Abstract
Introduction and importance
Surgeons may mistakenly consider the right hepatic duct as cystic duct, ligate, and divide it.
Case presentation
A 58-year-old woman presented with right upper quadrant (RUQ) abdominal pain, nausea, and RUQ tenderness, but negative Murphy's sign. Common bile duct was 10 mm based on abdominal ultrasound. Common hepatic duct and intrahepatic ducts consist of multiple common bile duct (CBD) stones with sludge and multiple small gallstones. Different diagnostic procedures (Computed tomography (CT) scan, magnetic resonance cholangiopancreatography (MRCP), and endoscopic retrograde cholangiopancreatography (ERCP)) showed the connection of the cystic duct to the right hepatic duct. Balloon sweeping for stones extraction and then laparoscopic cholecystectomy was successfully done.
Clinical discussion
Radiologic evaluations like MRCP, CT scan, ERCP or sonography before or during the surgery/endoscopic interventions seem logical at least for selected patients.
Conclusion
Before endoscopic/surgical interventions we need to be sure about the anatomy of biliary tree by a suitable para-clinic evaluation.
Keywords: Cystic duct, Hepatic duct, Endoscopic retrograde cholangiopancreatography, Magnetic resonance cholangiopancreatography, Computed tomography, Case report
Highlights
-
•
Drainage of the main right hepatic duct into the cystic duct is extremely rare.
-
•
No definite approach in biliary tree diseases for diagnosis of probable abnormalities
-
•
Do MRCP, CT scan, ERCP or sonography before/during surgical/endoscopic cholecystectomy
1. Introduction
This case study is reported in line with SCARE guidelines [1]. Knowledge about any anatomical variation in bile duct helps surgeons and endoscopists to decrease the chance of iatrogenic complication during the procedure [2]. Surgeons may mistakenly consider the right hepatic duct as cystic duct, ligate, and divide it [3]. Therefore, the patient may present with biliary fistula, biliary peritonitis, or cirrhosis of the liver at a later stage [4].
2. Presentation of case
The patient is a 58-year-old woman presented with right upper quadrant (RUQ) abdominal pain and nausea for ten days before being admitted to the hospital. Physical examination revealed tenderness in the RUQ without peritoneal signs. Murphy's sign was negative. The temperature was 36.5 °C and other vital signs were normal. Laboratory values showed a WBC: 12,100 (PMN: 75 %), total and direct bilirubin were 7.3 mg/dL and 4.1 mg/dL, respectively. Alanine aminotransferase was 162 U/L, aspartate aminotransferase: 101 U/L, alkaline phosphatase: 1090 U/L, amylase: 392 U/L, and lipase was 38 U/L. Abdominal ultrasound showed dilatation of common bile ducts (10 mm) and common hepatic duct and intrahepatic ducts consist of multiple common bile duct (CBD) stones with sludge and multiple small gallstones.
Computed tomography (CT) scan, magnetic resonance cholangiopancreatography (MRCP) (Fig. 1), and endoscopic retrograde cholangiopancreatography (ERCP) (Fig. 2) showed the connection of the cystic duct to the right hepatic duct.
Fig. 1.
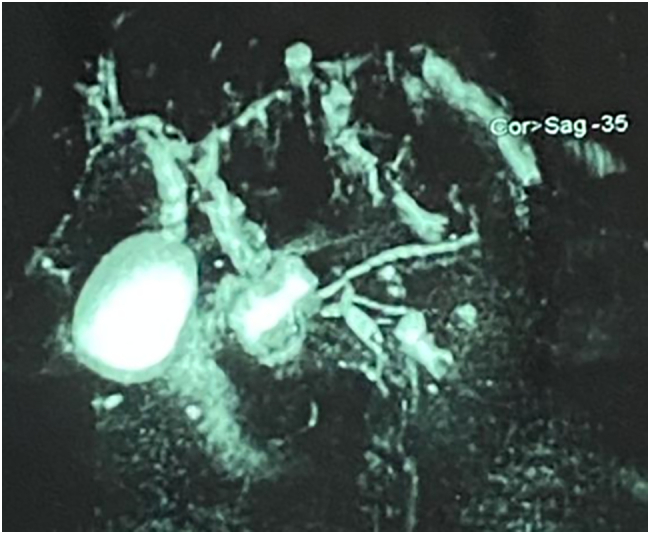
Magnetic resonance cholangiopancreatography (MRCP) showing the connection of the cystic duct to the right hepatic duct.
Fig. 2.

Endoscopic Retrograde Cholangiopancreatography (ERCP) showing the connection of the cystic duct to the right hepatic duct.
ERCP was requested and revealed choledocholithiasis with cystic duct variation (cystic duct was inserted to right hepatic duct) (Fig. 2).
Balloon sweeping for stones extraction and then laparoscopic cholecystectomy was successfully done.
Our literature review of similar cases showed both young and old involved patients, either black or white, with no preference in sex, with different clinical presentations like abdominal pain, fever, and/or jaundice and different accompanying symptoms and signs suspicious to pancreatitis, evidence of gall stones, with different laboratory findings like elevated serum amylase, evidence of cholestasis, either preoperatively or intraoperatively or both and with different diagnostic tools like sonography, CT scan, ERCP or MRCP [2], [3], [5], [6], [7], [8], [9].
3. Discussion
Drainage of the main right hepatic duct into the cystic duct is extremely rare and ranges from 0.3 to 0.4 % of patients [10]. Previous studies reported the prevalence of biliary duct anomalies as 12 %, with anomalous right hepatic duct emptying into the common hepatic or cystic duct as the most common one [11]. Although there are some reports about such aberrancies from the cystic duct to the right hepatic duct [2], [3], [5], [6], [7], [8], [9], cystic duct into the left hepatic duct [12], [13], [14], and even from the cystic duct to common hepatic duct [15], [16]. It seems important evaluating the biliary duct preoperatively and intraoperatively of probable aberrant biliary duct variations for preventing bile duct injury.
According to our literature review, there is no specific pattern or preferred diagnostic approach or tool in cases with biliary tree diseases for diagnosis of probable abnormalities, yet.
Studies on cadavers or livers before transplantation may better justify the exact prevalence of anomalies of the biliary tree [15].
Considering the common prevalence of anatomic variations in the biliary tree as mentioned in previous and newer studies [11], [17], cholecystectomy as the most prevalent surgery worldwide [18], many case reports of different anomalies as mentioned above [2], [3], [5], [6], [7], [8], [9], [12], [13], [14], [15], [16], variations of the cystic duct as the most important form of anomalies from the surgical point of view [19], elective nature of surgery or endoscopic diagnostic/therapeutic interventions in most cases of biliary tree diseases [20], and preventable disasters without knowing the anatomy of the biliary tree, it may be the time to reinforce radiologic evaluations like MRCP, CT scan, ERCP or sonography before such interventions before or during the surgery/endoscopic interventions.
4. Conclusions
It seems logical that physicians implement radiologic evaluations like MRCP, CT scan, ERCP or sonography, before either surgery or endoscopic interventions, at least for some selected patients.
Abbreviations
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Ethical approval is exempt at our institution.
Funding
N/A.
Guarantor
Dr Ali Kabir, Mahmoodreza Khoonsari and Abolfazl Namazi.
Research registration number
N/A.
CRediT authorship contribution statement
AN and AK: primary drafted
MK and MRM: critical revision.
All of them designed, revised and finally drafted the manuscript and guaranteed the manuscript.
Conflicts of interest
N/A.
Data availability statement
All data will be available by direct request from corresponding author.
References
- 1.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. International Journal of Surgery. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 2.Hathiramani V., Krishnan J., Raj V., Redkar R.G. Choledochal cyst with an aberrant right cholecysto-hepatic duct draining into cystic duct and a review of literature. J. Indian Assoc. Pediatr. Surg. 2016;21(4):205. doi: 10.4103/0971-9261.158101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hirao H., Okabe H., Ogawa D., Kuroda D., Taki K., Tomiyasu S., et al. A case of right hepatic duct entering cystic duct successfully treated by laparoscopic subtotal cholecystectomy through preoperatively placed biliary stent. Surg. Case Rep. 2020;6(1):221. doi: 10.1186/s40792-020-00994-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cachoeira E., Rivas A., Gabrielli C. Anatomic variations of extrahepatic bile ducts and evaluation of the length of ducts composing the cystohepatic triangle. Int. J. Morphol. 2012;30:279–283. doi: 10.4067/S0717-95022012000100050. [DOI] [Google Scholar]
- 5.Abe T., Ito S., Kaneda Y., Suto R., Noshima S. Main right hepatic duct entering the cystic duct: a case report. Surg. Case Rep. 2019;5(1):46. doi: 10.1186/s40792-019-0604-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Güngör F., Sür Y., Gür E., Dilek O.N. A rare anatomical variation of the bile ducts: cystic duct draining to the right hepatic duct. Turk. J. Gastroenterol. 2019;30(4):375–376. doi: 10.5152/tjg.2018.18321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rossi U.G., Ierardi A.M., Cariati M. Aberrant right hepatic duct and cystic duct joint drainage into the common hepatic duct. Rev. Gastroenterol. Mex. (Engl.) 2020;85(3):354–355. doi: 10.1016/j.rgmx.2019.08.010. [DOI] [PubMed] [Google Scholar]
- 8.Sofi A.A., Alaradi O.H., Abouljoud M., Nawras A.T. Aberrant right hepatic duct draining into the cystic duct: clinical outcomes and management. Gastroenterol. Res. Pract. 2011;2011 doi: 10.1155/2011/458915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suna N., Dişibeyaz S., Kuzu U.B., Yüksel M., Yıldız H., Kayaçetin E. Aberrant right posterior hepatic duct opening into the cystic duct: a very rarely seen biliary anatomic variation. Endoscopy. 2014;46(Suppl 1) doi: 10.1055/s-0034-1390843. UCTN:E657. [DOI] [PubMed] [Google Scholar]
- 10.Carbajo M.A., Martín del Omo J.C., Blanco J.I., Cuesta C., Martín F., Toledano M., et al. Congenital malformations of the gallbladder and cystic duct diagnosed by laparoscopy: high surgical risk. JSLS. 1999;3(4):319–321. PMID: 10694079. PMCID: PMC3015364. [PMC free article] [PubMed] [Google Scholar]
- 11.Berci G., Hamlin J.A. Wilhams & Wilkins; Baltimore: 1981. Operative Biliary Radiology. [DOI] [Google Scholar]
- 12.Contini S., Dalla Valle R., Zinicola R., Botta G.C. A further case of junction of the cystic duct into the left hepatic duct: a real risk for iatrogenic lesions of the bile ducts. Surg. Laparosc. Endosc. 1998;8(3):245–246. PMID: 9649055. [PubMed] [Google Scholar]
- 13.Fujita N., Shirai Y., Ohtani T., Tsukada K., Hirota M., Hatakeyama K. Junction of the cystic duct with the left hepatic duct: report of a case discovered during laparoscopic cholecystectomy. Surg. Laparosc. Endosc. 1996;6(6):445–447. PMID: 8948036. [PubMed] [Google Scholar]
- 14.Ozaslan E., Dağli N., Balkanci F., Bayraktar Y. Absence of the common bile duct and junction of the cystic duct with the left hepatic duct in a patient with chronic portal vein thrombosis. J. Clin. Gastroenterol. 2002;34(3):280–281. doi: 10.1097/00004836-200203000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Delić J., Savković A., Isaković E. Anatomic variations of the cystic duct and its junction with the common hepatic duct. Med. Arh. 2004;58(2):71–74. PMID: 15202309. [PubMed] [Google Scholar]
- 16.Kise Y., Uetsuji S., Takada H., Yamamura M., Yamamoto M. Dilatation of the cystic duct with its congenital low entry into the common hepatic duct. Am. J. Gastroenterol. 1990;85(6):769–770. PMID: 2353708. [PubMed] [Google Scholar]
- 17.Cawich S.O., Sinanan A., Deshpande R.R., Gardner M.T., Pearce N.W., Naraynsingh V. Anatomic variations of the intra-hepatic biliary tree in the Caribbean: a systematic review. World J. Gastrointest. Endosc. 2021;13(6):170–183. doi: 10.4253/wjge.v13.i6.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsu C.E., Lee K.T., Chang C.S., Chiu H.C., Chao F.T., Shi H.Y. Cholecystectomy prevalence and treatment cost: an 8-year study in Taiwan. Surg. Endosc. 2010;24(12):3127–3133. doi: 10.1007/s00464-010-1103-1. [DOI] [PubMed] [Google Scholar]
- 19.Andall R.G., Matusz P., du Plessis M., Ward R., Tubbs R.S., Loukas M. The clinical anatomy of cystic artery variations: a review of over 9800 cases. Surg. Radiol. Anat. 2016;38(5):529–539. doi: 10.1007/s00276-015-1600-y. [DOI] [PubMed] [Google Scholar]
- 20.Siegel J.H., Kasmin F.E. Biliary tract diseases in the elderly: management and outcomes. Gut. 1997;41(4):433–435. doi: 10.1136/gut.41.4.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data will be available by direct request from corresponding author.


