (2012). Emotion regulation and mental health: recent findings, current challenges, and future directions. Current Opinion in Psychiatry, 25(2), 128–134. [DOI] [PubMed] [Google Scholar]
- Bradley SJ (2003). Affect Regulation and the Development of Psychopathology Guilford Press. [Google Scholar]
- Bromberger JT, Kravitz HM, Matthews K, Youk A, Brown C, & Feng W (2009). Predictors of first lifetime episodes of major depression in midlife women. Psychological Medicine, 39(1), 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calkins SD, & Hill A (2007). Caregiver Influences on Emerging Emotion Regulation. In Gross JJ (Ed.), Handbook of Emotion Regulation, First Edition (pp. 229–248). The Guilford Press. [Google Scholar]
- Campbell-Sills L, & Barlow DH (2007). Incorporating emotion regulation into conceptualizations and treatments of anxiety and mood disorders. In Gross JJ (Ed.), Handbook of emotion regulation (pp. 542–559). New York: Guilford Press. [Google Scholar]
- Carpenter RW, & Trull TJ (2013). Components of Emotion Dysregulation in Borderline Personality Disorder: A Review. Current Psychiatry Reports, 15(1), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Data and statistics on children’s mental health (2020, June 15). Retrieved February 17, 2021, from https://www.cdc.gov/childrensmentalhealth/data.html
- de Lijster JM, Dierckx B, Utens EM, Verhulst FC, Zieldorff C, Dieleman GC, & Legerstee JS (2017). The age of onset of anxiety disorders: a meta-analysis. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 62(4), 237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L, Rogosch F, & Barrera M (1991). Substance use and symptomatology among adolescent children of alcoholics. Journal of Abnormal Psychology, 100(4), 449–463. [DOI] [PubMed] [Google Scholar]
- Cheetham A, Allen NB, Yücel M, & Lubman DI (2010). The role of affective dysregulation in drug addiction. Clinical Psychology Review, 30(6), 621–634. [DOI] [PubMed] [Google Scholar]
- Cisler JM, Olatunji BO, Feldner MT, & Forsyth JP (2010). Emotion Regulation and the Anxiety Disorders: An integrative review. Journal of Psychopathology and Behavioral Assessment, 32(1), 68–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cludius B, Mennin D, & Ehring T (2020). Emotion regulation as a transdiagnostic process. Emotion, 20(1), 37. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, & Melisaratos N (1983). The brief symptom inventory: an introductory report. Psychological Medicine, 13(3), 595–605. [PubMed] [Google Scholar]
- Dollar JM, Perry NB, Calkins SD, Keane SP, & Shanahan L (2018). Temperamental Anger and Positive Reactivity and the Development of Social Skills: Implications for Academic Competence During Preadolescence. Early Education and Development, 29(5), 747–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dormann C, & Griffin MA (2015). Optimal time lags in panel studies. Psychological Methods, 20(4), 489. [DOI] [PubMed] [Google Scholar]
- Fabes RA, & Eisenberg N (1992). Young Children’s Emotional Arousal and Anger/Aggressive Behaviors. In Fra̧czek A & Zumkley H (Eds.), Socialization and Aggression (pp. 85–101). Springer; Berlin Heidelberg. [Google Scholar]
- Famularo R, Kinscherff R, & Fenton T (1992). Psychiatric diagnoses of maltreated children: Preliminary findings. Journal of the American Academy of Child & Adolescent Psychiatry, 31(5), 863–867. [DOI] [PubMed] [Google Scholar]
- Finch JF, & West SG (1997). The Investigation of Personality Structure: Statistical models. Journal of Research in Personality, 31, 439–485. [Google Scholar]
- Goodman E, Slap GB, & Huang B (2003). The public health impact of socioeconomic status on adolescent depression and obesity. American Journal of Public Health, 93(11), 1844–1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granger CWJ (1969). Investigating causal relations by econometric models and cross-spectral methods. Econometrica, 37, 424–438. [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, … & Compton, W. M. (2009). Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Molecular Psychiatry, 14(11), 1051–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. [Google Scholar]
- Gratz KL, Weiss NH, & Tull MT (2015). Examining emotion regulation as an outcome, mechanism, or target of psychological treatments. Current Opinion in Psychology, 3, 85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ (2011). Handbook of Emotion Regulation, First Edition. Guilford Press. [Google Scholar]
- Gross JJ, & Feldman Barrett L (2011). Emotion Generation and Emotion Regulation: One or Two Depends on Your Point of View. Emotion Review, 3(1), 8–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guttman L (1945). A Basis for Analyzing Test-retest Reliability. Psychometrika, 10 (4), 255–282. [DOI] [PubMed] [Google Scholar]
- Hatch SL, & Dohrenwend BP (2007). Distribution of Traumatic and Other Stressful Life Events by Race/Ethnicity, Gender, SES and Age: A Review of the Research. American Journal of Community Psychology, 40, 313–332. [DOI] [PubMed] [Google Scholar]
- Herd T, King-Casas B, & Kim-Spoon J (2020). Developmental Changes in Emotion Regulation During Adolescence: Associations with Socioeconomic Risk and Family Emotional Context. Journal of Youth and Adolescence, 49(7), 1545–1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji L, Chow SM, Schermerhorn AC, Jacobson NC, & Cummings EM (2018). Handling Missing Data in the Modeling of Intensive Longitudinal Data. Structural Equation Modeling: A Multidisciplinary Journal, 25(5), 715–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, & Wittchen HU (2012). Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 21(3), 169–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, & Kendler KS (1994). Lifetime and 12-month Prevalence of DSM-III-R Psychiatric Disorders in the United States: Results from the National Comorbidity Survey. Archives of General Psychiatry, 51(1), 8–19. [DOI] [PubMed] [Google Scholar]
- Khantzian E (1985). The Self Medication Hypothesis of Addictive Disorders: Focus on Heroin and Cocaine Dependence. The American Journal of Psychiatry, 142, 1259–1264. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ (1997). The Self-Medication Hypothesis of Substance Use Disorders: A Reconsideration and Recent Applications. Harvard Review of Psychiatry, 4(5), 231–244. [DOI] [PubMed] [Google Scholar]
- Kober H (2014). Emotion regulation in Substance Use Disorders. In Gross JJ (Ed.), Handbook of emotion regulation (2nd ed., pp. 428–446). New York, NY: Guilford Press [Google Scholar]
- Kring AM, & Sloan DM (2009). Emotion Regulation and Psychopathology: A Transdiagnostic Approach to Etiology and Treatment Guilford Press. [Google Scholar]
- Kupek E (2005). Log-linear transformation of binary variables: a suitable input for SEM. Structural Equation Modeling, 12(1), 28–40. [Google Scholar]
- Marsh HW, Hau K-T, & Wen Z (2004). In Search of Golden rules: Comment on Hypothesis-Testing Approaches to Setting Cutoff Values for Fit Indexes and Dangers in Overgeneralizing Hu and Bentler’s (1999) Findings. Structural Equation Modeling, 11, 320–341. [Google Scholar]
- Mischel W, Ayduk O, Berman MG, Casey BJ, Gotlib IH, Jonides J, … & Shoda Y (2011). ‘Willpower’ over the life span: decomposing self-regulation. Social Cognitive and Affective Neuroscience, 6(2), 252–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Nolen-Hoeksema S (2011). Rumination as a transdiagnostic factor in depression and anxiety. Behaviour Tesearch and Therapy, 49(3), 186–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris AS, Houltberg BJ, Criss MM, & Bosler CD (2017). Family Context and Psychopathology: The Mediating Role of Children’s Emotion Regulation. In Centifanti LC & Williams DM (Eds.), The Wiley Handbook of Developmental Psychopathology (pp. 365–389). John Wiley & Sons, Ltd. [Google Scholar]
- Mulvey EP, Steinberg L, Fagan J, Cauffman E, Piquero AR, Chassin L, … & Losoya SH (2004). Theory and research on desistance from antisocial activity among serious adolescent offenders. Youth violence and juvenile justice, 2(3), 213–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton PJ, & Philipp LM (2008). Transdiagnostic approaches to the treatment of anxiety disorders: A quantitative review. Psychotherapy: Theory, Research, Practice, Training, 45(2), 214–226 [DOI] [PubMed] [Google Scholar]
- Park CL, Williams MK, Hernandez PR, Agocha VB, Lee SY, Carney LM, & Loomis D (2020). Development of emotion regulation across the first two years of college. Journal of Adolescence, 84, 230–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakesh D, Allen NB, & Whittle S (2020). Balancing act: Neural correlates of affect dysregulation in youth depression and substance use – A systematic review of functional neuroimaging studies. Developmental Cognitive Neuroscience, 42, 100775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria URL https://www.R-project.org/.
- RStudio Team (2019). RStudio: Integrated Development for R RStudio, Inc., Boston, MA: URL http://www.rstudio.com/. [Google Scholar]
- Rohde P, Lewinsohn PM, Kahler CW, Seeley JR, & Brown RA (2001). Natural Course of Alcohol Use Disorders from Adolescence to Young Adulthood. Journal of the American Academy of Child & Adolescent Psychiatry, 40(1), 83–90. [DOI] [PubMed] [Google Scholar]
- Rosseel Y (2012). “lavaan: An R Package for Structural Equation Modeling.” Journal of Statistical Software, 48(2), 1–36. http://www.jstatsoft.org/v48/i02/ [Google Scholar]
- Schneider RL, Arch JJ, Landy LN, & Hankin BL (2018). The longitudinal effect of emotion regulation strategies on anxiety levels in children and adolescents. Journal of Clinical Child & Adolescent Psychology, 47(6), 978–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheppes G, Suri G, & Gross JJ (2015). Emotion regulation and psychopathology. Annual Review of Clinical Psychology, 11, 379–405. [DOI] [PubMed] [Google Scholar]
- Silberg J, Pickles A, Rutter M, Hewitt J, Simonoff E, Maes H, … & Eaves L (1999). The influence of genetic factors and life stress on depression among adolescent girls. Archives of General Psychiatry, 56(3), 225–232. [DOI] [PubMed] [Google Scholar]
- Skeem JL, Schubert CA, Odgers C, Mulvey EP, Gardner W Lidz, C. (2006) Psychiatric Symptoms and Community Violence Among High-risk patients: A test of the relationship at the weekly level. Journal of Consulting and Clinical Psychology, 74(5), 967–979. [DOI] [PubMed] [Google Scholar]
- Sloan E, Hall K, Moulding R, Bryce S, Mildred H, & Staiger PK (2017). Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: A systematic review. Clinical Psychology Review, 57, 141–163. [DOI] [PubMed] [Google Scholar]
- Pathways to Desistence Study (n.d.). Measures Retrieved from: https://www.pathwaysstudy.pitt.edu/codebook/measures.html
- Pathways to Desistence Study (2016). Study Overview Retrieved from: https://www.pathwaysstudy.pitt.edu/index.html
- Rosseel Y (2012). “lavaan: An R Package for Structural Equation Modeling.” Journal of Statistical Software, 48(2), 1–36. https://www.jstatsoft.org/v48/i02/. [Google Scholar]
- Swendsen J, Burstein M, Case B, Conway KP, Dierker L, He J, & Merikangas KR (2012). Use and Abuse of Alcohol and Illicit Drugs in US Adolescents: Results of the National Comorbidity Survey–Adolescent Supplement. Archives of General Psychiatry, 69(4), 390–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobia V, Riva P, & Caprin C (2017). Who Are the Children Most Vulnerable to Social Exclusion? The Moderating Role of Self-Esteem, Popularity, and Nonverbal Intelligence on Cognitive Performance Following Social Exclusion. Journal of Abnormal Child Psychology, 45(4), 789–801. [DOI] [PubMed] [Google Scholar]
- Tubman JG, & Lerner RM (1994). Continuity and discontinuity in the affective experiences of parents and children: Evidence from the New York Longitudinal Study. American Journal of Orthopsychiatry, 64(1), 112–125. [DOI] [PubMed] [Google Scholar]
- Tull MT, Stipelman BA, Salters-Pedneault K, & Gratz KL (2009). An examination of recent non-clinical panic attacks, panic disorder, anxiety sensitivity, and emotion regulation difficulties in the prediction of generalized anxiety disorder in an analogue sample. Journal of Anxiety Disorders, 23(2), 275–282. [DOI] [PubMed] [Google Scholar]
- Usami S, Murayama K, & Hamaker EL (2019). A unified framework of longitudinal models to examine reciprocal relations. Psychological Methods, 24(5), 637. [DOI] [PubMed] [Google Scholar]
- Walden TA, Harris VS, Caltron TF (2003) How I Feel: A Self-Report Measure of Emotional Arousal and Regulation for Children. Psychological Assessment, 15(3), 399–412. [DOI] [PubMed] [Google Scholar]
- Walden T, Lemerise E, and Gentile J (1992, April). Emotional competence and peer acceptance among preschool children Paper presented at the Conference on Human Development, Atlanta, GA [Google Scholar]
- Weiss NH, Bold KW, Sullivan TP, Armeli S, & Tennen H (2017). Testing bidirectional associations among emotion regulation strategies and substance use: a daily diary study. Addiction, 112(4), 695–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman DG, Bitran D, Miller AB, Schaefer JD, Sheridan MA, & McLaughlin KA (2019). Difficulties with emotion regulation as a transdiagnostic mechanism linking child maltreatment with the emergence of psychopathology. Development and Psychopathology, 31(3), 899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox CE, Pommy JM, & Adinoff B (2016). Neural Circuitry of Impaired Emotion Regulation in Substance Use Disorders. American Journal of Psychiatry, 173(4), 344–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willett JB, & Sayer AG (1994). Using covariance structure analysis to detect correlates and predictors of individual change over time. Psychological Bulletin, 116, 363. [Google Scholar]
- Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, … & Steinhausen HC (2011). The size and burden of mental disorders and other disorders of the brain in Europe 2010. European neuropsychopharmacology, 21(9), 655–679. [DOI] [PubMed] [Google Scholar]
- Yap MB, Allen NB, & Sheeber L (2007). Using an emotion regulation framework to understand the role of temperament and family processes in risk for adolescent depressive disorders. Clinical Child and Family Psychology Review, 10(2), 180–196. [DOI] [PubMed] [Google Scholar]
- Yoon KL, Maltby J, & Joormann J (2013). A pathway from neuroticism to depression: Examining the role of emotion regulation. Anxiety, Stress & Coping, 26(5), 558–572. [DOI] [PubMed] [Google Scholar]
- Zisook S, Lesser I, Stewart JW, Wisniewski SR, Balasubramani GK, Fava M, … & Rush, A. J. (2007). Effect of Age at Onset on the Course of Major Depressive Disorder. American Journal of Psychiatry, 164(10), 1539–1546. [DOI] [PubMed] [Google Scholar]


