Abstract
Purpose
To report the incidence and clinical characteristics of pediatric ocular and adnexal injuries diagnosed over a 10-year period in Olmsted County, Minnesota.
Methods
This multicenter retrospective, population-based cohort study included all patients <19 years of age in Olmsted County diagnosed with ocular or adnexal injuries from January 1, 2000, through December 31, 2009.
Results
A total of 740 ocular or adnexal injuries occurred during the study period, yielding an incidence of 203 (95% CI, 189–218) per 100,000 children. Median age at diagnosis was 10.0 years, and 462 (62.4%) were males. Injuries presented to the emergency department or urgent care setting most frequently (69.6%) and often occurred while outdoors (31.6%) during summer months (29.7%). Common injury mechanisms included blunt force (21.5%), foreign bodies (13.8%), and sports activities (13.0%). Isolated anterior segment injuries occurred in 63.5% of injuries. Ninety-nine patients (13.8%) had visual acuity of 20/40 or worse at initial examination, and 55 patients (7.7%) had visual acuity of 20/40 or worse at final examination. Twenty-nine injuries (3.9%) required surgical intervention. Significant risk factors for reduced visual acuity and/or the development of long-term complications include male sex, age ≥12 years, outdoor injuries, sport and firearm/projectile injury mechanism, and hyphema or posterior segment injury (P < 0.05).
Conclusions
Most pediatric eye injuries are minor anterior segment injuries with infrequent long-lasting effects on visual development.
Trauma to the eye or ocular adnexa is a significant but often preventable cause of visual morbidity in children.1 Although pediatric ocular injuries and the resulting need for hospitalization have decreased over time,2–4 they continue to account for almost $200 million USD per year in US healthcare spending5 and thousands of activity-restricted days.6 Most prior reports of injuries to the pediatric eye included single institution, tertiary center cohorts, often with conflicting risk factors and results. Even population-based studies have been limited by occurring solely among inpatient cohorts,7–9 within a specific subspecialty,9 or surveying only a short time interval.7–9 The purpose of the current study was to report the incidence and clinical characteristics of pediatric ocular injuries diagnosed by any provider among residents of Olmsted County, Minnesota, over a 10-year period.
Methods
The medical records of all patients <19 years of age diagnosed with any form of ocular or adnexal injury while residing in Olmsted County, Minnesota, from January 1, 2000, through December 31, 2009, were retrospectively reviewed. Potential cases were identified by searching the Rochester Epidemiology Project (REP) database using ICD-9 codes that were related to ocular or adnexal injury (eSupplement 1, available at jaapos.org). The REP database is a medical record linkage system designed to capture data on any patient-physician encounter in Olmsted County.10 The population of this county is relatively isolated from other urban areas, and virtually all medical care is provided to its residents by Mayo Clinic, Olmsted Medical Center, and their affiliated hospitals. Patients were included if they had a history of injury to the globe, orbit, or adnexa with clinically significant ocular findings or if they received a diagnosis consistent with injury to the eye. Patients were excluded if the injuries occurred outside the time period of the study, if they lived outside Olmsted County at the time of diagnosis, or if they refused authorization for research. The entire medical record of each case was individually reviewed by the authors for demographic, clinical, and outcomes data, including initial and final visual acuity and contextual details of eye injury. This study was approved by the Institutional Review Boards of Mayo Clinic and Olmsted Medical Center and conformed to the requirements of the US Health Insurance Portability and Accountability Act of 1996.
Yearly incidence for age and sex groups were determined by dividing the cases of pediatric ocular and adnexal injuries within that group by estimated total Olmsted County population of the group for the given year using REP census data. Overall incidence rates were calculated adjusting to the age and sex distribution of the United States White population to make the results more generalizable. The 95% confidence intervals for overall incidence rates were calculated assuming Poisson error distribution. The trend of incidence rates over time period was tested using Poisson regression models given the predictors of age, sex, and time.
Continuous variables were summarized with the sample mean, median, and range. Categorical variables were summarized with number and percentage of injuries. One-way χ2 test was used to test whether the number of injuries in each season differed significantly from theoretical expectations. Statistical analysis was performed using R statistical software (version 4.0.3; R Foundation for Statistical Computing, Vienna, Austria).
Results
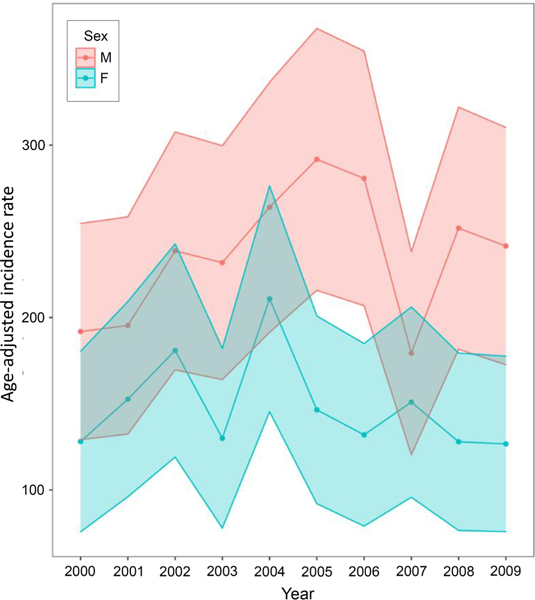
A total of 740 ocular or adnexal injuries occurred among 718 patients during the 10-year study period, yielding an annual age- and sex-adjusted incidence of 203 (95% CI, 189–218) per 100,000 patients <19 years of age. The historical and clinical characteristics of the 740 injuries are shown in Table 1. The mean age (with standard deviation) at diagnosis was 8.6 ± 5.6 years for females and 9.6 ± 5.6 years for males; 462 of the injuries (62.4%) were among males. Injuries were more common among those ≥12 years of age. The most common prior ocular history included previous injury (3.5%) and strabismus (2.3). At the time of injury, 121 patients (16.4%) had mental health comorbidities, including 79 (10.7%) with attention-deficit/hyperactivity disorder. The median number of injuries per year was 73 (range, 59–91) without a significant trend over time (P = 0.743). See Figure 1. However, injuries had significant seasonal variability (P < 0.001), with most injuries occurring during the summer months (29.7%) and fewest during winter months (17.6%).
Table 1.
Historical and clinical characteristics of 740 ocular or adnexal injuries among 718 patients <19 years old in Olmsted County, MN from 2000–2009
| Characteristics | Total | Age range, years | |||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| 0–2 | 3–5 | 6–8 | 9–11 | 12–14 | 15–18 | ||
| No. (%) | 740 | 118 (15.9) | 124 (16.8) | 96 (13.0) | 99 (13.4) | 132 (17.8) | 171 (23.1) |
| Incidence rate (per 100,000) | 202.7 | 201.7 | 211.3 | 168.7 | 168.5 | 228.3 | 229.6 |
| Sex, no. (%)a | |||||||
| Female | 277 (37.4) | 49 (41.5) | 54 (43.5) | 40 (41.7) | 36 (36.4) | 45 (34.1) | 53 (31.0) |
| Male | 462 (62.4) | 69 (58.5) | 70 (56.5) | 56 (58.3) | 63 (63.6) | 87 (65.9) | 117 (68.4) |
| Race (%) | |||||||
| White | 545 (73.6) | 80 (67.8) | 85 (68.5) | 69 (71.9) | 77 (77.8) | 107 (81.1) | 127 (74.3) |
| Black | 65 (8.8) | 8 (6.8) | 10 (8.1) | 13 (13.5) | 7 (7.1) | 10 (7.6) | 17 (9.9) |
| Asian | 21 (2.8) | 1 (0.8) | 8 (6.5) | 4 (4.2) | 5 (5.1) | 0 (0.0) | 3 (1.8) |
| American Indian | 2 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (10) | 1 (0.8) | 0 (0.0) |
| Hawaiian/Pacific Island | 2 (0.3) | 0 (0.0) | 1 (0.8) | 1 (1) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Other | 51 (6.9) | 19 (16.1) | 7 (5.6) | 7 (7.3) | 5 (5.1) | 7 (5.3) | 6 (3.5) |
| Unknown/declined | 54 (7.3) | 10 (8.5) | 13 (10.5) | 2(2.1) | 4 (4.0) | 7(5.3) | 18 (10.5) |
| Prior ocular history, no. (%) | |||||||
| Prior trauma | 26 (3.5) | 2 (1.7) | 1 (0.8) | 7 (7.3) | 3 (3.0) | 7 (5.3) | 6 (3.5) |
| Strabismus | 17 (2.3) | 1 (0.8) | 5 (4.0) | 5 (5.2) | 1 (1.0) | 4 (3.0) | 1 (0.6) |
| Adnexal / orbital disorders | 16 (2.2) | 8 (6.8) | 2 (1.6) | 2 (2.1) | 2 (2.0) | 2 (1.5) | 0 (0.0) |
| Amblyopia | 9 (1.2) | 1 (0.8) | 3 (2.4) | 0 (0.0) | 1 (1.0) | 2 (1.5) | 2 (1.2) |
| Retina/vitreous | 6 (0.8) | 2 (1.7) | 0 (0.0) | 1 (1.0) | 0 (0.0) | 1 (0.8) | 2 (1.2) |
| Cornea | 5 (0.7) | 0 (0.0) | 0 (0.0) | 1 (1.0) | 1 (1.0) | 2 (1.5) | 1 (0.6) |
| Uveitis | 2 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (1.2) |
| Lens | 2 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.8) | 1 (0.6) |
| Psychiatric history, no. (%) | |||||||
| ADHD | 79 (10.7) | 0 (0.0) | 3 (2.4) | 13 (13.5) | 14 (14.1) | 22 (16.7) | 27 (15.8) |
| Depression, anxiety, or substance use | 65 (8.8) | 0(0.0) | 0 (0.0) | 2 (2.1) | 11 (11.1) | 18 (13.6) | 34 (19.9) |
ADHD, attention-deficit/hyperactivity disorder.
One patient declined to answer.
FIG 1.
Annual age-adjusted incidence rate by sex of ocular and adnexal injuries in children from 2000–2009 in Olmsted County, MN.
Of the 718 patients who sustained ocular or adnexal injuries, 22 (3.1%) suffered more than one injury, and 74 injuries (10.0%) were bilateral, most commonly due to chemical injuries (n = 35 [4.7%]) and welding or pyrotechnics (n = 23 [3.1%]). Of the 740 injuries, 470 (63.5%) were limited to the anterior segment, 142 (19.2%) were limited to the orbit and adnexa, 80 (10.8%) sustained injuries impacting multiple segments, and 12 (1.6%) were limited to the posterior segment. The most common injuries included subconjunctival hemorrhages, corneal abrasions, and eyelid or adnexal edema and contusions (Table 2). Most injuries occurred as the result of accidents (655 injuries, 88.5%), whereas the remaining 85 (11.5%) resulted from assault or suspected nonaccidental trauma (Table 3). The most common location for injuries was outdoors (31.6%), followed by home (20.5%) and school (9.5%). Injuries were more likely to occur via blunt force trauma (21.5%), foreign bodies (13.8%), and sports (13.0%). Patients typically presented to the emergency department or urgent care location for initial care (69.6%) and were least likely to first present to an optometrist (2.7%). Among injuries where visual acuity was recorded, 99 (13.4%) had a visual acuity of 20/40 or worse in the injured eye at initial presentation.
Table 2.
Ten most prevalent diagnoses among 740 ocular or adnexal injuries diagnosed in Olmsted County, MN, 2000–2009
| Diagnosis | No. (%)a | Incidence rate (per 100,000) |
|---|---|---|
| Subconjunctival hemorrhage | 202 (27.3) | 53.5 |
| Corneal abrasion | 195 (26.4) | 51.8 |
| Eyelid contusion or edema | 167 (22.6) | 41.9 |
| Hyphema | 70 (9.5) | 19.4 |
| Conjunctival abrasion | 52 (7.0) | 13.9 |
| Conjunctival foreign body | 45 (6.1) | 12.2 |
| Traumatic iritis | 36 (4.9) | 9.92 |
| Corneal chemical injury | 36 (4.9) | 9.56 |
| Commotio retinae | 30 (4.1) | 8.22 |
| Eyelid laceration | 29 (3.9) | 7.59 |
Total percent of injuries leading to this diagnosis.
Table 3.
Environmental factors for 740 injuries among 718 patients diagnosed with ocular or adnexal injuries in Olmsted County, MN, 2000–2009
| Environmental factors | No. (%) |
|---|---|
| Time of year | |
| Summer | 220 (29.7) |
| Spring | 197 (26.6) |
| Fall | 193 (26.1) |
| Winter | 130 (17.6) |
| Location of injury | |
| Outside / street play | 234 (31.6) |
| Home | 152 (20.5) |
| School | 70 (9.5) |
| Indoor sports facility | 19 (2.6) |
| Vehicle | 19 (2.6) |
| Work | 10 (14) |
| Friend/peer’s house | 9 (12) |
| Unknown | 215 (29.1) |
| Other | 12 (16) |
| Intent | |
| Accident | 655 (88.5) |
| Assault | 34 (4.6) |
| Self-harm | 1 (0.1) |
| Suspected nonaccidental trauma | 50 (6.8) |
| Mechanism | |
| Blunt force | 159 (21.5) |
| Foreign body | 102 (13.8) |
| Sports | 96 (13.0) |
| Bug bite/sting | 83 (11.2) |
| Chemical injury | 71 (9.6) |
| Thrown object | 43 (5.8) |
| Fall | 35 (4.7) |
| Pyrotechnics, fireworks, or welding | 29 (3.9) |
| Sharp force | 25 (3.4) |
| Firearm or projectile | 21 (2.8) |
| Motor vehicle accidents | 17 (2.3) |
| Animal bite/scratch | 15 (2.0) |
| Nonaccidental trauma | 3 (0.4) |
| Other/unknown | 41 (5.5) |
| Wearing eye/face protection | 4 (0.5) |
| Initial presentation for care | |
| Emergency department or urgent care | 515 (69.6) |
| Primary care provider | 111 (15.0) |
| Ophthalmology | 94 (12.7) |
| Optometry | 20 (2.7) |
| OD:OS:OU | 329: 335:74 |
| VA < 20/40 at presentation | 99 (13.4) |
OD, right eye; OS, left eye; OU, both eyes; VA, visual acuity.
Of the 473 injuries (64.2%) that required treatment, topical antibiotics (n = 338 [45.7%]) and cycloplegic agents (n = 94 [12.7%]) were most commonly prescribed (eSupplement 2, available at jaapos.org). Less than 10% of patients received imaging at the time of injury, and 131 patients (17.7%) needed a procedural intervention at the time of injury, including foreign body removal (57), eye irrigation (52), and eyelid or adnexal laceration repair (16). Sixteen patients (2.2%) were hospitalized with a median length of stay of 2.5 days (range, 1–18), yielding a hospitalization rate of 4.06 (95% CI, 2.06–6.06) per 100,000 children. Thirty-seven patients (5.1%) required at least one surgical intervention to treat their injuries, with 6 patients requiring more than one surgery. The mean length of follow-up was 12.8 years (range, 0–21.8). Thirty-eight injuries (5.1%) led to post-traumatic sequelae, most commonly angle recession (19), corneal scar (9), and traumatic cataract (7). Of injuries where a final visual acuity was recorded, 55 (7.7%) had a final visual acuity of 20/40 or worse.
An analysis for injury risk factors found that age ≥12, sports injuries, firearm/projectile injuries, and a hyphema observed at the initial examination significantly increased the odds of presenting with visual acuity of 20/40 or worse. However, none of these risk factors increased the odds for decreased visual acuity at final eye examination (Table 4). Male sex, age ≥12 years, injuries occurring while outdoors, sports injuries, firearm/projectile injuries, hyphema seen on examination, and posterior segment involvement all significantly increased the likelihood that patients would develop post-traumatic sequelae.
Table 4.
Risk factors for the development of decreased visual acuity at initial and final exams or development of post-traumatic sequelae among 740 injuries in patients < 19 years of age in Olmsted County, MN from 2000–2009.
| Risk factor | Visual acuity of 20/40 or worse, OR (CI) | Development of post-traumatic sequelae | |
|---|---|---|---|
|
|
|||
| Initial exam | Final exam | OR (CI) | |
| Male sex | 1.23 (0.79–1.93) | 0.65 (0.37–1.13) | 3.36 (1.39–8.15)a |
| Age ≥ 12 years | 3.24 (2.08–5.05)* | 1.04 (0.60–1.81) | 2.93 (1.48–5.83)a |
| Psychiatric comorbidity | 1.35 (0.79–2.31) | 1 (0.48–2.10) | 0.77 (0.29–2.00) |
| Outdoor injury | 1.28 (0.82–1.99) | 0.8 (0.43–1.48) | 3.02 (1.41–6.49)a |
| Nonaccidental injury | 1.32 (0.71–2.45) | 1.34 (0.61–2.95) | 2.16 (0.96–4.89) |
| Sport injury | 2.71 (1.62–4.54)* | 0.65 (0.25–1.68) | 3.88 (1.91 −7.87)a |
| Blunt force injury | 0.91 (0.54–1.55) | 1.71 (0.94–3.12) | 0.54 (0.21–1.40) |
| Firearm/projectile injury | 5.24 (2.15–12.79)* | 1.32 (0.30–5.83) | 22.44 (8.80–57.21)a |
| Hyphema seen on exam | 7.58 (4.44–12.92)* | 0.53 (0.16–1.75) | 37.62 (17.49–80.92)a |
| Posterior segment involvement | 1.56 (0.88–2.78) | 0.39 (0.12–1.26) | 8.62 (4.36–17.02)a |
CI, confidence interval; OR, odds ratio.
P < 0.05.
Discussion
In this population-based cohort of 718 children diagnosed with ocular and adnexal injuries over a 10-year period, the incidence of ocular injury was 203 per 100,000. Injuries most commonly occurred as a result of accidents during outdoor activities, with male children and teenagers at highest risk. Isolated anterior segment injuries were most common, comprising roughly two-thirds of all injuries in this cohort of children. Approximately 1 in 20 injuries required surgical intervention or was associated with long-term sequelae, and 1 in 13 had permanently decreased vision.
The incidence of ocular injuries in this cohort was significantly higher than prior population-based studies that reported incidence rates ranging from 8.14 to 15.2 injuries per 100,000 children.7–9 However, all three prior reports limited inclusion to children who were admitted to the hospital for management of their injuries and limited data collection to a single year, with the most recent data reported from 2000.7 Further, Desai and colleagues9 only gathered data from patients receiving care from an ophthalmologist. As evidenced in this cohort, very few pediatric patients are hospitalized for ocular and adnexal injuries, and most patients initially presented to nonspecialist care (primary care or emergency department), which suggests that previous population-based studies have significantly underestimated the incidence of pediatric ophthalmic injuries. The incidence of ocular injury requiring hospitalization in this cohort was 4.06 per 100,000 children <19 years of age, significantly less than the incidence rates reported in the previous population-based studies limited to inpatient cohorts, but similar to the 3.7 per 100,000 admission rate reported among a Chinese cohort during a similar time period.11 This lower incidence rate for hospitalization may reflect a shift in management for ocular trauma over time, moving away from hospitalization to close outpatient follow-up. The medianlength of hospital stay in this cohort was longer than others,7,15 but the significance of this is uncertain given the limited sample size.
The predominance of anterior segment injuries in this pediatric cohort is consistent with other reports, but the prevalence of isolated posterior segment injuries was lower than others.2,12–13 The most common injuries to the anterior segment were subconjunctival hemorrhages, corneal abrasions, and hyphema. The higher proportion of anterior segment injuries relative to other anatomic regions seen in this cohort may be due to the inclusion of patients who presented to nonspecialist providers, because many minor anterior segment injuries, such as corneal abrasions, nonimplanted foreign bodies, or subconjunctival hemorrhages, are often managed by primary care or emergency department providers without the input of an ophthalmologist. Although posterior segment involvement was relatively less frequent in this cohort, it did increase the odds that such patients would develop long-term complications, though it did not seem to increase risk of decreased initial or final visual acuity.
Injuries were most likely to happen while outside and during the summer months. Other studies have found that injuries were most likely to happen at home,2,4,6,11,14–17 but a minority found injuries to be more common during outside or street play.6,13,18–19 Summer may be the most likely time for injury, because children are out of school and have more opportunities for unstructured or unsupervised activity. Moreover, summer weather permits children to spend more time outside, consistent with the finding that most injuries in this cohort occurred while outdoors. Because the study cohort resides in Minnesota, where residents are more likely to be outdoors during summer months compared to the significantly colder winter months, the seasonal relationship may not persist for cohorts that live in climates with favorable weather for outdoor play year-round. Just over 10% of injuries in this cohort were due to assault or nonaccidental trauma, which was similar to the 14.1% of violence-related injuries seen in a Chinese cohort during the same time period.11 Of note, nonaccidental injuries did not increase the risk for decreased visual acuity or the development of post-traumatic complications.
The observed predominance of males sustaining ocular injuries is consistent with the widely reported trend.2–4,6–9,11,13–20,23 The age groups reported in this study roughly coincide with various daycare or school stages (baby/toddler, preschool, early elementary, late elementary, middle school, and high school), and in this cohort, high school-aged children were at the highest risk of injury. Though the age group at greatest risk varied among previously reported data, most studies identified teenagers or preteens as the highest risk age groups,2,6–9,15,18–19 consistent with the current findings. Other studies reported the highest risk group to be the 0–6 age range,3–4,13,16,20 which was the second highest risk group in our cohort, supporting the notion that eye trauma in children may have a bimodal distribution for younger and older patients. This may be due to the developing gross and fine motor skills in the youngest group and the higher likelihood of sports participation or risky behaviors in the older age group.
Blunt force was the most common mechanism of injury in this cohort, consistent with other reports.2–3,8,13,15 Haring and colleagues21 found that sports injuries, one of the most common mechanisms in this cohort and others, disproportionately occur in children, and these injuries are on the rise.3–4,6 Further, these data suggest that sports injuries are at increased risk for complications. However, increased regulations around eye protection for children’s squash, field hockey, ice hockey, and lacrosse leagues has led to fewer ocular and orbital injuries among participating children.22 Despite these successes, very few patients in this cohort or others report wearing eye protection.16 Though firearm or projectile injuries were uncommonly observed in this cohort, Pollard and colleagues4 demonstrated that such injuries increased from 1990 to 2009 despite an overall decrease in pediatric eye trauma. More recent data has shown that these injuries are on the decline.3 As with sports, firearm and projectile injuries increased risk for long-term complications in this cohort, suggesting that sports and firearms may be meaningful areas of focus to improve visual outcomes in pediatric eye injuries.
The injuries in this cohort rarely required imaging or surgical intervention. Very few patients received ocular-specific imaging, such as optical coherence tomography or B-scan ultrasonography, perhaps due to the cooperation required for these images or due to the more widespread adoption of these imaging modalities since the study period. This cohort had a lower rate of sequelae development than other reports,2,23 likely because of the inclusion of relatively benign injuries seen by nonspecialists. The most common sequela in this cohort was angle recession, whereas other reports found traumatic cataracts to be the most common sequelae.2,20,23 Less than 10% of patients had a final recorded visual acuity worse than 20/40, supporting previous reports that most ocular injuries in children are at low risk for permanent vision loss.2–3,6,9,14,19,23
There are several limitations to the findings of this study. The retrospective design is limited by incomplete data and irregular follow-up. A small minority of patients were potentially not captured by this search if they sought care outside of Olmsted County, thereby underestimating the incidence in this cohort. Furthermore, the limited demographic diversity of Olmsted County compared to the US population limits its generalizability to other populations. The selected time range, local climate, and cultural makeup of the region may also influence generalizability because injuries vary based on these and other circumstances. For example, the presence of a trade school in the area teaching welding may have impacted the number of teenagers diagnosed with photokeratitis in our region compared to other areas. However, the results of this study provide population-based data of pediatric ocular injuries from all providers, demonstrating a higher rate than previously reported in US population studies. Most patients were older children and male, with trauma affecting the anterior segment alone in two-thirds of cases, and causing permanent visual loss in 1 in 10.
Supplementary Material
eSupplement 1. ICD-9 codes used to search the Rochester Epidemiology Project Database to identify potential cases of eye trauma.
eSupplement 2. Prescriptions, imaging, and interventions in the evaluation and treatment of 740 ocular and adnexal injuries.
Acknowledgments
This research was supported by funding from the Rochester Epidemiology Project {(REP) medical records-linkage system, which is supported by the National Institute on Aging (NIA; AG 058738), by the Mayo Clinic Research Committee, and by fees paid annually by REP users.} in Olmsted County, MN. The Rochester Epidemiology Project had no role in the study design, data collection, analysis, data interpretation, or in writing and submission of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Pizzarello LD. Ocular trauma: time for action. Ophthalmic Epidemiol 1998;5:115–16. [DOI] [PubMed] [Google Scholar]
- 2.Boret C, Brehin C, Cortey C, et al. Pediatric ocular trauma: characteristics and outcomes among a French cohort (2007–2016). Arch Pediatr 2020;27:128–34. [DOI] [PubMed] [Google Scholar]
- 3.Matsa E, Shi J, Wheeler KK, McCarthy T, McGregor ML, Leonard JC. Trends in US emergency department visits for pediatric acute ocular injury. JAMA Ophthalmol 2018;136:895–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pollard KA, Xiang H, Smith GA. Pediatric eye injuries treated in US emergency departments, 1990–2009. Clin Pediatr (Phila) 2012;51:374–81. [DOI] [PubMed] [Google Scholar]
- 5.Luo H, Shrestha S, Zhang X, Saaddine J, Zeng X, Reeder T. Trends in eye injuries and associated medical costs among children in the United States, 2002–2014. Ophthalmic Epidemiol 2018;25:280–87. [DOI] [PubMed] [Google Scholar]
- 6.Haavisto AK, Sahraravand A, Holopainen JM, Leivo T. Paediatric eye injuries in Finland—Helsinki eye trauma study. Acta Ophthalmol 2017;95:392–9. [DOI] [PubMed] [Google Scholar]
- 7.Brophy M, Sinclair SA, Hostetler SG, Xiang H. Pediatric eye injury-related hospitalizations in the United States. Pediatrics 2006;117:e1263–71. [DOI] [PubMed] [Google Scholar]
- 8.Strahlman E, Elman M, Daub E, Baker S. Causes of pediatric eye injuries: a populationbased study. Arch Ophthalmol 1990;108:603–6. [DOI] [PubMed] [Google Scholar]
- 9.Desai P, MacEwen CJ, Baines P. Minassian DC. Incidence of cases of ocular trauma admitted to hospital and incidence of blinding outcome. Br J Ophthalmol 1996;80:592–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Melton LJ. History of the Rochester Epidemiology Project. Mayo Clin Proc 1996;71:266–74. [DOI] [PubMed] [Google Scholar]
- 11.Cao H, Li L, Zhang M, Li H. Epidemiology of pediatric ocular trauma in the Chaochan Region, China, 2001–2010. PLoS One 2013;8:e60844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barry RJ, Sii F, Bruynseels A, et al. The UK Paediatric Ocular Trauma Study 3 (POTS3): clinical features and initial management of injuries. Clin Ophthalmol 2019;13:1165–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al Wadeai EAY, Abdellatif Osman A, Macky TA, Soliman MM. Epidemiological features of pediatric ocular trauma in Egypt. J Opthalmol 2016;2016:7874084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Archambault C, Gabias C, Fallaha N, Belanger C, Superstein R. Pediatric ocular injuries: a 3-year review of patients presenting to an emergency department in Canada. Can J Ophthalmol 2019;54:83–6. [DOI] [PubMed] [Google Scholar]
- 15.Puodžiuvienė E, Jokūbauskienė G, Vieversytė M, Asselineau K. A five-year retrospective study of the epidemiological characteristics and visual outcomes of pediatric ocular trauma. BMC Ophthalmol 2018;18:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferguson RA, Sung J, McKelvie J. New Zealand childhood ocular trauma study: analysis of 75 601 cases of ocular injury from 2007 to 2016. Clin Exp Ophthalmol 2019;47:718–25. [DOI] [PubMed] [Google Scholar]
- 17.Sii F, Barry RJ, Abbott J, Blanch RJ, MacEwen CJ, Shah P. The UK Paediatric Ocular Trauma Study 2 (POTS2): demographics and mechanisms of injuries. Clin Ophthalmol 2018;12:105–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gise R, Truong T, Poulsen DM, Soliman Y, Parsikia A, Mbekeani JN. Pediatric traumatic brain injury and ocular injury. J AAPOS 2018;22:421–5. [DOI] [PubMed] [Google Scholar]
- 19.Bućan K, Matas A, Lovrić JM, et al. Epidemiology of ocular trauma in children requiring hospital admission: a 16-year retrospective cohort study. J Glob Health 2017;7:010415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guo Y, Liu Y, Xu H, Zhao Z, Gan D. Characteristics of paediatric patients hospitalised for eye trauma in 2007–2015 and factors related to their visual outcomes. Eye (Lond) 2021;35:945–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haring RS, Sheffield ID, Canner JK, Schneider EB. Epidemiology of sports-related eye injuries in the United States. JAMA Ophthalmol 2016;134:1382–90. [DOI] [PubMed] [Google Scholar]
- 22.Hoskin AK, Philip SS, Yardley AM, Mackey DA. Eye injury prevention for the pediatric population. Asia Pac J Ophthalmol (Phila) 2016;5:202–11. [DOI] [PubMed] [Google Scholar]
- 23.Schneider K, Nguyen-Tran H, Segura BJ, Areaux RG, Nerheim D, Louie JP. Ocular injury presenting to a level-III pediatric trauma center. Pediatr Emerg Care 2020;36:e606–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eSupplement 1. ICD-9 codes used to search the Rochester Epidemiology Project Database to identify potential cases of eye trauma.
eSupplement 2. Prescriptions, imaging, and interventions in the evaluation and treatment of 740 ocular and adnexal injuries.