Abstract
Objectives:
To describe the incidence and presentation of pancreatitis in Children with Medical Complexity (CMC) while evaluating severity of disease and outlining risk factors.
Methods:
This was a retrospective chart review between January 2010 and December 2019 of patients seen in the complex care clinic at Nationwide Children’s Hospital (NCH) and Cincinnati Children’s Hospital Medical Center (CCHMC). Data collected included sex, underlying diagnosis, family history of pancreatitis, type of pancreatitis, signs/symptoms, abdominal imaging, severity of attack, and presence of various risk factors associated with pancreatitis. Severity and diagnosis of pancreatitis was determined based on North American Society for Pediatric Gastroenterology, Hepatology and Nutrition criteria.
Results:
One hundred and twelve patients from both institutions were included, 62% from NCH, median age 11.5 [interquartile range (IQR): 5–16 years], 50% male. Most patients were less than 18 years of age with a median age of 8 years (IQR: 4–13 years). Underlying diagnoses included seizures (67%), cerebral palsy/spastic quadriplegia (65%), diabetes (3.6%), and mitochondrial disease (3%). Majority of patients were found to have multiple underlying diagnoses (88%). Incidence of pancreatitis for both institutions was 336 of 100,000 patients/year which is significantly higher than the general pediatric population (P < 0.0001). Majority of first episodes of pancreatitis were mild (82%) with abdominal pain as the predominant symptom (50%). Adult patients were more likely to have pancreatitis related to medication use than pediatric patients (70% vs 38%, respectively P = 0.007).
Conclusions:
Individuals in the CMC population at our institutions have a high incidence of pancreatitis with unique risk factors compared to the general pediatric/young adult populations.
Keywords: children with medical complexity, incidence, pancreatitis, pediatric pancreatitis
The incidence of acute pancreatitis (AP) has stabilized at 1 per 10,000 children (1). Recent research identified unique aspects of pancreatitis in children compared to adults, including presentation, etiology, and prognosis. The most common etiologies for AP in the pediatric population are medication, infection, and trauma in contrast to biliary disease in adults (2,3). Most children with AP recover with no further sequelae; however, some will develop recurrent attacks [acute recurrent pancreatitis (ARP)] with a subset developing irreversible pancreatic damage consistent with chronic pancreatitis (CP). Additionally, up to 10% of children may present with CP without prior AP or ARP (4). Genetic variants play a strong role in recurrent or chronic pancreatic disease in children (5). Criteria for the diagnosis of AP and CP in children include symptom reporting along with biochemical and imaging findings. Symptom assessment can be difficult in very young children and in those with disorders limiting their ability to communicate. Children with Medical Complexity (CMC) are more likely to be exposed to medications and are less likely to be able to clearly communicate their pain. Genetic conditions may include pancreatic disease and physical disability may expose these individuals to procedures that also place them at risk for pancreatitis (6,7).
Nationwide Children’s Hospital (NCH) and Cincinnati Children’s Hospital Medical Center (CCHMC) offer specialized primary care clinics for individuals requiring medical care affecting multiple organ systems. These patients are generally referred to as Children with Medical complexity or “CMC” despite the fact that a significant proportion are 18 years of age or older. Due to their underlying diagnoses, these patients are often dependent on technologies such as enteral feeding tubes and mechanical ventilation. The CMC population faces unique challenges in the characterization, diagnosis, and management of pancreatitis.
Little has been published regarding the incidence of pancreatitis in the CMC population. We hypothesized these patients would have a higher incidence and more severe AP than the general pediatric population. Multiple risk factors for AP may also put this population at higher risk for recurrent AP and CP. The primary objective of this study was to describe the incidence, presentation, and diagnostic challenges of pancreatitis in CMC and into adulthood. The secondary objective was to evaluate the severity of pancreatitis and incidence of AP, ARP, and CP in this population, and potentially explicate lesser-known risk factors.
METHODS
This was a retrospective review between January 2010 and December 2019 of patients seen in the complex care clinics at NCH and CCHMC. The institutional review boards (IRB) approved this study (NCH IRB 00000240, CCHMC IRB 2020–0710). Subjects were enrolled and identified for further review based on several inclusion criteria including a diagnosis of AP, ARP, or CP (ICD-9 577.0 or 577.1 OR ICD-10 K86.1 or K85.9 on their problem list, admission diagnosis, or encounter diagnosis) an elevated lipase, or an elevated amylase. Data were collected from the electronic medical record systems utilized by NCH and CCHMC and recorded in Research Electronic Data Capture (REDCap).
Data collected from the patient’s chart included sex, institution, underlying diagnoses (eg, cerebral palsy, spastic quadriplegia, mitochondrial disorder, chromosomal abnormality, other), and any family history of pancreatitis. During the first encounter for pancreatitis, the following information was recorded: age, date of encounter, type of pancreatitis (acute, chronic, unknown), presenting signs and symptoms (abdominal pain, vomiting, diarrhea, feeding intolerance, other), abdominal imaging obtained during encounter, severity of attack (mild, moderate, severe) based on criteria published by the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (7), and the presence of various risk factors associated with pancreatitis including medications and structural abnormalities.
Diagnosis of AP was based on the presence of 2 or more of the following criteria: abdominal pain and symptoms characteristic of AP as defined using International Study Group of Pediatric Pancreatitis: In Search for a Cure (INSPPIRE) criteria (2,8,9). Moderately severe AP includes local pancreatic complications, exacerbation of previous comorbidity or the presence of transient (<48 hours) organ dysfunction, and severe AP includes the presence of persistent (>48 hours) systemic organ dysfunction as previously published (8). CP was defined per INSPPIRE and involves structural changes in the pancreas on imaging along with evidence of abdominal pain consistent with pancreatic origin, exocrine pancreatic insufficiency, or endocrine pancreatic insufficiency.
The episode was considered idiopathic if no specific cause or risk factor was identified.
Statistical Analysis
Data were analyzed using SAS®, version 9.4 (SAS Institute, Cary, NC). Due to skewed distributions, continuous data were summarized as medians with interquartile ranges (IQR: 25th–75th percentiles) while categorical data were summarized as frequency counts and percentages. For categorical data, Chi-square or Fisher’s exact tests were used, as appropriate, for group comparisons. A P value <0.05 was considered statistically significant.
RESULTS
Center Background Information
A total of 2129 patients (16,624 encounters) were seen at NCH and 1208 patients (19,464 encounters) at CCHMC between 2010 and 2019. The groups are similar in that the majority of patients have cerebral palsy, followed by feeding difficulties. See Table 1, Supplemental Digital Content, http://links.lww.com/MPG/C934, for further details.
A total of 163 charts were reviewed and 34 charts did not meet criteria for the diagnosis of acute, acute recurrent, or CP per INSPIRRE criteria and were not included in data analysis. Seventeen charts were excluded due to first episode of pancreatitis occurring before or after our allotted time frame or were seen at outside institutions (Figure 1, Supplemental Digital Content, http://links.lww.com/MPG/C934).
Demographics
A total of 112 CMC from both institutions were found to have the first episode of AP pancreatitis within our timeframe, 62% from NCH. Median age was 11.5 (IQR: 5–16 years), 50% were male. Underlying diagnoses included seizures (67%), cerebral palsy/spastic quadriplegia (65%), diabetes (3.6%), and mitochondrial disease (3%). Majority of patients were found to have multiple underlying diagnoses (88%). Only 2% of patients had a family history of pancreatitis, though many charts were missing this information. See Table 1 for further details. The incidence of pancreatitis was similar between the institutions with NCH 324 of 100,000 compared to CCHMC 356 of 100,000 unique patients per year during our study time frame. The overall incidence of pancreatitis for both institutions was 336 of 100,000 unique patients per year. This is significantly higher than the general pediatric population incidence published as between 3 and 13 of 100,000 patients, using 8 of 100,000 for comparison as a midpoint (P < 0.0001) (1,10).
TABLE 1.
Patient and first AP attack characteristics
| Patient characteristics | All N = 112 |
|---|---|
|
| |
| Institution | |
| NCH | 69 (62%) |
| CCHMC | 43 (38%) |
| Age, y, for first attack | 11.5 (5.0–16.0) [min–max: 0–36] |
| Sex (male) | 56 (50%) |
| Underlying diagnosis | |
| Cerebral palsy/spastic quadriplegia | 73 (65%) |
| Diabetes | 4 (3.6%) |
| Seizures | 75 (67%) |
| Mitochondrial disease | 3 (3%) |
| Chromosomal abnormalities | 26 (23%) |
| Other | 65 (58%) |
| Multiple underlying diagnoses | 99 (88%) |
| Family history of pancreatitis | |
| Yes | 2 (2%) |
| No | 84 (75%) |
| Unknown | 26 (23%) |
| First AP attack characteristics | |
| Classification of pancreatitis (first attack) | |
| Acute pancreatitis | 110 (98%) |
| Chronic pancreatitis | 2 (2%) |
| Age, y, by diagnosis | |
| Acute pancreatitis | 12.0 (5.0–16.0) |
| Chronic pancreatitis | 7.5 (7.0–8.0) |
| Signs and symptoms | |
| Abdominal pain | 56 (50%) |
| Vomiting | 38 (34%) |
| Diarrhea | 21 (19%) |
| Feeding intolerance | 25 (22%) |
| Other | 69 (62%) |
| Multiple signs and symptoms | 82 (73%) |
| Imaging | |
| CT | 41 (37%) |
| Ultrasound | 58 (52%) |
| MRI | 5 (4%) |
| None | 18 (16%) |
| Any imaging | 94 (84%) |
| Multiple imaging | 10/94 (11%) |
| Imaging show pancreatitis | |
| Yes | 22/94 (23%) |
| No | 72/94 (77%) |
| Severity of attack | |
| Mild | 92 (82%) |
| Moderate | 6 (5%) |
| Severe | 14 (13%) |
Data presented as n (%) or median (25th–75th percentile) [min–max]. AP = acute pancreatitis; CCHMC = Cincinnati Children’s Hospital Medical Center; CT = computed tomography; MRI = magnetic resonance imaging; NCH = Nationwide Children’s Hospital.
First Attack
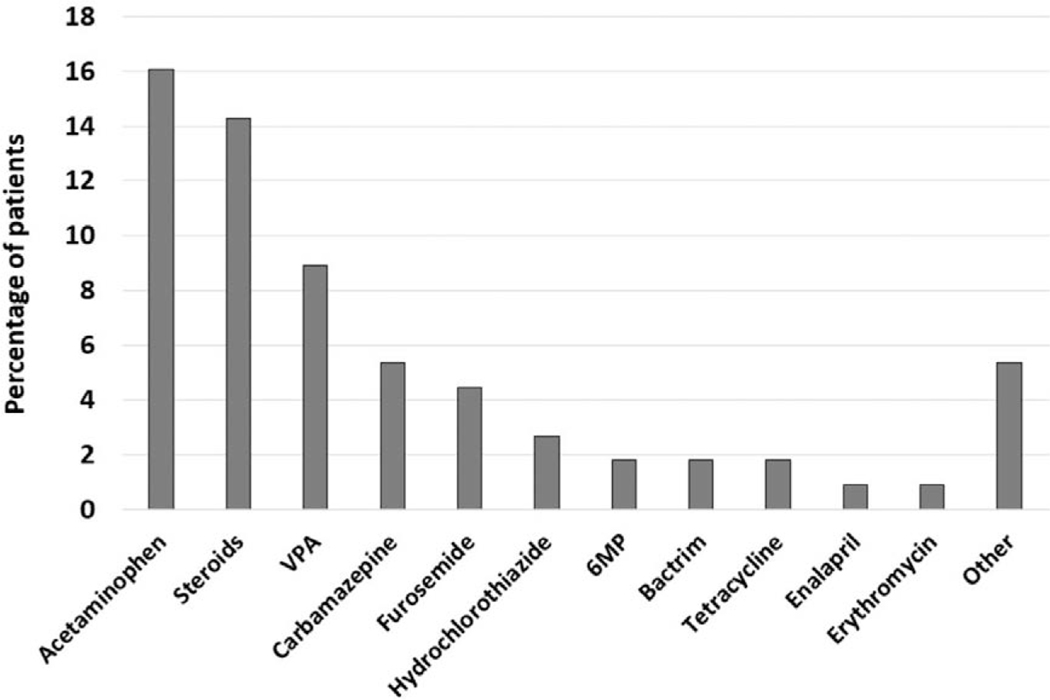
The majority first episodes of pancreatitis were mild (82%). Abdominal pain was the predominant symptom (50%) with vomiting as the second most common symptom (34%). Most patients had abdominal imaging (84%) and 11% (10/94) had multiple imaging. See Table 1 for further details. Structural abnormalities and chronic renal failure contributed to the etiology of AP in 14% and 13% of patients, respectively. Only 8% were felt to have an infectious etiology. Triglycerides greater than 1000 mg/dL were found in 19% of patients, whereas only 1% of patients were found to have significantly elevated calcium (greater than 12 mg/dL) at time of diagnosis. Nineteen percent of patients had spinal/abdominal surgery within 30 days of the pancreatitis episode. Forty-five percent of patients were on at least one medication associated with pancreatitis with 28% being on more than one medication associated with pancreatitis development (Fig. 1). Less than half (42%) of patients were deemed to have idiopathic pancreatitis. Three patients were evaluated with genetic testing that included PRSS1, SPINK1, CASR, CTRC, and CFTR, but none were found to have a genetic risk factor for pancreatitis. No patients had a sweat chloride test performed. Only 4% (4/112) had pancreatic fecal elastase tested and half had values consistent with pancreatic exocrine insufficiency.
FIGURE 1.
List of medications in use at time of pancreatitis diagnosis.
Pediatric Versus Adult Patients
Eighty-nine patients (79%) were less than or equal to 18 years of age and 23 (21%) were greater than 18 years of age. Median age of pediatric patients was 8 years (IQR: 4–13 years) and for adults 25 years (IQR: 20–27 years; Table 2). There was no significant difference in sex between pediatric and adult patients (P = 0.82). Underlying diagnoses were similar but more adult patients were diagnosed with cerebral palsy/spastic quadriplegia (83% vs 61%, P = 0.054) and seizure disorder (83% vs 63%, P = 0.09). The majority of both pediatric and adult patients had multiple underlying diagnoses (87% pediatric, 95% adult patients, P = 0.30).
TABLE 2.
Patient characteristics for pediatric vs adults
| ≤18 years old N = 89 | >18 years old N = 23 | P value | |
|---|---|---|---|
|
| |||
| Institution | NA | ||
| NCH | 50 (56%) | 19 (83%) | |
| CCHMC | 39 (44%) | 4 (17%) | |
| Age, y, for first AP attack | 8.0 (4.0–13.0) [min–max: 0–18] | 25.0 (20.0–27.0) [min–max: 19–36] | NA |
| Sex (male) | 44 (49%) | 12 (52%) | 0.82 |
| Underlying diagnosis | |||
| Cerebral palsy/spastic quadriplegia | 54 (61%) | 19 (83%) | 0.054 |
| Diabetes | 1 (1%) | 3 (13%) | 0.03 |
| Seizures | 56 (63%) | 19 (83%) | 0.09 |
| Mitochondrial disease | 3 (3%) | 0 (0%) | 1.00 |
| Chromosomal abnormalities | 18 (20%) | 8 (35%) | 0.14 |
| Other | 54 (61%) | 11 (48%) | 0.27 |
| Multiple underlying diagnoses | 77 (87%) | 22 (96%) | 0.30 |
| Family history of pancreatitis | |||
| Yes | 0/74 (0%) | 2/12 (17%) | 0.02 |
| No | 74/74 (100%) | 10/12 (83%) | |
| Classification of pancreatitis (first attack) | |||
| Acute pancreatitis | 87 (98%) | 23 (100%) | 1.00 |
| Chronic pancreatitis | 2 (2%) | 0 (0%) | |
| Age, y, by first attack diagnosis | |||
| Acute pancreatitis | 9.0 (4.0–13.0) | 25.0 (20.0–27.0) | NA |
| Chronic pancreatitis | 7.5 (7.0–8.0) | - | |
| Signs and symptoms | |||
| Abdominal pain | 43 (48%) | 13 (57%) | 0.48 |
| Vomiting | 31 (35%) | 7 (30%) | 0.69 |
| Diarrhea | 15 (17%) | 6 (26%) | 0.37 |
| Feeding intolerance | 20 (22%) | 5 (22%) | 1.00 |
| Other | 55 (62%) | 14 (61%) | 0.94 |
| Multiple signs and symptoms | 66 (74%) | 16 (70%) | 0.66 |
| Imaging | |||
| CT | 31 (35%) | 10 (43%) | 0.44 |
| Ultrasound | 47 (53%) | 11 (48%) | 0.67 |
| MRI | 3 (3%) | 2 (9%) | 0.27 |
| None | 15 (17%) | 3 (13%) | 1.00 |
| Any imaging | 74 (83%) | 20 (87%) | 1.00 |
| Multiple imaging | 7/74 (9%) | 3/20 (15%) | 0.44 |
| Imaging show pancreatitis | 0.39 | ||
| Yes | 19/74 (26%) | 3/20 (15%) | |
| No | 55/74 (74%) | 17/20 (85%) | |
| Severity of first attack | 0.89 | ||
| Mild | 72 (81%) | 20 (87%) | |
| Moderate | 5 (6%) | 1 (4%) | |
| Severe | 12 (13%) | 2 (9%) | |
| Eventual diagnosis | 0.052 | ||
| AP | 71 (80%) | 15 (65%) | |
| ARP | 15 (17%) | 4 (17%) | |
| CP | 3 (3%) | 4 (17%) | |
Data presented as n (%) or median (25th–75th percentile) [minim–max]. AP = acute pancreatitis; ARP = acute recurrent pancreatitis; CCHMC = Cincinnati Children’s Hospital Medical Center; CP = chronic pancreatitis; NA = not applicable; NCH = Nationwide Children’s Hospital.
First Attack Comparison in Pediatric Versus Adult Patients
Symptoms were similar between pediatric and adult patients. Adult patients tended to have more cross-sectional imaging though the difference was not significant (Computed tomography scans 43% adult vs 35% pediatric, P = 0.44 and MRIs 9% adult vs 3% pediatric, P = 0.27). Severity of the first attack was similar and the majority were found to have mild disease (81% vs 87%, P = 0.89).
Significantly more adult patients received medications with increased risk of pancreatitis (70%) than pediatric patients (38%; P = 0.007). There was a trend for adult patients to more likely have a structural etiology, primarily gallstones, compared to pediatric patients, but the difference was not significant. Adult patients were more likely to develop CP during follow-up (17% vs 3%, P = 0.052; Table 2).
DISCUSSION
In this study, we evaluated the incidence and characteristics of pancreatitis in the complex care population clinic. Previous literature reports the incidence of pediatric pancreatitis as roughly 8 of 100,000 patients per year with increasing likelihood of developing AP or CP with age (1,10). Our patient cohort exhibits a significantly higher incidence of pancreatitis (336/100,000) compared to the general pediatric population (an increase of over 40× the general population). Medical providers for the CMC population should be aware of this especially as these patients face challenges in communicating pain.
Our study also found that most patients in the CMC population with AP had mild disease with the first episode and only 2% of patients were found to have changes consistent with CP with their first attack (8). The relationship between ARP and CP and frequency of CP as the initial diagnosis of pancreatitis is unclear and incompletely defined in prior literature (11–15). The incidence of CP in this cohort, although similar to prior literature, is possibly due to the underlying nature of the patients’ comorbid conditions and inability to communicate effectively (1). This may confuse the clinical picture for AP attacks before diagnosis in the CMC population. Although most of our patients received a form of imaging to aid in diagnosis of pancreatitis, only a quarter had imaging findings consistent with pancreatitis, which can cause further diagnostic difficulties.
Half of our patients presented with signs or symptoms felt to indicate abdominal pain. As many of these patients are limited in their ability to communicate, this diagnosis likely relied heavily on caregiver interpretation. Vomiting was also prevalent in a third of patients as a more objective symptom. There was a wide variety in patient’s symptoms which constituted over half of the patients including “abdominal distention,” “agitation,” “altered mental status/increased seizures,” “fever/tachycardia/respiratory distress,” and a small number of patients without symptoms. As abdominal pain has been previously defined as 1 of 3 requirements in diagnosing AP, these “other” symptoms are somewhat unique to this population and may be an important reminder for providers to further investigate and maintain an index of suspicion for pancreatitis (9).
Although this patient cohort has many of the same possible risk factors known to the general pediatric population for pancreatitis such as infections, autoimmune diseases, structural abnormalities, and renal injury, many are also on multiple medications. Drug-induced pancreatitis has been previously published in the literature as the most common etiology in first attack AP in children (16–18). Interestingly, in our cohort, the majority of adult patients as compared to less than half of the pediatric group were on a medication with known risk for developing pancreatitis. This is likely due to multiple diagnosed co-morbidities (cerebral palsy, seizures, etc) traditionally requiring polypharmacy. However, it is unclear in our patient cohort if medications alone were the etiology of their pancreatitis episodes due to multiple risk factors that may contribute. For example, the not insignificant incidence of abdominal/spinal surgeries, also increases this population’s risk for postoperative mechanical, vascular, abnormal duodenal motility, or anatomic obstruction of the sphincter of Oddi (19–20). Further prospective research is needed to determine medication and other risk outcomes in this population.
There are several limitations to our study due to its retrospective design. Several charts were removed initially due to incorrect pancreatitis diagnosis based on current definitions. Although we were able to collect data centered on risk factors to further characterize pancreatitis in this population, further research is needed to assess outcomes and causation. However, we are the first to describe pancreatitis in a CMC population through a multicenter approach. We plan to further elaborate on our data by characterizing recurrent episodes of pancreatitis in this group.
CONCLUSIONS
In conclusion, pancreatitis is a diagnosis that is becoming more recognized in pediatrics and appears to be significantly more common in the medically complex population. We have outlined the incidence, signs, and symptoms and risks of pancreatitis in this population. Further prospective research is needed to determine outcomes in this population.
Supplementary Material
What Is Known.
The incidence of pancreatitis in the pediatric population has stabilized over time.
Medication-induced pancreatitis and infections are the leading causes of pancreatitis in pediatrics.
What Is New.
Children with medical complexity have not been previously studied for incidence, presentation, or severity of pancreatitis.
The incidence of pancreatitis in the medically complex population at our institutions is higher and presentation varies slightly compared to general pediatric patients.
When evaluated by age, adult patients were found to have more medication induced pancreatitis than pediatric patients.
Acknowledgments
M.A.-E.-H. is supported by NIDDK, grant number K23DK118190. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. G.N. has served as a medical advisor to Sarepta.
Footnotes
The remaining authors report no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jpgn.org).
REFERENCES
- 1.Sellers ZM, MacIsaac D, Yu H, et al. Nationwide trends in acute and chronic pancreatitis among privately insured children and nonelderly adults in the United States, 2007–2014. Gastroenterology 2018;155:469–78.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Husain SZ, Srinath AI. What’s unique about acute pancreatitis in children: risk factors, diagnosis and management. Nat Rev Gastroenterol Hepatol 2017;14:366–72. [DOI] [PubMed] [Google Scholar]
- 3.Suzuki M, Sai JK, Shimizu T. Acute pancreatitis in children and adolescents. World J Gastrointest Pathophysiol 2014;5:416–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abu-El-Haija M, Lowe M, Barth B, et al. Pediatric chronic pancreatitis without prior acute or acute recurrent pancreatitis: a report from the INSPPIRE consortium. Pancreatology 2020;20:781–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ellery KM, Uc A. Recurrent pancreatitis in children: past, present, and future. J Pediatr Gastroenterol Nutr 2020;70:413–6. [DOI] [PubMed] [Google Scholar]
- 6.Verhofste BP, Berry JG, Miller PE, et al. Risk factors for gastrointes-tinal complications after spinal fusion in children with cerebral palsy. Spine Deform 2021;9:567–78. [DOI] [PubMed] [Google Scholar]
- 7.Cohen E, Kuo DZ, Agrawal R, et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics 2011;127:529–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abu-El-Haija M, Kumar S, Szabo F, et al. Classification of acute pancreatitis in the pediatric population: clinical report from the NASPGHAN pancreas committee. J Pediatr Gastroenterol Nutr 2017;64:984–90. [DOI] [PubMed] [Google Scholar]
- 9.Morinville VD, Husain SZ, Bai H, et al. Definitions of pediatric pancreatitis and survey of present clinical practices. J Pediatr Gastroenterol Nutr 2012;55:261–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nydegger A, Heine RG, Ranuh R, et al. Changing incidence of acute pancreatitis: 10-year experience at the Royal Children’s Hospital, Melbourne. J Gastroenterol Hepatol 2007;22:1313–6. [DOI] [PubMed] [Google Scholar]
- 11.Beyer G, Habtezion A, Werner J, et al. Chronic pancreatitis. Lancet 2020;396:499–512. [DOI] [PubMed] [Google Scholar]
- 12.Machicado JD, Dudekula A, Tang G, et al. Period prevalence of chronic pancreatitis diagnosis from 2001–2013 in the commercially insured population of the United States. Pancreatology 2019;19:813–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yadav D, Timmons L, Benson JT, et al. Incidence, prevalence, and survival of chronic pancreatitis: a population-based study. Am J Gastroenterol 2011;106:2192–9. [DOI] [PubMed] [Google Scholar]
- 14.Hori Y, Vege SS, Chari ST, et al. Classic chronic pancreatitis is associated with prior acute pancreatitis in only 50% of patients in a large single-institution study. Pancreatology 2019;19:224–9. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed Ali U, Issa Y, Hagenaars JC, et al. Risk of recurrent pancreatitis and progression to chronic pancreatitis after a first episode of acute pancreatitis. Clin Gastroenterol Hepatol 2016;14:738–46. [DOI] [PubMed] [Google Scholar]
- 16.Abu-El-Haija M, Hornung L, Lin TK, et al. Drug induced pancreatitis is the leading known cause of first attack acute pancreatitis in children. Pancreatology 2020;20:1103–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Badalov N, Baradarian R, Iswara K, et al. Drug-induced acute pancreatitis: an evidence-based review. Clin Gastroenterol Hepatol 2007;5:648–61; quiz 644. [DOI] [PubMed] [Google Scholar]
- 18.Trivedi CD, Pitchumoni CS. Drug-induced pancreatitis: an update. J Clin Gastroenterol 2005;39:709–16. [DOI] [PubMed] [Google Scholar]
- 19.Sharbidre KG, Galgano SJ, Morgan DE. Traumatic pancreatitis. Abdom Radiol (NY) 2020;45:1265–76. [DOI] [PubMed] [Google Scholar]
- 20.Carter AE. Post-operative pancreatitis. Postgrad Med J 1956;32:248–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.