Abstract
Background:
Many patients do not engage in health behaviors that can control common, chronic illnesses. Clinicians have opportunities to promote health behaviors yet may lack skills for coaching effectively about health behaviors.
Objectives:
Our aims are to: present definitions of coaching, propose concepts for coaching about behavior change from two theories, share theory-guided research on behavior change relevant to ambulatory care settings, and delineate how concepts from these theories can guide coaching.
Methods:
In our discussion, we explain how two behavioral theories are complementary and applicable to coaching, present empirical support for these theories, and describe applications of these concepts for practice.
Conclusions & Practice Implications:
Self-determination theory can guide clinicians in how to interact with patients to meet patients’ psychological needs, to promote health behaviors, and subsequent health status. Self-regulation theory can guide coaches in what concepts to address for behavior change. These complementary theories have been supported in rigorous research with adult populations in ambulatory care settings.
Key words from MeSH headings: Behavior, Health promotion, Disease, Secondary Prevention, Psychosocial intervention, Primary prevention
1. Introduction
Chronic illnesses (CIs), such as hypertension and diabetes, are major threats to morbidity and mortality [1]. The top twenty reasons for U.S. ambulatory visits reflect issues regarding CIs. These include progress visits for monitoring CIs, completion of exams or tests for CIs, discussion of test results, monitoring of side effects of medications, and counseling [2].
Differences continue to exist between clinicians’ recommendations for health behaviors to control CIs and patients’ actual health behaviors [3–5]. Only about 22.5% of U.S. adults have met physical activity guidelines for aerobic and strengthening activity; only 6–9% of U.S. adults have met dietary recommendations to eat 2 cups of fruit daily [6]. Patients report knowing health recommendations yet experience barriers to initiating and sustaining health behaviors [3, 7]. Diverse barriers can inhibit health behaviors including personal, interpersonal, socio-cultural, and environmental factors (e.g., affordability, accessibility, and acceptability of services). Social determinants of health interfere with health behaviors, such as economic stability, health care access, and social and community contexts [3, 8]. Because people have feelings, beliefs, and values about what is important in life and these aspects can influence health behaviors, clinicians need to understand and discuss these aspects with patients [3].
Many clinicians – including exercise physiologists, nurse practitioners, pharmacists, physician assistants, and physicians -- work in ambulatory settings. Clinicians have opportunities to discuss health behaviors that are associated with CIs (e.g., diet, stress management). With evidence-based, communication skills, clinicians can be effective in promoting patients’ health behaviors and controlling CIs [9]. Yet, clinicians do not engage patients in substantive discussions about health behavior change as often as desired for CI control; they may have organizational, structural, and professional barriers to doing so [10]. Busy clinicians tend to inform patients about what they should do for health, rather than engaging patients in discussions about their beliefs, behaviors, and health goals. We acknowledge increasing demands for efficiency in ambulatory settings. Nevertheless, CI control is needed to maximize people’s health and minimize clinicians’ demands in the long term.
Scholars have identified effective communications that can promote patients’ health behaviors [9, 11–13]. In this paper, we share concepts that clinicians can use to guide such communications. Having a set of concepts to guide coaching could improve clinicians’ efficiency and effectiveness in promoting health behaviors. Our aims are to: 1) present a definition of coaching drawn from literature, 2) propose concepts to guide coaching about behavior change from two, complementary theories; 3) share theory-guided research on behavior change, and 4) describe how concepts from theories can guide coaching in ambulatory care. We use the term “clinician” to refer to health practitioners in general and “coach” to refer to one who has communication skills for behavior change.
1.1. Coaching in health care contexts
The term “coaching” has been used frequently in health care, yet inconsistently [9]. Coaching has been described as an approach or service that is patient-centered [14, 15] as well as an integration and application of health education and promotion skills [12]. Coaches facilitate patients in taking actions towards healthy behaviors, using education and motivational strategies [10, 12, 16–19]. The desired outcomes are for patients to reach their feasible health goals and improve overall health [12, 17, 18]. We propose that health coaching involves clinicians working collaboratively to support patients in reaching a mutually agreed upon health goal, with “health” broadly defined.
For effective coaching, clinicians and patients have respect for each other [13, 16, 19]. Clinicians respect patients’ expertise about themselves, their life context, preferences, and values; patients’ respect the professional expertise of clinicians. Skillful coaches are sensitive to potential status or power differences, have knowledge about the frequency of, and rationale for, health behaviors, as well as mastery of concepts for effective communication and behavior change [19]. Ethically, patients have moral autonomy to decide how to address health threats from CIs (including non-action) if they are cognitively intact and mentally stable [20, 21].
1.2. Challenges to coaching in practice
We recognize demands for efficiency that influence clinicians’ capacity to offer meaningful coaching [22]; these are beyond the scope of this paper. For example, building rapport with patients is critical and can take time that clinicians may not perceive they have. However, clinicians can build rapport in a time-efficient manner by modifying their communication patterns. Clinicians can pose open-ended questions at the start of visits to gather patient-centered information and then collaboratively discuss setting agendas for visits and long-term care plans. Clinicians’ communications – such as clarifying information and acknowledging patients’ feelings -- can influence patient satisfaction and health status [23, 24]. Patient satisfaction can be fostered by clinicians intentionally listening and/or clarifying meanings of issues. Time spent “upfront” to understand patients’ concerns can “pay off” later when discussing steps to control CIs. In ambulatory settings, there are challenges to improving quality of care and clinicians’ discussions with patients about recommended preventive behaviors, including screening [22]. Time constrictions are one example of this, however time per visit should not be the only important outcome in providing healthcare.
For instance, imagine a clinician who has completed their assessment of a patient who has CIs that are not well-controlled. If they were to discuss all the ways the patient could improve their health, then the patient could be overwhelmed, and they could run late. Instead, they can pose a focused, open-ended question: “Given your conditions and situation, what step(s) would you be willing to take now for your health, if any?” Responses to this question can direct the clinician’s conversation mindful of the patient’s goal(s) [3, 19]. Clinicians can support many patient-chosen steps (e.g., eating less fat or sugar) and focus on one behavioral step at a time. They can address essential medical content and ask the patient to return for follow up.
2. Applying behavioral theories to coaching
As interdisciplinary clinicians in ambulatory care, the authors sought ways to improve communications with patients for behavior change. Because theories can be useful roadmaps in practice and research, the last author had reviewed behavioral theories critically for usefulness, clarity, adequacy, parsimony, and empirical support. From this review, two theories were identified as promising to guide coaching: self-determination theory and self-regulation theory [14, 25, 26]. We discuss these two theories and their corresponding concepts, that is, “key ingredients”, in relation to coaching. Thus, we answer a scholars’ call to clarify theoretical foundations for coaching [15]. We present concepts from self-determination theory (SDT) because they can guide clinicians in how to communicate effectively to elicit patients’ autonomous motivation for health behaviors and outcomes. We present concepts from self-regulation theory (SRT) because they reflect what type of information patients need to adopt new behaviors and monitor progress.
2.1. Self-regulation theory
In self-regulation theory (SRT) [17, 18], self-regulation refers to one’s abilities to initiate, monitor, persist and/or alter one’s behavior, emotions, and cognitive strategies, with new stimuli or information, and reach one’s personal goals. Concepts in SRT include information, reference points, comparisons, feedback, decision points, and actions [12, 17]. Figure 1 presents self-regulation processes. For example, consider people hearing that they should “be more active” or “maintain a normal blood pressure”. For people to interpret whether activity or BP levels are desirable, they need to know specific recommendations for such. The recommendations serve as reference points, that is, standards, for comparison [17, 27].
Figure 1.
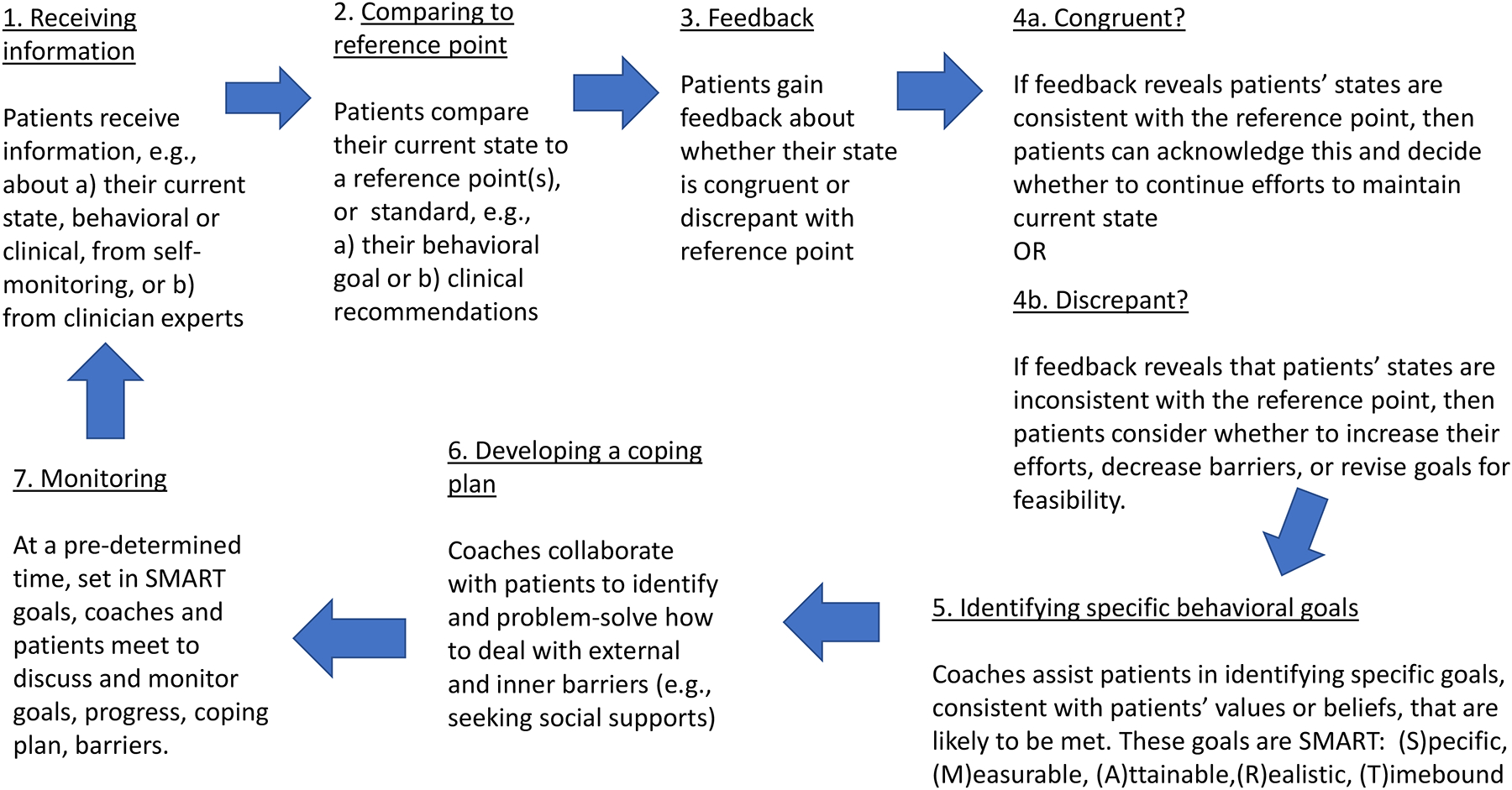
Concepts and processes of self-regulation theory
Many peoples’ behaviors are discrepant with recommendations [3–5]. When peoples’ current states are moderately or markedly discrepant with recommendations, coaches and patients can collaborate to set short-term, learning, or proximal goals to strive to achieve longer-term, performance, or distal goals [28, 29]. When this situation exists, patients compare their behavioral states to their behavioral goals, rather than to actual recommendations.
By making such comparisons, patients receive feedback about whether their states are congruent with their behavioral goals. If patients’ states are congruent with their goals or recommendations, they can affirm their behavioral efforts, decide to maintain or revise their goals, and monitor their progress again. If patients’ states are discrepant with their goals, then they can discuss with coaches what to do next, such as: try harder, address barriers, or revise their goal for feasibility.
Coaches collaborate with patients to establish behavioral goals with certain criteria because these goals are likely to be met. These SMART criteria are: (S)pecific, (M)easurable, (A)ttainable, (R)ealistic and (T)ime-bound [7, 29]. Although some discrepancy between ones’ current and ideal states can be motivating, high levels can be inhibiting [17]. Effective coaches also facilitate patients in making coping plans to deal with expected barriers goals (see Table 1) to maximize behavioral progress. The SRT process repeats as patients maintain, or strive to improve, health behaviors, refine goals, or deal with relapse [17, 29].
Table 1.
Content to address in health coaching, according to self-regulation theory
|
2.2. Empirical support for self-regulation theory
Scholars have conducted rigorous reviews about intervention efficacy on health behaviors, guided by SRT. In a meta-analysis, Epton and colleagues examined the efficacy of interventions with goal setting components on health behaviors [30]. They found goal setting had a unique effect on promoting different behaviors, consistent with another meta-analysis [31]. This approach was most effective when goals were moderately difficult, set in front of others (vs. online), and shared by a group (vs. an individual). Harkin’s team found the frequency with which coaches monitored patients’ goals was associated with patients’ behavioral progress [18, 30], especially when contacts were recorded [18]. Monitoring progress is analogous to comparing current and desired states (c.f., Figure 1). Clinical interventions incorporating electronic devices were associated with more frequent monitoring and goal attainment [18, 30].
Michie and colleagues identified theoretically-based, intervention components that improved activity and eating behaviors [32]. These included prompting of self-monitoring and self-monitoring with another SRT component (e.g., goal setting, feedback). Other researchers [31] reported that individualized feedback, along with other SRT component, can support behavior change [31, 32]. Cochrane reviewers [33] concluded feedback can be helpful when it is individualized, behaviorally specific, shared non-judgmentally, more than once, verbally and in writing, with particular plans. Suls and team [12] documented that monitoring has been associated with improvements in blood pressure, activity, and eating. In another review, the interventional approaches that improved physical activity were goal setting, self-monitoring, and problem solving [29, 31]. Problem-solving about barriers can involve incorporating social supports into one’s coping plans [34].
2.3. Self-determination theory (SDT)
Psychologists [35] developed and tested SDT, based in part on humanistic assumptions. SDT includes the concepts of relatedness, autonomy, perceived competence, which are psychological needs, and type of motivation. According to SDT, when peoples’ psychological needs are met, they are likely to be autonomously motivated to engage in corresponding behaviors [14, 35]. See Figure 2.
Figure 2.
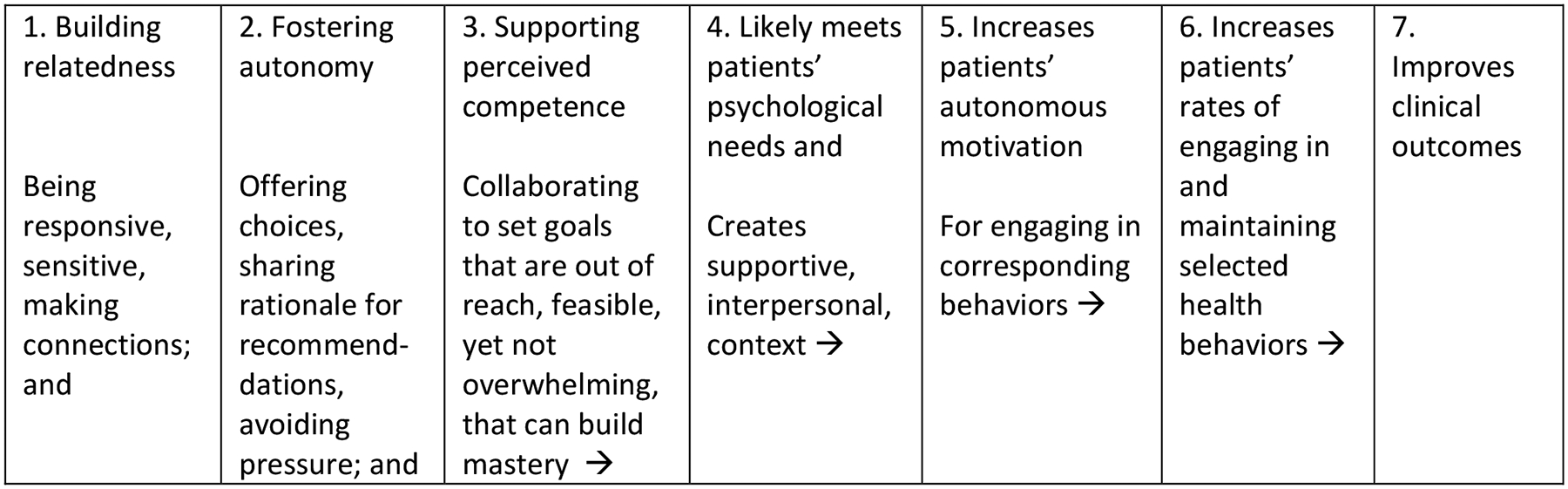
How clinicians can guide discussions with patients to create supportive environments for behavior change, based on self-determination theory
“Relatedness” refers to peoples’ experiences of others as responsive and sensitive as well as having abilities to be responsive and sensitive to others [35]. Relatedness is characterized as feeling close and connected with significant people, including clinicians [36]. “Autonomy” refers to peoples’ sense of willingness or volition regarding goals and behaviors. Autonomy is characterized by people choosing freely, without pressure, from within or outside themselves [35, 37]. “Perceived competence” refers to feeling effective and capable as well as having some mastery regarding behaviors that correspond with goals [36, 37]; it is analogous to self-efficacy. Perceived competence has been consistently and positively associated with starting new behaviors when behaviors had been adopted for people’s own motives [13]. Figure 3.
Figure 3.
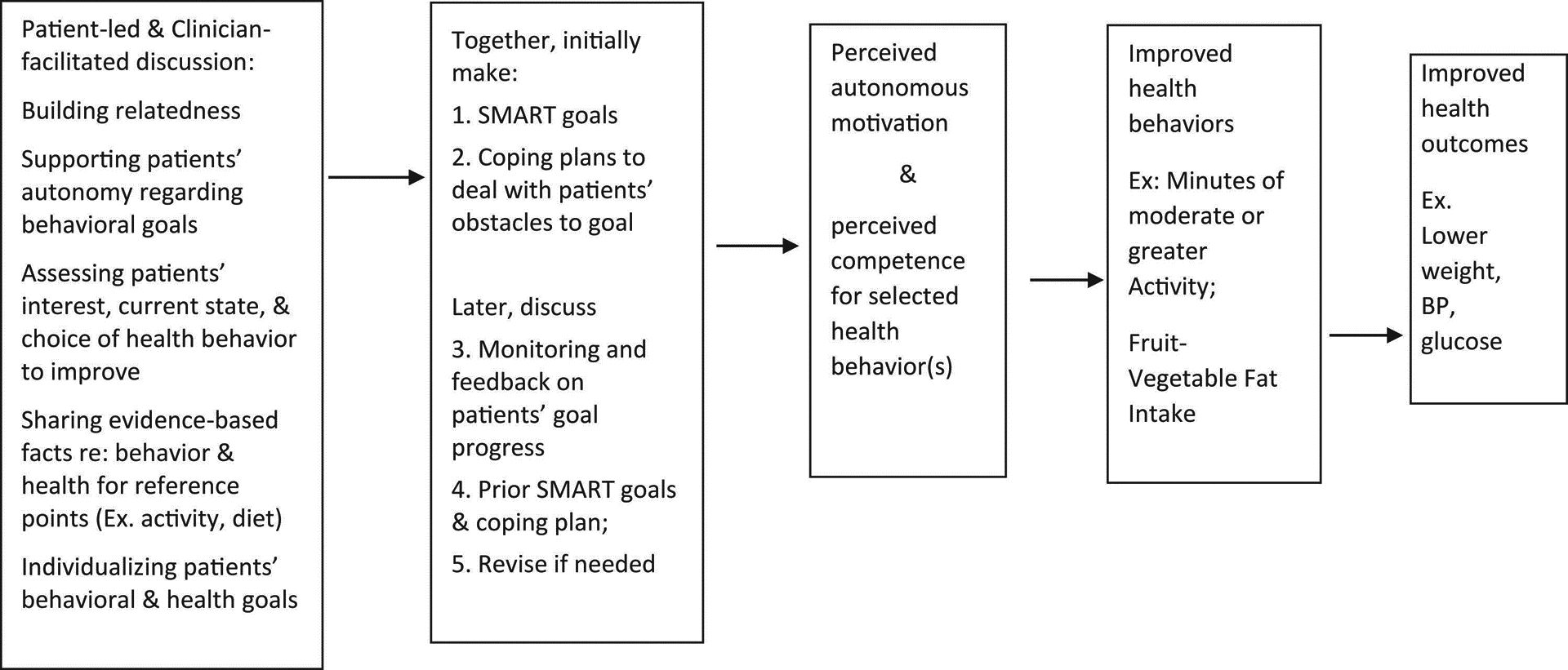
Combining concepts reflecting “what” to address and “how” to discuss topics in health coaching;
Integrating concepts from self-regulation & self-determination theories to health behavior coaching
People can experience controlling or autonomous motivation or amotivation. Controlling motivation refers to feeling pressured to act, from within oneself or from others; autonomous motivation refers to having the abilities to choose freely. Whereas in SDT, motivation refers to a type or quality of motivation [37], in common usage, motivation refers to the degree of reasons for action. Experiencing controlled motivation can inhibit people from engaging in a corresponding behavior [35, 36]. When patients are amotivated, clinicians can discuss deferring behavioral changes until patients’ motivation or situations improve [8].
2.4. Empirical support for SDT
In experimental studies based on SDT, researchers interacted with adults to meet their psychological needs, set health behavior goals, and observe health outcomes. Williams’ team [38] created a supportive environment and addressed autonomous motivation and perceived competence with patients who were smokers and had elevated cholesterol levels. Compared to usual care, intervention participants had a) higher scores on autonomous motivation and perceived competence at 6 months; b) higher smoking cessation and medication use rates, and lower LDL-C levels, at 12-months. Silva’s team [39] interacted with women to improve weight control. Compared to controls, intervention participants had higher autonomous motivation and activity scores, and weight loss one year later. In another intervention guided by SDT, researchers demonstrated improved autonomous motivation and perceived competence for dental care among patients post-intervention and subsequently less gingivitis and plaque in these patients [40]. In a systematic review, researchers [24] reported that autonomous motivation and perceived competence in activity predicted physical activity. In another systematic review, researchers concluded that interventions based on SDT improved health outcomes [13].
3. Integrating & Applying complementary concepts to coaching in healthcare
At the start of patient interactions, coaches use open-ended questions and assess patients’ current situation, beliefs, and values [3, 7, 19, 41]. Establishing relatedness, coaches demonstrate concern, use silence, and listen empathetically when collecting histories [36, 37]. Supporting relatedness and autonomy, coaches assess patients’ issues and reasons for seeking care now [7, 34]. Coaches share their clinical assessments and recommendations with rationale [36]; they ask patients for their questions.
Coaches can support patients’ autonomy when discussing diagnoses and plans [36, 37]. Coaches ask permission to share relevant information (e.g., “Would it be alright if I shared more …?”). Coaches offer a set of good options (e.g., medications, tests, or watchful waiting). To avoid conveying control, coaches make more open-ended questions than declarative statements [19, 37]. Patients may express ambivalence to proposed plans or behaviors. If so, coaches assess patients’ perceived advantages and disadvantages regarding behavior change to understand patients and tailor discussions [3, 9, 41, 42]. If patients prefer to take approaches that clinicians consider risky, then clinicians explain their concerns for patients’ safety (i.e., rationale) if they were to take these approaches. By doing so, clinicians can act beneficently and respectfully [20, 21].
Coaches elicit from patients what behavioral goals they would be interested in pursuing for health (i.e., assessing autonomous motivation]. When asked about goals, patients typically offer general statements (e.g., “to avoid medicines” or “to lose weight”). These desired states are relatively abstract, reflect patients’ values, and can be motivating, yet are not specific enough to guide behavior effectively [17, 27, 32]. Coaches typically need to clarify what specific type of short-term, proximal, behavioral goal would be realistic and aligned with patients’ long-term, distal, health goals. Coaches strive to be as specific in clarifying patients’ goals as clinicians are when writing prescriptions. Patients need to know the type, intensity, frequency, and duration of activities that could result in improved outcomes (e.g., lower weight, blood pressure) for self-monitoring purposes, consistent with SRT [17, 43].
Coaches assess patients’ perceived competence in implementing their plans and explain that lacking competence can interfere with adopting new behaviors. Providing some structure, coaches collaborate on identifying behavioral goals with patients; goals likely to be met are achievable, moderately difficult, yet psychologically challenging [17, 35, 36]. By identifying feasible goals with patients, coaches foster patients’ perceived and actual competence at new behaviors. Coaches ask about realistic barriers (e.g., “What might stand in your way of taking your planned steps?”). Coaches elicit from patients how they would deal with barriers and discuss coping plans [7, 17]. Withholding suggestions, coaches encourage patients to problem-solve ways to deal with barriers. When patients have identified realistic solutions to their barriers, they may be likely to overcome barriers because they have mentally rehearsed how to do so. If patients’ barriers are, “I haven’t gotten around to it yet” or lack of motivation, coaches can ask something such as, “What would it take to change this situation?”. Coaches can also assess patients’ past experiences with similar barriers and how patients dealt with them. Coaches acknowledge patients’ feelings related to barriers (e.g., discouragement), unsuccessful attempts, or uneasiness about changing an undesired habit [3, 4, 17].
By identifying patients’ short- and long-term health goal(s), coaches and patients have standards (per SRT) against which to monitor progress [17, 27]. Patients can compare their current behaviors to short-term goals (e.g., “fitting in a black dress”), long-term goals (e.g., maintaining a healthy weight), and/or clinical recommendations (e.g., recommended BMI). If patients’ weights are discrepant with recommendations, then patients may be motivated to improve their behaviors and meet their goals (“fitting in a black dress”). When coaches collaborate with patients on behavioral goals that meet SMART criteria, then goal attainment may be likely [42].
At follow-up visits, coaches continue to apply SDT concepts to meet patients’ psychological needs. Coaches prompt patients to monitor their behaviors against their goals or clinical recommendations, consistent with SRT [17, 27]. If patients have met their goals, then coaches acknowledge progress objectively and specifically (e.g., “What you did is impressive!”), rather than generally or with evaluative comments (e.g., “You’re awesome!”) [33, 35, 36]. This approach can support patients’ continued efforts [33]. To support patients’ perceived competence with new behaviors, coaches can ask, “What worked well for you?”. When patients’ behaviors and goals are discrepant, coaches can ask, “How does your behavior of X fit with your health goal of Y?”. Coaches re-assess patients’ barriers and feasible ways of dealing with them. If patients’ goals were too difficult, then coaches non-judgmentally ask about barriers or revision of goals. Coaches can make reflections rather than asking many questions; they avoid asking questions beginning with “Why didn’t you…?”; to avoid defensiveness. By acting neutrally, coaches can foster patients’ autonomy in choosing new behaviors [24].
4. Conclusions
In this paper, we presented an innovative integration of SRT and SDT to guide coaching to promote recommended health behaviors. The SRT and SDT concepts are complementary and useful to clinician interactions with adult patients who are cognitively intact [14, 25]. Guided by SDT concepts, clinicians create supportive environments in which to meet patients’ psychological needs. In turn, coaches foster autonomous motivation for patients’ behavioral goals and health. Guided by SRT concepts, clinicians can offer the type of information that patients need to adopt, monitor, and self-regulate their efforts towards behavioral goals and health. By applying this integrated set of concepts in coaching, clinicians can support patients in improving their health behaviors and corresponding CIs.
Acknowledgements:
This manuscript was written as part of a larger project; the larger project is entitled, Testing outcomes of coaching interventions to control hypertension among young adults in a health maintenance organization. The project is funded from National Heart, Lung, and Blood Institute at the National Institutes of Health (NIH), 1R01HL132148-01A1. To clarify, no institute at NIH has been involved in any aspect of this manuscript.
Contributor Information
Megan Knutson Sinaise, Department of Obstetrics and Gynecology, Division of Maternal Fetal Medicine, University of Wisconsin-Madison School of Medicine and Public Health, 1010 Mound Street, Madison, WI 53715.
Abigail Tran, System Cancer Service Line, Advocate-Aurora Health, 2900 W. Oklahoma Ave., Milwaukee, WI 53215.
Heather M. Johnson, Christine E. Lynn Women’s Health & Wellness Institute, Boca Raton Regional Hospital; Baptist Health South Florida, Florida Atlantic University, 690 Meadows Road; Boca Raton, FL 33486.
Lisa Sullivan Vedder, Department of Family Medicine, Advocate-Aurora University of Wisconsin Group, Aurora Sinai Medical Center, 945 N 12th Street, Milwaukee, WI 53233.
Kara K Hoppe, Department of Obstetrics and Gynecology, Division of Maternal Fetal Medicine, University of Wisconsin-Madison School of Medicine and Public Health, 1010 Mound Street, Madison, WI 53715.
Diane Lauver, School of Nursing & School of Medicine and Public Health, University of Wisconsin-Madison.
References
- [1].Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP): About Chronic Diseases, https://www.cdc.gov/chronicdisease/about/; 2021. [accessed 7 July 2021].
- [2].Centers for Disease Control and Prevention. National Ambulatory Medical Care Survey: 2018 National Summary Tables, https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2018-namcs-web-tables-508.pdf; 2018. [accessed 7 July 2021].
- [3].Herrera PA, Moncada L, Defey D. Understanding non-adherence from the inside: Hypertensive patients’ motivations for adhering and not adhering. Qual Health Res. 2017;27:1023–34. 10.1177/1049732316652529. [DOI] [PubMed] [Google Scholar]
- [4].Mogre V, Johnson NA, Tzelepis F, Shaw JE, Paul C. A systematic review of adherence to diabetes self-care behaviours: Evidence from low- and middle-income countries. J Adv Nurs. 2019;75:3374–89. 10.1111/jan.14190. [DOI] [PubMed] [Google Scholar]
- [5].Tollosa DN, Tavener M, Hure A, James EL. Adherence to multiple health behaviours in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv. 2019;13:327–43. 10.1007/s11764-019-00754-0. [DOI] [PubMed] [Google Scholar]
- [6].Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: A report from the American Heart Association. Circulation. 2019;139:e56–e528. 10.1161/cir.0000000000000659. [DOI] [PubMed] [Google Scholar]
- [7].Lenzen SA, Daniëls R, van Bokhoven MA, van der Weijden T, Beurskens A. Disentangling self-management goal setting and action planning: A scoping review. PLoS One. 2017;12:e0188822. 10.1371/journal.pone.0188822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Adler NE, Glymour MM, Fielding J. Addressing Social Determinants of Health and Health Inequalities. Jama. 2016;316:1641–2. 10.1001/jama.2016.14058. [DOI] [PubMed] [Google Scholar]
- [9].An S, Song R. Effects of health coaching on behavioral modification among adults with cardiovascular risk factors: Systematic review and meta-analysis. Patient Educ Couns. 2020;103:2029–38. 10.1016/j.pec.2020.04.029. [DOI] [PubMed] [Google Scholar]
- [10].Wändell PE, de Waard AM, Holzmann MJ, Gornitzki C, Lionis C, de Wit N, et al. Barriers and facilitators among health professionals in primary care to prevention of cardiometabolic diseases: A systematic review. Fam Pract. 2018;35:383–98. 10.1093/fampra/cmx137. [DOI] [PubMed] [Google Scholar]
- [11].Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health. 2011;26:1479–98. 10.1080/08870446.2010.540664. [DOI] [PubMed] [Google Scholar]
- [12].Suls J, Mogavero JN, Falzon L, Pescatello LS, Hennessy EA, Davidson KW. Health behaviour change in cardiovascular disease prevention and management: meta-review of behaviour change techniques to affect self-regulation. Health Psychology Review. 2020;14:43–65. 10.1080/17437199.2019.1691622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Teixeira PJ, Carraça EV, Markland D, Silva MN, Ryan RM. Exercise, physical activity, and self-determination theory: a systematic review. Int J Behav Nutr Phys Act. 2012;9:78. 10.1186/1479-5868-9-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Worawong C, Borden MJ, Cooper KM, Pérez OA, Lauver D. Evaluation of a Person-Centered, Theory-Based Intervention to Promote Health Behaviors. Nurs Res. 2018;67:6–15. 10.1097/nnr.0000000000000254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Hill B, Richardson B, Skouteris H. Do we know how to design effective health coaching interventions: a systematic review of the state of the literature. Am J Health Promot. 2015;29:e158–68. 10.4278/ajhp.130510-LIT-238. [DOI] [PubMed] [Google Scholar]
- [16].Olsen JM, Nesbitt BJ. Health coaching to improve healthy lifestyle behaviors: an integrative review. Am J Health Promot. 2010;25:e1–e12. 10.4278/ajhp.090313-LIT-101. [DOI] [PubMed] [Google Scholar]
- [17].Carver CS, & Scheier MF. A Model of Behavioral Self-Regulation. Handbook of Theories of Social Psychology: Volume 1. London: SAGE Publications Ltd.; 2012. [Google Scholar]
- [18].Harkin B, Webb TL, Chang BP, Prestwich A, Conner M, Kellar I, et al. Does monitoring goal progress promote goal attainment? A meta-analysis of the experimental evidence. Psychol Bull. 2016;142:198–229. 10.1037/bul0000025. [DOI] [PubMed] [Google Scholar]
- [19].Linden A, Butterworth SW, Prochaska JO. Motivational interviewing-based health coaching as a chronic care intervention. J Eval Clin Pract. 2010;16:166–74. 10.1111/j.1365-2753.2009.01300.x. [DOI] [PubMed] [Google Scholar]
- [20].Beauchamp TL. Methods and principles in biomedical ethics. J Med Ethics. 2003;29:269–74. 10.1136/jme.29.5.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].American Nurses Association. Guide to the code of ethics for nurses: Interpretation and application, Second Edition. MD: American Nurses Association: Silver Spring; 2015. [Google Scholar]
- [22].Chen LM, Farwell WR, Jha AK. Primary care visit duration and quality: does good care take longer? Arch Intern Med. 2009;169:1866–72. 10.1001/archinternmed.2009.341. [DOI] [PubMed] [Google Scholar]
- [23].Robinson JD, Heritage J. Physicians’ opening questions and patients’ satisfaction. Patient Educ Couns. 2006;60:279–85. 10.1016/j.pec.2005.11.009. [DOI] [PubMed] [Google Scholar]
- [24].Ntoumanis N, Ng JYY, Prestwich A, Quested E, Hancox JE, Thøgersen-Ntoumani C, et al. A meta-analysis of self-determination theory-informed intervention studies in the health domain: effects on motivation, health behavior, physical, and psychological health. Health Psychology Review. 2021;15:214–44. 10.1080/17437199.2020.1718529. [DOI] [PubMed] [Google Scholar]
- [25].Johnson HM, Sullivan-Vedder L, Kim K, McBride PE, Smith MA, LaMantia JN, et al. Rationale and study design of the MyHEART study: A young adult hypertension self-management randomized controlled trial. Contemp Clin Trials. 2019;78:88–100. 10.1016/j.cct.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Ramly E, Lauver DR, Gilmore-Bykovskyi A, Bartels CM. Interactive and Participatory Audit and Feedback (IPAF): theory-based development and multi-site implementation outcomes with specialty clinic staff. Implement Sci Commun. 2021;2:58. 10.1186/s43058-021-00155-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Taylor SD, Bagozzi RP, Gaither CA, Jamerson KA. The bases of goal setting in the self-regulation of hypertension. Journal of Health Psychology. 2006;11:141–62. 10.1177/1359105306058869. [DOI] [PubMed] [Google Scholar]
- [28].Locke EA, Latham GP. The development of goal setting theory: A half century retrospective. Motivation Science. 2019;5:93–105. [Google Scholar]
- [29].Swann C, Rosenbaum S, Lawrence A, Vella SA, McEwan D, Ekkekakis P. Updating goal-setting theory in physical activity promotion: a critical conceptual review. Health Psychol Rev. 2021;15:34–50. 10.1080/17437199.2019.1706616. [DOI] [PubMed] [Google Scholar]
- [30].Epton T, Currie S, Armitage CJ. Unique effects of setting goals on behavior change: Systematic review and meta-analysis. J Consult Clin Psychol. 2017;85:1182–98. 10.1037/ccp0000260. [DOI] [PubMed] [Google Scholar]
- [31].Hennessy EA, Johnson BT, Acabchuk RL, McCloskey K, Stewart-James J. Self-regulation mechanisms in health behavior change: a systematic meta-review of meta-analyses, 2006–2017. Health Psychol Rev. 2020;14:6–42. 10.1080/17437199.2019.1679654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28:690–701. 10.1037/a0016136 [DOI] [PubMed] [Google Scholar]
- [33].Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012:Cd000259. 10.1002/14651858.CD000259.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Gillison FB, Rouse P, Standage M, Sebire SJ, Ryan RM. A meta-analysis of techniques to promote motivation for health behaviour change from a self-determination theory perspective. Health Psychol Rev. 2019;13:110–30. 10.1080/17437199.2018.1534071. [DOI] [PubMed] [Google Scholar]
- [35].Ryan RM, Deci EL. Psychological needs: Varied concepts and a preliminary description of SDT’s approach, Self-determination theory: Basic psychological needs in motivation, development, and wellness. New York: Guilford Press; 2017 [Google Scholar]
- [36].La Guardia J Self-determination theory in practice. How to create an optimally supportive health care environment: Self published; 2017. [Google Scholar]
- [37].Sheldon KM, Williams G. Joiner T. Self-determination theory in the clinic: Motivating physical and mental health. New Haven & London: Yale University Press; 2003. [Google Scholar]
- [38].Williams GC, McGregor H, Sharp D, Kouldes RW, Lévesque CS, Ryan RM, et al. A self-determination multiple risk intervention trial to improve smokers’ health. J Gen Intern Med. 2006;21:1288–94. 10.1111/j.1525-1497.2006.00621.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Silva MN, Vieira PN, Coutinho SR, Minderico CS, Matos MG, Sardinha LB, et al. Using self-determination theory to promote physical activity and weight control: a randomized controlled trial in women. Journal of Behavioral Medicine. 2010;33(2):110–22. 10.1007/s10865-009-9239-y. [DOI] [PubMed] [Google Scholar]
- [40].Halvari AEM, Halvari H. Motivational predictors of change in oral health: An experimental test of self-determination theory. Motivation and Emotion. 2006;30:295–306. 10.1007/s11031-006-9035-8. [DOI] [Google Scholar]
- [41].Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. Second Edition. New York, New York: Guilford Press; 2002. [Google Scholar]
- [42].Moore M, Tschannen-Moran B, Jackson E. Coaching Psychology Manual, Second Edition. Philadelphia, PA: Wolters Kluwer; 2016. [Google Scholar]
- [43].Anderson EJ, Axon DR, Taylor AM, Towers V, Warholak T, Johnson M, et al. Impact evaluation of a four-year academic-community partnership in provision of medication management and tertiary prevention services for rural patients with diabetes and/or hypertension. Prev Med Rep. 2020;17:101038. 10.1016/j.pmedr.2019.101038. [DOI] [PMC free article] [PubMed] [Google Scholar]


