Abstract
Myopia typically starts and progresses during childhood, but onset and progression can occur during adulthood. The goals of this review are to summarize published data on myopia onset and progression in young adults, aged 18 to 40 years, to characterize myopia in this age group, to assess what is currently known, and to highlight the gaps in the current understanding. Specifically, the peer-reviewed literature was reviewed to: characterize the timeline and age of stabilization of juvenile-onset myopia; estimate the frequency of adult-onset myopia; evaluate the rate of myopia progression in adults, regardless of age of onset, both during the college years and later; describe the rate of axial elongation in myopic adults; identify risk factors for adult onset and progression; report myopia progression and axial elongation in adults who have undergone refractive surgery; and discuss myopia management and research study design. Adult-onset myopia is common, representing a third or more of all myopia in western populations, but less in East Asia, where onset during childhood is high. Clinically meaningful myopia progression continues in early adulthood and may average 1.00 diopters (D) between 20 and 30 years. Higher levels of myopia are associated with greater absolute risk of myopia-related ocular disease and visual impairment, and thus myopia in this age group requires ongoing management. Modalities established for myopia control in children would be options for adults, but it is difficult to predict their efficacy. The feasibility of studies of myopia control in adults is limited by the long duration required.
Keywords: myopia, axial length, contact lenses, myopia control, adults
Although the majority of myopia appears and progresses during childhood, it has long been recognized that refractive changes persist throughout adulthood. In his seminal monograph, Goldschmidt1 observed that some individuals develop myopia after the cessation of body growth. He termed this type of myopia spätmyopie or late myopia. He also noted that it was typically associated with environmental factors, such as large amounts of near work. Grosvenor2 proposed four categories based on age of onset: congenital, youth-onset, early adult-onset, and late adult-onset. Youth-onset myopia, more commonly referred to as juvenile-onset myopia,3 accounts for most cases. In Grosvenor's construct, young adult-onset myopia encompassed onset from 20 years to around 40 years. This category is the focus of this paper, with a minor modification to the age range. Although some authors have adopted Grosvenor's lower age limit of 20 years as their criterion for the lower bound of adulthood,4,5 a more common and convenient cut point of 18 years has been used by others, as it represents the most common age at which individuals graduate high school and begin college.6–9 Hereafter, the terms adult-myopia onset and adult myopia progression are used. Refractive error changes beyond this age have been documented elsewhere, can be strongly influenced by changes to the crystalline lens,10 and are not discussed here.
Now that a number of optical11–13 and pharmaceutical therapies14 have been shown to substantially reduce myopia progression in children,15–17 eyecare practitioners are speculating about how to manage progression in young adults. Although a large number of studies were identified showing that myopia can emerge and progress in young adults, particularly in college and university students, there are no large clinical studies investigating myopia control in this age group.
In this summary of the published peer-reviewed literature, the following aspects are addressed:
-
•
What is the typical timeline and age of stabilization of juvenile-onset myopia?
-
•
How common is adult-onset myopia?
-
•
How rapidly does myopia progress in adults, both during the college years and later?
-
•
What is the rate of axial elongation in myopic adults?
-
•
What are the risk factors for adult onset and progression?
-
•
What are the rates of myopia progression and axial elongation in adults who have undergone refractive surgery?
-
•
Finally, when is myopia management necessary in adults and what are the research study design issues for determining myopia control treatment efficacy in this age group?
When Does Juvenile-Onset Myopia Stabilize?
Childhood or juvenile-onset myopia begins when the human eye is still growing.3 Onset most commonly occurs between 8 and 13 years, with some variation across races and populations.18–20 In contrast, adult-onset myopia and progression occur in eyes for which normal eye growth has ceased.21,22 Whereas the trajectory of myopia progression in children has been well described,23–25 data on the stabilization of juvenile-onset myopia are surprisingly scarce. The long duration of myopia progression in children, its exponential slowing,26,27 and difficulties in following children as they transition through the education system and into the workforce creates challenges in accurately identifying the age at which myopia progression ceases.
A 1983 retrospective study analyzed 299 patient records of myopic children from 3 optometry practices.28 Estimates of the age at which myopia stabilized were derived using four different analyses—two graphical and two based on regression analysis. All four methods suggested that myopia stabilizes earlier in female patients than in male patients: 14.4 to 15.3 years versus 15.0 to 16.7 years. There was, however, a great deal of individual variability in the age of stabilization—the standard deviation was around 2 years for both genders, and the authors did not consider the influence of the degree of myopia.
A more recent retrospective study reported the rate of soft contact lens power change and its associated predictive factors in 912 wearers aged between 8 and 22 years in the Contact Lens Assessment in Youth Study.29 Participants with at least 6 months of follow-up were included (4341 visits, mean follow-up 25 months), comprising 37% wearers of hydrogel and 63% of silicone hydrogel lenses. During this period 36% had a change in lens power of at least −0.50 diopters (D). The mean annualized power change decreased with age: −0.31 D/year for 8- to 13-year-olds to −0.10 D/year for 20- to 22-year-olds. The latter value is smaller than the 0.25 D increments available for contact lenses, reflecting the fact that much of the myopia had stabilized by this age. Furthermore, each year there was a 16% reduction in the likelihood that an increase in minus lens power was required. This agrees with the yearly slowing of annual axial elongation in myopic children.30
Few studies have followed myopic children from childhood into their college years, the exception being the Correction of Myopia Evaluation Trial (COMET), which estimated the age and the myopia level at stabilization and evaluated associated factors.31 This was a carefully designed prospective study that collected longitudinal refractive data over 11 years from a large ethnically diverse cohort in the United States. Right eye data from 440 of the original 469 children with at least 6 years of follow-up and at least 7 refraction measurements after the age of 11 years were available for analysis. Age and myopia at stabilization could be established in 426 participants. The mean age at which myopia stabilized (defined as the age at which the estimated spherical refractive error was within 0.50 D of the asymptote) was 15.6 ± 4.2 years, and the mean refractive error at this point was −4.87 ± 2.01 D. Ethnicity was associated with the age at stabilization, but not gender, contrasting with the difference observed in a prior study.28 This may be due to changes in attitudes toward education and gender over the 30 years between studies, or simply the prospective nature and rigor of the more recent work.28,31 African Americans stabilized at a mean of 13.8 years, significantly younger that the 15.8 to 16.3 years for other ethnicities and had the least myopia at stabilization (mean: −4.36 vs. −4.87 to −5.45 D), although the authors note that this “may be influenced by factors in the visual or social environment.”31
Around half (48%) of the COMET cohort were stable by 15 years of age. The proportion whose myopia had stabilized increased to 77% (330 of 426) by age 18 years and to 90% (384 of 426) by age 21 years. COMET began as a 3-year clinical trial to evaluate whether progressive addition lenses (PALs) slowed myopia progression. Age and myopia at stabilization were similar between those who wore PALs (n = 211, 15.7 years, and –4.9 D) and single vision lenses (n = 215, 15.5 years, and –4.9 D) for the first 3 years. These data, therefore, show that over 50% of children are still progressing at 15 years, nearly 25% at 18 years, and 10% at age 21 years. These latter statistics may be an underestimate as they only include children whose myopia developed at a young age. This is because the original COMET study recruited children between the age of 6 and 11 years with at least −1.25 D of myopia.
The Myopia of Adulthood
Although the majority of myopia appears during childhood2 and stabilizes by the age of 18 years,28,31 a number of individuals may still exhibit myopic changes as adults.2 This may be an increase in myopia in an existing myopic individual, that is, adult myopia progression, or the onset of myopia in an emmetrope or hyperope, such as adult-onset myopia. The US National Research Council Committee on Vision Working Group on Myopia Prevalence and Progression32 reviewed over 500 articles on myopia. Their main conclusion was that up to 40% of low hyperopes and emmetropes entering university and military academies were likely to become myopic by the age of 25 years, compared with less than 10% of those not attending university, thus emphasizing the important role of environmental factors in the development of myopia in this age group.32 Their comprehensive review of the literature includes work from the 19th and early 20th centuries.
As described in the introductory paragraph, Grosvenor's classification of 40 years as the upper age limit for young adult-onset myopia2 has been adopted in this white paper, whereas using the more convenient cut point of 18 years as the lower limit. Some data beyond this range are included to inform the discussion. Studies of university students have divided juvenile- or youth-onset myopia into early- and late-onset myopia, using 15 years as the cut point.33,34 The International Myopia Institute (IMI) report on Defining and Classifying Myopia considered age of onset as a possible basis for classification of myopia, but concluded that it was unclear “whether the biological processes underlying myopia at age 7 differ from those in myopia that develop in early adults.”3 For the remainder of this paper, the criteria used by various authors is specified. Regardless, the criterion merely provides an arbitrary quantization of a continuous distribution of age of onset and does not necessarily establish a category of myopia with a separate etiology. In the following sections, unless stated, values are for spherical equivalent and myopia is defined as −0.50 D or worse.3
How Common Is Adult-Onset Myopia?
Cross-Sectional Studies of Adult-Onset Myopia
A number of cross-sectional studies have estimated the proportion of all cases of myopia represented by adult-onset myopia in samples with mean ages from 21 to 52 years. Table 1 summarizes cross-sectional studies reporting the frequency of adult-onset myopia, all relying on self-reported age of onset.4–9,35–42 Obtaining the age of onset through questionnaires has been shown to have good validity,43 particularly in adults.44 The quoted proportion varies from 15 to 80% across these studies, with 30 to 50% most commonly reported with a median of 42%. The details of these studies, the participant demographics, and other potential reasons for the differences are discussed.
Table 1.
Cross-Sectional Studies of Self-Reported Age of Myopia Onset in Adults and the Proportion With Adult-Onset Myopia
| Authors | Population | Number With Myopia/Total | Age Range (Years) | Mean Age (Years) | Criteria for Adult Onset (Years) | % Adult Onset |
|---|---|---|---|---|---|---|
| Septon35 | US optometry students | 332/447 | 20 to 27 | 25 | 16 | 19% |
| Shulkin and Bari6 | US medical students | 107/150 | 21 to 29 | 24.3 | 18 | 43% |
| Bullimore et al.36 | UK optometry students | 105/189 | 18 to 36 | 20.7 | 15 | 41% |
| Midelfart et al.5 | Norwegian medical students | 67/133 | 21 to 33 | 24.9 | 20 | 43% |
| McBrien and Adams4 | UK microscopists | 163/245 | 21 to 63 | 30 | 20 | 48% |
| Loman et al.7 | US law students | 110/177 | 23 to 44 | 27 | 18 | 30% |
| Ting et al.42 | Hong Kong microscopists | 47/54 | 22 to 44 | 31 | 16 | 25% |
| Iribarren et al.37 | Argentinian office workers | 95/349 | 25 to 65 | 37.6 | 18 | 48% |
| Bullimore et al.38 | US university staff | 396/396 | 25 to 35 | 30.7 | 15 | 37% |
| Onal et al. 8 | Turkish medical students | 68/270 | 18 to 26 | 21.1 | 18 | 15% |
| Dirani et al.9 | Australian twins | 347/1,170 | 18 to 86 | 52 | 18 | 28% |
| Iribarren et al.39 | Argentinian office workers | 347/347 | 25 to 65 | 42.6 | 19 | 51% |
| Rahi et al.40 | UK adults | 1,214/2,487 | 44 | 44 | 16 | 81% |
| Malik et al.41 | Pakistani medical students | 92/110 | 65% below 22 | 21? | 18 | 62% |
Studies are listed in chronological order.
Several authors have reported the age of onset of myopia among students in professional programs. A questionnaire was distributed to 150 freshman and sophomore medical students, aged 21 to 29 years and a comparison group of 150 art students of the same age range.6 Of those questioned, 71% of the medical students wore corrective lenses, compared with 37% of the art students. Among the medical students wearing corrective lenses, over 40% obtained their eyewear after 18 years of age, compared with 19% of art students. Among medical students, 55% of first years and 74% of second years reported worsening of their eyesight since leaving high school, compared with only 22% of art students. The authors attribute the changes to accommodative spasm, an explanation that has not stood the test of time, given that adult myopia onset and progression have been shown to be axial in origin.4 In an examination of 133 Norwegian engineering students at the end of their training,5 50% were myopic (mean = −2.34 ± 2.01 D). Of the myopic students wearing corrective lenses, 43% stated that they received the first prescription at or after the age of 19 years. The mean age at first prescription was 16.2 ± 4.9 years (range = 7 to 23 years). Age of myopia onset was also surveyed in 177 third-year law students aged between 23 and 44 years,7 of whom 66% were myopic with a median refractive error of −3.00 D (interquartile range = −1.69 to −5.00 D). Of the 110 students in whom age of onset of myopia could be established, 70% developed myopia prior to college, 17% between entering college and entering law school, and 13% during law school. Finally, among 270 Turkish medical students aged 18 to 26 years,8 33% were myopic (at least −0.75 D) of whom 15% reported onset at age 18 years or older.
Among 396 myopic university employees between 25 and 35 years of age,38 37% developed myopia after the age of 15 years. Those reporting onset prior to 15 years had significantly higher levels of myopia (mean = −4.23 ± 1.71 D) than the later onset group (mean = −2.40 ± 1.18 D), and each year of later onset was associated with −0.16 D less myopia. Two studies of Argentinian office workers report higher frequencies of adult-onset myopia. The first reported on 349 workers aged 25 to 65 years consecutively attending a general health examination.37 Of the 117 myopic adults, 48% reported receiving their first prescription at 18 years or older. The second study used the same recruitment method, but only reported results on myopic adults aged 25 to 65 years.39 Of the 397 examined 347 reported their age of first prescription, with 51% receiving it at 19 years or older.
The frequency of adult-onset myopia was assessed in 1224 White Australian twins between 18 and 86 years of age.9 Refractive error data were available on 1170 twins of whom 347 (30%) were myopic. Of those with myopia, 96 (28%) reported receiving their first spectacle or contact lens correction at or after 18 years. More than 90% of those with adult-onset myopia reported onset between the ages of 18 and 30 years, the remainder between 31 and 45 years.
The incidence of adult-onset myopia has been reported to be markedly higher in some occupational groups. In a comprehensive assessment of 251 UK clinical microscopists aged 21 to 63 years,4 163 (67%) were myopic of whom 78 (48%) developed myopia after the age of 20 (based on their table 1, which presents data on 245 right eyes). Among the early onset participants, 38 (23%) developed myopia between the age of 15 and 20 years and 47 (29%) prior to the age of 15 years. The mean refractive error in these 3 groups was −1.68 ± 1.15, −2.46 ± 1.66, and −3.74 ± 2.13 D, respectively. A smaller study of 54 Hong Kong microscopists found that 47 (87%) were myopic, of whom 12 (25%) developed myopia after the age of 16 years. Fifty-five percent of the myopic adults reported an increase of between −0.25 and −1.00 D when they last updated their prescriptions.42
The highest proportion of adult-onset myopia has been reported in a cohort of 2487 randomly selected 44-year-old members of the 1958 British birth cohort (27% subsample).40 Participants were dichotomized as early (by 16 years) or late-onset, using a combination of information from prior examinations, parental reports, use of spectacles, and medical records at 7, 11, and 16 years, in the absence of refraction data. Based on non-cycloplegic auto-refraction, 1214 of the 44-year-olds (49%) were myopic (at least −0.75 D). Of these, a remarkable 979 (81%) had self-reported myopia onset at or after 16 years. This implies that less than 19% of this cohort were myopic prior to 16 years (in 1974), but this is consistent with other reports of largely White children in the United Kingdom,45 although refractive error was not measured in this cohort until the age of 44 years.46 Overall, the prevalence of myopia reported is high, but the proportion of participants with late-onset (81%) is even higher than the 48% of microscopists who report onset after the age of 15 years.4 In summary, these data are challenging to reconcile with other work, although the cohort is older and born earlier than other studies.
Longitudinal Studies of Adult-Onset Myopia
A number of prospective studies have documented the incidence of adult-onset myopia, and these are summarized in Table 2.4,47–55 Most report data on university students, followed as they progress through their degree courses. There is good consensus across the studies—many of the myopes progressed during this time, and a meaningful portion of emmetropes, but very few hyperopes, developed myopia. The annual incidence of new myopia cases ranged from 10 to 24% across the studies with most reporting an annual incidence between 5 and 14%. Rather than presenting studies in the chronological order in which they appear in Table 2, we discuss them by cohort type: military personnel, engineering students, medical students, an occupational group, and a birth cohort.
Table 2.
Longitudinal Studies of Adult-Onset Myopia
| Author | Population | Number of Emmetropes/Total | Mean Age (Years) | Duration (Years) | Incidence | 95% CI | Annual Incidence | Percentage of All Myopes With Adult Onset |
|---|---|---|---|---|---|---|---|---|
| O'Neal and Connon47 | US military recruits | 184/994 eyes | 17 to 21 | 2.5 | 22% | 16 to 35% | 9% | 9% |
| Lin et al.55 | Taiwanese medical students | 25/345 | 18 to 21 | 5 | 42% | 23 to 59% | 5% | 3% |
| McBrien and Adams4 | UK microscopists | 95/332 eyes | 21 to 63 | 2 | 48% | 38 to 59% | 24% | 17% |
| Kinge and Midelfart.48 | Norwegian engineering students | 49/192* | 20.6 | 3 | 59% | 44 to 73% | 20% | 20% |
| Fesharaki et al.49 | Iranian medical students | 70/131 | 19.8 | 5.5 | 33% | 22 to 45% | 6% | 27% |
| Jorge et al.50 | Portuguese university students | 34/118 | 20.6 | 3 | 15% | 5 to 31% | 5% | 16% |
| Jacobsen et al.51 | Danish medical students | 90/156* | 23.1 | 2 | 12% | 6 to 21% | 6% | 17% |
| Lv and Zhang52 | Chinese university students | 400/2,053 | 18.3 | 2 | 28% | 24 to 33% | 14% | 6% |
| Lee et al.53 | Australian birth cohort | 516/813 | 18 to 22 | 8 | 14% | 11 to 17% | 2% | 29% |
| Duan et al.54 | Chinese medical students | 20/291 | 18.7 | 2 | 10% | 3 to 30% | 5% | 1% |
The number of emmetropes is shown as well as the total number of participants. The incidence is based on the number of emmetropes.
Studies are listed in chronological order. All except McBrien and Adams4 used cycloplegic refraction.
Includes both emmetropes and hyperopes.
Data were reported from the physical examinations of recruits at the United States Air Force Academy, covering 2.5 years, from entrance to third year.47 Among 497 cadets, aged 17 to 21 years at entrance, 184 eyes (18.5%) were classified as emmetropic (–0.12 to +0.12 D). Over 2.5 years, the mean change was −0.21 D, with 25% progressing by at least −0.50 D. From the data presented, it can be estimated that 22% of emmetropes were at least −0.50 D myopic after 2.5 years. An earlier Dutch study of 18 to 20-year-old pilots who had no myopia at baseline reported 5% of the hyperopes and 31% of the emmetropes became myopic during the first 2 years of their education.56 In a 3-year longitudinal cohort study of 224 Norwegian engineering students, 192 completed the study.48 Over the 3 years, 29 of the 49 emmetropes (59%) and 4 of the 51 hyperopes became myopic (8%). In a corresponding 3-year longitudinal study of 118 Portuguese university students,50 5 of the 34 emmetropes (15%) and one of the 58 hyperopes (2%) became myopic.
Refractive error trends in medical students have been studied in a number of countries. In a 5.5-year longitudinal study of 150 randomly selected first-year Iranian medical students, 131 completed the study.49 Myopia, defined as at least −0.25 D spherical equivalent, was present in 62 (47%) students at baseline and 84 (64%) at the end of the study, with 33% of the non-myopic eyes becoming myopic. In a 2-year longitudinal study of 143 Danish first year medical students,51 11 of the 90 nonmyopic students developed myopia (12%). In a 2-year study of 2053 Chinese medical students,52 the overall prevalence of myopia increased significantly from 79 to 84%. In other words, of the 400 students classified as emmetropic at the start of the study, 112 became myopic by the end (28%). The median age of onset of myopia in initially emmetropic eyes was 26 years. In a second, smaller Chinese study54 of 291 medical students, only 20 were non-myopic at baseline and became myopic (10%) over 2 years.
Two studies evaluated non-university cohorts. In the aforementioned study of clinical microscopists, 166 completed a 2-year longitudinal study.4 Of the 95 eyes emmetropic at the start of the study, 37 (39%) underwent a myopic shift greater than −0.37 D (mean = −0.58 ± 0.24 D) and 24 eyes (26%) became myopic. This was associated with a vitreous chamber elongation of 0.26 ± 0.30 mm.
A birth cohort of Australians have been followed since their prenatal periods in 1989 to 1991 when nearly 3000 pregnant women were recruited. At the 20-year follow-up, 1328 participants underwent their first study eye examination which included cycloplegic autorefraction and ocular biometry.53 Eight years later, participants were invited to return for a second eye examination. Among the 701 participants who attended for both examinations, 516 were emmetropic or hyperopic at the first examination and, 8 years later, 72 had developed myopia (14%).
It is also worth noting a recent study of 800 Chinese male emmetropic teenagers (14- to 16-years of age) who do not quite meet the age criteria for young adults.57 Students with cycloplegic refractive error between −0.25 and +1.75 D were followed for 20 months. The mean refractive error changed from +0.39 ± 0.44 D at baseline to −0.10 ± 0.38 D, a change of −0.50 D (95% confidence interval [CI] = −0.53 to −0.47) and 124 of the students became myopic (16%), although the criterion for myopia was not specified.
Summary of Myopia Onset in Adults
In summary, cross-sectional studies show that a meaningful proportion of individuals report developing myopia after leaving high school (see Table 1). It is important to note that most individuals obtain their first driver's license or learner's permit between 15 and 18 years of age. As part of the process, they may discover, for the first time, that they have myopia. This may influence the reporting of age of onset, as many are entering employment or beginning military service.
The criterion for late-onset or adult-onset myopia adopted by authors ranges from 15 years to 20 years, making direct comparison difficult. Equally challenging is the variation in age of participants being surveyed. Figure 1 shows the relationship between the proportion of adult-onset myopia as a function of the age of the participants surveyed. One hypothesis is that the older the sample, the higher the proportion of adult-onset myopia, but the relationship is not significant (r2 = 0.07, P = 0.37).
Figure 1.
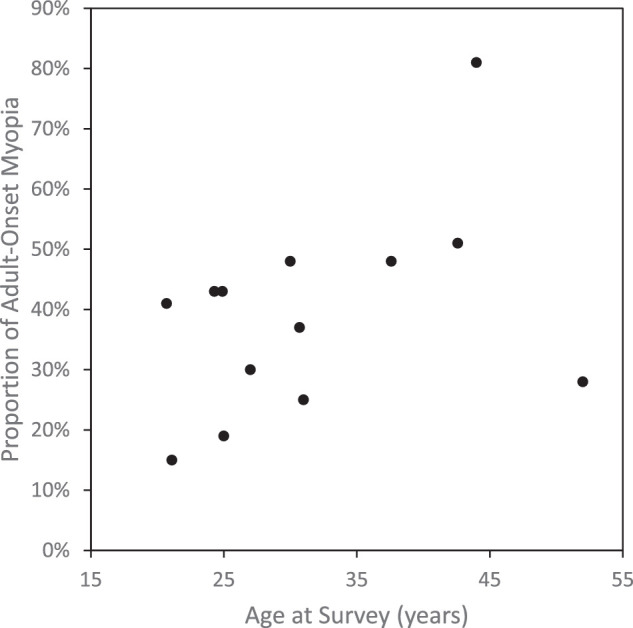
The proportion of myopia that is adult-onset as a function of the mean age of surveyed participants. The data are from the 14 studies listed in Table 1.
Prospective studies of emmetropic adults, demonstrate that many enrolled in college, graduate, or professional education programs, or in certain occupations will become myopic. Clearly the proportion of adult-onset myopia will be low in a group or population with a high prevalence of juvenile-onset myopia, but the incidence of adult-onset myopia among those reaching adulthood without myopia may still be meaningful. In this respect, most of the studies discussed above are from outside of East Asia. Adult-onset myopia is rare in that part of the world and anyone likely to develop myopia exhibit it before 18 years (see Table 2).
Adult Myopia Progression
There have been a number of reports of myopia progression in adulthood,4,44,48,50,51,58–62 some of which document myopia progression beyond 30 years of age.4,59,62 The studies of adult populations 25 years and younger are discussed first and summarized in Table 3 (many of these also appear in Table 2). Some of these studies report refractive changes in all participants, but where available, data are shown for myopic adults only. The studies of adult populations 25 to 40 years are summarized in Table 4. Comparison of progression in the 2 age groups shows that the myopia progression continues beyond 25 years, albeit at a slower rate.
Table 3.
Studies of Myopia Progression in Adults 18 to 25 Years
| Author | Population | Number With Myopia/Total | Mean Age (Years) | Duration (Years) | Annual Progression (D) | Annual Axial Elongation (mm) | % Progressing ≥0.50 D |
|---|---|---|---|---|---|---|---|
| O'Neal and Connon47 | US military recruits | 439/994 eyes | 17 to 21 | 2.5 | −0.23 | — | 55% |
| Grosvenor and Scott58 | New Zealand optometry students and patients | 36/53 | 21.4 | 3 | −0.08 | +0.06 | 56%† |
| Lin et al.55 | Taiwanese medical students | 320/345 | 18 to 21 | 5 | −0.14 | — | — |
| Kinge and Midelfart48,63 | Norwegian engineering students | 92/192 | 20.6 | 3 | −0.22 | +0.13 | 32% |
| Jiang et al.64 | US Optometry students | 29/35 | 24.9* | 1 | −0.20* | — | — |
| Fesharaki et al.49 | Iranian medical students | 62/131 | 19.8 | 5.5 | −0.19 | — | 45% |
| Onal et al.8 | Turkish medical students | 89/207 | 21.1 | 1 | +0.02 | +0.01* | — |
| Jorge et al.50 | Portuguese university students | 26/118 | 20.6 | 3 | −0.10* | +0.04* | 22%* |
| Lv and Zhang52 | Chinese university students | 1,612/2,053 | 18.3 | 2 | −0.18 | — | |
| Jacobsen et al.51 | Danish medical students | 53/156 | 23.1 | 2 | −0.22 | +0.07* | — |
| Parssinen et al.65,66 | Finnish adults | 160 | 23.7 | 10 | −0.06 | +0.04 | 45% |
| Verkicharla et al.70 | Indian practice patients | 1,032 | 21 to 25 | 1 | −0.14 | — | — |
| Ducloux et al.69 | French spectacle wearers | 11,299 | 18 to 19 | 1 to 2.2 | −0.10 | — | — |
| Polling et al.68 | Dutch spectacle wearers | 1,270 | 19 to 21 | 3 | −0.08 | — | — |
| Lee et al.53 | Australian birth cohort | 177/813 | 18 to 22 | 8 | −0.04* | +0.02* | 38%* |
| Duan et al.54 | Chinese medical students | 271/291 | 18.7 | 2 | −0.20* | +0.05* | 26%* |
Table 4.
Studies of Myopia Progression in Adults 25 to 40 Years
| Author | Population | Number With Myopia/Total | Age (Years) | Duration (Years) | Annual Progression (D) | % Progressing |
|---|---|---|---|---|---|---|
| Zadnik and Mutti.71 | US law students | 87 | — | ∼4 | 47% by ≥0.50 D | |
| Waring et al.59 | Fellow eye of US RK patients | 45 | Mean = 33.5 | 10 | −0.06 | — |
| Ellingsen et al.60 | US practice patients | 39 | 30 to 39 | 10 | −0.04 | 32% by >0.50 D |
| McBrien and Adams4 | UK microscopists | 223/316 | Median = 29.9 | 2 | −0.18 | 48% by ≥0.37 D |
| Loman et al.7 | US law students | 96/177 | 27 | 2 | Self-report | 86% |
| Bullimore et al.62 | US soft contact lens wearers | 291 | Mean = 28.5 | 5 | −0.09 | 36% by ≥0.75 D 49% by ≥0.50 D |
| Bullimore et al.72 | US university staff | 268 | Mean = 30.7 | 5 | −0.03 | 5% by ≥0.75 D 16% by ≥0.50 D |
| Li et al.74 | Chinese rural adults | ?/595 | 30 to 39 | 5 | −0.03 | |
| Verkicharla et al.70 | Indian practice patients | 656 | 26 to 30 | 1 | −0.07 | — |
Myopia Progression in College-Aged Adults (18 to 25 Years)
Several studies on myopia progression, mostly longitudinal, in student populations have been published. As described above,47 among 497 US Air Force cadets, aged 17 to 21 years at entrance, 44% were myopic (at least −0.25 D). Over 2.5 years, the mean refractive change was −0.57 D with 55% progressing by at least −0.50 D. A 3-year study of 79 young adults included 29 who had developed myopia before 16 years and 26 years whose myopia developed at 16 years or later.58 Mean ages at baseline were 20.4 ± 1.0 and 22.4 ± 3.4 years, respectively, and both groups showed myopic changes: −0.26 ± 0.52 and −0.18 ± 0.40 D and correlated axial elongation of 0.18 ± 0.21 and 0.20 ± 0.18 mm.
In a 5-year longitudinal study of 345 Taiwanese medical students,55 93% were myopic at baseline. Mean refractive error increased significantly by −0.70 ± 0.65 and −0.54 ± 0.64 D for male and female students, respectively. Axial length increased by 0.49 mm, from 25.39 ± 1.34 to 25.88 ± 1.27 mm. Corneal curvature, anterior chamber depth, and lens thickness remained relatively unchanged. Subsequent studies confirm these findings in similar cohorts. In the aforementioned study of Iranian medical students,49 45 of the 62 initially myopic students (73%, data from the right eye), progressed by more than −0.50 D over the 5.5 years. In a cohort of 271 Chinese myopic medical students,54 72 (26.6%) progressed by at least −0.50 D over 2 years with a mean progression of −0.2 D and a mean axial elongation of 0.05 mm. The largest prospective study of myopia progression was a 2-year study of 2053 Chinese medical students.52 The 1612 participants who were myopic at baseline progressed by −0.36 ± 0.34 D. In a 2-year longitudinal study of 143 Danish first-year medical students,51 53 (37%) were myopic at baseline. After 2 years, these myopic students progressed by −0.40 ± 0.46 D. Axial length increased by 0.13 ± 0.13 mm across all students (separate data on myopic adults are not given). One study did not observe myopia progression among this high-risk student group. Among 270 Turkish medical students, 89 (33%) were myopic (at least −0.75 D).8 No change in refractive error (mean = +0.02 D) or axial length was observed after 1 year.
Other student cohorts show similar findings. In a 3-year longitudinal study of 224 Norwegian engineering students, 192 completed the study.48 At baseline, 48% of students were at least −0.25 D myopic. Over the 3 years, mean refractive error changed by a mean of −0.66 ± 0.51 D among those with myopia with 73% progressing by at least −0.37 D and 32% by at least −1.00 D. Biometric data were available on 73 myopic adults.63 Mean refractive change was −0.67 ± 0.43 D, accompanied by a 0.38 ± 0.30 mm increase in axial length. Around 80% of the axial elongation was due to increased vitreous chamber depth, with the remainder due to increased crystalline lens thickness.
Some studies do not present separate data for myopes. In a sample of 64 optometry students of whom 35 (29 with myopia) were examined a year later,64 the mean myopic shift was −0.20 D. In a longitudinal study of 118 Portuguese university science students,50 26 were initially myopic (22%). After 3 years, the mean change in refractive error among all students was −0.29 ± 0.38 D, with 26 (22%) changing by at least −0.50 D with a mean axial elongation of 0.11 ± 0.28 mm. Younger students were more likely to show clinically significant myopia progression. The mean myopic shift in the entire sample was about half that in the 3-year longitudinal study of Norwegian engineering students,48 perhaps due to the smaller proportion of myopic adults in the Portuguese sample as myopic shifts are greater in myopic than non-myopic adults.47,51,52
Non-university populations also show adult myopia progression, although the rates appear lower. In a longitudinal study that began as a clinical trial of 240 children aged 8 to 12 years, 20-year follow-up data were reported.65,66 Participants were examined annually for 3 years and twice thereafter at around 10-year intervals with data supplemented with values received from external clinicians. Adult progression data were available on 160 of the original cohort presented as a function of gender and parental history.66 Calculating mean values from the authors’ multiple tables reveals that from a mean age of 23.7 years, the 10-year myopia progression was −0.41 D and the 10-year axial elongation was 0.42 mm. In the earlier paper, the authors report that 45% of 147 adults progressed at least −0.50 D over 8 years.65
The Cambridge Anti-Myopia Study was a 2-year clinical trial in which neither a contact lens, nor vision therapy, or both influenced progression in 142 participants, aged 14 to 21 years.67 Ninety-five participants completed the 2-year trial. Among the 50% of participants over 16.9 years, the 2-year progression was around −0.25 D. Across all participants, the mean progression was −0.33 D and accompanied by a mean axial elongation of 0.15 mm.
As described earlier,53 a birth cohort of Australians aged 18 to 22 years were re-examined 8 years later. Among the 701 participants who attended both examinations, 177 were myopic at the first examination. The authors only report progression and elongation data for the entire group (see Table 3). Despite a low mean annual progression of −0.04 D, 38% of all participants progressed by at least −0.50 D over 8 years.
Finally, three recent studies report large practice-based datasets.68,69 Retrospective data on 2555 patients with myopia from a branch of opticians in the Netherlands were analyzed.68 Among the 1270 individuals with data at both 19 to 21 years and 22 to 25 years, the median annual progression was −0.08 D/year (interquartile range [IQR] = −0.21 to 0.00), but fewer than 10% progressed by more than −0.25 D/year. Likewise, a 6-year prospective study of 630,487 adults and teenagers with myopia used data from 696 opticians across France.69 Among the 20,044 patients examined at age 18 to 19 years, 11,299 received a second examination 12 to 26 months later and 1468 (13%) progressed by more than −0.50 D. Mean progression was −0.10 D/year. Finally, a retrospective study reported 1-year myopia progression in Indian myopes across different age groups.70 Mean myopia progression among the 1032 patients aged 21 to 25 years was −0.11 ± 0.51 D.
Myopia Progression in Adults 25 to 40 Years
A smaller number of studies, mostly retrospective, report myopia progression beyond college age, although some cohorts were in professional degree programs and are summarized in Table 4.4,7,59,60,62,70–74 Whereas some studies include adults younger than 25 years, the mean or median age is at least 27 years. Among the previously described group of law students,7 96 were myopic when entering law school. Myopia progression, defined as “a self-reported need for a stronger myopic spectacle prescription,” was reported by 83 students (86%) during law school. Even those adults with myopia over 30 years of age reported high rates of myopia progression (71%). In an earlier retrospective survey of 87 law students,71 previous spectacle correction was compared to the current refractive error. Forty-one students (47%) showed an increase of at least −0.50 D in at least one eye.
In the study of clinical microscopists aged 21 to 63 years, 166 completed a 2-year longitudinal study.4 Of the eyes that were myopic at the start of the study, 48% progressed by at least −0.37 D. The mean increase in myopia for this progressing group was −0.77 ± 0.31 D compared with −0.01 ± 0.21 D in the eyes that did not undergo a refractive change of at least −0.37 D. The only significant difference in ocular component changes for these two groups was vitreous chamber elongation (0.24 ± 0.42 mm vs. 0.03 ± 0.32 mm). Those progressing were younger than those not progressing (median = 29.3 vs. 34.4 years). This study appears to be the only report of acceleration of myopia when previously stable. Among myopes who progressed during the study, around 60% reported no change in refractive correction for the 5 years prior to becoming a clinical microscopist.
In the fellow eye of 47 patients with radial keratotomy who elected not to undergo surgery on their second eye (median refractive error in 675 eyes undergoing radial keratotomy = −3.87 D), there was a mean myopic shift of −0.65 D over 10 years.59 A retrospective study identified 208 adults with myopia who were followed for more than 20 years.60 Myopia increased by −0.60, –0.39, and −0.29 D per decade, among patients during their 20s, 30s, and 40s, respectively (n = 13, 39, and 65). Although practice-based data may be biased by those with myopia progression returning more frequently for care, the 20-year follow-up may limit this effect. A retrospective study of Indian myopes,70 reported 1-year myopia progression among 656 patients aged 26 to 30 years of −0.07 ± 0.54 D.
Another retrospective study62 reported a 5-year rate of myopia progression in soft contact lens wearers. Patients aged between 20 and 40 years and with at least 5 years of follow-up were selected from a clinical research database, resulting in 291 adults with a mean baseline refractive error of −3.29 ± 1.92 D and a mean age of 28.5 ± 5.0 years. Over 5 years, 21% progressed by at least −1.00 D, 36% progressed by at least −0.75 D, and 49% progressed by at least −0.50 D. Mean 5-year progression was −0.44 ± 0.60 D and decreased with increasing age. A subsequent 5-year prospective study enrolled 396 adults between 25 and 35 years of age, with at least −0.50 D spherical equivalent of myopia.72 Mean age was 30.7 ± 3.5 years and mean refractive error was −3.54 ± 1.77 D determined by cycloplegic auto-refraction. Of those enrolled, 268 (68%) completed the 5-year study. Of these, 5% progressed by at least −0.75 D. The less conservative criteria of −0.50 D gave a progression rate of 16%. The difference in progression rates between the above two studies is pronounced.62,72 They differ in their outcome measures with the retrospective study relying on presumably non-cycloplegic subjective refraction and the prospective study using cycloplegic auto-refraction. In the retrospective study, all participants were soft contact lens wearers in the 1980s and 1990s. Contact lens materials and designs have evolved with modern lenses being thinner and more oxygen permeable and this may have resulted in less myopic progression.75
Finally, 5-year refractive changes were reported in a rural Chinese adult population.74 Of the original cohort of 6830 adults aged 30 years and older, 5394 of the 6323 survivors participated in the 5-year follow-up. There were 595 individuals who were between 30 and 39 years at baseline and, among those myopic at baseline, the 5-year change in refractive error was −0.17 D. The number of participants with myopia is not specified, based on a previous paper it is around 40% in this age range.76
Summary of Refractive and Axial Length Changes in Adult Myopia Progression
Progression is very common in college-attending myopic adults, although the proportion of progressors varies with age, study duration, and criterion.8,48–52,55,58 Inspection of Table 3 suggests that the annual rate of progression in myopic adults aged 18 to 25 years is between −0.1 and −0.2 D/year with a crude average of −0.14 D/year. Half of the studies report rates at the upper end of this range, whereas one reports no mean change in refractive error. The lowest reported rate may be an underestimate as it represents all students of whom only 22% were myopic.50 Studies that are not limited to college students show lower rates of progression.53,58,65 Like progression during childhood, progression in adulthood slows with age. Between 25 and 40 years, annual progression is usually lower than −0.1 D/year. Of course, the mean change in refractive error masks the presence of a subset of fast progressors (see the last column of Table 4) and a small group showing hyperopic shifts.
Figure 2 shows the relationship further by plotting mean annual progression and age at the midpoint of the study period. Linear regression shows a significant relationship (r2 = 0.23, P = 0.02), although an exponential fit might be more appropriate.30 The gradient of the slope is +0.055 D per decade (95% CI = +0.009 to +0.102). Methodology differs among studies with most of those on college students (see Table 3) using cycloplegic refraction and most of those on adults 25 years and older (see Table 4) using non-cycloplegic refraction. This distinction is made in Figure 2 with no clear suggestion of bias introduced by the lack of cycloplegia.
Figure 2.
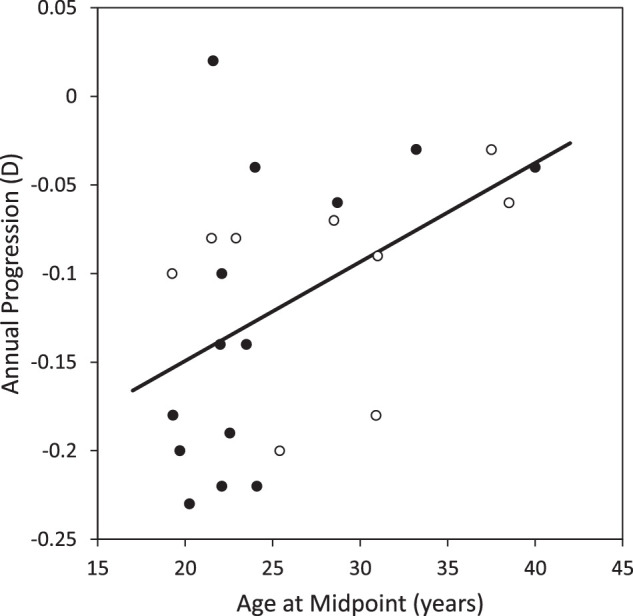
Mean annual myopia progression as a function of age at the midpoint of the study period. The data are from the 23 of the 25 studies listed in Tables 3 and 4 with data on myopia progression. Closed symbols are data based on cycloplegic refraction. Open symbols are data based on non-cycloplegic refraction.
Revisiting the comprehensive COMET data,31 the authors found that 25% of the 426 myopic individuals were still progressing at 18 years. It is important to note that their criterion for progression beyond this age was greater than −0.50 D, albeit over multiple years, so a quarter of those with early onset myopia could be expected to progress significantly during college. Note that these participants all developed myopia prior to the age of 10 years, and myopia of later onset may progress later into adolescence and adulthood.
Early cross-sectional studies suggested that adult myopic changes are a result of axial elongation.77–81 This has been supported unequivocally by longitudinal studies.4,50,51,55,58,63 A recent review of axial length changes in adults showed that reports of axial length decreasing with age were artifacts of using cross-sectional data.82 Inspection of Table 3 suggests that the annual rate of axial elongation in myopic adults between 18 and 25 years is between 0.05 and 0.1 mm/year with a crude average of 0.07 mm/year. Five of the seven studies only report elongation for all subjects, so the rates in these studies are likely to be slightly higher among myopic adults. For reference, a recent analysis of annual rates of axial elongation among myopic children predicts 1-year elongation of 0.09 and 0.07 mm in 18-year-old East Asians and Non-East Asians, respectively, and 0.06 and 0.05 mm in 21-year-olds.30 The ratio of mean myopia progression (–0.14 D/year) to mean axial elongation (0.07 mm/year) is around −2 D/mm (see Table 4), consistent with data from 3-year clinical trials in myopic children.11,83 In adults 25 years and older, the ratio may be slightly higher, with one study reporting elongation of 0.24 mm in myopic adults progressing by −0.77 D or −3.2 D/mm,4 and another similarly found elongation of 0.27 mm in those progressing by −0.76 D or −2.8 D/mm.72 These higher ratios suggest that optical component changes, such as lens thickening, may play a role or the partial compensatory changes in lens power that occur in younger progressing myopes are no longer accessible.
Myopia Progression and Axial Elongation After Refractive Surgery
One further group that should be considered is young adults who have undergone kerato-refractive surgery for myopia, where post-surgical myopia progression is common. For example, in 58 eyes of 34 patients aged 20 to 54 years who underwent photorefractive keratectomy (PRK),84 the mean refractive error was +0.06 ± 0.59 D, −0.27 ± 0.55 D, and −0.58 ± 0.72 D at 1, 2, and 12 years postoperatively, respectively. Likewise, a retrospective study of 42 eyes of 29 patients (aged 21 to 60 years) who underwent PRK and were followed for more than 10 years found mean change of −0.51 ± 1.78 D.85 Longer term follow-up of 160 eyes of 160 patients for 19 to 30 years found a substantial myopic shift from +0.02 ± 0.58 at 6 months to −1.00 ± 1.62 D at 16 years.86
Without axial length measurements it is challenging to determine whether the above refractive changes represent myopic progression or post-surgical regression due to corneal changes. A retrospective study followed 140 patients for more than 5 years postoperatively.87 Patients were in their 20s or 30s when they underwent laser-assisted in situ keratomileusis (LASIK) or epithelial LASIK (epi-LASIK; n = 108 and 32, respectively). Among the LASIK patients, the mean 4-year change in refractive error was +0.05 ± 0.26 D and +0.05 ± 0.33 D in patients in their 20s and 30s, respectively. The corresponding changes in axial length were +0.06 ± 0.13 mm and +0.03 ± 0.13 mm. In the epi-LASIK group, the mean 4-year change in refractive error was −0.44 ± 0.21 D and −0.26 ± 0.45 D in patients in their 20s and 30s, respectively. The corresponding changes in axial length were +0.12 ± 0.14 mm and +0.09 ± 0.17 mm. This suggests that axial elongation is still ongoing and accounts for most of any observed myopic shift.
Follow-up data were reported on 42 eyes of 42 patients who had undergone PRK 20 years previously.88 Between 1- and 20-years post-surgery there was myopic shift of −0.92 D in the 23 patients younger than 40 years at the time of surgery and −0.08 D in those older than 40 years. Complete axial length data were available in 25 eyes and showed a mean increase of 0.84 mm (range = –0.17 to +1.5 mm) over the 20 years. It is important to note that, pre-operatively, axial length was measured with B-scan ultrasonography, whereas after 20 years, partial coherence interferometry was used. In the absence of any change in other ocular parameters, a 0.84 mm change in axial length results in a myopic shift between −1.6 and −2 D, substantially greater than the mean of −0.54 D in all 42 eyes.
Finally, in a retrospective case series of 1219 LASIK patients aged 21 to 50 years followed for 1 year,89 582 of 2316 eyes (25%) showed a myopic shift of at least −0.50 D. Among these eyes, the mean 1-year axial elongation was 0.3 mm. Those eyes showing myopic shifts tended to be more myopic before LASIK (–7.5 ± 2.3 vs. −3.3 ± 1.7 D) with longer axial lengths (26.6 ± 0.44 vs. 24.38 ± 0.73 mm).
In summary, axial elongation continues in myopic adults who have undergone kerato-refractive surgery, although these patients tend to have higher levels of pre-operative myopia. The extent of these changes may depend on the refractive stability prior to surgery. Stability is commonly defined as less than 0.50 D change over a 1 year or more, a value that some regard as far from stable,90 but can be vague.91
Factors Associated With Adult Myopia Onset and Progression
A 2021 IMI report summarized the risk factors for myopia.92 Whereas studies on adults are included in the comprehensive review, no distinction is made regarding age of onset. The paper observes consistent associations between various measures of education duration and pressure and myopia, while noting that associations between more near work and more myopia are generally weak. The authors also conclude that associations between less time outdoors and myopia are robust. The only other risk factor classified as having strong evidence is parental history of myopia.
Data on the factors associated with adult myopia onset and progression are scarce with most papers limited to reporting their frequency. Nonetheless, several factors have been reported to be associated with adult myopic changes. These factors may be categorized as demographic (age, gender, and race), anatomic (e.g. choroidal thickness), or environmental.
Demographic Factors
Myopia progression rate clearly decreases with age based on comparison of the studies summarized in Tables 3 and 4 and those which report larger age ranges.68,69 In medical students,51 younger age has been associated with a myopia shift. Studies consistently show that myopic shifts in adults are more common in myopes than in other refractive groups.47,51,52 Thus, adult myopia progression of early onset myopia, particularly patients with higher levels, could be considered the greater issue. Adult-onset myopia has been associated with a parental history of myopia and female gender,53 although other studies report faster progression among male than female patients.55 In studies with ethnic diversity, adult-onset myopia is more common in those of East Asian than of European descent.53
Low hyperopia and emmetropia are associated with the risk of myopia onset in children.93 None of the papers in Table 2 present data on adult myopia incidence as a function of baseline hyperopia, although some note that incidence is lower in hyperopes than emmetropes.48,52 O'Neal and Connon stratify their cohort by refractive error at baseline, including ranges of −0.12 to +0.12, +0.25 to +0.37, and +0.50 to +0.87 D.47 The mean annual change in all 3 groups, representing between 164 and 184 eyes, was around −0.07 D/year. The authors do not present data on myopia incidence, but it can be inferred to be higher among those with less hyperopia. An earlier prospective study of 3969 students of the US Naval Academy reported a 4-year incidence of myopia (any negative spherical equivalent by cycloplegic refraction) of 40% among those between 0.00 and +0.50 D at baseline, but only 5% in those with more than +0.50 D of hyperopia.94
Anatomic Factors
Thinner choroids have previously been associated with higher levels of myopia in children95 and young adults96 (see IMI reviews on the choroid97 and ocular tissue changes98). In later life, the choroid typically becomes thinner with age.82 Choroidal thickness was evaluated in a subset of the above Australian birth cohort.99 Myopia progression was associated with choroid thinning, whereas, overall, thickening was observed over an 8-year period. The association of baseline choroidal thickness with both myopic shift and axial elongation achieved borderline significance and was unrelated to refractive error at baseline. Conversely, no relationship was found between baseline choroidal thickness and 2-year myopic changes among 291 Chinese medical students.54
Baseline axial length-corneal radius ratio was no different between emmetropic eyes that developed adult-onset myopia and those that did not in the UK microscopists study.4 The potential role of the crystalline lens has not been studied longitudinally. Its thickness continues to increase throughout adulthood but is offset by flattening and changes to the gradient index.100 A reduction in crystalline lens power could offset any ongoing axial elongation in young adulthood, as it appears to beyond the age of 35 years.101
Environmental Factors
Among adults 18 to 25 years (see Table 3) the annual myopia progression rate is higher among student populations than broader samples,53,65 with estimates from practice-based samples falling in between.68,69
Studies of university populations have explored the relationship between visual activities and myopic changes. The study of Norwegian engineering students61 found a relationship between myopic changes and time spent reading scientific literature, practical near work, and time spent in lectures, but not with computer or television use. Likewise, among Danish medical students51 myopic changes were associated with time spent reading scientific literature. In the study of 800 Chinese male emmetropic teenagers,57 longer reading/writing time, frequent, continuous, and longer duration reading/writing, and shorter reading/writing distance were associated with myopic shifts. Studies on broader populations have found no association between adult myopia onset and educational level.53 Among the 268 myopic US adults aged 25 to 35 years completing a 5-year prospective study, there was no association between progression and near work.72 Among US law students,7 no association was found between progression and hours of near work, sleep, or darkness per day.
As in children,102 outdoor activity appears to be protective against myopia. In the Australia birth cohort study,53 myopia incidence was most strongly associated with less sun exposure, as indicated by smaller conjunctival ultraviolet autofluorescence (CUVAF) areas—an objective method that has been shown to correlate with self-reported time spent outdoors in adults. Conversely, CUVAF areas were not associated with myopia progression. The lack of association between time outdoors and progression is somewhat in contrast to a previous study that found myopic shifts in refraction were inversely related to physical activity, although the study did not assess outdoor time per se.51 In the study of 800 Chinese male emmetropic teenagers,57 outdoor activity greater than 1 hour/day was protective against myopic shifts.
Accommodation and its relationship to myopia has been a topic of interest for decades,34,79,103,104 but a recent IMI report105 summarized key studies concluding that “the role of accommodation and binocular vision in the development and progression of myopia is not fully understood” and that “Researchers have not ruled out the role of the accommodative system in this field, but current methods of intervention based on this theory have not yielded significant results.” Higher accommodative lag has been associated with myopia and its progression,79,103,104 but a 5-year prospective study of 268 adults between 25 and 35 years of age72 found that lower accommodative lag was associated with myopia progression.72
Contact lens material or design may also play a role in adult myopia progression. In the Contact Lens Assessment in Youth study,29 those who wore silicone hydrogel lenses were 47% less likely to have an increase in minus lens power than those wearing hydrogel lenses, a finding consistent with other reports.75,106 The pronounced myopic shifts in a retrospective study of adult contact lens wearers may thus be partly attributable to older, lower oxygen permeable hydrogel materials and thicker designs.62
Summary and Implications for Clinical Trials and Patient Care
Adult myopia onset and progression is common among adults aged 18 to 25 years, particularly among students enrolled in the most intensive study programs (e.g. optometry, medical, and law). The frequency of progression appears similar among Europeans and Asians. Likelihood of progression declines with increasing age.69 Finally, kerato-refractive surgery may not insulate previously myopic adults from axial elongation. Surgeons and candidates for surgery should be made aware that myopia progression remains common in young adults. Surgery in a patient's early 20s, may result in a re-emergence of myopia later in adulthood leading to reduced long-term satisfaction and a reassessment of the cost-effectiveness of procedures. Interestingly, the post-surgical corneal profile resembles that created by overnight orthokeratology, albeit with a larger area of central flattening. This profile seems not to make the eye immune to elongation, although it may have been worse had surgery not been performed.
The worldwide increase in myopia prevalence has been well documented,107,108 but has the prevalence of adult-onset myopia changed? Inspection of the data in Table 1, that span over 35 years, suggests that the proportion of all myopia that is adult onset has not changed over time. Of course, if the proportion has not changed, but the overall prevalence of myopia has increased, then this suggests that the prevalence of adult-onset myopia will have increased. It should be noted, however, that few of the cited studies are from East Asia, where the most dramatic increase in myopia prevalence has been observed.108 If the prevalence of juvenile-onset myopia has increased to 80% or higher in East Asia, then the proportion of adult-onset myopia will have likely decreased. One limitation of the studies in young adults is that nearly all have been conducted in university cohorts, but there does not appear to be a change in the incidence of adult-onset myopia among these students based on the studies summarized in Table 2. Hopefully, ongoing large population-based studies will continue long enough to explore risk factors in young adults.109,110 In the meantime, it is difficult to make definite statements regarding temporal trends for adult-onset myopia due to the diversity of populations studied.
Considering the annual rates of adult myopia progression among students in Table 3, no increase was seen across the span of 35 years. Figure 3 shows the annual progression rate as a function of year of publication, a surrogate measure for approximately when the data were collected. The relationship is not significant (r2 = 0.11, P = 0.22). A recent meta-analysis of annual axial elongation in children found that year of publication was not a significant factor.30 Finally, based on US-based data published in 1983 and 2013, the age of stabilization of juvenile-onset myopia does not appear to have changed.28,31 Thus, in spite of changes in digital handheld technology, myopia correction modalities, and education, there do not appear to have been any changes in age of myopia stabilization, incidence of myopia among university students, or rate of myopia progression in adults.
Figure 3.
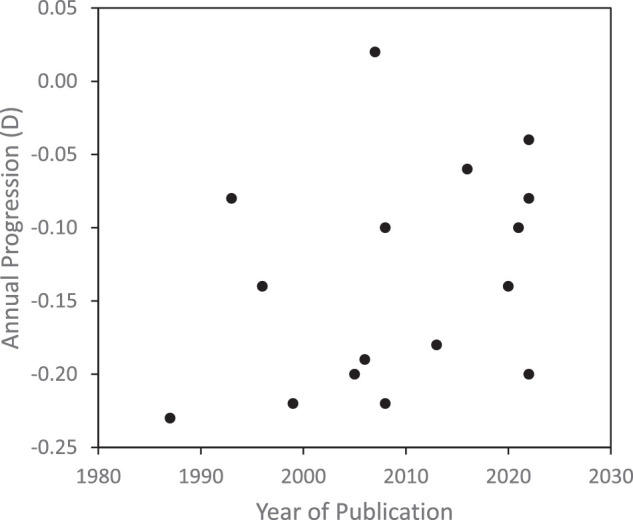
Mean annual myopia progression among adults 18 to 25 years as a function of year of publication. The data are from the 16 studies listed in Table 3.
Although there is compelling evidence for effective reduction of myopia progression in children using a range of modalities,15–17 no studies evaluated newer myopia control treatments in adults, such as dual-focus or multifocal contact lenses or spectacle lenses with mid-peripheral lenslets. Given that juvenile, adolescent, and adult progression are all related to axial elongation, it is reasonable to assume that established modalities would be effective in adults, but it is difficult to predict their efficacy.111 Evaluating myopia control in an adult population presents some challenges. First, progression is slower and thus treatment benefit more difficult to quantify (see Tables 3, 4). Second, it is uncertain when myopia will stabilize, so there may be an illusion of successful control when the myopia stabilized naturally, so a concurrent age-matched control group would appear mandatory. Third, recruitment and retention of working-age adults into longitudinal studies may be challenging.
Adult myopia progression is more common in young adults attending university,32 so recruiting at-risk subjects from academic programs would be an efficient approach. Even in these settings, progression rates are lower in myopic adults than in children with mean annual changes of less than −0.25 D. Thus, a minimum 2-year study duration would be required to demonstrate a clinically meaningful treatment effect of 0.25 D. Axial length using optical biometry can provide a more sensitive outcome measure than refractive error,111,112 given that smaller amounts of progression can be detected with confidence and it can be measured validly without cycloplegia.111 Short-term choroidal changes could also be used to evaluate potential treatments in this age group.113 It could be considered unnecessary and burdensome to establish that an individual's myopia is progressing. This is unlikely to predict their subsequent progression and merely adds to the study's duration and cost.111 For contact lens interventions, safety is an important consideration. The rate of contact lens-related adverse events has been reported to be higher in a young adult population than in children.114 Unplanned overnight wear may also occur more frequently in university students.115
Studies of working adults may be the most difficult in terms of recruitment and retention. These adults may be starting their first full-time jobs, enrolling in graduate degree programs, or starting families. This age is also the time adults may move within their country or abroad for work. Furthermore, these young adults may not regard myopia as a sight-threatening condition, limiting motivation to enroll in a study.
In the absence of an evidence base, clinicians could still consider myopic adults at risk for progression or with demonstrated progression as candidates for myopia control. Later onset of myopia is associated with less risk of higher myopia.23,24,116 Thus, myopic adults of recent onset are at lower absolute risk of myopia-related ocular disease and visual impairment, although preserving a functional level of uncorrected vision is a worthy goal.117–119 Likewise, adults with low myopia may not be as motivated to wear their refractive correction on a full-time basis, limiting the efficacy of myopia control.120,121 In contrast, adults with higher myopia are at greater absolute risk of myopia-related ocular disease and visual impairment are thus considered candidates.117–119 The benefit to cost ratio will thus be greatest in these patients.119,122 The interaction between axial length and refractive error in determining the risk of visual impairment is worthy of further study, although the former appears more important. Factors may emerge that further identify those who would benefit most from myopia control. For example, reduced choroidal thickness is associated with progression of myopic maculopathy. The mean annual progression may appear modest in myopic adults, particularly in those not continuing their education or in specific professions, the cumulative toll of adult progression should not be ignored, and ongoing evaluation is warranted. A mean annual progression of 0.05 D/year between the age of 20 and 40 years will add a diopter to an individual's myopia and further increase their risk of eye disease and visual impairment later in life.
So, what are the considerations in selecting a myopia control option in a young adult? First, evidence of axial elongation may be a useful way of identifying adult myopic patients who would benefit from the intervention, particularly those with higher myopia who have an elevated risk of myopia-related eye disease and visual impairment.117–119 This would also be important to exclude other, rarer causes of myopic shifts in adults, such as corneal ectasia and lenticular changes. A range of modalities have demonstrated efficacy in children,15–17 but no data are available on their effect on adult myopia progression. Given that the patient needs to wear a vision correction anyway, prescribing one that incorporates technology for myopia control should be considered. The potential effect of both optical and pharmaceutical interventions on vision is important as the young adult may be more visually discerning than a child. Overnight orthokeratology has little effect on high contrast visual acuity, but with larger pupils, low contrast visual acuity is reduced123 and associated with increased symptoms of glare.124 Likewise, myopia control soft contact lenses and multifocal designs have greater impact on low contrast than high contrast visual acuity125,126 and may affect ratings of visual quality.127 Thus, whereas acceptance of these lenses in children is high,128 caution should be exercised in extrapolating this to young adults. Likewise, whereas tolerance of novel spectacle lens designs for myopia control is high in children13,121 and vision relatively unaffected through the peripheral portion containing lenslets,129 young adults may or may not be as tolerant. Low concentration atropine is well-tolerated in children14 and young adults,130 but efficacy will be dependent on the concentration, so practitioners will need to balance this with its effect on vision and accommodation. Furthermore, given that no immediate benefit will be apparent and, unlike spectacles and contact lenses, the drops are not needed for clear vision, compliance may be a challenge. Finally, adult patients should be counselled about environmental factors, particularly the potential benefits of outdoor activity.51,53,57
Acknowledgments
The authors thank Arthur Bradley, Noel Brennan, Serge Resnikoff, Nina Tahhan, and IMI harmonizer Ian Flitcroft for their comments on previous versions of this white paper.
Supported by the International Myopia Institute. The publication and dissemination costs of the International Myopia Institute reports were supported by donations from the Brien Holden Vision Institute, Carl Zeiss Vision, CooperVision, EssilorLuxottica, Hoya, Thea, Alcon, and Oculus.
Disclosure: M.A. Bullimore, Alcon Research (C), CooperVision (C), EssilorLuxottica (C), Euclid Systems (C), Eyenovia (C), Genentech (C), Johnson & Johnson Surgical (C), Johnson & Johnson Vision (C), Lentechs (C), Novartis (C), Oculus(C), Pentavision (C), Presbia (C), Sydnexis (C), Vyluma (C), Ridgevue Publishing (O), Ridgevue Vision (O); S.S.-Y. Lee, None; K.L. Schmid, Carl Zeiss Vision Australia (F); Aspen Australia (C); J.J. Rozema, None; N. Leveziel, None; E.A.H. Mallen, EssilorLuxottica (C); N. Jacobsen, None; R. Iribarren, None; P.K. Verkicharla, None; J.R. Polling, Hoya (C), Essilor (C), Vyluma (C), CooperVision (C); P. Chamberlain, CooperVision (E)
References
- 1. Goldschmidt E. On the etiology of myopia. An epidemiological study. Acta Ophthalmol (Copenh). 1968;Suppl 98: 1+. [PubMed] [Google Scholar]
- 2. Grosvenor T. A review and a suggested classification system for myopia on the basis of age-related prevalence and age of onset. Am J Optom Physiol Opt. 1987; 64: 545–554. [DOI] [PubMed] [Google Scholar]
- 3. Flitcroft DI, He M, Jonas JB, et al.. IMI—Defining and classifying myopia: A proposed set of standards for clinical and epidemiologic studies. Invest Ophthalmol Vis Sci. 2019; 60: M20–M30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McBrien NA, Adams DW.. A longitudinal investigation of adult-onset and adult-progression of myopia in an occupational group. Refractive and biometric findings. Invest Ophthalmol Vis Sci. 1997; 38: 321–333. [PubMed] [Google Scholar]
- 5. Midelfart A, Aamo B, Sjohaug KA, Dysthe BE.. Myopia among medical students in Norway. Acta Ophthalmol (Copenh). 1992; 70: 317–322. [DOI] [PubMed] [Google Scholar]
- 6. Shulkin DJ, Bari MM.. Deteriorating vision: An occupational risk for the medical student. Arch Ophthalmol. 1986; 104: 1274. [DOI] [PubMed] [Google Scholar]
- 7. Loman J, Quinn GE, Kamoun L, et al.. Darkness and near work: Myopia and its progression in third-year law students. Ophthalmology. 2002; 109: 1032–1038. [DOI] [PubMed] [Google Scholar]
- 8. Onal S, Toker E, Akingol Z, et al.. Refractive errors of medical students in Turkey: One year follow-up of refraction and biometry. Optom Vis Sci. 2007; 84: 175–180. [DOI] [PubMed] [Google Scholar]
- 9. Dirani M, Shekar SN, Baird PN.. Adult-onset myopia: The Genes in Myopia (GEM) twin study. Invest Ophthalmol Vis Sci. 2008; 49: 3324–3327. [DOI] [PubMed] [Google Scholar]
- 10. Bomotti S, Lau B, Klein BEK, et al.. Refraction and change in refraction over a 20-year period in the beaver dam eye study. Invest Ophthalmol Vis Sci. 2018; 59: 4518–4524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chamberlain P, Peixoto-de-Matos SC, Logan NS, Ngo C, Jones D, Young G.. A 3-year randomized clinical trial of misight lenses for myopia control. Optom Vis Sci. 2019; 96: 556–567. [DOI] [PubMed] [Google Scholar]
- 12. Cho P, Cheung SW.. Retardation of myopia in Orthokeratology (ROMIO) study: A 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012; 53: 7077–7085. [DOI] [PubMed] [Google Scholar]
- 13. Lam CSY, Tang WC, Tse DY, et al.. Defocus incorporated multiple segments (DIMS) spectacle lenses slow myopia progression: A 2-year randomised clinical trial. Br J Ophthalmol. 2020; 104: 363–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yam JC, Jiang Y, Tang SM, et al.. Low-concentration atropine for myopia progression (LAMP) study: A randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology. 2019; 126: 113–124. [DOI] [PubMed] [Google Scholar]
- 15. Bullimore MA, Richdale K.. Myopia Control 2020: Where are we and where are we heading? Ophthalmic Physiol Opt. 2020; 40: 254–270. [DOI] [PubMed] [Google Scholar]
- 16. Walline JJ, Lindsley KB, Vedula SS, et al.. Interventions to slow progression of myopia in children. The Cochrane Database of Systematic Reviews. 2020; 1: CD004916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wildsoet CF, Chia A, Cho P, et al.. IMI—Interventions myopia institute: Interventions for controlling myopia onset and progression report. Invest Ophthalmol Vis Sci. 2019; 60: M106–M131. [DOI] [PubMed] [Google Scholar]
- 18. Saw SM, Tong L, Chua WH, et al.. Incidence and progression of myopia in Singaporean school children. Invest Ophthalmol Vis Sci. 2005; 46: 51–57. [DOI] [PubMed] [Google Scholar]
- 19. Kleinstein RN, Sinnott LT, Jones-Jordan LA, et al.. New cases of myopia in children. Arch Ophthalmol. 2012; 130: 1274–1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Li SM, Wei S, Atchison DA, et al.. Annual incidences and progressions of myopia and high myopia in Chinese schoolchildren based on a 5-year cohort study. Invest Ophthalmol Vis Sci. 2022; 63: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zadnik K, Mutti DO, Mitchell GL, Jones LA, Burr D, Moeschberger ML.. Normal eye growth in emmetropic schoolchildren. Optom Vis Sci. 2004; 81: 819–828. [DOI] [PubMed] [Google Scholar]
- 22. Fledelius HC, Christensen AS, Fledelius C.. Juvenile eye growth, when completed? An evaluation based on IOL-Master axial length data, cross-sectional and longitudinal. Acta Ophthalmol. 2014; 92: 259–264. [DOI] [PubMed] [Google Scholar]
- 23. Chua SY, Sabanayagam C, Cheung YB, et al.. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol Opt. 2016; 36: 388–394. [DOI] [PubMed] [Google Scholar]
- 24. Hu Y, Ding X, Guo X, Chen Y, Zhang J, He M.. Association of age at myopia onset with risk of high myopia in adulthood in a 12-year follow-up of a Chinese cohort. JAMA Ophthalmol. 2020; 138: 1129–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jones-Jordan LA, Sinnott LT, Chu RH, et al.. Myopia progression as a function of sex, age, and ethnicity. Invest Ophthalmol Vis Sci. 2021; 62: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ong E, Grice K, Held R, Thorn F, Gwiazda J.. Effects of spectacle intervention on the progression of myopia in children. Optom Vis Sci. 1999; 76: 363–369. [DOI] [PubMed] [Google Scholar]
- 27. Thorn F, Gwiazda J, Held R.. Myopia progression is specified by a double exponential growth function. Optom Vis Sci. 2005; 82: 286–297. [DOI] [PubMed] [Google Scholar]
- 28. Goss DA, Winkler RL.. Progression of myopia in youth: Age of cessation. Am J Optom Physiol Opt. 1983; 60: 651–658. [DOI] [PubMed] [Google Scholar]
- 29. Kinoshita BT, Chalmers RL, Mitchell GL, et al.. Rate of change and predictive factors for increasing minus contact lens powers in young myopes. Clin Exp Optom. 2015; 98: 323–329. [DOI] [PubMed] [Google Scholar]
- 30. Shamp W, Brennan NA, Maynes E, Cheng X, Bullimore MA.. Influence of age and race on axial elongation in myopic children. Invest Ophthalmol Vis Sci. 2022; 63: 257. [DOI] [PubMed] [Google Scholar]
- 31. COMET Group. Myopia stabilization and associated factors among participants in the correction of myopia evaluation trial (COMET). Invest Ophthalmol Vis Sci. 2013; 54: 7871–7884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. National Research Council. Working Group on Myopia Prevalence and Progression. Myopia: Prevalence and Progression. Washington, D.C.: National Academy Press; 1989. Available at: https://www.ncbi.nlm.nih.gov/books/NBK235062/pdf/Bookshelf_NBK235062.pdf. [Google Scholar]
- 33. Bullimore MA, Gilmartin B.. Aspects of tonic accommodation in emmetropia and late-onset myopia. Am J Optom Physiol Opt. 1987; 64: 499–503. [DOI] [PubMed] [Google Scholar]
- 34. McBrien NA, Millodot M.. The relationship between tonic accommodation and refractive error. Invest Ophthalmol Vis Sci. 1987; 28: 997–1004. [PubMed] [Google Scholar]
- 35. Septon RD. Myopia among optometry students. Am J Optom Physiol Opt. 1984; 61: 745–751. [DOI] [PubMed] [Google Scholar]
- 36. Bullimore MA, Conway R, Nakash A.. Myopia in optometry students: Family history, age of onset and personality. Ophthalmic Physiol Opt. 1989; 9: 284–288. [DOI] [PubMed] [Google Scholar]
- 37. Iribarren R, Cerrella MR, Armesto A, Iribarren G, Fornaciari A.. Age of lens use onset in a myopic sample of office-workers. Curr Eye Res. 2004; 28: 175–180. [DOI] [PubMed] [Google Scholar]
- 38. Bullimore MA, Reuter KS, Jones LA, Mitchell GL, Zoz J, Rah MJ.. The study of progression of adult nearsightedness (SPAN): Design and baseline characteristics. Optom Vis Sci. 2006; 83: 594–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Iribarren R, Cortinez MF, Chiappe JP.. Age of first distance prescription and final myopic refractive error. Ophthalmic Epidemiol. 2009; 16: 84–89. [DOI] [PubMed] [Google Scholar]
- 40. Rahi JS, Cumberland PM, Peckham CS.. Myopia over the lifecourse: Prevalence and early life influences in the 1958 British birth cohort. Ophthalmology. 2011; 118: 797–804. [DOI] [PubMed] [Google Scholar]
- 41. Malik MH, Mohydin M, Saeed A, et al.. Prevalence and risk factors of myopia among medical students. Pakistan J Med Health Sci. 2022; 16: 173–175. [Google Scholar]
- 42. Ting PW, Lam CS, Edwards MH, Schmid KL.. Prevalence of myopia in a group of Hong Kong microscopists. Optom Vis Sci. 2004; 81: 88–93. [DOI] [PubMed] [Google Scholar]
- 43. Walline JJ, Zadnik K, Mutti DO.. Validity of surveys reporting myopia, astigmatism, and presbyopia. Optom Vis Sci. 1996; 73: 376–381. [DOI] [PubMed] [Google Scholar]
- 44. Adams DW, McBrien NA.. Prevalence of myopia and myopic progression in a population of clinical microscopists. Optom Vis Sci. 1992; 69: 467–473. [DOI] [PubMed] [Google Scholar]
- 45. Rudnicka AR, Owen CG, Nightingale CM, Cook DG, Whincup PH.. Ethnic differences in the prevalence of myopia and ocular biometry in 10- and 11-year-old children: The child heart and health study in England (CHASE). Invest Ophthalmol Vis Sci. 2010; 51: 6270–6276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Power C, Elliott J.. Cohort profile: 1958 British birth cohort (national child development study). Int J Epidemiol. 2006; 35: 34–41. [DOI] [PubMed] [Google Scholar]
- 47. O'Neal MR, Connon TR.. Refractive error change at the United States Air Force Academy–class of 1985. Am J Optom Physiol Opt. 1987; 64: 344–354. [DOI] [PubMed] [Google Scholar]
- 48. Kinge B, Midelfart A.. Refractive changes among Norwegian university students–a three-year longitudinal study. Acta Ophthalmol Scand. 1999; 77: 302–305. [DOI] [PubMed] [Google Scholar]
- 49. Fesharaki H, Kamali B, Karbasi M, Fasihi M.. Development of myopia in medical school. Asian J Ophthalmol. 2006; 8: 199–202. [Google Scholar]
- 50. Jorge J, Almeida JB, Parafita MA.. Refractive, biometric and topographic changes among Portuguese university science students: A 3-year longitudinal study. Ophthalmic Physiol Opt. 2007; 27: 287–294. [DOI] [PubMed] [Google Scholar]
- 51. Jacobsen N, Jensen H, Goldschmidt E.. Does the level of physical activity in university students influence development and progression of myopia? A 2-year prospective cohort study. Invest Ophthalmol Vis Sci. 2008; 49: 1322–1327. [DOI] [PubMed] [Google Scholar]
- 52. Lv L, Zhang Z.. Pattern of myopia progression in Chinese medical students: A two-year follow-up study. Graefes Arch Clin Exp Ophthalmol. 2013; 251: 163–168. [DOI] [PubMed] [Google Scholar]
- 53. Lee SS, Lingham G, Sanfilippo PG, et al.. Incidence and progression of myopia in early adulthood. JAMA Ophthalmology. 2022; 140: 162–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Duan F, Yuan Z, Deng J, et al.. Incidence of myopic shift and related factors in young Chinese adults [published online ahead of print March 7, 2022]. Clin Exp Optom, 10.1080/08164622.2022.2048172. [DOI] [PubMed] [Google Scholar]
- 55. Lin LL, Shih YF, Lee YC, Hung PT, Hou PK.. Changes in ocular refraction and its components among medical students–a 5-year longitudinal study. Optom Vis Sci. 1996; 73: 495–498. [DOI] [PubMed] [Google Scholar]
- 56. Hoogerheide J, Rempt F, Hoogenboom WP.. Acquired myopia in young pilots. Ophthalmologica. 1971; 163: 209–215. [DOI] [PubMed] [Google Scholar]
- 57. Yao L, Qi LS, Wang XF, et al.. Refractive change and incidence of myopia among a group of highly selected senior high school students in China: A prospective study in an aviation cadet prerecruitment class. Invest Ophthalmol Vis Sci. 2019; 60: 1344–1352. [DOI] [PubMed] [Google Scholar]
- 58. Grosvenor T, Scott R.. Three-year changes in refraction and its components in youth-onset and early adult-onset myopia. Optom Vis Sci. 1993; 70: 677–683. [DOI] [PubMed] [Google Scholar]
- 59. Waring GO 3rd, Lynn MJ, McDonnell PJ.. Results of the prospective evaluation of radial keratotomy (PERK) study 10 years after surgery. Arch Ophthalmol. 1994; 112: 1298–1308. [DOI] [PubMed] [Google Scholar]
- 60. Ellingsen KL, Nizam A, Ellingsen BA, Lynn MJ.. Age-related refractive shifts in simple myopia. J Refract Surg. 1997; 13: 223–228. [DOI] [PubMed] [Google Scholar]
- 61. Kinge B, Midelfart A, Jacobsen G, Rystad J.. The influence of near-work on development of myopia among university students. A three-year longitudinal study among engineering students in Norway. Acta Ophthalmol Scand. 2000; 78: 26–29. [DOI] [PubMed] [Google Scholar]
- 62. Bullimore MA, Jones LA, Moeschberger ML, Zadnik K, Payor RE.. A retrospective study of myopia progression in adult contact lens wearers. Invest Ophthalmol Vis Sci. 2002; 43: 2110–2113. [PubMed] [Google Scholar]
- 63. Kinge B, Midelfart A, Jacobsen G, Rystad J.. Biometric changes in the eyes of Norwegian university students–a three-year longitudinal study. Acta Ophthalmol Scand. 1999; 77: 648–652. [DOI] [PubMed] [Google Scholar]
- 64. Jiang BC, Schatz S, Seger K.. Myopic progression and dark focus variation in optometric students during the first academic year. Clin Exp Optom. 2005; 88: 153–159. [DOI] [PubMed] [Google Scholar]
- 65. Parssinen O, Kauppinen M, Viljanen A.. The progression of myopia from its onset at age 8-12 to adulthood and the influence of heredity and external factors on myopic progression. A 23-year follow-up study. Acta Ophthalmol. 2014; 92: 730–739. [DOI] [PubMed] [Google Scholar]
- 66. Parssinen O, Kauppinen M.. What is the influence of parents' myopia on their children's myopic progression? A 22-year follow-up study. Acta Ophthalmol. 2016; 94: 579–585. [DOI] [PubMed] [Google Scholar]
- 67. Price H, Allen PM, Radhakrishnan H, et al.. The cambridge anti-myopia study: Variables associated with myopia progression. Optom Vis Sci. 2013; 90: 1274–1283. [DOI] [PubMed] [Google Scholar]
- 68. Polling JR, Klaver C, Tideman JW.. Myopia progression from wearing first glasses to adult age: The DREAM study. Br J Ophthalmol. 2022; 106: 820–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Ducloux A, Marillet S, Ingrand P, Bullimore MA, Bourne RRA, Leveziel N.. Progression of myopia in teenagers and adults: A nationwide longitudinal study of a prevalent cohort [published online ahead of print December 22, 2021]. Br J Ophthalmol, 10.1136/bjophthlmol-2021-319568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Verkicharla PK, Kammari P, Das AV.. Myopia progression varies with age and severity of myopia. PLoS One. 2020; 15: e0241759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Zadnik K, Mutti DO.. Refractive error changes in law students. Am J Optom Physiol Opt. 1987; 64: 558–561. [DOI] [PubMed] [Google Scholar]
- 72. Bullimore MA, Mitchell GL, Jones LA, Reuter KS.. Progression of myopia in an adult population. Invest Ophthalmol Vis Sci. 2008; 49: 2606.18515589 [Google Scholar]
- 73. Fernandez-Montero A, Olmo-Jimenez JM, Olmo N, et al.. The impact of computer use in myopia progression: A cohort study in Spain. Prev Med. 2015; 71: 67–71. [DOI] [PubMed] [Google Scholar]
- 74. Li SM, Lin C, Wan Y, et al.. Five-year refractive changes in a rural Chinese adult population and its related factors: The handan eye study. Clin Exp Ophthalmol. 2018; 46: 873–881. [DOI] [PubMed] [Google Scholar]
- 75. Blacker A, Mitchell GL, Bullimore MA, et al.. Myopia progression during three years of soft contact lens wear. Optom Vis Sci. 2009; 86: 1150–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Liang YB, Wong TY, Sun LP, et al.. Refractive errors in a rural Chinese adult population the Handan eye study. Ophthalmology. 2009; 116: 2119–2127. [DOI] [PubMed] [Google Scholar]
- 77. McBrien NA, Millodot M.. A biometric investigation of late onset myopic eyes. Acta Ophthalmol (Copenh). 1987; 65: 461–468. [DOI] [PubMed] [Google Scholar]
- 78. Adams AJ. Axial length elongation, not corneal curvature, as a basis of adult onset myopia. Am J Optom Physiol Opt. 1987; 64: 150–152. [DOI] [PubMed] [Google Scholar]
- 79. Bullimore MA, Gilmartin B, Royston JM.. Steady-state accommodation and ocular biometry in late-onset myopia. Doc Ophthalmol. 1992; 80: 143–155. [DOI] [PubMed] [Google Scholar]
- 80. Fledelius HC. Adult onset myopia–oculometric features. Acta Ophthalmol Scand. 1995; 73: 397–401. [DOI] [PubMed] [Google Scholar]
- 81. Grosvenor T, Scott R.. Comparison of refractive components in youth-onset and early adult-onset myopia. Optom Vis Sci. 1991; 68: 204–209. [DOI] [PubMed] [Google Scholar]
- 82. Rozema JJ, Ni Dhubhghaill S. Age-related axial length changes in adults: A review. Ophthalmic Physiol Opt. 2020; 40: 710–717. [DOI] [PubMed] [Google Scholar]
- 83. Hyman L, Gwiazda J, Hussein M, et al.. Relationship of age, sex, and ethnicity with myopia progression and axial elongation in the correction of myopia evaluation trial. Arch Ophthalmol. 2005; 123: 977–987. [DOI] [PubMed] [Google Scholar]
- 84. O'Connor J, O'Keeffe M, Condon PI. Twelve-year follow-up of photorefractive keratectomy for low to moderate myopia. J Refract Surg. 2006; 22: 871–877. [DOI] [PubMed] [Google Scholar]
- 85. Koshimizu J, Dhanuka R, Yamaguchi T.. Ten-year follow-up of photorefractive keratectomy for myopia. Graefes Arch Clin Exp Ophthalmol. 2010; 248: 1817–1825. [DOI] [PubMed] [Google Scholar]
- 86. Vestergaard AH, Hjortdal JO, Ivarsen A, Work K, Grauslund J, Sjolie AK.. Long-term outcomes of photorefractive keratectomy for low to high myopia: 13 to 19 years of follow-up. J Refract Surg. 2013; 29: 312–319. [DOI] [PubMed] [Google Scholar]
- 87. Sasaki M, Hieda O, Wakimasu K, Yamamura K, Kinoshita S, Sotozono C.. Myopia progression over a 4-year period after laser-assisted refractive surgery in patients in their 20s and 30s. Jpn J Ophthalmol. 2020; 64: 450–454. [DOI] [PubMed] [Google Scholar]
- 88. O'Brart DP, Shalchi Z, McDonald RJ, Patel P, Archer TJ, Marshall J.. Twenty-year follow-up of a randomized prospective clinical trial of excimer laser photorefractive keratectomy. Am J Ophthalmol. 2014; 158: 651–663.e1. [DOI] [PubMed] [Google Scholar]
- 89. Gab-Alla AA. Is the axial length a risk factor for post-LASIK myopic regression? Graefes Arch Clin Exp Ophthalmol. 2021; 259: 777–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Sugar A, Rapuano CJ, Culbertson WW, et al.. Laser in situ keratomileusis for myopia and astigmatism: Safety and efficacy: A report by the American academy of ophthalmology. Ophthalmology. 2002; 109: 175–187. [DOI] [PubMed] [Google Scholar]
- 91. Jacobs DS, Lee JK, Shen TT, et al.. Refractive surgery preferred practice pattern. Ophthalmology. 2022; 130(3): P61–P135. [DOI] [PubMed] [Google Scholar]
- 92. Morgan IG, Wu PC, Ostrin LA, et al.. IMI risk factors for myopia. Invest Ophthalmol Vis Sci. 2021; 62: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Zadnik K, Sinnott LT, Cotter SA, et al.. Prediction of juvenile-onset myopia. JAMA Ophthalmol. 2015; 133: 683–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Hynes EA. Refractive changes in normal young men. AMA Arch Ophthalmol. 1956; 56: 761–767. [DOI] [PubMed] [Google Scholar]
- 95. Read SA, Collins MJ, Vincent SJ, Alonso-Caneiro D. Choroidal thickness in myopic and nonmyopic children assessed with enhanced depth imaging optical coherence tomography. Invest Ophthalmol Vis Sci. 2013; 54: 7578–7586. [DOI] [PubMed] [Google Scholar]
- 96. Harb E, Hyman L, Gwiazda J, et al.. Choroidal thickness profiles in myopic eyes of young adults in the correction of myopia evaluation trial cohort. Am J Ophthalmol. 2015; 160: 62–71.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Ostrin LA, Harb EN, Nickla DL, et al.. IMI—The dynamic choroid: New insights, challenges and potential significance for human myopia. Invest Ophthalmol Vis Sci. 2023; 64(6): 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Jonas JB, Spaide R, Logan NS, Flitcroft I, Panda-Jonas S. IMI—Non-pathological human ocular tissue changes with myopia. Invest Ophthalmol Vis Sci. 2023; 64(6): 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Lee SS, Alonso-Caneiro D, Lingham G, et al.. Choroidal thickening during young adulthood and baseline choroidal thickness predicts refractive error change. Invest Ophthalmol Vis Sci. 2022; 63: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Garner LF, Ooi CS, Smith G.. Refractive index of the crystalline lens in young and aged eyes. Clin Exp Optom. 1998; 81: 145–150. [DOI] [PubMed] [Google Scholar]
- 101. Han X, Guo X, Lee PY, Morgan IG, He M.. Six-year changes in refraction and related ocular biometric factors in an adult Chinese population. PLoS One. 2017; 12: e0183364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Jones LA, Sinnott LT, Mutti DO, Mitchell GL, Moeschberger ML, Zadnik K.. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci. 2007; 48: 3524–3532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Gwiazda J, Thorn F, Bauer J, Held R.. Myopic children show insufficient accommodative response to blur. Invest Ophthalmol Vis Sci. 1993; 34: 690–694. [PubMed] [Google Scholar]
- 104. Abbott ML, Schmid KL, Strang NC.. Differences in the accommodation stimulus response curves of adult myopes and emmetropes. Ophthalmic Physiol Opt. 1998; 18: 13–20. [PubMed] [Google Scholar]
- 105. Logan NS, Radhakrishnan H, Cruickshank FE, et al.. IMI accommodation and binocular vision in myopia development and progression. Invest Ophthalmol Vis Sci. 2021; 62: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Jalbert I, Stretton S, Naduvilath T, Holden B, Keay L, Sweeney D.. Changes in myopia with low-Dk hydrogel and high-Dk silicone hydrogel extended wear. Optom Vis Sci. 2004; 81: 591–596. [DOI] [PubMed] [Google Scholar]
- 107. Holden BA, Fricke TR, Wilson DA, et al.. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016; 123: 1036–1042. [DOI] [PubMed] [Google Scholar]
- 108. Morgan IG, French AN, Ashby RS, et al.. The epidemics of myopia: Aetiology and prevention. Prog Retin Eye Res. 2018; 62: 134–149. [DOI] [PubMed] [Google Scholar]
- 109. Tideman JWL, Polling JR, Vingerling JR, et al.. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. 2018; 96: 301–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Tideman JWL, Polling JR, Jaddoe VWV, Vingerling JR, Klaver CCW.. Environmental risk factors can reduce axial length elongation and myopia incidence in 6- to 9-year-old children. Ophthalmology. 2019; 126: 127–136. [DOI] [PubMed] [Google Scholar]
- 111. Brennan NA, Toubouti YM, Cheng X, Bullimore MA.. Efficacy in myopia control. Prog Retin Eye Res. 2021; 83: 100923. [DOI] [PubMed] [Google Scholar]
- 112. Bullimore MA, Slade S, Yoo P, Otani T.. An evaluation of the IOLMaster 700. Eye Contact Lens. 2019; 45: 117–123. [DOI] [PubMed] [Google Scholar]
- 113. Read SA, Fuss JA, Vincent SJ, Collins MJ, Alonso-Caneiro D. Choroidal changes in human myopia: Insights from optical coherence tomography imaging. Clin Exp Optom. 2019; 102: 270–285. [DOI] [PubMed] [Google Scholar]
- 114. Chalmers RL, Wagner H, Mitchell GL, et al.. Age and other risk factors for corneal infiltrative and inflammatory events in young soft contact lens wearers from the Contact Lens Assessment in Youth (CLAY) study. Invest Ophthalmol Vis Sci. 2011; 52: 6690–6696. [DOI] [PubMed] [Google Scholar]
- 115. Wagner H, Richdale K, Mitchell GL, et al.. Age, behavior, environment, and health factors in the soft contact lens risk survey. Optom Vis Sci. 2014; 91: 252–261. [DOI] [PubMed] [Google Scholar]
- 116. Bullimore MA, Brennan NA.. Myopia: An ounce of prevention is worth a pound of cure. Ophthalmic Physiol Opt. 2023; 43: 116–121. [DOI] [PubMed] [Google Scholar]
- 117. Bullimore MA, Brennan NA.. Myopia control: Why each diopter matters. Optom Vis Sci. 2019; 96: 463–465. [DOI] [PubMed] [Google Scholar]
- 118. Tideman JW, Snabel MC, Tedja MS, et al.. Association of axial length with risk of uncorrectable visual impairment for Europeans with myopia. JAMA Ophthalmol. 2016; 134: 1355–1363. [DOI] [PubMed] [Google Scholar]
- 119. Bullimore MA, Ritchey ER, Shah S, Leveziel N, Bourne RRA, Flitcroft DI.. The risks and benefits of myopia control. Ophthalmology. 2021; 128: 1561–1579. [DOI] [PubMed] [Google Scholar]
- 120. Lam CS, Tang WC, Tse DY, Tang YY, To CH.. Defocus incorporated soft contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: A 2-year randomised clinical trial. Br J Ophthalmol. 2014; 98: 40–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Bao J, Huang Y, Li X, et al.. Spectacle lenses with aspherical lenslets for myopia control vs single-vision spectacle lenses: A randomized clinical trial. JAMA Ophthalmol. 2022; 140: 472–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Fricke TR, Sankaridurg P, Naduvilath T, et al.. Establishing a method to estimate the effect of antimyopia management options on lifetime cost of myopia [published online ahead of print March 9, 2022]. Br J Ophthalmol, 10.1136/bjophthalmol-2021-320318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Berntsen DA, Barr JT, Mitchell GL.. The effect of overnight contact lens corneal reshaping on higher-order aberrations and best-corrected visual acuity. Optom Vis Sci. 2005; 82: 490–497. [DOI] [PubMed] [Google Scholar]
- 124. Berntsen DA, Mitchell GL, Barr JT.. The effect of overnight contact lens corneal reshaping on refractive error-specific quality of life. Optom Vis Sci. 2006; 83: 354–359. [DOI] [PubMed] [Google Scholar]
- 125. Kollbaum PS, Jansen ME, Tan J, Meyer DM, Rickert ME.. Vision performance with a contact lens designed to slow myopia progression. Optom Vis Sci. 2013; 90: 205–214. [DOI] [PubMed] [Google Scholar]
- 126. Sha J, Tilia D, Diec J, et al.. Visual performance of myopia control soft contact lenses in non-presbyopic myopes. Clin Optom (Auckl). 2018; 10: 75–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Schmid KL, Gifford KL, Atchison DA.. The effect of concentric and aspheric multifocal soft contact lenses on binocular vision in young adult myopes. Cont Lens Anterior Eye. 2023; 46: 101588. [DOI] [PubMed] [Google Scholar]
- 128. Chamberlain P, Bradley A, Arumugam B, et al.. Long-term effect of dual-focus contact lenses on myopia progression in children: a 6-year multicenter clinical trial. Optom Vis Sci. 2022; 99: 204–212. [DOI] [PubMed] [Google Scholar]
- 129. Gao Y, Lim EW, Yang A, Drobe B, Bullimore MA.. The impact of spectacle lenses for myopia control on visual functions. Ophthalmic Physiol Opt. 2021; 41: 1320–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Loughman J, Flitcroft DI.. The acceptability and visual impact of 0.01% atropine in a Caucasian population. Br J Ophthalmol. 2016; 100: 1525–1529. [DOI] [PubMed] [Google Scholar]


