Abstract
Background
Maternal exposure to pesticides during early pregnancy is associated with increased risks of birth defects, while the association between maternal exposure to chemical fertilizer during pregnancy and the risk of birth defects remains unknown.
Methods
Data were from a population-based birth defects surveillance system between 2007 and 2012 in Pingding County, Shanxi Province, northern China. A total of 14 074 births with 235 birth defects were used to estimate spatial clustering and correlations at the village level. A population-based case–control study of 157 cases with birth defects and 204 controls was performed to investigate the association between maternal chemical fertilizer exposure and the risk of birth defects by a two-level logistic model.
Results
The total prevalence of birth defects between 2007 and 2012 was 167.0/10 000 births. The spatial analysis indicated a remarkable high-risk area of birth defects in the southeast of Pingding County and the use of chemical fertilizer was associated with the risk of birth defects at the village level. After adjusting for confounders at the individual level, mothers who live in villages with chemical fertilizer application ≥65 tons/y had an increased risk of birth defects (adjusted odds ratio 2.06 [95% confidence interval 1.23 to 3.46]) compared with those of <65 tons/y.
Conclusions
Our findings suggest that the risk of birth defects may be associated with the use of chemical fertilizer in rural northern China. The findings must be cautiously interpreted and need to be investigated on larger samples.
Keywords: birth defects, chemical fertilizer exposure, spatial multilevel logistic regression, spatial variations
Introduction
Birth defects are a global public health issue, affecting about 8 million infants (3–6% of infants) worldwide every year, accounting for 11% of child deaths in China1 and contributing substantially to childhood and adult disability.2,3 Epidemiological studies found that the prevalence rate of birth defects was 232.4/10 000 births in 2003.4 The prevalence rate of neural tube defects (major birth defects) was 138.7–199.4/10 000 births between 2003 and 2006 in Shanxi Province in China.5,6 Also, there were seven kinds of birth defects with a prevalence rate of >10 per 10 000 births in this region, including anencephaly (65.9/10 000), spina bifida (58.1/10 000), hydrocephaly (47.7/10 000), polydactyly (26.0/10 000), cleft palate (21.7/10 000), encephalocele (14.7/10 000) and cleft lip (10.4/10 000).7 The risk of birth defects in the same areas of Shanxi Province was associated with maternal age, race, behavioural factors, nutritional deficiency, medication use, history of the disease, persistent organic pollutants, air pollution (particulate matter <10 μm [PM10]), infection during early pregnancy8–13 and genetic variations at the individual level.14–17 However, the aetiology of birth defects is complex, thus exposure to the above factors at the individual level does not explain the high prevalence of birth defects throughout the region. Studies have shown that most birth defects are influenced by genetic and environmental factors17–19 or an interaction of multiple factors.14,20 However, few studies have assessed the influence of macro-environmental factors such as long-term exposure to chemical fertilizers or pesticides application. Some studies have mainly focused on the association between pesticide exposure during pregnancy and the risk of birth defects at the individual level.11,21,22
China is the largest consumer of chemical fertilizer in the world. The use efficiency of nitrogen, phosphorus and potassium fertilizer in China is 10–50%.23 The overuse of chemical fertilizer contributes to heavy metal contamination of the water and soil.24 Chemical fertilizers are recognized as a potential source of elements that could contribute to soil pollution with cadmium (Cd), iron (F), magnesium (Mg) and zinc (Zn), among others. Another primary source of heavy soil metals is the application of large amounts of low-grade fertilizer.25 Our previous study investigated associations between geochemical feature distributions and the risk of birth defects in Shanxi Province, China.26 The results revealed that the arsenic levels in cropland soil showed a significant association with the risk of birth defects in this area, consistent with existing evidence of arsenic as a teratogen.27 A recent study indicated that maternal exposure to high levels of Cd and lead (Pb) was associated with an elevated risk for orofacial clefts in a dose–response relationship in rural northern China.28 The research above indicated that maternal heavy metal exposure was a significant risk factor for birth defects. Studies in other countries found associations between the risk of birth defects and exposure to agricultural pollution such as pesticides and fertilizers.22,29 Individuals who had direct occupational exposures to agricultural chemicals had increased risks of adverse outcomes.30–32 Residential proximity to locations where agricultural chemicals were applied increased the risk of neural tube defects.33 The extensive application of agricultural fertilizer may play an essential role in the high prevalence of birth defects in areas of Shanxi Province. However, the aforementioned studies focused mainly on the association of environmental exposure at the individual level with the risk of birth defects, and there is little information available in the existing literature.26,34 Based on the above objectives, we hypothesized that maternal exposure to chemical fertilizer at the village level might be associated with the risk of birth defects in a rural population in northern China, independent of known confounding factors at the individual level. A spatial multilevel logistic model was performed to estimate the spatially dependent macro effect on the risk of birth defects and provide a more robust result.35
Methods
Study population
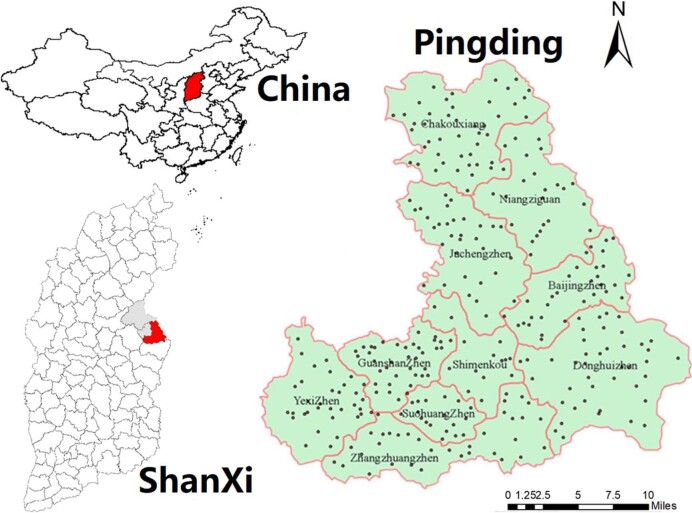
This study was performed in Pingding County in Shanxi Province, northern China (37°–38°04' N, 113°26'–114°03' E; Figure 1). Pingding County covers 1394 km2 and is divided into eight town-level administrative units and two township-level administrative units, with a total population of 345 039. The urban and rural populations are 149 300 and 195 700, respectively, with 177 533 males and 167 506 females. The landscape of Pingding County is mainly mountains and hills, with a warm temperate continental monsoon climate. By 2011, the total area sown with crops in Pingding County was 22 944 ha. A total of 22 220 ha were planted with food crops and 723.9 ha were sown with cash crops and other crops. All births and birth defects cases were from 313 villages in Pingding County.
Figure 1.
The location and distribution of villages in Pingding County. Pingding County is in the eastern part of Shanxi Province in northern China. All the birth defect cases from 2007 to 2012 in the study area were collected from 313 villages (black dots on the map denote each village). The base map was downloaded from Geographic Information Professional Knowledge Service System (http://kmap.ckcest.cn/nationwideMap/index).
Collection of birth data
Data were derived from the population-based birth defects surveillance system, established in 1993. This system monitors women and their foetuses/infants from the onset of pregnancy to day 42 after delivery in Pingding County. All women in the monitoring area lived in the county for ≥1 y. Information on pregnancy outcomes was collected during the first week after delivery or at the time of termination of the pregnancy and, at the same time, trained healthcare workers took photos of the baby with birth defects and confirmed the diagnosis. Pregnancy outcomes included live birth, stillbirth, foetal death and pregnancy termination due to the diagnosis of birth defects. Therefore the surveillance system can completely and accurately detect dynamic changes in the incidence of adverse pregnancy outcomes.
From 2007 to 2012, 14 074 births with 235 birth defects were used to estimate the spatial clustering of birth defect risks. Among the 235 birth defects, neural tube defects account for 37.5% (including anencephaly, spina bifida encephalocele and hydrocephaly), orofacial cleft 14.0%, congenital heart disease 6.4%, limb deformities 6.8%, polydactyly 20.4%, oesophageal or anal atresia 3.8%, genital malformation 3.4%, hydronephrosis 3.0%, eye and ear deformities 1.7%, hypospadias 1.7%, haemangioma and naevus 0.9% and conjoined twins 0.4%.
We then derived a sample from the whole population to conduct a case–control study to estimate the association between the risk of birth defects and chemical fertilizer use. Mothers with significant and severe birth defects were selected from the surveillance system. Mothers with normal birth outcomes were selected as controls through random sampling to represent the population from which the case group was derived during the same period. Sample size for the case–control study was estimated. The sample size per group was 150 and the total sample size (both groups) was 300 when the parameter including expected proportion in controls (0.25), expected odds ratio (2.0), confidence level (0.95) and test power (0.8) was assumed correctly. There was a sample size of 157 cases and 204 controls in the analysis. Finally, 157 mothers with infants with major birth defects and 204 mothers with healthy infants were selected through random sampling. Among the 157 cases with birth defects, neural tube defects accounted for 56.1%, orofacial cleft 21.0%, limb deformities10.2%, congenital heart disease 9.6% and polydactyly3.2%. All of the birth defects cases and controls were delivered between 2007 and 2012. Trained healthcare workers followed up within 1 y after birth or termination of the pregnancy and conducted face-to-face interviews with mothers of infants with birth defects and the control group. Maternal exposure information was collected using a structured questionnaire, including parental demographic characteristics, lifestyle and behaviours, illness, medication taken during early pregnancy, nutrient intake, history of diseases, first-trimester fever or influenza in the current pregnancy, periconceptional folic acid supplementation and the family's use of chemical fertilizer. A flow diagram of the selection of cases and controls is presented in Figure 2.
Figure 2.
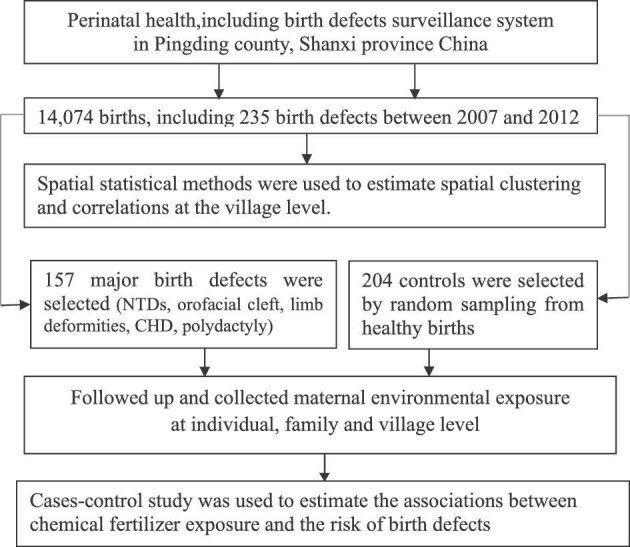
Flow diagram of the selection of cases and controls.
Definition and collection of chemical fertilizer
Chemical fertilizer was defined as any of a large number of natural and synthetic materials, including manure and nitrogen, phosphorus and potassium compounds, that are spread on or worked into the soil to increase its capacity to support plant growth. Maternal chemical fertilizer exposure during pregnancy was measured at both the household and village level. Household chemical fertilizer use was collected through the questionnaire and village annual fertilizer use was derived from the Annals of National Economic Statistics of Pingding County between 2007 and 2012. The annals were published by the Bureau of Statistics of Pingding County and reported the average chemical fertilizer application during the 5 y. Since the arable land area and the number of crops planted remained unchanged, fertilizer application did not change annually within the 5 y. Therefore we used the 5-y average data to represent annual data from 2007 to 2012.
Regarding the exposure and exposure timing, the annual average fertilizer use can be used as the actual exposure dose because the cultivated area is stable. We emphasized that exposure to the application of chemical fertilizer was before pregnancy or in early pregnancy. Macro agricultural and economic data at the village level, including electricity consumption, per capita net income, cultivated area and the total population, were also collected from Annals of National Economic Statistics of Pingding County.
The study protocol was reviewed and approved by the Institutional Review Board of Peking University Health Science Center and written informed consent was obtained from all subjects before completing the questionnaire.
Statistical analysis
Spatial statistical analysis
Spatial clustering of the risk of birth defects and its correlations with chemical fertilizer use at the village level were analysed through spatial statistical analysis. There were 313 villages with geocode data in Pingding County. Thiessen polygons were used to form the geographic borders of each village and build the base map. We then joined the macro agricultural and environmental data to construct a geo-database of birth defects.
Birth defects are usually low-probability events in a small area, leading to an extreme incidence value by directly using the raw rate. Also, total births and birth defects risk in a spatial area is related to nearby adjacent areas due to nearby common environments. That is, the closer the villages, the more similar the situations in these villages. Hence the Bayesian hierarchical spatial conditional autoregressive (CAR) model was adopted to control the potential spatial autocorrelation and estimate the relative risk of birth defects in different villages.36,37
Spatial autocorrelation measurements (Moran's I and local Moran's I; local indicators of spatial association [LISA]) were used to detect areas with a significantly high risk of birth defects.38 The Moran's I statistic and the LISA were calculated from the risk of birth defects at the village level, where each district was regarded as a unit in the cluster analysis. Moran's I was used to estimate whether there was clustering or dispersion of birth defects in the study area. The value of Moran's I ranges between −1 and +1, with −1 indicating perfect dispersion, 0 indicating perfect randomness and +1 indicating perfect clustering of similar values. The local Moran's I (LISA) was used to identify each area's spatial relationship with its neighbours. LISA has a spatial typology consisting of four region types: high–high is a positive autocorrelation, corresponding to a spatial cluster of high risk at the village level; low–low is also a positive autocorrelation, but indicating a spatial cluster of low risk; and high–low and low–high are negative autocorrelations indicating spatial outliers.
Based on the spatial exploratory analysis above, the bivariate LISA39 was used to explore the associations between agricultural and environmental factors and the risk of birth defects. In bivariate LISA high–high and low–low indicate a positive spatial correlation of two variables under the spatial relation and high–low and low–high indicate a negative spatial correlation.
Two-level logistic regression analysis
A two-level logistic regression analysis was performed in the case–control study to estimate the association between the risk of birth defects and chemical fertilizer exposure. In particular, we adopted a spatial multilevel logistic model to analyse the spatially dependent macro effect on the risk of birth defects and provide a more robust result.35
We used a univariate χ2 test to assess differences between cases and controls regarding individual exposures (including offspring sex, maternal age, maternal education, paternal education, parity, family income, passive smoke, cold or high fever during pregnancy, folic acid supplementation, meat intake, milk/egg intake, fresh vegetables, fresh fruits, bean products, family land and household chemical fertilizer use) and macro-environmental exposures at the village level (including electricity consumption, per income and chemical fertilizer use). Univariate analyses at the p<0.05 level were also performed. Variables that passed the significant level in the univariate analysis were adopted in the regression model.
A two-level logistic regression model was then performed to estimate the association between macro-environmental factors and the risk of birth defects after adjusting for potential confounding factors and the adjusted odds ratios (aORs) with 95% confidence intervals (CIs) were calculated.40 Confounding variables included maternal demographic characteristics (maternal age and education, paternal education), parity, dietary factors (these questions were used to measure the intake frequency of different foods such as meat intake, milk/egg intake, fresh vegetables and fruit), common cold or fever in the first trimester, folic acid supplementation and passive smoke. All the Bayesian models in our study were inferred and computed using the integrated nested Laplace approximation (INLA)41 in R version 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Spatial analysis of the risks of birth defects at the village level
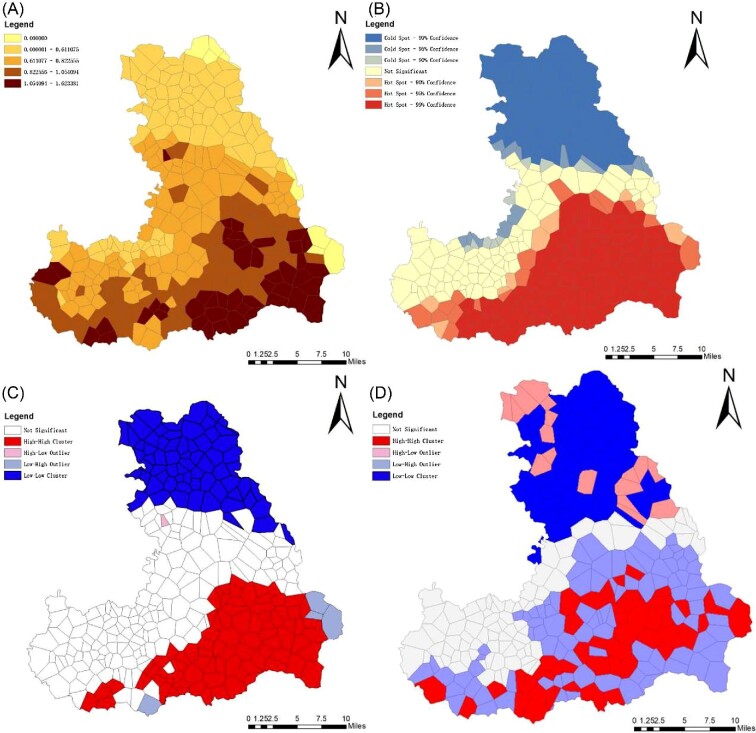
The total prevalence of birth defects between 2007 and 2012 was 167.0/10 000 births. The distribution of the risk of birth defects at the village level in Pingding County between 2007 and 2012 is presented in Figure 3 (map A). The relative risk map showed that there was a high-risk area in the southeast region. The high-risk area was a relatively low-developing area. Due to the inaccessibility of the mountainous region, this area's main economic activity is agricultural production.
Figure 3.
(A) Distribution of 2007–2012 village-level risk of birth defects in Pingding County. (B) Getis-Ord Gi* spatial hot spots. (C) LISA plot of village-level risk of birth defects in Pingding County. (D) Bivariate LISA plot of village-level risk of birth defects and chemical fertilizer use in Pingding County. Map A shows the spatial distribution of the relative risk of birth defects in Pingding County, identifying a risk region in the south. Map B shows spatial hot and cold spots, indicated by a high-risk clustering region (red marker) and a low-risk clustering region (blue marker). Map C shows a LISA plot where there is low–low clustering (negative autocorrelation, blue markers) in the northern area and high–high clustering (positive autocorrelation, red markers) in the southeast area of Pingding County. Map D shows a bivariate LISA plot indicating that there was a positive association between the risk of birth defects and chemical fertilizer use.
Moran's I showed a significant spatial autocorrelation among the study areas (I=0.59, Z>1.96, p<0.05). Based on the Getis G* statistic, hot spots (red markers) and cold spots (blue markers) were identified. The hot spots with a high risk of birth defects were concentrated in the southeast, while the cold spots with a low risk of birth defects were in the north of Pingding County (Figure 3, map B). Local Moran's I (LISA) showed that there was a significant low–low clustering (negative autocorrelation) in the northern area and high–high clustering (positive autocorrelation) in the southeast area of Pingding County (I=0.42, p<0.05) (Figure 3, map C).
The significant spatial clustering of birth defects risk detected by exploratory spatial analysis could result from environmental factors. Therefore we used bivariate LISA to estimate the association between chemical fertilizer application and the risk of birth defects. The result of the bivariate LISA (both red and blue markers) indicated that there was a positive correlation (I=0.04, p<0.05), as can be seen in Figure 3 (map D).
Two-level logistic regression analysis of the birth defects risk
The results of the univariate analysis showed that there were significant differences between cases and controls in maternal age, maternal education, paternal education, maternal parity, cold or high fever during pregnancy, folic acid supplementation, meat intake, milk/egg intake and maternal exposure to chemical fertilizer at the village level (p<0.05; Table 1). The variables with statistical significance as confounders were controlled in a two-level logistic regression model.
Table 1.
Demographic characteristics and exposure factors between cases with birth defects and controls
| Birth defectsa (n=157) | Controls (n=204) | ||||
|---|---|---|---|---|---|
| Characteristics | n | % | n | % | p-Value for χ2 test |
| Offspring sex | 0.26 | ||||
| Female | 66 | 42.0 | 98 | 48.0 | |
| Male | 91 | 58.0 | 106 | 52.0 | |
| Maternal age (years) | <0.01 | ||||
| <25 | 79 | 50.3 | 102 | 50.0 | |
| 25–<35 | 42 | 26.8 | 77 | 37.7 | |
| ≥35 | 36 | 22.9 | 25 | 12.3 | |
| Maternal education | <0.01 | ||||
| Primary school or lower | 33 | 21.2 | 18 | 8.8 | |
| Junior high school | 108 | 68.6 | 150 | 73.5 | |
| High school or above | 16 | 10.3 | 36 | 17.6 | |
| Paternal education | <0.01 | ||||
| Primary school or lower | 24 | 15.3 | 11 | 5.4 | |
| Junior high school | 109 | 69.4 | 158 | 77.5 | |
| High school or above | 24 | 15.3 | 35 | 17.2 | |
| Parity | 0.02 | ||||
| Primiparous | 60 | 38.2 | 104 | 51.0 | |
| Multiparous | 97 | 61.8 | 100 | 49.0 | |
| Family income (RMB) | |||||
| <15 000 | 43 | 27.4 | 54 | 26.5 | 0.62 |
| 15 000–<25 000 | 37 | 23.6 | 57 | 27.9 | |
| ≥25 000 | 77 | 49.0 | 93 | 45.6 | |
| Passive smoke | 0.10 | ||||
| Never | 43 | 27.4 | 77 | 37.7 | |
| Occasional | 75 | 47.8 | 79 | 38.7 | |
| Everyday | 39 | 24.8 | 48 | 23.5 | |
| Cold or high fever during pregnancy | <0.01 | ||||
| No | 128 | 81.5 | 192 | 94.1 | |
| Yes | 29 | 18.5 | 12 | 5.9 | |
| Folic acid supplementationb | <0.01 | ||||
| No | 92 | 58.6 | 83 | 40.7 | |
| Yes | 65 | 41.4 | 121 | 59.3 | |
| Meat intake (times/week) | <0.01 | ||||
| ≤1 | 116 | 73.9 | 121 | 59.3 | |
| 2–3 | 30 | 19.1 | 68 | 33.3 | |
| ≥4 | 11 | 7.0 | 15 | 7.4 | |
| Milk/egg intake (times/week) | 0.02 | ||||
| ≤3 | 74 | 47.1 | 69 | 33.8 | |
| 4–5 | 41 | 26.1 | 80 | 39.2 | |
| 6–7 | 42 | 26.8 | 55 | 27.0 | |
| Fresh vegetable (times/week) | 0.11 | ||||
| ≤3 | 24 | 15.3 | 17 | 8.3 | |
| 4–5 | 75 | 47.8 | 109 | 53.4 | |
| 6–7 | 58 | 36.9 | 78 | 38.2 | |
| Fresh fruit (times/week) | 0.26 | ||||
| ≤3 | 54 | 34.4 | 54 | 26.5 | |
| 4–5 | 58 | 36.9 | 82 | 40.2 | |
| 6–7 | 45 | 28.7 | 68 | 33.3 | |
| Bean products (times/week) | 0.67 | ||||
| ≤1 | 79 | 50.3 | 105 | 51.5 | |
| 2–3 | 65 | 41.4 | 87 | 42.6 | |
| ≥4 | 13 | 8.3 | 12 | 5.9 | |
| Household land (Mu) | 0.22 | ||||
| <2.0 | 101 | 64.3 | 127 | 62.3 | |
| 2.0–<4.0 | 33 | 21.0 | 34 | 16.7 | |
| ≥4.0 | 23 | 14.6 | 43 | 21.1 | |
| Household chemical fertilizer use (kg/y) | 0.95 | ||||
| None | 99 | 63.1 | 130 | 63.7 | |
| <100 | 13 | 8.3 | 18 | 8.8 | |
| ≥100 | 45 | 28.7 | 56 | 27.5 | |
| Electricity consumption at the village level (10 000 kWh) | 0.26 | ||||
| <10 | 38 | 24.2 | 55 | 27.0 | |
| 10–<30 | 35 | 22.3 | 58 | 28.4 | |
| 30–<85 | 38 | 24.2 | 48 | 23.5 | |
| ≥85 | 46 | 29.3 | 43 | 21.1 | |
| Per income at the village level (RMB) | 0.31 | ||||
| <5800 | 40 | 25.5 | 49 | 24.0 | |
| 5800–<6500 | 35 | 22.3 | 45 | 22.1 | |
| 6500–<6900 | 15 | 9.6 | 33 | 16.2 | |
| ≥6900 | 67 | 42.7 | 77 | 37.7 | |
| Chemical fertilizer consumption at the village level (tons) | 0.02 | ||||
| <65 | 101 | 64.3 | 155 | 76.0 | |
| ≥65 | 56 | 35.7 | 49 | 24.0 | |
The cases group is 157 families with infants with birth defects, including neural tube defects (56.1%), orofacial cleft (21.0%), limb deformities (10.2%), congenital heart disease (9.6%) and polydactyly (3.2%).
Folic acid supplementation was defined as periconceptional supplementation of folic acid.
RMB: renminbi (the official currency of China).
After adjusting for confounding factors, the risk of birth defects for maternal exposure to annual application of chemical fertilizer ≥65 tons by two-level logistic regression and spatial multilevel logistic regression were 2.06 (95% CI 1.23 to 3.46) and 2.06 (95% CI 1.23 to 3.47), respectively, as compared with exposure of <65 tons (Table 2).
Table 2.
Risk of birth defects with chemical fertilizer exposure by a two-level logistic regression model and a spatial multilevel logistic model
| Variables | Two-level logistic model, aOR (95% CI)a | Spatial multilevel logistic model, aOR (95% CI)a |
|---|---|---|
| Chemical fertilizer consumption at the village level (tons)b | ||
| <65 | 1.00 | 1.00 |
| ≥65 | 2.06 (1.23 to 3.46) | 2.06 (1.23 to 3.47) |
aOR: odds ratio after adjusting for confounding factors, including maternal age and education, paternal education, parity, meat intake, milk/egg intake, cold or fever in the first trimester during pregnancy and folic acid supplementation.
After adjusting for confounding factors, the risk of birth defects for maternal exposure to chemical fertilizer ≥65 tons annually by two-level logistic regression and spatial multilevel logistic regression as compared with exposure to <65 tons.
Discussion
The present study explored the spatial variation of birth defects and their association with chemical fertilizer application in a rural area in northern China. By both global and local Moran's I analysis, our study identified a significant spatial clustering of the overall risk of birth defects in Pingding County, and by the spatial hotspots detection method, we identified a high-risk area indicating a high-prevalence cluster of birth defects in the southeast of Pingding County. Further analysis through both bivariate LISA and two-level logistic models found that the village level's chemical fertilizer use was significantly associated with an increased risk of birth defects.
In northern China, Shanxi Province has been identified as an area with the highest prevalence of neural tube defects in the world.6 Pingding County is high-prevalence area of neural tube defects in Shanxi Province. Although the intervention program, including supplementation of folic acid and improving socio-economic status and nutritional levels for reproductive women, has been implemented for >30 y, the prevalence of birth defects in this area remains high. The cause is still unknown. We hypothesized that the risk of birth defects was associated with macro-environmental factors in a rural area of northern China.
China is the largest producer and consumer of chemical fertilizer globally, with high intensity and low utilization efficiency. The utilization efficiency of chemical fertilizer in China ranges from 10 to 50% (nitrogen fertilizer 30–35%, phosphorus 10–20% and potassium 35–50%) and the rate of nitrogen loss (33–74%) is much higher than that in developed countries.42 Major environmental issues are often caused by the overuse of chemical fertilizers, including eutrophication of surface water, nitrate contamination of groundwater and soil contaminated by heavy metals.24 Previous studies have found that chemical fertilizer use can influence the heavy metal content of the soil and affects the ecological environment.43,44 The long-term accumulation of such chemicals in soil and plants may transfer to the human body through the food chain. The accumulation of heavy metals in vegetables resulting from irrigation with water contaminated with chemical fertilizer may create a potential public health risk.45 Drinking water contaminated by agricultural chemicals or eating food grown in soil contaminated by heavy metals may increase the risk of adverse pregnancy outcomes.46 Recent studies have shown that maternal exposure to high levels of Cd and Pb in placenta tissue is associated with an elevated risk for orofacial clefts in a dose–response relationship in the population of northern China.26 The source of these heavy metals may be the application of chemical fertilizers.
The excessive application of chemical fertilizers may be one reason for the high prevalence of birth defects in the southeastern region of Pingding County, where agricultural production dominates economic activity. According to the statistical yearbook of Pingding County, 51% of villages use >50 tons of chemical fertilizer annually and 26% use >100 tons. Therefore chemical fertilizer application has been higher at the village level. Residents living in a rural area in northern China mainly grow wheat and potatoes, which are the main foods of their daily diet. Cd is a common impurity in phosphate fertilizers and may contribute to soil Cd accumulation. Cd accumulated in the edible portion of wheat and potato crops grown at these sites and showed a strong positive dose–response with fertilizer treatment.47 The main Cd exposure pathway in humans is the ingestion of contaminated foods.
The risk of major birth defects can be attributed to maternal exposure to teratogens in the first pregnancy phase. Chemical pollutants can act on the embryo through the placenta during this most vulnerable prenatal period.48 Previous studies investigated the association between heavy metal pollution and the risk of birth defects,49–51 but the potential confounding factors at the individual and macro level were not controlled. In contrast, our study used total chemical fertilizer consumption data rather than collecting data on chemical elements, which could provide supporting evidence for this approach.52 As a comprehensive study, our findings at both the village and individual levels were consistent.
Implications for future studies and practice
Future studies evaluating the effects of chemical fertilizer and pesticides on birth defects should consider using a similar framework. Our findings were consistent with a previous study in Heshun County with a high prevalence of birth defects, which is near Pingding County in Shanxi Province. The study found two typical hot spot clustering phenomena related to soil type and socio-economic activities.53 Based on this and related studies,26,54 we believe that the effects of environmental pollution on the risk of birth defects need additional scientific research.55
We emphasize that maternal exposures occurred before outcomes. Mothers who live in rural areas where fertilizers are used were considered to be fertilizer exposed, especially in early pregnancy stages, because the first trimester is a critical period for structural malformations. However, fertilizer application serves as the proxy variable of the long-term accumulation of some teratogens and may be an indirect cause of birth defects rather than a direct cause. This hypothesis needs to be evaluated through internal exposure measurement for chemical fertilizer–related pollutants and heavy metals.
In particular, our findings may be an important clue to the source of pollution, such as the existing association between high levels of heavy metals in placenta tissue and the risk of birth defects in a population in northern China.28 Potential sources of heavy metals in rural women may be excessive use of chemical fertilizers. Tracking macro-environment pollution can provide evidence for the prevention of birth defects due to exposure to environmental pollutants during early pregnancy.
Strengths and limitations of the study
Our study had several strengths. First, our data were derived from long-term birth defects surveillance systems that collected high-quality data: participants were interviewed within a short time after delivery or pregnancy termination to collect data on maternal exposure factors through a structured questionnaire, minimizing recall bias in this study. Data on chemical fertilizer use at the village level came from the Annals of National Economic Statistics, which provided an accurate long-term exposure measure. Second, a population-based case–control study was conducted to investigate the association between chemical fertilizer use and the risk of birth defects. The control group was selected by random sampling to represent the population from which the case group was derived, thus minimizing selective bias. Third, a spatial multilevel logistic model was performed to estimate the spatially dependent macro effect on the risk of birth defects and provide a more robust result.35 Fourth, the strength in the spatial analysis was that 313 villages were used to estimate G statistics, which was a reasonably large size for robust cluster analysis.
There are limitations to our study. First, the epidemiological study found that maternal exposure to pesticides increased the risk of birth defects,22,31 but rural residents in Pingding County did not use pesticides, pesticide exposure data were not available and its potential effect was unknown. Second, we did not know the seasonal variation of fertilizer use, so the association between seasonal exposure and the risk of birth defects could not be estimated. However, the annual average fertilizer application was regarded as the actual exposure dose because the cultivated area was stable. Third, maternal mobility may lead to exposure misclassification,56,57 as we assigned the village-level exposure variable based on the maternal address listed on the birth record. However, considering women included in our analysis were those who lived in the local area for >1 y and might not migrate during pregnancy, the misclassification bias is small in our study.
Conclusions
Our findings suggest that the consumption of chemical fertilizer at the village level may be associated with an increased risk of birth defects in the high-prevalence areas of neural tube defects in China. Potential sources of heavy metals may be the excessive use of chemical fertilizer. The findings must be cautiously interpreted and need to be investigated in a larger sample. Further research should investigate the interactions between individual maternal exposure factors and macro-environmental exposures and the mechanisms of pesticide and other agricultural chemical exposures, as the resulting information may contribute to the prevention of birth defects.
Acknowledgements
None.
Contributor Information
Jiajia Li, Institute of Population Research/China Center on Population Health and Development, Peking University, No. 5 Yiheyuan Road, Haidian District, Beijing,100871, China.
Shiqi Lin, Institute of Population Research/China Center on Population Health and Development, Peking University, No. 5 Yiheyuan Road, Haidian District, Beijing,100871, China.
Jilei Wu, Institute of Population Research/China Center on Population Health and Development, Peking University, No. 5 Yiheyuan Road, Haidian District, Beijing,100871, China.
Lijun Pei, Institute of Population Research/China Center on Population Health and Development, Peking University, No. 5 Yiheyuan Road, Haidian District, Beijing,100871, China.
Xuejun Shang, Department of Andrology, Jinling Hospital, School of Medicine, Nanjing University, No. 305, East Zhongshan Road, Nanjing, 210002, China.
Authors’ contributions
JJL and LJP were responsible for conceptualization of the study. JJL and SQL were responsible for the methodology. JJL was responsible for the software, formal analysis and writing the draft manuscript. JLW and LJP were responsible for the investigation. XJS and LJP were responsible for reviewing and editing the manuscript and the acquisition of funding. LJP was responsible for project administration. All authors have read and agreed to the published version of the article.
Funding
This work was supported by the National Key Research and Development Program of China (2018YFC1004303), National Natural Science Foundation of China (41871360) and National Health Commission Key Laboratory of Birth Defects Prevention, Henan Province (ZD202002).
Confict of interest
None declared.
Ethical approval
Not required.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1. Rudan I, Chan KY, Zhang JSet al. Causes of deaths in children younger than 5 years in China in 2008. Lancet. 2010;375(9720):1083–9. [DOI] [PubMed] [Google Scholar]
- 2. Groisman B, Bermejo-Sánchez E, Romitti PAet al. Join World Birth Defects Day. Pediatr Res. 2019;86(1):3–4. [DOI] [PubMed] [Google Scholar]
- 3. Carmona RH. The global challenges of birth defects and disabilities. Lancet. 2005;366(9492):1142–4. [DOI] [PubMed] [Google Scholar]
- 4. Li Z, Ren A, Zhang Let al. Prevalence of major external birth defects in high and low risk areas in China, 2003. Zhonghua Liu Xing Bing Xue Za Zhi. 2005;26(4):252–7. [PubMed] [Google Scholar]
- 5. Gu X, Lin L, Zheng Xet al. High prevalence of NTDs in Shanxi Province: a combined epidemiological approach. Birth Defects Res A Clin Mol Teratol. 2007;79(10):702–7. [DOI] [PubMed] [Google Scholar]
- 6. Li Z, Ren A, Zhang Let al. Extremely high prevalence of neural tube defects in a 4-county area in Shanxi Province, China. Birth Defects Res A Clin Mol Teratol. 2006;76(4):237–40. [DOI] [PubMed] [Google Scholar]
- 7. Li Z-w, Ren A-g, Zhang L. Epidemiology of major external birth defects in high risk areas of Shanxi province, China (2003). Chin J Birth Health Hered 2005;13(6):87–89. [Google Scholar]
- 8. Li Z, Ren A, Liu Jet al. Maternal flu or fever, medication use, and neural tube defects: a population-based case-control study in northern China. Birth Defects Res A Clin Mol Teratol. 2007;79(4):295–300. [DOI] [PubMed] [Google Scholar]
- 9. Li Z, Zhang L, Ye Ret al. Indoor air pollution from coal combustion and the risk of neural tube defects in a rural population in Shanxi Province, China. Am J Epidemiol. 2011;174(4):451–8. [DOI] [PubMed] [Google Scholar]
- 10. Zhang B-Y, Zhang T, Liang-Ming Let al. Correlation between birth defects and dietary nutrition status in a high incidence area of China. Biomed Environ Sci. 2008;21(1):37–44. [DOI] [PubMed] [Google Scholar]
- 11. Huang Y-F, Pan W-C, Tsai Y-Aet al. Concurrent exposures to nonylphenol, bisphenol A, phthalates, and organophosphate pesticides on birth outcomes: a cohort study in Taipei, Taiwan. Sci Total Environ. 2017;607–608:1126–35. [DOI] [PubMed] [Google Scholar]
- 12. Zhang JY, Wu QJ, Huang YHet al. Association between maternal exposure to ambient PM(10) and neural tube defects: a case–control study in Liaoning Province, China. Int J Hyg Environ Health. 2020;225:113453. [DOI] [PubMed] [Google Scholar]
- 13. Ren A, Qiu X, Jin Let al. Association of selected persistent organic pollutants in the placenta with the risk of neural tube defects. Proc Natl Acad Sci USA. 2011;108(31):12770–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pei L, Zhu H, Ye Ret al. Interaction between the SLC19A1 gene and maternal first trimester fever on offspring neural tube defects. Birth Defects Res A Clin Mol Teratol. 2015;103(1):3–11. [DOI] [PubMed] [Google Scholar]
- 15. Tian T, Wang L, Shen Yet al. Hypomethylation of GRHL3 gene is associated with the occurrence of neural tube defects. Epigenomics. 2018;10(7):891–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang L, Xiao Y, Tian Tet al. Digenic variants of planar cell polarity genes in human neural tube defect patients. Mol Genet Metab. 2018;124(1):94–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Huang Y, Ren A, Wang Let al. Casp8 hypomethylation and neural tube defects in association with polycyclic aromatic hydrocarbon exposure. Clin Epigenetics. 2019;11(1):72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lin S, Ren A, Wang Let al. Aberrant methylation of Pax3 gene and neural tube defects in association with exposure to polycyclic aromatic hydrocarbons. Clin Epigenetics. 2019;11(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhu H, Kartiko S, Finnell R. Importance of gene–environment interactions in the etiology of selected birth defects. Clin Genet. 2009;75(5):409–23. [DOI] [PubMed] [Google Scholar]
- 20. Pei L, Wu J, Li Jet al. Effect of periconceptional folic acid supplementation on the risk of neural tube defects associated with a previous spontaneous abortion or maternal first-trimester fever. Hum Reprod. 2019;34(8):1587–94. [DOI] [PubMed] [Google Scholar]
- 21. Kalra S, Dewan P, Batra Pet al. Organochlorine pesticide exposure in mothers and neural tube defects in offsprings. Reprod Toxicol. 2016;66:56–60. [DOI] [PubMed] [Google Scholar]
- 22. Shaw GM, Wasserman CR, O'Malley CDet al. Maternal pesticide exposure from multiple sources and selected congenital anomalies. Epidemiology. 1999;10(1):60–6. [PubMed] [Google Scholar]
- 23. Liu HB, Li ZH, Zhang YGet al. Nitrate contamination of groundwater and its affecting factors in rural areas of Beijing plain. Acta Pedol Sin. 2006;43(3):413. [Google Scholar]
- 24. Sun B, Zhang L, Yang Let al. Agricultural non-point source pollution in China: causes and mitigation measures. Ambio. 2012;41(4):370–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chen Y, Hu W, Huang Bet al. Accumulation and health risk of heavy metals in vegetables from harmless and organic vegetable production systems of China. Ecotoxicol Environ Saf. 2013;98:324–30. [DOI] [PubMed] [Google Scholar]
- 26. Wu J, Zhang C, Pei Let al. Association between risk of birth defects occurring level and arsenic concentrations in soils of Lvliang, Shanxi province of China. Environ Pollut. 2014;191:1–7. [DOI] [PubMed] [Google Scholar]
- 27. Jin X, Tian X, Liu Zet al. Maternal exposure to arsenic and cadmium and the risk of congenital heart defects in offspring. Reprod Toxicol. 2016;59:109–16. [DOI] [PubMed] [Google Scholar]
- 28. Pi X, Qiao Y, Wei Yet al. Concentrations of selected heavy metals in placental tissues and risk for neonatal orofacial clefts. Environ Pollut. 2018;242:1652–8. [DOI] [PubMed] [Google Scholar]
- 29. Stillerman KP, Mattison DR, Giudice LCet al. Environmental exposures and adverse pregnancy outcomes: a review of the science. Reprod Sci. 2008;15(7):631–50. [DOI] [PubMed] [Google Scholar]
- 30. Heeren GA, Tyler J, Mandeya A. Agricultural chemical exposures and birth defects in the Eastern Cape Province, South Africa: a case–control study. Environ Health. 2003;2(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kielb C, Lin S, Herdt-Losavio Met al. Maternal periconceptional occupational exposure to pesticides and selected musculoskeletal birth defects. Int J Hyg Environ Health. 2014;217(2–3):248–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Restrepo M, Munoz N, Day Net al. Birth defects among children born to a population occupationally exposed to pesticides in Colombia. Scand J Work Environ Health. 1990;16(4):239–46. [DOI] [PubMed] [Google Scholar]
- 33. Rull RP, Ritz B, Shaw GM. Neural tube defects and maternal residential proximity to agricultural pesticide applications. Am J Epidemiol. 2006;163(8):743–53. [DOI] [PubMed] [Google Scholar]
- 34. Yu H-y, Zhang K-l. Links between environmental geochemistry and rate of birth defects: Shanxi Province, China. Sci Total Environ. 2011;409(3):447–51. [DOI] [PubMed] [Google Scholar]
- 35. Arcaya M, Brewster M, Zigler CMet al. Area variations in health: a spatial multilevel modeling approach. Health Place. 2012;18(4):824–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Besag J, York J, Mollié A. Bayesian image restoration, with two applications in spatial statistics. Ann Inst Stat Math. 1991;43:1–20. [Google Scholar]
- 37. Lichstein JW, Simons TR, Shriner SAet al. Spatial autocorrelation and autoregressive models in ecology. Ecol Monogr. 2002;72(3):445–63. [Google Scholar]
- 38. Anselin L. Local indicators of spatial association—LISA. Geogr Anal. 1995;27(2):93–115. [Google Scholar]
- 39. Anselin L, Syabri I, Smirnov O. Visualizing multivariate spatial correlation with dynamically linked windows. Urbana. 2002;51:61801. [Google Scholar]
- 40. Westreich D, Greenland S. The table 2 fallacy: presenting and interpreting confounder and modifier coefficients. Am J Epidemiol. 2013;177(4):292–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lindgren F, Rue H. Bayesian spatial modelling with R-INLA. J Stat Softw. 2015;63(19):1–25. [Google Scholar]
- 42. Peng K, Zhu B, Kazuko A. Study on the input and output parameters and the balance of nitrogen in the eco-system of purple soil watershed. J Mt Sci. 2001;19:30–5. [Google Scholar]
- 43. Gimeno-García E, Andreu V, Boluda R. Heavy metals incidence in the application of inorganic fertilizers and pesticides to rice farming soils. Environ Pollut. 1996;92(1):19–25. [DOI] [PubMed] [Google Scholar]
- 44. Wong M. Heavy metal contamination of soils and crops from auto traffic, sewage sludge, pig manure and chemical fertilizer. Agri Ecosyst Environ. 1985;13(2):139–49. [Google Scholar]
- 45. Hu A, Yu Z, Liu Xet al. The effects of irrigation and fertilization on the migration and transformation processes of main chemical components in the soil profile. Environ Geochem Health. 2019;41(6):2631–48. [DOI] [PubMed] [Google Scholar]
- 46. Holtby CE, Guernsey JR, Allen ACet al. A population-based case-control study of drinking-water nitrate and congenital anomalies using Geographic Information Systems (GIS) to develop individual-level exposure estimates. Int J Environ Res Public Health. 2014;11(2):1803–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Pérez AL, Anderson KA. DGT estimates cadmium accumulation in wheat and potato from phosphate fertilizer applications. Sci Total Environ. 2009;407(18):5096–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Garcia AM. Birth defects in an agricultural environment. In: Jacobs M, Dinham B, editors. Silent invaders: pesticides, livelihoods and women's health. New Delhi: Orient Longman; 2004:159–166. [Google Scholar]
- 49. Brender JD, Suarez L, Felkner Met al. Maternal exposure to arsenic, cadmium, lead, and mercury and neural tube defects in offspring. Environ Res. 2006;101(1):132–9. [DOI] [PubMed] [Google Scholar]
- 50. Jin L, Zhang L, Li Zet al. Placental concentrations of mercury, lead, cadmium, and arsenic and the risk of neural tube defects in a Chinese population. Reprod Toxicol. 2013;35:25–31. [DOI] [PubMed] [Google Scholar]
- 51. Demir N, Başaranoğlu M, Huyut Zet al. The relationship between mother and infant plasma trace element and heavy metal levels and the risk of neural tube defect in infants. J Matern Fetal Neonatal Med. 2019;32(9):1433–40. [DOI] [PubMed] [Google Scholar]
- 52. Subramanian S, Jones K, Kaddour Aet al. Revisiting Robinson: the perils of individualistic and ecologic fallacy. Int J Epidemiol. 2009;38(2):342–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Wu J, Wang J, Meng Bet al. Exploratory spatial data analysis for the identification of risk factors to birth defects. BMC Public Health. 2004;4:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Savci S. An agricultural pollutant: chemical fertilizer. Int J Environ Sci Dev. 2012;3(1):77–80. [Google Scholar]
- 55. Wang JF, Li XH, Christakos Get al. Geographical detectors-based health risk assessment and its application in the neural tube defects study of the Heshun Region, China. Int J Geogr Inf Sci. 2010;24(1):107–27. [Google Scholar]
- 56. Chen L, Bell EM, Caton ARet al. Residential mobility during pregnancy and the potential for ambient air pollution exposure misclassification. Environ Res. 2010;110(2):162–8. [DOI] [PubMed] [Google Scholar]
- 57. Hodgson S, Lurz PW, Shirley MDet al. Exposure misclassification due to residential mobility during pregnancy. Int J Hyg Environ Health. 2015;218(4):414–21. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.