Abstract
Background and Hypothesis
Previous studies have shown a robust relationship between childhood adversity and subsequent psychotic symptoms. However, the role of familial risk factors underlying this relationship remains largely unclear. Here, we tested whether offspring childhood adversity and postnatal maternal psychopathology mediated the relationship between maternal childhood adversity and offspring psychotic experiences.
Study Design
N = 3068 mother-offspring dyads were included. Maternal history of childhood adversity was retrospectively assessed using the Childhood Trauma Questionnaire during pregnancy. Maternal psychopathology was assessed during and after pregnancy. Twenty-four offspring childhood adversities were assessed by maternal interview when the child was 10 years old. Offspring psychotic experiences were examined using self-report at 14 years. Structural equation mediation models were conducted to explore whether maternal postnatal psychopathology and offspring childhood adversities sequentially mediated the relationship between maternal childhood adversity and offspring psychotic experiences. Analyses were adjusted for sociodemographic confounders.
Study Results
Maternal history of childhood adversity was associated with offspring childhood adversities (β = 0.12, 95% CI: 0.09 to 0.16). Offspring childhood adversity mediated the association of maternal childhood adversity with offspring hallucinations (βindirect effect = 0.008, 95% CI: 0.002 to 0.014, proportion mediated = 16.3%) and delusions (βindirect effect = 0.006, 95% CI: 0.000 to 0.012, proportion mediated = 13.1%).
Conclusions
Intergenerational transmission of childhood adversity can be considered of relevance in the etiology of psychosis vulnerability and can potentially serve as a modifiable risk factor.
Keywords: schizophrenia, maltreatment, mediation analysis, development, Generation R, child psychiatry
Introduction
A growing body of literature suggests that parental adverse childhood experiences can influence offspring development and future health. The concept of this intergenerational trauma postulates that exposure to adverse childhood experiences affects parents to such a degree that their offspring might also be afflicted by this familial post adversity state.1 Animal research has suggested that early life adversity can lead to behavioral changes in the offspring that can persist across several generations.2,3 Most research in humans so far has focused on maternal childhood adversity, and although the majority of mothers who have been exposed to childhood adversity do not pass on this risk to their children,4 research has highlighted that maternal exposure to childhood adversity can have negative effects on offspring mental health.5 Systematic reviews have suggested that maternal history of childhood adversity can lead to maladaptive parenting practices6,7 and mental health difficulties, which often persist after their child’s birth,5,8 and could, in turn, increase the risk of offspring exposure to adverse childhood experiences. However, few studies have explored whether intergenerational transmission of childhood adversity extends its risk on offspring mental health in early adolescence9,10—an important developmental window of risk—or have jointly modeled maternal psychopathology and offspring childhood adversities as potential mediating routes of intergenerational risk. As recently recommended in the review by Sideli et al., studies should focus on longitudinal prospective data with adequate assessments at different time points to establish temporal links between exposure, mediator, and outcome.11
Few studies have explored the role of intergenerational vulnerability to adversity in the context of psychosis spectrum symptoms. Childhood adversities have been identified as one of the most robust risk factors for psychosis,12,13 which is supported by many studies in the general population14–18 as well as clinical samples.19,20 This implies a continuity of risk for psychotic symptoms on a spectrum of severity ranging from common subclinical hallucinations and delusions to clinical—less prevalent—psychotic disorders.21,22 Youth with psychotic experiences are at increased risk for poorer long-term outcomes, including psychotic and nonpsychotic mental disorders, reduced quality of life, and suicidal behavior,23–26 warranting more research into modifiable risk factors for psychotic experiences. Although previous work has identified childhood adversity as a robust (and potentially modifiable) risk for psychotic experiences in youth,17 the role of familial risk factors in this relationship is still unclear. More specifically, although other studies have explored the relationship between intergenerational transmission of childhood adversity with the development of internalizing and externalizing problems, it remains unresolved whether intergenerational transmission of childhood adversity precedes the development of psychotic experiences in young people.
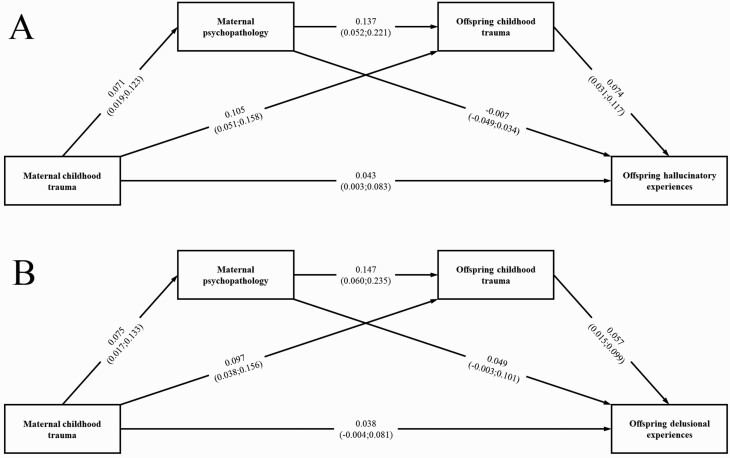
Using data from a large prospective population-based cohort, this long-term follow-up study investigated the potential intergenerational transmission of childhood adversity between mothers and offspring in association with offspring psychotic experiences in adolescence. This study starting in utero with follow-up in adolescence utilized comprehensive structural equation models with sequential mediation analysis, modeling direct and indirect paths between maternal childhood adversity, maternal postnatal psychopathology, offspring childhood adversity, and offspring psychotic experiences, while adjusting for relevant sociodemographic and clinical confounders. Whereas many studies on psychotic experiences focused on hallucinations only, the current study had data on both hallucinatory and delusional experiences available. We hypothesized that maternal childhood adversity would be associated with more postnatal maternal psychopathology, which would then be associated with greater exposure to offspring childhood adversity and this would subsequently relate to more offspring psychotic experiences. Postnatal maternal psychopathology and offspring childhood adversities were each treated as mediators, both separately and in a sequential manner (figure 1).
Fig. 1.
Structural equation mediation model of associations of maternal childhood adversity with offspring hallucinatory (A) and delusional (B) experiences, mediated through maternal postnatal psychopathology and offspring childhood adversity. Path coefficients are standardized and presented with 95% confidence intervals. Paths were adjusted for sociodemographic covariates and maternal prenatal psychopathology. Fit indices for hallucinations model: CFI = 0.997, TLI = 0.985, RMSEA = 0.017. Fit indices for delusions model: CFI = 0.996, TLI = 0.981, RMSEA = 0.017. Please note that maternal postnatal psychopathology and offspring childhood adversities were each treated as individual mediators as well as sequential mediators as demonstrated by the paths above. CFI, comparative fit index; RMSEA, root mean square error of approximation; TLI, Tucker–Lewis index.
Methods
Population
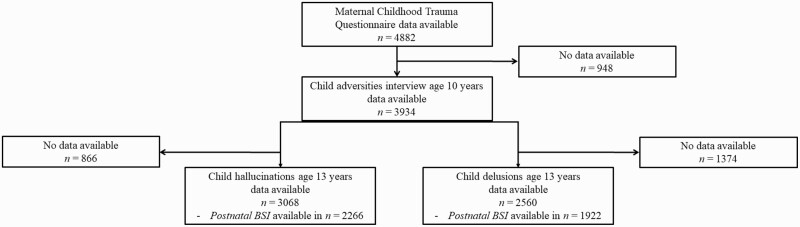
This study was embedded in the Generation R Study, a prospective population-based birth cohort study from Rotterdam, the Netherlands. The Generation R Study follows participants from fetal life towards adulthood, and more detailed information can be found elsewhere.27 This study was approved by the Medical Ethical Committee of the Erasmus Medical Center Rotterdam and written informed consent and assent were obtained from parents and children, respectively. Two separate—but overlapping—final samples were used that were different in size because the questionnaire assessing delusions was sent after the questionnaire assessing hallucinations, this led to a higher non-response (see figure 2 for a flowchart). While n = 3068 participants had complete data on child-reported hallucinatory experiences, n = 2560 participants had complete data on child-reported delusional experiences. Loss to follow-up analyses are presented in the Supplement.
Fig. 2.
Flowchart.
Measures
Exposure
Maternal Childhood Adversity
During pregnancy, frequency and severity of traumatic experiences of mothers during their childhood were measured with the 34-item short version of the Childhood Trauma Questionnaire (CTQ) collected at 20 weeks gestation.28 The scale comprised 5 subscales, ie, physical abuse, sexual abuse, emotional abuse, physical neglect, and emotional neglect. The CTQ is a validated self-report questionnaire which is widely used in retrospective studies of childhood maltreatment. Mothers rated CTQ items on a 5-point Likert-type scale to indicate the extent to which each item was true for them before age 18 years. The CTQ has demonstrated good test–retest reliability.28,29 In the current study, the weighted total score was calculated if missingness did not exceed 25%. The internal consistency for the CTQ total score was α = 0.92 in this sample. The items and their endorsement in this sample are shown in Supplementary table S1.
Outcomes
Child Psychotic Experiences
Hallucinations
Hallucinatory experiences were examined using the Youth Self-Report when children were 14 years of age. This questionnaire consisted of 2 items: (1) I hear sounds or voices that according to other people are not there, (2) I see things that other people think are not there, which were selected on appropriateness for capturing hallucinatory experiences.15,30 These items were rated on a 3-point Likert scale, namely (0) not at all, (1) a bit or sometimes, and (2) clearly or often. Because of skewness and few items, this sum score was dichotomized into absent (score = 0; n = 2670, 87.0%) and present (score > 0, coded 1; n = 398, 13.0%).
Delusions
At age 14 years, delusions were assessed using self-reported questionnaire items derived from the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS31,32;). Six items were used to evaluate 6 different types of delusional experiences: (1) Have other people ever read your thoughts? (2) Have you ever believed that you were being sent special messages through television or radio? (3) Have you ever thought you were being followed or spied on? (4) Have you ever felt as though your body had been changed in some way that you could not understand? (5) Does somebody have the power to control your mind or body (like a robot)? (6) Have you ever believed you are an important person or have special gifts other people do not have? These 6 items were adapted for self-report and resemble similarly worded questions from other studies.33 Moreover, these questions have previously been used in another ethnically diverse cohort from the Netherlands.32 Children responded on a 3-point scale to what extent they agreed with an item: No (0), Yes, probably (1), and Yes, certainly (2). A sum score of the 6 delusion items was calculated and treated continuously in our analyses.
Potential Mediators
Offspring Childhood Adversities
When children were on average 10 years, primary caregivers (mothers in 96% of cases) were asked by a trained interviewer whether their child had experienced any of 24 potential childhood adversities, eg, parental divorce/separation, death of a loved one, and physical or sexual maltreatment.34 In case of an endorsed event, the child’s age at the adverse event was registered. Also, mothers were asked whether the distress caused by each event was “none,” “a little,” “moderate,” or “a lot.” Only events with at least “moderate” or “a lot” of impact were coded as adversities in the present analyses. These were then summed to generate a continuous score, with higher scores indicating having been exposed to a higher number of adversities. Prevalence of each childhood adversity is reported in Supplementary table S2.
Maternal Psychopathology
Continuous scores of maternal psychopathology were collected prenatally (at 20 weeks gestation) as well as at 2 months postnatally with the Brief Symptom Inventory (BSI),35 a validated self-reported continuous measure of 53 items encompassing a spectrum of psychiatric symptoms. The BSI encompasses several syndrome scales, including somatization, obsession-compulsion, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. Both prenatal and postnatal BSI scores were available in smaller subsamples and missing data were imputed using full information maximum likelihood (ML) estimation. Postnatal BSI scores were treated as a mediator in the structural equation models. In sensitivity analyses, prenatal BSI scores were treated as a covariate to adjust for earlier maternal mental health problems and to account for potential recall bias as the CTQ was administered concomitantly.
Covariates
The following covariates that have previously been associated with psychotic experiences, were taken into consideration in the current analyses.21 Child age and sex were obtained from medical records. Maternal age at intake and marital status were obtained from self-reported questionnaires. National heritage of the child and mother were considered as European-descent when both parents were born in Europe, while participants were classified as non-European if at least one of the parents was born outside Europe. Maternal education was assessed through a self-reported questionnaire during pregnancy and defined by the highest attained educational level and classified into low/medium (primary school or lower or lower/intermediate vocational training) or high (higher vocational education and university).
Statistical Analyses
Correlations were calculated between study variables. First, regression analyses were conducted to examine the individual associations between study variables of interest. These analyses were adjusted for covariates (including maternal prenatal psychopathology), which were imputed for missingness using multiple imputation with the mice package in R.36 Logistic regression was performed when offspring hallucinatory experiences (dichotomous) were the outcome. Linear regression was performed in all other association analyses, in which case variables were square root transformed to approximate a normality of the distribution and z-transformed to provide standardized regression estimates.
Next, mediation analyses were conducted (figure 1). In a single model, we tested the independent mediating effects of offspring childhood adversity and maternal psychopathology, as well as the hypothesized combined (ie, serial/sequential) pathway in which maternal childhood trauma would relate to postnatal psychopathology, which would in turn be associated with offspring childhood adversities, and subsequently relate to offspring psychotic experiences. Analyses were performed using the lavaan structural equation modeling package in R software.37 In one comprehensive serial mediation model, individual regression paths were modeled for the following associations: (1) between exposure (maternal childhood adversity) and outcome (child psychotic experiences, the c path); (2) between exposure and the 2 mediators (maternal postnatal psychopathology and offspring childhood adversity) as well as between the 2 mediators (ie, the a paths); and (3) between the mediators and the outcome, controlling for exposure (ie, the b path). The indirect effect was calculated as the product of the a and b paths and this indirect effect was subtracted from the total effect (ie, the c path) to calculate the direct effect (ie, the cʹ path). The proportion mediated was calculated by dividing the indirect effect by the total effect.
Analyses were performed separately for the 2 outcomes child-reported hallucinations (N = 3068) and child-reported delusion (N = 2560). P-values were bootstrapped 5000 times and exogenous categorical covariates were dummy-coded and missingness was dealt with using full information ML in the lavaan.37 As described above, offspring hallucinatory experiences were coded as present/absent (ie, 0/1) and delusional experiences were treated continuously in these models. Sensitivity analyses were done with hallucinations coded on a scale from 0 to 4, which was treated as a continuous variable in the ML estimator, and with hallucinations coded on a scale of 0–1–2, which was treated as an ordinal variable in the weighted least squares with robust standard errors, and a mean- and variance-adjusted test statistic (WLSMV) estimator. The latter could only be used for complete data,38 hence, this model was only run on data unadjusted for covariates. All other analyses were adjusted for sociodemographic covariates and maternal prenatal psychopathology. We adjusted for maternal prenatal psychopathology to minimize possible reporter bias in relation to maternal childhood trauma and to specifically parse out temporal effects considering the high stability between pre and postnatal psychopathology scores (Supplementary table S3). In a sensitivity step, we adjusted for prenatal maternal psychopathology to parse out temporal effects considering the high stability between pre and postnatal psychopathology scores (Supplementary table S3) and to account for possible recall bias as the CTQ was administered concomitantly.
Results
Descriptive Analyses
Descriptive characteristics are presented in table 1. In this sample, 24.2% and 5.2% of the offspring were exposed to 1–2 and >2 adversities, respectively. Descriptive characteristics were similar in the dataset using data on delusional experiences (Supplementary table S2). Correlations between study variables are shown in supplementary table S3, demonstrating small to moderate correlations between variables.
Table 1.
Descriptive Characteristics of the Study Population Using Data on Offspring Hallucinations (n = 3068)
| N | Statistic | |
|---|---|---|
| Child characteristics | ||
| Gender (% girls) | 3068 (0.0% missing) | 52.7% |
| Age at follow-up in years, mean (SD) | 3068 (0.0% missing) | 13.58 (0.40) |
| Ethnicity | 3067 (0.0% missing) | |
| European % | 2380 | 77.6% |
| Non-European % | 687 | 22.4% |
| Hallucinations | 3068 (0.0% missing) | |
| Absent | 2670 | 87.0% |
| Present | 398 | 13.0% |
| Delusions sum score, median (IQR; range) | 2475 (19.3% missing) | 6.00 (1.00; 6–16) |
| Childhood adversities, median (IQR; range) | 3068 (0.0% missing) | 0.00 (1.00; 0–12) |
| Zero life events | 2170 | 70.7% |
| One or two life event(s) | 743 | 24.2% |
| Three or more life events | 159 | 5.2% |
| Maternal characteristics | ||
| Age at intake in years, mean (SD) | 3068 (0.0% missing) | 31.41 (4.43) |
| Ethnicity | 3067 (0.0% missing) | |
| Western | 2316 | 75.5% |
| Non-Western | 751 | 24.5% |
| Educational level | 3009 (1.8% missing) | |
| Low/medium | 1249 | 41.5% |
| High | 1760 | 58.5% |
| Marital status | 2987 (2.6% missing) | |
| Married or partnered | 2733 | 91.5% |
| No partner | 254 | 8.5% |
| Prenatal psychopathology, median (IQR; range) | 3008 (2.0% missing) | 0.13 (0.23; 0.00–3.06) |
| Postnatal psychopathology, median (IQR; range) | 2266 (35.4% missing) | 0.12 (0.21; 0.00–3.19) |
| Childhood adversities weighted score, median (IQR; range) | 3068 (0% missing) | 6.23 (1.73; 5.00–21.10) |
Note: IQR, interquartile range; SD, standard deviation.
Regression Analyses
Both maternal and offspring childhood adversity were significantly associated with more offspring hallucinatory experiences (table 2; odds ratio [OR] = 1.41, 95% CI: 1.04 to 1.90 and OR = 1.34, 95% CI: 1.14 to 1.57, respectively) and delusional experiences (β = 0.04, 95% CI: 0.00 to 0.08 and β = 0.06, 95% CI: 0.02 to 0.10, respectively). Maternal childhood adversity was associated with higher scores of maternal postnatal psychopathology (β = 0.12, 95% CI: 0.09 to 0.16) and offspring childhood adversity (β = 0.12, 95% CI: 0.09 to 0.16), and maternal postnatal psychopathology was also associated with more offspring childhood adversity (β = 0.14, 95% CI: 0.08 to 0.20). Conversely, maternal postnatal psychopathology was not associated with either offspring hallucinatory or delusional experiences (OR = 0.93, 95% CI: 0.51 to 1.64 and β = 0.04, 95% CI: −0.02 to 0.09, respectively).
Table 2.
Individual Association Analyses Between Maternal Childhood Adversities, Maternal Psychopathology, Offspring Childhood Adversities, and Offspring Psychotic Experiences (N = 3068)
| Exposure | Outcome | |
|---|---|---|
| Offspring hallucinatory experiences | ||
| OR (95% CI) | P | |
| Maternal childhood adversities | 1.41 (1.04 to 1.90) | .026 |
| Maternal postnatal psychopathology | 0.93 (0.52 to 1.64) | .793 |
| Offspring childhood adversities | 1.34 (1.14 to 1.57) | <.001 |
| Offspring delusional experiencesa | ||
| β (95% CI) | P | |
| Maternal childhood adversities | 0.04 (0.00 to 0.08) | .047 |
| Maternal postnatal psychopathology | 0.04 (−0.02 to 0.09) | .202 |
| Offspring childhood adversities | 0.06 (0.02 to 0.10) | .005 |
| Offspring childhood adversities | ||
| β (95% CI) | P | |
| Maternal childhood adversities | 0.12 (0.09 to 0.16) | <.001 |
| Maternal postnatal psychopathology | 0.14 (0.08 to 0.20) | <.001 |
| Maternal postnatal psychopathology | ||
| β (95% CI) | P | |
| Maternal childhood adversities | 0.12 (0.09 to 0.16) | <.001 |
Note: CI, confidence interval; OR, odds ratio.
Note: All analyses are adjusted for maternal age at intake, maternal educational level, marital status, maternal prenatal psychopathology, child age, child sex, and child ethnicity.
aAnalyses were performed in the sample of n = 2560.
Mediation Analyses
Hallucinatory Experiences
Figure 1A shows the mediation path analysis of the association between maternal childhood adversity and offspring hallucinatory experiences, mediated through maternal postnatal psychopathology and offspring childhood adversity. Model fit indices indicated excellent fit. In this model, the main effect was significant (β = 0.044, 95% CI: 0.004 to 0.084) and there was a direct effect of maternal childhood adversity on offspring hallucinations (β = 0.043, 95% CI: 0.003 to 0.083). The indirect path through maternal postnatal psychopathology was not significant (β = −0.001, 95% CI: −0.003 to 0.002, P = .727), but the indirect path through offspring childhood adversity was statistically significant (β = 0.008, 95% CI: 0.002 to 0.014, proportion mediated = 15.3%). The serial-mediation path from maternal childhood adversity to offspring hallucinations through both maternal postnatal psychopathology and offspring childhood adversity was significant (β = 0.003, 95% CI: 0.001 to 0.005, P = .013, proportion mediated = 6.7%).
Sensitivity analyses with alternative categorisations of offspring hallucinatory experiences yielded very comparable results with the same significant results of similar effect estimates (Supplementary figures S1 and S2).
Delusional Experiences
Figure 1B shows the mediation path analysis of the association between maternal childhood adversity and offspring delusional experiences, mediated through maternal postnatal psychopathology and offspring childhood adversity. Model fit indices indicated excellent fit. In contrast to the findings regarding hallucinations, in this model the main effect was not significant (β = 0.039, 95% CI −0.004 to 0.082, P = .073) and there was no significant direct effect of maternal childhood adversity on offspring delusions (β = 0.038, 95% CI: −0.004 to 0.081, P = .079). An indirect path through maternal postnatal psychopathology was not significant (β = 0.004, 95% CI: −0.001 to 0.009, P = .138), but the indirect path through offspring childhood adversity was statistically significant (β = 0.005, 95% CI 0.000;0.011, proportion mediated = 12.5%). The indirect path from maternal childhood adversity to offspring delusions through both maternal postnatal psychopathology and offspring childhood adversity was significant (β = 0.003, 95% CI: 0.000 to 0.005, P = .025, proportion mediated = 6.6%).
Sensitivity Analyses
With additional adjustment for prenatal maternal psychopathology, there was no sequential mediation path through both maternal postnatal psychopathology and offspring childhood adversity to hallucinations (β = 0.001, 95% CI: 0.000 to 0.002, P = .099) or delusions (β = 0.001, 95% CI: 0.000 to 0.001, P = .106) (Supplementary figure S3). All other paths were identical to what was found in the main analyses.
Discussion
Based on prospective data in a sample of over 2500 dyads spanning pregnancy to early adolescence, we found that maternal history of childhood adversity is associated with more psychotic experiences in their children through intergenerational transmission of adverse childhood experiences. We highlight several key findings. First, regression analyses demonstrated that maternal childhood adversity was associated with more maternal psychopathology, offspring childhood adversities, and offspring psychotic experiences. Second, offspring childhood adversity mediated the relationship between maternal childhood adversity and offspring psychotic experiences independent of sociodemographic confounders and prenatal assessments of maternal psychopathology. Third, maternal history of childhood adversity was associated with more maternal psychopathology, through which there was a greater likelihood of the offspring to be exposed to childhood adversities, and this was ultimately associated with a higher endorsement of psychotic experiences. This serial mediation disappeared when adjusted for prenatal maternal psychopathology. Together, the current findings contribute to our understanding of the intergenerational risk factors influencing psychotic experiences in adolescence, and could be used as a framework for further exploration of causal mechanisms and refinement of diagnostic formulations.
Previous research has found an association of maternal history of childhood trauma with past and s adversities in their children.1,4,39 Meta-analyses and systematic reviews also suggested that maternal childhood adversity can have negative consequences, including a wide range of mental health problems5,8 and poorer parenting practices.6,7 Earlier reports found an association between maternal childhood trauma and offspring psychopathology, such as autism, internalizing and externalizing symptoms,9,10,40–43 and our study extends these findings to psychosis spectrum symptoms. Previous studies found that maternal psychopathology mediated the relationship between maternal childhood adversity and offspring psychopathology,40 which we also observed in this study. Importantly, this mediation through maternal postnatal psychopathology became non-significant when adjusted for prenatal assessments of maternal psychopathology, suggesting that the continuity of maternal psychopathology is important to account for in intergenerational patterns of mental health.
Findings from the current study extend a vast body of literature highlighting the important role for adverse childhood experiences in the etiology of psychosis spectrum symptoms. Adolescent psychotic experiences have previously been associated with a variety of familial characteristics, such as parental history of mental illness and substance use,44,45 parental separation,46 insecure parent-child attachment,11 and family ethnic minority or migrant status.47,48 Our study as well as other publications underscore the importance of the family environment in shaping psychosis vulnerability, which could partly be explained through intergenerational vulnerabilities to exposure to adverse life events.
There is a variety of processes potentially underlying the intergenerational vulnerability to childhood adversity. For example, attachment and learning theories posit that intergenerational transmission could occur through imitation of others by observation or through the passing on of dysfunctional mental representations of relationships (ie, how individuals evaluate others) from one maltreated generation to the next.49 Mothers with a history of trauma may be less sensitive to their offspring’s needs, which could compromise the development of secure attachment, contributing to the intergenerational transmission of childhood adversity.50,51 Psychopathology could influence the relationship between exposure to trauma and subsequent dysfunctional mental representations and behavioral learning strategies.6,7 While maternal psychopathology is a likely mechanism between maternal and offspring adversity, we found that postnatal maternal psychopathology did not mediate the relationship between maternal childhood adversity and offspring psychotic experiences independent of prenatal psychopathology. This can be explained by the high stability between prenatal and postnatal assessments, suggesting that repeated assessments of maternal psychopathology are needed when studying intergenerational vulnerability. Another explanation could be that preconception trauma in parents or offspring’s early environmental exposures may result in epigenetic changes in the offspring that might, in turn, increase their psychopathology risk.1
Alternatively, these associations might be explained through common causes, such as shared genetic liabilities. Previously, we demonstrated in the same cohort that the molecular genetic heritability of childhood adversity was estimated around 23%,52 which is in line with earlier reviews of the twin heritability literature53,54 and recent molecular genetic studies.55,56 Furthermore, previous work from other groups as well as our own has demonstrated that the genetic vulnerability to schizophrenia increases the risk for exposure to childhood adverse experiences.52,57 This most likely reflects a gene-environment correlation,56,58 ie, childhood adversities arise from heritable vulnerabilities that parents transmit to the next generation. Such gene-environment correlations can be conceptualized in different ways. For example, parental genetic vulnerability may negatively affect the social environment of the offspring (ie, passive gene-environment correlation), whereas the offspring’s genotype may also negatively affect their own behavior (ie, active or reactive gene-environment correlation), both contributing to a higher likelihood of exposure to childhood adversity.56,59 Taken together, shared genetic liabilities could potentially explain the intergenerational relationship between maternal and offspring childhood adversity and subsequent psychosis experiences. Prospective genetically informed designs with repeated assessments of adversity and mental health across development, and including genetic data of both parents and offspring, are needed to improve our understanding of causality in these associations.60 In addition, this might inform researchers and clinicians on particular windows of developmental risk, eg, puberty or transition from primary to secondary education. Besides shared genetic liabilities, there may be unknown or unmeasured environmental confounders that could explain the associations observed in the current study. While we adjusted for a range of potential confounders, there may be other (unmeasured) socio-environmental factors that might have not been fully captured in our analyses. Because these heritable and environmental confounds potentially explain the link between maternal and offspring exposure to childhood adversity, our findings should be interpreted as providing evidence for an intergenerational vulnerability to adversity rather than intergenerational transmission of adversity.
Our findings might have several clinical implications, although it should be noted that estimates were relatively small precluding any causal inference. This notwithstanding, our findings might generate novel hypotheses for future clinical studies. First, diagnostic screening of a history of childhood adversity in pregnant women for identification of vulnerable groups may benefit (future) parents and their offspring. This could result in more comprehensive diagnostic evaluations, although this needs to be examined in help-seeking populations. Studies on screening of parental childhood trauma and identification of resilience factors, including academic achievement, social support, and strong peer relationships, against the development of offspring psychotic experiences in vulnerable families are needed to shed more light on this complex matter.61 However, the effects of such screenings should first be investigated using controlled trials.
The strengths of the current study include the large population-based sample, adjustment for relevant sociodemographic and clinical confounders, and prospective data on childhood adversity and psychotic experiences that allowed mediation analyses. In addition, we also included data on both hallucinatory and delusional experiences. However, there are several limitations. First, maternal childhood trauma was retrospectively measured during pregnancy and may be subject to recall bias,62 and we did not include paternal report. Future studies should focus on both maternal and paternal routes of intergenerational risk transmission. Second, childhood psychotic experiences were self-reported, which may be subject to reporting bias. Nevertheless, it has been demonstrated that assessment of psychotic experiences using self-reported inventories in 11–13-year-olds has a substantial positive predictive value for clinician-confirmed symptoms,63 which is stronger for hallucinatory compared to delusional experiences, and this is relevant when extrapolating our findings to clinical contexts. However, in population-based settings, self-report assessments of psychotic experiences have been shown to be valid and reliable for this age group.64 Third, the attrition analyses showed that mother-child dyads lost to follow-up comprised mothers with higher CTQ total scores and were of more disadvantaged socioeconomic backgrounds. This selection may have led to an underestimation of our findings. Fourth, offspring childhood adversities were mother-reported due to the child’s young age, which could have resulted in misclassification of adversities unknown to the mother and could have increased shared-rater variance as maternal psychopathology and offspring adversities were also mother-reported.
In conclusion, we observed that maternal history of childhood adversity was associated with offspring hallucinatory and delusional experiences, which was partially mediated through offspring’s exposure to childhood adversity. Attenuation of these findings following adjustment for preexisting maternal mental health problems suggests that other mechanisms—eg, shared genetic risk, parenting—explain these intergenerational links between childhood adversity and psychotic experiences. These findings provide support for an intergenerational vulnerability to adverse childhood experiences in the etiology of psychosis susceptibility and potentially could give rise to novel hypotheses for future studies to elucidate the developmental pathways and possible windows of risk for developing psychotic experiences.
Supplementary Material
Supplementary material is available at https://academic.oup.com/schizophreniabulletin/.
Acknowledgments
The authors gratefully acknowledge the contribution of all children and parents, general practitioners, hospitals, midwives, and pharmacies involved in the Generation R Study. The Generation R Study is conducted by the Erasmus Medical Centre (Rotterdam) in close collaboration with the School of Law and Faculty of Social Sciences of the Erasmus University Rotterdam; the Municipal Health Service Rotterdam area, Rotterdam; the Rotterdam Homecare Foundation, Rotterdam; and the Stichting Trombosedienst & Artsenlaboratorium Rijnmond, Rotterdam. We are grateful to Sandjana Parag, MSc for her valuable contribution to this manuscript.
Contributor Information
Koen Bolhuis, Department of Child and Adolescent Psychiatry/Psychology, Erasmus Medical Center – Sophia Children’s Hospital, Rotterdam, The Netherlands.
Lisa R Steenkamp, Department of Child and Adolescent Psychiatry/Psychology, Erasmus Medical Center – Sophia Children’s Hospital, Rotterdam, The Netherlands.
Henning Tiemeier, Department of Child and Adolescent Psychiatry/Psychology, Erasmus Medical Center – Sophia Children’s Hospital, Rotterdam, The Netherlands; Department of Social and Behavioral Science, Harvard TH Chan School of Public Health, Boston, USA.
Laura Blanken, Department of Child and Adolescent Psychiatry/Psychology, Erasmus Medical Center – Sophia Children’s Hospital, Rotterdam, The Netherlands; Department of Psychiatry, Amsterdam UMC – location AMC, Amsterdam, The Netherlands.
Jean-Baptiste Pingault, Clinical, Educational and Health Psychology, Division of Psychology and Language Sciences, Faculty of Brain Sciences, University College London, London, UK.
Charlotte A M Cecil, Department of Child and Adolescent Psychiatry/Psychology, Erasmus Medical Center – Sophia Children’s Hospital, Rotterdam, The Netherlands; Department of Epidemiology, Erasmus Medical Center, Rotterdam, the Netherlands.
Hanan El Marroun, Department of Child and Adolescent Psychiatry/Psychology, Erasmus Medical Center – Sophia Children’s Hospital, Rotterdam, The Netherlands; Department of Pediatrics, Erasmus Medical Center – Sophia Children’s Hospital, Rotterdam, The Netherlands; Department of Psychology, Education and Child Studies, Erasmus School of Social and Behavioral Sciences, Erasmus University Rotterdam, Rotterdam, The Netherlands.
Funding
This work was supported by the Erasmus MC (Mrace 2016 107569 to LRS, HT, HEM, LB, and KB); the Netherlands Organisation for Scientific Research (NWO-grant 016.VICI.170.200 to HT); the Sophia Children’s Hospital Research Foundation (research fellowship grant 921 to KB); the European Union’s Horizon 2020 Research and Innovation Programme (grant agreement No 848158 [EarlyCause] to CAMC); Stichting Volksbond Rotterdam (to HEM); the Brain & Behavior Research Foundation (NARSAD Young Investigator Grant 27853 to HEM); the Netherlands Organization for Health Research and Development (Aspasia grant No. 015.016.056 to HEM), and the European Union’s Horizon 2020 Research and Innovation Program (grant agreement 733206 to HEM). The Generation R Study received financial support from the Erasmus MC; Erasmus University Rotterdam; The Netherlands Organisation for Health Research and Development (ZonMw).
Conflict of Interest
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Yehuda R, Lehrner A.. Intergenerational transmission of trauma effects: putative role of epigenetic mechanisms. World Psychiatry. 2018;17(3):243–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bohacek J, Mansuy IM.. Molecular insights into transgenerational non-genetic inheritance of acquired behaviours. Nat Rev Genet. 2015;16(11):641–652. [DOI] [PubMed] [Google Scholar]
- 3. Franklin TB, Russig H, Weiss IC, et al. Epigenetic transmission of the impact of early stress across generations. Biol Psychiatry. 2010;68(5):408–415. [DOI] [PubMed] [Google Scholar]
- 4. Thornberry TP, Knight KE, Lovegrove PJ.. Does maltreatment beget maltreatment? A systematic review of the intergenerational literature. Trauma Violence Abuse. 2012;13(3):135–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Su Y, D’Arcy C, Meng X.. Intergenerational effect of maternal childhood maltreatment on next generation’s vulnerability to psychopathology: a systematic review with meta-analysis. Trauma Violence Abuse. 2022;23(1):152–162. [DOI] [PubMed] [Google Scholar]
- 6. Greene CA, Haisley L, Wallace C, Ford JD.. Intergenerational effects of childhood maltreatment: a systematic review of the parenting practices of adult survivors of childhood abuse, neglect, and violence. Clin Psychol Rev. 2020;80:101891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lotto CR, Altafim ERP, Linhares MBM.. Maternal history of childhood adversities and later negative parenting: a systematic review [published online ahead of print August 3, 2021]. Trauma Violence Abuse. doi: 10.1177/15248380211036076. [DOI] [PubMed] [Google Scholar]
- 8. Narayan AJ, Lieberman AF, Masten AS.. Intergenerational transmission and prevention of adverse childhood experiences (ACEs). Clin Psychol Rev. 2021;85:101997. [DOI] [PubMed] [Google Scholar]
- 9. Collishaw S, Dunn J, O’Connor TG, Golding J, Avon Longitudinal Study of P, Children Study T. Maternal childhood abuse and offspring adjustment over time. Dev Psychopathol. 2007;19(2):367–383. [DOI] [PubMed] [Google Scholar]
- 10. Rijlaarsdam J, Stevens GW, Jansen PW, et al. Maternal childhood maltreatment and offspring emotional and behavioral problems: maternal and paternal mechanisms of risk transmission. Child Maltreat. 2014;19(2):67–78. [DOI] [PubMed] [Google Scholar]
- 11. Sideli L, Murray RM, Schimmenti A, et al. Childhood adversity and psychosis: a systematic review of bio-psycho-social mediators and moderators. Psychol Med. 2020;50(11):1761–1782. [DOI] [PubMed] [Google Scholar]
- 12. Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38(4):661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Arango C, Dragioti E, Solmi M, et al. Risk and protective factors for mental disorders beyond genetics: an evidence-based atlas. World Psychiatry. 2021;20(3):417–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fisher HL, Schreier A, Zammit S, et al. Pathways between childhood victimization and psychosis-like symptoms in the ALSPAC birth cohort. Schizophr Bull. 2013;39(5):1045–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bolhuis K, Koopman-Verhoeff ME, Blanken LME, et al. Psychotic-like experiences in pre-adolescence: what precedes the antecedent symptoms of severe mental illness? Acta Psychiatr Scand. 2018;138(1):15–25. [DOI] [PubMed] [Google Scholar]
- 16. Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A.. Childhood trauma and children’s emerging psychotic symptoms: a genetically sensitive longitudinal cohort study. Am J Psychiatry. 2011;168(1):65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kelleher I, Keeley H, Corcoran P, et al. Childhood trauma and psychosis in a prospective cohort study: cause, effect, and directionality. Am J Psychiatry. 2013;170(7):734–741. [DOI] [PubMed] [Google Scholar]
- 18. Croft J, Heron J, Teufel C, et al. Association of trauma type, age of exposure, and frequency in childhood and adolescence with psychotic experiences in early adulthood. JAMA Psychiatry. 2019;76(1):79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Trotta A, Murray RM, Fisher HL.. The impact of childhood adversity on the persistence of psychotic symptoms: a systematic review and meta-analysis. Psychol Med. 2015;45(12):2481–2498. [DOI] [PubMed] [Google Scholar]
- 20. Morgan C, Gayer-Anderson C.. Childhood adversities and psychosis: evidence, challenges, implications. World Psychiatry. 2016;15(2):93–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Linscott RJ, van Os J.. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. 2013;43(6):1133–1149. [DOI] [PubMed] [Google Scholar]
- 22. Kelleher I, Connor D, Clarke MC, Devlin N, Harley M, Cannon M.. Prevalence of psychotic symptoms in childhood and adolescence: a systematic review and meta-analysis of population-based studies. Psychol Med. 2012;42(9):1857–1863. [DOI] [PubMed] [Google Scholar]
- 23. Healy C, Brannigan R, Dooley N, et al. Childhood and adolescent psychotic experiences and risk of mental disorder: a systematic review and meta-analysis. Psychol Med. 2019;49(10):1589–1599. [DOI] [PubMed] [Google Scholar]
- 24. Rimvall MK, van Os J, Verhulst F, et al. Mental health service use and psychopharmacological treatment following psychotic experiences in preadolescence. Am J Psychiatry. 2020;177(4):318–326. [DOI] [PubMed] [Google Scholar]
- 25. Trotta A, Arseneault L, Caspi A, et al. Mental health and functional outcomes in young adulthood of children with psychotic symptoms: a longitudinal cohort study. Schizophr Bull. 2020;46(2):261–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yates K, Lang U, Cederlof M, et al. Association of psychotic experiences with subsequent risk of suicidal ideation, suicide attempts, and suicide deaths: a systematic review and meta-analysis of longitudinal population studies. JAMA Psychiatry. 2019;76(2):180–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kooijman MN, Kruithof CJ, van Duijn CM, et al. The generation R study: design and cohort update 2017. Eur J Epidemiol. 2016;31(12):1243–1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bernstein DP, Fink L, Handelsman L, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151(8):1132–1136. [DOI] [PubMed] [Google Scholar]
- 29. Bernstein DP, Ahluvalia T, Pogge D, Handelsman L.. Validity of the childhood trauma questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry. 1997;36(3):340–348. [DOI] [PubMed] [Google Scholar]
- 30. Koopman-Verhoeff ME, Bolhuis K, Cecil CAM, et al. During day and night: childhood psychotic experiences and objective and subjective sleep problems. Schizophr Res. 2019;206:127–134. [DOI] [PubMed] [Google Scholar]
- 31. Kaufman J, Birmaher B, Brent D, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. [DOI] [PubMed] [Google Scholar]
- 32. Adriaanse M, van Domburgh L, Hoek HW, Susser E, Doreleijers TA, Veling W.. Prevalence, impact and cultural context of psychotic experiences among ethnic minority youth. Psychol Med. 2015;45(3):637–646. [DOI] [PubMed] [Google Scholar]
- 33. Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H.. Children’s self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Arch Gen Psychiatry. 2000;57(11):1053–1058. [DOI] [PubMed] [Google Scholar]
- 34. Amone-P’Olak K, Ormel J, Huisman M, Verhulst FC, Oldehinkel AJ, Burger H.. Life stressors as mediators of the relation between socioeconomic position and mental health problems in early adolescence: the TRAILS study. J Am Acad Child Adolesc Psychiatry. 2009;48(10):1031–1038. [DOI] [PubMed] [Google Scholar]
- 35. Derogatis LR, Melisaratos N.. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13(3):595–605. [PubMed] [Google Scholar]
- 36. van Buuren S, Groothuis-Oudshoorn K.. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1–67. [Google Scholar]
- 37. Rosseel Y. lavaan: an R package for structural equation modeling. J Stat Softw. 2012;48(2):1–36. [Google Scholar]
- 38. Rosseel Y. lavaan latent variable analysis: categorical data. https://lavaan.ugent.be/tutorial/cat.html. Accessed December 28, 2021.
- 39. Randell KA, O’Malley D, Dowd MD.. Association of parental adverse childhood experiences and current child adversity. JAMA Pediatr. 2015;169(8):786–787. [DOI] [PubMed] [Google Scholar]
- 40. Plant DT, Jones FW, Pariante CM, Pawlby S.. Association between maternal childhood trauma and offspring childhood psychopathology: mediation analysis from the ALSPAC cohort. Br J Psychiatry.. 2017;211(3):144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Roberts AL, Lyall K, Rich-Edwards JW, Ascherio A, Weisskopf MG.. Association of maternal exposure to childhood abuse with elevated risk for autism in offspring. JAMA Psychiatry. 2013;70(5):508–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Jovanovic T, Smith A, Kamkwalala A, et al. Physiological markers of anxiety are increased in children of abused mothers. J Child Psychol Psychiatry. 2011;52(8):844–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Schickedanz A, Halfon N, Sastry N, Chung PJ.. Parents’ adverse childhood experiences and their children’s behavioral health problems. Pediatrics. 2018;142(2):e20180023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Jeppesen P, Larsen JT, Clemmensen L, et al. The CCC2000 birth cohort study of register-based family history of mental disorders and psychotic experiences in offspring. Schizophr Bull. 2015;41(5):1084–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bolhuis K, Kushner SA, Yalniz S, et al. Maternal and paternal cannabis use during pregnancy and the risk of psychotic-like experiences in the offspring. Schizophr Res. 2018;202:322–327. [DOI] [PubMed] [Google Scholar]
- 46. Ayerbe L, Perez-Pinar M, Foguet-Boreu Q, Ayis S.. Psychosis in children of separated parents: a systematic review and meta-analysis. Eur Psychiatry. 2020;63(1):e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Leaune E, Dealberto MJ, Luck D, et al. Ethnic minority position and migrant status as risk factors for psychotic symptoms in the general population: a meta-analysis. Psychol Med. 2019;49(4):545–558. [DOI] [PubMed] [Google Scholar]
- 48. Selten JP, van der Ven E, Termorshuizen F.. Migration and psychosis: a meta-analysis of incidence studies. Psychol Med. 2020;50(2):303–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Zeanah CH, Zeanah PD.. Intergenerational transmission of maltreatment—insights from attachment theory and research. Psychiatry. 1989;52(2):177–196. [DOI] [PubMed] [Google Scholar]
- 50. Iyengar U, Kim S, Martinez S, Fonagy P, Strathearn L.. Unresolved trauma in mothers: intergenerational effects and the role of reorganization. Front Psychol. 2014;5:966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hesse E, Main M.. Second‐generation effects of unresolved trauma in nonmaltreating parents: dissociated, frightened, and threatening parental behavior. Psychoanal Inq. 1999;19(4):481–540. [Google Scholar]
- 52. Bolhuis K, Steenkamp LR, Blanken LME, et al. Schizophrenia polygenic risk is associated with child mental health problems through early childhood adversity: evidence for a gene-environment correlation. Eur Child Adolesc Psychiatry. 2022;31:529–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Kendler KS, Baker JH.. Genetic influences on measures of the environment: a systematic review. Psychol Med. 2007;37(5):615–626. [DOI] [PubMed] [Google Scholar]
- 54. Vinkhuyzen AAE, van der Sluis S, de Geus EJC, Boomsma DI, Posthuma D.. Genetic influences on “environmental” factors. Genes Brain Behav. 2010;9(3):276–287. [DOI] [PubMed] [Google Scholar]
- 55. Dalvie S, Maihofer AX, Coleman JRI, et al. Genomic influences on self-reported childhood maltreatment. Transl Psychiatry. 2020;10(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Warrier V, Kwong ASF, Luo MN, et al. Gene-environment correlations and causal effects of childhood maltreatment on physical and mental health: a genetically informed approach. Lancet Psychiatry. 2021;8(5):373–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Sallis HM, Croft J, Havdahl A, et al. Genetic liability to schizophrenia is associated with exposure to traumatic events in childhood. Psychol Med. 2021;51(11):1814–1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Jaffee SR, Price TS.. The implications of genotype-environment correlation for establishing causal processes in psychopathology. Dev Psychopathol. 2012;24(4):1253–1264. [DOI] [PubMed] [Google Scholar]
- 59. Knafo A, Jaffee SR.. Gene-environment correlation in developmental psychopathology. Dev Psychopathol. 2013;25(1):1–6. [DOI] [PubMed] [Google Scholar]
- 60. Kong A, Thorleifsson G, Frigge ML, et al. The nature of nurture: effects of parental genotypes. Science. 2018;359(6374):424–428. [DOI] [PubMed] [Google Scholar]
- 61. Jaffee SR, Bowes L, Ouellet-Morin I, et al. Safe, stable, nurturing relationships break the intergenerational cycle of abuse: a prospective nationally representative cohort of children in the United Kingdom. J Adolesc Health. 2013;53(4):S4–S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Williams LM. Recall of childhood trauma: a prospective study of women’s memories of child sexual abuse. J Consult Clin Psychol. 1994;62(6):1167–1176. [DOI] [PubMed] [Google Scholar]
- 63. Kelleher I, Harley M, Murtagh A, Cannon M.. Are screening instruments valid for psychotic-like experiences? A validation study of screening questions for psychotic-like experiences using in-depth clinical interview. Schizophr Bull. 2011;37(2):362–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Rimvall MK, Gundersen S, Clemmensen L, et al. Evidence that self-reported psychotic experiences in children are clinically relevant. Schizophr Res. 2019;204:415–416. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.